Summary
Background
High temperatures and heatwaves are occurring more frequently and lasting longer because of climate change. A synthesis of existing evidence of heat-related health impacts in the Western Pacific Region (WPR) is lacking. This review addresses this gap.
Methods
The Scopus and PubMed databases were searched for reviews about heat impacts on mortality, cardiovascular morbidity, respiratory morbidity, dehydration and heat stroke, adverse birth outcomes, and sleep disturbance. The last search was conducted in February 2023 and only publications written in English were included. Primary studies and reviews that did not include specific WPR data were excluded. Data were extracted from 29 reviews.
Findings
There is strong evidence of heat-related mortality in the WPR, with the evidence concentrating on high-income countries and China. Associations between heat and cardiovascular or respiratory morbidity are not robust. There is evidence of heat-related dehydration and stroke, and preterm and still births in high-income countries in the WPR. Some evidence of sleep disturbance from heat is found for Australia, Japan and China.
Interpretation
Mortality is by far the most studied and robust health outcome of heat. Future research should focus on morbidity, and lower income countries in continental Asia and Pacific Island States, where there is little review-level evidence.
Funding
Funded by the World Health Organization WPR Office.
Keywords: Heat impacts, Mortality, Morbidity, Western Pacific, Climate change
Introduction
Average temperatures and extreme heatwaves have increased in Asia,1 Pacific Small Islands,2 and Australasia3 because of human induced climate change. These trends will continue and diverge in the coming decades depending on greenhouse gas emissions. Heat affects human health and wellbeing, and puts a strain on health and care systems globally.4
Human exposure to heat can result in mortality through multiple physiological pathways, including increased blood flow to the skin, reduced blood flow to other organs, and cell damage.5 It can also increase heart rate, blood viscosity and cholesterol levels, enhancing the risk of cardiovascular dysfunctions such as ischemic stroke and heart disease.6,7 High temperatures and increased sunshine elevate the concentration of particulate matter (PM), surface ozone, sulphate aerosols and other air pollutants,8 which can have an inflammatory effect on the airways of susceptible individuals and increase respiratory illnesses.9 Longer and earlier pollination seasons in a warming climate increases pollen sensitization rate and allergic symptom duration.10
Under conditions of heat stress, increased sweat production can lead to dehydration if water is not adequately replenished in the body. Dehydration and hyperthermia leading to electrolyte and water imbalance place stress on the kidneys.4,11 The impact of heat on dehydration may be increased where individuals engage in moderate to high strenuous activity, such as manual labour in agriculture commonly practiced in low and middle income countries.12
When the thermoregulatory capacity of the human body is exceeded, the core body temperature may reach or exceed 40 °C and central nervous systems complications may occur.13 This is the definition of a heat stroke, which is a medical emergency. Potential outcomes of a heat stroke include organ dysfunction and death,4,13,14 and persisting neurological deficits.13 For pregnant women who have a compromised ability to thermoregulate because of increased core body temperature and decreased body area-to-mass ratio for heat loss,15,16 fetal development can be at risk.17 Preterm birth (birth before 37 weeks of gestation), stillbirth, and low birth weight (live births that weigh below 2500 g) are adverse birth outcomes that have been associated with heat in the literature.15
Furthermore, night-time heat can decrease thermal comfort in homes, reducing people's ability to relieve from day-time heat load and disrupting sleep. The urban heat island effect, a phenomenon where urban areas are warmer than surrounding sub-urban or rural areas, is often greater at night, contributing to additional night-time heat to urban inhabitants.18
While global19,20 and regional21 reports are available in the context of heat and health, no systematic review designed for the World Health Organization (WHO) Western Pacific Region (WPR) exists in the literature. Such a review complements the global overview of evidence contained in the Intergovernmental Panel on Climate Change (IPCC) 6th Assessment Report20 by providing more specific indications of adverse health outcomes likely to be found in the WPR, which contains a large and diverse group of countries. Assessing the current state of review level evidence in an umbrella review gives us a great scope to capture the outcomes and geographical diversity in the WPR. It also gives the most consolidated view of evidence, giving great confidence in the findings for informing regional and national decision making and identifying key evidence gaps and research priorities for the WPR and its sub-regions.
This umbrella review is the first consolidated synthesis on heat and health in the WPR and provides a clear indication of the strength of evidence across the region rather in specific countries. Here, we answer the question “How do high daytime and night-time temperatures affect human health in the WPR?” based on published systematic and literature reviews. Six direct heat-related health outcomes are examined: mortality, cardiovascular morbidity, respiratory morbidity, dehydration and heat stroke, adverse birth outcomes, and sleep disturbance.
Search strategy and selection criteria
This umbrella review adopted methods based on those described in the Cochrane Handbook for Systematic Reviews of Interventions.22 Based on the selected health outcomes, search terms were developed for the Scopus and PubMed databases (Supplementary Materials). Searching additional databases was deemed unnecessary because after the Scopus search, only three additional reviews resulted from the PubMed search. Results were limited to systematic reviews, scoping reviews or meta-analyses with full-text available in English. No restrictions were placed on the date of publication. The last search was conducted in February 2023.
Reviews whose title or abstract indicated that they did not include heat as the environmental exposure, reviews that did not associate the selected health outcomes with heat, reviews that were about animals or plants, reviews that focused only on policy or interventions, and reviews that had a geographical focus outside of the WPR, were excluded. After applying the above exclusion criteria to titles and abstracts, full-text screening was carried out. A review was included if it had clear inclusion and exclusion criteria, described its search strategy including search terms, and contained specific information about any of the selected heat-related health outcomes in any of the WPR countries (see Supplementary Materials for detailed eligibility criteria).
Title, abstract and full-text screening were done by two authors (Lo and Vosper) separately. Title and abstract screening were carried out by both authors on search results on the databases. Reviews that passed this stage were downloaded by Lo to Mendeley Reference Manager under six folders, one for each included health outcome, where she then did full-text screening. Vosper used an Excel spreadsheet to manage her list of screened reviews and did full-text screening online. The inter-rater reliability, represented by percentage agreement, was 78% after full text screening. Six conflicts over inclusion arose, and they were resolved in a meeting between the two authors where each review and its justification for inclusion/exclusion was discussed. Specific data for WPR countries were extracted from the included reviews. No additional analysis was performed on the data. We cite the reviews along with the primary studies from which data were extracted in the reference list.
Additional climate change and health reports relevant for the heat-related health outcomes included in this review were included manually. This was based on the lead authors' knowledge of the literature.
With guidance from the WHO WPR Office, regions in the WPR are grouped into (1) high-income countries (HICs), (2) Pacific Island States (PIs), (3) least developed countries and low- and middle-income countries in continental Asia (LDC/LMIC Continental Asia) and (4) upper middle-income countries in continental Asia (UMIC Continental Asia) (Table 1). The quality of evidence for each included heat-related health outcome in each WPR country category was assessed by applying a modified form of the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) tool.23 A score of 4 indicates high quality, 3 indicates moderate quality, 2 indicates low quality, and 1 indicates very low quality. The following GRADE assessment process was used. First, a GRADE score of 4 was given. Then, 1 point was deducted for each of these reasons: (i) study limitations (risk of bias), (ii) indirectness of evidence, (iii) inconsistency of results, (iv) imprecision, and (v) publication bias. A GRADE score was not given where no reviews were found for a certain health outcome in a WPR country category.
Table 1.
Disaggregation of countries or regions within countries based on their geographical and/or economic status.
| HICs | Pacific Island states (LDCs, UMICs, HICs) | Continental Asia (LDCs & LMICs) | Continental Asia (UMICs) |
|---|---|---|---|
| Australia Brunei Darussalam Cook Islands French Polynesia Guam Macau Nauru (If remains HIC) New Caledonia New Zealand N Mariana Islands Japan Palau Pitcairn Republic of Korea Singapore |
Fiji (UMIC) Kiribati (LDC) Marshall Islands (UMIC) Micronesia (UMIC) Niue (HIC)a Papua New Guinea (LMIC) Solomon Islands (LDC) Samoa (LMIC) Tokelau (LMIC) Tuvalu (LDC) Vanuatu (LMIC) Wallis & Futuna (HIC)b |
Cambodia (LDC) Lao PDR (LDC) Mongolia (LMIC) Philippines (LMIC) Vietnam (LMIC) |
China Malaysia |
Niue is a self-governing territory within the realm of New Zealand with gross domestic product (GDP) per capita and living standards equivalent to a high-income country.
Wallis & Futuna is a French collectivity and is considered high income.
Role of funding source
The funder had no role in study design, data extraction or writing of this review.
Results
A total of 29 reviews are included in this study (Fig. 1). This consists of 26 reviews resulting from the Scopus and PubMed searches and 3 reports added through authors judgement (Table S1, Supplementary Materials). The three reports are included because they are authoritative climate and health reports relevant for the WPR from the IPCC, Lancet Countdown, and United Nations Children's Fund (UNICEF).
