Abstract
Electroconvulsive therapy (ECT) is one of the most efficacious interventions for treatment-resistant depression. Despite its efficacy, ECT’s neural mechanism of action remains unknown. Although ECT has been associated with “slowing” in the electroencephalogram (EEG), how this change relates to clinical improvement is unresolved. Until now, increases in slow-frequency power have been assumed to indicate increases in slow oscillations, without considering the contribution of aperiodic activity, a process with a different physiological mechanism. In this exploratory study of nine MDD patients, we show that aperiodic activity, indexed by the aperiodic exponent, increases with ECT treatment. This increase better explains EEG “slowing” when compared to power in oscillatory peaks in the delta (1–3 Hz) range and is correlated to clinical improvement. In accordance with computational models of excitation-inhibition balance, these increases in aperiodic exponent are linked to increasing levels of inhibitory activity, suggesting that ECT might ameliorate depressive symptoms by restoring healthy levels of inhibition in frontal cortices.
Subject terms: Neuroscience, Depression, Biomarkers
Introduction
Since its introduction as a treatment for psychotic disorders more than 80 years ago, electroconvulsive therapy (ECT) has been widely used to treat affective illness. Indeed, ECT is the most efficacious treatment for Major Depressive Disorder (MDD), and it is often the preferred treatment for individuals who have failed to respond to numerous antidepressant trials. Similarly, ECT is the preferred treatment option for patients who are severely ill and require rapid relief of symptoms (e.g., due to active suicidality, psychotic depression or depression associated with loss of appetite and severe weight loss). One study showed that up to 80% of patients with treatment-resistant depression responded to ECT and many achieved full remission of their symptoms and were able to resume normal functioning [1]. In extreme cases of MDD involving suicidal intent, a 10-session course of ECT can rapidly reduce suicidal thoughts and acts, as reported by one multisite collaborative study of over 100 patients [2].
Given how well established, widely used, and clinically effective ECT is for the treatment of psychiatric conditions, it is surprising that its precise neural mechanism of action has not yet been identified. This is, however, not to say that no neural effects of ECT have been identified. Perhaps the most widely replicated observation is that ECT is associated with a “slowing” of the electroencephalogram (EEG). Specifically, patients who receive ECT display increases in “slower”, or lower-frequency, delta (1–3 Hz) and theta (3–8 Hz) band power [3–8]. This “slowing” is observable both acutely, after any single treatment, and longitudinally over the course of a multi-session course of ECT [9]. Despite this, the neural mechanism behind EEG slowing remains unclear. In addition, how this increase in spectral power in the low-frequency range is related to clinical outcome remains ambiguous [10]: several studies link EEG “slowing” to clinical ECT improvement [4, 5, 11–13], some show the inverse relationship [14, 15], and others find no significant relationship [7, 16–18].
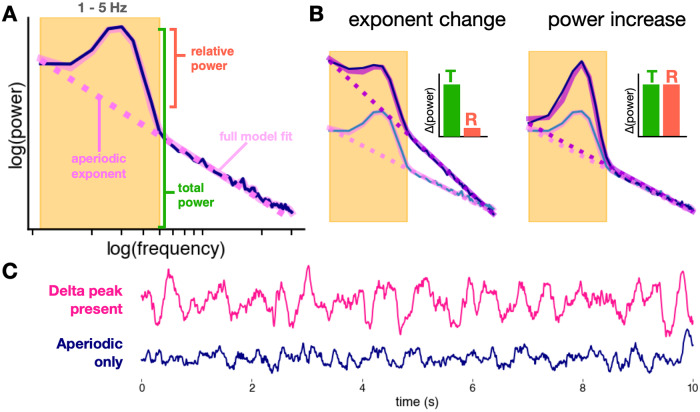
Although EEG “slowing” is one of the largest and most consistent effects in the ECT literature, it is not the only electrophysiological feature that has been associated with ECT treatment. For instance, decreases in alpha power [6], decreases in beta and gamma power [18], and increases in total spectral power (<30 Hz) [4, 7, 16] have all been observed with ECT. We hypothesize that these effects are actually the result of a change in a single, often overlooked EEG process: a change in aperiodic activity (Fig. 1). Specifically, we hypothesize that the plethora of EEG alterations observed in depression and in ECT treatment may be more parsimoniously explained by a change in aperiodic EEG activity. This interpretation may help disambiguate past observations of changes in spectral band power while simultaneously being better grounded by theoretical models of the physiological generators of aperiodic activity [19].
Fig. 1. Hypothesis (aperiodic vs. oscillatory delta).
A Spectral parameterization quantifies the power spectrum as a composite of periodic and aperiodic components. Unlike traditional band power measures that conflate periodic and aperiodic activity, oscillatory power is defined as relative power above the aperiodic component (pink dashed line). B Increases in the aperiodic exponent can cause apparent increases in total (T) band power, while power relative (R) to the aperiodic component remains unchanged. True increases in oscillatory power show increases in both total power and relative power. C Delta in the EEG trace vs. aperiodic activity. EEG with delta oscillations (where a delta peak is present in the spectra) is visibly different from EEG with only aperiodic activity, though both can qualitatively look like EEG “slowing”. Only 4/9 EEG patients had delta peaks in their spectra for every session and 6/9 had a delta peak for any session.
To understand aperiodic activity, it is important to contrast it with the more well-studied periodic—or oscillatory—activity. Methodologically, aperiodic and oscillatory activity are both reflected in the power spectrum of EEG data. While oscillatory power is concentrated at specific frequencies, neural power spectra also exhibit a broadband 1/fχ scaling, where power is inversely proportional to frequency. The aperiodic exponent, χ, characterizes the slope of the power spectrum (Fig. 1A). An increase in the aperiodic exponent would cause a “steepening” rotation in the power spectrum, producing a large, consistent increase in low-frequency power (Fig. 1B). This rotation could additionally produce apparent increases in total power, and/or decreases in alpha, beta, and gamma power depending on the spectral rotation frequency, like the fulcrum of a lever [20, 21]. Changes in the aperiodic component have been linked to cognitive and perceptual states [21, 22], development [23], aging [24], anesthesia [25], and disease states such as ADHD [26] and schizophrenia [27]. Aperiodic activity has also been linked to the physiological effects of deep brain stimulation treatment for major depressive disorder [28].
Importantly, if changes in the aperiodic exponent are not controlled for in analyses, changes in spectral band power can be misinterpreted as changes in oscillatory power, even where no true oscillation exists. Recent methods allow for explicitly separating oscillations and aperiodic activity [20, 29]. Because neural oscillations likely have fundamentally different physiological origins than aperiodic activity [30–32], conflating the two can lead to false conclusions about the neurobiological underpinnings of a particular electrophysiological change, which in turn can impact the development of more effective, targeted treatments. Thus far, analyses of EEG power spectra from ECT studies have not looked at aperiodic activity, but rather have measured power in the delta and theta ranges, under the assumption that power in those bands is equivalent to the existence of an oscillation in that frequency. Here, we investigate the hypothesis that ECT produces an increase, or steepening, in the aperiodic exponent in a population of 9 patients with MDD receiving a 12-session treatment of ECT. We analyze aperiodic and oscillatory EEG from frontal electrodes before and after approximately every fourth ECT session, repeating this procedure periodically throughout a full course of ECT. To test the aperiodic hypothesis, we compare changes in the aperiodic exponent to changes in canonical delta band power and delta oscillatory power as measured via spectral parameterization. We find that, acutely, increases in the aperiodic exponent better explain the observed increases in delta band power post-ECT, as opposed to true increases in delta oscillation power. Furthermore, we demonstrate that the aperiodic exponent continues to increase longitudinally through a course of ECT treatment and that the magnitude of this increase is related to clinical symptom improvement, an effect not seen in canonical delta band power. These results identify aperiodic activity as a promising avenue for further research on the mechanism of ECT, especially in light of the relationship of aperiodic activity to excitation-inhibition balance [32] and the cortical inhibition theory of depression [33].
