Abstract
BACKGROUND
Supra- and infratentorial epidural hematomas (SIEDHs) are a rare subtype of epidural hematoma (EDH), showing expanding bleeding on both sides of the tentorium, and account for <2% of EDHs (Aji, Apriawan, and Bajamal, 2018). These lesions can typically expand and decompensate quickly, making immediate diagnosis and surgical intervention crucial.
OBSERVATIONS
The authors’ patient presented >48 hours from a blunt trauma to the right side of the head with progressive vomiting and bruising behind the right ear. He had a Glasgow Coma Scale score of 15 on arrival. Head computed tomography showed an SIEDH measuring approximately 3 cm, and, given the hematoma’s size and mass effect, the patient was taken emergently to the operating room for decompression, where the source of bleeding was noted to be an emissary vein from the transverse sinus. The linear parietooccipital fracture was mended with mesh cranioplasty. Patient imaging and follow-up showed an excellent recovery.
LESSONS
Although SIEDH is rare, patients can present in a delayed fashion and be neurologically intact. The threshold to obtain imaging to rule out delayed hemorrhage should be low in any patient with a history of trauma in the region of a dural venous sinus.
Keywords: supratentorial and infratentorial epidural hematoma, posterior fossa epidural hematoma, epidural hematoma
ABBREVIATIONS: CT = computed tomography, CTV = computed tomography venography, ED = emergency department, EDH = epidural hematoma, GCS = Glasgow Coma Scale, PFEDH = posterior fossa epidural hematoma, SIEDH = supra- and infratentorial epidural hematoma, TBI = traumatic brain injury
Traumatic brain injury (TBI) occurs in 1.5 million people per year in the United States, with approximately 2% of cases (range 1%–4%) resulting in an epidural hematoma (EDH).1,2 Posterior fossa EDH (PFEDH) accounts for 2%–15% of EDH cases.3–9 Prognosis can depend on time delay to surgery and presenting Glasgow Coma Scale (GCS) score.10 Mortality reported in the literature has ranged from 8% to 26%.10
Supra- and infratentorial epidural hematoma (SIEDH), a rare subtype of PFEDH, occurs in <2% of all EDHs.1 SIEDH is clinically important because, although blood can accumulate more slowly, once enough blood has accumulated, rapid compression of the brainstem or fourth ventricle can occur in over 30% of PFEDHs. This can lead to potentially devastating neurological outcomes.11 Symptoms can often be nonspecific initially, but clinical suspicion should remain high, given the severity of untreated SIEDH. The case in the present report demonstrates a delayed onset of SIEDH, which was treated with right-sided craniotomy and mesh cranioplasty and was found to have a right parietooccipital comminuted skull fracture.
Illustrative Case
A 35-year-old male with a history of polysubstance use disorder presented to the emergency department (ED) for trauma with 2 days of headache, nausea, and emesis. He fell 2 days after an altercation in which he struck the right side of his head. Subsequently, he developed nausea and vomiting and had poor oral intake. When these symptoms failed to improve, he presented to the ED for further evaluation. He also complained of headache and was noted to have bruising behind the right ear. On examination, he had a GCS score of 15. He was awake, alert, oriented, and without any focal motor or cranial nerve deficit. He was noted to have posterior neck tenderness to palpation, right hemotympanum, and Battle’s sign. Head computed tomography (CT) without contrast revealed a large, right-sided SIEDH measuring approximately 3 cm in maximal thickness with approximately 4–5 mm of leftward shift (Fig. 1A and B). There were scattered foci of pneumocephalus, along with an overlying comminuted fracture of the right parietooccipital bones extending into the right petrous temporal bone with hemorrhage in the right mastoid. CT venography (CTV) showed right transverse and sigmoid sinus injury with little contrast filling.
FIG. 1.
