Abstract
Plasmodium falciparum malaria drives immunoregulatory responses across multiple cell subsets, which protects from immunopathogenesis, but also hampers the development of effective anti-parasitic immunity. Understanding malaria induced tolerogenic responses in specific cell subsets may inform development of strategies to boost protective immunity during drug treatment and vaccination. Here, we analyse the immune landscape with single cell RNA sequencing during P. falciparum malaria. We identify cell type specific responses in sub-clustered major immune cell types. Malaria is associated with an increase in immunosuppressive monocytes, alongside NK and γδ T cells which up-regulate tolerogenic markers. IL-10-producing Tr1 CD4 T cells and IL-10-producing regulatory B cells are also induced. Type I interferon responses are identified across all cell types, suggesting Type I interferon signalling may be linked to induction of immunoregulatory networks during malaria. These findings provide insights into cell-specific and shared immunoregulatory changes during malaria and provide a data resource for further analysis.
Subject terms: Parasite immune evasion, Malaria, Immune evasion, Regulatory T cells, B cells
The use of single cell sequencing has enabled more detailed analysis of the immune response to infection. Here the authors characterise the immune response to malaria infection in an endemic region using single cell transcriptomics indicating regulatory signatures associated with infection.
Introduction
Plasmodium falciparum causes significant disease burden globally, with >240 million cases of malaria and >600,000 deaths reported in 20211. In areas of high malaria transmission children rarely experiencing recurrence of severe malaria due to the rapid acquisition of anti-disease or tolerogenic immunity2, and/or antibody mediate protection from severe disease-causing parasite strains3. However, anti-parasitic immunity and protection from mild disease develops more slowly, with children experiencing multiple patent, symptomatic infections throughout childhood before developing levels of protection that control parasite growth to sub-patent levels4. These phenomena are thought to be linked, with the slow acquisition of anti-parasitic immunity attributed to tolerogenic responses across multiple cell subsets required for robust adaptive immune development. These tolerogenic mechanisms may also contribute to reduced malaria vaccine efficacy in exposed populations5. As such, a better understanding of tolerogenic immune responses during infection may inform the development of more effective vaccine strategies for areas of high malaria endemicity.
Malaria driven tolerogenic and immunoregulatory responses allow parasite persistence by evading and disrupting anti-parasitic mechanisms employed by both innate and adaptive immune cells. Multiple studies have shown that monocytes and dendritic cells (DCs), that are initiators of the immune responses, are tolerized during malaria. During experimental human malaria and natural infection, monocytes and DCs have reduced responsiveness to toll-like receptor (TLR) stimulation and antigen presentation is suppressed6–9. Increased IL-10 production10 and higher frequencies of monocytes with a regulatory phenotype are also detected in children and adults from malaria endemic areas11,12. Tolerogenic phenotypes have also been reported in other innate cells. For example, natural killer (NK) cells expressing the regulatory marker PD1, are expanded in populations in malaria endemic areas13. Additionally, gamma-delta (γδ) T cells, particularly Vδ2+ subsets which are important innate inflammatory responders to malaria parasites, become tolerized in children in high transmission settings14,15. Immunoregulation also exists in adaptive cell responses to malaria. Within the CD4 T cell compartment, type 1 regulatory (Tr1) cells that co-produce IFNγ and IL-10 during malaria, dominate antigen-specific CD4 T cell responses in children in high endemic areas16–18. These Tr1 cells develop rapidly during a primary malaria infection in previously naive adults19. CD4 T cells also upregulate additional inhibitory pathways during malaria infection, including expression of multiple co-inhibitory receptors and production of TGFβ20–22. Within the B cell compartment, multiple studies have shown that atypical memory B cells expand in response to malaria23–25. These cells have reduced functional capacity compared to ‘typical’ memory B cells26,27, and an immunoregulatory role for these cells in malaria is also possible. Malaria responsive regulatory B cells (Bregs), which produce IL-10, have been reported in mouse models28, but have not been identified in human malaria. While the drivers of tolerogenic cell responses are incompletely understood, Type I IFN signalling is key to the emergence of Tr1 CD4 T cells during malaria19, and is recognised as both an activating and regulatory driver of the malaria immune response29.
Transcriptional changes associated with immune cell tolerance have been reported in limited studies. For example, monocytes from Malian children and adults following parasite stimulation in vitro had reduced induction of NFKB1 (positive regulator of inflammation) in tolerized adult cells11, and transcriptional analysis of Vδ2+ γδ T cells in Ugandan children identified upregulation of multiple immunoregulatory pathways in highly exposed children14. Additionally, a large whole-blood transcriptomic study revealed the upregulation of interferon responses, and that p53 activation in monocytes attenuated Plasmodium-induced inflammation and predicted protection from fever30. However, to date, no studies have comprehensively investigated transcriptional signatures of malaria-driven tolerance across all cell subsets in the same individuals during infection.
The advent of single-cell RNA sequencing (scRNAseq) has allowed comprehensive analysis of distinct immune cell subsets during human infection, and identification of key changes driven by infection. To date, while scRNAseq has been applied to the malaria parasites31–33, and to immune cells in a single experimental infection study34, no comprehensive scRNAseq mapping of the immune landscape during malaria infection has been undertaken. In the present study, we applied scRNAseq to peripheral blood mononuclear cells (PBMCs) from patients during acute P. falciparum malaria and post treatment. Cell linages and subsets were identified, differential expressed genes (DEGs) associated with acute malaria infection compared to convalescence analysed and key transcriptional changes confirmed at the protein level in additional patients. Together this study advances our understanding of the regulatory immune landscape during malaria and provides opportunities to manipulate these pathways for clinical advantage.
Results
Altered immune cell profiles during acute malaria infection
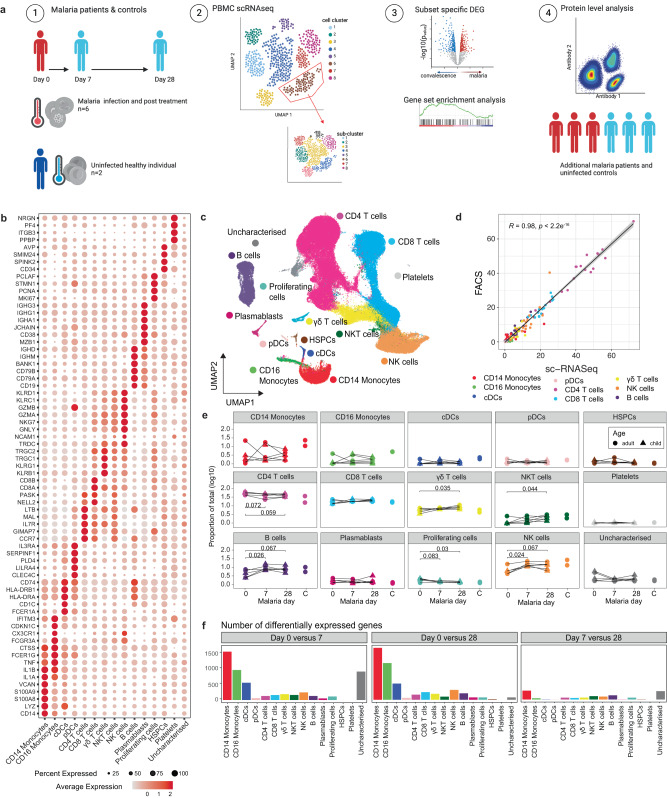
To undertake a global analysis of the immune response during malaria infection, we performed droplet-based scRNAseq on peripheral blood mononuclear cells (PBMCs) from 6 individuals (age 6–24 years) with uncomplicated P. falciparum malaria at enrolment (day 0, acute malaria time point) and at 7 and 28 days after drug treatment, along with 2 healthy adult endemic controls (EC, ages 20 and 27 years) (Fig. 1a, Supplementary Table 1). We sequenced a total of 115,526 cells, with 106,076 cells passing quality control (QC; minimum of 220 genes expressed and <20% mitochondrial reads per cell) (Supplementary Fig. 1A). Due to a 10X Chromium wetting error, no quality cells were retained from one individual at the acute infection time point (child1day0, Supplementary Fig. 1B). Data were integrated to harmonize data sets across batch, donor and infection timepoints, and cell clusters visualized with uniform manifold approximation and projection (UMAP) (Supplementary Fig. 1C). Expression of canonical and lineage marker genes were used to annotate cell clusters into 15 high level cell states: CD14+ classical monocytes, CD16+ non-classical monocytes, classical dendritic cells (cDCs), plasmacytoid dendritic cells (pDCs), CD4 T cells, CD8 T cells, γδ T cells, NKT cells, B cells, plasma cells, proliferating [which appeared to be of mixed cell types], hematopoietic stem and progenitor cells (HSPCs), platelets, and one uncharacterized cluster (Fig. 1b/c, Supplementary Data 1, Supplementary Fig. 1D). The uncharacterized cluster did not express any known linage marker genes, and had relatively increased expression of mitochondrial genes, possibly indicating low quality cells. The relative proportions of identified cell clusters correlated strongly with the proportions of cells identified by flow cytometry analysis of the same cell samples (R = 0.95, p < 0.001, Fig. 1d, Supplementary Fig. 2). During malaria infection, there were some changes to the distribution of cell types, with trends of increases in CD4 T cells (p = 0.059 day 0 v day 28) and proliferating cells (p = 0.03 day 0 v day 28, and marked decreases in NK cells (p = 0.024 day 0 v day 7), γδ T cells (p = 0.035 day 0 v day 28) and B cells (p = 0.026 day 0 v day 28), as a proportion of total analyzed cells within each individual (Fig. 1e). To characterize gene expression profiles during malaria infection, we performed differential gene expression analysis within each cell subset between acute infection (day 0), and 7 and 28 days after treatment (Fig. 1f). We observed the largest number of DEGs when comparing between day 0 and day 28, with monocytes and cDCs exhibiting the highest transcriptional changes relative to other cell types (Fig. 1f, Tables S3A–C). Large numbers of DEGs were also detected between day 0 and day 7, with a large proportion of these also detected 28-days post-treatment for each subset (for example, majority of DEGs for day 0 compared to day 7 and day 0 compared to day 28, were shared for CD14+ classical monocytes [64%], CD16+ non-classical monocytes [60%], cDCs [53%] and pDCs [47%]). DEGs were also detected between day 28 (convalescence) and endemic controls, possibly indicated sustained changes to cell transcriptional profiles up to a month after infection, or alternatively, due to the different baseline transcriptional profiles between individuals (Supplementary Fig. 1E). DEGs were not calculated for each individual for each cell cluster due to low number of contributing cells for some individuals once subsets were identified (Supplementary Table 2). Subsequently, to identify DEGs caused by malaria infection compared to convalescence, we focused analysis on DEGs identified between day 0 (16,192 cells) and day 28 (34,286 cells).
Fig. 1. Single cell transcriptional landscape of malaria infection.
a A schematic outline depicting workflow for sample collection and scRNAseq analysis. PBMCs were collected from P. falciparum malaria patients at day 0 (n = 5), and at day 7 (n = 6) and 28 (n = 6) post treatment and from healthy endemic controls without malaria (EC, n = 2). Live PBMCs were analysed by 3’ 10X Chromium single cell sequencing, and cell types identified. For each cell type and sub-cluster, genes with differential expression between days were identified and analysed. Key findings were confirmed at the protein level in additional patients. Created with BioRender.com. b Dot plot of the mean expression of marker genes used to annotate cell types. c UMAP of all cells in integrated analysis. Cells are coloured by cell subtypes. d Correlation between relative proportion of cells identified by scRNAseq and flow cytometry analysis (data from n = 19, from day 0 n = 5, day 7 n = 6, day 28 n = 6, endemic controls n = 2). Pearson’s R and p (two-sided) is indicated. Error is 95% confidence interval. e Relative proportion of identified subsets from scRNAseq analysis as a proportion of total cells analysed per timepoint/individual at day 0 during malaria, and day 7-, and 28-days post-treatment, and in healthy endemic control individuals. P-value (two-sided) is calculated by Mann Whitney U test between day 0 and subsequent time points. f Number of DEGs for each cell type between day 0/7, day 0/28 and day 7/28. See also Supplementary Fig. 1-2 and Supplementary Tables 1-2 and Supplementary Data 1-2. Source data are provided as a Source Data file.
Shared and subset-specific immunosuppressive signatures in monocytes and cDCs during malaria
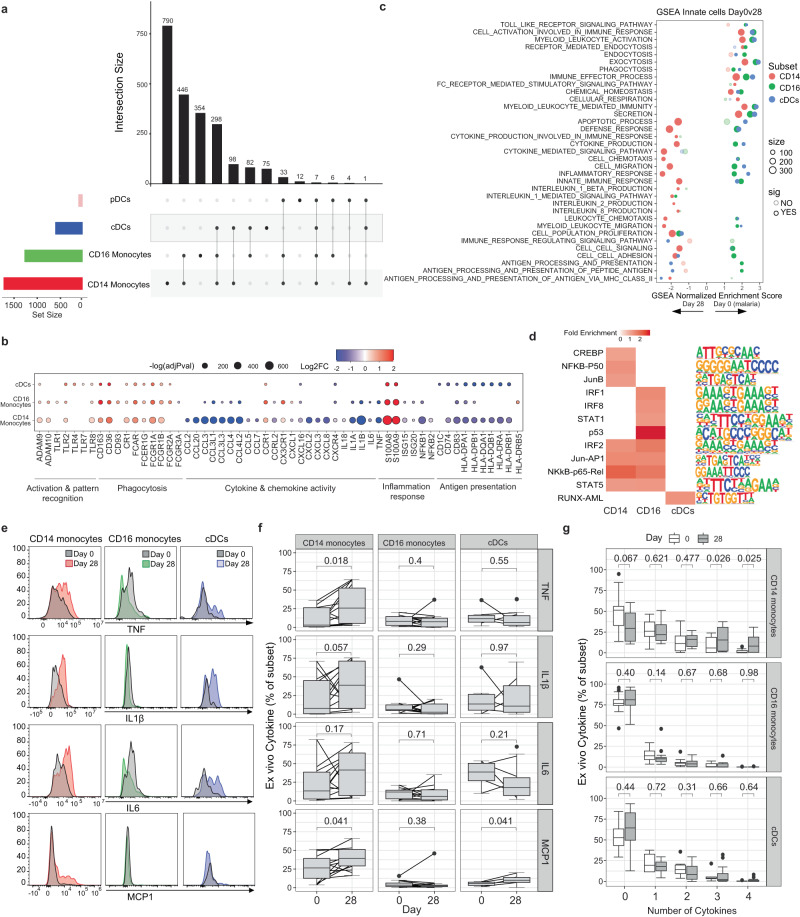
We first analysed transcriptional changes to innate myeloid cells comparing day 0 to day 28 and identified 1674, 1182, 521 DEGs in CD14+ classical monocytes, CD16+ non-classical monocytes and cDCs, respectively (Supplementary Data 2). DEGs were identified by comparing all cells at day 0 to day 28 in each cell cluster, regardless of individual donor. However, for all DEGs, the changes to expression between day 0 and day 28 were largely consistent across individuals (Supplementary Fig. 3). The high transcriptional activity of monocytes and cDCs during malaria contrasted with the low number of DEGs detected in pDCs (n = 60). Of pDC DEGs, 23% were associated with the long non-coding RNA family and 15% were histone genes (Supplementary Data 2). Low transcriptional activation of pDCs is consistent with our previous bulk-RNA sequencing analysis of isolated pDCs during experimental malaria infection, which showed that pDCs were transcriptionally stable during infection35. Transcriptional changes during malaria in both monocyte subsets and cDCs were both shared and cell type specific (Fig. 2a). Both CD14+ and CD16+ monocytes were activated, with marked upregulation of innate cell activation genes such as Toll-like Receptors (TLRs), disintegrin and metallopeptidase domain (ADAM9 and ADAM10) proteins36, as well as alarmins, S100A8 and S100A9, which are typically upregulated in monocytes under inflammatory conditions37. In contrast, MHC class II HLA-DR genes were down-regulated in both CD14+ and CD16+ monocytes (Fig. 2b, Supplementary Data 2). High expression of S100A8/A9, along with RETN, ALOX5AP and reduced expression of MHC class II HLA-DR genes has recently been used to define immunosuppressive MS1 monocytes in sepsis38 and proportional increases in these immune-suppressive monocytes has been detected in both sepsis and COVID-1939, however these immunosuppressive monocytes have not been identified in other acute infections such as dengue40. Consistent with an enrichment of immunosuppressive monocytes during malaria infection, inflammatory cytokine genes including TNF, IL1α, IL1β, IL6, IL18 were markedly reduced at day 0, compared with 28 days post treatment (Fig. 2b, Supplementary Data 2). There was also reduced expression of multiple chemokine genes including CCL2 (encoding MCP-1), CCL3, CCL4, CCL5, CCL7, CXCL8 (encoding IL8), CXCL2, CXCL3, CCL20, CXCL1 and CXCL16 in both monocyte subsets, with a greater magnitude of reduction in CD14+ monocytes. Consistent with reduced expression of these cytokine and chemokine genes, we also observed reduced expression of NK-κB family members, NF-κB1, NF-κB2, and REL, central transcriptional factors for pro-inflammatory gene induction41. Immune-suppressive phenotypes were also detected in cDCs during infection, with notable downregulation of HLA-DR genes HLA-DRA and HLA-DRB1 along with multiple paralogues (HLA-DPA1/B1 and HLA-DQA1/B1) in cDCs but not cytokine/chemokine genes. The reduction of HLA-DR genes in cDCs is consistent with previous reports showing reduced HLA-DR expression at the protein level on DCs during experimental6, and naturally acquired malaria8,42,43.