Results
Clinical effects
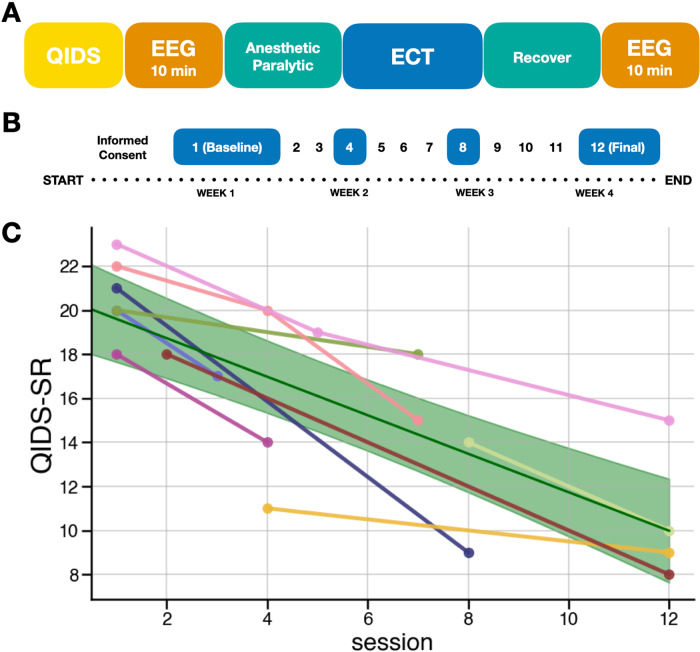
The severity of depressive symptomatology as measured by the QIDS-SR decreased over the course of a 12-session ECT treatment for all nine patients included in the study (β = −0.87, p = 7.42 × 10−12, 95% CI[−1.12, −0.62]), demonstrating the efficacy of ECT as a treatment of MDD (Fig. 2C).
Fig. 2. Schematic of the study.
A Single session process to capture acute effects of ECT on EEG. B An example of the longitudinal protocol, in which the single session process for EEG is repeated at ECT treatment sessions 1, 4, 8, and 12. C Clinical symptoms improve over the course of ECT treatment as measured by the Quick Inventory of Depressive Symptomatology–Self Report (QIDS-SR) scale (β = −0.87, p = 7.42 × 10−12). The solid green line is the population-level model prediction, with shaded areas representing the 95% confidence interval of the prediction. Due to the constraints of recording in a clinical environment, a complete set of EEG recordings/clinical ratings was not possible for every subject, but subjects were included with a minimum of 2 sessions of pre- and post-ECT EEG recording (n = 9).
Acute EEG effects
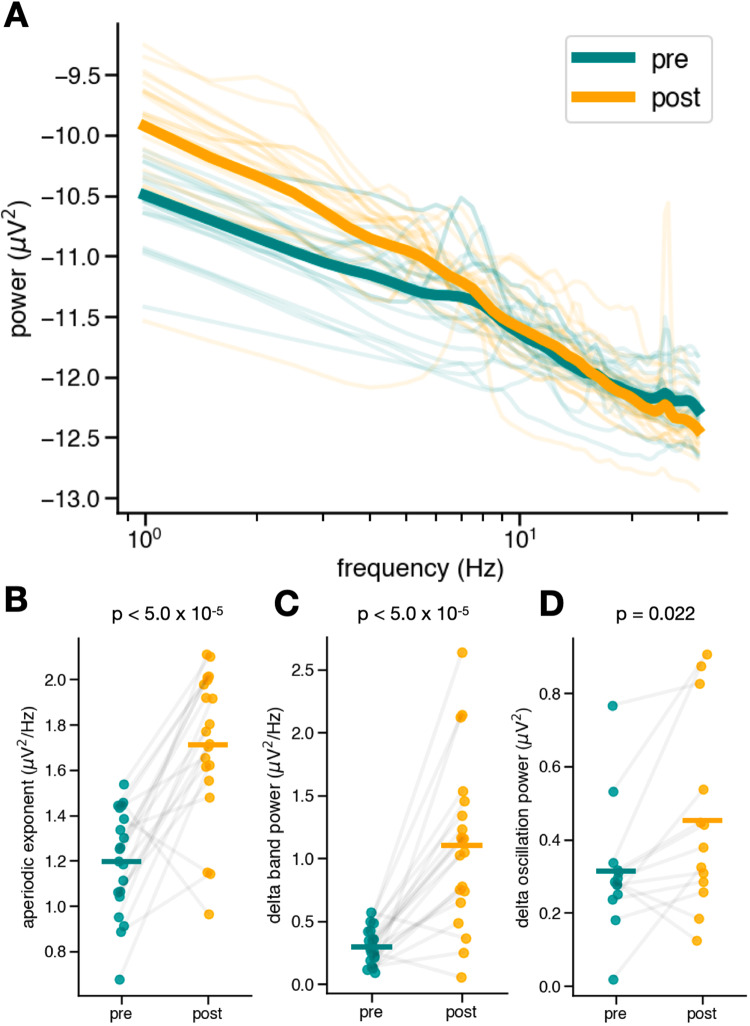
Following a session of ECT, EEG signals recorded from frontal electrodes displayed a significant increase in aperiodic exponent (pre = 1.20 ± 0.23 μV2 Hz−1, post = 1.71 ± 0.32 μV2 Hz−1; t(19) = −5.98, dz = 1.81, p = 9.20 × 10−6). This increase appears as a striking steepening of the power spectrum, with the average spectra across channels and subjects seeming to “rotate” around a frequency between 20 and 22 Hz (Fig. 3A, B).
Fig. 3. Acute effects.
A Power spectra of frontal electrodes pre- and post-ECT treatment. There is a visible “steepening” of the spectrum after ECT treatment. B The aperiodic exponent of the power spectra pre- and post-ECT treatment, averaged across frontal electrodes for each patient. There is a large, highly significant (t(19) = −5.98, dz = 1.81, p = 9.20 × 10−6) increase in the aperiodic exponent for almost every patient. C Delta (1–3 Hz) band power pre- and post-ECT treatment, averaged across frontal electrodes for each patient. When measured canonically, not controlling for the aperiodic exponent, a large, significant increase (t(19) = −5.73, dz = 1.70, p = 1.59 × 10−5) in delta band power appears. D There is a small, yet significant increase in true oscillatory peak power in the delta range (t(12) = −2.62, dz = 0.63, p = 0.022). Only 6/9 patients had a detectable delta oscillation pre- and post-ECT for any session. The effect size of the delta band power increase is more similar in magnitude to that of the aperiodic increase than the effect size of the delta oscillation power.