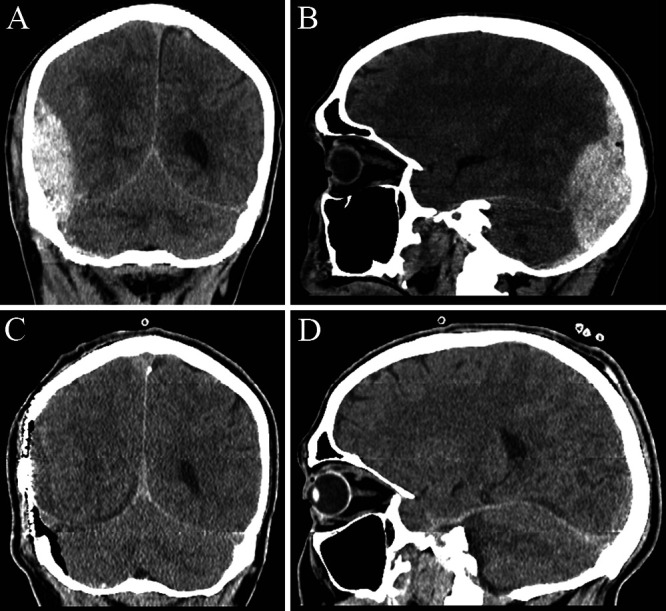
Initial head CT images of SIEDH in coronal (A) and sagittal (B) sections. Postsurgical imaging (C, D).
The patient was taken to the operating room for emergent right-sided craniotomy for EDH with mesh cranioplasty. An inverted U-shaped incision was made from anterior to the tragus to the vertex and then to the external occipital protuberance (Fig. 2A). A myocutaneous flap was raised. The right parietooccipital comminuted skull fracture was identified (Fig. 2B). A high-speed drill with the perforator bit was used to make a tangential burr hole, and the fracture was carefully dissected with a combination of the Penfield 1 and periosteal elevator. A large, organized hematoma covered the supratentorial and infratentorial dura (Fig. 2C). Gentle irrigation was initially used to free the hematoma from the dura. A further clot was freed carefully using a Penfield 1. Of note, there was significant adhesion of the blood clot, most likely a result of the delayed presentation. Imaging and clinical sequelae were initially concerning for sinus injury, and the bleeding source was identified as an emissary vein off of the transverse sinus. A mesh plate to which the dura was tacked was used for cranioplasty (Fig. 2D). The patient was admitted to the neurosurgical intensive care unit for postoperative monitoring. Postoperative head CT showed resolution of the hematoma (Fig. 1C and D). The patient was medically ready for discharge by postoperative day 3. The 2-week follow-up showed stable imaging and resolution of symptoms.
FIG. 2.

A: Right Battle’s sign noted and U-shaped skin incision. B: Right parietooccipital comminuted skull fracture was identified intraoperatively, and this fracture location was consistent with the preoperative imaging. C: Large clotted and fibrous blood products covered the dura upon removal of the bone flap. D: Mesh cranioplasty.
Patient Informed Consent
The necessary patient informed consent was obtained in this study.
