Summary.
What is already known about this topic?
CDC and the Advisory Committee on Immunization Practices recommend that health care personnel (HCP) receive an annual influenza vaccine and stay up to date with recommended COVID-19 vaccination.
What is added by this report?
During the 2022–23 influenza season, influenza vaccination coverage was 81% among HCP at acute care hospitals and 47% among those at nursing homes. Up-to-date COVID-19 vaccination coverage was 17% among HCP at acute care hospitals and 23% among those at nursing homes.
What are the implications for public health practice?
There is a need to promote evidence-based strategies to improve vaccination coverage among HCP. Tailored strategies might be useful to reach all HCP with recommended vaccines to protect them and their patients from vaccine-preventable respiratory diseases.
Abstract
The Advisory Committee on Immunization Practices recommends that health care personnel (HCP) receive an annual influenza vaccine and that everyone aged ≥6 months stay up to date with recommended COVID-19 vaccination. Health care facilities report vaccination of HCP against influenza and COVID-19 to CDC’s National Healthcare Safety Network (NHSN). During January–June 2023, NHSN defined up-to-date COVID-19 vaccination as receipt of a bivalent COVID-19 mRNA vaccine dose or completion of a primary series within the preceding 2 months. This analysis describes influenza and up-to-date COVID-19 vaccination coverage among HCP working in acute care hospitals and nursing homes during the 2022–23 influenza season (October 1, 2022–March 31, 2023). Influenza vaccination coverage was 81.0% among HCP at acute care hospitals and 47.1% among those working at nursing homes. Up-to-date COVID-19 vaccination coverage was 17.2% among HCP working at acute care hospitals and 22.8% among those working at nursing homes. There is a need to promote evidence-based strategies to improve vaccination coverage among HCP. Tailored strategies might also be useful to reach all HCP with recommended vaccines and protect them and their patients from vaccine-preventable respiratory diseases.
Introduction
Vaccination of health care personnel (HCP) is a critical strategy to minimize transmission of infection in health care settings (1,2). HCP are at high risk for work-related exposure to viruses such as influenza and SARS-CoV-2 but are less likely to transmit these infections when they are vaccinated (3). The Advisory Committee on Immunization Practices (ACIP) recommends that HCP receive an annual influenza vaccine (4). ACIP also recommends that persons aged ≥6 months stay up to date with recommended COVID-19 vaccination.† The Centers for Medicare & Medicaid Services (CMS) monitors the implementation of these recommendations by requiring health care facilities such as nursing homes and acute care hospitals to report influenza§ and COVID-19¶ vaccination coverage among HCP** to CDC’s National Healthcare Safety Network (NHSN). This study examined influenza and up-to-date COVID-19 vaccination coverage among HCP working in acute care hospitals and nursing homes during the 2022–23 influenza season.
Methods
Data Collection
Acute care hospitals and nursing homes report data to NHSN according to surveillance protocols for influenza and COVID-19 vaccination. Acute care hospitals and nursing homes began reporting COVID-19 vaccination among HCP in 2021; nursing homes were required to report influenza vaccination among HCP for the first time during the 2022–23 influenza season.†† To assess influenza vaccination coverage, facilities are required to report an annual count of HCP working in the facility for ≥1 day during an influenza season (October 1–March 31)§§ and the number of HCP who 1) received influenza vaccination, 2) had a medical contraindication to influenza vaccination, 3) declined vaccination, and 4) had unknown vaccination status. The protocol for COVID-19 vaccination coverage includes parallel data fields for COVID-19; however, data collection occurs at a different cadence. Nursing homes and acute care facilities report on schedules mandated by their respective regulatory programs at CMS. Nursing homes submit COVID-19 vaccination coverage weekly¶¶; acute care facilities submit ≥1 week of data per month.*** Both types of facilities report COVID-19 vaccination coverage data among HCP who were eligible to work in the facility ≥1 day during the reporting week.