Fig. 2. Immuno-suppressive signatures of innate cells during malaria.
DEGs in CD14+ and CD16+ monocytes, and cDCs and pDCs of day 0 compared to day 28 were identified (n = 5 day 0, n = 6 day 28). a Upset plot of shared and subset specific DEGs of each subset identified between day 0 and day 28. b DEGs of interest in monocytes and cDCs. Genes with known monocyte function are indicated. Log transformed p values (Wilcox test, two-sided, Bonferroni correction). c GSEA of DEGs in CD14+ and CD16+ monocytes and cDCs. d Common and unique upstream regulators of DEGs in CD14+ and CD16+ monocytes and cDCs. e Ex vivo secretion of TNF, IL1β, IL6 and MCP1 was measured in CD14+ and CD16+ monocytes, and cDCs. Representative cytokine expression of a single individual at day 0 compared to day 28 in each subset. Subset gates from each sample were excluded if <50 events (CD14+ monocytes – Day 0 n = 15, Day 28 n = 14; CD16+ monocytes – Day 0 n = 14, Day 28 n = 14; cDCs – Day 0 n = 6, Day 28 n = 14). f Cell subset level expression of cytokines. Box and whisker plots indicate first and third quartiles for the hinges, median line, and lowest and highest values no further that 1.5 interquartile range from the hinges for whisker lines. g Frequency of cell subset expressing none or a combination of the 4 cytokines: TNF, IL1β, IL6 and MCP1. P-value (two-sided) indicated is calculated by Mann-Whitney U test. See also Supplementary Fig. 3-4 and Supplementary Tables 1-2, Supplementary Data 1-2. Source data are provided as a Source Data file.
In contrast to down-regulation of inflammatory gene signatures, multiple genes involved in pathogen recognition, scavenging and phagocytosis were upregulated in both monocyte subsets and cDCs during acute infection, including CD163 and FCGR1A (encoding CD64/FcγRI) which we have previously shown to be upregulated at the protein level on both classical and non-classical monocytes during malaria7 (Fig. 2b). Similarly, FCAR (encoding the Fc fragment of IgA receptor) was also upregulated on both monocyte subsets and cDCs, consistent with a possible role of IgA antibodies in immunity against malaria44–46. CD93 and FCGR2A (encoding CD32/FcγRIIa) which mediate the enhancement of phagocytosis in monocytes and macrophages were upregulated during infection on CD16+ monocytes and cDCs, but not CD14+ monocytes. COMPLEMENT RECEPTOR 1 (CR1), a membrane immune adherence receptor that plays a critical role in the capture and clearance of complement-opsonized pathogens, was upregulated on both CD14+ and CD16+ monocytes and cDCs during malaria. This transcriptional upregulation of CR1 is in contrast to previous reports of down regulated CR1 on splenic monocytes/macrophages in murine models of malaria, and on CD16+ monocytes/macrophages in P. falciparum and P. vivax malaria patients from Peru47. CD36, involved in antibody independent phagocytosis was also upregulated on both subsets and cDCs. The downregulation of cytokine and chemokine responses in the myeloid compartment, but upregulation of receptors involved in antibody mediated parasite clearance during malaria is supported by recent work by others48.
To further investigate shared and cell type specific transcriptional changes, DEGs were analysed using the Gene Set Enrichment Analysis (GSEA) and overrepresented upstream regulators identified. These analyses revealed both shared and cell specific gene signature enrichment and regulators (Fig. 2c, d). Consistent with DEGs for each subset, both monocyte subsets and cDCs were enriched for pathways such as secretion, phagocytosis, myeloid leukocyte mediated immunity and immune effector processes during malaria. In contrast, multiple subset specific pathways were also identified. For example, leukocyte migration and chemotaxis, inflammatory and defence response, and cytokine production were enriched at day 0 during malaria in CD16+ monocytes and cDCs but enriched at day 28 in CD14+ monocytes. In contrast, pathways associated with antigen presentation were consistently enriched only in CD16+ monocytes during malaria. In agreement with cell type specific pathway enrichment, analysis of upstream regulators identified motifs that were shared between CD14+ and CD16+ monocytes including NFκB-p5, IRF2, STAT5 and JUN-AP1-binding cis-elements, but also regulators that were specific for each subset. For CD16+ monocytes, this included p53, STAT1, IRF1, and IRF8-binding cis-elements. p53 was previously identified in bulk transcriptional analysis as an important contributor of innate cell responses and immunity to malaria30. The enrichment of IFR1/8/2 and STAT1/5 are consistent with a key role of Type I IFN pathways in both activation and regulation of innate immune cell responses in malaria29.
To assess some of these key findings at the protein level, ex vivo secretion of cytokine/chemokines TNF, IL-1β, IL-6 and MCP-1 (CCL2) from CD14+ monocytes, CD16+ monocytes and cDCs were measured in additional P. falciparum malaria patients from the same study site at day 0 and day 28 (n = 15) (Fig. 2e–g, Supplementary Fig. 4A, B, Supplementary Table 1). Consistent with transcriptional findings, the majority of individuals had reduced inflammatory cytokine/chemokine secretion in CD14+ monocytes at day 0 compared to day 28 (Fig. 2e, f). This reduction was significant at the population level for TNF and MCP1. MCP1 expression was also reduced at day 0 compared to day 28 in cDCs. Cytokine production was not associated with age/parasitemia or sex (Supplementary Fig. 4C–E). To measure the co-expression of cytokines, responses were analysed by SPICE (Simplified presentation of incredibly complex evaluations49), and cells expressing 0, 1, 2, 3, or 4 cytokines in any combination calculated. CD14+ monocytes were significantly less polyfunctional at day 0 compared to day 28 (Fig. 2g). Collectively, data reveal a significant enrichment of regulatory innate cells during malaria infection which down-regulate multiple cytokine and chemokine responses along with HLA-DR associated genes and pathways required for robust inflammatory control and antigen presentation in a cell subset specific manner, regulated by cell subset specific pathways. In contrast, multiple receptors involved in antibody mediated functions are upregulated, consistent with a potential role of innate cells in antibody mediated parasite clearance during infection48.
Subset-specific activation and regulation of NK cells during malaria
Along with innate myeloid cells, NK cells are important early responders to Plasmodium infection, but also have roles in adaptive immunity as effector cells. Broadly, NK cells exist in multiple distinct functional subsets along a spectrum of least differentiated CD56bright cells, towards highly differentiated CD56dimCD16+CD57+ senescent cells. CD56bright NK cells and other more differentiated subsets produce IFNγ following parasite stimulation in vitro50,51 and during controlled human malaria infection52. In contrast, adaptive and highly differentiated NK cells expand in malaria exposed individuals, and function via antibody dependent cellular cytotoxicity (ADCC) to protect from malaria53,54.
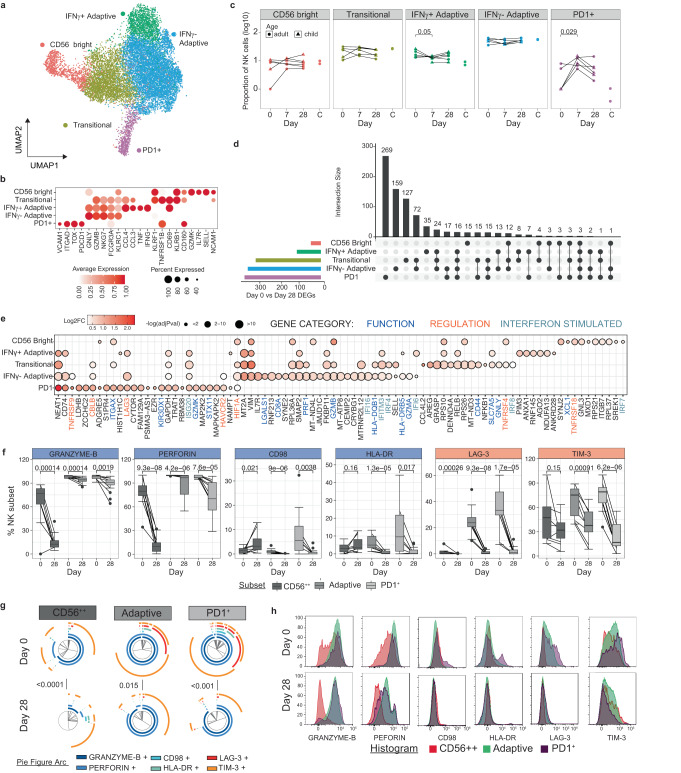
To investigate the transcriptional activation of these phenotypically distinct NK cell populations during malaria, we performed sub-clustering of NK cells identified in PBMCs (Fig. 1). Sub-clustering identified five subsets which were annotated based on cluster markers as CD56bright, Transitional, IFNγ+ Adaptive, IFNγ- Adaptive and PD1+ NK cell subsets (Fig. 3a, Supplementary Data 3). CD56bright cells expressed the highest levels of NCAM1 (encoding CD56), SELL, KLRF1, GZMK and IL7R. The Adaptive cell subsets had increased expression of NKG7, GZMB and FCGR3A (encoding CD16). Transitional NK cells expressed markers from both CD56bright and Adaptive subsets, consistent with previous scRNAseq analysis55,56(Fig. 3b). Within the Adaptive cell subsets, clusters were differentiated as IFNγ+ and IFNγ- Adaptive subsets based on IFNG expression, along with TNF, CCL3 and CCL4. Additionally, our unsupervised clustering isolated an NK cell cluster expressing high levels of PDCD1 (encoding PD1). PD1+ NK cells have previously been shown to expand with age in malaria endemic populations and have increased ADCC function13. PD1+ NK cells also expressed genes related to NK recruitment and activation, VCAM1, ITGAD (encoding CD11d), TOX, TNFRSF1B (encoding TNFRII) and CD160 (Fig. 3b). During malaria, there was a significant increase in the proportion of IFNγ+ Adaptive cells, consistent with an increased inflammatory and cytokine responsiveness of Adaptive NK cells during infection. Additionally, there was a proportional decrease in PD1+ NK cells during acute infection compared to 7 days following treatment (Fig. 3c). This decreased proportion of PD1+ NK cells during acute malaria is in contrast to previous reports of the expansion of this subset identified by flow-cytometry in Malians with P. falciparum malaria13.
Fig. 3. Subset specific activation and regulation of NK cells in malaria.
a/b Five subsets of NK cells were identified based on unsupervised clustering and marker expression as CD56bright, Transitional, IFNγ+ Adaptive, IFNγ- Adaptive and PD1+ subsets. c Relative proportion of identified subsets during malaria infection (day 0, n = 5), 7- (n = 6) and 28-days (n = 6) post treatment, and in healthy uninfected individuals (n = 2). P-value (two-sided) indicated is calculated by Mann-Whitney U test between day 0 and indicated subsequent time points. d Upset plot of DEGs in NK cell subsets at day 0 compared to day 28. The number of shared and subset specific DEGs indicated. e Top 20 DEGs of in each NK subsets, and additional genes of interest with p ≤ 0.05. Genes with known roles in regulation and/or function are indicated. Log transformed p values (Wilcox test, two-sided, Bonferroni correction). f PBMCs from individuals with P. falciparum malaria (Day 0, n = 11), and convalescent malaria patients 28-days post-infection (Day 28, n = 17) were analysed ex vivo to detect NK cell protein expression of identified genes by flow cytometry. Expression of proteins related to function and regulation of NK cells, shown as positive frequencies of NK cell subsets CD56bright (CD56++), Adaptive and PD1+. Box plots show the median and IQR of volunteers, lines represent paired observations, group comparisons performed by Mann-Whitney U test (two-sided). g Co-expression of proteins related to function and regulation of NK cells analysed by SPICE. Pie graphs comparisons performed by Permutation test. h Concatenated histograms normalised to mode show expression of gene-related proteins within NK cell subsets. See also Supplementary Fig. 6-10, Supplementary Table 3, Supplementary Data 3-4. Source data are provided as a Source Data file.
To investigate malaria-driven transcriptional changes to NK cells, we identified DEGs from day 0 to day 28 within each subset (Supplementary Data 4). While individuals contributed different cell numbers to each cluster, DEG changes were consistently expressed across individuals (Supplementary Table 3, Supplementary Fig. 5). Transitional, IFNγ- Adaptive and PD1+ subsets were more transcriptionally active during malaria compared to CD56bright and IFNγ+ Adaptive subsets (Fig. 3d). PD1+, Transitional and IFNγ- Adaptive NK cells, had a large proportion of subset specific DEGs, suggesting unique NK cell subset specific activation pathways during malaria (subset specific DEGs 76%, 42% and 47% respectively, Fig. 3d). During acute malaria, there was evidence for increased cytotoxic potential across multiple NK cell subsets, with upregulation of genes with known cytotoxic functions (Granzyme members GZMB, GZMA, GZMK57, Granulysin [GNLY], Perforin [PRF1]) and NK cell activation/degranulation (CD4458, CCL4L259, STX11 [encoding Syntaxin 1160], CD8A61, LGALS1 [encoding Galectin 162], XCL1, SLC7A5 [encoding CD98/LAT163] and SELL [encoding CD62L64]) (Fig. 3e). GSEA confirmed upregulation of multiple pathways associated with cell function, particularly within Transitional, IFNγ- Adaptive and IFNγ+ Adaptive subsets (Supplementary Fig. 6). In PD1+ NK cells, there was also evidence for subset specific upregulation of the MAPK pathway (increased MAPKAPK2 and MAP2K2). Additionally, PD1+ NK cells had a large increase in ITGAX (encoding CD11c) expression during acute infection, with smaller increases in ITGAX in CD56bright and Transitional NK cells. CD11c expression in NK cells is upregulated in response to inflammatory cytokines65, and is a marker of bitypic NK cells which can produce inflammatory cytokines and also drive the proliferation of γδ T cells66. Further, upregulation of HLA-DR genes HLA-DQB1 and HLA-DRB5 were also detected, with HLA-DR previously associated with NK cell activation and antigen-presentation in some settings67.
Upregulation of genes mediating increased cytotoxicity and function during malaria was balanced by increases in multiple negative regulators of NK cells, including TNFRSF4 (encoding CD134/OX4068), TNFRSF9 (encoding CD137/4-1BB69), TNFRSF18 (encoding CD357/GITR70), LAG371, HAVCR2 (encoding TIM-372) and CBLB73. GSEA showed significant enrichment of negative regulatory pathways in PD1+ and IFNγ- Adaptive subsets (‘negative regulation of immune system process’ and ‘negative regulation of lymphocyte activation’) (Fig. 3e and Supplementary Fig. 7). Across all subsets, multiple Type I IFN signalling genes were upregulated including ISG20, IFI16, IFI6, IFITM3, IRF4, IRF8, and IRF7 and GSEA confirmed upregulation of ‘response to Type I IFN’ in Transitional and IFNγ- Adaptive cells (Supplementary Fig. 6). Type I IFN signalling in NK cells has been shown to suppress IFNγ production during viral infection74. Taken together data suggest that Type I IFN signalling is activated in NK cells in response to malaria, which may be linked to the induction of regulatory NK cells during infection.
To investigate these key transcriptional changes at the protein level, we analysed NK cells by flow cytometry in additional P. falciparum malaria patients (day 0) (n = 11) and patients 28 days after infection (n = 17). NK cells were identified as CD56bright, Adaptive and PD1+ subsets13(Supplementary Fig. 7A-B). Within these patients, there was a slight increase in CD56bright cells within the NK compartment during infection (Supplementary Fig. 7C). Across all three NK subsets, there was a significant increase in Granzyme-B and Perforin expression at day 0 compared to day 28 post treatment (Fig. 3f). In contrast, CD98 and HLA-DR expression were increased on Adaptive and PD1+ NK cells, but not CD56bright NK cells, and expression levels were much higher on PD1+ cell subset. Similarly, the regulatory marker LAG-3 was increased in expression on all NK cell subsets at day 0 (at very low levels on CD56bright cells), but TIM-3 was only increased on Adaptive and PD1+ cells (Fig. 3f). Expression of activation and regulatory markers on NK cell subsets was not associated with parasitemia, age or sex, aside from a relatively weak association between CD98 expression on PD1+ NK cells with parasitemia (rho = 0.4, p = 0.037) (Supplementary Fig. 8A, 9A, 10A). IFNγ and TNF expression were also assessed. While ex vivo IFNγ expression was below the limit of detection for all NK cell subsets, there was a significant increase in TNF production in Adaptive, but not CD56bright NK cells during malaria (Supplementary Fig. 7D). Additionally, there was a significant increase in CD11c expression on Adaptive NK, but not CD56bright cells (Supplementary Fig. 7E). When considering the total profile of Granzyme-B, Perforin, CD98, HLA-DR, LAG-3 and TIM-3 on the three distinct NK cell subsets, there was a significant difference in the overall composition of marker expression in each subset between day 0 and day 28, indicating significant upregulation of both cytotoxic and regulatory markers during infection (Fig. 3g). However, PD1+ NK cells are the most highly activated and regulatory during malaria due to the increased overall level of expression of these markers during acute infection, particularly CD98, HLA-DR, LAG-3 and TIM-3, compared to adaptive and CD56bright NK cells (Fig. 3h, Supplementary Fig. 7F).