Fig. 1.
Identification, screening, and inclusion of reviews from database searches, and additional reports identified through authors judgement. The number of excluded reviews and the reason for exclusion are detailed at each stage.
Table 2 provides brief information extracted from each included review or report, collective referred to as ‘included reviews' hereafter for simplicity, grouped by health outcomes. A summary of findings for each health outcome in the WPR country categories is tabulated in Table 3, along with the number of reviews and judgement on their quality. The following sections present the extracted information for each selected health outcome.
Table 2.
Brief information about the included reviews, including the number of studies therein, their geographical coverage, and the information extracted for specific WPR sub-regions.
| Review | Citation | No. of studies | Coverage | Extracted information | Extracted region(s) |
|---|---|---|---|---|---|
| Mortality | |||||
| Campbell et al., 2018 | 24 | 188 | Global | Older people are more susceptible to extreme heat-related death in Australia and China. Urban heat islands in China increase the risk of impact. | HICs UMIC Continental Asia |
| Hansen et al., 2011 | 25 | 28 | Global | Older people with poor health are at a higher risk of heat-related mortality in Australia. | HICs |
| Mason et al., 2022 | 26 | 45 | Australia | The most common risk factor for heatwave mortality across Australia is advanced age (above 60 years old). | HICs |
| Lakhoo et al., 2022 | 27 | 26 | Global | Increased risk of infant (0–1 year old) mortality per degree increase in temperature. | HICs |
| Xu et al., 2014 | 28 | 12 | Global | Larger heatwave mortality in children in Australia and South Korea, compared with other ages. No evidence of this in some other heatwaves in Korea and China. | HICs UMIC Continental Asia |
| Chan et al., 2019 | 29 | 196 | China | Stronger heat effect on mortality in urban areas in China. Excess heat-related deaths are associated with cardiovascular and respiratory diseases, and diabetes. | UMIC Continental Asia |
| Cheng et al., 2019b | 30 | 97 | Global | Fractions of all mortality attributable to heat in Australia, Japan, South Korea, and China. | HICs UMIC Continental Asia |
| Cissé et al., 2022a | 20 | 1659 | Global | High death tolls and hospitalisations in the 2018 heatwave in Japan. | HICs |
| Chae and Kim, 2020 | 31 | 43 | Korea | Numbers of heat-related deaths in South Korea in the 2016 and 2018 heatwaves. | HICs |
| Luo et al., 2019 | 32 | 45 | China | Increased rate of non-accidental mortality per degree increase in temperature above threshold. | UMIC Continental Asia |
| Cai et al., 2021a | 21 | 103 | China | An increasing trend in heat-related mortality in China, with provinces in east and south-central China being most affected. Heat deaths can be attributed to exacerbation of cardiovascular and respiratory diseases. | UMIC Continental Asia |
| Ma et al., 2020 | 33 | 175 | China | Percentage increases in respiratory mortality and chronic obstructive pulmonary disease (COPD) mortality per degree increase in temperature in China. | UMIC Continental Asia |
| Cardiovascular morbidity | |||||
| Ma et al., 2020 | 33 | 175 | China | Positive and significant associations between heat exposure and cardiovascular illnesses in some cities in China. | UMIC Continental Asia |
| Cheng et al., 2019a | 6 | 54 | Global | Non-significant associations between heatwaves and cardiovascular morbidity in Australia, South Korea, and Vietnam. Positive and significant associations for China. | HICs LDC/LMIC Continental Asia UMIC Continental Asia |
| Phung et al., 2016 | 30 | 64 | Global | Inconsistent heat-cardiovascular health associations in Australia and Japan. Increased risk of acute myocardial infarction in South Korea and cardiovascular hospital admissions in Vietnam, per degree increase in temperature. Protective effect of heat on ischemic stroke hospitalisation in China. | HICs LDC/LMIC Continental Asia UMIC Continental Asia |
| Sun et al., 2018 | 34 | 30 | Global | Increased risk of acute myocardial infarction per degree increase in temperature above a threshold in South Korea. | HICs |
| Lian et al., 2015 | 35 | 20 | Global | Protective or non-significant effect of heat on stroke morbidity in China. | UMIC Continental Asia |
| Respiratory morbidity | |||||
| Mason et al., 2022 | 26 | 45 | Australia | Increases in respiratory-related emergency department presentations and ambulance call outs associated with heatwaves in Australia. | HICs |
| Cheng et al., 2019a | 6 | 54 | Global | Non-significant associations between heatwaves and respiratory morbidity in Australia, Vietnam, and China. Positive associations in South Korea. | HICs LDC/LMIC Continental Asia UMIC Continental Asia |
| Uibel et al., 2022 | 36 | 24 | High income countries | Excess respiratory-related ambulance call outs in Australia during the 2008 and 2009 heatwaves. | HICs |
| Grigorieva and Lukyanets, 2021 | 8 | 40 | Global | Increased risk of acute bronchiolitis-related hospitalisation in young children and respiratory-related emergency visits under high temperatures in China. | UMIC Continental Asia |
| Hu et al., 2022 | 37 | 20 | Global | Increased emergency department admissions for childhood asthma due to heat exposure in Australia. | HICs |
| Xu et al., 2018 | 38 | 19 | Global | Positive associations between heat and childhood asthma attack in Japan. The risk of asthma hospital admissions increases with temperature in Hong Kong. | HICs UMIC Continental Asia |
| Bunker et al., 2016 | 39 | 121 | Global | Non-significant heat effects on respiratory-related hospitalisations and negative effect of heat on asthma-related emergency department visits in South Korea. | HICs |
| Burton et al., 2011a | 40 | 15 | Kiribati, Vanuatu | Heat islands in Kiribati and Vanuatu potentially exposing children living in urban areas to heat stress and lung diseases. | PIs |
| Dehydration, heat stroke | |||||
| Uibel et al., 2022 | 36 | 20 | High income countries | Significant increases in renal emergency department presentations and hospital admissions in Australia during heatwaves. | HICs |
| Li et al., 2015 | 11 | 33 | Global | Significant increases in renal emergency department presentations and hospital admissions in Australia during heatwaves. | HICs |
| Nizam et al., 2021 | 41 | 20 | Global | Male mine workers in Australia show signs of dehydration when working in extreme heat stress. | HICs |
| Adverse birth outcomes | |||||
| Ma et al., 2020 | 33 | 175 | China | Heat exposure increases risk of preterm birth in China. | UMIC Continental Asia |
| Dalugoda et al., 2022 | 15 | 75 | Global | High temperatures in the second trimester significantly increase risk of stillbirth in Australia. | HICs |
| Chersich et al., 2020 | 16 | 70 | Global | Increased risk of preterm birth in Australia, South Korea and China, and of stillbirth in Australia. No significant association between heat and low birth weight in South Korea. | HICs UMIC Continental Asia |
| Zhang et al., 2017 | 42 | 36 | Global | Increased risk of preterm birth in Australia and China. No temperature effect on birth weight in New Zealand. | HICs UMIC Continental Asia |
| Sleep disturbance | |||||
| Gulcebi et al., 2021 | 18 | 126 | Global | Sleep efficiency and rapid eye movement sleep decrease with bedroom temperature in Australia. Standard effective temperature negative impacts sleep quality in China, but not temperature or relative humidity alone. | HICs UMIC Continental Asia |
| Zisis et al., 2021b | 43 | 8 | Global | Sleep problems attributed to rising temperatures in Japan. | HICs |
The reviews are grouped by the selected heat-related health outcomes.
Some reviews contain relevant information about more than one health outcomes and, therefore, appear more than once in this table. Citations that are not region-specific or are primary research papers cited within the included reviews are excluded from this table.
Indicates a report included through authors judgement, and its number of studies indicates the total number of citations in that report.
Indicates an umbrella review, and its number of studies indicates the number of reviews examined in it.
Table 3.
