Abstract
Acute phlegmonous gastritis (APG), a rare clinical condition, is mainly characterized by bacterial invasion in the gastric lining and is associated with a high mortality rate. The symptoms of APG include abdominal pain, nausea, vomiting, fever, and infection. Notably, the lack of specificity in the clinical presentation presents challenges in the early diagnosis of the disease. APG is often prevalent in adults, with a higher incidence in men than women. However, patients of other ages may also be affected. We herein present a case report of a 12-year-old girl who was admitted to the hospital with gastrointestinal symptoms and fever. The patient’s imaging findings were compatible with APG. Despite the requirement for surgical treatment in most cases of phlegmonous gastritis, our patient rapidly improved with imaging and antibiotic therapy. This case demonstrates the success of antibiotic therapy with early diagnosis.
Keywords: Acute phlegmonous gastritis, antibiotic therapy, early diagnosis, adolescent, fever, case report
Introduction
Acute phlegmonous gastritis (APG) is a rare clinical condition mainly characterized by a severe fulminating pyogenic bacterial infection in the gastric lining, and it is associated with a high mortality rate. 1 This bacterial infection can progress rapidly, leading to life-threatening septic shock. Early diagnosis of phlegmonous gastritis (PG) is important because of its nonspecific clinical presentation, including epigastric pain, nausea, and vomiting. However, if left untreated, APG can be rapidly fatal; it has a high mortality rate of 27% to 40%, even with appropriate diagnosis and antimicrobial therapy.2–4 Moreover, therapeutic decision-making is highly challenging because no standardized treatment protocols for managing APG have been established. However, surgical intervention is an important treatment modality. Nevertheless, pharmacological treatment after early definitive diagnosis was successful in a 64-year-old patient with APG. 5 The therapeutic effects of antibiotics have also been reported in children. We herein report the first case of early diagnosis and successful antibiotic treatment of APG in a 12-year-old patient.
Case report
The requirement for ethical approval was not enforced for this case report. However, written informed consent was obtained from the patient. The reporting of this study conforms to the CARE guidelines. 6
A 12-year-old girl presented with persistent, vague periumbilical pain. Before admission, she had developed a fever that peaked at 40°C and a cough that produced yellow mucous sputum. After infusion treatment, she did not experience significant relief in her symptoms. Moreover, the pain gradually shifted to the subxiphoid process. Outpatient abdominal computed tomography (CT) showed interstitial hepatogastric lesions with peripheral exudation. Nevertheless, no signs of perforation were evident.
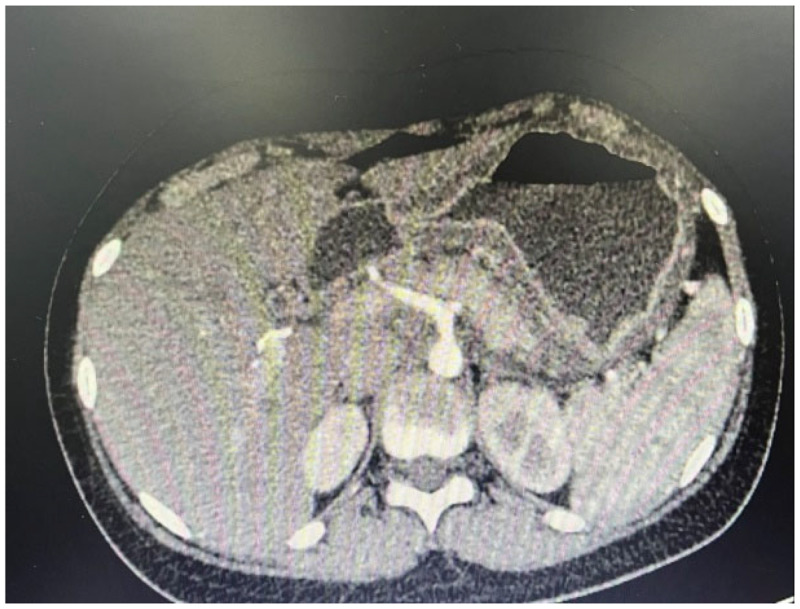
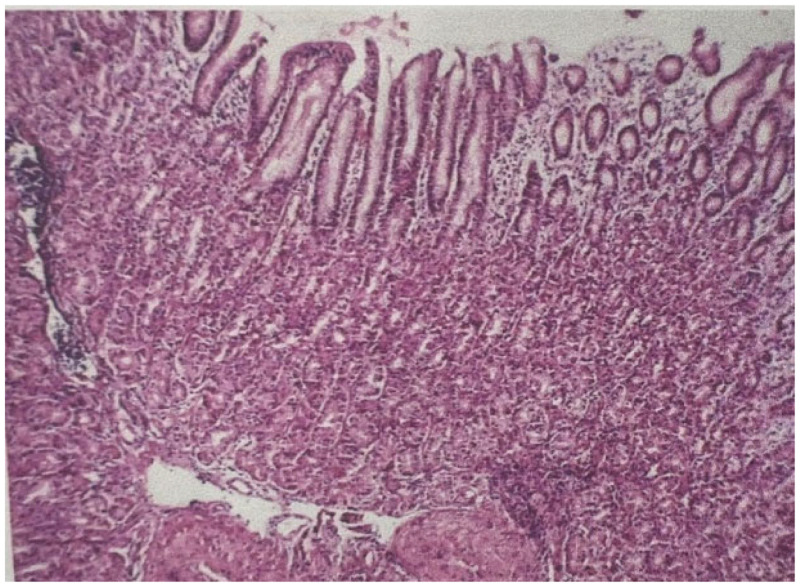