Activation and regulation of γδ T cells with diverse functions during malaria
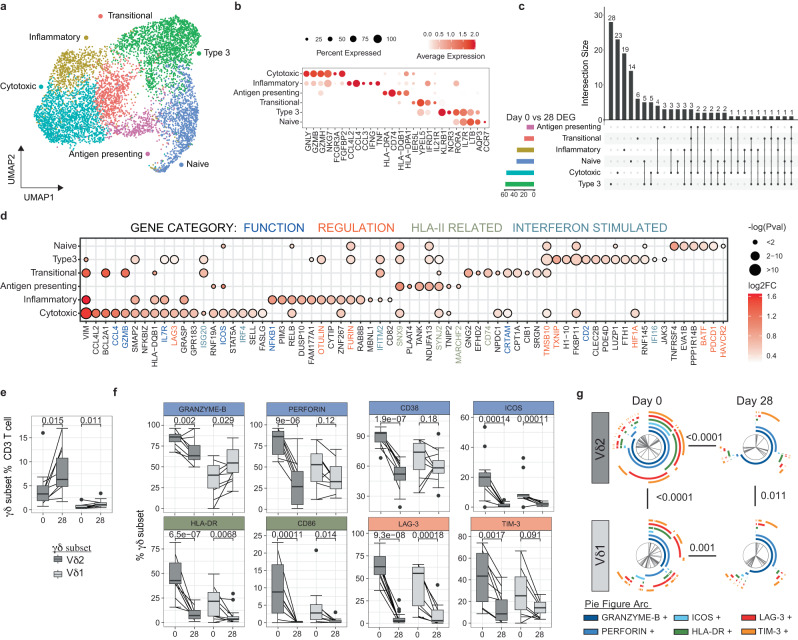
γδ T cells are key innate cell responders during malaria which proliferate in response to malaria parasites and produce inflammatory cytokines with important roles in protection75. γδ T cells can also recognize and kill parasites via lysis, and opsonic phagocytosis76, and present antigen to activate T cells77. However, in individuals who have had repeated malaria infections, γδ T cell activation is highly regulated, with reduced cell frequency, reduced inflammatory responsiveness and increased expression of proteins related to γδ T cell immunoregulation and exhaustion14,78. γδ T cells with increased expression of regulatory markers are associated with protection from symptomatic disease and, also have increased CD16 expression and CD16-dependent cytolytic responsiveness to opsonized parasites14,79. To explore these multiple roles and tolerization mechanisms of γδ T cells in the patients with acute malaria in a low endemic setting in this study, we sub-clustered γδ T cells identified in PBMCs (Fig. 1) and categorized 6 clusters as Cytotoxic, Inflammatory, Antigen-presenting, Transitional, Type 3 and Naive γδ T cells (Fig. 4a, Supplementary Data 5). Cytotoxic subset cells expressed the highest levels of GNLY, GZMB, GZMH, NKG7, FCGR3A (encoding CD16) and FGFBP2; Inflammatory subset cells expressed high levels of CCL4L2, CCL4, CCL3, IFNG and TNF; Antigen-presenting subset cells expressed HLA-II related genes; and Transitional γδ T cells were characterized by expression of genes that drive the early differentiation of T cells IL21R, IER5L, YPEL5 and IFRD1 (Fig. 4b). We also identified Type 3-like γδ T cells with high expression of KLRB1, NCR3, RORA and IL7R, and Naive γδ T cells with high expression of LTB, CCR7 and AQP4, as in previous scRNAseq data sets80. There was an increased proportion of the Cytotoxic cell with the γδ T cells compartment at day 7 and 28 after infection and increased Transitional cell subset at day 7 (p = 0.052, Supplementary Fig. 11A).
Fig. 4. Inflammatory activation and regulation of effector γδ T cells during malaria.
a/b Five subsets of γδ T cells were identified based on unsupervised clustering and marker expression as Cytotoxic, Inflammatory, Antigen-presenting, Transitional, Type 3 and naive. c Numbers of upregulated DEGs in γδ T cell subsets day 0 (n = 5) compared to day 28 (n = 6). The number of shared and subset specific DEGs indicated. d Top 20 upregulated DEGs in each γδ T cell subsets, and additional genes of interest with p ≤ 0.05. Genes with known roles in regulation and/or function are indicated. Log transformed p values (Wilcox test, two-sided, Bonferroni correction). e PBMCs from patients with P. falciparum malaria (day 0, n = 11) and convalescent malaria patients 28-days post-infection (day 28, n = 17) were analysed ex vivo to detect Vδ2+ and Vδ1+ γδ T cells and measure protein expression of identified genes by flow cytometry. f Expression of proteins related to function and regulation of γδ T cells (day 0, n = 11, day 28 n = 17), shown as positive frequencies of Vδ2+ and Vδ1+ γδ T cells. Box plots show the median and IQR of volunteers, lines represent paired observations, P values (two-sided) indicated are calculated by Mann-Whitney U test. Box and whisker plots indicate first and third quartiles for the hinges, median line, and lowest and highest values no further that 1.5 interquartile range from the hinges for whisker lines. g Co-expression of proteins related to function and regulation of Vδ2+ and Vδ1+ γδ T cells analysed in SPICE. Pie graphs comparisons performed by Permutation test (day 0, n = 11, day 28 n = 17). See also Supplementary Fig. 8-12, Supplementary Table 4 and Supplementary Data 5-6. Source data are provided as a Source Data file.
To investigate γδ T cell transcriptional changes during malaria, DEGs were identified in γδ T cell subsets, (Fig. 4c, d, Supplementary Data 6). Both shared and subset specific transcriptional changes between day 0 and day 28 where identified (Fig. 4c, d). Individual contributions to each cell subset and expression of DEGs at day 0 and day 28 is presented in Supplementary Table 4 and Supplementary Fig. 12. DEGs included genes associated with T cell activation (including VIM, ICOS, IL7R (encoding CD127)) across multiple subsets, consistent with inflammatory responsiveness during malaria infection75. Additionally, consistent with increased cytotoxic capacity during malaria reported previously76, expression of cytotoxic serine protease GZMB was increased in both Cytotoxic and Transitional γδ T cells during malaria. Further, CRTAM, which drives the development of cytotoxic CD4 and CD8 T cells81, was increased during infection, consistent with the expansion of Cytotoxic γδ T cell subsets at days 7 and 28 (Fig. 4d). Along with increased inflammatory and cytotoxic capacity, there was a suggestion of increased antigen presenting properties during infection, with upregulation of HLA-II related genes (CD74, HLA-DPB1, HLA-DQB1), and genes related to endocytosis and intracellular vesicle trafficking (such as SNX9 and SYNJ2). Together, these data are indicative of polyfunctional γδ T cell activation during infection, consistent with previous phenotypic data75–77.
Along with activation of multiple γδ T cell functions, increased expression of genes with roles in immunoregulation and cell exhaustion were detected (Fig. 4d). These included upregulation of LAG3 on Cytotoxic γδ T cells and increased expression of inflammatory regulators OTULIN82 and FURIN83 on Inflammatory γδ T cells. Within Type 3 and Naive γδ T cells, upregulated genes included those related to inflammatory regulation (TMSB10; which suppresses inflammatory macrophages)84, HIF1A; which controls γδ T cell mediated inflammation85 and BATF; which is upregulated in exhausted CD8 T cells86), cell exhaustion (PDCD1 (encoding PD1); which dampens inflammatory and cytotoxic potential of γδ T cell87,88, TNFRSF4 (encoding OX40) and HAVCR2 (encoding TIM-3); which reduces cytokine and cytotoxic potential of γδ T cells89 and pro-apoptotic signaling (TXNIP). Like myeloid and NK cell responses, DEGs included upregulation of multiple Type I IFN response genes including ISG20, IRF4, IRF1, IFITM2, IFI16. γδ T cells have been reported to respond to Type I IFNs produced from poly(I:C) activated cDCs in other settings90. However, to the best of our knowledge, a role of Type I IFNs in driving responding γδ T cells during malaria, has not been explored.
To confirm our transcriptional findings, we assessed protein-level expression of multiple functional and regulatory markers in additional patient samples, by flow cytometry (Supplementary Fig. 11B, C). While we were unable to differentiate between Vδ2+ and Vδ1+ γδ T cells in our 3’ transcriptional data set, the large majority of circulating γδ T cell within the CD3 T cell compartment at both day 0 during acute infection and day 28 post treatment were Vδ2+ γδ T cells (Fig. 4e). Within Vδ2+ cells γδ T cells, there was increased expression of Granzyme-B and CD38 at day 0, but not in Vδ1+ γδ T cells as detected (Fig. 4f). Other functional and activation markers, Perforin, ICOS, and HLA-DR were increased on both Vδ2+ and Vδ1+ γδ T cells during malaria. Similarly, LAG-3 was increased on both Vδ2+ and Vδ1+ γδ T cells during malaria but TIM-3 was only increased in Vδ2+ γδ T cells (Fig. 4f). Granzyme-B, ICOS and HLA-DR expression was higher on Vδ2+ compared to Vδ1+ γδ T cells during malaria (Supplementary Fig. 11D). Increased parasitemia during peak infection was associated with increased cell frequency and expression of CD38, ICOS and CD86 by Vδ2+ T cells and increased CD86 and HLA-DR by Vδ1+ T cells (Supplementary Fig. 8B). Additionally, Vδ1+ T cell expression of Perforin and TIM-3 increased with age in malaria-infected individuals (Supplementary Fig. 9B). No sex-dependent differences in γδ T cell phenotypes were observed (Supplementary Fig. 10B). To understand the expression of different functional, activation and regulatory markers on Vδ2+ and Vδ1+ γδ T cell subsets, marker expression was analysed by SPICE. Both Vδ2+ and Vδ1+ γδ T cells had high levels of co-expression of key proteins related to multiple functions and regulation (Fig. 4g). The magnitude and composition of marker co-expression by γδ T cells was increased at day 0 compared to day 28 expression.
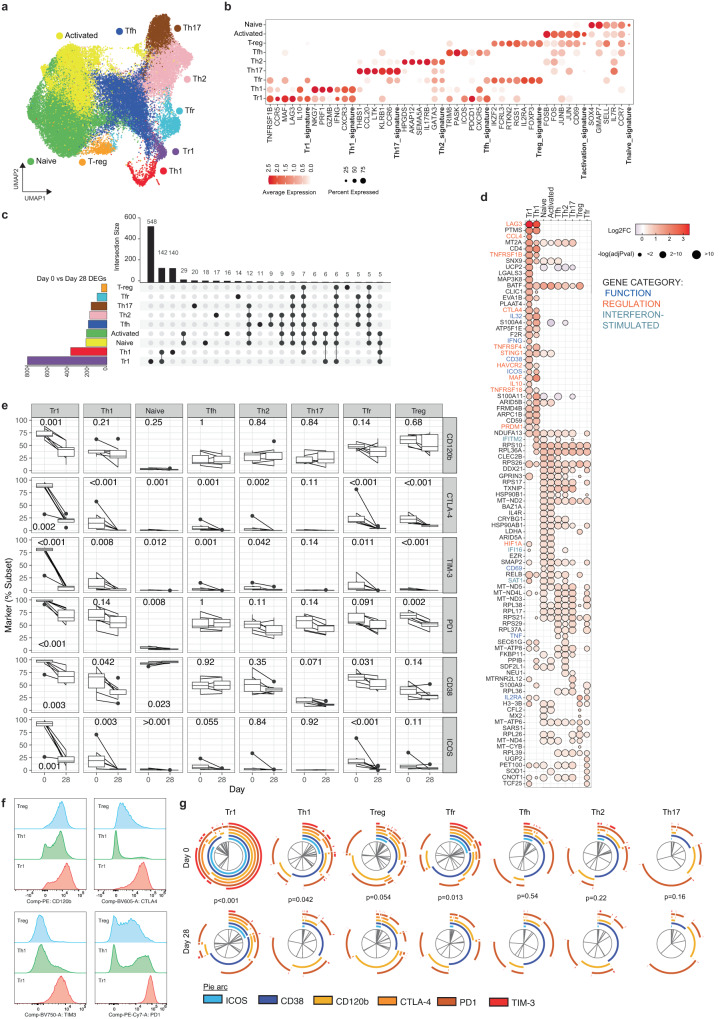
CD4 T cell response is dominated by Type 1 regulatory cells during malaria which share signatures with Th1 cells
CD4 T cells play multiple essential roles in protection from malaria, including IFNγ mediated direct killing of parasites, and by providing help to B cells to produce antibodies required for protection91. However, multiple lines of evidence have shown that malaria drives the expansion of regulatory CD4 T cells, particularly Type 1 regulatory (Tr1) cells that co-produce IFNγ and IL-10 in this disease. These cells rapidly expand via Type I IFN signalling in initial parasite infection in humans19, and dominate the parasite specific CD4 T cell response in children in endemic areas16–18. To investigate CD4 T cells transcriptionally during malaria, we subclustered CD4 T cells from PBMCs, with 9 subsets identified (Fig. 5a). These CD4 T cell subsets were annotated as naive, activated, T-regulatory (Treg), T-follicular helper (Tfh), T-follicular regulatory (Tfr), T-helper (Th) 1, Tr1, Th2 and Th17 subsets based on expression of T naive, activation, T-reg and T helper signatures92–95 and canonical marker genes (Fig. 5b, Supplementary Data 7). The proportions of each scRNAseq identified subset within the CD4 T cells compartment did not significantly change between acute infection and post treatment timepoints (Supplementary Fig. 13). We conducted DEG analysis for each CD4 T cell subset, on day 0 (malaria) compared to day 28 (post treatment (Supplementary Data 8, individual contribution to each subset was consistent, Supplementary Table 5, and DEG day 0 and day 28 expression at the individual level is presented in Supplementary Fig. 14). Tr1 and Th1 CD4 T cells were highly transcriptionally active during infection, while T-regs and Tfr were the least activated (Fig. 5c, Supplementary Data 8). In Tr1 cells, 68% of DEGs were unique, consistent with a Tr1 specific activation program during malaria (Fig. 5c). Upregulated genes included canonical markers of IFNG and IL10, and many other genes of co-inhibitory receptors with known roles in immunosuppression and/or function of regulatory T cells including LAG3, HAVCR2 (encoding TIM-396), TNFR297, CTLA498, TNFRSF4 (encoding OX40/CD13499), TNFRSF18 (encoding GITR/CD375100), PDCD1 (encoding PD1) and CCL4101 (Fig. 5d). These upregulated genes were also core signature genes used to identify Tr1 cells within the sub-clustered CD4 T cells at day 0 and 28 (Fig. 5a/b, Supplementary Data 7), suggesting that while the overall frequency of Tr1 cells in the periphery didn’t change with infection (Supplementary Fig. 13), the regulatory capacity of Tr1 cells was increased during malaria. The upregulation of multiple co-inhibitory receptors is consistent with our recent data showing Tr1 cells express overlapping co-regulatory proteins22. Additionally, IKZF3 which has been shown to have high expression in IL-10+ CD4 T cells102, and LAIR2 which has been identified as a core Treg cell signature gene in humans103 had increased expression on Tr1 cells during malaria (Fig. 5d). Tr1 cells also showed significant activation during infection, with marked upregulation of CD38 and ICOS during infection. CD38 upregulation was unique to Tr1 cells, while ICOS was also increased on Th1 cells.
Fig. 5. Tr1 CD4 T cells dominate the response during malaria.
a/b Nine subsets of CD4 T cells were identified based on unsupervised clustering and categorized based on canonical marker expression and T helper expression signatures. c DEGs in CD4 T cell subsets at day 0 (n = 5) compared to day 28 (n = 6) were identified. The number of shared and subset specific DEGs indicated in Upset plot. Overlaps of >5 genes are shown. d Top upregulated 20 DEGs in CD4 T cell subsets. Genes with known roles in regulation and/or function are indicated. Log transformed p values (Wilcox test, two-sided, Bonferroni correction). PBMCs from patients with P. falciparum malaria (day 0, n = 7) and convalescent malaria patients 28-days post-infection (day 28, n = 9) were analysed ex vivo to detect CD4 T and measure protein expression of identified genes by flow cytometry. e Expression of proteins related to function and regulation, shown as positive frequencies of CD4 T cell subsets: naive (CD45RA+ ), Tr1 (CD45RA-LAG3+CD49b+ ), Treg (CD45RA-Tr1-/FOXP3+CD127lo), Tfh (CD45RA-Tr1-/Treg-/CXCR5+ ), Tfr (CD45RA-Tr1-/Treg+ /CXCR5+ ), Th1 (CD45RA-Tr1-/Treg-/CXCR5-/CXCR3+CCR6-), Th2 (CD45RA-Tr1-/Treg-/CXCR5-/CXCR3-CCR6-) and Th17 (CD45RA-Tr1-/Treg-/CXCR5-/CXCR3-CCR6+ ). Box plots show the median and IQR of volunteers, lines represent paired observations, P values (two-sided) indicated are calculated by Mann-Whitney U test (day 0 n = 7, day 28 n = 9). Box and whisker plots indicate first and third quartiles for the hinges, median line, and lowest and highest values no further that 1.5 interquartile range from the hinges for whisker lines. f Concatenated histograms normalised to mode show expression of gene-related proteins within CD4 T cell subsets. g Co-expression of proteins related to function and regulation of CD4 T cell subsets analysed in SPICE. Pie graphs comparisons performed by Permutation test (day 0 n = 7, day 28 n = 9). See also Supplementary Fig. 13-17, Supplementary Table 5, and Supplementary Data 7-8. Source data are provided as a Source Data file.