Summary of findings.
| Health outcome | Region | Results | No. of reviews | GRADE |
|---|---|---|---|---|
| Mortality | HICs | Strong evidence of heat-related mortality in observed warm periods and heatwaves | 8 | 4 |
| PIs | N/A | 0 | N/A | |
| LDC/LMIC Continental Asia | N/A | 0 | N/A | |
| UMIC Continental Asia | Evidence of heat-related mortality in China, including cause-specific mortality | 7 | 4 | |
| Cardiovascular morbidity | HICs | Inconsistent, weak or no apparent associations between heat exposure and cardiovascular morbidity | 3 | 2 |
| PIs | N/A | 0 | N/A | |
| LDC/LMIC Continental Asia | Non-significant effects of heat on cardiovascular morbidity in Vietnam | 2 | 2 | |
| UMIC Continental Asia | Inconsistent or non-significant associations between heat and cardiovascular health in China | 4 | 2 | |
| Respiratory morbidity | HICs | The effect of heat on respiratory morbidity depends on the study location and health indicator | 6 | 2 |
| PIs | One suggestion of urban heat exposing children in Kiribati and Vanuatu to lung diseases, but without evidence | 1 | 1 | |
| LDC/LMIC Continental Asia | Non-significant associations between heatwaves and respiratory hospital admissions in Vietnam | 1 | 2 | |
| UMIC Continental Asia | Mixed or non-significant evidence of the heat impacts on respiratory health indicators in China | 3 | 2 | |
| Dehydration, heat stroke | HICs | Evidence of heat-related dehydration in Australia | 3 | 3 |
| PIs | N/A | 0 | N/A | |
| LDC/LMIC Continental Asia | N/A | 0 | N/A | |
| UMIC Continental Asia | N/A | 0 | N/A | |
| Adverse birth outcomes | HICs | Strong evidence of heat impacts on preterm birth and stillbirth | 3 | 3 |
| PIs | N/A | 0 | N/A | |
| LDC/LMIC Continental Asia | N/A | 0 | N/A | |
| UMIC Continental Asia | Evidence of heat impacts of preterm birth in China | 3 | 3 | |
| Sleep disturbance | HICs | Some evidence of sleep disturbance from heat in Australia and Japan | 2 | 3 |
| PIs | N/A | 0 | N/A | |
| LDC/LMIC Continental Asia | N/A | 0 | N/A | |
| UMIC Continental Asia | Standard effective temperature affects sleep quality in China, but temperature or relative humidity does not | 1 | 2 |
GRADE stands for Grades of Recommendation, Assessment, Development and Evaluation, and is the adopted approach in this review to assessing the quality of evidence. A GRADE score of 4 indicates high quality, 3 indicates moderate quality, 2 indicates low quality, whereas 1 indicates very low quality. Judgement on (i) study limitations (risk of bias), (ii) indirectness of evidence, (iii) inconsistency of results, (iv) imprecision, and (v) publication bias downgrades GRADE. ‘N/A′ stands for ‘not applicable’ and is used when no review is included for a health outcome in a country category, and therefore no results or GRADE can be given.
For transparency, reviews that are not included in this paper due to meeting exclusion criteria (Search strategy and selection criteria and Fig. 1) are listed in Table S2 in Supplementary Materials.
Mortality
Everyone can be at risk of heat-related mortality, but some people are more vulnerable than others. Older people are more at risk of heat-related mortality than other age groups in Australia and China.24, 25, 26 The evidence of heat-related child mortality is less consistent for the WPR. Increased risk of infant mortality has been reported in South Korea based on data from seven cities in 2004–2007.27,44 Larger increases in mortality in 0–14 year-olds than other age groups were observed in the 1994 heatwave in South Korea.28,45 However, non-significant changes in mortality in 0–14 year-olds during 1993–2006 heatwaves in Adelaide, Australia28,46; in 0–4 year-olds in the 2003 heatwave in Shanghai, China28,47; or during major heatwaves in 2000–2007 in Seoul, South Korea have been reported.28,48 These discrepancies may have arisen from methodological differences in heat definition, statistical modelling and age stratification, and the characterstics of individual heatwaves.
In the WPR high-income countries, there is consistent evidence of heat-related mortality (including all ages). Up to ∼1% of year-round all-cause or non-accidental mortality has been attributed to heat in Australia, Japan and South Korea, in periods before 2000 and 2000–2010.30, 35, 49, 50, 51, 52 In particular, the 2018 heatwave in Japan resulted in high death tolls and hospitalisations.20,53 The Korean Centers for Disease Control and Prevention reported 17 and 48 heat-related deaths in the 2016 and 2018 summers, respectively.31
There are no reviews in the literature covering heat-related mortality in the Pacific Island States, or in LDCs and LMICs in continental Asia. With most countries in these categories being in the Tropics (Table 1), these results are consistent with a review that stated that tropical climates were under-represented in heat and health impact research.24
There is a substantial body of research providing evidence of heat-related mortality in China, a UMIC in continental Asia. Overall, there is a 2% increase in non-accidental deaths per 1 °C increase in temperature above the optimal value.32 In the period 2000–2018, between 0.6 and 1.3% of all-cause or non-accidental mortality in China has been attributable to heat.30,49,54 In 2019, 26,800 heat-related deaths occurred.21 A four-fold increase in heat-related mortality between the years 1990 and 2019 indicates a rising trend in heat impact in the country.21 East and south-central China have seen the most numbers of deaths from heatwaves.21 There is also a stronger heat-mortality effect in cities such as Hong Kong and Shanghai,24,29, 55, 56 although research on the urban heat island effect on mortality is limited for China.29
Excess deaths attributable to heat are seen in the exacerbation of cardiovascular and respiratory diseases in China.21,29 In Jinan, every 1 °C increase above a daily mean temperature of 31 °C (threshold above which excess deaths significantly increases) is associated with a 25% increase in respiratory mortality.33,57 In Nanjing, heatwaves are associated with a 48% increase in chronic obstructive pulmonary disease (COPD) mortality and a 32% increase in respiratory mortality.33,58
Cardiovascular morbidity
While there is evidence of increased cardiovascular mortality in high temperatures, previous analyses have reported inconsistent, weak or no apparent associations between heat exposure and cardiovascular morbidity or hospitalisations,59 including in children.36
In Brisbane, Australia, the risk of cardiovascular ambulance attendances is significantly higher when maximum temperatures are above 37 °C for at least 2 days (the local definition of a heatwave).59,60 For younger (25–64-year-old) female indigenous people in Australia, the risk of ischemic heart disease at the 95th percentile of maximum temperature is about 32% higher than the risk at a lower temperature (90th percentile), according to data from the period 1992–2011.59,61 However, inconsistent results or non-significant associations have also been found between heat and cardiovascular hospital admissions, ambulance attendances and stroke in Brisbane,59,62,63 Perth59,64 and Sydney.6,59,65
In 16 South Korean cities, the risk of emergency visits due to acute myocardial infarction is 1.26 times higher per degree increase in mean temperature above 28.5 °C (inflection point in the temperature-myocardial infarction relationship), according to data from the period 2006–2010.34,59,66 However, two other studies using data from different sets of cities or provinces in 2003–20086,67 and 2013–20146,68 reported no significant heatwave effects on cardiovascular morbidity. These results suggest heterogeneity depending on the location and cardiovascular health indicator.
In Japan, increased risks of emergency admissions for acute coronary syndrome and intracerebral hemorrhage in the Ina area are associated with temperature increases.59,69 However, the risk of out-patient cardiac arrest in older people aged 75 or above decreases when average temperature increases under warm conditions in Osaka, according to data from 1998 to 2007.59,70 Increases in daily maximum temperature have also been reported to decrease hospital emergency transports for hypertension, a precursor for congestive heart failure, in adults above the age of 65 in Tokyo.59,71
There are no reviews in the literature covering heat-related cardiovascular morbidity in the Pacific Island states.
In Hanoi, Vietnam, although a higher risk of cardiovascular hospital admissions is found per degree increase in temperature above 26 °C (temperature of minimum cardiovascular admissions), this result is not significant at the 95% confidence level.59,72 Similar non-significant results have been found for heatwaves in Ho Chi Minh City and other locations in Vietnam.6,59,73
In China, there is evidence of positive and significant associations between heatwaves and cardiovascular morbidity.6,33 In Shanghai, an 8% increase in cardiovascular hospital admissions has been found to be associated with a heatwave in 2007.74 However, in Jinan, exposure to high temperatures could have a protective effect on ischemic stroke hospitalisation, with exposure to 30 °C being associated with a significantly reduced risk of stroke hospital admissions than exposure to 15 °C.59,75,76
Respiratory morbidity
In Australia, there is evidence that heatwaves are significantly associated with increases in respiratory-related emergency department presentations26,77,78 and ambulance call outs.26,60,79 In Brisbane during the period 2003–2009, the risk of asthma emergency department admissions in children was 1.8 times at 26.5 °C, compared with 24 °C, with male children and children under the age of 4 being most vulnerable.37,80 In Adelaide, 360 and 518 excess ambulance call outs have been estimated for the 15–64 age group during the 2008 and 2009 heatwaves, respectively.36,79 However, unchanged or even reduced respiratory-related emergency department presentations during the heatwaves have been reported in the same study, suggesting that not all respiratory-related health indicators respond to extreme heat in the same way. Indeed, other studies have reported non-significant associations between heatwaves and respiratory morbidity.6,81
In Japan, higher daily average temperature has been found to increase emergency visits for childhood asthma in Tokyo,38,82 and the odds of summer night-time primary care visits due to childhood asthma attack in Himeiji City.38,83 Conversely, a negative, albeit less strong, association has been found with daily maximum temperature in Tokyo in the same study.