After admission, a blood analysis showed a C-reactive protein concentration of 135.24 mg/L, white blood cell count of 12.57 × 109/L, neutrophil ratio of 88.30%, neutrophil count of 11.10 × 109/L, and procalcitonin concentration of 0.770 ng/mL. Blastocystis was detected in the patient’s stool culture. Unfortunately, she did not undergo a further blood culture. In addition, abdominal enhanced CT showed diffuse thickening of the gastric wall (Figures 1, 2). Endoscopic ultrasound showed diffuse congestion and swelling in the mucosal folds of the gastric body, with localized hypoechogenicity in the submucosa and unclear submucosal layers (Figure 3). The endoscopic pathological examination revealed moderate chronic non-atrophic gastritis with interstitial capillary dilatation, congestion, and high inflammatory activity but no erosion or Helicobacter pylori (Figure 4).
Figure 1.
Thickening of the gastric wall without involvement of the pyloric duct.
Figure 2.
Exudation around the gastric wall with significant wall thickening.
Figure 3.
Endoscopic ultrasound shows hypoechoic areas in the submucosal layer of the mucosal muscle of the gastric wall.
Figure 4.
Microscopic observations show interstitial capillary dilatation and congestion.
The patient was treated by fasting, rehydration, anti-inflammatory therapy with piperacillin sulbactam, and expectoration. Under consideration of septic gastritis, magnetic resonance imaging of the upper abdomen was repeated to validate the diffuse thickening of the gastric wall with blurring of the fatty interstitial space, and the thickening of the gastric wall was found to have significantly improved. In addition, the perigastric exudate had considerably improved (Figures 5, 6). After treatment, the patient’s blood count returned to normal and her clinical symptoms were markedly less severe.
Figure 5.
Magnetic resonance imaging of the gastric antrum after antibiotic therapy shows a significant reduction in gastric wall thickening and perigastric exudation.
Figure 6.
Magnetic resonance imaging of the gastric body after antibiotic therapy shows a significant reduction in gastric wall thickening and perigastric exudation.
Discussion
This case report provides the details of a 12-year-old girl with APG, a rare bacterial infection in the stomach lining. Before admission, the patient exhibited abdominal pain, fever, and cough with production of yellow mucous sputum. The initial diagnostic imaging and preliminary evaluation tests confirmed gastric wall thickening and elevated inflammatory markers. Treatment involved fasting, rehydration, anti-inflammatory medication, and antibiotic therapy. Furthermore, the follow-up imaging reports showed improvement in the gastric wall thickness and clinical symptoms. Overall, this case demonstrates the successful application of antibiotic treatment for APG in a pediatric patient, highlighting the importance of early diagnosis and prompt intervention in managing this potentially life-threatening condition.