Tr1 cells can emerge from Th1 cells that gain IL10 expression104. Consistent with this, most of the top upregulated genes in Tr1 cells were shared with Th1 cells, including regulatory markers LAG3, TNFRSF4 (encoding OX40), TNFRSF1B (encoding TNFR2), TNFRSF18 (encoding GITR), HAVCR2 (encoding TIM-3) and CTLA4 (Fig. 5d). Additional upregulated genes in Th1 cells included MAF, which drives IL10 expression in Th1 cells in murine malaria models105, PRDM1 (encoding BLIMP1), which promotes IL10 in Tr1 cells in murine malaria models106 and is highly expressed in malaria-specific Tr1 cells in Ugandan children16, and STING1 (encoding STING – stimulator of interferon response cGAMP interactor 1), which we have recently shown to be a central driver of Tr1 cell development107. In Th1 and/or Tr1 cells, several other Type I IFN responses genes were up regulated, including IFITM2, IFI16, SAT1, IFI35, IFI27L2, LYE6 and ISG15 (Fig. 5d, Supplementary Data 8). In other CD4 T cell subsets, the number of DEGs and magnitudes of fold changes to expression were relatively lower, with many ribosomal and mitochondrial genes shared across non-Th1/Tr1 subsets (Fig. 5c, d). However, BATF, which is critical for Th17 and Tfh cell differentiation108,109 was upregulated across all CD4 T cell subsets except for FoxP3+ Treg cells. While the roles of Th17 cells in human malaria are largely unknown, Tfh cell activation and development is critical for the induction of humoral responses required to drive protection against malaria110. Tfh cell activation during malaria is skewed towards Th1-Tfh cell responses111–113, and consistent with this, Th2 and Tfh cells subsets upregulated both the Th1 associated cytokine TNF, and ETS1 which represses Th2-Tfh subset differentiation in both human and mouse models of systemic lupus erythematosus114. ETS1 is also essential for BATF function in effector T cells115. While DEGs of Treg cells and Tfr cells were the lowest of all subsets, IL2RA, essential for Treg cell function116, was upregulated in malaria in both subsets, suggestive of increased functional Treg and Tfr cells during infection. Together these data are indicative of CD4 T cell activation dominated by Tr1 cells with increases suppressive function during malaria. The increase in Type I IFN signalling, is consistent with the the emergence of Tr1 cells from Th1 cells via Type I IFN signalling as shown previously19,22.
To further investigate the regulatory program in Tr1 and Th1 cells during malaria, we analysed responses on CD4 T cells subset at the protein level in additional study participants at day 0 and 28. CD4 T cells were gated as naive (CD45RA+), and non-naive (CD45RA-) cells, which were further analysed as Tr1 (LAG3+ CD49b+), Treg (Tr1-/FOXP3+CD127lo), Tfh (Tr1-/Treg-/CXCR5+), Tfr (Tr1-/Treg+ /CXCR5+ ), Th1 (Tr1-/Treg-/CXCR5-/CXCR3 + CCR6-), Th2 (Tr1-/Treg-/CXCR5-/CXCR3-CCR6-) and Th17 (Tr1-/Treg-/CXCR5-/CXCR3-CCR6+ ) cell subsets (Fig. S15A). Consistent with the emergence of Tr1 cells from Th1 subsets, the majority of Tr1 cells where Th1-like (CXCR3+/CCR6-/CXCR5-/FoxP3-) at day 0 during malaria (median 65.4%, IQR 62.5-73.8%, Supplementary Fig. 15B). Unlike scRNAseq identified subsets, there were increased proportions of Tr1 and Th2 cells, and decreased proportions of naive, Tfh, and Tfr cell subsets at day 0 compared to day 28 (Supplementary Fig. 15C). This difference may be due to the limited surface makers used to identify cells by flow cytometry compared to the overall transcriptional profile used in scRNAseq data, or the stable maintenance of underlying transcriptional programs compared to changes of chemokine receptor expression. On each CD4 subset, the proportion of cells expressing regulatory and activation markers CD120b (TNFRSF1B), CTLA-4, TIM-3 (HAVCR2), PD1 (PDCD1), CD38 and ICOS were analysed (Fig. 5e). Consistent with scRNAseq data, at day 0 during malaria, there was significantly higher proportion of Tr1 cells expressing CD120b, CTLA-4, TIM-3, PD1, CD38 and ICOS (Fig. 5e). Additionally, higher proportions of Th1 cells also expressed CTLA-4, TIM-3, CD38 and ICOS during malaria. Increased regulatory and activation markers were also seen on Treg and Tfr cells, but not Tfh, Th2, or Th17 subsets. The expression levels of co-inhibitory markers on Tr1 and Th1 cells was as high or higher than that on FoxP3+ Treg cells which are known to have suppressive function (Fig. 5f). Additionally, Tr1 cells expressed multiple co-inhibitory receptors during malaria (Fig. 5g). Increased parasitemia during infection was associated with increased proportions of PD1 expressing Tr1 cells and decreased proportions of CD120b expressing Tfh cells (Supplementary Fig. 16A). Age and sex were not associated with regulatory or activation markers on CD4 T cell subsets during malaria (Supplementary Fig. 16B and 17). To the best of our knowledge, the high regulatory T cell program seen here within the scRNAseq malaria data set has not been reported in other diseases38–40,117. Together data is supportive of specific upregulation of a regulatory program within CD4 T cells during malaria.
The role of CD8 T cells in immunity to P. falciparum blood stage malaria is unclear, particularly due to the lack of MHCI on the surface of RBCs. However, limited studies have reported activation and increased function of CD8 T cells during P. falciparum malaria, particularly in hospitalised patients118. To investigate CD8 T cell activation in acute malaria, CD8 T cells identified in PBMCs were subclustered. Naive/Central memory, Memory progenitor, Effector memory and Cytotoxic effector cells were identified (Supplementary Fig. 18A, B, Supplementary Data 9), the proportion of which was largely consistent between infected (day 0) and convalescence (day 28) (Supplementary Fig. 18C). We conducted DEG analysis for each CD8 T cell subset, on day 0 (malaria) compared to day 28 (post treatment (Supplementary Data 10, individual contribution to each subset was consistent (Supplementary Table 6), and DEGs at the individual level is presented in Supplementary Fig. 19). Compared to CD4 T cells only a small number of DEGs between day 0 and 28 were identified, the largest number being in cytotoxic effector CD8 cells (Supplementary Fig. 18D, Supplementary Data 10). Upregulated genes included those relating to increased inflammation and cytotoxicity (IFNG, TNF, CCL4, CCL3, IFNGR1, GZMB, PRF1) (Supplementary Fig. 18E). Genes associated with regulation were also upregulated in Effector subsets but no other CD8 T cell subsets (including LAG3 and CTLA4) (Supplementary Fig. 18E). While CD8 T cells can also differentiate into a phenotypically distinct regulatory lineage and produce IL-10 like Tr1 CD4 T cells in other diseases119, DEGs during malaria in CD8 T cells subsets had limited overlap with DEGs that dominated the Tr1/Th1 response in CD4 T cells, and no evidence of increased IL10 expression was detected (Supplementary Fig. 18F, G).
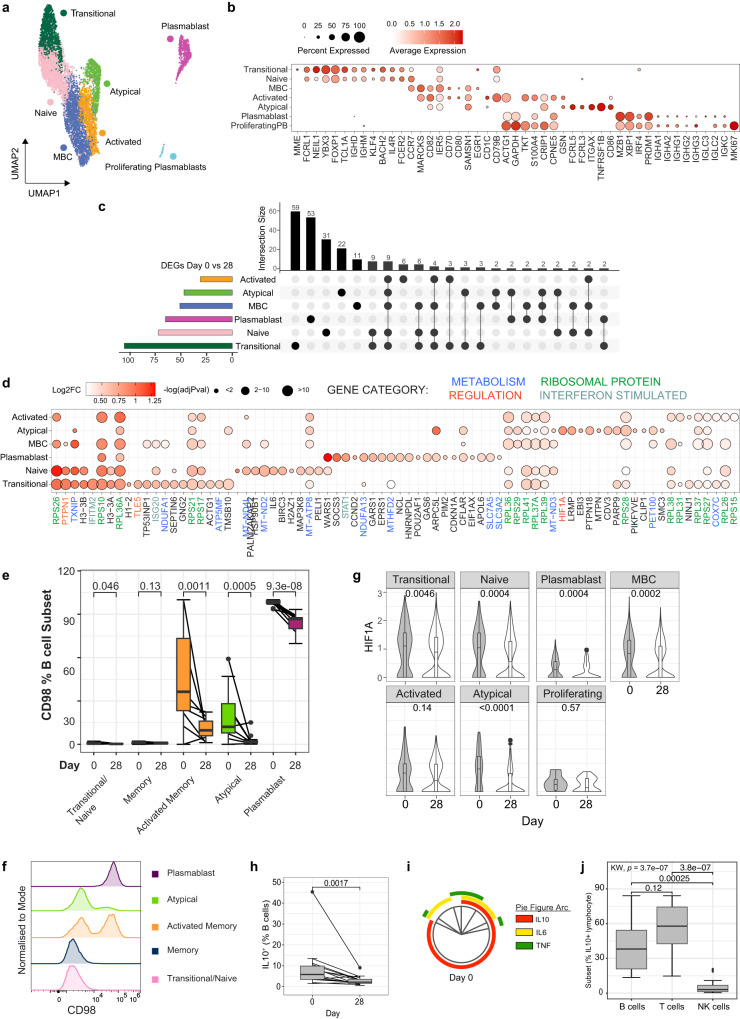
Expansion of IL-10+ regulatory B cells during malaria infection
Malaria specific B cell responses are essential for development of immunity against malaria, with antibodies being key mediators of protection through control of parasite burden120. While robust memory B cells and sustained antibodies can develop against malaria25, there is evidence that these responses may also be negatively impacted by malaria driven immunomodulation. Memory B cell responses are suboptimal in some malaria transmission settings, with lower levels of antibody production, short-lived antibody responses and expanded atypical memory B cells23–25. Atypical memory B cells express high levels of FCLR5 and appear to have reduced functional capacity compared to ‘typical’ memory B cells26,27. However, atypical responses emerge in both infection and vaccination121, mount recall responses122 and can produce antibodies with the support of T-follicular helper cells123. Therefore, whether atypical memory B cells are protective or disruptive in protective immunity remains unclear.
To investigate transcriptional changes to B cells during malaria within our PBMC data set, B cells were sub-clustered to identify 7 subsets of B cells (Fig. 6a). Based on previously published studies121,124,125, identified subsets included transitional B cells with high expression of MME (encoding CD10) and naive B cells with high expression of TCL1A, NEIL1, IGHD, IGHM, FOXP1, BACH2 and IL4R; quiescent memory B cells which had relatively high expression of memory marker CCR7, and upregulated MARCKS, CD82, IER5, CD70 and CD80 which are increased in expression on memory relative to naive B cells in previously published data sets126,127 annotated by the Human Protein Atlas (proteinatlass.org); activated B cells with increased expression of CD1C, CD79B, ACTG1, GAPDH, TKT, S100A10, CRIP2, CPNE5, and GSN; Atypical memory B cells with high expression of FCLR5, FCLR3, ITGAX (encoding CD11c), TNFRSF1B and CD86; plasmablasts with expression of MZB1, XBP1, IRF4, PRDM1 (encoding BLIMP1), and switched IgG genes; and proliferating plasmablasts which expressed plasmablast marker genes along with high levels of MKI67 (Fig. 6b, Supplementary Data 11). During infection (day 0), there was an increased proportion of plasmablasts, which made up to 20% of the B cell compartment, consistent with previous studies of in Ugandan128 and Kenyan children with malaria129, and in adults during controlled human malaria infection130 (Supplementary Fig. 20A).
Fig. 6. B cell activation and induction of IL-10+ Bregs during infection.
a/b Subsets of B cells were identified based on unsupervised clustering and categorised based on marker expression. c DEGs in B cell subsets day 0 (n = 5) compared to day 28 (n = 6) were identified. The number of shared and subset specific DEGs indicated in Upset plot. d Top upregulated 20 DEGs in B cell subsets. Genes with known roles in regulation and/or function are indicated, Log transformed p values, (Wilcox test, two-sided, Bonferroni correction). e CD98 protein expression was quantified on plasmablasts, transitional, atypical, memory and activated memory B cell subsets at day 0 (n = 11) and day 28 (n = 17). Box plots show the median and IQR of volunteers, lines represent paired observations, group comparisons performed by Mann-Whitney U test (two-sided). f CD98 MFI of concatenated samples at day 0 (n = 5). g HIF1A mRNA expression in each B cell subset at day 0 and 28. P-value calculated by Mann-Whitney U test P (two-sided) is indicated (unadjusted), data from scRNAseq analysis of day 0 n = 5 and day 28 n = 6 individuals. h IL-10 protein expression on B cells during malaria (day 0, n = 15) and day 28 post treatment (n = 14), Wilcoxon rank sum test (two-sided) is indicated. i Co-expression of B cell IL-10 production with IL6 and TNF during malaria (n = 15) analysed in SPICE. j The proportion of each lymphocyte subset contributing to IL-10 lymphocyte production during malaria (n = 15 individuals, at day 0). P-value (two-sided) calculated using Kruskal wallis and post-Dunn test (FDR adjusted for multiple comparisons) indicated. Box and whisker plots indicate first and third quartiles for the hinges, median line, and lowest and highest values no further that 1.5 interquartile range from the hinges for whisker lines. See also Supplementary Fig. 21-22, Supplementary Table 7 and Supplementary Data 11-12. Source data are provided as a Source Data file.
DEG analysis of each B cell subset comparing day 0 to day 28, identified large numbers of DEGs across all subsets except proliferating plasmablasts (Fig. 6c, Supplementary Data 12, individual cell numbers Supplementary Table 7, and DEG expression at day 0 and day 28, Supplementary Fig. 21). DEGs were both shared and subset specific, and a large number of the top DEGs for each subset were ribosomal proteins, possibly indicating increased protein synthesis and highly activated states of B cells during infection (Fig. 6d). Additionally, many DEGs had roles in metabolism, consistent with reshaping of energy use and metabolic programs during B cell activation131 (metabolic associated DEGs include members of NADH dehydrogenase complex NDUFA1, NDUFA13, MT-ND4L, MT-ND2, MT-ND3, cytochrome C oxidase subunit COX7C and chaperone PET100, ATP synthase subunits ATP5MF and MT-ATP8). Across B cell subsets, multiple upregulated Type I IFN signaling response genes were detected, including IFNITM2, ISG20, and STAT1, consistent with the important role of Type I IFN signaling in malaria immune responses across multiple cell subsets. There was evidence that metabolic remodeling during infection was B cell subset specific. For example, transitional, naive, memory B cells and atypical memory B cells during acute infection had increased expression of TXNIP, a glucose feedback sensor which inhibits glucose uptake132,133. In contrast, plasmablasts had increased SLC7A5 (encoding LAT1) and SLC3A2 (encoding CD98 which interacts with LAT1 to transport L-glutamine), consistent with our recent findings of the importance of plasmablasts as negative regulators of germinal centre development via acting as a nutrient sink in mice models of malaria130. To confirm upregulation of glutamine transport on plasmablasts, CD98 levels were measured across B cell subsets in additional patients. We assessed CD98 expression during and after malaria in plasmablasts (CD27+CD38+), transitional/naive IgD+ B cells, and IgD- B cell subsets (atypical [CD27-CD21-], memory [CD27+CD21+] and activated memory [CD27+CD21-]) (Supplementary Fig. 20B, C). In these additional participants, plasmablasts made up to 30% of the B cell compartment during malaria, but less than 2% at 28 days post-treatment (Supplementary Fig. 20D). There was also a significant increase in the proportion of activated memory cells during malaria (Supplementary Fig. 20D). The frequency of CD98+ cells in each subset increased during malaria in plasmablasts, transitional/naive, atypical and activated memory B cells (Fig. 6e). However, the frequency of CD98+ cells, and the magnitude of CD98 expression was far greater on plasmablasts compared to other subsets (Fig. 6f, Supplementary Fig. 20E, F). Together, these data are consistent with a potential negative role of plasmablast expansion and CD98 expression as a nutrient sink that limits productive germinal center activation during infection130, but shows that activated memory B cells also upregulate glutamine transport during infection.