Discussion
Observations
Sharafat et al.,10 in their 6-year study of 1252 patients with EDH, found 104 patients to have PFEDH, corresponding to approximately 8% of cases. SIEDH is estimated to be a rarer subtype of PFEDH, with an incidence of less than 2% of all EDHs1 and 11%–70% of all PFEDHs.7 Because of its less common occurrence, SIEDH has not been studied to the extent of other TBI pathologies and therefore lacks standardized guidelines and approaches. Su et al.,12 in their paper investigating diagnostic and surgical considerations for SIEDH, discussed the relative paucity of case series investigating SIEDH. Each study has different surgical indications. Xiaoyu and Guoping,13 in their retrospective study of 25 patients treated for SIEDH, used CT findings to determine surgical indications as follows: 1) obliteration of the perimesencephalic cistern, 2) compression and/or displacement of the fourth ventricle and the presence of hydrocephalus, and 3) extension of the hematoma to the supratentorial area with cerebral compression. Lan et al.,14 in their series of 34 patients with traumatic PFEDH crossing the transverse sinus, sent all patients with signs of brain herniation immediately to the operating room, and other patients underwent surgery as clinically indicated. Nasi et al.,7 in their study of 42 patients with SIEDH, had the following surgical indications: 1) compression or obliteration of the cerebellar perimesencephalic cisterns, 2) compression or displacement or obliteration of the fourth ventricle, 3) hydrocephalus, 4) marked supratentorial brain compression, 5) neurological deterioration, and 6) hematoma thickness to more than 15 ml. Uppar et al.,15 in their study of 61 patients undergoing surgery for SIEDH, had the following surgical indications: 1) SIEDH volume to more than 33 ml, 2) fourth ventricle mass effect with or without related hydrocephalus, 3) mass effect on the basal cisterns, and 4) decrease in GCS score by 2 points after the first assessment or new bradycardia or signs of increased intracranial pressure. Given our patient’s initial CTV findings suspicious for right transverse and sigmoid sinus injury, an EDH size of 3 cm in maximal thickness, and the 4–5 mm of midline shift, our patient required surgery. Our patient met at least one surgical criterion for all the above studies, except for the indications of Uppar et al.,15 but the SIEDH volume in our patient was close to their lower limit for performing surgery.
Fracture location and bleeding source varied among the different studies. Aji et al.1 described three patients treated for traumatic SIEDH, one of whom had a linear fracture of the occipital bone and two of whom had a linear fracture of the occipital bone with lambdoid suture separation. The observed source of bleeding was the transverse sinus in one patient, the site of fracture and emissary vein in one patient, and unknown in one patient. Xiaoyu and Guoping13 observed a linear fracture of the occipital bone intraoperatively in 21 patients, with bleeding from the transverse sinus in 3 patients; the authors emphasized that if the transverse sinus is compressed, this can be a sign of disrupted venous return, leading to intracranial hypertension and herniation. The initial CTV suspicion of right transverse sinus and sigmoid sinus injury in our patient aligns with this observation and demonstrates the need to perform decompressive surgery. Nasi et al.7 identified a venous source of bleeding in all cases, with transverse or sigmoid sinus injury in 22% of cases; these authors reported that venous hemorrhage leads to slower accumulation of blood, and, once a threshold amount of blood is present, fatal mass effect on the brainstem can occur quickly. In their study of 19 patients with SIEDH, Su et al.12 observed bleeding from the injured transverse sinus in 7 patients during evacuation, and 5 (71.4%) of these patients had a diastatic fracture of the lambdoid suture. Our initial CTV findings demonstrated possible right transverse and sigmoid sinus injury, and the bleeding source in our patient was found to be an emissary vein from the transverse sinus.
Although the overall number of studies on SIEDH is not large, advances in surgical technique for SIEDH have been well described in this body of literature. The classic surgical approach tends to involve large suboccipital craniotomy or craniectomy, with craniotomies larger than the size of the hematoma.1,13 This large craniotomy allows visualization of the hematoma borders. A bone bridge can be left over the transverse sinus. The classic approach involves a longer procedure time and larger postoperative wound and results in a larger defect in the skull.13 Nasi et al.7 described a combined supratentorial craniotomy and suboccipital craniotomy, leaving bone over the transverse sinus for dural tenting sutures. These authors believe this to be a safe approach, and they reposition both bone flaps with hardware to avoid complications of decompression craniectomy.7 Uppar et al.15 described a similar approach, with a hockey stick incision, craniotomy above the transverse sinus, a thin strip of bone over the sinus, and a craniectomy or craniotomy for the infratentorial part. Xiaoyu and Guoping13 used a supratentorial approach, which offers a more minimally invasive approach with the advantage of easier hemostasis due to no major meningeal arteries in the posterior fossa and therefore no tearing of the sinuses. Lan et al.14 described a supratentorial craniotomy with an endoscope-assisted approach to evacuate the infratentorial compartment of the hematoma. This approach offers the advantage of a reduced operative time, better visualization using the endoscope, and the avoidance of opening up the posterior fossa.14 Su et al.12 described the pitfalls of surgical treatment for SIEDH, with the likelihood of significant hemorrhage from a damaged transverse sinus and overall blood loss. Our surgical approach involved a tangential burr hole close to the parietooccipital fracture and the use of a Penfield 1 retractor to elevate the fracture off the hematoma, followed by irrigation of the hematoma off the dura. Our approach did not require a suboccipital craniotomy or craniectomy, similar to Xiaoyu and Guoping13 and Lan et al.14 Given the rarity of this entity, it will be difficult to identify the safest and most effective surgical plan for SIEDH, other than to say that the best option is the method that is best for the individual patient.
