Abstract
Purpose
Telemedicine care dramatically expanded during the COVID-19 pandemic. We characterized facilitators and barriers to telemedicine implementation among safety-net primary care clinics serving patients with limited English proficiency (LEP).
Methods
We collected data on telemedicine volume and patient demographics among safety-net clinics participating in a telemedicine learning collaborative. Data on various metrics were reported to the collaborative from February 2019 through August 2021. We conducted semi-structured interviews with clinical and quality leaders, purposively sampling clinics serving high proportions of patients with LEP. We analyzed interviews with a mixed inductive-deductive approach applying the Consolidated Framework for Implementation Research.
Results
By September 2020, the 23 sites served 121,589 unique patients with in-person and 120,338 with telephone visits; 47% of these patients had LEP. Of 10,897 unique patients served by video visits, 38% had LEP. As a proportion of total visits, telemedicine (telephone and video) visits increased from 0–17% in October 2019–March 2020 to 10–98% in March–August 2020. We conducted 14 interviews at 11 sites. Themes included (1) existing telemedicine platforms and interpreter services were not optimized to support patients with LEP; (2) clinics invested significant labor iterating workflows; (3) sites with technological infrastructure and language-concordant staff were best suited to serve patients; (4) patients speaking less-represented languages or experiencing intersecting literacy barriers were underserved with telemedicine. Interviewees recommended innovations in telemedicine platforms and community-based access.
Conclusions
Safety-net sites relied on existing resources to accommodate patients with LEP, but struggled providing access for the most marginalized. Proactive, data-driven strategies to address patient and community barriers as well as optimize clinical workflows with high-quality, certified medical interpreters are needed to ensure equitable access.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-023-08304-2.
KEY WORDS: telemedicine, health equity, limited English proficiency, safety-net clinics, access to care
INTRODUCTION
There are 25.6 million people with limited English proficiency (LEP) in the United States (USA).1 Patients with LEP experience a range of healthcare disparities compared to English-proficient patients. These include decreased access to outpatient and preventive care,2, 3 greater number and length of hospitalizations,4, 5 and more emergency department visits.2, 4 This is likely due to healthcare system factors, such as inadequate communication and structural and interpersonal racism in healthcare systems,6–11 as well as socioeconomic and political barriers to health such as lower health literacy, low income, and anti-immigrant legislative policies.12–14
The COVID-19 pandemic spurred a rapid, dramatic expansion of telemedicine.15, 16 Healthcare systems quickly pivoted from providing primarily in-person care to remote care via telephone and video in order to limit viral transmission and aid social distancing.17 This shift was especially marked for safety-net healthcare institutions, which largely did not offer telemedicine services prior to the pandemic.18 While most policymakers, healthcare leaders, and clinicians anticipate that telemedicine use will continue well beyond the COVID-19 pandemic, safety-net settings faced the highest barriers to telemedicine rollout and will need specific attention as we move forward.
Telemedicine not only has the potential to increase access and reduce health disparities affecting patients with LEP, but it also has the potential to exacerbate existing inequities.19 There is a “digital divide” in the USA affecting access to devices, internet, and digital skills—each of which are needed to access telemedicine.20 Racial and ethnic minoritized groups and patients receiving public insurance (who are more likely to have LEP) are less likely to receive telemedicine visits, and those receiving telemedicine are more likely to have a telephone visit rather than video.21–30 Some of this differential access is due to “digital redlining”—structural racism resulting in reduced access and affordability of technology services and infrastructure among neighborhoods with low-income and people of color.31–34
Beyond these individual- and neighborhood-level barriers to digital access and use, we know that healthcare systems serve a critical role in fostering or impeding digital health equity among ethnically and linguistically diverse patient populations. However, little is known about on-the-ground experiences of safety-net clinical practices providing telemedicine to LEP patients during the COVID-19 pandemic. We sought to assess LEP-specific telemedicine facilitators and barriers using an implementation science framework. By describing telemedicine implementation in the frontlines of primary care, we may inform efforts to better serve LEP patients in the future as telemedicine continues.
METHODS
This study aimed to characterize the experience of safety-net primary care clinics providing telemedicine to patients with LEP during the COVID-19 pandemic using mixed methods.
Study Population
Our study setting included safety-net primary care clinics in California participating in a learning collaborative called the Connected Care Accelerator35 between August 13, 2020, and August 12, 2021. The collaborative functioned as a quality improvement initiative in which participating sites provided data for evaluation and received funding, resources, and technical assistance. There was a competitive process to identify and select the participating health centers. The final cohort was selected to ensure representation on core domains such as geographic region of the state, size of clinics, rural/urban, patient population, Medicaid/uninsured patients, and readiness for engagement to identify innovative approaches for telehealth.
Eligibility criteria included (1) providers actively using an electronic health record (EHR), (2) serving at least 8000 unique patients, and (3) reaching Medi-Cal and uninsured patients (defined as either serving at least 70% Medi-Cal and/or uninsured, at least 40% Medi-Cal and/or uninsured as well as 20% Black, or at least 40% Medi-Cal and/or uninsured as well as 70% non-white). The learning collaborative staff (KF, VA) regularly corresponded with participating sites, whereas the evaluation teams (AS, SL, JF, MJ, NA, CL, US) corresponded with participating sites during data collection activities and follow-up related to this study.
Data Collection
Participating sites submitted clinic characteristics (e.g., site location, number of unique patients, number of visits) and patient demographics (e.g., insurance type, race, ethnicity, age, gender, preferred language) at the collaborative launch. This was collected in 2020 but covered a longer time period (beginning in Feb 2019). Health centers also submitted data on unique patients seen by their health center in 2019, and all visits in 2019 segmented by payer. Data regarding prevalence of patients with limited English proficiency was defined as “Patients Best Served in a Language Other than English,” which is identical to how participating sites report patients with LEP to the Health Resources and Services Administration.36 The collaborative collected data on telemedicine utilization at three time points: September 2020, March 2021, and September 2021. These data included overall visit volume and telemedicine utilization, along with modality (e.g., phone, in-person), using an Excel template (Microsoft Corporation, Redmond, WA). The learning collaborative staff (KF, VA) provided the evaluation team (AS, SL, JF, MJ, NA, CL, US) with data summaries from each clinic.