Along with a potential disruptive role of plasmablasts in malaria infection, several upregulated DEGs where suggestive of other tolerized/immunosuppressed B cell responses during infection. For example, PTPNI (encoding PTP1B) which was upregulated in transitional, naive and memory B cell subsets, negatively regulates B cell signally via CD40, BAFF-R and TLR4, and downregulates T-dependent immune responses134. TLE5 (also known as AES), which negatively regulates NF-κβ signaling135, required for B cell activation and survival136, was upregulated on transitional B cells during infection. Of note, HIF1A, which drives B cell IL10 production in hypoxic conditions137, was significantly upregulated in Atypical B cell during acute infection. Further interrogation of HIF1A suggested increased expression during acute infection also occurred in transitional, naive, memory B cells and plasmablasts subsets (Fig. 6g), consistent with the capacity of diversity of human B cells subsets to produce IL-10138. IL-10 production by B cells is indicative of Breg subsets, which have been shown in mice to be a major source of IL-10 during experimental malaria infection, and protect from experimental cerebral malaria28,139, however have yet to be identified during human malaria. To confirm the expansion of IL-10+ Bregs during P. falciparum malaria, we quantified IL-10+ production in B cells in additional study participants. We analyzed the total B cell population, due to the diverse B cell phenotypes of IL-10+ Bregs, and measured TNF and IL-6 production, which are often co-produced with IL-10138 (Supplementary Fig. 22A). Data showed there was significant increase in IL-10 production in B cells during malaria, indicating of malaria induction of Bregs (Fig. 6h). In contrast, there was no evidence for increased B cells expression of IL6 nor TNF, despite increased IL6 transcript levels (Supplementary Fig. 22B). IL-10 B cell production was not associated with parasitemia, age or sex (Supplementary Fig. 22C/D/E). Although a previous study reported co-expression of TNF and IL6 by IL-10 producing Bregs138, only a small fraction of IL-10+ Bregs co-produced IL6 during malaria, and there was minimal co-expression with TNF (Fig. 6i). To assess the relative importance of Bregs, compared to IL-10+ T cells (largely Tr1 CD4 T cells), the proportion of B cells amongst all IL-10 producing lymphocytes was measured. The proportion of IL-10 lymphocytes that were Bregs was comparable to CD3 cells as the source of IL-10 from lymphocytes (Fig. 6j), identifying IL-10 Bregs as a potentially important contributor to the regulatory/tolerogenic response during malaria infection in humans.
Discussion
Malaria drives tolerogenic immune cell responses which protect from inflammation mediated immunopathogenesis at the costs of reduced parasite control and suboptimal adaptive immunity. Here, using scRNAseq analysis of PBMCs during and following P.falciparum malaria, we comprehensively map malaria associated tolerogenic responses across innate and adaptive immune cells. These data show that malaria driven immunomodulation occurs across the immune landscape, with subset specific activation and regulatory programs identified. By analysing malaria-driven transcriptional changes at the subset level, we not only increase our understanding of how malaria modulates specific immune cell subsets, but also identify IL-10+ Bregs as a major tolerogenic response in human adaptive immune cells during infection.
The use of scRNAseq analysis PBMC immune responses during other infections has identified key protective and disrupted responses in various disease states39,117,140,141. Here, we leveraged a large data set of >40,000 cells to understand malaria driven immune responses within major immune subsets, but also within subclustered cells. This approach allows for a granularity of understanding of subset specific cell responses not previously possible with bulk-level analysis. Within innate myeloid cells, malaria drove changes to monocytes consistent with the induction of immunosuppressive MS1-like monocytes, which have high expression of alarmins S100A8/A9, along with RETN and ALOX5AP and reduced expression of MHC class II. These immunosuppressive monocytes have been identified in scRNAseq data sets in both sepsis and COVID-19 patients (particularly those with severe disease), but not HIV infected individuals or during dengue infection38–40,117. During sepsis and COVID-19, immunosuppressive monocytes appear to emerge directly from inflammation-induced myelopoiesis within the bone marrow38,142. This pathway may also be important in malaria, with parasite infection shown to drive emergency myelopoiesis in mouse models143. How these immunosuppressive monocytes protect from parasite-mediated immunopathology is unknown, however, the importance of tolerized monocytes in anti-disease immunity to malaria has been suggested by others11. This anti-disease protection may come at a cost to both adaptive immunity by disruption of antigen presentation via down regulation of HLA-DR, which was also seen in DCs8, and more broadly. For example, in sepsis, immunosuppressive monocytes have reduced responsiveness to LPS (TLR4 stimulation), consistent with dysregulated response to future bacterial infection in these patients38. Reduced responsiveness to LPS has also been reported for monocytes exposed to P. falciparum parasites in vitro11. As such, immunosuppressive monocytes may also be an important factor in the increased risk of bacterial infection in children with recent or acute malaria144. Despite the down regulation of cytokines and chemokines within the myeloid compartment, we also observed that many receptors involved in antibody mediated parasite control, including CD163, CD93, FCGR1A & 2A, FCAR and CR1 were upregulated, consistent with recent reports by others48, and an important role in monocytes in antibody Fc mediated protection. As such, while inflammatory monocyte responses are diminished, other functions are maintained during acute infection.
Evidence of malaria induced immunosuppression within our data was also observed in NK and γδ T cell subsets, where multiple co-inhibitory receptors were upregulated during infection (including TNFRSF4, TNFRSF9, TNFRSH18, HAVCR2, LAG3, and PDCD1). Co-inhibitory receptors play important roles in regulating immune response to chronic infections, including malaria145. For NK cell responses, increased PD1 expression has been previously reported in malaria exposed individuals previously13, however the roles of other co-inhibitory receptors in regulating NK cell responses during malaria have not been investigated. With others, we have recently shown that a CD56neg NK cell subset is expanded in areas of high malaria burden and have important functional roles in protecting from diseases via antibody dependent cellular cytotoxicity146. These CD56negNK cells had high expression of LAG-3, a molecule which has been shown in other studies to be expressed on NK cells with increased glycolytic activity and to negatively regulate NK cytokine production but not cytotoxic activity71. Here, LAG-3 and other co-inhibitory receptors appeared to be expressed to the highest levels on PD1+ NK cells, which contained both CD56++/bright and CD56dim cells. PD1+ NK cells were the most highly activated NK cells during malaria, and had high granzyme-B and perforin expression, consistent with retained cytolytic capacity. Further studies are required to understand the relationship between CD56neg NK subsets, and PD1+ cells.
Within γδ T cells, upregulation of co-inhibitory receptors on Vδ2+ cells to mediate tolerance has previously been shown in areas of high malaria burden14. Indeed, several of these regulatory genes (BATF, HAVCR2, TXNIP) have been previously shown to be increased transcriptionally and at the protein level in Vδ2+ γδ T cells in children with recent or high levels of repeated infection14,78,89. While Vδ1+ γδ T cells are less well studied in malaria, some LAG-3 expression was detected on Vδ1+ γδ T cells during controlled human malaria infection of Tanzanian adults147. Here we show that multiple co-inhibitory receptors are also upregulated on γδ T cell during an acute infection in a low transmission setting, on both Vδ2+ cells, which dominated the response, but also on Vδ1+ γδ T cells. In areas of high malaria burden, Vδ2+ γδ T cells with inhibitory receptors maintain or have enhanced cytolytic capacity and antibody dependent functions79, and recent studies have suggested that on Vδ1+ γδ T cells with increased cytotoxic capacity expand with repeated malaria infection148. Consistent with this, co-inhibitory markers were upregulated concurrently with increased Granzyme-B and perforin, indicative of cytolytic function. Together, these data suggest that regulatory proteins have the potential to play a role in controlling inflammation, while other cytotoxic functions of NK and γδ T cells are maintained.
Within CD4 and B cell subsets, tolerogenic responses appeared dominated by a major upregulation of IL10. Within CD4 T cells, the Tr1 cell subset was the most highly activated during malaria, and these cells had significantly increased transcription of both canonical cytokines IL10 and IFNγ, and multiple co-inhibitory receptors (including LAG3, OX40, TNFR2, GITR, TIM3 and CTLA4). A large proportion of malaria driven DEGs in Tr1 cells were shared with Th1 cells, consistent with an emergence of Tr1 cells from the Th1 cell subset104. Indeed, the majority of Tr1 cells identified at the protein level expressed Th1 chemokine receptor CXCR3. DEGs in Tr1 cells also included transcriptional factors with known roles in Tr1 cell development (MAF, PRDM1 and STING)22,105–107. Similarly, within B cell subsets, malaria drove a significant increase in HIF1A expression, which has previously been shown to be a critical transcription factor for the induction of IL-10 producing Bregs in mouse models137. Consistent with this, we show significantly increased ex vivo secretion of IL-10 from B cells during malaria compared with 28 days post-treatment in additional individuals. Indeed, during infection B cells were a major contributor of IL-10 from lymphocytes during malaria. While IL-10 producing CD4 T cells have been well recognised in malaria16,18,22,106,107,149, this study identifies B cells as a major source of IL-10 during human malaria. Further studies are needed to understand the development of Bregs during malaria, their roles in anti-disease and anti-parasitic immunity and/or immunosuppression150. Additionally, the potential link between Tr1 cells as the driver of Breg activation to suppress inflammation and disease as shown in other settings should be investigated151.
Taken together, data here and previous studies, highlight the multiple tolerogenic responses induced during malaria across the immune landscape. These regulatory landscapes are not common across all infections, and the upregulation of multiple co-inhibitory markers have not been detected in comparable scRNAseq analysis of PBMCs during SARS-CoV-2, influenza, HIV or dengue38–40,117. A potential link of malaria-induced tolerogenic responses across all immune cell subsets, is Type I IFN signalling, with Type I IFN responses and increased transcription of IFN-stimulated genes detected across the immune landscape. While first described in viral infection as critical effector cytokines, other studies have also shown that Type I IFNs exhibit immunoregulatory effects that impeded control of some non-viral pathogens152, including protozoan parasites153. In malaria infection, Type I IFNs have both protective and detrimental impacts on immune response, parasite clearance and protection from immunopathogenesis, dependent on timing, parasite species and model system (reviewed in ref. 29). Indeed, previous studies in human experimental infection have shown that P. falciparum parasites rapidly induce Type I IFNs that drive development of regulator Tr1 CD4 T cells19. While not directly investigated in malaria, Type I IFN signalling has been reported to negatively regulate NK cell inflammatory response during viral infection74, promote upregulation of LAG-3 on NK cells in healthy donors71, and drives Breg induction in helminth infection154. While the causative role of Type I IFN signalling in driving the upregulation of regulatory cell phenotypes seen here remains to be confirmed mechanistically, our team is currently exploring whether host-directed therapies that transiently block Type I IFNs may have therapeutic roles in enhancing protective anti-parasitic immunity155,156.
A number of limitations of our study should be noted. The primary aim of this study was to identify malaria driven transcriptional changes at the cell subset level. However, once PBMC cells are subclustered, relatively low cell numbers were available for analysis to identify malaria DEGs in rare cell types. As such, we were not able to identify DEGs at the individual donor level, and therefore may have overlooked individual level heterogeneity. While the overall expression levels of DEGs at day 0 and 28 were consistent across individual, we further investigated this potential heterogeneity by confirming key transcriptional changes at the protein level in additional patients. In all cases, we considered day 28 ‘convalescent’ time point, but it should be noted that others have reported sustained changes to multiple cell subsets up to a year after a malaria infection48, and there were significant DEGs between day 28 and endemic control cells, as such day 28 may not be a completely ‘healthy’ time point. Future studies are required to better understand maintained changes at day 28 post infection, along with more detailed study of immune cell activation between treatment (day 0) and day 7. The limited number of individuals analysed by scRNAseq also precludes the analysis of the impact of other host factors such as age, sex, parasite burden and/or disease manifestations on transcriptional changes. Future studies could take advantage of rapidly developing technologies to increase cell numbers and/or individuals used in transcriptional studies. Additional technical limitations include the use of 3’ sequencing, as such clonal development and TCR/VDJ usage was not investigated. Additionally, only PBMCs responses were assessed, and how these peripheral responses related to the immune response within tissues is unknown. Further, malaria antigen specific T and B cells were not assessed, and future studies are required to specifically investigate antigen specific response during and after infection. Our study only investigates one study site with all patients >3 years of age and presenting with uncomplicated malaria where other important genetic factors are unknown (such as sickle cell trait which influences malaria symptoms and immune responses157), and as such the broad application of results to other malaria transmission settings, young patients, known genetic backgrounds and/or disease phenotypes is unknown. Finally, while data is indicative of a tolerogenic response across multiple immune cell populations, further mechanistic studies are required to confirm that these cell responses are functionally suppressive. Future studies are also required to investigate whether Tr1/Th1 CD4 cells and Bregs induced in malaria responding in an antigen specific, or globally suppressive manner.
In conclusion, we use scRNAseq analysis of a large number of PBMC cells to make a granular level study of immunoregulatory responses across the immune landscape during P. falciparum malaria. All data sets and interactive integrated scRNAseq data file is made publicly available for future analysis of the malaria immune landscape by the research community.
Methods
Study design
To investigate malaria driven transcriptional changes in specific immune cell subsets, we sorted live PBMCs from 6 malaria infected donors (day 0), and two subsequent time points after drug treatment (day 7 and 28), along with PBMCs from 2 healthy controls. We performed scRNAseq of these cells and used clustering and sub-clustering to identify specific immune cell subsets. Differential gene analysis between day 0 and day 28 was performed for each cell cluster and sub-cluster. Key transcriptional changes were confirmed at the protein level with additional donor samples. Patient demographics are in Supplementary Table 1.
Ethics statement
Ethics approval for the use of human samples was obtained from the QIMR Berghofer Human Research Ethics Committee (HREC P3444), the Northern Territory Department of Health and Menzies School of Health Research ethics committee (HREC 2010-1431), and Medical Research and Ethics Committee, Ministry of Health, Malaysia (NMRR-10-754-6684 and NMRR-12-499-1203). Written informed consent was obtained from all adult study participant or, in the case of children, parents or legal guardians. Participants were compensated for transport costs for follow up visits to clinics following discharge.
Study participants and peripheral blood mononuclear cell processing
Peripheral blood mononuclear cells (PBMCs) and plasma were obtained by convenience sampling of patients with uncomplicated malaria from previous conducted clinical trials and cohort studies of malaria conducted in Sabah Malaysia between 2010 and 2016. During this period, P. falciparum malaria was low in Sabah Malaysia, with an estimated incidence of 0.18/1000 people in 2011158. These studies included a randomized controlled trial of artemether-lumefantrine against chloroquine159, and a clinical efficacy study of oral artesunate followed by oral mefloquine160, both conduced on patients with acute malaria at three district hospital sites (Kudat, Kota Marudu and Pitas)160,161, and a prospective observational study which malaria patients conducted at the tertiary referral center (Queen Elizabeth Hospital, Kota Kinabalu)162. Within these studies, non-pregnant patients (aged >3 years) with microscopy-diagnosed malaria who provided written informed consent were enrolled. For the drug treatment trials, treatment for individuals followed randomization. All individuals regardless of treatment were aparasitemic by 72 hours, confirmed by thick smear or PCR159,160. For the observational study, treatment followed hospital guidelines: artemether-lumefantrine for P. falciparum and P. knowlesi malaria; chloroquine and primaquine or ACT for P. vivax malaria; and intravenous artesunate for severe malaria, or if deemed warranted by the treating clinician. Severe malaria was defined according to 2014 WHO guidelines, and patients with severe disease were not included in current immunology study. No treatment failures were reported. Across all trials/cohorts a higher proportion of infected males was observed across all malaria species, possibly because of infection risk of forest worker161. Within these parent studies, blood samples were collected and archived for future studies from individuals at enrolment (acute malaria timepoint, day 0), and 7- and 28-days post-treatment. Additionally, samples were collected from individuals who had been living in the area in the preceding 3 weeks, who were negative for Plasmodium by microscopy, and who had no history of fever in previous 48 hours were as endemic healthy control samples (EC). Blood was collected in lithium-heparin collection tubes, then PBMCs and plasma were isolated from whole blood via density centrifugation with Ficoll-Paque prior to cryopreservation.
For the current immunology study, individuals for scRNAseq analysis were selected from parent studies based on sample availability of repeated blood samples at day 0, 7 and 28 after enrolment/treatment and confirmed uncomplicated P. falciparum mono-infection by PCR. For phenotypic analysis, further individuals from the same parent clinical trials/cohort were selected based on sample availability at day 0 (acute malaria and enrolment) with uncomplicated malaria and confirmed P. falciparum mono-infection by PCR. Not all day 0 samples also had a day 28 sample available, so additional day 28 (convalescence) time points were selected. Sex (self-determined) and age, reported in Supplementary Table 1, were not considered in sample selection, but all sex and age associations are reported in supplementary figures. Patient had a range of parasitemia during infection and clinical characteristics, which are presented in Supplementary Table 1. Cytomegalovirus sero-status was measured using plasma samples using the Human Anti-cytomegalovirus IgG ELISA Kit (CMV) ab108724. 100% of individuals were CMV positive (Supplementary Table 1).