Data Analysis
To assess HCP vaccination coverage during the 2022–23 influenza season, analyses were conducted using influenza and up-to-date COVID-19 coverage data (specifically, up-to-date COVID-19 coverage data from the week ending March 26, 2023, or the last submitted week of data) reported to NHSN. NHSN defined up-to-date COVID-19 vaccination as the receipt of a bivalent booster dose or completion of a primary series within the previous 2 months (i.e., not yet eligible to receive a bivalent vaccine).††† Facilities reporting data for both vaccine types and employing at least five HCP were included in the analysis. Pooled mean influenza and up-to-date COVID-19 vaccination coverage rates were calculated as the number of HCP who had received each recommended vaccine or vaccination series divided by the number of HCP working in all facilities. HCP reported to have a medical contraindication to COVID-19 vaccination were subtracted from the denominator of the up-to-date COVID-19 vaccination coverage calculation, to align with the measure adopted by CMS’s quality reporting programs.§§§ Coverage with each vaccine was calculated for HCP working at each facility type (nursing home or acute care hospital). Results were further stratified by employment category (employee, licensed practitioner, and student or volunteer); rural-urban classification (rural or urban)¶¶¶; county-level social vulnerability index (SVI) tertile****; facility size tertile††††; state; and U.S. region.§§§§ Counties in a lower SVI tertile are less socially vulnerable than are those in an upper SVI tertile. All analyses were conducted using SAS (version 9.4; SAS Institute). This activity was reviewed by CDC, deemed not research, and was conducted consistent with applicable federal law and CDC policy.¶¶¶¶
Results
Influenza Vaccination Coverage
Among approximately 8.4 million HCP working in 4,057 acute care hospitals, influenza vaccination coverage was 81.0% overall (Table 1); coverage was lowest (67.2%) among nonemployee licensed practitioners and was substantially higher among employees (83.1%) and nonemployee students and volunteers (85.2%). Among HCP working in acute care hospitals, influenza vaccination coverage was highest in the Midwest (84.7%) and lowest in the Pacific region (74.4%).
TABLE 1. Pooled mean influenza vaccination coverage among health care personnel working at acute care hospitals and nursing homes, by facility type — National Healthcare Safety Network, United States, October 1, 2022–March 31, 2023*.
| Characteristic | Influenza vaccination coverage |
|||||||
|---|---|---|---|---|---|---|---|---|
| Nursing homes |
Acute care hospitals |
|||||||
| No. of facilities | No. of vaccinated HCP | No. of HCP | Coverage, % | No. of facilities | No. of vaccinated HCP | No. of HCP | Coverage, % | |
|
Total
|
13,794
|
956,149
|
2,030,770
|
47.1
|
4,057
|
6,854,771
|
8,465,804
|
81.0
|
|
Staff member type
| ||||||||
| Employee |
13,794 |
844,380 |
1,832,394 |
46.1 |
4,054 |
5,245,329 |
6,315,763 |
83.1 |
| Nonemployee licensed practitioner |
11,365 |
61,060 |
110,432 |
55.3 |
3,695 |
828,669 |
1,234,011 |
67.2 |
| Nonemployee student or volunteer |