We also observe the expected acute increase in delta band power (pre = 0.30 ± 0.14 μV2 Hz−1, post = 1.10 ± 0.65 μV2 Hz−1; t(19) = −5.73, dz = 1.70, p = 1.59 x 10−5) (Fig. 3C). However, the apparent EEG “slowing” effect is largely driven by the observed steepening of aperiodic activity; after controlling for changes in the aperiodic exponent (decomposing oscillatory and non-oscillatory estimates of PSD), oscillatory delta power changes were much less pronounced (pre = 0.31 ± 0.17 μV2, post = 0.45 ± 0.26 μV2 t(12) = −2.62, dz = 0.63, p = 0.022) (Fig. 3D). Oscillatory delta power in pre-ECT recordings was not parametrically distributed, but a non-parametric Wilcoxon signed-rank test returned a similar result (W(12) = 15.0, p = 0.033). The effect size of the increase in delta band power is comparable to that of the increase in aperiodic activity, more so than the effect size of the change in delta oscillation power. Crucially, only four out of the nine patients had a detectable delta oscillation in frontal electrodes for every session and only six out of the nine had a detectable delta oscillation in frontal electrodes in any session. This highlights the importance of spectral parameterization to detect oscillations. These results suggest that the well-replicated effect of ECT on delta band power is largely driven by the aperiodic exponent increase, instead of an increase in the power of an oscillation in the delta band.
Longitudinal EEG effects
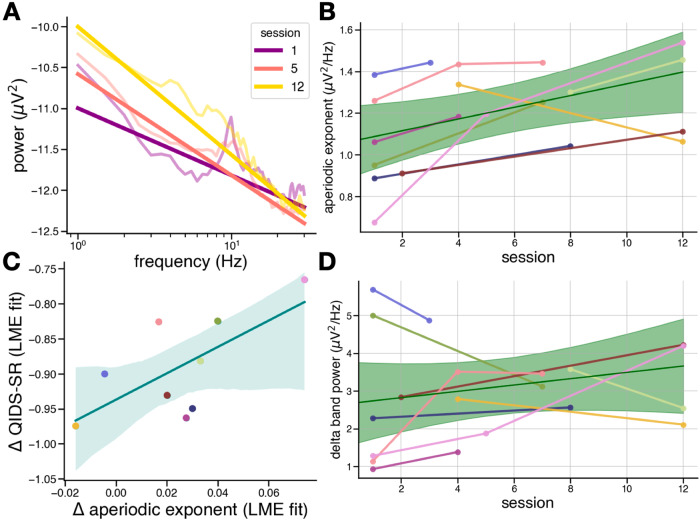
The acute effect of ECT on EEG activity is potentially confounded by the effects of the anesthetic used during ECT treatment. Therefore, it is critical to also assess longitudinal changes in ECT treatment. To do this, we examined EEG activity across treatment days, before the introduction of anesthesia (Fig. 2). We found that the aperiodic exponent in frontal electrodes increases with repeated ECT treatments throughout a 12-session ECT course, as modeled by a linear mixed-effects model (β = 0.027, p = 0.018, 95% CI[0.005, 0.048]) (Fig. 4A, B).
Fig. 4. Longitudinal effects.
A Power spectra and aperiodic fits (straight lines) for average frontal PSDs for a single patient at three pre-treatment sessions. B Aperiodic exponent significantly increases longitudinally (β = 0.027, p = 0.018). The solid green line is the population-level model prediction, with shaded areas representing the 95% confidence interval of the prediction. C Across patients, improvements in QIDS-SR scores, as quantified by the coefficients of a linear mixed-effects (LME) model fit to the data, are correlated to the increase in aperiodic exponent (r = 0.68, p = 0.046); however, this correlation should be interpreted with caution due to the small sample size. The solid teal line is the population-level model prediction, with shaded areas representing the 95% confidence interval of the prediction. D Delta band power does not significantly change longitudinally (β = 0.072, p = 0.269).
Unlike some previous studies that have found longitudinal increases in canonical delta band power, we find no significant effect of treatment on delta band power (β = 0.072, p = 0.269, 95% CI[−0.056, 0.201]) (Fig. 4D). This finding highlights the importance of spectral parameterization and its ability to disambiguate aperiodic and oscillatory activity, thereby allowing us to identify the longitudinal increase in aperiodic activity, a result which would have been impossible using only canonical band power.
Clinical improvement and the aperiodic exponent vs. delta band power
The longitudinal increase in aperiodic exponent significantly tracks clinical improvement in this cohort of MDD patients receiving ECT, as indexed by QIDS-SR assessment (Fig. 4C). We extracted the linear mixed-effects coefficients (β) and intercepts of each variable (aperiodic exponent and QIDS-SR score) as it improved over repeated sessions for each patient. Each coefficient represents the rate of change for each variable with repeated treatments, and each intercept represents a proxy for a baseline measurement, as only 6 out of 9 patients had a baseline EEG recording. We then performed a Pearson correlation of the rates of QIDS-SR improvement and exponent increase for each patient and found a significant relationship (r = 0.68, p = 0.046, 95% CI[0.02, 0.92]), in which greater improvements in clinical severity were associated with smaller longitudinal increases in aperiodic exponent. Additionally, we found no significant correlation between clinical improvement and delta band power (r = 0.086, p = 0.83, 95% CI[−0.61, 0.71]).
The observation that a greater improvement in QIDS-SR is associated with less of a change in aperiodic activity over ECT treatment is counterintuitive; however, there is a strong correlation between the change in aperiodic activity over treatment and the baseline aperiodic activity (r = −0.89, p = 0.001, 95% CI[−0.98, −0.54]). This means that patients whose baseline aperiodic activity was steepest showed the least amount of aperiodic steepening with treatment. When we perform a multiple linear regression, the change in QIDS-SR is related to both the change in aperiodic activity and the baseline aperiodic activity (Radj2 = 0.67, F(2, 6) = 9.16, p = 0.015). Importantly, after controlling for baseline aperiodic activity, the correlation between change in QIDS-SR and change in aperiodic activity remains significant (t = 3.92, p = 0.008). Additionally, when controlling for the change in aperiodic activity, the correlation between QIDS-SR and baseline aperiodic activity is also significant (t = 2.69, p = 0.036). In other words, patients whose baseline aperiodic activity was already steep showed the smallest amount of aperiodic steepening and the greatest change in QIDS-SR.
However, these results should be considered exploratory and be interpreted with caution due to the small sample of the cohort included in this study. For example, a non-parametric Spearman rank correlation suggests a weaker correlation (Spearman’s ρ = 0.63 p = 0.067, 95% CI[−0.05, 0.91]), and an analysis of the Cook’s difference value indicates that the Pearson correlation was influenced by a single patient. More investigation is needed to definitively identify a relationship between changes in aperiodic activity and reduction of symptom severity for patients with MDD.