10X Genomics Chromium GEX Library preparation and sequencing
PBMC samples were thawed in RPMI 1640 (Gibco) containing 10% FCS and 0.02% Benzonase. 1E6 PBMCs were stained for viability with Propidium iodide (PI), and live cells were sorted on BD FACSAria III Cell Sorter into 2% FBS/PBS and counted on hemocytometer. Up to 10,000 cells were loaded into each lane of Chromium Next GEM Single Cell 3ʹ Reagent Kit v3.1 and Gel Bead-in-Emulsion (GEMs) generated in Chromium Controller (Chromium Next GEM Single Cell 3’ GEM, Library & Bead Kit v3.1, PN-1000121, Chromium Next GEM Chip G Single Cell Kit PN-1000120, Single Index Kit T Set A, PN-1000213). Samples were run in two batches, which were later integrated. 3’ Gene Expression Libraries were then generated according to manufacturer’s instructions. Generated libraries were sequenced in a NextSeq 550 System using High Output Kit (150 Cycles) version 1 according to manufacturer’s protocol using paired-end sequencing (150-bp Read 1 and 150 bp Read 2) with the following parameters Read 1: 28 cycles, Index 1: 8 cycles, Read 2: 91 cycles.
scRNAseq transcriptomic analysis
Pre-processing of raw sequencing files
Single cell sequencing data was demultiplexed, aligned and quantified using Cell Ranger version 3.1.0 software (10x Genomics) against the human reference genome (GRCh38-3.0.0), with default parameters. Raw sequencing data and processed Cell Ranger outputs are found at GSE217930, https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE217930. Cell ranger count matrices for each sample (donor and day) were loaded, merged and analysed using Seurat package v4163.Cell cycle scores, mitochondria DNA transcripts and complexity score (log10genes per UMI) were calculated per cell using Seurat built-in functions. Cell cycle score was assigned to each cell using the CellCycleScoring function and evaluated with Principal Component Analysis (PCA). Cells with less than 20% of mitochondria DNA transcripts, complexity score higher than 0.8 and at least 250 genes and 500 UMIs were retained (Supplementary Fig. 1A). We observed a low cell number and mitochondrial ratio in the ‘child1day0’ sample due to a 10X Chromium wetting error, therefore this sample was removed from further analysis (Supplementary Fig. 1B). At the gene level, any haemoglobin-associated genes and genes expressed in less than ten cells were filtered out. The filtered dataset was scaled to regress out the effects of mitochondria DNA transcripts content and cell cycle using the ScaleData function, which regresses each variable individually. We followed the integration workflow included in Seurat to remove sources of variation due to donor (Supplementary Fig. 1C). To do so, filtered data was split per donor and day. Each dataset was normalise using the NormalizeData function, and the most variable genes in each of them were selected using FindVariableFeatures. Before integration, the most variable genes shared among the datasets were identified using FindIntegrationAnchors and used to integrate the datasets using IntegrateData function. During integration we also performed CellCycleScoring to improve the accuracy and robustness of downstream analyses by accounting for the effects of the cell cycle on gene expression.
Cell clustering and sub-clustering
We applied a linear transformation using ScaleData and regressed out mitochondrial contamination a source of unwanted variation. The top 30 principal components (PCs) were calculated using RunPCA. From these 30 PCs we constructed a k-nearest neighbour graph Euclidean distance in PCA space and refine the edge weights between any two cells based on the shared overlap in their local neighbourhoods (Jaccard similarity), based on standard Seurat workflow. Next, we applied the Louvain algorithm as our modularity optimization technique to set the granularity of clusters at a resolution of 0.6. The non-linear dimensionality reduction technique ‘UMAP’ was used to visualise cluster in 2D space. Clusters were annotated based on canonical marker expression, with 15 cell subsets identified (Supplementary Fig. 1C). NK, γδ T, CD4 T, CD8 T and B cells clusters were extracted into individual Seurat objects after scaling, we identified principal components, clustered with the Louvain algorithm at unique resolutions for each subset and annotated by dimensionality and expression of genes related to canonical subset phenotypes as above. For all cell subsets, integration allowed for identification of cell subset clusters across all individuals (Supplementary Fig. 23).
For CD4 T cells, T helper signatures from prior publications; Tfh92, Tr195 and Th1, Th2, Th17, Treg93 were analysed within sub clusters. For high level cell clusters, and sub-clustering analysis, marker genes for all clusters (outputs from ‘FindAllMarkers’) are in Supplementary Data 1, 3, 5, 7, 9, 11. Individual contributions to identified clusters, and total cell numbers in each cluster are found in Supplementary Tables 2-7. Processed Seurat file “annotated_Sabah_data_21Oct2022.rds” is found at 10.5281/zenodo.6973241. Analysis code can be accessed at https://github.com/MichelleBoyle/scRNAseq_malaria_2023.
Differential gene expression analysis
To identify genes differentially expressed during malaria, ‘FindMarkers’ function with default parameters in Seurat (including p value calculated with Wilcox test, two sided, with Bonferroni correction) was used comparing specific cell subsets at different time points. DEGs for each cluster and subcluster are found in Supplementary Data 2, 4, 6, 8, 10, 12. Identified DEGs were analysed via Gene Set Enrichment Analysis, using GSEA publicly available software (https://www.gsea-msigdb.org/gsea/index.jsp)164,165, to identify significantly enriched gene ontology (GO) terms for each high-level cluster and subcluster during malaria infection. The HOMER v4.9 package was used to identify significantly overrepresented upstream regulators, of cis-elements 1 kb upstream of the transcription start site (TSS) of the DEGs using the findMotifs.pl script166. Shared and subset specific DEGs were visualised using Upset plots using UpSetR package v1.4.0167. DEGs were identified as a tolerogenic signature based on previously described functions as co-inhibitory receptors145.
Flow cytometric cell phenotyping comparison of scRNAseq samples
2 million cells from the same PBMC vial as used for scRNAseq was used for phenotyping of major cell subsets (Supplementary Table 1). Cells were stained at room temperature with LIVE/DEAD Fixable Blue and surface markers with antibodies purchased from BD Biosciences or Biolegend (Supplementary Table 8). Data were acquired with 3-laser Cytek Aurora, and subsets identified as described in Supplementary Fig. 1.
Flow cytometric ex vivo cytokine production analysis
PBMCs were thawed and 1 million cells incubated at 37°, 5% CO2 for 2 hours without additional stimulation as above, in additional study patients with P. falciparum malaria at day 0 and day 28 post-treatment. Protein transport inhibitor containing Monensin and protein transport inhibitor containing Brefeldin A were added to cells (both 10μg/ml, BD Biosciences) and cells cultured for an additional 4 hours to capture the cytokine production of these cells due to current/recent infection without further stimulation ex vivo via re-stimulation. Cell surface staining was performed at RT for 15 minutes with a panel of antibodies purchased from Biolegend, BD Biosciences or Miltenyi-Biotec (Supplementary Table 9). Following 2 washes with 2%FCS/PBS, cells were permeabilised with BD cytofix/cytoperm solution for 20 minutes on ice. Intracellular staining (ICS) was performed following this to assess cytokine production. Intracellular staining was performed using antibodies listed in (Supplementary Table 9). Samples were incubated with the antibodies for 30 minutes on ice, washed twice with BD perm wash buffer then fixed with BD stabilising fixative. All samples were resuspended in 200 µl of 2%FCS/PBS to be acquired the following day. Data were acquired using a Cytek Aurora 5, and subsets identified as shown in Supplementary Fig. 4A, B, 7A and 22A. To identify CD16 monocytes, an alternative gating strategy based on CCR2 and CD33 expression168, due to the rapid down regulation of CD16 in cultured cells.
Flow cytometric ex vivo cell phenotyping of DEGs
PBMCs were thawed in additional malaria study patients as above, at day 0, and day 28 post malaria infection. Due to sample limitations, not all patients had paired samples for this analysis. γδT-B-NK ex vivo cell phenotyping contained 11 day 0 samples and 17 day 28 (paired observations, n = 8) and CD4 ex vivo cell phenotyping contained 7 day 0 samples and 9 day 28 (paired observations, n = 7). Surface markers, dead cell stains and intracellular stains were performed at the concentrations provided with antibodies purchased from Becton-Dickson Biosciences, Biolegend or Invitrogen (γδT-B-NK: Supplementary Table 10 and CD4: Supplementary Table 11). CD4 ex vivo cell stains were rested for 2 hours prior to staining protocol. PBMCs were stained in Fc block with CD366 (TIM-3) and CD223 (LAG-3) at 37 °C for 90 minutes in γδT-B-NK ex vivo and with CD223 (LAG-3), CD49b and CCR7 at 37 °C for 45 minutes in CD4 ex vivo. Cells were then washed and stained at RT for 15 minutes with LIVE/DEAD Fixable Blue Dead Cell Stain, washed twice with 2% FCS/PBS and stained at RT for 30 minutes for additional surface markers. Following 2 washes with 2% FCS/PBS, cells were permeabilised with eBioscience Fixation/Permeabilization solution for 20 minutes on ice. Intracellular staining (ICS) was performed for 30 minutes on ice following washes to assess intracellular proteases and glycoproteins. Cells were fixed with BD stabilising fixative then resuspended in 200 µl of 2%FCS/PBS until acquisition. Data were acquired using a Cytek Aurora 5 and subsets and marker expression identified as described in Supplementary Figs. 2, 7A, B, 11B, C, 15A, and 20B.
Flow cytometric data analysis
Flow cytometry data were analyzed in FlowJo version 10. Gating strategies are outlined in Supplementary Fig. 2, 4A, B, 7A, B, 11B, C, 15A, 20B and 22A. To measure the co-expression of cytokines or other markers on specific subsets, expression was analysed by SPICE (Simplified presentation of incredibly complex evaluations49), and permutation tests between combinations of cytokines/markers performed. For myeloid cytokine analysis, data was not included in analysis if <50 cell events were gated.
Statistical analysis
All statistical analysis was performed in RStudio (R version 4.0 or greater). All statistical tests are two-sided. To assess correlations between cellular clusters identified by scRNAseq and flow cytometry, Pearson correlations were calculated. For cell proportions and expression levels, for paired data, Wilcoxon signed-rank test was used and for unpaired data, Mann-Whitney U test was performed. Graphing was done with ggplot2 v 3.4.1169.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Supplementary information
Description of Additional Supplementary Files
Source data
Acknowledgements
We thank all the participants and parents of guardians involved in the clinical studies, along with the Malaysian Ministry of Health hospital directors and clinical staff at Kudat, Kota Marudu and Pitas district hospitals and at Queen Elizabeth Hospital, Kota Kinabalu. We thank support staff in QIMR Flow Cytometry and Imaging Facility, QIMR Sample Processing and Sequencing Service, and Dr. Jessica Engel for laboratory support. This work was supported by the National Health and Medical Research Council of Australia (Career Development Fellowship 1141632 to M.J.B., Ideas Grant 1181932 to M.J.B., Program Grants 1037304 and 1132975 to NMA, Senior Principal Research Fellowship 1135820 to NMA and by The Australian Centre of Research Excellence in Malaria Elimination Seed Grant to J.R.L.
Author contributions
T.C., J.L., M.J.B. designed research study; N.D., J.L., K.B., D.A., A.S.N. conducted experiments; N.D., T.C., Z.P., J.L., J.H., D.A., M.S., M.J.B. analysed data; K.P., T.W., B.B., M.G., N.A. conducted and supervised the clinical studies and sampling; N.D., T.C., J.H., D.A., M.S., M.J.B. generated figures; N.D., T.C., Z.P., J.L., J.H., D.A., M.S., M.J.B. verified underlying data; A.L., C.E., M.J.B. provided supervision for staff and students and contributed to study design, interpretation and contextualization of data; N.D., M.J.B. led manuscript preparation with feedback from all other authors. All authors have read and approved the final version of the manuscript. M.J.B. approves this version of the manuscript on behalf of TC (deceased).
Peer review
Peer review information
: Nature Communications thanks Christopher Sundling, Vanessa Amana-Bokagne, Thomas Jacobs and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Data availability
All data generated or analysed during this study are included in this article and supplementary information files or from the corresponding author upon request. The raw sequencing data and processed Cell Ranger outputs used in this study have been deposited in the NCBI data base under accession code GSE217930 https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE217930
The processed single cell RNA seq data are available in the Zenodo data base, here “annotated_Sabah_data_21Oct2022.rds” 10.5281/zenodo.6973241. All other data generated in this study are provided in Supplementary Information. Source data are provided with this paper.
Code availability
The code generated during this study is available at 10.5281/zenodo.8378626, https://github.com/MichelleBoyle/scRNAseq_malaria_2023
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Nicholas L. Dooley, Tinashe G. Chabikwa.
Deceased: Tinashe G. Chabikwa.
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-023-43181-7.
References
- 1.Organization, W. H. World malaria report 2022. (2022).
- 2.Gonçalves BP, et al. Parasite Burden and Severity of Malaria in Tanzanian Children. New Engl J. Med. 2014;370:1799–1808. doi: 10.1056/NEJMoa1303944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tessema SK, et al. Protective Immunity against Severe Malaria in Children Is Associated with a Limited Repertoire of Antibodies to Conserved PfEMP1 Variants. Cell Host Microbe. 2019;26:579–590.e5. doi: 10.1016/j.chom.2019.10.012. [DOI] [PubMed] [Google Scholar]
- 4.Doolan DL, Dobaño C, Baird JK. Acquired Immunity to Malaria. Clin. Microbiol. Rev. 2009;22:13–36. doi: 10.1128/CMR.00025-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beeson JG, et al. The RTS,S malaria vaccine: Current impact and foundation for the future. Sci. Transl. Med. 2022;14:eabo6646. doi: 10.1126/scitranslmed.abo6646. [DOI] [PubMed] [Google Scholar]
- 6.Loughland JR, et al. Profoundly Reduced CD1c+ Myeloid Dendritic Cell HLA-DR and CD86 Expression and Increased Tumor Necrosis Factor Production in Experimental Human Blood-Stage Malaria Infection. Infect. Immun. 2016;84:1403–1412. doi: 10.1128/IAI.01522-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loughland JR, et al. Transcriptional profiling and immunophenotyping show sustained activation of blood monocytes in subpatent Plasmodium falciparuminfection. Clin. Transl. Immunol. 2020;9:126–18. doi: 10.1002/cti2.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pinzon-Charry A, et al. Apoptosis and dysfunction of blood dendritic cells in patients with falciparum and vivax malariaBlood DC dysfunction in malaria. J. Exp. Med. 2013;210:1635–1646. doi: 10.1084/jem.20121972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Woodberry T, et al. Low-Level Plasmodium falciparum Blood-Stage Infection Causes Dendritic Cell Apoptosis and Dysfunction in Healthy Volunteers. J. Infect. Dis. 2012;206:333–340. doi: 10.1093/infdis/jis366. [DOI] [PubMed] [Google Scholar]
- 10.Portugal S, et al. Exposure-Dependent Control of Malaria-Induced Inflammation in Children. Plos Pathog. 2014;10:e1004079. doi: 10.1371/journal.ppat.1004079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guha R, et al. Plasmodium falciparum malaria drives epigenetic reprogramming of human monocytes toward a regulatory phenotype. Plos Pathog. 2021;17:e1009430. doi: 10.1371/journal.ppat.1009430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weinberg JB, et al. Monocyte polarization in children with falciparum malaria: relationship to nitric oxide insufficiency and disease severity. Sci. Rep. 2016;6:29151. doi: 10.1038/srep29151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moebius, J. et al. PD-1 Expression on NK Cells in Malaria-Exposed Individuals Is Associated with Diminished Natural Cytotoxicity and Enhanced Antibody-Dependent Cellular Cytotoxicity. Infect. Immun.88, e00711–19 (2020). [DOI] [PMC free article] [PubMed]