In South Korea, there is general evidence of positive associations between heatwaves and respiratory morbidity.6,67,68 However, studies have also reported non-significant heat effects on hospitalisations for allergic disease, asthma and other respiratory diseases across 8 Korean cities,39,67 and a drop in the risk of asthma-related emergency department visits when daily mean temperature rises above 21–23 °C in Seoul.39,84
According to a UNICEF report for the countries of Kiribati and Vanuatu, the heat island effect exposes children living in urban areas to heat stress and lung diseases from photo-chemical smog.40 However, there is not enough data to confirm the existence of urban heat islands in these countries.
In Vietnam, non-significant associations between heatwaves and respiratory hospital admissions have been reported.6,73
In Hong Kong, China, significantly increased risk of acute bronchiolitis-related hospitalisation in young children under the age of 2 has been shown under high ambient and apparent temperatures for the period 2008–2017.8,85 The risk of asthma hospital admissions across all ages also increases with temperature above 27 °C in the hot season (May to October), peaking at 30 °C.38,86 In Guangzhou, interactions of sulphate aerosols and high daily temperatures between 27 and 31 °C have been shown to significantly increase respiratory-related emergency department visits.8,87 However, pooling togehter two studies in China, one of which reported significantly increased respiratory emergency visit risks in hot weather in Beijing88 and the other one did not for respiratory hospital admissions in Shanghai,74 another review summarised an overall non-significant association between heatwaves and respiratory morbidity in China.6
Dehydration and heat stroke
Male mine workers in Northern Australia who worked in extreme heat stress (i.e., wet bulb globe temperature above 32 °C) had an increased urine specific gravity (a sign of dehydration) during their shift.41,89 Significant increases in renal emergency department presentations and hospital admissions have also been observed during heatwaves in Adelaide,36,79 Brisbane11,90 and Perth.11,64
Diabetic patients are more prone to both dehydration and heat stroke when exposed to hot weather.91 The effects of heat on dehydration and heat stroke have not been found in existing systematic reviews for other WPR countries. This is likely to be due to the close relation between dehydration and cardiovascular health, and between heat stroke and death.
Adverse birth outcomes
In Brisbane, Australia, there is strong evidence of heat impacts on preterm birth and stillbirth. The odds ratio of preterm birth is at least 1.13 (95% confidence interval: 1.03–1.24) for women who are exposed to at least one heatwave after 20 weeks of gestation and before giving birth.16,42,92 High temperatures in the second trimester15,93 and the last 4 weeks of pregnancy16,94 also significantly increase the risk of stillbirth, with the association being generally more pronounced towards the later stages of pregnancy.16 One study for Brisbane reports a 1.46-fold (hazard ratio; 95% CI: 1.09–1.96) increase in stillbirth risk when heatwave exposure occurs in the eighth gestational month.16,95 In New Zealand, no effect of temperature during any trimester on infant birth weight has been found.42,96
In Seoul, South Korea, exposure to heat during pregnancy has been found to significantly increase the risk of preterm birth. Women with low education levels and socioeconomic status are more at risk, with a 1.1-fold (hazard ratio; 95% CI: 1.03–1.17) increase in preterm birth risk per quartile increase in temperature.16,97 However, the same study did not find a significant association between heat and low birth weight.16,97 The literature is less consistent about the heat impact on birth weight than that on preterm or stillbirth.
No reviews that include adverse heat-related birth outcomes in the Pacific Island States and LDCs or LMICs in continental Asia have been found.
In Chinese cities, exposure to extreme heat during different stages of pregnancy increases the risk of preterm birth in hot areas.16,98 In Guangzhou, exposure to 31.9 °C extreme heat in the last 4 weeks of pregnancy has been found to increase preterm birth risk by 10% (95% CI: 2.9–17.6%), relative to 24.4 °C.33,42,99 Conversely, one study has reported a protective effect of heat on preterm birth in Shenzhen, with the authors suggesting high air conditioning prevalence in the area being a reason.16,42,100
Sleep disturbance
Some evidence of heat impacts on sleep has been found for HICs. A study monitoring indoor temperature and the residents’ sleep quality through wristband sensors in Sydney households reports a 1.04 and 1.65% decrease in sleep efficiency and rapid eye movement sleep (both significant at the 5% level), respectively, per degree increase in bedroom temperature.18,101 Similarly, in Japan, primary physicians conclude that a rising burden of sleep problems could be attributed to rising temperatures.43, 102, 103
No reviews covering the topic of heat and sleep have been found for the PIs and LDCs or LMICs in continental Asia.
For UMICs in continental Asia, information has been found for Beijing, China, where the thermal environment is believed to have a significant effect on sleep quality of participants.18,104 However, the same study reports no correlation between ambient temperature or relative humidity and sleep quality.
Discussion and conclusions
Summary of findings
By reviewing 29 reviews in the literature, we have found a strong association between heat exposure and mortality in the WPR. This is supported by observations over long time periods as well as individual heatwaves, in various locations, despite different study designs (see Confounding factors). Older people are more vulnerable to heat-related mortality than other age groups. The same cannot be concluded for young children with existing evidence.
Cardiovascular morbidity indicated by hospital admissions, emergency visits and ambulance attendances, has a moderate association with heat. While a significant positive association has been found for some groups, locations, and heatwaves, non-significant or even negative associations have been found in other cases. A similar moderate association between heat exposure and respiratory morbidity has been found in the WPR.
There is a strong association between heat exposure and dehydration and heat stoke. There is also a strong association between heat exposure and the risks of preterm birth and stillbirth. However, a weak to non-existent association has been found with low birth weight. The association between heat exposure and sleep quality in the WPR is moderate.
Confounding factors
Studying the effects of heat on humans is complex due to the presence of confounders. Of the 29 reviews examined here, 16 had confounders in their study grading criteria or directly assessed study confounders where relevant. Specifically, five of the reviews26, 27, 28,30,32 that focused on mortality included confounders in their results, with the most controlled factor being air pollution, and most commonly particulate matter <10 μm in diameter (PM10) and nitrogen dioxide. Humidity was also noted by26 as being an important factor in studying extreme heat and mortality, as the presence of high humidity increases heat stress.
Four of the five cardiovascular reviews6,34,59,75 evaluated the studies' ability to include confounders as part of their grading criteria. The most common factors controlled for in these studies were seasonal and long-term trends, with days of the week, holidays, air pollution and the lag effect of temperature included in some studies. None of the reviews made comprehensive summaries on how confounders were treated in the reviewed literature.
Four respiratory reviews8,37, 38, 39 included confounders in their grading schema. The most comprehensive of which was,8 who noted that (i) relative humidity is an important factor along with temperature in determining respiratory system reaction to environmental exposures, and (ii) long-term exposure to high temperatures and air pollution had a larger effect on respiratory health than short-term exposure. Therefore, including a lag in study design is important when studying respiratory responses.
One review11 looking at dehydration and heat stroke made note of air pollution being explored in some of their reviewed studies. Among the birth outcome reviews, two15,42 assessed confounders within their search criteria. Specifically,15 found that in general studies agreed that heat exposure within the last few weeks of pregnancy may be associated with an increased risk of preterm birth and stillbirth. Neither of the sleep disturbance reviews mentioned confounders, highlighting a lack of existing knowledge in this area.
Future directions
Heat already adversely affects various aspects of human health in the current climate, albeit to different extents. Of the WPR countries, the proportion of heat-related mortality in the period 1991–2008 attributed to human-induced climate change ranges from 21.3% in China to 61.2% in the Philippines.105 Even warmer climates in the future, therefore, pose a substantial risk to human health in the WPR. Future projections suggest that Australia, in particular the northern part, is at a high risk of exceeding wet-bulb temperature thresholds for human survival.24 South East Asia will also be one of the worst-hit regions in terms of heat-related mortality in all adaptation scenarios.20 In China, 25,800–37,800 additional heat-related deaths per year are projected for 51 cities by the period 2014–2060, depending on the climate change scenario.29 A global average warming of 2 °C above pre-industrial levels would see tens of thousands more heat-related deaths, including cardiovascular mortality, in China, compared with 1.5 °C global average warming.20,21
Mitigating climate change by reducing greenhouse gas emissions to net-zero is extremely important to avoid worse heat-health impacts. Simultaneously, adapting the WPR populations to rising temperatures is crucial to reducing present-day impacts and avoiding future impacts. Targeted adaptation strategies for individual WPR countries and the vulnerable groups within them (e.g., older people, city residents, indigenous females, children with asthma, manual labour workers, and pregnant women) are effective ways of increasing population resilience to heat.