Members of the study team (AS, JF, CL, US) then conducted semi-structured qualitative interviews with a subset of sites participating in the learning collaborative. Using the quantitative data reported from each site, we purposively sampled clinics for the qualitative portion of the study that 1) served a high proportion of patients with LEP (≥40%, measured between March and August 2020) and 2) represented a range of telemedicine implementation maturity (assessed by study team as “early”, “middle,” or “advanced”)—to better understand and characterize the telemedicine implementation experiences in a diverse range of care settings. Members of the study team (AS, JF, CL, US) developed and piloted an interview guide that covered overall telemedicine implementation and workflows, facilitators, and barriers for patients with LEP in accessing telemedicine, and solutions and suggestions for improving LEP access (see appendix for Interview Guide). We invited representatives from sites to participate in a 45–60-min videoconference interview. The study team invited participants over e-mail. We asked to interview individuals who held dual roles as clinician as well as clinical leadership with close vantage point of telemedicine implementation; if no individual occupied both roles, we interviewed two individuals from the site. Interviews took place between February and May 2021. Faculty and senior research staff at UCSF with experience in qualitative methods conducted each interview via videoconference software (AS, JF, CL, US). Participants were offered a $75 Amazon e-gift card after the interview as a token of appreciation. We did not share detailed transcripts or codes back with interviewees unless requested. We conducted interviews until we as a group concluded that we had achieved thematic saturation.37 We audio recorded the interviews and took detailed field notes, and then had each interview recording professionally transcribed.
Data Analysis
For the quantitative data reported by clinics, we used descriptive statistics in Excel to summarize the clinic characteristics (unique patients visits, total visit volume, telemedicine visit volume including telephone and video visits), as well as their patient populations (race/ethnicity, proportion preferred to receive care in a language other than English, insurance payor, age, gender). Using the baseline and follow-up data on telemedicine utilization, we also summarized the increase in telemedicine encounters from the 6 months prior to March 2020 and the 6 months after March 2020 across all sites.
For the qualitative analysis, we used inductive and deductive approaches, first identifying themes that emerged from the data and then mapping these themes to the Consolidated Framework for Implementation Research (CFIR) conceptual framework.38, 39 We selected CFIR because it allows for a wide range of contextual factors used to characterize complex interventions in varied healthcare settings. All analyses were conducted in Dedoose software (SocioCultural Research Consultants, Hermosa Beach, CA). Three authors (AS, JF, SL) performed open coding with a specific focus on the experiences of implementing telemedicine for patients with LEP. Five authors (AS, SL, JF, CRL, US) met first in small groups and then jointly to determine the final codebook. After finalizing the codebook, two authors (AS, SL) dual coded 25% of all transcripts, meeting to discuss and resolve discrepancies. One author (SL) then coded the remaining 75% of transcripts, which another author (AS) reviewed for agreement. The entire study team utilized the codes to develop inductive themes, and then performed a final mapping of concepts to key CFIR domains. We used the Consolidated criteria for Reporting Qualitative research (COREQ)40 and Statistical Analyses and Methods in the Published Literature (SAMPL) checklists for quality reporting of qualitative and quantitative findings, respectively.
The UCSF IRB reviewed the survey (#20-32225) and interview activities (#19-29025) and deemed them exempt, granting a waiver of informed consent.
RESULTS
Quantitative Data
There were a total of 47 applicants for the Connected Care Accelerator, and 23 health centers were selected to participate in the Learning Collaborative. On average, these 23 sites reported serving a mean of 48,579 unique patients annually in 2019 (SD 47,187) and a mean of 166,111 (SD 180,055) visits. Learning collaborative sites served between 425 and 42,948 unique patients monthly in August 2021 (time point when monthly data were available), and provided care in urban, suburban, and rural areas across the state of California. Full characteristics of clinics surveyed and represented by interviewees are listed in Tables 1, 2 and 3. Data on race/ethnicity and age were collected by unique patient (Table 1); patient gender and language preference were collected monthly by visit modality (Table 2); payor was collected by total visits (Table 3); these are thus reported separately. The collaborative data collection form is available in the Appendix.
Table 1.
Site and Patient Characteristics of All Learning Collaborative Sites and the Subset of Interviewed Sites
| Patient characteristics* | N=23 (all sites in learning collaborative) | N=11 (interviewed sites) | |
|---|---|---|---|
| N (%) | N (%) | ||
| Race/ethnicity‡ | White | 502,488 (45%) | 205,830 (28%) |
| Black or African American | 86,731 (8%) | 69,893 (10%) | |
| Asian | 134,636 (12%) | 118,199 (16%) | |
| More than one race | 10,906 (1%) | 6,842 (1%) | |
| Other | 242,947 (22%) | 232,102 (32%) | |
| Unreported | 139,605 (12%) | 99,881 (14%) | |
| Hispanic/Latino | 599,484 (54%) | 380,021 (52%) | |
| Age | ≤ 17 | 366,097 (33%) | 205,764 (28%) |
| 18–44 | 352,060 (31%) | 227,656 (31%) | |
| 45–64 | 281,757 (25%) | 206,389 (28%) | |
| 65+ | 118,572 (11%) | 92,938 (13%) | |
*Data collected from all registered patients in 2019
‡ Data was collected using the USA Office of Management and Budget standards. The study team suggests that future data be collected with further disaggregation. https://www.rwjf.org/en/library/research/2021/10/charting-a-course-for-an-equity-centered-data-system.html
Table 2.
Gender and Preferred Language of Patients Seen at All Learning Collaborative Sites in September 2020, Segmented by Visit Modality
| Patient characteristics † | N=23 (all sites in learning collaborative) | |||
|---|---|---|---|---|
| Unique patients seen in person (n=121, 589) | Unique patients seen by phone (n=120,338) | Unique patients seen by video (n=10,897) | ||
| N (%) | N (%) | N (%) | ||
| Gender § | Female | 74,344 (61%) | 77,576 (63%) | 6964 (64%) |
| Male | 47,885 (39%) | 45,576 (37%) | 3839 (35%) | |
| Nonbinary gender or unreported | 312 (<1%) | 156 (<1%) | 150 (1%) | |
| Language preference | Best served in a language other than English | 57,490 (47%) | 57,050 (47%) | 4146 (38%) |
| Best served in English | 64,099 (53%) | 63,288 (53%) | 6751 (62%) | |
† Data collected in September 2020; some patients may have had multiple visits in different visit modalities in the month of data collection
§ A few sites reported gender using best practices for collecting, coding, and reporting gender identity data, but most did not at the time data was collected. https://www.sfdph.org/dph/files/PoliciesProcedures/COM9_SexualOrientationGuidelines.pdf
Table 3.