- 14.Jagannathan P, et al. Loss and dysfunction of Vδ2+ γδ T cells are associated with clinical tolerance to malaria. Sci. Transl. Med. 2014;6:251ra117-251ra117. doi: 10.1126/scitranslmed.3009793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dantzler KW, Jagannathan P. γδ T cells in antimalarial immunity: new Insights into their diverse functions in protection and tolerance. Fronteirs Immunology. 2018;9:2445. doi: 10.3389/fimmu.2018.02445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boyle MJ, et al. The Development of Plasmodium falciparum-Specific IL10 CD4 T Cells and Protection from Malaria in Children in an Area of High Malaria Transmission. Front. Immunol. 2017;8:1329. doi: 10.3389/fimmu.2017.01329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boyle MJ, et al. Effector Phenotype of Plasmodium falciparum-Specific CD4+ T Cells Is Influenced by Both Age and Transmission Intensity in Naturally Exposed Populations. J. Infect. Dis. 2015;212:416–425. doi: 10.1093/infdis/jiv054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jagannathan P, et al. IFNγ/IL-10 co-producing cells dominate the CD4 response to malaria in highly exposed children. PLoS Pathog. 2014;10:e1003864. doi: 10.1371/journal.ppat.1003864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oca MMde, et al. Type I Interferons Regulate Immune Responses in Humans with Blood-Stage Plasmodium falciparum. Infection. CellRep. 2016;17:399–412. doi: 10.1016/j.celrep.2016.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abel A, et al. Differential expression pattern of co-inhibitory molecules on CD4+ T cells in uncomplicated versus complicated malaria. Sci Rep-uk. 2018;8:4789. doi: 10.1038/s41598-018-22659-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mackroth MS, Abel A, Steeg C, Wiesch JSzur, Jacobs T. Acute Malaria Induces PD1+CTLA4+ Effector T Cells with Cell-Extrinsic Suppressor Function. Plos Pathog. 2016;12:e1005909. doi: 10.1371/journal.ppat.1005909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Edwards CL, et al. IL-10-producing Th1 cells possess a distinct molecular signature in malaria. J. Clin. Investig. 2023;133:e153733. doi: 10.1172/JCI153733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sundling, C. et al. B cell profiling in malaria reveals expansion and remodelling of CD11c+ B cell subsets. JCI insight4, e126492 (2019). [DOI] [PMC free article] [PubMed]
- 24.Weiss GE, et al. Atypical memory B cells are greatly expanded in individuals living in a malaria-endemic area. J. Immunol. 2009;183:2176–2182. doi: 10.4049/jimmunol.0901297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pérez-Mazliah D, Ndungu FM, Aye R, Langhorne J. B‐cell memory in malaria: Myths and realities. Immunol. Rev. 2019;293:57–69. doi: 10.1111/imr.12822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Portugal S, et al. Malaria-associated atypical memory B cells exhibit markedly reduced B cell receptor signaling and effector function. eLife. 2015;4:1748. doi: 10.7554/eLife.07218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sullivan RT, et al. FCRL5 Delineates Functionally Impaired Memory B Cells Associated with Plasmodium falciparum Exposure. PLoS Pathog. 2015;11:e1004894. doi: 10.1371/journal.ppat.1004894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Han X, et al. Potential Role for Regulatory B Cells as a Major Source of Interleukin-10 in Spleen from Plasmodium chabaudi-Infected Mice. Infect. Immun. 2018;86:e00016–e00018. doi: 10.1128/IAI.00016-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.He X, Xia L, Tumas KC, Wu J, Su X-Z. Type I Interferons and Malaria: A Double-Edge Sword Against a Complex Parasitic Disease. Front. Cell Infect. Mi. 2020;10:594621. doi: 10.3389/fcimb.2020.594621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tran, T. M. et al. A Molecular Signature in Blood Reveals a Role for p53 in Regulating Malaria-Induced Inflammation. Immunity 1–27 10.1016/j.immuni.2019.08.009 (2019). [DOI] [PMC free article] [PubMed]
- 31.Real E, et al. A single-cell atlas of Plasmodium falciparum transmission through the mosquito. Nat Commun. 2021;12:3196. doi: 10.1038/s41467-021-23434-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reid AJ, et al. Single-cell RNA-seq reveals hidden transcriptional variation in malaria parasites. Elife. 2018;7:e33105. doi: 10.7554/eLife.33105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Poran A, et al. Single-cell RNA sequencing reveals a signature of sexual commitment in malaria parasites. Nature. 2017;551:95–99. doi: 10.1038/nature24280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oyong DA, et al. Distinct immune responses associated with vaccination status and protection outcomes after malaria challenge. PLOS Pathog. 2023;19:e1011051. doi: 10.1371/journal.ppat.1011051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Loughland JR, et al. Plasmacytoid dendritic cells appear inactive during sub-microscopic Plasmodium falciparum blood-stage infection, yet retain their ability to respond to TLR stimulation. Sci. Rep. 2017;7:2. doi: 10.1038/s41598-017-02096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Namba K, et al. Involvement of ADAM9 in Multinucleated Giant Cell Formation of Blood Monocytes. Cell Immunol. 2001;213:104–113. doi: 10.1006/cimm.2001.1873. [DOI] [PubMed] [Google Scholar]
- 37.Wang S, et al. S100A8/A9 in Inflammation. Front. Immunol. 2018;9:1298. doi: 10.3389/fimmu.2018.01298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Reyes, M. et al. An immune-cell signature of bacterial sepsis. Nat. Med. 1–26 10.1038/s41591-020-0752-4 (2020). [DOI] [PMC free article] [PubMed]
- 39.Liu, N. et al. Single-cell analysis of COVID-19, sepsis, and HIV infection reveals hyperinflammatory and immunosuppressive signatures in monocytes. Cell Rep. 109793 10.1016/j.celrep.2021.109793 (2021). [DOI] [PMC free article] [PubMed]
- 40.Waickman AT, et al. Temporally integrated single cell RNA sequencing analysis of PBMC from experimental and natural primary human DENV-1 infections. Plos Pathog. 2021;17:e1009240. doi: 10.1371/journal.ppat.1009240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu T, Zhang L, Joo D, Sun S-C. NF-κB signaling in inflammation. Signal Transduct. Target. Ther. 2017;2:17023. doi: 10.1038/sigtrans.2017.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Arama C, et al. Interethnic Differences in Antigen-Presenting Cell Activation and TLR Responses in Malian Children during Plasmodium falciparum Malaria. Plos One. 2011;6:e18319. doi: 10.1371/journal.pone.0018319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Urban BC, et al. The Frequency of BDCA3-Positive Dendritic Cells Is Increased in the Peripheral Circulation of Kenyan Children with Severe Malaria∇. Infect. Immun. 2006;74:6700–6706. doi: 10.1128/IAI.00861-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Suscovich TJ, et al. Mapping functional humoral correlates of protection against malaria challenge following RTS,S/AS01 vaccination. Sci. Transl. Med. 2020;12:eabb4757. doi: 10.1126/scitranslmed.abb4757. [DOI] [PubMed] [Google Scholar]
- 45.Minassian, A. M. et al. Reduced blood-stage malaria growth and immune correlates in humans following RH5 vaccination. Med10.1016/j.medj.2021.03.014 (2021). [DOI] [PMC free article] [PubMed]
- 46.Tan J, et al. Functional human IgA targets a conserved site on malaria sporozoites. Sci. Transl. Med. 2021;13:eabg2344. doi: 10.1126/scitranslmed.abg2344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fernandez-Arias C, et al. Malaria Inhibits Surface Expression of Complement Receptor 1 in Monocytes/Macrophages, Causing Decreased Immune Complex Internalization. J. Immunol. 2013;190:3363–3372. doi: 10.4049/jimmunol.1103812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lautenbach MJ, et al. Systems analysis shows a role of cytophilic antibodies in shaping innate tolerance to malaria. Cell Rep. 2022;39:110709. doi: 10.1016/j.celrep.2022.110709. [DOI] [PubMed] [Google Scholar]
- 49.Roederer M, Nozzi JL, Nason MC. SPICE: Exploration and analysis of post‐cytometric complex multivariate datasets. Cytom Part A. 2011;79A:167–174. doi: 10.1002/cyto.a.21015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Korbel DS, Newman KC, Almeida CR, Davis DM, Riley EM. Heterogeneous Human NK Cell Responses to Plasmodium falciparum-Infected Erythrocytes. J. Immunol. 2005;175:7466–7473. doi: 10.4049/jimmunol.175.11.7466. [DOI] [PubMed] [Google Scholar]
- 51.Artavanis-Tsakonas K, Riley EM. Innate Immune Response to Malaria: Rapid Induction of IFN-γ from Human NK Cells by Live Plasmodium falciparum-Infected Erythrocytes. J. Immunol. 2002;169:2956–2963. doi: 10.4049/jimmunol.169.6.2956. [DOI] [PubMed] [Google Scholar]
- 52.McCall MBB, et al. Memory-like IFN-γ response by NK cells following malaria infection reveals the crucial role of T cells in NK cell activation by P. falciparum. Eur. J. Immunol. 2010;40:3472–3477. doi: 10.1002/eji.201040587. [DOI] [PubMed] [Google Scholar]
- 53.Hart GT, et al. Adaptive NK cells in people exposed to Plasmodium falciparumcorrelate with protection from malaria. J. Exp. Med. 2019;2:jem.20181681–14. doi: 10.1084/jem.20181681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Arora G, et al. NK cells inhibit Plasmodium falciparum growth in red blood cells via antibody-dependent cellular cytotoxicity. Elife. 2018;7:e36806. doi: 10.7554/eLife.36806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yang C, et al. Heterogeneity of human bone marrow and blood natural killer cells defined by single-cell transcriptome. Nat Commun. 2019;10:3931. doi: 10.1038/s41467-019-11947-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pfefferle, A. et al. A Temporal Transcriptional Map of Human Natural Killer Cell Differentiation. Biorxiv 630657 10.1101/630657 (2019).
- 57.Jiang W, Chai NR, Maric D, Bielekova B. Unexpected Role for Granzyme K in CD56bright NK Cell-Mediated Immunoregulation of Multiple Sclerosis. J. Immunol. 2011;187:781–790. doi: 10.4049/jimmunol.1100789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sague SL, Tato C, Pur E, Hunter CA. The Regulation and Activation of CD44 by Natural Killer (NK) Cells and Its Role in the Production of IFN- J. Interf Cytokine Res. 2004;24:301–309. doi: 10.1089/107999004323065093. [DOI] [PubMed] [Google Scholar]
- 59.Andrade LFde, et al. Discovery of specialized NK cell populations infiltrating human melanoma metastases. Jci Insight. 2019;4:e133103. doi: 10.1172/jci.insight.133103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.D’Orlando O, et al. Syntaxin 11 is required for NK and CD8+ T‐cell cytotoxicity and neutrophil degranulation. Eur. J. Immunol. 2013;43:194–208. doi: 10.1002/eji.201142343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ahmad F, et al. High Frequencies of Polyfunctional CD8 + NK Cells in Chronic HIV-1 Infection Are Associated with Slower Disease Progression. J. Virol. 2014;88:12397–12408. doi: 10.1128/JVI.01420-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Clemente T, et al. Proteomic and functional analysis identifies galectin-1 as a novel regulatory component of the cytotoxic granule machinery. Cell Death Dis. 2017;8:e3176. doi: 10.1038/cddis.2017.506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Loftus RM, et al. Amino acid-dependent cMyc expression is essential for NK cell metabolic and functional responses in mice. Nat. Commun. 2018;9:2341. doi: 10.1038/s41467-018-04719-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Peng H, Sun R, Tang L, Wei H, Tian Z. CD62L Is Critical for Maturation and Accumulation of Murine Hepatic NK Cells in Response to Viral Infection. J. Immunol. 2013;190:4255–4262. doi: 10.4049/jimmunol.1202395. [DOI] [PubMed] [Google Scholar]
- 65.Aranami T, Miyake S, Yamamura T. Differential Expression of CD11c by Peripheral Blood NK Cells Reflects Temporal Activity of Multiple Sclerosis. J. Immunol. 2006;177:5659–5667. doi: 10.4049/jimmunol.177.8.5659. [DOI] [PubMed] [Google Scholar]
- 66.Tsuda J, et al. Involvement of CD56brightCD11c+ Cells in IL-18–Mediated Expansion of Human γδ T Cells. J. Immunol. 2011;186:2003–2012. doi: 10.4049/jimmunol.1001919. [DOI] [PubMed] [Google Scholar]
- 67.Erokhina SA, et al. HLA‐DR‐expressing NK cells: Effective killers suspected for antigen presentation. J. Leukocyte Biol. 2021;109:327–337. doi: 10.1002/JLB.3RU0420-668RR. [DOI] [PubMed] [Google Scholar]
- 68.Turaj AH, et al. Augmentation of CD134 (OX40)-dependent NK anti-tumour activity is dependent on antibody cross-linking. Sci Rep-uk. 2018;8:2278. doi: 10.1038/s41598-018-20656-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Baessler T, et al. CD137 ligand mediates opposite effects in human and mouse NK cells and impairs NK-cell reactivity against human acute myeloid leukemia cells. Blood. 2010;115:3058–3069. doi: 10.1182/blood-2009-06-227934. [DOI] [PubMed] [Google Scholar]
- 70.Liu B, et al. Glucocorticoid-induced Tumor Necrosis Factor Receptor Negatively Regulates Activation of Human Primary Natural Killer (NK) Cells by Blocking Proliferative Signals and Increasing NK Cell Apoptosis*. J. Biol. Chem. 2008;283:8202–8210. doi: 10.1074/jbc.M708944200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Narayanan, S. et al. LAG3 is a Central Regulator of NK Cell Cytokine Production. Biorxiv10.1101/2020.01.31.928200 (2020).
- 72.Ndhlovu LC, et al. Tim-3 marks human natural killer cell maturation and suppresses cell-mediated cytotoxicity. Blood. 2012;119:3734–3743. doi: 10.1182/blood-2011-11-392951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lu T, et al. Cbl-b Is Upregulated and Plays a Negative Role in Activated Human NK Cells. J. Immunol. 2021;206:677–685. doi: 10.4049/jimmunol.2000177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lee AJ, et al. Type I Interferon Receptor on NK Cells Negatively Regulates Interferon-γ Production. Front. Immunol. 2019;10:1261. doi: 10.3389/fimmu.2019.01261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dantzler KW, Jagannathan P. γδ T Cells in Antimalarial Immunity: New Insights Into Their Diverse Functions in Protection and Tolerance. Front. Immunol. 2018;9:2445. doi: 10.3389/fimmu.2018.02445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Junqueira, C. et al. γδ T cells suppress Plasmodium falciparum blood-stage infection by direct killing and phagocytosis. Nat. Immunol. 1–11 10.1038/s41590-020-00847-4 (2021). [DOI] [PMC free article] [PubMed]
- 77.Howard J, et al. The Antigen-Presenting Potential of Vγ9Vδ2 T Cells During Plasmodium falciparum Blood-Stage Infection. J. Infect. Dis. 2017;215:1569–1579. doi: 10.1093/infdis/jix149. [DOI] [PubMed] [Google Scholar]
- 78.Jagannathan P, et al. Vδ2+ T cell response to malaria correlates with protection from infection but is attenuated with repeated exposure. Sci. Rep. 2017;7:11487. doi: 10.1038/s41598-017-10624-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Farrington LA, et al. Opsonized antigen activates Vδ2+ T cells via CD16/FCγRIIIa in individuals with chronic malaria exposure. Plos Pathog. 2020;16:e1008997. doi: 10.1371/journal.ppat.1008997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tan, L. et al. A fetal wave of human type 3 effector γδ cells with restricted TCR diversity persists into adulthood. Sci. Immunol.6, eabf0125 (2021). [DOI] [PubMed]
- 81.Takeuchi A, et al. CRTAM determines the CD4+ cytotoxic T lymphocyte lineage. J. Exp. Med. 2016;213:123–138. doi: 10.1084/jem.20150519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Damgaard RB, et al. The Deubiquitinase OTULIN Is an Essential Negative Regulator of Inflammation and Autoimmunity. Cell. 2016;166:1215–1230.e20. doi: 10.1016/j.cell.2016.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ortutay Z, et al. Identification of Novel Genetic Regulatory Region for Proprotein Convertase FURIN and Interferon Gamma in T Cells. Front. Immunol. 2021;12:630389. doi: 10.3389/fimmu.2021.630389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zeng J, Yang X, Yang L, Li W, Zheng Y. Thymosin β10 promotes tumor-associated macrophages M2 conversion and proliferation via the PI3K/Akt pathway in lung adenocarcinoma. Respir. Res. 2020;21:328. doi: 10.1186/s12931-020-01587-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Suzuki T, et al. Loss of hypoxia inducible factor‐1α aggravates γδ T‐cell‐mediated inflammation during acetaminophen‐induced liver injury. Hepatol. Commun. 2018;2:571–581. doi: 10.1002/hep4.1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Quigley M, et al. Transcriptional analysis of HIV-specific CD8+ T cells shows that PD-1 inhibits T cell function by upregulating BATF. Nat. Med. 2010;16:1147–1151. doi: 10.1038/nm.2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hsu H, et al. Age-related changes in PD-1 expression coincide with increased cytotoxic potential in Vδ2 T cells during infancy. Cell Immunol. 2020;359:104244. doi: 10.1016/j.cellimm.2020.104244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hsu H, et al. Prolonged PD1 Expression on Neonatal Vδ2 Lymphocytes Dampens Proinflammatory Responses: Role of Epigenetic Regulation. J. Immunol. 2016;197:1884–1892. doi: 10.4049/jimmunol.1600284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Schofield L, et al. Synergistic effect of IL-12 and IL-18 induces TIM3 regulation of γδ T cell function and decreases the risk of clinical malaria in children living in Papua New Guinea. Bmc Med. 2017;15:114. doi: 10.1186/s12916-017-0883-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kunzmann V, Kretzschmar E, Herrmann T, Wilhelm M. Polyinosinic‐polycytidylic acid‐mediated stimulation of human γδ T cells via CD11c+ dendritic cell‐derived type I interferons. Immunology. 2004;112:369–377. doi: 10.1111/j.1365-2567.2004.01908.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kurup SP, Butler NS, Harty JT. T cell-mediated immunity to malaria. Nat. Rev. Immunol. 2019;19:457–471. doi: 10.1038/s41577-019-0158-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Locci M, et al. Human Circulating PD-1+CXCR3-CXCR5+ Memory Tfh Cells Are Highly Functional and Correlate with Broadly Neutralizing HIV Antibody Responses. Immunity. 2013;39:758–769. doi: 10.1016/j.immuni.2013.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Radens CM, Blake D, Jewell P, Barash Y, Lynch KW. Meta-analysis of transcriptomic variation in T-cell populations reveals both variable and consistent signatures of gene expression and splicing. RNA. 2020;26:1320–1333. doi: 10.1261/rna.075929.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gallagher MP, et al. Hierarchy of signaling thresholds downstream of the T cell receptor and the Tec kinase ITK. Proc Natl Acad. Sci. 2021;118:e2025825118. doi: 10.1073/pnas.2025825118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Roncarolo MG, Gregori S, Bacchetta R, Battaglia M, Gagliani N. The Biology of T Regulatory Type 1 Cells and Their Therapeutic Application in Immune-Mediated Diseases. Immunity. 2018;49:1004–1019. doi: 10.1016/j.immuni.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 96.Anderson AC, Joller N, Kuchroo VK. Lag-3, Tim-3, and TIGIT: Co-inhibitory Receptors with Specialized Functions in Immune Regulation. Immunity. 2016;44:989–1004. doi: 10.1016/j.immuni.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yang S, Wang J, Brand DD, Zheng SG. Role of TNF–TNF Receptor 2 Signal in Regulatory T Cells and Its Therapeutic Implications. Front. Immunol. 2018;9:784. doi: 10.3389/fimmu.2018.00784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.So T, Lee S-W, Croft M. Immune regulation and control of regulatory T cells by OX40 and 4-1BB. Cytokine Growth F R. 2008;19:253–262. doi: 10.1016/j.cytogfr.2008.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zander RA, et al. Th1-like Plasmodium-Specific Memory CD4+ T Cells Support Humoral Immunity. Cell Rep. 2017;21:1839–1852. doi: 10.1016/j.celrep.2017.10.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ronchetti S, et al. Glucocorticoid-Induced Tumour Necrosis Factor Receptor-Related Protein: A Key Marker of Functional Regulatory T Cells. J. Immunol. Res. 2015;2015:171520. doi: 10.1155/2015/171520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Patterson SJ, et al. T regulatory cell chemokine production mediates pathogenic T cell attraction and suppression. J. Clin. Investig. 2016;126:1039–1051. doi: 10.1172/JCI83987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ridley ML, et al. IKZF3/Aiolos Is Associated with but Not Sufficient for the Expression of IL-10 by CD4+ T Cells. J. Immunol. 2020;204:ji1901283. doi: 10.4049/jimmunol.1901283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Schmidl C, et al. The enhancer and promoter landscape of human regulatory and conventional T-cell subpopulations. Blood. 2014;123:e68–e78. doi: 10.1182/blood-2013-02-486944. [DOI] [PubMed] [Google Scholar]