Successful adaptation strategies in the WPR include urban planning solutions such as increasing the reflectivity of urban surfaces, shown to work in Melbourne, Australia, and combining cooling materials, increased greenery and shading which showed to reduce peak ambient temperatures in Darwin, Australia.106 Moreover, studies reviewing early warning systems in Australia and Japan found them to be an effective ‘no-regret’ public health plan.107 While individual members of the WPR have engaged in successful adaptation efforts, different countries may have different constraints and adaptation requirements. We suggest that WPR countries that do not have similar adaptation actions pilot these interventions and test their effectiveness in protecting their population. Because the WPR as a whole is lacking in widespread published and actionable heatwave plans, future research reviewing other feasible adaptation methods for this region is recommended.
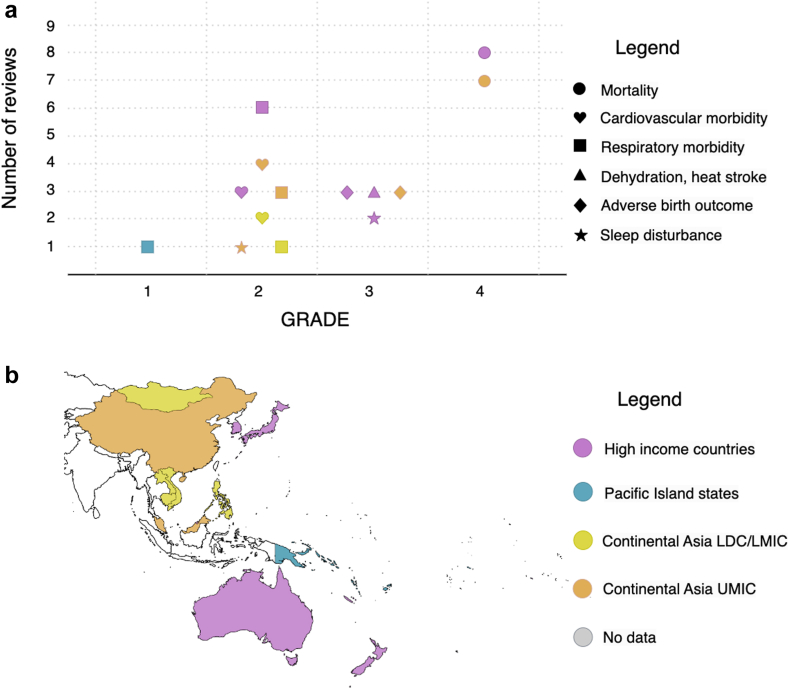
There are spatial and socio-economic clusters within the WPR on which heat-health research has been focused in the literature. HICs such as Australia, Japan and South Korea have been highly studied, with low to high quality evidence found for all of the included health outcomes (Fig. 2). UMICs in continental Asia, predominantly China, have also been well studied, with low to high quality evidence in all but one included health outcomes (except dehydration, heat stroke). However, only cardiovascular and respiratory morbidity have been systematically reviewed for LDCs and LMICs in continental Asia in the literature, both with low quality (GRADE = 2). The Pacific Island States have hardly been reviewed in terms of heat and health. This could partly be due to the fact that only reviews published in English were examined. Nevertheless, future research on LDCs and LMICs in continental Asia and the Pacific Island States is recommended, as it will help stakeholders better understand the local health risks of heat and ways to reduce them. The compound and cascading health impacts of multiple hazards (e.g., heat and floods) are also important to examine.
Fig. 2.
(a) The number of extracted reviews and their quality (GRADE score) for the selected health outcomes, which are indicated by the shape of markers. Note that GRADE scores are discrete, with possible values of 1, 2, 3, or 4. Some markers are moved slightly along the x-axis to separate them from other overlapping markers. The colour of the markers indicates country categories for which data have been extracted: high-income countries (pink), Pacific Island States (blue), LDCs or LMICs in continental Asia (yellow), and UMICs in continental Asia (orange). (b) A map showing which category (coloured) WPR countries belong to (see also Table 1). American Samoa and Tonga are coloured grey because they are on the WHO WPR country list but not in Table 1. White colour indicates countries that are not on the WHO WPR list.
This umbrella review has only included reviews published before February 2023, meaning that research published in the most recent 1–2 years would not have been captured. It has also only covered major acute and direct health outcomes of heat, with mortality being the most studied health outcome (Fig. 2). Morbidity is less studied and its association with heat is less robust. Additionally, the casual linkages between heat and injury, the health effects of long-term slow-onset heat exposure, future projections of heat-related maternal, fetal and neonatal health, and the indirect effects of climate change on migration and therefore health and wellbeing are identified research gaps by the IPCC.20 Future reviews of primary studies, including the most recent literature, as well as novel primary research in these areas would be highly valuable to provide a fuller picture of the complexity of the heat-health problem in the WPR.
Contributors
GH developed the scope of this review with WHO's WPR Office. GH and YTEL conceived the review. YTEL developed the search strategy and inclusion/exclusion criteria with input from JPTH and GH. YTEL and EV searched the databases and screened the reviews. YTEL extracted data from the reviews and wrote the manuscript. EV made the figures. JPTH provided guidance on GRADE. All authors edited the manuscript and agreed the final submission.
Data sharing statement
The sources of all data extracted for this review can be found in References. Search terms used in Scopus and PubMed are in Supplementary Materials.
Editorial note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
We declare no competing interests.
Acknowledgements
We thank the World Health Organization Western Pacific Regional Office for an initial meeting scoping this review and for guiding the categorisation of the countries. YTEL was also supported by the Elizabeth Blackwell Institute for Health Research, University of Bristol, and funded in whole, or in part, by the Wellcome Trust Institutional Strategic Support Fund [grant number 204813/Z/16/Z]. JPTH is a National Institute for Health and Care Research (NIHR) Senior Investigator (NIHR203807).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100952.
Appendix A. Supplementary data
References
- 1.Intergovernmental panel on climate change, “regional fact sheet - Asia. 2021. https://www.ipcc.ch/report/ar6/wg1/downloads/factsheets/IPCC_AR6_WGI_Regional_Fact_Sheet_Asia.pdf Available: [Google Scholar]
- 2.Intergovernmental panel on climate change, “regional fact sheet - small Islands. 2021. https://www.ipcc.ch/report/ar6/wg1/downloads/factsheets/IPCC_AR6_WGI_Regional_Fact_Sheet_Small_Islands.pdf Available: [Google Scholar]
- 3.Intergovernmental panel on climate change. Regional Fact Sheet - Australasia; 2021. https://www.mbie.govt.nz/dmsdocument/11445-regional-factsheet-gisborne-pdf Available: [Google Scholar]
- 4.Ebi K.L., Capon A., Berry P., et al. Hot weather and heat extremes: health risks. Lancet. 2021;398(10301):698–708. doi: 10.1016/S0140-6736(21)01208-3. [DOI] [PubMed] [Google Scholar]
- 5.Mora C., Counsell C.W.W., Bielecki C.R., Louis L.V. Twenty-seven ways a heat wave can kill you: deadly heat in the era of climate change. Circ Cardiovasc Qual Outcomes. 2017;10(11):1–3. doi: 10.1161/CIRCOUTCOMES.117.004233. [DOI] [PubMed] [Google Scholar]
- 6.Cheng J., Xu Z., Bambrick H., et al. Cardiorespiratory effects of heatwaves: a systematic review and meta-analysis of global epidemiological evidence. Environ Res. 2019;177 doi: 10.1016/j.envres.2019.108610. [DOI] [PubMed] [Google Scholar]
- 7.Liu J., Varghese B.M., Hansen A., et al. Heat exposure and cardiovascular health outcomes: a systematic review and meta-analysis. Lancet Planet Health. 2022;6(6):e484–e495. doi: 10.1016/S2542-5196(22)00117-6. [DOI] [PubMed] [Google Scholar]
- 8.Grigorieva E., Lukyanets A. Combined effect of hot weather and outdoor air pollution on respiratory health: literature review. Atmosphere. 2021;12(6):1–30. doi: 10.3390/atmos12060790. [DOI] [Google Scholar]
- 9.Urrutia-Pereira M., Badellino H., Ansotegui I.J., Guidos G., Solé D. Climate change and allergic diseases in children and adolescents. Allergol Immunopathol (Madr) 2022;50:7–16. doi: 10.15586/AEI.V50ISP1.545. [DOI] [PubMed] [Google Scholar]
- 10.Patella V., Florio G., Magliacane D., et al. Urban air pollution and climate change: ‘The Decalogue: allergy Safe Tree’ for allergic and respiratory diseases care. Clin Mol Allergy. 2018;16(1):1. doi: 10.1186/s12948-018-0098-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li M., Gu S., Bi P., Yang J., Liu Q. Heat waves and morbidity: current knowledge and further direction-a comprehensive literature review. Int J Environ Res Public Health. 2015;12(5):5256–5283. doi: 10.3390/ijerph120505256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Howard G., Bartram J., Williams A., Overbo A., Fuente D., Geere J.-A. World Health Organisation; Geneva: 2020. Domestic water quantity, accessibility and health. [Google Scholar]