Distribution of 2019 Visits by Payor
| N (%) | N (%) | |
|---|---|---|
| Medicaid or CHIP | 2,530,281 (66%) | 1,777,603 (71%) |
| Medicare | 162,987 (4%) | 98,268 (4%) |
| Other public | 226,348 (6%) | 149,921 (6%) |
| Private/commercial | 246,789 (6%) | 68,850 (3%) |
| None/uninsured | 394,953 (10%) | 226,295 (9%) |
| Dual eligible | 259,184 (7%) | 179,118 (7%) |
Demographics of Patients Served
Across all 23 participating sites, 54% of patients were Hispanic/Latino, 45% were white, 12% were Asian, 8% were Black/African American, 1% were more than one race, and 22% identified as another race. Thirty-three percent of patients seen across all sites were 17 or younger, 32% were between 18 and 44, 25% were between 45 and 64, and 11% were 65 or older.
Of clinical sites interviewed for the qualitative portion of this project, 54% (6/11) served at least 50% LEP patients and 100% (11/11) served at least 40% LEP patients (Fig. 1).
Figure 1.
Patient language preference, by site interviewed. Blue horizontal bar represents patients best served in a language other than English. Orange horizontal bar represents patients best served in English. Data collected between March 2019 and February 2020.
Telemedicine Visit Utilization
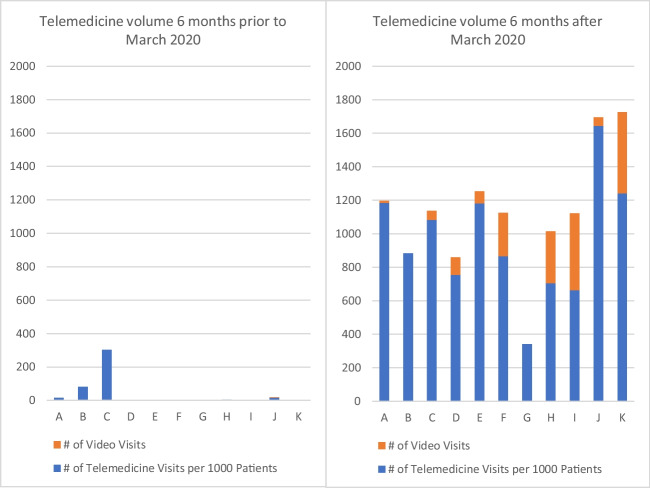
Health centers increased from a range of 0–17% telemedicine visits (both telephone and video) in the 6 months prior to March 2020, to a range of 10–98% of total visits by September 2020. See Fig. 2 for a visual depiction of telemedicine visit volume over time.
Figure 2.
Change in telemedicine visit volume for all patients across sites interviewed. Left bar graph represents telemedicine volume 6 months prior to March 2020. Orange bars represent the total number of video visits at each site. Blue bars represent the number of telemedicine visits per 1000 patients at each site. Right bar graph represents telemedicine volume 6 months after March 2020. Orange bars represent the total number of video visits at each site. Blue bars represent the number of telemedicine visits per 1000 patients at each site.
In the month of September 2020, the 23 sites served 121,589 unique patients via in-person visits, 120,338 via telephone visits, and only 10,897 with video visits. Of the unique patients served by in-person and telephone visits, 47% preferred a language other than English. Of video visits, 38% (4146) were with patients with LEP.
Payor data was tabulated for the 2019 year and was expected to be similar for following years (see Table 3). The majority (66%) of total visits seen for primary care at the sites in the learning collaborative in 2019 were covered by Medicaid or CHIP (2,530,281), with 4% covered by Medicare (162,987), 7% under dual eligibility (259,184), 6% by other public insurance (226,348), 6% by private/commercial insurance (246,789), and 10% of visits were uninsured (394,953).
Qualitative Analysis
We invited representatives from 12 of the learning collaborative sites to participate. We completed interviews with 14 individuals representing 11 sites (24%, 11/45); one site did not respond to the invitation. Interviewee and clinic demographics, including phase of telemedicine implementation, are in Table 4.
Table 4.
Interviewee Characteristics
| Site letter | Participant ID | Role | Setting location | Setting type | Telemedicine utilization | ||
|---|---|---|---|---|---|---|---|
| Telemedicine maturity at the launch of the learning collaborative (early, middle, advanced) | No. of telemedicine visits per 1000 patients in 6 months prior to March 2020 | No. of telemedicine visits per 1000 patients in 6 months after March 2020 | |||||
| A | 1 | Internal medicine physician, Associate Medical Director | Large urban | Public healthcare system | Middle | 16 | 1185 |
| A | 2 | Family medicine physician, Residency Program Director, telemedicine implementer | Large urban | Public healthcare system | Middle | 16 | 1185 |
| B | 3 | Pediatrician, Medical Director of Outpatient Health Center | Large urban | Public healthcare system | Middle | 81 | 883 |
| C | 4 | Pediatric medical director | Urban | Community health center | Advanced | 303 | 1083 |
| D | 5 | Family nurse practitioner, telemedicine platform implementation lead | Urban, agricultural | FQHC | Early | 0 | 754 |
| E | 6 | Director of Clinic Operations | Urban | Community health center | Advanced | 0 | 1182 |
| F | 7 | Family medicine physician, Director of Clinical Informatics | Large urban and Urban | FQHC | Middle | 0 | 865 |
| G | 8 | Internal medicine physician, Associate Chief Medical Informatics Officer for Ambulatory Care | Urban | Public healthcare system | Early | 0 | 340 |
| H | 9 | Clinical Pharmacy Manager | Urban | FQHC | Early | 4 | 704 |
| H | 10 | Family medicine physician, Medical Director | Urban | FQHC | Early | 4 | 704 |
| I | 11 | Pediatrician, telemedicine implementer | Large urban | Community health center | Advanced | 0 | 663 |
| I | 12 | Quality improvement project lead | Large urban | Community health center | Advanced | 0 | 663 |
| J | 13 | Family medicine physician, Chief Medical Officer | Urban, agricultural | Community health center | Middle | 17 | 1644 |
| K | 14 | Family medicine physician, Chief Medical Officer | Large urban | FQHC | Middle | 0 | 1242 |
Our qualitative analysis identified key themes relating to the implementation of telemedicine for patients with LEP. We describe four major themes below organized with respect to CFIR domains; additional themes with exemplar quotes are listed in the Appendix.