Discussion
The observations that the aperiodic exponent increases as an acute effect of ECT and that it continues to increase throughout a course of multi-session ECT treatment are novel and present a promising avenue for future research. Specifically, if supported by future evidence, the observation that frontal aperiodic activity increases in ECT has the potential to connect long-standing EEG evidence to a potential mechanism of action. Although the exact physiological processes that produce the aperiodic activity indexed by the aperiodic exponent have not been precisely identified, one simple, yet promising, model suggests aperiodic activity in the local field potential (LFP) represents a summation of postsynaptic and transmembrane currents in a region [31]. A simplified model of excitatory glutamatergic and inhibitory GABAergic activity was able to capture changes in the aperiodic exponent [32]. In that model, the aperiodic exponent indexes the ratio of excitatory (E) to inhibitory (I) potentials present in the LFP, or excitation/inhibition (EI) balance. Specifically, the model indicates that a population of neurons with an EI balance biased toward a greater proportion of inhibitory activity would produce a more steeply sloped power spectrum and thus, a larger aperiodic exponent, than a population with an EI balance biased toward excitation. Normal changes in EI balance have been related to aspects of cognition, perception, and brain state [25] and dysfunctions in EI balance have been linked to several neuropsychiatric and mood disorders, including MDD [34, 35].
This model of aperiodic activity and its relationship to EI balance is especially pertinent in light of the cortical inhibition theory of depression. This theory states that patients experiencing symptoms of MDD have insufficient or dysfunctional inhibitory processes in various brain areas, including frontal cortices [33, 36]. Specifically, these patients have insufficient GABAergic activity, reflected by reduced numbers of GABA neurons in the prefrontal cortex [37]. The prefrontal cortex plays an essential role in regulating EI balance in distributed networks throughout the brain [38] and therefore, disruptions in EI balance in the prefrontal cortex could have widespread consequences affecting multiple networks, including limbic structures [39] and the serotonergic and noradrenergic systems targeted by pharmacological antidepressants [40].
The cortical inhibition theory has accumulated support from electrophysiology [41], proton magnetic resonance spectroscopy [42, 43], and cell type-specific molecular genetics [44], all of which highlight an abnormally low level of GABAergic activity in patients suffering from depression. Pharmacologically, this imbalance has been treated using factors that directly or indirectly reduce excitatory glutamatergic activity and increase inhibition with GABA agonists [34]. Treatments for depression, including ECT and serotonin-reuptake inhibitor antidepressants, have been shown to increase cortical GABA concentrations using proton magnetic resonance spectroscopy [45, 46]. However, the link to how the electrophysiological changes seen with ECT could be reflecting changes in EI balance has not yet been established [47]. In line with cortical inhibition theory, one proposed mechanism of ECT is that ECT ameliorates the symptoms of depression by directly inducing inhibitory activity over large portions of the cortex, causing widespread changes in functional connectivity and network dynamics [48]. The data presented here supports this proposed mechanism, suggesting that ECT increases inhibition as indexed by the aperiodic exponent of the power spectrum.
Although cortical inhibition theory has accumulated support from the multi-modal studies described above and is supported by the results of this exploratory EEG study, it is not the only theory of depression and the mechanisms underlying the efficacy of ECT. Patients with MDD have also been observed to have reductions in anatomical volume, particularly in the hippocampus and amygdala [49]. Other theories cite disruptions in network connectivity across brain regions [50]. Hemispheric differences in EEG measures have also been a popular subject of MDD research, the most well-known being frontal alpha asymmetry [51] (however, recent high-powered meta-analyses have not been able to replicate this result [52, 53]). Furthermore, we found no significant hemispheric differences in any of the measures used in our analyses including the aperiodic exponent, delta band power, or delta oscillatory power (Supplementary Fig. 1). It is important to note that most of the patients included in our study received bilateral stimulation during ECT and therefore, hemispheric differences might be less pronounced. Future investigations are needed to assess the relationship between stimulation laterality and potential hemispheric differences in EEG measures like aperiodic activity.
Questions remain about whether the aperiodic exponent is a suitable non-invasive indicator for depression treatment response. We found a significant relationship between the degree of clinical symptom improvement and aperiodic exponent change, given that the directionality of the relationship indicates that larger increases in exponent are associated with smaller improvements in depressive symptomatology. Although counterintuitive, this is not incongruent with our interpretation that ECT restores aperiodic activity to healthy levels. Both baseline aperiodic activity and the change in aperiodic exponent throughout treatment are significantly related to treatment response. Specifically, patients who exhibit the lowest aperiodic activity (“flatter” spectra) at baseline show the greatest increases (“steepening”) in aperiodic exponent, but they also show smaller improvements in clinical symptoms. We hypothesize that patients who begin treatment with lower aperiodic activity have the greatest capacity to show increases in aperiodic exponent because they have more “room to improve”. However, baseline aperiodic activity can also bias treatment response, where patients who begin ECT with elevated aperiodic activity might be more sensitive to ECT, thereby exhibiting a greater therapeutic response. These exploratory results present testable hypotheses regarding the role of aperiodic activity, both longitudinally and at baseline, in the therapeutic neural mechanism of ECT.
While promising, the size of the cohort included in this study was limited due to constraints of a clinical environment and restrictions around research during the COVID-19 pandemic, potentially leading to underpowered analyses of relationships between EEG and clinical improvement. At the relatively short timescales of a 4-week ECT treatment, ECT-induced restoration of inhibition might also not be related to clinical improvement. For instance, a recent method for estimating EI balance using spectral dynamic causal modeling for RS-fMRI found no relationship between treatment effectiveness and changes in EI balance when patients were scanned before and after treatment [54]. Furthermore, due to ethical considerations and the exploratory nature of this study, the analysis described here did not include a control group of healthy adults receiving ECT or of MDD patients receiving a sham ECT treatment. The lack of a control condition limits the generalizability of these results. However, the profound and significant within-patient, longitudinal increase in frontal aperiodic activity still presents a novel electrophysiological finding and a promising avenue for a potential mechanism of function for ECT in MDD.
Although the short timescale of this study prohibits us from drawing firm conclusions about long-term changes in aperiodic activity and its relationship to the clinical efficacy of ECT, other studies have shown abnormally elevated levels of slow-frequency activity in EEG persisting weeks to months post-treatment [16, 55, 56]. Like the results seen in this study, this increase in slow-frequency power might be better explained by an increase in the aperiodic exponent, potentially suggesting a similar inhibition-related mechanism for ECT at longer timescales. Whether the aperiodic exponent could be used to predict treatment response from ECT, or from other treatment methods such as TMS or various pharmacological interventions, remains an open but enticing path for understanding the neurobiological basis for individualized treatment of MDD.
Methods
Participants
Nine patients with a diagnosis of MDD as per the Diagnostic and Statistical Manual of Mental Disorders V were included in the study. Patients were recruited from the population of patients preparing to undergo ECT as part of their regular clinical treatment. Only patients with complete EEG recordings pre- and post-ECT treatment from at least two sessions were included in the present analysis. Written informed consent was provided by all patients and the study received ethical approval from the Veterans Association San Diego Health System (VASDHS) Institutional Research Board under the protocol H150012.
Electroconvulsive therapy
ECT was administered three times per week according to VASDHS protocol. ECT was administered with a square wave, constant-current, brief-pulse device Thymatron System IV. Treatment was provided clinically at the discretion of the provider. Per standing clinical protocol, treatments were generally initiated at 5–10%, with subsequent treatments adjusted according to electrode placement (2x threshold for bilateral, 6x threshold for unilateral) with further adjustments as needed based upon seizure quality and duration (with a target of at least 30 s by EEG.) ECT was administered three times per week. See Table 1 for measures used per patient. Methohexital and succinylcholine were the typical anesthetic medications used (see Table 1). Treatment termination was based on response, clinical factors, and/or the patient’s expressed wish to discontinue ECT.