- 13.Lawton E.M., Pearce H., Gabb G.M. Review article: environmental heatstroke and long-term clinical neurological outcomes: a literature review of case reports and case series 2000-2016. Emerg Med Australas. 2019;31(2):163–173. doi: 10.1111/1742-6723.12990. [DOI] [PubMed] [Google Scholar]
- 14.Xia D.M., Wang X.R., Zhou P.Y., Le Ou T., Su L., Xu S.G. Research progress of heat stroke during 1989–2019: a bibliometric analysis. Mil Med Res. 2021;8(1):1–11. doi: 10.1186/s40779-021-00300-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dalugoda Y., Kuppa J., Phung H., Rutherford S., Phung D. Effect of elevated ambient temperature on maternal, foetal, and neonatal outcomes: a scoping review. Int J Environ Res Public Health. 2022;19(3) doi: 10.3390/ijerph19031771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chersich M.F., Pham M.D., Area A., et al. Associations between high temperatures in pregnancy and risk of preterm birth, low birth weight, and stillbirths: systematic review and meta-analysis. BMJ. 2020;371:1–13. doi: 10.1136/bmj.m3811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Syed S., O'Sullivan T.L., Phillips K.P. Extreme heat and pregnancy outcomes: a scoping review of the epidemiological evidence. Int J Environ Res Public Health. 2022;19(4) doi: 10.3390/ijerph19042412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gulcebi M.I., Bartolini E., Lee O., et al. Climate change and epilepsy: insights from clinical and basic science studies. Epilepsy Behav. 2021;116 doi: 10.1016/j.yebeh.2021.107791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Romanello M., McGushin A., Di Napoli C., et al. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet. 2021;398(10311):1619–1662. doi: 10.1016/S0140-6736(21)01787-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cissé G., et al. In: Climate change 2022: impacts, adaptation and vulnerability. Contribution of working group II to the sixth assessment report of the intergovernmental Panel on climate change. Pörtner H.-O., Roberts D.C., Tignor M., et al., editors. Cambridge University Press; 2022. Health, wellbeing and the changing structure of communities; pp. 1041–1170. [Google Scholar]
- 21.Cai W., Zhang C., Suen H.P., et al. The 2020 China report of the Lancet Countdown on health and climate change. Lancet Public Health. 2021;6(1):e64–e81. doi: 10.1016/S2468-2667(20)30256-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Higgins J., Thomas J., Chandler J., et al. Cochrane Handbook for systematic reviews of interventions. The Cochrane Collaboration; 2019. [DOI] [Google Scholar]
- 23.Guyatt G., Oxman A.D., Akl E.A., et al. GRADE guidelines: 1. Introduction - GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 24.Campbell S., Remenyi T.A., White C.J., Johnston F.H. Heatwave and health impact research: a global review. Health Place. 2018;53:210–218. doi: 10.1016/j.healthplace.2018.08.017. [DOI] [PubMed] [Google Scholar]
- 25.Hansen A., Bi P., Nitschke M., Pisaniello D., Newbury J., Kitson A. Older persons and heat-susceptibility : the role of health promotion in a changing climate. Health Promot J Aust. 2011;22:17–20. doi: 10.1071/HE11417. [DOI] [PubMed] [Google Scholar]
- 26.Mason H., C King J., Peden A.E., C Franklin R. Systematic review of the impact of heatwaves on health service demand in Australia. BMC Health Serv Res. 2022;22(1):1–13. doi: 10.1186/s12913-022-08341-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lakhoo D.P., Blake H.A., Chersich M.F., Nakstad B., Kovats S. The effect of high and low ambient temperature on infant health: a systematic review. Int J Environ Res Public Health. 2022;19:15. doi: 10.3390/ijerph19159109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xu Z., Sheffield P.E., Su H., Wang X. The impact of heat waves on children’s health: a systematic review. Int J Biometeorol. 2014;58:239–247. doi: 10.1007/s00484-013-0655-x. [DOI] [PubMed] [Google Scholar]
- 29.Chan E.Y.Y., Ho J.Y., Hung H.H.Y., Liu S., Lam H.C.Y. Health impact of climate change in cities of middle-income countries: the case of China. Br Med Bull. 2019;130(1):5–24. doi: 10.1093/bmb/ldz011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cheng J., Xu Z., Bambrick H., Su H., Tong S., Hu W. Impacts of exposure to ambient temperature on burden of disease: a systematic review of epidemiological evidence. Int J Biometeorol. 2019;63(8):1099–1115. doi: 10.1007/s00484-019-01716-y. [DOI] [PubMed] [Google Scholar]
- 31.Chae S.M., Kim D. Research trends in agenda-setting for climate change adaptation policy in the public health sector in Korea. J Prev Med Public Health. 2020;53(1):3–14. doi: 10.3961/jpmph.19.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Luo Q., Li S., Guo Y., Han X., Jaakkola J.J.K. A systematic review and meta-analysis of the association between daily mean temperature and mortality in China. Environ Res. 2019;173:281–299. doi: 10.1016/j.envres.2019.03.044. [DOI] [PubMed] [Google Scholar]
- 33.Ma Y., Zhang Y., Cheng B., et al. A review of the impact of outdoor and indoor environmental factors on human health in China. Environ Sci Pollut Res. 2020;27(34):42335–42345. doi: 10.1007/s11356-020-10452-5. [DOI] [PubMed] [Google Scholar]
- 34.Sun Z., Chen C., Xu D., Li T. Effects of ambient temperature on myocardial infarction: a systematic review and meta-analysis. Environ Pollut. 2018;241:1106–1114. doi: 10.1016/j.envpol.2018.06.045. [DOI] [PubMed] [Google Scholar]
- 35.Lee W., Choi H.M., Lee J.Y., Kim D.H., Honda Y., Kim H. Temporal changes in mortality impacts of heat wave and cold spell in Korea and Japan. Environ Int. 2018;116:136–146. doi: 10.1016/j.envint.2018.04.017. [DOI] [PubMed] [Google Scholar]
- 36.Uibel D., Sharma R., Piontkowski D., Sheffield P.E., Clougherty J.E. Association of ambient extreme heat with pediatric morbidity: a scoping review. Int J Biometeorol. 2022;66:1683–1698. doi: 10.1007/s00484-022-02310-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hu Y., Cheng J., Liu S., et al. Evaluation of climate change adaptation measures for childhood asthma: a systematic review of epidemiological evidence. Sci Total Environ. 2022;839 doi: 10.1016/j.scitotenv.2022.156291. [DOI] [PubMed] [Google Scholar]
- 38.Xu Z., Crooks J.L., Davies J.M., Khan A.F., Hu W., Tong S. The association between lead exposure and childhood asthma: a systematic review. Int J Biometeorol. 2018;62:471–481. doi: 10.1007/s00484-017-1455-5. [DOI] [PubMed] [Google Scholar]
- 39.Bunker A., Wildenhain J., Vandenbergh A., et al. Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. EBioMedicine. 2016;6:258–268. doi: 10.1016/j.ebiom.2016.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Burton D., Mustelin J., Ulrich P. 2011. Climate change impacts on children in the Pacific: a focus on Kiribati and Vanuatu; pp. 1–80.http://www.unicef.org/pacificislands/Children_and_Climate_Change_.pdf Available: [Google Scholar]
- 41.Nizam C.M., Ismail A.R., Husshin N. A review of heat stress impact towards construction workers productivities and health based on several heat stress model. J. Adv Res Fluid Mech Therm Sci. 2021;85(1):161–168. doi: 10.37934/arfmts.85.1.161168. [DOI] [Google Scholar]
- 42.Zhang Y., Yu C., Wang L. Temperature exposure during pregnancy and birth outcomes: an updated systematic review of epidemiological evidence. Environ Pollut. 2017;225:700–712. doi: 10.1016/j.envpol.2017.02.066. [DOI] [PubMed] [Google Scholar]
- 43.Zisis E., Hakimi S., Lee E.Y. Climate change, 24-hour movement behaviors, and health: a mini umbrella review. Glob Health Res Policy. 2021;6(1) doi: 10.1186/s41256-021-00198-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Son J.Y., Lee J.T., Bell M.L. Is ambient temperature associated with risk of infant mortality? A multi-city study in Korea. Environ Res. 2017;158:748–752. doi: 10.1016/j.envres.2017.07.034. [DOI] [PubMed] [Google Scholar]
- 45.Kyselý J., Kim J. Mortality during heat waves in South Korea, 1991 to 2005: how exceptional was the 1994 heat wave? Clim Res. 2009;38(2):105–116. doi: 10.3354/cr00775. [DOI] [Google Scholar]