First, telemedicine delivery was not optimized to support patients with LEP, due to limitations of the existing platforms and interpreter services (Intervention Characteristics domain). For both telephone and video visits, most sites did not have linkage between the telemedicine modality platform and interpreter services. Patient outreach for telemedicine encounters, including pre-set portal or text messaging, was not consistently interpreted, meaning patients with LEP received less awareness of appointment options. During telemedicine encounters, interviewees had to troubleshoot means to devise three-way calls using a speakerphone or utilize additional staff to connect to an interpreter. Participants recommended innovations such as software platforms that actually link to interpreter services, and innovative clinic templates that deliberately add more time to encounters which require working with interpreters: “This is the one chance to really revolutionize the way we deliver primary care. You could make new patient visits, three 20-minute blocks to make it a 60-minute visit, or certain patients where you need 40 minutes like an interpreter, right?” (Participant 2, Site A).
To meet the needs of patients with LEP, safety-net sites trialed complex iterations of work processes, based on the organizations’ existing expertise serving diverse populations (Process domain). The process of telemedicine delivery was adapted to the existing workflows to support patients with LEP at each site. This involved both the rapid adaptation of workflows, to iteratively identify what worked well, as well as the development of workarounds: individual means to circumvent workflows which impeded clinical care. This was a finding both for telephone as well as video visits. While individual workarounds were cited as successful in completing telemedicine encounters, workarounds could also be cumbersome or difficult to standardize. Adaptations of workflows could add to confusion as processes were iterated: “This is just so egregious…the initial workflow was to call interpreting services on the landline and just speakerphone them onto the call…these computers had no microphones or audio. So, then the clinicians were supposed to get on [telemedicine platform] video through [the EHR] and then call-in on the phone…it’s really challenging to even find the call number and the password. And then somehow there was a conference call in interpreting services but…no one trained doctors how to conference call or put people on hold” (Participant 8, Site G).
Existing process facilitators included language-specific trainings for patients on how to access a telemedicine encounter, and inclusive appointment outreach that did not presume the telemedicine preferences of the patient prior to asking. Respondents named lack of equity-based data as a process barrier and desired more evaluation and accurate telemedicine utilization data to inform the implementation process. They recommended analyses stratified by race/ethnicity and language preference in order to address telemedicine equity through quality improvement projects: “We’ve tried to look at the data a couple of times – we haven’t actually shared that data with the clinic because we have never been quite sure of how accurate our data is, but we didn’t see a ton of differences and as much as we expect it by race, ethnicity, language, gender – and that was just our own data analyst taking a look at the data that we had” (Participant 1, Site A). In addition to language or racial/ethnic-based parameters of telemedicine utilization, measurements of health literacy, cellphone/computer device access, and digital literacy were also named as important needed telemedicine metrics.
Resources available in the Inner Setting domain, such as strong information technology infrastructure, were major facilitators of telemedicine implementation at each site for LEP patients. Consistently, interpretation for telemedicine visits was the same as interpreter services prior to the pandemic: “If I have a specific question…I would contact my [bilingual] MA [medical assistant] and then we could actually do a three-way phone call. So, for me, it hasn’t changed a lot” (Participant 7, Site F). In general, the move to any specific telemedicine platform or vendor in the urgency of the pandemic did not prioritize interpretation functions; rather, sites sought to connect existing interpreter services with the new platform or vendor. As many sites already had existing telephone language lines, transitions to telephone visits were smoother once three-way calls were arranged. Video interpretation, when not conducted directly by a bilingual clinician or staff, was exceedingly rare.
As implied above, language access availability for patients relied heavily on language-concordant staff (Individual Characteristics domain). This was relevant both for appointment access, outreach, and reminders to prepare patients for a novel telemedicine visit (such as front office staff or medical assistants spending additional time helping patients log into a telemedicine visit), as well as during the telemedicine encounter (such as medical assistants providing real-time interpretation if a clinician was not language-concordant). Limited clinician comfort or willingness to engage in a non-English telemedicine visit was also a barrier.
Despite valiant efforts by primary care clinics to provide telemedicine services, multiple intersecting structural barriers impeded telemedicine access for patients with LEP (Outer Setting domain). For example, patients who speak less-represented languages, and/or languages not traditionally supported in the healthcare system, including deaf or hard of hearing patients who speak American Sign Language (ASL) and require visual interpretation, were often left behind if there were no language-concordant or fluent staff: “Our call center staff are all bilingual. So, if they speak Spanish, they're going to speak with them in Spanish, and they will select Spanish language from the appointment system. So, they’re going to get their text to get on to the system in Spanish. If it's another language, all bets are off” (Participant 4, Site C). Health literacy, availability of devices, and competing work demands were also named as external factors that impeded access for patients with LEP. Respondents highlighted that improved LEP access would include enhanced linkages and referrals to community resources to proactively support patients who are LEP with digital literacy or device access, such as technology training classes or organizations that provide devices or internet access.
DISCUSSION
Our work provides an in-depth analysis of the implementation of telemedicine services for clinics serving high proportions of patients with LEP. This is highly relevant for safety-net clinics across the state whose panels are approximately 31% LEP on average.41 This matches national data regarding safety-net clinic populations.42 Data on visit volume shows an explosive increase in telemedicine volume for clinics serving large proportions of patients with LEP. Patients with LEP in this sample were more likely to receive telephone visits, consistent with other studies showing safety-net sites are less likely to provide video visits to patients with LEP, racial/ethnic minorities, and/or patients with lower health or digital literacy.22, 29
Our qualitative analysis illustrates the resilience and resourcefulness of safety-net clinics in a time of crisis to deliver care for patients with LEP, while also identifying the underlying reasons for disparities in telemedicine visit type. Site personnel rapidly iterated workflows and processes, based on limited resources and available language-concordant staff, until arriving at workable solutions. However, despite these creative attempts, patients with LEP who spoke less-represented languages and those with low health or digital literacy were at risk of being left even further behind.