- 104.Meiler F, et al. In vivo switch to IL-10–secreting T regulatory cells in high dose allergen exposure. J. Exp. Med. 2008;205:2887–2898. doi: 10.1084/jem.20080193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Gabryšová L, et al. c-Maf controls immune responses by regulating disease-specific gene networks and repressing IL-2 in CD4+ T cells. Nat. Immunol. 2018;19:497–507. doi: 10.1038/s41590-018-0083-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Oca MMde, et al. Blimp-1-Dependent IL-10 Production by Tr1 Cells Regulates TNF-Mediated Tissue Pathology. Plos Pathog. 2016;12:e1005398. doi: 10.1371/journal.ppat.1005398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wang, Y. et al. STING activation promotes autologous type I interferon-dependent development of type 1 regulatory T cells during malaria. bioRxiv10.1101/2022.09.04.506109 (2022). [DOI] [PMC free article] [PubMed]
- 108.Schraml BU, et al. The AP-1 transcription factor Batf controls TH17 differentiation. Nature. 2009;460:405–409. doi: 10.1038/nature08114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ise W, et al. The transcription factor BATF controls the global regulators of class-switch recombination in both B cells and T cells. Nat. Immunol. 2011;12:536–543. doi: 10.1038/ni.2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Soon MSF, Nalubega M, Boyle MJ. T-follicular helper cells in malaria infection and roles in antibody induction. Oxf Open Immunol. 2021;2:iqab008. doi: 10.1093/oxfimm/iqab008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Oyong DA, et al. Adults with Plasmodium falciparum malaria have higher magnitude and quality of circulating T-follicular helper cells compared to children. Ebiomedicine. 2022;75:103784. doi: 10.1016/j.ebiom.2021.103784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chan J-A, et al. Th2-like T Follicular Helper Cells Promote Functional Antibody Production during Plasmodium falciparum Infection. Cell Rep. Med. 2020;1:100157. doi: 10.1016/j.xcrm.2020.100157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Obeng-Adjei N, et al. Circulating Th1-Cell-type Tfh Cells that Exhibit Impaired B Cell Help Are Preferentially Activated during Acute Malaria in Children. CellReports. 2015;13:425–439. doi: 10.1016/j.celrep.2015.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kim CJ, et al. The Transcription Factor Ets1 Suppresses T Follicular Helper Type 2 Cell Differentiation to Halt the Onset of Systemic Lupus Erythematosus. Immunity. 2018;49:1034–1048.e8. doi: 10.1016/j.immuni.2018.10.012. [DOI] [PubMed] [Google Scholar]
- 115.Pham D, et al. Batf Pioneers the Reorganization of Chromatin in Developing Effector T Cells via Ets1-Dependent Recruitment of Ctcf. Cell Rep. 2019;29:1203–1220.e7. doi: 10.1016/j.celrep.2019.09.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Chinen T, et al. An essential role for the IL-2 receptor in Treg cell function. Nat. Immunol. 2016;17:1322–1333. doi: 10.1038/ni.3540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Consortium, Co.-19 M. B. At. (COMBAT et al. A blood atlas of COVID-19 defines hallmarks of disease severity and specificity. Cell. 2022;185:916–938.e58. doi: 10.1016/j.cell.2022.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kaminski L-C, et al. Cytotoxic T Cell-Derived Granzyme B Is Increased in Severe Plasmodium Falciparum Malaria. Front. Immunol. 2019;10:2917. doi: 10.3389/fimmu.2019.02917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Noble A, Giorgini A, Leggat JA. Cytokine-induced IL-10–secreting CD8 T cells represent a phenotypically distinct suppressor T-cell lineage. Blood. 2006;107:4475–4483. doi: 10.1182/blood-2005-10-3994. [DOI] [PubMed] [Google Scholar]
- 120.Cohen S, McGregor IA, Carrington S. Gamma-globulin and acquired immunity to human malaria. Nature. 1961;192:733–737. doi: 10.1038/192733a0. [DOI] [PubMed] [Google Scholar]
- 121.Sutton HJ, et al. Atypical B cells are part of an alternative lineage of B cells that participates in responses to vaccination and infection in humans. Cell Rep. 2021;34:108684. doi: 10.1016/j.celrep.2020.108684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Kim CC, Baccarella AM, Bayat A, Pepper M, Fontana MF. FCRL5+ Memory B Cells Exhibit Robust Recall Responses. CellReports. 2019;27:1446–1460.e4. doi: 10.1016/j.celrep.2019.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Hopp CS, et al. Atypical B cells up-regulate costimulatory molecules during malaria and secrete antibodies with T follicular helper cell support. Sci. Immunol. 2022;7:eabn1250. doi: 10.1126/sciimmunol.abn1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Horns F, Dekker CL, Quake SR. Memory B Cell Activation, Broad Anti-influenza Antibodies, and Bystander Activation Revealed by Single-Cell Transcriptomics. CellReports. 2020;30:905–913.e6. doi: 10.1016/j.celrep.2019.12.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ellebedy AH, et al. Defining antigen-specific plasmablast and memory B cell subsets in human blood after viral infection or vaccination. Nat. Immunol. 2016;17:1226–1234. doi: 10.1038/ni.3533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Schmiedel BJ, et al. Impact of Genetic Polymorphisms on Human Immune Cell Gene Expression. Cell. 2018;175:1701–1715.e16. doi: 10.1016/j.cell.2018.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Monaco G, et al. RNA-Seq Signatures Normalized by mRNA Abundance Allow Absolute Deconvolution of Human Immune Cell Types. Cell Rep. 2019;26:1627–1640.e7. doi: 10.1016/j.celrep.2019.01.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Sullivan RT, et al. B cell sub-types following acute malaria and associations with clinical immunity. Malaria J. 2016;15:139. doi: 10.1186/s12936-016-1190-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Nduati E, et al. The Plasma Concentration of the B Cell Activating Factor Is Increased in Children With Acute Malaria. J. Infect. Dis. 2011;204:962–970. doi: 10.1093/infdis/jir438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Vijay R, et al. Infection-induced plasmablasts are a nutrient sink that impairs humoral immunity to malaria. Nat. Immunol. 2020;21:790–801. doi: 10.1038/s41590-020-0678-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Jellusova J. Metabolic control of B cell immune responses. Curr. Opin. Immunol. 2020;63:21–28. doi: 10.1016/j.coi.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 132.Wu N, et al. AMPK-Dependent Degradation of TXNIP upon Energy Stress Leads to Enhanced Glucose Uptake via GLUT1. Mol. Cell. 2013;49:1167–1175. doi: 10.1016/j.molcel.2013.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Patwari P, et al. Thioredoxin-independent Regulation of Metabolism by the α-Arrestin Proteins*. J. Biol. Chem. 2009;284:24996–25003. doi: 10.1074/jbc.M109.018093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Medgyesi D, et al. The protein tyrosine phosphatase PTP1B is a negative regulator of CD40 and BAFF-R signaling and controls B cell autoimmunity. J. Exp. Med. 2014;211:427–440. doi: 10.1084/jem.20131196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Ono T, et al. Inhibition of Nuclear Factor-κB-mediated Transcription by Association with the Amino-terminal Enhancer of Split, a Groucho-related Protein Lacking WD40 Repeats*. J. Biol. Chem. 2000;275:4383–4390. doi: 10.1074/jbc.275.6.4383. [DOI] [PubMed] [Google Scholar]
- 136.Sasaki Y, Iwai K. B Cell Receptor Signaling. Curr. Top Microbiol. 2015;393:177–209. doi: 10.1007/82_2015_479. [DOI] [PubMed] [Google Scholar]
- 137.Meng X, et al. Hypoxia-inducible factor-1α is a critical transcription factor for IL-10-producing B cells in autoimmune disease. Nat. Commun. 2018;9:251. doi: 10.1038/s41467-017-02683-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Glass MC, et al. Human IL-10-producing B cells have diverse states that are induced from multiple B cell subsets. Cell Rep. 2022;39:110728. doi: 10.1016/j.celrep.2022.110728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Liu Y, et al. Role of IL‐10‐producing regulatory B cells in control of cerebral malaria in Plasmodium berghei infected mice. Eur. J. Immunol. 2013;43:2907–2918. doi: 10.1002/eji.201343512. [DOI] [PubMed] [Google Scholar]
- 140.Zhu L, et al. Single-Cell Sequencing of Peripheral Mononuclear Cells Reveals Distinct Immune Response Landscapes of COVID-19 and Influenza Patients. Immunity. 2020;53:685–696.e3. doi: 10.1016/j.immuni.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Kazer SW, et al. Integrated single-cell analysis of multicellular immune dynamics during hyperacute HIV-1 infection. Nat. Med. 2020;26:511–518. doi: 10.1038/s41591-020-0799-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Reyes M, et al. Plasma from patients with bacterial sepsis or severe COVID-19 induces suppressive myeloid cell production from hematopoietic progenitors in vitro. Sci. Transl. Med. 2021;13:eabe9599. doi: 10.1126/scitranslmed.abe9599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Nahrendorf W, Ivens A, Spence PJ. Inducible mechanisms of disease tolerance provide an alternative strategy of acquired immunity to malaria. Elife. 2021;10:e63838. doi: 10.7554/eLife.63838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Church J, Maitland K. Invasive bacterial co-infection in African children with Plasmodium falciparum malaria: a systematic review. BMC Med. 2014;12:31. doi: 10.1186/1741-7015-12-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Attanasio J, Wherry EJ. Costimulatory and Coinhibitory Receptor Pathways in Infectious Disease. Immunity. 2016;44:1052–1068. doi: 10.1016/j.immuni.2016.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Ty M, et al. Malaria-driven expansion of adaptive-like functional CD56-negative NK cells correlates with clinical immunity to malaria. Sci. Transl. Med. 2023;15:eadd9012. doi: 10.1126/scitranslmed.add9012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Rutishauser T, et al. Activation of TCR Vδ1+ and Vδ1−Vδ2− γδ T Cells upon Controlled Infection with Plasmodium falciparum in Tanzanian Volunteers. J. Immunol. 2020;204:180–191. doi: 10.4049/jimmunol.1900669. [DOI] [PubMed] [Google Scholar]
- 148.Borstel Avon, et al. Repeated Plasmodium falciparum infection in humans drives the clonal expansion of an adaptive γδ T cell repertoire. Sci. Transl. Med. 2021;13:eabe7430. doi: 10.1126/scitranslmed.abe7430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Walther M, et al. Distinct Roles for FOXP3+ and FOXP3− CD4+ T Cells in Regulating Cellular Immunity to Uncomplicated and Severe Plasmodium falciparum Malaria. Plos Pathog. 2009;5:e1000364. doi: 10.1371/journal.ppat.1000364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Guthmiller JJ, Graham AC, Zander RA, Pope RL, Butler NS. Cutting Edge: IL-10 Is Essential for the Generation of Germinal Center B Cell Responses and Anti-Plasmodium Humoral Immunity. J. Immunol. 2017;198:617–622. doi: 10.4049/jimmunol.1601762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Clemente-Casares X, et al. Expanding antigen-specific regulatory networks to treat autoimmunity. Nature. 2016;530:434–440. doi: 10.1038/nature16962. [DOI] [PubMed] [Google Scholar]
- 152.González-Navajas JM, Lee J, David M, Raz E. Immunomodulatory functions of type I interferons. Nat. Rev. Immunol. 2012;12:125–135. doi: 10.1038/nri3133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Silva-Barrios S, Stäger S. Protozoan Parasites and Type I IFNs. Front. Immunol. 2017;8:14. doi: 10.3389/fimmu.2017.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Obieglo K, et al. Type I interferons provide additive signals for murine regulatory B cell induction by Schistosoma mansoni eggs. Eur. J. Immunol. 2019;49:1226–1234. doi: 10.1002/eji.201847858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Chughlay MF, et al. Safety, Tolerability, Pharmacokinetics, and Pharmacodynamics of Coadministered Ruxolitinib and Artemether-Lumefantrine in Healthy Adults. Antimicrob. Agents Ch. 2021;66:e01584–21. doi: 10.1128/AAC.01584-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Kumar R, Loughland JR, Ng SS, Boyle MJ, Engwerda CR. The regulation of CD4+ T cells during malaria. Immunol. Rev. 2020;293:70–87. doi: 10.1111/imr.12804. [DOI] [PubMed] [Google Scholar]
- 157.Loiseau C, et al. A novel population of memory‐activated natural killer cells associated with low parasitaemia in Plasmodium falciparum‐exposed sickle‐cell trait children. Clin. Transl. Immunol. 2020;9:270–18. doi: 10.1002/cti2.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.William T, et al. Increasing incidence of Plasmodium knowlesi malaria following control of P. falciparum and P. vivax Malaria in Sabah, Malaysia. PLoS Negl. Trop. Dis. 2013;7:e2026. doi: 10.1371/journal.pntd.0002026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Grigg MJ, et al. Artemether-Lumefantrine Versus Chloroquine for the Treatment of Uncomplicated Plasmodium knowlesi Malaria: An Open-Label Randomized Controlled Trial CAN KNOW. Clin. Infect. Dis. 2018;66:229–236. doi: 10.1093/cid/cix779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Grigg MJ, et al. Plasmodium falciparum artemisinin resistance monitoring in Sabah, Malaysia: in vivo therapeutic efficacy and kelch13 molecular marker surveillance. Malaria J. 2018;17:463. doi: 10.1186/s12936-018-2593-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Grigg MJ, et al. Age-Related Clinical Spectrum of Plasmodium knowlesi Malaria and Predictors of Severity. Clin. Infect. Dis. 2018;67:350–359. doi: 10.1093/cid/ciy065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Barber BE, et al. A prospective comparative study of knowlesi, falciparum, and vivax malaria in Sabah, Malaysia: high proportion with severe disease from Plasmodium knowlesi and Plasmodium vivax but no mortality with early referral and artesunate therapy. Clin. Infect. Dis. 2013;56:383–397. doi: 10.1093/cid/cis902. [DOI] [PubMed] [Google Scholar]
- 163.Hao, Y. et al. Integrated analysis of multimodal single-cell data. Cell10.1016/j.cell.2021.04.048 (2021). [DOI] [PMC free article] [PubMed]
- 164.Subramanian A, et al. Gene set enrichment analysis: A knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl Acad Sci. 2005;102:15545–15550. doi: 10.1073/pnas.0506580102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Mootha VK, et al. PGC-1α-responsive genes involved in oxidative phosphorylation are coordinately downregulated in human diabetes. Nat. Genet. 2003;34:267–273. doi: 10.1038/ng1180. [DOI] [PubMed] [Google Scholar]
- 166.Heinz S, et al. Simple Combinations of Lineage-Determining Transcription Factors Prime cis-Regulatory Elements Required for Macrophage and B Cell Identities. Mol Cell. 2010;38:576–589. doi: 10.1016/j.molcel.2010.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Conway JR, Lex A, Gehlenborg N. UpSetR: an R package for the visualization of intersecting sets and their properties. Bioinformatics. 2017;33:2938–2940. doi: 10.1093/bioinformatics/btx364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Ong S-M, et al. A Novel, Five-Marker Alternative to CD16–CD14 Gating to Identify the Three Human Monocyte Subsets. Front. Immunol. 2019;10:1761. doi: 10.3389/fimmu.2019.01761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Wilkinson L. ggplot2: Elegant Graphics for Data Analysis by WICKHAM, H. Biometrics. 2011;67:678–679. doi: 10.1111/j.1541-0420.2011.01616.x. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of Additional Supplementary Files
Data Availability Statement
All data generated or analysed during this study are included in this article and supplementary information files or from the corresponding author upon request. The raw sequencing data and processed Cell Ranger outputs used in this study have been deposited in the NCBI data base under accession code GSE217930 https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE217930
The processed single cell RNA seq data are available in the Zenodo data base, here “annotated_Sabah_data_21Oct2022.rds” 10.5281/zenodo.6973241. All other data generated in this study are provided in Supplementary Information. Source data are provided with this paper.
The code generated during this study is available at 10.5281/zenodo.8378626, https://github.com/MichelleBoyle/scRNAseq_malaria_2023