4,500 |
50,709 |
87,944 |
57.7 |
3,447 |
780,773 |
916,030 |
85.2 |
|
Facility size†
| ||||||||
| Small |
4,573 |
156,855 |
327,271 |
47.9 |
1,352 |
351,836 |
455,343 |
77.3 |
| Medium |
4,614 |
269,800 |
585,075 |
46.1 |
1,352 |
1,268,677 |
1,648,273 |
77.0 |
| Large |
4,607 |
529,494 |
1,118,424 |
47.3 |
1,353 |
5,234,258 |
6,362,188 |
82.3 |
|
Urbanicity
§
| ||||||||
| Rural |
3,817 |
191,508 |
426,368 |
44.9 |
1,173 |
659,881 |
824,714 |
80.0 |
| Urban |
9,977 |
764,641 |
1,604,402 |
47.7 |
2,884 |
6,194,890 |
7,641,090 |
81.1 |
|
Social vulnerability index
¶
| ||||||||
| Low |
4,724 |
333,282 |
660,593 |
50.5 |
1,228 |
2,030,870 |
2,437,031 |
83.3 |
| Medium |
4,605 |
332,622 |
725,843 |
45.8 |
1,341 |
2,463,062 |
3,086,676 |
79.8 |
| High |
4,463 |
290,129 |
644,194 |
45.0 |
1,487 |
2,360,245 |
2,941,443 |
80.2 |
|
Region** | ||||||||
| Midwest |
4,476 |
247,750 |
584,925 |
42.4 |
1,034 |
1,747,029 |
2,061,455 |
84.7 |
| Mountain |
484 |
38,160 |
64,260 |
59.4 |
200 |
330,765 |
398,865 |
82.9 |
| Northeast |
2,291 |
250,904 |
436,621 |
57.5 |
573 |
1,333,833 |
1,620,573 |
82.3 |
| Pacific |
1,421 |
126,090 |
206,518 |
61.1 |
471 |
854,017 |
1,148,524 |
74.4 |
| South | 5,122 | 293,245 | 738,446 | 39.7 | 1,779 | 2,589,127 | 3,236,387 | 80.0 |
Abbreviation: HCP = health care personnel.
* Each facility reported summary influenza vaccination data among HCP working in the facility for ≥1 day during October 1, 2022–March 31, 2023. Up-to-date COVID-19 vaccination coverage was reported to National Healthcare Safety Network each week; data from the week ending March 26, 2023, or the last submitted week of data, were used for analysis.
† Facility size was calculated separately for acute care hospitals and nursing homes and was based on the tertile distribution of the total number of staff members per facility.
§ https://www.cdc.gov/nchs/data_access/urban_rural.htm
¶ https://www.atsdr.cdc.gov/placeandhealth/svi/index.html
** South: Alabama, Arizona, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, New Mexico, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia; Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin; Mountain: Colorado, Idaho, Montana, Nevada, Utah, and Wyoming; Pacific: Alaska, California, Hawaii, Oregon, and Washington; Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont.
Among approximately 2.0 million HCP working in 13,794 nursing homes, influenza vaccination coverage was 47.1% overall; coverage was lowest among employees (46.1%) and substantially higher among nonemployee licensed practitioners (55.3%) and nonemployee students and volunteers (57.7%). Among HCP working in nursing homes, influenza vaccination coverage was highest in the Pacific region (61.1%) and lowest in the South (39.7%). Influenza vaccination coverage among HCP was similar across facility size, urban-rural status, and SVI for both nursing homes and acute care hospitals. Nursing homes in six states reported influenza vaccination coverage of ≥75% among HCP, whereas this level of coverage was reported in acute care hospitals in 40 states (Figure) (Supplementary Table, https://stacks.cdc.gov/view/cdc/134928).
FIGURE.