Table 1.
Patient demographics, clinical characteristics, and ECT treatment information.
| Demographics | CLINICAL INFORMATION | ECT INFORMATION | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ID | Sex (M/F) | Age | Dx | QIDS | Antidepressant | Mood stabilizer | BZD | Antipsychotic | Stimulant | Tx # | Total Tx | Laterality | Pulse width (msec) | Stimulus (%) | Seizure (sec) | Anesthesia |
| 1 | FTM | 30 s | MDD, PTSD, Unspecified anxiety |
21 9 |
DUL DUL |
1 8 |
10 10 |
BL RUL |
0.3 0.5 |
10 50 |
300 117 |
MTX, SUX MTX, SUX, Alfent, CAFF |
||||
| 2 | M | 50 s |
MDD, PTSD, Alcohol use d/o |
20 17 |
VEN VEN |
Lithium Lithium |
1 3 |
3 3 |
BL BL |
0.5 0.5 |
30 30 |
69 76 |
MTX, SUX MTX, SUX |
|||
| 3 | F | 40 s | MDD, PTSD, Eating d/o |
20 18 |
FLU, BUP NTP |
1 7 |
9 9 |
BL BL |
0.5 0.5 |
10 40 |
163 50 |
MTX, SUX MTX, SUX, CAFF |
||||
| 4 | M | 60 s |
MDD, Alcohol use d/o |
14 10 |
MIR MIR |
Quetiapine Quetiapine |
8 12 |
12 12 |
BL BL |
0.5 0.5 |
75 100 |
38 36 |
MTX, SUX, CAFF MTX, SUX, CAFF |
|||
| 5 | M | 40 s |
Bipolar II d/o, Polysubstance abusea |
11 9 |
BUP, DUL BUP, DUL |
Lurasidone Lurasidone |
4 12 |
12 12 |
BL BL |
0.5 0.5 |
60 100 |
36 59 |
MTX, SUX MTX, SUX, Alfent, CAFF, Glycopyr |
|||
| 6 | M | 60 s |
Bipolar II d/o, PTSD, Social anxiety |
18 8 |
DUL DUL |
Lorazepam Lorazepam |
Ritalin Ritalin |
2 12 |
12 12 |
RUL RUL |
0.5 0.5 |
60 90 |
35 21 |
MTX, SUX, Alfent MTX, SUX, Alfent |
||
| 7 | M | 50 s |
MDD, PTSD Alcohol use d/o |
22 20 15 |
VEN VEN VEN |
Quetiapine Quetiapine Quetiapine |
1 4 7 |
7 7 7 |
BL BL BL |
0.5 0.5 0.3 |
30 50 100 |
25 134 18 |
MTX, SUX MTX, SUX, Alfent MTX, SUX, Alfent, CAFF, KET |
|||
| 8 | M | 30 s | MDD, PTSD, |
18 14 |
FLU, MIR FLU, MIR |
1 4 |
10 10 |
BL BL |
0.3 0.3 |
10 20 |
66 71 |
MTX, SUX MTX, SUX |
||||
| 9 | M | 40 s |
MDD, PTSD, Alcohol use d/o |
23 19 - 15 |
DUL DUL DUL |
Risperidone |
1 5 9 12 |
12 12 12 12 |
BL BL BL BL |
0.3 0.3 0.5 0.5 |
5 10 80 100 |
130 40 64 43 |
MTX, SUX MTX, SUX, Glycopyr MTX, SUX, Glycopyr MTX, SUX, Glycopyr |
|||
BUP bupropion, ESC escitalopram, DUL duloxetine, FLU fluoxetine, MIR mirtazapine, NTP nortriptyline, VEN venlafaxine, MTX methotrexate, SUX succinylcholine, Alfent alfentanil, CAFF caffeine, Glycopyr glycopyrrolate, KET ketamine.
aPolysubstance abuse is no longer a DSM-V diagnosis. The patient for which that is listed was using Alcohol, Cannabis, Cocaine, Amphetamine and Opioid Dependence. All, apparently, in remission (not used for at least 1 year).
Clinical measures
Quick Inventory of Depressive Symptomatology–Self Report (QIDS-SR) [57] was administered by a clinician before each treatment session.
EEG recording and data preprocessing
EEG recording procedures were designed to capture both acute effects of a single ECT treatment as well as longitudinal changes in EEG throughout the course of treatment (Fig. 2A). At the beginning of each session, 10 min of eyes closed, resting state EEG was recorded prior to administration of anesthetics or seizure induction. Following the seizure, patients were allowed to recover for at least 30 min until fully conscious and verbally communicative. This period was included in the study design in order to allow for recovery from the anesthetic medication as well as allow the research team to communicate with the patient about the recording procedure. This collection procedure was performed for multiple ECT sessions of the 4-week treatment (Fig. 2B). Due to constraints of the clinical environment, full recordings were not collected from every patient, but every patient included in the study had, at minimum, complete pre- and post-ECT recordings from two treatment sessions (Fig. 2C). A 14-channel EEG headset device (Emotiv EPOC+, https://emotiv.com) containing saline-soaked felt pad sensors (online reference located at left/right mastoid) was used for all recordings. EEG data was sampled at 2048 Hz with internal downsampling at 256 or 128 Hz and built-in notch filters at 50 and 60 Hz for a bandwidth of 0.16–43 Hz.
EEG data was preprocessed to remove artifacts using a custom script in Python and MNE v.0.23.0 [58]. First, channels with excessive noise and evidence of displacement were rejected manually based on visual inspection. Data were then high-pass filtered at 1 Hz. To detect and remove ocular artifacts and eyeblinks, ICA was applied to the filtered data. Components containing ocular artifacts were removed. Due to the small number of channels, ICA could not always remove ocular and muscular artifacts, so as a final step, data segments were selected manually. Data was inspected visually and artifact-free segments were selected. Once selected, these segments were then detrended and concatenated. The first 100 s of this concatenated data was used for analysis. We employed this procedure due to the amount of noise in the data and the small number of channels in the device. Because this concatenation technique produced high-amplitude, high-frequency artifacts, we restricted our analyses to a low-frequency range (1–30 Hz) to avoid any contamination of the power spectra. Because the preprocessing procedure used in this study was abnormal, an analysis of concatenated segments was performed and found no relationship between the length of the segments used and the EEG features quantified in this study, namely aperiodic exponent, delta band power, and delta oscillation power.
Data analysis
Data analysis was performed with python using numpy v.1.18.1 [59], scipy v.1.6.2 [60], MNE v.0.23.0 [58], neurodsp v.2.1.0 [61], and specparam v.1.0.0. Statistics were performed with python using statsmodels [62] and with R [63] to calculate linear mixed models using the lme4 library [64]. Only frontal channels AF3, AF4, F7, F8, F3, and F4 were included in the analysis. The code needed to reproduce the analysis and figures is provided here: https://github.com/voytekresearch/smith_ect.
Computing power spectral density (PSD)
PSDs were estimated using Welch’s method [65] using 1.0 s Hamming windows with 0.5 s overlap. Custom functions for this can be found in NeuroDSP [61], an open-source digital signal processing (DSP) toolbox for neural time series.