Prior work has described language-based disparities in telemedicine access.22, 30, 43–46 These primarily consist of population-level quantitative studies utilizing EHR or survey data to describe disparities in telemedicine use and modality among patients with LEP. Chang et al.’s rapid qualitative analysis of 25 providers at 8 community health centers mentioned challenges integrating interpreters into telemedicine visits, but did not report proportions of patients with LEP served. Payán et al. assessed telemedicine implementation with a focus on patients with LEP at two health centers. To our knowledge, our study is the first in-depth mixed-methods assessment of telemedicine across a diverse array of clinical sites with an emphasis on implementation for patients with LEP.47
Telemedicine disparities for patients with LEP have been a concern since the beginning of the pandemic.48–50 Our work emphasizes the importance of centering equity throughout telemedicine implementation.51 Interviewees reflected on how the rapid transformation to a new telemedicine reality benefited from utilizing existing interpreter lines and language-concordant staff to support LEP patients. This finding resonates with the prior qualitative study of two community health centers, showing a heavy reliance on bilingual providers/staff to make telemedicine work in LEP settings who also served as “transcultural providers.”47 Interviewees relied on existing bilingual staff as well as family members and children to facilitate connections to telemedicine. Although linguistically-concordant staff is important, patients who speak languages not represented by the workforce are left behind. Moreover, reliance on family or children to serve as digital navigators places unwarranted responsibility on them to facilitate care access.
We heard from many clinicians that they involved a medical assistant or care team member to interpret for telemedicine visits. This may cause additional undue burden on non-certified bilingual staff. One study found that 21% of healthcare team members (including medical assistant) who were “bilingual” and served in interpreter roles did not pass medical interpreter proficiency levels.52 Placing medical interpreter responsibilities on medical assistants may also increase strain and staff burnout; medical social workers who are asked to translate for other staff endorsed higher workloads due to performing translation yet similar caseloads overall.53
Our findings reflect the diversity of needs for LEP patients and the primacy of intersectionality,54 where patients with multiple marginalized identities including disability, immigrant status, and/or lower health or digital literacy experienced compounding barriers to telemedicine access. Although many sites opted to provide telephone visits to patients with LEP, telephone visits are predicted to not be reimbursed long term.55 Safety-net sites will need to address telemedicine equity holistically, and ensure reimbursement in a shifting policy landscape.55
From an implementation science perspective, the CFIR framework enabled us to identify the narrative of the “adaptable periphery” from participant interviews. According to this concept, core components of an intervention are adapted to the local realities of the site of implementation. The strength of this adaptability was a facility to rapidly iterate when telemedicine workflows were not successful, and resulted in care delivery that was uniquely tailored to that clinic’s circumstances. However, the weakness of this approach was lack of a proactive process to prioritize the most marginalized patients, including patients with LEP and/or low digital literacy. Rather, telemedicine implementation occurred more reactively, from the selection of telemedicine platform and its capacity to link with interpretation, a lack of telemedicine outreach that was language-concordant, provider reticence, and staff biases around what kind of encounter a patient with LEP may prefer. As telemedicine will likely remain as a significant component of outpatient care for the long term, an implementation science lens allows for clinic leaders to take stock of current access and enact processes to improve language-based equity.
Interviewees provided several suggestions for innovations to enhance telemedicine equity. A key ask from interviewees was integrated, on demand, remote interpretation services that synchronized smoothly with telemedicine platforms. Other solutions developed by interviewees included using one’s own speakerphone in a video visit and maximizing team-based telemedicine care so that medical assistants could easily utilize interpreter lines.
Our findings emphasize that equitable telemedicine access for LEP patients goes far beyond interpreter services. Clinical leaders emphasized the need for accurate telemedicine utilization data by LEP status, to direct proactive, quality improvement-focused projects to achieve access equity. Innovations such as flexible visit templates to allow more time for patients with LEP, team-based telemedicine encounters which are currently rare in safety-net visits, and community outreach and navigation services to connect patients to devices and digital skills, would reflect an investment by healthcare institutions rather than leaving patients behind. These recommendations, including assessing patient digital needs and collaborating with community partners, have been emphasized by other experts and are shared by patients when asked how to solve the digital divide.20, 56, 57
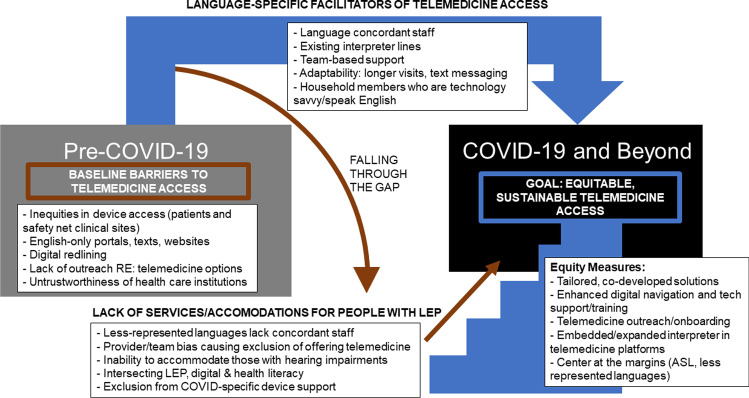
We have synthesized the results of our findings to demonstrate both the strengths and weaknesses of telemedicine implementation at safety-net primary care clinics serving patients with LEP (Fig. 3). The launch to a pandemic world of telemedicine benefited from facilitators such as language-concordant staff, family members serving as interpreters, and those with higher digital literacy. However, patients with intersecting marginalized identities fell through an implementation gap. Proactive, equity-based solutions will help ensure the digital divide does not continue to widen.
Figure 3.
Visual synthesis of strengths and weaknesses of telemedicine implementation at safety-net primary care clinics serving patients with LEP. Gray box describes baseline barriers to telemedicine access pre-COVID-19. Black box describes barriers to telemedicine access during COVID-19.
From a policy perspective, our work highlights the gaps that existed in care for patients with LEP even prior to the pandemic. Access to a professional medical interpreter is legally required as per the Civil Rights Act, Executive Order 13166, and the Affordable Care Act.58 This legally mandates all healthcare sites receiving federal funding (meaning almost all safety-net clinics) to have certified medical interpreters. However, Medicare and Medicaid do not reimburse language service expenses, although they may be claimed as administrative fees. Sadly, uptake of certified medical interpreters is variable.59, 60 A clear policy implication of this paper would be to ensure certified medical interpretation is reimbursed as it is an additional cost to healthcare centers, regardless of visit modality. Although clinics often relied on lay interpreters such as family and staff, certified medical interpreters are associated with higher quality care than lay interpreters such as bilingual staff and family members.61 Work to improve reimbursement for medical interpretation and adherence to federal mandates for certified interpreter access via telemedicine are important next steps.