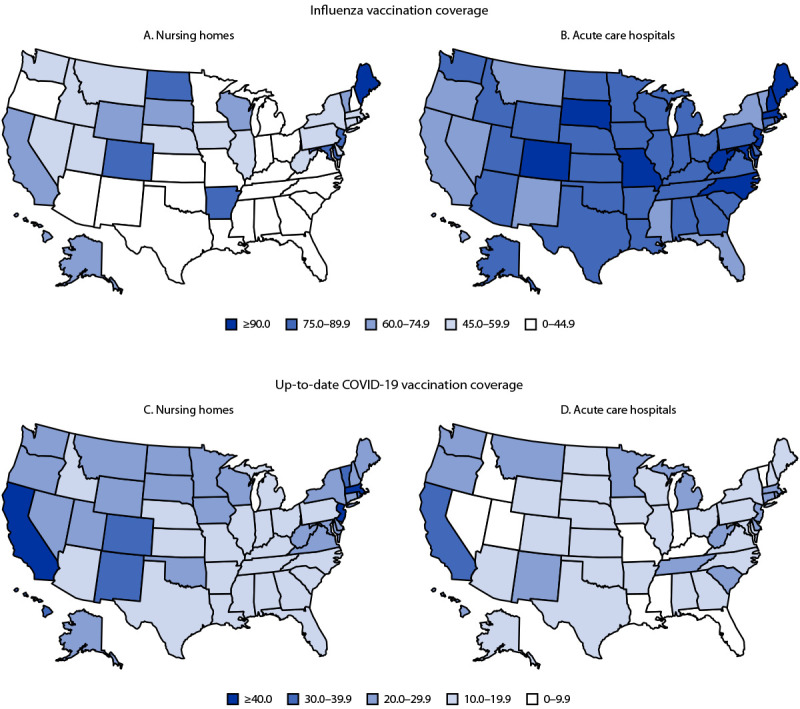
Percentage of pooled mean influenza vaccination coverage (A and B) and up-to-date COVID-19 vaccination*,† coverage (C and D) among health care personnel working at nursing homes (A and C) and acute care hospitals (B and D), by facility type and U.S. state — National Healthcare Safety Network, United States, October 1, 2022–March 31, 2023
* Up-to-date COVID-19 vaccination coverage was defined by the National Healthcare Safety Network during the study period as the receipt of a bivalent booster dose, completion of a primary series, or receipt of a monovalent booster dose within the previous 2 months.
† Each facility reported summary influenza vaccination data among health care personnel working in the facility for ≥1 day during October 1, 2022–March 31, 2023. Up-to-date COVID-19 vaccination coverage was reported to the National Healthcare Safety Network each week; data from the week ending March 26, 2023, or the last week of submitted data, were used for analysis.
Up-to-Date COVID-19 Vaccination Coverage
Among approximately 7.7 million HCP working in 4,057 acute care hospitals, up-to-date COVID-19 vaccination coverage was 17.2% overall (Table 2) and was highest in the Pacific region (28.9%) and lowest in the Mountain region (9.1%). No substantial differences by staff member type or urbanicity were observed.
TABLE 2. Pooled mean up-to-date COVID-19 vaccination coverage* among health care personnel working at nursing homes and acute care hospitals, by facility type — National Healthcare Safety Network, United States, October 1, 2022–March 31, 2023†.
| Characteristic | Up-to-date COVID-19 vaccination coverage |
|||||||
|---|---|---|---|---|---|---|---|---|
| Nursing homes |
Acute care hospitals |
|||||||
| No. of facilities | No. of vaccinated HCP | Total no. of HCP | Coverage, % | No. of facilities | No. of vaccinated HCP | Total no. of HCP | Coverage, % | |
|
Total
|
13,794
|
376,837
|
1,652,744
|
22.8
|
4,057
|
1,328,820
|
7,725,167
|
17.2
|
|
Staff member type
| ||||||||
| Employee |
13,794 |
341,672 |
1,523,365 |
22.4 |
4,051 |
1,029,896 |
5,879,220 |
17.5 |
| Nonemployee licensed practitioner |
10,006 |
25,372 |
89,975 |
28.2 |
3,496 |
199,869 |
1,203,932 |
16.6 |
| Nonemployee student or volunteer |
3,522 |
9,793 |
39,404 |
24.9 |
3,148 |
99,055 |
642,015 |
15.4 |
|
Facility size
§
| ||||||||
| Small |
4,573 |
76,018 |
309,005 |
24.6 |
1,352 |
70,547 |
448,596 |
15.7 |
| Medium |
4,614 |
116,077 |
494,368 |
23.5 |
1,352 |
228,176 |
1,540,690 |
14.8 |
| Large |
4,607 |
184,742 |
849,371 |
21.8 |
1,353 |
1,030,097 |
5,735,881 |
18.0 |
|
Urbanicity
¶
| ||||||||
| Rural |
3,817 |
60,121 |
343,954 |
17.5 |
1,173 |
109,089 |
745,548 |
14.6 |
| Urban |
9,977 |
316,716 |
1,308,790 |
24.2 |
2,884 |
1,219,731 |
6,979,619 |
17.5 |
|
Social vulnerability index** | ||||||||
| Low |
4,724 |
125,753 |
544,753 |
23.1 |
1,228 |
415,883 |