- 46.Nitschke M., Tucker G.R., Bi P. Morbidity and mortality during heatwaves in metropolitan Adelaide. Med J Aust. 2007;187(11–12):662–665. doi: 10.5694/j.1326-5377.2007.tb01466.x. [DOI] [PubMed] [Google Scholar]
- 47.Huang W., Kan H., Kovats S. The impact of the 2003 heat wave on mortality in Shanghai, China. Sci Total Environ. 2010;408(11):2418–2420. doi: 10.1016/j.scitotenv.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 48.Son J.Y., Lee J.-T., Anderson G.B., Bell M.L. The impact of heat waves on mortality in seven major cities in Korea. Environ Health Perspect. 2012;120(4):566–571. doi: 10.1289/ehp.1103759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gasparrini A., Guo Y., Hashizume M., et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet. 2015;386:369–375. doi: 10.1016/S0140-6736(14)62114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kim C.T., Lim Y.H., Woodward A., Kim H. Heat-attributable deaths between 1992 and 2009 in Seoul, South Korea. PLoS One. 2015;10(2):1–14. doi: 10.1371/journal.pone.0118577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vardoulakis S., Dear K., Hajat S., Heaviside C., Eggen B., McMichael A.J. Comparative assessment of the effects of climate change on heat- and cold-related mortality in the United Kingdom and Australia. Environ Health Perspect. 2014;122(12):1285–1292. doi: 10.1289/ehp.1307524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee W.H., Lim Y.-H., Dang T.N., et al. An investigation on attributes of ambient temperature and diurnal temperature range on mortality in five East-Asian countries. Sci Rep. 2017;7(10207):1–9. doi: 10.1038/s41598-017-10433-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hayashida K., Shimizu K., Yokota H. Severe heatwave in Japan. Acute Med Surg. 2019;6(2):206–207. doi: 10.1002/ams2.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gasparrini A., Guo Y., Sera F., et al. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet Health. 2017;1(9):e360–e367. doi: 10.1016/S2542-5196(17)30156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tan J., Zheng Y., Tang X., et al. The urban heat island and its impact on heat waves and human health in Shanghai. Int J Biometeorol. 2010;54(1):75–84. doi: 10.1007/s00484-009-0256-x. [DOI] [PubMed] [Google Scholar]
- 56.Goggins W.B., Chan E.Y.Y., Ng E., Ren C., Chen L. Effect modification of the association between short-term meteorological factors and mortality by urban heat islands in Hong Kong. PLoS One. 2012;7(6):9–14. doi: 10.1371/journal.pone.0038551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Li J., Xu X., Yang J., et al. Ambient high temperature and mortality in Jinan, China: a study of heat thresholds and vulnerable populations. Environ Res. 2017;156:657–664. doi: 10.1016/j.envres.2017.04.020. [DOI] [PubMed] [Google Scholar]
- 58.Chen K., Bi J., Chen J., Chen X., Huang L., Zhou L. Influence of heat wave definitions to the added effect of heat waves on daily mortality in Nanjing, China. Sci Total Environ. 2015;506–507:18–25. doi: 10.1016/j.scitotenv.2014.10.092. [DOI] [PubMed] [Google Scholar]
- 59.Phung D., Thai P.K., Guo Y., Morawska L., Rutherford S., Chu C. Ambient temperature and risk of cardiovascular hospitalization: an updated systematic review and meta-analysis. Sci Total Environ. 2016;550:1084–1102. doi: 10.1016/j.scitotenv.2016.01.154. [DOI] [PubMed] [Google Scholar]
- 60.Turner L.R., Connell D., Tong S. The effect of heat waves on ambulance attendances in Brisbane, Australia. Prehosp Disaster Med. 2013;28(5):482–487. doi: 10.1017/S1049023X13008789. [DOI] [PubMed] [Google Scholar]
- 61.Webb L., Bambrick H., Tait P., Green D., Alexander L. Effect of ambient temperature on Australian northern territory public hospital admissions for cardiovascular disease among indigenous and non-indigenous populations. Int J Environ Res Public Health. 2014;11(2):1942–1959. doi: 10.3390/ijerph110201942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ren C., Williams G.M., Tong S. Does particulate matter modify the association between temperature and cardiorespiratory diseases? Environ Health Perspect. 2006;114(11):1690–1696. doi: 10.1289/ehp.9266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang X.Y., Barnett A.G., Hu W., Tong S. Temperature variation and emergency hospital admissions for stroke in Brisbane, Australia, 1996-2005. Int J Biometeorol. 2009;53(6):535–541. doi: 10.1007/s00484-009-0241-4. [DOI] [PubMed] [Google Scholar]
- 64.Williams S., Nitschke M., Weinstein P., Pisaniello D.L., Parton K.A., Bi P. The impact of summer temperatures and heatwaves on mortality and morbidity in Perth, Australia 1994-2008. Environ Int. 2012;40(1):33–38. doi: 10.1016/j.envint.2011.11.011. [DOI] [PubMed] [Google Scholar]
- 65.Vaneckova P., Bambrick H. Cause-specific hospital admissions on hot days in Sydney, Australia. PLoS One. 2013;8(2) doi: 10.1371/journal.pone.0055459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lee S., Lee E., Park M.S., et al. Short-term effect of temperature on daily emergency visits for acute myocardial infarction with threshold temperatures. PLoS One. 2014;9(4) doi: 10.1371/journal.pone.0094070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Son J.Y., Bell M.L., Lee J.T. The impact of heat, cold, and heat waves on hospital admissions in eight cities in Korea. Int J Biometeorol. 2014;58(9):1893–1903. doi: 10.1007/s00484-014-0791-y. [DOI] [PubMed] [Google Scholar]
- 68.Heo S., Bell M.L., Lee J.T. Comparison of health risks by heat wave definition: applicability of wet-bulb globe temperature for heat wave criteria. Environ Res. 2019;168:158–170. doi: 10.1016/j.envres.2018.09.032. [DOI] [PubMed] [Google Scholar]
- 69.Hori A., Hashizume M., Tsuda Y., Tsukahara T., Nomiyama T. Effects of weather variability and air pollutants on emergency admissions for cardiovascular and cerebrovascular diseases. Int J Environ Health Res. 2012;22(5):416–430. doi: 10.1080/09603123.2011.650155. [DOI] [PubMed] [Google Scholar]
- 70.Tanigawa-Sugihara K., Iwami T., Nishiyama C., et al. Association between atmospheric conditions and occurrence of out-of-hospital cardiac arrest: 10-year population-based survey in Osaka. Circ J. 2013;77(8):2073–2078. doi: 10.1253/circj.CJ-13-0076. [DOI] [PubMed] [Google Scholar]
- 71.Ye F., Piver W.T., Ando M., Portier C.J. Effects of temperature and air pollutants on cardiovascular and respiratory diseases for males and females older than 65 years of age in Tokyo, July and August 1980-1995. Environ Health Perspect. 2001;109(4):355–359. doi: 10.1289/ehp.01109355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Giang P.N., Van Dung D., Giang K.B., Van Vinh H., Rocklöv J. The effect of temperature on cardiovascular disease hospital admissions among elderly people in Thai Nguyen Province, Vietnam. Glob Health Action. 2014;7(1) doi: 10.3402/gha.v7.23649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Phung D., Chu C., Rutherford S., Nguyen H.L.T., Do C.M., Huang C. Heatwave and risk of hospitalization: a multi-province study in Vietnam. Environ Pollut. 2017;220:597–607. doi: 10.1016/j.envpol.2016.10.008. [DOI] [PubMed] [Google Scholar]
- 74.Ma W., Xu X., Peng L., Kan H. Impact of extreme temperature on hospital admission in Shanghai, China. Sci Total Environ. 2011;409(19):3634–3637. doi: 10.1016/j.scitotenv.2011.06.042. [DOI] [PubMed] [Google Scholar]
- 75.Lian H., Ruan Y., Liang R., Liu X., Fan Z. Short-term effect of ambient temperature and the risk of stroke: a systematic review and meta-analysis. Int J Environ Res Public Health. 2015;12(8):9068–9088. doi: 10.3390/ijerph120809068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wang Q., Gao C., Wang H., Lang L., Yue T., Lin H. Ischemic stroke hospital admission associated with ambient temperature in Jinan, China. PLoS One. 2013;8(11):1–8. doi: 10.1371/journal.pone.0080381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Toloo G., Guo Y., Turner L., Qi X., Aitken P., Tong S. Socio-demographic vulnerability to heatwave impacts in Brisbane, Australia: a time series analysis. Aust N Z J Public Health. 2014;38(5):430–435. doi: 10.1111/1753-6405.12253. [DOI] [PubMed] [Google Scholar]