Spectral methods
The spectral parameterization method and toolbox were used for the calculation of aperiodic exponents as well as oscillatory power [20]. In this model, the power spectrum is composed of two electrophysiological components: aperiodic and periodic (oscillation) activity (Fig. 2A). This approach permits the disambiguation of contributions from oscillatory and aperiodic activity to the power spectrum. The aperiodic component of neural power spectra is described by the exponent and offset. Oscillatory activity is described by the center frequency, power, and bandwidth of identified peaks. Oscillation peaks are defined as peaks in the power spectrum exceeding a threshold of 1.5 standard deviations from the rest of the power values in the spectrum. If delta peaks were detected in the 1–3 Hz range, delta oscillatory power was defined as the power in the peak relative to the aperiodic component.
For methodological comparison, canonical delta band power was calculated as the mean of spectral power in the delta (1–3 Hz) frequency band.
Spectral parameterization and canonical band power evaluation were performed on the power spectrum of each channel (AF3, AF4, F3, F4, F7, and F8) for each recording session (pre and post). For each session, each EEG feature (aperiodic exponent, delta oscillatory power, and delta band power) was averaged across all six frontal channels. For acute effects analysis, EEG features from each pre-ECT session were compared to those from the corresponding post-ECT session. For longitudinal analyses, only features from pre-ECT sessions were used to ensure that longitudinal changes in EEG features were not contaminated by effects of lingering anesthesia or postictal states unrelated to treatment efficacy.
Statistical analysis
Clinical effects
Statistical evaluation of clinical effects was performed using a linear mixed-effects model fit to the total QIDS-SR clinical rating score. Patients were included as a random effect and ECT session number as a fixed effect.
Acute EEG effects
Effects of any given session of ECT on the aperiodic exponent, delta oscillatory power, and canonical delta band power were statistically evaluated using two-sided, related-measures t-tests. Specifically, pre-ECT values were compared to post-ECT values for each patient, independent of session number. Each feature is reported as a mean ± standard deviation. Data were tested for normality using a Shapiro-Wilk test, and a Wilcoxon signed-rank test was used to evaluate data that was non-parametric.
Longitudinal EEG effects
Similar to the statistical evaluation of clinical effects, the evaluation of longitudinal effects of repeated ECT sessions on the three EEG features (aperiodic exponent, delta oscillatory power, and canonical delta power) was performed using linear mixed-effects models. A linear mixed effect model was fit to each EEG feature with patient as a random effect and ECT session number as a fixed effect. Only pre-ECT values were included in the model to avoid the potential confounding effects of the anesthetic on EEG activity.
Associating EEG features with clinical effectiveness
To determine if a significant relationship between the aperiodic exponent and clinical rating score was present, we used the lme4 library in R to extract the coefficients for each variable from the linear mixed-effects models. This approach produced three coefficients for each patient, corresponding to a rate of change for the QIDS-SR score, aperiodic exponent, and delta band power. We then used a Pearson correlation to assess the relationship between QIDS-SR score x aperiodic exponent and QIDS-SR x delta band power. To account for the influence of outliers, we performed the same analysis using a Spearman correlation. To investigate the relationship between the QIDS-SR score, aperiodic exponent, and baseline aperiodic exponent, we performed a multiple linear regression. As only 6 out of 9 patients had a baseline EEG measurement, a proxy measure of baseline aperiodic exponent was computed as the intercept of the LME model.
Supplementary information
Acknowledgements
Support: NIH National Institute of General Medical Sciences grant R01GM134363-01 (to BV), UCSD Pace Grant (to MS), Majda Grant (to MS), Veterans Medical Research Foundation Pilot Grant (to MS). Thanks: We thank Itay Hadas, Natalie Schaworonkow, Ryan Hammonds, Eena Kosik, Michael Preston, Quirine Van Engen, and Andrew Bender for their advice and feedback on the manuscript.
Author contributions
MS and BV conceived the experiment(s) and developed the analyses. SS wrote the analysis code and analyzed the data. SS, VM, and CG collected the data and SS and AC analyzed the clinical data. DP provided data and advised analyses. SS, MS, and BV wrote the manuscript, and all authors edited the manuscript.
Data availability
All code used for all analyses and plots are publicly available on GitHub at https://github.com/voytekresearch/smith_ect/. The data collected in this study is considered sensitive medical information and is therefore not available at this time under restriction of the VASDHS Institutional Review Board.
Code availability
All code used for all analyses and plots are publicly available on GitHub at https://github.com/voytekresearch/smith_ect/.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Bradley Voytek, Maryam Soltani.
Supplementary information
The online version contains supplementary material available at 10.1038/s41398-023-02634-9.
References
- 1.Prudic J, Sackeim HA, Devanand DP. Medication resistance and clinical response to electroconvulsive therapy. Psychiatry Res. 1990;31:287–96. doi: 10.1016/0165-1781(90)90098-P. [DOI] [PubMed] [Google Scholar]
- 2.Kellner CH, Fink M, Petrides G, Husain M, Rummans T, Mueller M, et al. Relief of expressed suicidal intent by ECT: a consortium for research in ECT study. Am J Psychiatry. 2005;162:977–82. doi: 10.1176/appi.ajp.162.5.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levy NA, Serota HM, Grinker RR. Disturbances in brain function following convulsive shock therapy: electroencephalographic and clinical studies. Arch Neurol Psychiatry. 1942;47:1009. doi: 10.1001/archneurpsyc.1942.02290060147009. [DOI] [Google Scholar]
- 4.Roth M. Changes in the EEG under barbiturate anaesthesia produced by electro-convulsive treatment and their significance for the theory of ECT action. Electroencephalogr Clin Neurophysiol. 1951;3:261–80. doi: 10.1016/0013-4694(51)90073-9. [DOI] [PubMed] [Google Scholar]
- 5.Fink M. Relation of electroencephalographic delta activity to behavioral response in electroshock: quantitative serial studies. AMA Arch Neurol Psychiatry. 1957;78:516. doi: 10.1001/archneurpsyc.1957.02330410080012. [DOI] [PubMed] [Google Scholar]
- 6.Kriss A, Halliday AM, Halliday E, Pratt RTC. EEG immediately after unilateral ECT. Acta Psychiatr Scand. 1978;58:231–44. doi: 10.1111/j.1600-0447.1978.tb06935.x. [DOI] [PubMed] [Google Scholar]
- 7.Kolbeinsson H, Pétursson H. Electroencephalographic correlates of electroconvulsive therapy. Acta Psychiatr Scand. 1988;78:162–8. doi: 10.1111/j.1600-0447.1988.tb06316.x. [DOI] [PubMed] [Google Scholar]