Delayed intracranial hemorrhage is a relatively common phenomenon and can have a variety of clinical presentations, with many patients experiencing relatively minor symptoms initially before hematoma progression.16 Our patient experienced symptoms for multiple days after his initial traumatic injury before his indication for surgery was discovered. His initial examination was relatively unremarkable, with a GCS score of 15 and no focal deficit, but he did have posterior neck tenderness to palpation, right hemotympanum, and likely a right Battle’s sign (mastoid region ecchymosis). In a study of three patients by Aji et al.,1 one patient had an initial GCS score of less than 8, and two patients had a GCS score of 9–12. The chief complaint of the patients was decreased consciousness, with headache, nausea, and vomiting as well.1 Xiaoyu and Guoping13 found that 19 of 25 patients with SIEDH in their study had an initial GCS score of 13–15. The patients had a history of occipital trauma as well as headache, vomiting, loss of consciousness, neck resistance, and Battle’s sign.13 Twenty-two of 25 patients in their study had SIEDH diagnosed within 24 hours, whereas 3 of 25 patients were diagnosed with SIEDH from 3 to within 7 days.13 In the study by Nasi et al.,7 20% of patients were in a coma with a GCS score <8 on admission. These studies demonstrate that SIEDH can have a delayed presentation, up to within 7 days. Among the 19 patients treated surgically for SIEDH in the study by Su et al.,12 6 patients underwent a delayed operation because their SIEDH grew in size or was seen for the first time on a subsequent CT scan. In addition, the initial neurological examination is variable, with some patients having a mild GCS score and some in a coma with a GCS score <8. Battle’s sign can be observed, and other nonspecific symptoms (headache, nausea, and vomiting) are not sufficient for diagnosis. Taken together, these results demonstrate the need for serial CT scans and neurological examinations in certain patients with a history of occipital trauma.
Lessons
SIEDH is a rare and potentially more devastating subtype of posterior fossa extradural hematoma. There is currently limited guidance for the treatment and approach. This case demonstrates that patients can have a delayed presentation and present without specific neurological findings, making delayed imaging important to avoid missing this entity.
Author Contributions
Conception and design: Pathak, Ziechmann, Gupta, Villanueva. Acquisition of data: Ziechmann. Analysis and interpretation of data: Pathak, Ziechmann, Gupta, Villanueva. Drafting the article: Pathak, McAuliffe. Critically revising the article: Pathak, Ziechmann. Reviewed submitted version of manuscript: Pathak, Ziechmann, Gupta. Approved the final version of the manuscript on behalf of all authors: Pathak. Administrative/technical/material support: Pathak. Study supervision: Ziechmann, Gupta.
References
- 1. Aji YK, Apriawan T, Bajamal AH. Traumatic supra- and infra-tentorial extradural hematoma: Case series and literature review. Asian J Neurosurg. 2018;13(2):453–457. doi: 10.4103/ajns.AJNS_282_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Traumatic brain injury and concussion. Published April 26, 2023. Accessed August 6, 2023. https://www.cdc.gov/traumaticbraininjury/index.html.