Limitations
Our analysis reflects several limitations. Our project focused on clinic leaders; and thus, we did not interview patients, caregivers, nor other staff who would have valuable insights into telemedicine implementation, such as nurses, medical assistants, front desk staff, and information technology personnel. We had a relatively small sample size which precluded us from conducting comparative analysis for those serving more versus less proportions of patients with LEP. We did not summarize prevalence of each language spoken by patients across the sample, which would have enabled subgroup analyses based on specific languages and identified all languages needed to provide language-concordant care. We did not collect data at a level of detail that would enable comparison of pre-COVD professional in-person or telephone interpreter use with telehealth interpreter use. Data were collected differently at various time points; the categories for gender, race, and ethnicity could have been more expansive.62 We were not able to connect themes to specific visit modality within telemedicine, such as telephone versus video-only visits, as telephone visits were the majority of visits. We did not capture data on telemedicine funding or reimbursement, as these factors are in flux. However, study strengths include a broad range of clinical sites for qualitative study across California and a rigorous grounding in an implementation science framework.
CONCLUSIONS
Telemedicine continues to be a key driver of access for LEP patients served by the primary care safety net. Robust equity data and evaluation of telemedicine implementation, proactive access to patients speaking less-commonly represented languages, and reimbursement to allow adequate technical support for high-quality interpretation are all recommendations from frontline stakeholders. Intentional innovation at this stage will enhance our capacity to deliver equitable language access as telemedicine becomes the new normal.
Supplementary Information
(DOCX 89 kb)
Acknowledgements
The authors would like to thank all participants in the Connected Care Accelerator, and all the interviewees, Erica Shin, BA, Elaine Khoong, MD, MAS, Sofi Bergkvist, MS, MBA, and Jeanette Wong, BS.
Funding
This work was supported by The Commonwealth Fund, a national, private foundation based in New York City that supports independent research on healthcare issues and makes grants to improve healthcare practice and policy (Grant No. 20202842). The views presented here are those of the author and not necessarily those of The Commonwealth Fund, its directors, officers, or staff. The Connected Care Accelerator was supported by the California Health Care Foundation (Grant No. G-31003). Dr. Sharma was supported by K08 HS028477-01 (Agency for Healthcare Research and Quality) and KL2 TR001870 (National Center for Advancing Translational Sciences of the National Institutes of Health). Dr. Sarkar was supported by K24 CA212294 (National Cancer Institute).This paper’s contents are solely the responsibility of the authors and do not necessarily represent the official views of AHRQ nor the NIH.
Declarations:
Conflict of Interest:
Dr Sarkar received contract funding from InquisitHealth, AppliedVR, and SomnologyMD; is supported by a gift from The Doctors Company Foundation; serves as a scientific/expert advisor for nonprofit organizations HealthTech 4 Medicaid and HopeLab (no compensation); is a member of the American Medical Association’s Equity and Innovation Advisory Group (for which she receives honoraria); and previously served as a clinical advisor for Omada Health and as an advisory board member for Doximity (for which she received honoraria). Dr. Lyles received contract funding from InquisitHealth, AppliedVR, and SomnologyMD. She is currently a Visiting Researcher at Google.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Urmimala Sarkar and Courtney R. Lyles are joint senior authors
References
- 1.Selected Social Characteristics in the United States. Published 2019. Accessed May 25, 2022. https://data.census.gov/cedsci/table?q=dp02&tid=ACSDP5Y2019.DP02
- 2.Anderson TS, Karliner LS, Lin GA. Association of Primary Language and Hospitalization for Ambulatory Care Sensitive Conditions. Med Care. 2020;58(1):45–51. doi: 10.1097/MLR.0000000000001245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ponce NA, Hays RD, Cunningham WE. Linguistic Disparities in Health Care Access and Health Status Among Older Adults. Journal of General Internal Medicine. 2006;21(7):786–791. doi: 10.1111/j.1525-1497.2006.00491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rawal S, Srighanthan J, Vasantharoopan A, Hu H, Tomlinson G, Cheung AM. Association Between Limited English Proficiency and Revisits and Readmissions After Hospitalization for Patients With Acute and Chronic Conditions in Toronto, Ontario, Canada. JAMA. 2019;322(16):1605–1607. doi: 10.1001/jama.2019.13066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.John-Baptiste A, Naglie G, Tomlinson G, et al. The effect of English language proficiency on length of stay and in-hospital mortality. J GEN INTERN MED. 2004;19(3):221–228. doi: 10.1111/j.1525-1497.2004.21205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nápoles AM, Santoyo-Olsson J, Karliner LS, Gregorich SE, Pérez-Stable EJ. Inaccurate Language Interpretation and its Clinical Significance in the Medical Encounters of Spanish-speaking Latinos. Med Care. 2015;53(11):940–947. doi: 10.1097/MLR.0000000000000422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Flores G. Language Barriers to Health Care in the United States. https://doi.org/10.1056/NEJMp058316. 10.1056/NEJMp058316
- 8.Allen MP, Johnson RE, McClave EZ, Alvarado-Little W. Language, Interpretation, and Translation A Clarification and Reference Checklist in Service of Health Literacy and Cultural Respect. NAM Perspectives. Published online February 18, 2020. 10.31478/202002c [DOI] [PMC free article] [PubMed]
- 9.Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;90(8):1212–1215. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schiaffino MK, Nara A, Mao L. Language Services In Hospitals Vary By Ownership And Location. Health Affairs. 2016;35(8):1399–1403. doi: 10.1377/hlthaff.2015.0955. [DOI] [PubMed] [Google Scholar]