2,247,508 |
18.5 |
| Medium |
4,605 |
130,598 |
591,079 |
22.1 |
1,341 |
472,906 |
2,816,438 |
16.8 |
| High |
4,463 |
120,463 |
516,798 |
23.3 |
1,487 |
439,848 |
2,660,648 |
16.5 |
|
Region
††
| ||||||||
| Midwest |
4,476 |
91,258 |
475,948 |
19.2 |
1,034 |
291,758 |
1,811,254 |
16.1 |
| Mountain |
484 |
13,227 |
49,615 |
26.7 |
200 |
33,396 |
365,336 |
9.1 |
| Northeast |
2,291 |
101,633 |
381,642 |
26.6 |
573 |
289,194 |
1,515,844 |
19.1 |
| Pacific |
1,421 |
70,245 |
172,738 |
40.7 |
471 |
308,765 |
1,066,996 |
28.9 |
| South | 5,122 | 100,474 | 572,801 | 17.5 | 1,779 | 405,707 | 2,965,737 | 13.7 |
Abbreviations: HCP = health care personnel.
* COVID-19 up-to-date coverage was defined by National Healthcare Safety Network during the study period as the receipt of a bivalent booster dose or completion of a primary series or receipt of a monovalent booster dose within the previous 2 months.
† Each facility reported summary influenza vaccination data among HCP working in the facility for ≥1 day during October 1, 2022–March 31, 2023. Up-to-date COVID-19 vaccination coverage was reported to National Healthcare Safety Network each week; data from the week ending March 26, 2023, or the last submitted week of data, were used for analysis.
§ Facility size was calculated separately for acute care hospitals and nursing homes and was based on the tertile distribution of the total number of staff members per facility.
¶ https://www.cdc.gov/nchs/data_access/urban_rural.htm
** https://www.atsdr.cdc.gov/placeandhealth/svi/index.html
†† South: Alabama, Arizona, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, New Mexico, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia; Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin; Mountain: Colorado, Idaho, Montana, Nevada, Utah, and Wyoming; Pacific: Alaska, California, Hawaii, Oregon, and Washington; Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont.
Among approximately 1.6 million HCP working at 13,794 nursing homes, up-to-date COVID-19 vaccination coverage was 22.8% overall; coverage was highest among nonemployee licensed practitioners (28.2%) and lowest among employees (22.4%). Among HCP working in nursing homes, up-to-date COVID-19 vaccination coverage was highest among those working in the Pacific region (40.7%) and lowest among those working in the South (17.5%). Up-to-date COVID-19 vaccination was also substantially higher among HCP working at nursing homes in urban (24.2%) than in rural (17.5%) areas. No substantial differences in COVID-19 vaccination coverage among HCP by facility staff size or SVI were observed at either facility type. Up-to-date COVID-19 vaccination coverage was ≥20% among HCP working in nursing homes in 30 states but among HCP in acute care hospitals, approximately one half as many states (16) achieved this level of coverage (Supplementary Table, https://stacks.cdc.gov/view/cdc/134928).