- 8.Farzan F, Atluri S, Mei Y, Moreno S, Levinson AJ, Blumberger DM, et al. Brain temporal complexity in explaining the therapeutic and cognitive effects of seizure therapy. Brain. 2017;140:1011–25. doi: 10.1093/brain/awx030. [DOI] [PubMed] [Google Scholar]
- 9.Rosen I, Silfverskiold P. The effects of electroconvulsive therapy on quantitative electroencephalograms: relationship to clinical outcome. Eur Arch Psychiatry Neurol Sci. 1987;236:209–13. doi: 10.1007/BF00383850. [DOI] [PubMed] [Google Scholar]
- 10.Krystal AD, Weiner RD. EEG correlates of the response to ECT: a possible antidepressant role of brain-derived neurotrophic factor. J ECT. 1999;15:27–38. doi: 10.1097/00124509-199903000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Proctor L, Goodwin J. Comparitive electroencephalographic observations following electroshock therapy using raw 60 cycle alternating and unidirectional fluctuating current. Am J Psychiatry. 1943;99:525–30. doi: 10.1176/ajp.99.4.525. [DOI] [Google Scholar]
- 12.Strömgren LS, Juul-Jensen P. EEG in unilateral and bilateral electroconvulsive therapy. Acta Psychiatr Scand. 1975;51:340–60. doi: 10.1111/j.1600-0447.1975.tb00013.x. [DOI] [PubMed] [Google Scholar]
- 13.Hill AT, Hadas I, Zomorrodi R, Voineskos D, Farzan F, Fitzgerald PB, et al. Modulation of functional network properties in major depressive disorder following electroconvulsive therapy (ECT): a resting-state EEG analysis. Sci Rep. 2020;10:17057. doi: 10.1038/s41598-020-74103-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Høncke P, Zahle V. On the correlation between clinical and electroencephalographic observations in patients treated with electro-shock. Acta Psychiatr Scand. 1947;22:451–8. doi: 10.1111/j.1600-0447.1947.tb03990.x. [DOI] [Google Scholar]
- 15.Mosovich A, Katzenelbogen S. Electroshock therapy, clinical and electroencelphalographic studies. J Nerv Ment Dis. 1948;107:517–30. doi: 10.1097/00005053-194810760-00002. [DOI] [PubMed] [Google Scholar]
- 16.Volavka J, Feldstein S, Abrams R, Dornbush R, Fink M. EEG and clinical change after bilateral and unilateral electroconvulsive therapy. Electroencephalogr Clin Neurophysiol. 1972;32:631–9. doi: 10.1016/0013-4694(72)90100-9. [DOI] [PubMed] [Google Scholar]
- 17.Chusid JG, Pacella BL. The electroencephalogram in the electric shock therapies. J Nerv Ment Dis. 1952;116:92–107. [PubMed]
- 18.Takamiya A, Hirano J, Yamagata B, Takei S, Kishimoto T, Mimura M. Electroconvulsive therapy modulates resting-state EEG oscillatory pattern and phase synchronization in nodes of the default mode network in patients with depressive disorder. Front Hum Neurosci. 2019;13:1. doi: 10.3389/fnhum.2019.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Donoghue T, Dominguez J, Voytek B. Electrophysiological frequency band ratio measures conflate periodic and aperiodic neural activity. eNeuro. 2020;7:ENEURO.0192–20.2020. doi: 10.1523/ENEURO.0192-20.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Donoghue T, Haller M, Peterson EJ, Varma P, Sebastian P, Gao R, et al. Parameterizing neural power spectra into periodic and aperiodic components. Nat Neurosci. 2020;23:1655–65. doi: 10.1038/s41593-020-00744-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Podvalny E, Noy N, Harel M, Bickel S, Chechik G, Schroeder CE, et al. A unifying principle underlying the extracellular field potential spectral responses in the human cortex. J Neurophysiol. 2015;114:505–19. doi: 10.1152/jn.00943.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.He BJ, Zempel JM, Snyder AZ, Raichle ME. The temporal structures and functional significance of scale-free brain activity. Neuron. 2010;66:353–69. doi: 10.1016/j.neuron.2010.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.He W, Donoghue T, Sowman PF, Seymour RA, Brock J, Crain S, et al. Co-increasing neuronal noise and beta power in the developing brain. [Preprint]. 2019. Available from: 10.1101/839258.
- 24.Voytek B, Kramer MA, Case J, Lepage KQ, Tempesta ZR, Knight RT, et al. Age-related changes in 1/f neural electrophysiological noise. J Neurosci. 2015;35:13257–65. doi: 10.1523/JNEUROSCI.2332-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Colombo MA, Napolitani M, Boly M, Gosseries O, Casarotto S, Rosanova M, et al. The spectral exponent of the resting EEG indexes the presence of consciousness during unresponsiveness induced by propofol, xenon, and ketamine. NeuroImage. 2019;189:631–44. doi: 10.1016/j.neuroimage.2019.01.024. [DOI] [PubMed] [Google Scholar]
- 26.Robertson MM, Furlong S, Voytek B, Donoghue T, Boettiger CA, Sheridan MA. EEG power spectral slope differs by ADHD status and stimulant medication exposure in early childhood. J Neurophysiol. 2019;122:2427–37. doi: 10.1152/jn.00388.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Molina JL, Voytek B, Thomas ML, Joshi YB, Bhakta SG, Telledo, JA, et al. Memantine effects on EEG measures of putative excitatory/inhibitory balance in schizophrenia. Biol Psychiatry Cogn Neurosci Neuroimaging. 2020;5:562–8. [DOI] [PMC free article] [PubMed]
- 28.Veerakumar A, Tiruvadi V, Howell B, Waters AC, Crowell AL, Voytek B, et al. Field potential 1/ f activity in the subcallosal cingulate region as a candidate signal for monitoring deep brain stimulation for treatment-resistant depression. J Neurophysiol. 2019;122:1023–35. doi: 10.1152/jn.00875.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wen H, Liu Z. Separating fractal and oscillatory components in the power spectrum of neurophysiological signal. Brain Topogr. 2016;29:13–26. doi: 10.1007/s10548-015-0448-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buzsáki G, Draguhn A. Neuronal oscillations in cortical networks. Science. 2004;304:1926–9. doi: 10.1126/science.1099745. [DOI] [PubMed] [Google Scholar]
- 31.Buzsáki G, Anastassiou CA, Koch C. The origin of extracellular fields and currents—EEG, ECoG, LFP and spikes. Nat Rev Neurosci. 2012;13:407–20. doi: 10.1038/nrn3241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gao R, Peterson EJ, Voytek B. Inferring synaptic excitation/inhibition balance from field potentials. NeuroImage. 2017;158:70–8. doi: 10.1016/j.neuroimage.2017.06.078. [DOI] [PubMed] [Google Scholar]
- 33.Sackeim HA, Decina P, Prohovnik I, Malitz S, Resor SR. Anticonvulsant and antidepressant properties of electroconvulsive therapy: a proposed mechanism of action. Biol Psychiatry. 1983;18:1301–10. [PubMed] [Google Scholar]
- 34.Krystal JH, Sanacora G, Blumberg H, Anand A, Charney DS, Marek G, et al. Glutamate and GABA systems as targets for novel antidepressant and mood-stabilizing treatments. Mol Psychiatry. 2002;7:S71–S80. doi: 10.1038/sj.mp.4001021. [DOI] [PubMed] [Google Scholar]
- 35.Sohal VS, Rubenstein JLR. Excitation-inhibition balance as a framework for investigating mechanisms in neuropsychiatric disorders. Mol Psychiatry. 2019;24:1248–57. doi: 10.1038/s41380-019-0426-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Petty F. GABA and mood disorders: a brief review and hypothesis. J Affect Disord. 1995;34:275–81. doi: 10.1016/0165-0327(95)00025-I. [DOI] [PubMed] [Google Scholar]