- 11.Fernandez A, Schillinger D, Warton EM, et al. Language Barriers, Physician-Patient Language Concordance, and Glycemic Control Among Insured Latinos with Diabetes: The Diabetes Study of Northern California (DISTANCE) J Gen Intern Med. 2011;26(2):170–176. doi: 10.1007/s11606-010-1507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saadi A, Sanchez Molina U, Franco-Vasquez A, Inkelas M, Ryan GW. Barriers and Facilitators to Implementation of Health System Interventions Aiming to Welcome and Protect Immigrant Patients: a Qualitative Study. J Gen Intern Med. 2021;36(10):3071–3079. doi: 10.1007/s11606-021-06788-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saadi A, Sanchez Molina U, Franco-Vasquez A, Inkelas M, Ryan GW. Assessment of Perspectives on Health Care System Efforts to Mitigate Perceived Risks Among Immigrants in the United States: A Qualitative Study. JAMA Network Open. 2020;3(4):e203028. doi: 10.1001/jamanetworkopen.2020.3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Title VI of the Civil Rights Act of 1964; Policy Guidance on the Prohibition Against National Origin Discrimination As It Affects Persons With Limited English Proficiency. Federal Register. Published August 30, 2000. Accessed November 14, 2021. https://www.federalregister.gov/documents/2000/08/30/00-22140/title-vi-of-the-civil-rights-act-of-1964-policy-guidance-on-the-prohibition-against-national-origin
- 15.Volk J, Palanker D, O’Brien M, Goe C. States’ Actions to Expand Telemedicine Access During COVID-19 and Future Policy Considerations. The Commonwealth Fund. 10.26099/r95z-bs17
- 16.Jun 22 EHP, 2020. State Efforts to Expand Medicaid Coverage & Access to Telehealth in Response to COVID-19. KFF. Published June 22, 2020. Accessed December 17, 2021. https://www.kff.org/coronavirus-covid-19/issue-brief/state-efforts-to-expand-medicaid-coverage-access-to-telehealth-in-response-to-covid-19/
- 17.Cantor JH, McBain RK, Pera MF, Bravata DM, Whaley CM. Who Is (and Is Not) Receiving Telemedicine Care During the COVID-19 Pandemic. Am J Prev Med. 2021;61(3):434–438. doi: 10.1016/j.amepre.2021.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uscher-Pines L, Sousa J, Jones M, et al. Telehealth Use Among Safety-Net Organizations in California During the COVID-19 Pandemic. JAMA. 2021;325(11):1106–1107. doi: 10.1001/jama.2021.0282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.López L, Green AR, Tan-McGrory A, King RS, Betancourt JR. Bridging the Digital Divide in Health Care: The Role of Health Information Technology in Addressing Racial and Ethnic Disparities. The Joint Commission Journal on Quality and Patient Safety. 2011;37(10):437–445. doi: 10.1016/S1553-7250(11)37055-9. [DOI] [PubMed] [Google Scholar]
- 20.David E. Velasquez BS, Adam L. Beckman BS, Jorge A. Rodriguez MD. The Missing Strategy in Addressing Language Barriers. The American Journal of Managed Care. 2020;27(3). Accessed June 22, 2022. https://www.ajmc.com/view/the-missing-strategy-in-addressing-language-barriers [DOI] [PubMed]
- 21.Gilson SF, Umscheid CA, Laiteerapong N, Ossey G, Nunes KJ, Shah SD. Growth of Ambulatory Virtual Visits and Differential Use by Patient Sociodemographics at One Urban Academic Medical Center During the COVID-19 Pandemic: Retrospective Analysis. JMIR Medical Informatics. 2020;8(12):e24544. doi: 10.2196/24544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rodriguez JA, Betancourt JR, Sequist TD, Ganguli I. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care. 2021;27(1):21–26. doi: 10.37765/ajmc.2021.88573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park J, Erikson C, Han X, Iyer P. Are State Telehealth Policies Associated With The Use Of Telehealth Services Among Underserved Populations? Health Affairs. 2018;37(12):2060–2068. doi: 10.1377/hlthaff.2018.05101. [DOI] [PubMed] [Google Scholar]
- 24.Chang JE, Lindenfeld Z, Albert SL, et al. Telephone vs. Video Visits During COVID-19: Safety-Net Provider Perspectives. J Am Board Fam Med. 2021;34(6):1103–1114. doi: 10.3122/jabfm.2021.06.210186. [DOI] [PubMed] [Google Scholar]
- 25.Benjenk I, Franzini L, Roby D, Chen J. Disparities in Audio-only Telemedicine Use Among Medicare Beneficiaries During the Coronavirus Disease 2019 Pandemic. Medical Care. 2021;59(11):1014–1022. doi: 10.1097/MLR.0000000000001631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reed ME, Huang J, Graetz I, et al. Patient Characteristics Associated With Choosing a Telemedicine Visit vs Office Visit With the Same Primary Care Clinicians. JAMA Netw Open. 2020;3(6):e205873. doi: 10.1001/jamanetworkopen.2020.5873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nouri S, Khoong EC, Lyles CR, Karliner L. Addressing Equity in Telemedicine for Chronic Disease Management During the Covid-19 Pandemic. NEJM Catalyst Innovations in Care Delivery. Published online May 4, 2020. Accessed November 13, 2021. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0123
- 28.Eberly LA, Khatana SAM, Nathan AS, et al. Telemedicine Outpatient Cardiovascular Care During the COVID-19 Pandemic. Circulation. 2020;142(5):510–512. doi: 10.1161/CIRCULATIONAHA.120.048185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hsueh L, Huang J, Millman AK, et al. Disparities in Use of Video Telemedicine Among Patients With Limited English Proficiency During the COVID-19 Pandemic. JAMA Network Open. 2021;4(11):e2133129. doi: 10.1001/jamanetworkopen.2021.33129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rodriguez JA, Saadi A, Schwamm LH, Bates DW, Samal L. Disparities In Telehealth Use Among California Patients With Limited English Proficiency. Health Affairs. 2021;40(3):487–495. doi: 10.1377/hlthaff.2020.00823. [DOI] [PubMed] [Google Scholar]
- 31.Merid B, Robles MC, Nallamothu BK. Digital Redlining and Cardiovascular Innovation. Circulation. 2021;144(12):913–915. doi: 10.1161/CIRCULATIONAHA.121.056532. [DOI] [PubMed] [Google Scholar]
- 32.Skinner B, Levy H, Burtch T. Digital redlining: the relevance of 20th century housing policy to 21st century broadband access and education. EdWorking Paper, Retrieved from Annenberg Institute at Brown University. 2021;21(471):10.26300/Q9AV-9C93. [Google Scholar]
- 33.Vogels E a. Digital divide persists even as Americans with lower incomes make gains in tech adoption. Pew Research Center. Accessed November 13, 2021. https://www.pewresearch.org/fact-tank/2021/06/22/digital-divide-persists-even-as-americans-with-lower-incomes-make-gains-in-tech-adoption/
- 34.Atske S, Perrin R. Home broadband adoption, computer ownership vary by race, ethnicity in the U.S. Pew Research Center. Accessed November 14, 2021. https://www.pewresearch.org/fact-tank/2021/07/16/home-broadband-adoption-computer-ownership-vary-by-race-ethnicity-in-the-u-s/