Discussion
During the 2022–23 influenza season, fewer than one quarter of HCP working in acute care hospitals and nursing homes were up to date with recommended COVID-19 vaccination, and fewer than one half of HCP working in nursing homes had received influenza vaccine. Coverage varied by geographic region, health care facility type, employment category, and urbanicity. Recent reports indicate that influenza and COVID-19 vaccination coverage among HCP has declined during the COVID-19 pandemic (5). During the 2017–18 and 2018–19 influenza seasons, influenza vaccination coverage among HCP in acute care hospitals was 88.6% and 90.0%, respectively (6). From November 2021 to June 2023, CMS required all HCP at CMS-certified facilities to be vaccinated for COVID-19*****; this requirement likely contributed to COVID-19 primary series vaccination coverage reaching 94.3% among HCP in nursing homes (7) and 91.2% among those at acute care hospitals (5). The current findings suggest that factors associated with low vaccination coverage might have been exacerbated by the COVID-19 pandemic and compounded by emerging concerns such as vaccine fatigue (8) and other as yet unidentified factors.
In this analysis, up-to-date COVID-19 vaccination coverage was higher among HCP working in nursing homes than among those working in acute care hospitals. CMS requires nursing homes to report weekly up-to-date COVID-19 vaccination status among HCP and publishes weekly results on a public-facing website†††††; this might have resulted in higher coverage among HCP in nursing homes. CDC also worked with nursing homes to facilitate access to vaccination for both patients and staff members,§§§§§ which might have also improved coverage.
This report identified low up-to-date COVID-19 vaccination coverage among HCP in both acute care hospitals and nursing homes and low influenza vaccination coverage among HCP in nursing homes, both important threats to patient health and safety that need to be addressed. Implementation of vaccination recommendations for HCP has been a long-standing challenge for the public health and health care sectors. In an effort to improve vaccination coverage among HCP, health care facilities and federal and state governments have implemented interventions including jurisdiction-wide and facility-wide vaccination mandates (7,9). Mandates for HCP to receive influenza vaccination have been in place since before the COVID-19 pandemic and might contribute to the high vaccination rates reported to NHSN. However, such mandates might not be easily enforceable among nonemployee HCP in acute care hospitals, among whom coverage with both vaccines was lower than that among employees. Compared to influenza vaccines, COVID-19 vaccines are newer, and availability can be more sporadic; therefore, facilities do not have as much experience promoting vaccination and might not have the ability to conduct mass vaccination events. This might have contributed to lower COVID-19 vaccination coverage. Further, given the variations in vaccination coverage by region and urbanicity, campaign strategies tailored by region and focusing on rural areas might have the potential to increase vaccination coverage.
Limitations
The findings in this report are subject to at least four limitations. First, influenza vaccination and up-to-date COVID-19 vaccination coverage rates were reported separately using different definitions of total HCP working within the facility. Whether the same personnel are represented in seasonal influenza vaccination coverage counts and weekly COVID-19 vaccination counts is unknown. This nuance limits the direct comparability of coverage with the two vaccines; therefore, statistical comparisons of vaccination coverage were not conducted. Second, this report includes data reported by facilities on behalf of HCP, which could have resulted in underestimates of vaccination acquired outside the health care facility, particularly by HCP not employed directly by the reporting facility. Third, vaccination coverage could not be stratified by recent history of SARS-CoV-2 infection. CDC recommendations state that persons may consider delaying an updated vaccine by 3 months after infection. Therefore, some persons might not have considered themselves eligible for vaccination, leading to an underestimate of COVID-19 vaccination coverage. Finally, this analysis was conducted using aggregate data reported to NHSN at the facility level. Therefore, vaccination coverage could not be stratified by person-level covariates that might have enabled an assessment of potential differences, such as age, race, and ethnicity.
Implications for Public Health Practice
Closely monitoring influenza and up-to-date COVID-19 vaccination coverage among HCP might help facilitate evaluation of effective implementation of vaccination promotion strategies.¶¶¶¶¶ Studies are needed to identify additional factors associated with low vaccination coverage and approaches to improve coverage among HCP, with particular attention to geographic region, health care facility type, and employment category. Understanding these factors and promoting evidence-based strategies to increase vaccination coverage among HCP, such as making vaccines free and accessible at work (10), might allow for targeted interventions to improve coverage during future respiratory virus seasons. HCP should receive annual influenza vaccines and remain up to date with recommended COVID-19 vaccination to protect themselves and their patients from vaccine-preventable diseases.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
Footnotes
These authors contributed equally to this report.