Previous reports have suggested that APG is more common in adult patients, affecting mainly middle-aged people aged 45 to 74 years. Moreover, the affected population reportedly comprises approximately 65% men. 4 Although immunocompromised states associated with malignancy, chemotherapy-induced neutropenia, acquired immunodeficiency syndrome, alcoholism, and immunosuppressive drugs have been considered important risk factors, the underlying etiology of APG remains unknown. 7 The current case involved a 12-year-old girl. Although cases of APG in younger patients (including an 11-month-old infant 8 ) and a pregnant woman 9 have been reported, cases occurring in adolescent girls are still relatively uncommon.
The pathological features of APG were first described by Verandeaeus in 1617. 10 A case of limited PG was later described by Cruveilhier in 1820, and a more common case of diffuse PG was described by Andral in 1839. 10 Rankin and Miller 11 determined that about 12% of such cases involved localized lesions. In the present case, the lesion was predominantly located in the gastric wall, and imaging revealed no involvement of the cardia or pylorus. These findings were consistent with the CT imaging of PG in another study. 12
Accordingly, early enhanced CT can help to validate the diagnosis of PG. Alpha-hemolytic streptococci are reportedly the most common causative organisms. However, culture may reveal other microorganisms, including but not limited to Staphylococcus, Aspergillus, Escherichia, pneumococcus, Klebsiella, and Enterobacter. 8 Several routes of infection are possible. One is the direct route, in which infection is directly caused by sputum rich in pathogenic bacteria within the stomach. Another route is via certain local lesions, such as gastric ulcers and gastric cancer. Furthermore, in patients with a low immune status, hematogenous infection may be caused by bacteria in the blood. Notably, APG is not characterized by any specific clinical manifestations. However, some patients exhibit common symptoms of intense epigastric pain, high fever, and vomiting. 1 In our case, the patient presented with abdominal pain, vomiting, and fever.
The diagnosis of APG relies on the aid of enhanced CT and endoscopic ultrasound of the abdomen. Such imaging can clarify the manifestations specific to PG, such as CT lesions that show no involvement of the cardia and pylorus as well as significant thickening of the gastric wall tissues. 12 Endoscopic ultrasound may also reveal secretion and attachment of pus to the gastric wall. 13 Microscopic examination may reveal polymorphonuclear leukocyte infiltration, foci of necrosis, thrombosis, and hemorrhage in the submucosa; the muscularis might be less severely affected. 14 Our patient was re-examined by gastroscopy and biopsy after the clinical diagnosis and treatment of PG, and the pathological findings showed marked improvement in the elevated inflammatory cells.
Surgical and endoscopic drainage and antibiotic therapy are generally prescribed for treatment of PG.1,4 Previous reports have recommended antibiotic treatment alone. The mortality rate approached 92% before the advent of antibiotics and was still as high as 64% even after the availability of antibiotics. 15 However, we believe that early enhanced CT of the abdomen and antibiotic treatment are crucial, especially in adolescent patients.
In summary, our case describes the resolution of APG with antibiotic treatment, and the patient was followed up for 6 months without symptom recurrence.
Supplemental Material
Supplemental material, sj-pdf-1-imr-10.1177_03000605231202136 for Abdominal pain in an adolescent girl with acute phlegmonous gastritis: a case report by Tian Wang, Peizhen Xiao, Jiawen Xue, Jiaojiao Ma and Chunhua Zheng in Journal of International Medical Research
Author contributions: Chunhua Zheng: Conceptualization
Tian Wang: Preparation of the original manuscript draft
Peizhen Xiao: Writing–review and editing
Jiawen Xue: Data curation
Jiaojiao Ma and Chunhua Zheng: Resources
The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD: Tian Wang https://orcid.org/0000-0001-9452-9455
Data availability statement
All data are included in the manuscript.