- 37.Rajkowska G, O’Dwyer G, Teleki Z, Stockmeier CA, Miguel-Hidalgo JJ. GABAergic neurons immunoreactive for calcium binding proteins are reduced in the prefrontal cortex in major depression. Neuropsychopharmacology. 2007;32:471–82. doi: 10.1038/sj.npp.1301234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Knight RT, Richard Staines W, Swick D, Chao LL. Prefrontal cortex regulates inhibition and excitation in distributed neural networks. Acta Psychol. 1999;101:159–78. doi: 10.1016/S0001-6918(99)00004-9. [DOI] [PubMed] [Google Scholar]
- 39.Drevets WC, Price JL, Furey ML. Brain structural and functional abnormalities in mood disorders: implications for neurocircuitry models of depression. Brain Struct Funct. 2008;213:93–118. doi: 10.1007/s00429-008-0189-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Luscher B, Shen Q, Sahir N. The GABAergic deficit hypothesis of major depressive disorder. Mol Psychiatry. 2011;16:383–406. doi: 10.1038/mp.2010.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Voineskos D, Levinson AJ, Sun Y, Barr MS, Farzan F, Rajji TK, et al. The relationship between cortical inhibition and electroconvulsive therapy in the treatment of major depressive disorder. Sci Rep. 2016;6:37461. doi: 10.1038/srep37461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sanacora G, Mason GF, Rothman DL, Behar KL, Hyder F, Petroff OAC, et al. Reduced cortical gamma-aminobutyric acid levels in depressed patients determined by proton magnetic resonance spectroscopy. Arch Gen Psychiatry. 1999;56:1043–7. doi: 10.1001/archpsyc.56.11.1043. [DOI] [PubMed] [Google Scholar]
- 43.Hasler G, Meyers N, Shen J, Drevets WC. Reduced prefrontal glutamate/glutamine and γ-aminobutyric acid levels in major depression determined using proton magnetic resonance spectroscopy. Arch Gen Psychiatry. 2007;64:8. doi: 10.1001/archpsyc.64.2.193. [DOI] [PubMed] [Google Scholar]
- 44.Fee C, Banasr M, Sibille E. Somatostatin-positive gamma-aminobutyric acid interneuron deficits in depression: cortical microcircuit and therapeutic perspectives. Biol Psychiatry. 2017;82:549–59. doi: 10.1016/j.biopsych.2017.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sanacora G, Mason GF, Rothman DL, Krystal JH. Increased occipital cortex GABA concentrations in depressed patients after therapy with selective serotonin reuptake inhibitors. Am J Psychiatry. 2002;159:663–5. doi: 10.1176/appi.ajp.159.4.663. [DOI] [PubMed] [Google Scholar]
- 46.Sanacora G, Mason GF, Rothman DL, Hyder F, Ciarcia JL, Ostroff RB, et al. Increased cortical GABA concentrations in depressed patients receiving ECT. Am J Psychiatry. 2003;160:577–9. doi: 10.1176/appi.ajp.160.3.577. [DOI] [PubMed] [Google Scholar]
- 47.Kato N. Neurophysiological mechanisms of electroconvulsive therapy for depression. Neurosci Res. 2009;64:3–11. doi: 10.1016/j.neures.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 48.Farzan F, Boutros NN, Blumberger DM, Daskalakis ZJ. What does the electroencephalogram tell us about the mechanisms of action of ECT in major depressive disorders? J ECT. 2014;30:98–106. doi: 10.1097/YCT.0000000000000144. [DOI] [PubMed] [Google Scholar]
- 49.Singh A, Kar SK. How electroconvulsive therapy works?: Understanding the neurobiological mechanisms. Clin Psychopharmacol Neurosci. 2017;15:210–21. doi: 10.9758/cpn.2017.15.3.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kaltenboeck A, Harmer C. The neuroscience of depressive disorders: a brief review of the past and some considerations about the future. Brain Neurosci Adv. 2018;2:239821281879926. doi: 10.1177/2398212818799269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Olbrich S, Arns M. EEG biomarkers in major depressive disorder: discriminative power and prediction of treatment response. Int Rev Psychiatry. 2013;25:604–18. doi: 10.3109/09540261.2013.816269. [DOI] [PubMed] [Google Scholar]
- 52.van der Vinne N, Vollebregt MA, van Putten MJAM, Arns M. Frontal alpha asymmetry as a diagnostic marker in depression: fact or fiction? A meta-analysis. NeuroImage Clin. 2017;16:79–87. doi: 10.1016/j.nicl.2017.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kołodziej A, Magnuski M, Ruban A, Brzezicka A. No relationship between frontal alpha asymmetry and depressive disorders in a multiverse analysis of five studies. eLife. 2021;10:e60595. doi: 10.7554/eLife.60595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.ten Doesschate F, Bruin W, Zeidman P, Abbott CC, Argyelan M, Dols A, et al. Neural excitation/inhibition imbalance and the treatment of severe depression. [Preprint]. 2021. Available from: 10.1101/2021.07.09.451784.
- 55.Weiner RD. The persistence of electroconvulsive therapy-induced changes in the electroencephalogram. J Nerv Ment Dis. 1980;168:224–8. doi: 10.1097/00005053-198004000-00006. [DOI] [PubMed] [Google Scholar]
- 56.Sutherland EM, Oliver JE, Knight DREEG. Memory and confusion in dominant, non-dominant and bi-temporal E.C.T. Br J Psychiatry. 1969;115:1059–64. doi: 10.1192/bjp.115.526.1059. [DOI] [PubMed] [Google Scholar]
- 57.Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, et al. The 16-Item quick inventory of depressive symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54:573–83. doi: 10.1016/S0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- 58.Gramfort A, Luessi M, Larson E, Engemann DA, Strohmeier D, Brodbeck C, et al. MEG and EEG data analysis with MNE-Python. Front Neurosci. 2013;7:267. [DOI] [PMC free article] [PubMed]
- 59.Harris CR, Millman KJ, van der Walt SJ, Gommers R, Virtanen P, Cournapeau D, et al. Array programming with NumPy. Nature. 2020;585:357–62. doi: 10.1038/s41586-020-2649-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Virtanen P, Gommers R, Oliphant TE, Haberland M, Reddy T, Cournapeau D, et al. SciPy 1.0: fundamental algorithms for scientific computing in Python. Nat Methods. 2020;17:261–72. doi: 10.1038/s41592-019-0686-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cole S, Donoghue T, Gao R, Voytek B. NeuroDSP: a package for neural digital signal processing. J Open Source Softw. 2019;4:1272. doi: 10.21105/joss.01272. [DOI] [Google Scholar]
- 62.Seabold S, Perktold J. Statsmodels: econometric and statistical modeling with Python. In: Proceedings of the 9th Python in Science Conference. 2010. p. 92–6. 10.25080/Majora-92bf1922-011.
- 63.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria; 2022. https://intro2r.com/citing-r.html.
- 64.Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67:1–48. doi: 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- 65.Welch P. The use of fast Fourier transform for the estimation of power spectra: a method based on time averaging over short, modified periodograms. IEEE Trans Audio Electroacoust. 1967;15:70–3. doi: 10.1109/TAU.1967.1161901. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All code used for all analyses and plots are publicly available on GitHub at https://github.com/voytekresearch/smith_ect/. The data collected in this study is considered sensitive medical information and is therefore not available at this time under restriction of the VASDHS Institutional Review Board.
All code used for all analyses and plots are publicly available on GitHub at https://github.com/voytekresearch/smith_ect/.