- 78.Khalaj B., Lloyd G., Sheppeard V., Dear K. The health impacts of heat waves in five regions of New South Wales, Australia: a case-only analysis. Int Arch Occup Environ Health. 2010;83(7):833–842. doi: 10.1007/s00420-010-0534-2. [DOI] [PubMed] [Google Scholar]
- 79.Nitschke M., Tucker G.R., Hansen A.L., Williams S., Zhang Y., Bi P. Impact of two recent extreme heat episodes on morbidity and mortality in Adelaide, South Australia: a case-series analysis. Environ Health. 2011;10(42):1–9. doi: 10.1186/1476-069X-10-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Xu Z., Huang C., Hu W., Turner L.R., Su H., Tong S. Extreme temperatures and emergency department admissions for childhood asthma in Brisbane, Australia. Occup Environ Med. 2013;70(10):730–735. doi: 10.1136/oemed-2013-101538. [DOI] [PubMed] [Google Scholar]
- 81.Mayner L., Arbon P., Usher K. Emergency department patient presentations during the 2009 heatwaves in Adelaide. Collegian. 2010;17(4):175–182. doi: 10.1016/j.colegn.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 82.Hashimoto M., Fukuda T., Shimizu T., et al. Influence of climate factors on emergency visits for childhood asthma attack. Pediatr Int. 2004;46(1):48–52. doi: 10.1111/j.1442-200X.2004.01835.x. [DOI] [PubMed] [Google Scholar]
- 83.Yamazaki S., Shima M., Yoda Y., et al. Association of ambient air pollution and meteorological factors with primary care visits at night due to asthma attack. Environ Health Prev Med. 2013;18(5):401–406. doi: 10.1007/s12199-013-0339-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kim J., Lim Y., Kim H. Outdoor temperature changes and emergency department visits for asthma in Seoul, Korea: a time-series study. Environ Res. 2014;135:15–20. doi: 10.1016/j.envres.2014.07.032. [DOI] [PubMed] [Google Scholar]
- 85.Leung S.Y., Lau S.Y.F., Kwok K.L., Mohammad K.N., Chan P.K.S., Chong K.C. Short-term association among meteorological variation, outdoor air pollution and acute bronchiolitis in children in a subtropical setting. Thorax. 2021;76(4):360–369. doi: 10.1136/thoraxjnl-2020-215488. [DOI] [PubMed] [Google Scholar]
- 86.Lam H.C.Y., Li A.M., Chan E.Y.Y., Goggins W.B. The short-term association between asthma hospitalisations, ambient temperature, other meteorological factors and air pollutants in Hong Kong: a time-series study. Thorax. 2016;71(12):1097–1109. doi: 10.1136/thoraxjnl-2015-208054. [DOI] [PubMed] [Google Scholar]
- 87.Chen Y., Zheng M., Lv J., et al. Interactions between ambient air pollutants and temperature on emergency department visits: analysis of varying-coefficient model in Guangzhou, China. Sci Total Environ. 2019;668:825–834. doi: 10.1016/j.scitotenv.2019.03.049. [DOI] [PubMed] [Google Scholar]
- 88.Song X., Wang S., Li T., et al. The impact of heat waves and cold spells on respiratory emergency department visits in Beijing, China. Sci Total Environ. 2018;615(222):1499–1505. doi: 10.1016/j.scitotenv.2017.09.108. [DOI] [PubMed] [Google Scholar]
- 89.Brake D.J., Bates G.P. Fluid losses and hydration status of industrial workers under thermal stress working extended shifts. Occup Environ Med. 2003;60(2):90–96. doi: 10.1136/oem.60.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wang X.Y., Barnett A.G., Yu W., et al. The impact of heatwaves on mortality and emergency hospital admissions from non-external causes in Brisbane, Australia. Occup Environ Med. 2012;69(3):163–169. doi: 10.1136/oem.2010.062141. [DOI] [PubMed] [Google Scholar]
- 91.Cuschieri S., Agius J.C. The interaction between diabetes and climate change – a review on the dual global phenomena. Early Hum Dev. 2021;155 doi: 10.1093/ptj/54.6.677. [DOI] [PubMed] [Google Scholar]
- 92.Wang J., Williams G., Guo Y., Pan X., Tong S. Maternal exposure to heatwave and preterm birth in Brisbane, Australia. BJOG. 2013;120(13):1631–1641. doi: 10.1111/1471-0528.12397. [DOI] [PubMed] [Google Scholar]
- 93.Li S., Chen G., Jaakkola J.J.K., Williams G., Guo Y. Temporal change in the impacts of ambient temperature on preterm birth and stillbirth: Brisbane, 1994–2013. Sci Total Environ. 2018;634:579–585. doi: 10.1016/j.scitotenv.2018.03.385. [DOI] [PubMed] [Google Scholar]
- 94.Strand L.B., Barnett A.G., Tong S. Maternal exposure to ambient temperature and the risks of preterm birth and stillbirth in Brisbane, Australia. Am J Epidemiol. 2012;175(2):99–107. doi: 10.1093/aje/kwr404. [DOI] [PubMed] [Google Scholar]
- 95.Wang J., Tong S., Williams G., Pan X. Exposure to heat wave during pregnancy and adverse birth outcomes: an exploration of susceptible windows. Epidemiology. 2019;30:S115–S121. doi: 10.1097/EDE.0000000000000995. [DOI] [PubMed] [Google Scholar]
- 96.Tustin K., Gross J., Hayne H. Maternal exposure to first-trimester sunshine is associated with increased birth weight in human infants. Dev Psychobiol. 2004;45(4):221–230. doi: 10.1002/dev.20030. [DOI] [PubMed] [Google Scholar]
- 97.Son J.Y., Lee J.T., Lane K.J., Bell M.L. Impacts of high temperature on adverse birth outcomes in Seoul, Korea: disparities by individual- and community-level characteristics. Environ Res. 2019;168:460–466. doi: 10.1016/j.envres.2018.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Guo T., Wang Y., Zhang H., et al. The association between ambient temperature and the risk of preterm birth in China. Sci Total Environ. 2018;613–614:439–446. doi: 10.1016/j.scitotenv.2017.09.104. [DOI] [PubMed] [Google Scholar]
- 99.He J.R., Liu Y., Xia X.-Y., et al. Ambient temperature and the risk of preterm birth in Guangzhou, China (2001-2011) Environ Health Perspect. 2016;124(7):1100–1106. doi: 10.1289/ehp.1509778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Liang Z., Lin Y., Ma Y., et al. The association between ambient temperature and preterm birth in Shenzhen, China: a distributed lag non-linear time series analysis. Environ Health. 2016;15(1):1–11. doi: 10.1186/s12940-016-0166-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Xiong J., Lan L., Lian Z., De dear R. Associations of bedroom temperature and ventilation with sleep quality. Sci Technol Built Environ. 2020;26(9):1274–1284. doi: 10.1080/23744731.2020.1756664. [DOI] [Google Scholar]
- 102.Rifkin D.I., Long M.W., Perry M.J. Climate change and sleep: a systematic review of the literature and conceptual framework. Sleep Med Rev. 2018;42:3–9. doi: 10.1016/j.smrv.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 103.Fukuda S., Ihara T., Genchi Y., Narumi D. Japanese sleep disturbance and fatigue disability weights in evaluating the effects of increasing temperatures on health by a life cycle approach. Int J Life Cycle Assess. 2013;18(5):1089–1097. doi: 10.1007/s11367-013-0551-y. [DOI] [Google Scholar]
- 104.Zhu M.L., Ouyang Q., Shen H.G., Zhu Y.X. Field study on the objective evaluation of sleep quality and sleeping thermal environment in summer. Energy Build. 2016;133:843–852. doi: 10.1016/j.enbuild.2016.10.007. [DOI] [Google Scholar]
- 105.Vicedo-Cabrera A.M., Scovronick N., Sera F., et al. The burden of heat-related mortality attributable to recent human-induced climate change. Nat Clim Change. 2021;11:492–500. doi: 10.1038/s41558-021-01058-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Adnan M.S.G., Dewan A., Botje D., Shahid S., Hassan Q.K. Vulnerability of Australia to heatwaves: a systematic review on influencing factors, impacts, and mitigation options. Environ Res. 2022;213 doi: 10.1016/j.envres.2022.113703. [DOI] [PubMed] [Google Scholar]
- 107.Martinez G.S., Imai C., Masumo K. Local heat stroke prevention plans in Japan: characteristics and elements for public health adaptation to climate change. Int J Environ Res Public Health. 2011;8(12):4563–4581. doi: 10.3390/ijerph8124563. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.