References
- 1.Yang H, Yan Z, Chen J, et al. Diagnosis and treatment of acute phlegmonous gastritis: a case report. Medicine (Baltimore) 2018; 97: E0629. doi:10.1097/MD.0000000000010629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guo J, Young SK, Lorenzo CR, et al. Phlegmonous gastritis in a patient with myeloid sarcoma: a case report. Appl Immunohistochem Mol Morphol 2009; 17: 458–462. doi:10.1097/pai.0b013e31819f86e2. [DOI] [PubMed] [Google Scholar]
- 3.Kim KH, Kim CG, Kim YW, et al. Phlegmonous gastritis with early gastric cancer. J Gastric Cancer 2016; 16: 195–199. doi:10.5230/jgc.2016.16.3.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Iqbal M, Saleem R, Ahmed S, et al. Successful antimicrobial treatment of phlegmonous gastritis: a case report and literature review. Case Rep Hematol 2018; 2018: 8274732. doi:10.1155/2018/8274732. eCollection 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kato K, Tominaga K, Sugimori S, et al. Successful treatment of early-diagnosed primary phlegmonous gastritis. Intern Med 2015; 54: 2863–2866. doi:10.2169/internalmedicine.54.4257. Epub 2015 Nov 15. [DOI] [PubMed] [Google Scholar]
- 6.Gagnier JJ, Kienle G, Altman DG, et al. ; CARE Group. The CARE guidelines: consensus-based clinical case reporting guideline development. Headache 2013; 53: 1541–1547. [DOI] [PubMed] [Google Scholar]
- 7.Huang YC, Cheng CY, Liao CY, et al. A rare case of acute phlegmonous esophagogastritis complicated with hypopharyngeal abscess and esophageal perforation. Am J Case Rep 2017; 18: 125–130. doi:10.12659/ajcr.902180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feng J, Weng Y, Yuan J, et al. Acute phlegmonous gastritis in an infant. J Pediatr Surg 2005; 40: 745–747. doi:10.1016/j.jpedsurg.2005.01.036. [DOI] [PubMed] [Google Scholar]
- 9.Hommel S, Savoye G, Lorenceau-Savale C, et al. Phlegmonous gastritis in a 32-week pregnant woman managed by conservative surgical treatment and antibiotics. Dig Dis Sci 2007; 52: 1042–1046. doi:10.1007/s10620-006-9235-9. [DOI] [PubMed] [Google Scholar]
- 10.Weiner CI, Kumpe DA, Diaconis JN. Idiopathic gastric abscess. A bizarre intramural lesion. Am J Gastroenterol 1975; 64: 452–459. [PubMed] [Google Scholar]
- 11.Rankin FW, Miller CD. Intramural abscess of the lesser curvature of the stomach. Mayo Clin Bull 1931; 6: 278–281. [Google Scholar]
- 12.Sood BP, Kalra N, Suri S. CT features of acute phlegmonous gastritis. Clin Imaging 2000; 24: 287–288. doi: 10.1016/s0899-7071(00)00216-3. [DOI] [PubMed] [Google Scholar]
- 13.Hu DC, McGrath KM, Jowell PS, et al. Phlegmonous gastritis: successful treatment with antibiotics and resolution documented by EUS. Gastrointest Endosc 2000; 52: 793–795. doi: 10.1067/mge.2000.108926. [DOI] [PubMed] [Google Scholar]
- 14.Mezni F, Chadli-Debbiche A, Khalfallah T, et al. Acute phlegmonous gastritis. apropos of a case. Arch Anat Cytol Pathol 1994; 42: 184–187. [PubMed] [Google Scholar]
- 15.Fan JQ, Liu DR, Li C, et al. Phlegmonous gastritis after esophagectomy: a case report. World J Gastroenterol 2013; 19: 1330–1332. doi: 10.3748/wjg .v19.i8.1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-imr-10.1177_03000605231202136 for Abdominal pain in an adolescent girl with acute phlegmonous gastritis: a case report by Tian Wang, Peizhen Xiao, Jiawen Xue, Jiaojiao Ma and Chunhua Zheng in Journal of International Medical Research
Data Availability Statement
All data are included in the manuscript.