- 3. Hooper R. Observations on extradural haemorrhage. Br J Surg. 1959;47:71–87. doi: 10.1002/bjs.18004720114. [DOI] [PubMed] [Google Scholar]
- 4. Roda JM, Giménez D, Pérez-Higueras A, Blázquez MG, Pérez-Alvarez M. Posterior fossa epidural hematomas: a review and synthesis. Surg Neurol. 1983;19(5):419–424. doi: 10.1016/0090-3019(83)90138-6. [DOI] [PubMed] [Google Scholar]
- 5. Jamieson KG, Yelland JD. Extradural hematoma. Report of 167 cases. J Neurosurg. 1968;29(1):13–23. doi: 10.3171/jns.1968.29.1.0013. [DOI] [PubMed] [Google Scholar]
- 6. Mckissock W, Taylor Julien C, Bloom William H, Till K. Extradural hæmatoma: observations on 125 cases. Lancet. 1960;276(7143):167–172. [Google Scholar]
- 7. Nasi D, Iaccarino C, Romano A, et al. Surgical management of traumatic supra and infratentorial extradural hematomas: our experience and systematic literature review. Neurosurg Rev. 2020;43(3):893–901. doi: 10.1007/s10143-019-01083-7. [DOI] [PubMed] [Google Scholar]
- 8. Cordobés F, Lobato RD, Rivas JJ, et al. Observations on 82 patients with extradural hematoma. Comparison of results before and after the advent of computerized tomography. J Neurosurg. 1981;54(2):179–186. doi: 10.3171/jns.1981.54.2.0179. [DOI] [PubMed] [Google Scholar]
- 9. Kırcelli A, Özel Ö, Can H, Sarı R, Cansever T, Elmacı İ. Is the presence of a linear fracture a predictor of delayed posterior fossa epidural hematoma? Ulus Travma Acil Cerrahi Derg. 2016;22(4):355–360. doi: 10.5505/tjtes.2015.52563. [DOI] [PubMed] [Google Scholar]
- 10. Sharafat S, Azam F, Khan Z. Posterior fossa epidural hematoma: a 6-year management experience. Pak J Med Sci. 2023;39(1):253–256. doi: 10.12669/pjms.39.1.6408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Verma SK, Borkar SA, Singh PK, et al. Traumatic posterior fossa extradural hematoma: experience at level I trauma center. Asian J Neurosurg. 2018;13(2):227–232. doi: 10.4103/1793-5482.228536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Su TM, Lin CC, Lan CM, Lee TH, Hsu SW, Lu CH. Head trauma associated with supra- and infratentorial epidural hematoma: diagnostic and surgical considerations. World Neurosurg. 2023;176:e273–e280. doi: 10.1016/j.wneu.2023.05.048. [DOI] [PubMed] [Google Scholar]
- 13. Xiaoyu W, Guoping L. Surgical treatment of supra- and infratentorial epidural hematoma. Turk Neurosurg. 2013;23(3):299–303. doi: 10.5137/1019-5149.JTN.5043-11.1. [DOI] [PubMed] [Google Scholar]
- 14. Lan Z, Richard SA, Chen M, Yang C. Endoscopically assisted supratentorial evacuation of infratentorial epidural hematomas crossing the transverse sinus. Interdiscip Neurosurg. 2018;13:129–133. [Google Scholar]
- 15. Uppar A, Kadregula S, Sadashiva N, et al. Surgical outcomes of Supra- Infra Tentorial Extradural Hematoma (SIEDH): A retrospective study from a single institution. Clin Neurol Neurosurg. 2021;200:106369. doi: 10.1016/j.clineuro.2020.106369. [DOI] [PubMed] [Google Scholar]
- 16. Ziechmann R, Pathak SM, Welch J, Villanueva P. Delayed traumatic intracerebral hematoma: a pathophysiological classification and literature review. Cureus. 2023;15(8):e42987. doi: 10.7759/cureus.42987. [DOI] [PMC free article] [PubMed] [Google Scholar]