NHSN defines up-to-date vaccination for surveillance purposes at the start of each quarter; the definition has been updated since the study was conducted. Bivalent COVID-19 vaccines are no longer recommended or available. https://www.cdc.gov/nhsn/pdfs/hps/covidvax/UpToDateGuidance-508.pdf
Facility size was calculated separately for acute care hospitals and nursing homes and was based on the tertile distribution of the total number of staff members per facility.
South: Alabama, Arizona, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, New Mexico, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia; Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin; Mountain: Colorado, Idaho, Montana, Nevada, Utah, and Wyoming; Pacific: Alaska, California, Hawaii, Oregon, and Washington; Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont.
45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d); 5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq.
References
- 1.Ahmad IA, Osei E. Occupational health and safety measures in healthcare settings during COVID-19: strategies for protecting staff, patients and visitors. Disaster Med Public Health Prep 2021;17:e48. 10.1017/dmp.2021.294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pearson ML, Bridges CB, Harper SA; Healthcare Infection Control Practices Advisory Committee; Advisory Committee on Immunization Practices. Influenza vaccination of health-care personnel: recommendations of the Healthcare Infection Control Practices Advisory Committee (HICPAC) and the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2006;55(No. RR-2):1–16. [PubMed] [Google Scholar]
- 3.Waldman SE, Buehring T, Escobar DJ, et al. Secondary cases of Delta variant coronavirus disease 2019 among vaccinated healthcare workers with breakthrough infections is rare. Clin Infect Dis 2022;75:e895–7. 10.1093/cid/ciab916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Advisory Committee on Immunization Practices; CDC. Immunization of health-care personnel: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2011;60(No. RR-7):1–45. [PubMed] [Google Scholar]
- 5.CDC. Influenza (flu). Vaccination coverage among health care personnel—United States, 2022–23 influenza season. Atlanta, GA: US Department of Health and Human Services, CDC; 2023. https://www.cdc.gov/flu/fluvaxview/hcp-coverage_22-23-estimates.htm
- 6.Lymon HML, Reses H, Barbre K, et al. Declines in influenza vaccination coverage among health care personnel in acute care hospitals during the COVID-19 pandemic—United States, 2017–2023. MMWR Morb Mortal Wkly Rep 2023;72:1244–7. https://www.cdc.gov/mmwr/volumes/72/wr/mm7245a6.htm?s_cid=mm7245a6_w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reses HE, Soe M, Dubendris H, et al. Coronavirus disease 2019 (COVID-19) vaccination rates and staffing shortages among healthcare personnel in nursing homes before, during, and after implementation of mandates for COVID-19 vaccination among 15 US jurisdictions, National Healthcare Safety Network, June 2021–January 2022. Infect Control Hosp Epidemiol 2023. Epub May 5, 2023. 10.1017/ice.2023.87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Israel Ministry of Health. Influenza vaccination of healthcare workers in Israel: report for 2014–2021. Jerusalem, Israel: Israel Ministry of Health; 2022. https://www.gov.il/BlobFolder/reports/flu-report-medical-staff-2017-2021/he/files_publications_units_qauality_and_patient_safety_flu-report-medical-staff-2017-2021-Executive-Summary.pdf
- 9.. CDC. Influenza vaccination coverage among health care personnel—United States, 2019–20 influenza season. Atlanta, GA: US Department of Health and Human Services, CDC; 2020. https://www.cdc.gov/flu/fluvaxview/hcp-coverage_1920estimates.htm
- 10.Community Preventative Services Task Force; CDC. Worksite: seasonal influenza vaccinations using interventions with on-site, free, actively promoted vaccinations—healthcare workers. Atlanta, GA: US Department of Health and Human Services, CDC; 2010. https://www.thecommunityguide.org/findings/worksite-seasonal-influenza-vaccinations-healthcare-on-site.html