- 35.Connected Care Accelerator. Center for Care Innovations. Accessed January 12, 2021. https://www.careinnovations.org/programs/connected-care-accelerator/
- 36.Uniform Data System Reporting Requirements for 2022 Health Center Data. Bureau of Primary Health Care; 2022. https://bphc.hrsa.gov/sites/default/files/bphc/data-reporting/2022-uds-manual.pdf
- 37.Walker D, Myrick F. Grounded theory: an exploration of process and procedure. Qual Health Res. 2006;16(4):547–559. doi: 10.1177/1049732305285972. [DOI] [PubMed] [Google Scholar]
- 38.Damschroder LJ, Lowery JC. Evaluation of a large-scale weight management program using the consolidated framework for implementation research (CFIR) Implement Sci. 2013;8(1):51. doi: 10.1186/1748-5908-8-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Damschroder L, Aron D, Keith R, Kirsh S, Alexander J, Lowery J. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation science : IS. 2009;4. 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed]
- 40.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 41.Community Health Centers: 2021 State Profile. California Primary Care Association; 2021. https://www.dropbox.com/s/fk25l6guc1prqv0/2021_CPCA_CAstateprofile.pdf?dl=0
- 42.Serving Patients with Limited English Proficiency: Results of a Community Health Center Survey. National Association of Community Health Centers; 2008. http://nachc.org/wp-content/uploads/2015/06/LEPReport.pdf
- 43.Eberly LA, Kallan MJ, Julien HM, et al. Patient Characteristics Associated With Telemedicine Access for Primary and Specialty Ambulatory Care During the COVID-19 Pandemic. JAMA Netw Open. 2020;3(12):e2031640. doi: 10.1001/jamanetworkopen.2020.31640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pagán VM, McClung KS, Peden CJ. An Observational Study of Disparities in Telemedicine Utilization in Primary Care Patients Before and During the COVID-19 Pandemic. Telemed J E Health. Published online December 20, 2021. 10.1089/tmj.2021.0412 [DOI] [PubMed]
- 45.Sachs JW, Graven P, Gold JA, Kassakian SZ. Disparities in telephone and video telehealth engagement during the COVID-19 pandemic. JAMIA Open. 2021;4(3):ooab056. doi: 10.1093/jamiaopen/ooab056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.El-Toukhy S, Méndez A, Collins S, Pérez-Stable EJ. Barriers to Patient Portal Access and Use: Evidence from the Health Information National Trends Survey. J Am Board Fam Med. 2020;33(6):953–968. doi: 10.3122/jabfm.2020.06.190402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Payán DD, Frehn JL, Garcia L, Tierney AA, Rodriguez HP. Telemedicine implementation and use in community health centers during COVID-19: Clinic personnel and patient perspectives. SSM - Qualitative Research in Health. 2022;2:100054. doi: 10.1016/j.ssmqr.2022.100054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nguyen MLT, Garcia F, Juarez J, et al. Satisfaction can co-exist with hesitation: qualitative analysis of acceptability of telemedicine among multi-lingual patients in a safety-net healthcare system during the COVID-19 pandemic. BMC Health Serv Res. 2022;22(1):195. doi: 10.1186/s12913-022-07547-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rodriguez JA, Clark CR, Bates DW. Digital Health Equity as a Necessity in the 21st Century Cures Act Era. JAMA. 2020;323(23):2381–2382. doi: 10.1001/jama.2020.7858. [DOI] [PubMed] [Google Scholar]
- 50.Khoong EC. Policy Considerations To Ensure Telemedicine Equity. Health Aff (Millwood). 2022;41(5):643–646. doi: 10.1377/hlthaff.2022.00300. [DOI] [PubMed] [Google Scholar]
- 51.Lyles C, Sharma A, Fields J, Getachew Y, Sarkar U, Zephyrin L. Centering Health Equity in Telemedicine. Annals of Family Medicine. Accepted, In Press;20(4). [DOI] [PMC free article] [PubMed]
- 52.Moreno MR, Otero-Sabogal R, Newman J. Assessing Dual-Role Staff-Interpreter Linguistic Competency in an Integrated Healthcare System. J GEN INTERN MED. 2007;22(S2):331–335. doi: 10.1007/s11606-007-0344-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Engstrom DW, Piedra LM, Min JW. Bilingual Social Workers: Language and Service Complexities. Administration in Social Work. 2009;33(2):167–185. doi: 10.1080/03643100902768832. [DOI] [Google Scholar]
- 54.Crenshaw. Demarginalizing the Intersection of Race and Sex: A Black Feminist Critique of Antidiscrimination Doctrine, Feminist Theory and Antiracist Politics. University of Chicago Legal Forum. 1989(1). Accessed April 12, 2022. https://chicagounbound.uchicago.edu/uclf/vol1989/iss1/8
- 55.Goodman R, Lacktman N, Ferrante T. Medicare Telehealth Services for 2023 – CMS Proposes Substantial Changes | Foley & Lardner LLP. Health Care Law Today. Published July 14, 2022. Accessed July 28, 2022. https://www.foley.com/en/insights/publications/2022/07/medicare-telehealth-services-2023-cms-changes
- 56.Alkureishi MA, Choo ZY, Rahman A, et al. Digitally Disconnected: Qualitative Study of Patient Perspectives on the Digital Divide and Potential Solutions. JMIR Hum Factors. 2021;8(4):e33364. doi: 10.2196/33364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Anaya YBM, Mota AB, Hernandez GD, Osorio A, Hayes-Bautista DE. Post-Pandemic Telehealth Policy for Primary Care: An Equity Perspective. J Am Board Fam Med. 2022;35(3):588–592. doi: 10.3122/jabfm.2022.03.210509. [DOI] [PubMed] [Google Scholar]
- 58.Basu G, Costa VP, Jain P. Clinicians’ obligations to use qualified medical interpreters when caring for patients with limited English proficiency. AMA journal of ethics. 2017;Mar 1;19(3):245–52. doi: 10.1001/journalofethics.2017.19.3.ecas2-1703. [DOI] [PubMed] [Google Scholar]
- 59.Lion KC, Gritton J, Scannell J, et al. Patterns and Predictors of Professional Interpreter Use in the Pediatric Emergency Department. Pediatrics. 2021;147(2):e20193312. doi: 10.1542/peds.2019-3312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schulson LB, Anderson TS. National Estimates of Professional Interpreter Use in the Ambulatory Setting. J GEN INTERN MED. 2022;37(2):472–474. doi: 10.1007/s11606-020-06336-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727–754. doi: 10.1111/j.1475-6773.2006.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Charting a Course for an Equity-Centered Data System. Robert Wood Johnson Foundation | National Commission to Transform Public Health Data Systems; 2021. Accessed October 5, 2022. https://www.rwjf.org/en/library/research/2021/10/charting-a-course-for-an-equity-centered-data-system.html
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 89 kb)