Abstract
Introduction:
Resilience is a person's capacity to overcome adversity. The purpose was to determine what patient factors correlate with resilience using the Brief Resilience Score. We hypothesize that characteristics of female sex, younger age, Workers’ Compensation status, and preoperative opioid use are predictors of a lower preoperative resilience score and that patients with positive psychosocial factors would have higher resilience scores.
Methods:
Eight hundred nine patients undergoing knee or shoulder arthroscopy were preoperatively categorized into low, normal, and high-resilience groups. Preoperative patient-reported outcome measures (PROMs) and demographics were assessed. Statistical analyses evaluated differences in demographics and PROMs between resilience groups.
Results:
Analysis disclosed notable differences between low, normal, and high-resilience groups regarding demographics and PROMs. High resilience was seen in older patients, male patients, and patients with positive psychosocial factors. Low resilience scores were discovered in Workers’ Compensation patients and those with a history of preoperative opioid use. No difference in resilience scores was observed between smokers and nonsmokers.
Discussion:
Preoperative resilience score is associated with age, sex, preoperative opioid use, Workers' Compensation status, and smoking status of patients undergoing knee or shoulder arthroscopy.
Resilience can be described as a person's potential to thrive and prosper in an unfamiliar environment; however, the scientific community has most commonly described it as one's mental and physical capacity to overcome adversity and recuperate from a major trauma.1-3 Medical professionals have been analyzing and exploring resilience in recent years to gain a better understanding of what factors contribute to one's ability to recover from stress on both the body and the mind.3-5 Thus, the Brief Resilience Scale (BRS) was established to generate a compass for assessing resilience as a measurable patient characteristic. The validity of the BRS is confirmed.2,4 Given that describing the nature of resilience can be nebulous and complex, the BRS is a useful tool because it reliably highlights the psychological factors of resilience as they relate to the recovery process.
The goal of surgery is to return an individual to their optimal physical health as quickly as possible; however, there are myriad biological and psychological factors that can contribute to operative outcomes that must be considered. A collection of studies has been conducted analyzing the recovery of operative patients and the significance of psychological factors involved in the rehabilitation process.6 When patients demonstrate unsatisfactory outcomes after undergoing a procedure, it is imperative to address and understand what factors might have contributed to these worse results. While many patient factors may contribute to their postsurgical outcomes, it has been suggested that the resilience of a patient and their psychological ability to bounce back from stress might be a contributing factor.5,6 Currently, most of the musculoskeletal literature reporting on operative outcomes is centered around the physical wellness of patients with little focus given to psychological factors.3 Meanwhile, it has been demonstrated that there is, in fact, a correlation between a patient's cognitive fitness and their patient-reported outcome measures (PROMs).7-9 Silverman et al, Trinh et al, and Magaldi et al discovered that patients undergoing elective orthopaedic surgery with high BRS scores had superior PROMs in comparison with those with low BRS scores.7-9
The purpose of this study was to determine what patient factors, if any, correlate with patients' resilience using the BRS and investigate the relationship between resilience along with commonly used preoperative demographics and PROMs for knee and shoulder arthroscopy patients. Researchers were particularly interested in the association between one's resilience, measured by the BRS, and the VR-12 Mental Health Component Score, a commonly used PROM to measure mental aptitude. It was hypothesized that patients with positive psychosocial factors, demonstrating by a strong VR-12 MCS, would have higher preoperative resilience scores. It was also hypothesized that the patient characteristics of female sex, younger age, Workers' Compensation status, and opioid use before surgery are predictors of lower preoperative resilience scores.
Methods
All patients who underwent shoulder or knee arthroscopy with the senior author (E.G.M.), a fellowship-trained sports medicine orthopaedic surgeon, between October 2017 and February 2022 were approached for participation in this study. International Review Board approval was obtained before the initiation of this study (International Review Board #2011P002663). Consent for participation was conducted by the research assistant and took place at the preoperative clinic visit. Criteria for participation required patients to be older than 18 years and indicated for surgery after exhausting the appropriate conservative therapies including physical therapy, NSAIDs, and injections. Patients were excluded if they had prior knee or shoulder surgery in the operative limb and/or any incomplete preoperative questionnaires.6 The patients in this study underwent either a knee or shoulder arthroscopy in an outpatient surgery center and followed a standard postoperative protocol that corresponded with their procedure. Before the date of their operation, patients completed an electronic questionnaire that incorporated the visual analog scale to determine experienced pain levels, 2-item Pain Self-Efficiency Questionnaire, 2-item Patient Health Questionnaire, history of opioid pain medication usage, BRS questionnaire, and standard preoperative form which encompassed operative history along with the severity of current symptoms. Demographic variables were collected and included age, sex, race, body mass index, current use of opioid pain medication, smoking status, and Workers' Compensation status. Subsequently, patients were asked to complete a preoperative form that assessed patient-reported outcome measures, including the Veterans Rand 12-item Health Survey (VR-12), Marx Activity Scale, Knee Injury and Osteoarthritis Outcome Score, and Single Assessment Numerical Evaluation score for knee arthroscopy patients and the American Shoulder and Elbow Surgeons Standardized Shoulder Assessment (ASES) and Simple Shoulder Test for shoulder arthroscopy patients.6
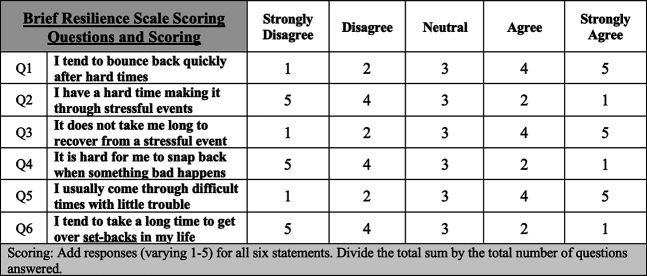
The BRS is a qualitative modality encompassing six statements that are scaled on a progression of one to five. A ‘one’ on the BRS scale represents the lower end of the scale strongly disagreeing with the statement. On the other hand, a ‘five’ represents a strong agreement to the query posed. To eliminate a positive response bias, it was important that the BRS be organized with an equivalent number of positive and negative modules.3 Statements one, three, and five are communicated using positive language while BRS assertions two, four, and six are expressed with negative undertones. The BRS is scored by reverse coding phrases two, four, and six. Patients were divided based on deviation of the mean from BRS score into low-to-normal–resilience and high-resilience groups. Standard cutoff values were used for evaluating resilience scores (1.00 to 2.99, low resilience; 3.00 to 4.30, normal resilience; 4.31 to 5.00, high resilience).8 The BRS is displayed in Figure 1.
Figure 1.
Illustration showing the Brief Resilience Scale assessment tool
Multivariable linear regression was used to assess the association between continuous BRS score and patient factors, including age, sex, body mass index, race, preoperative opioid use, smoking status, Workers' Compensation status, surgery type (knee versus shoulder), and preoperative activity level. An age by sex interaction term was included to assess whether the association between age and resilience was the same for male and female patients. The association between preoperative BRS and PROMs was assessed with Pearson correlation. All statistical analyses were conducted using SAS v9.4 (SAS Institute).
Results
Of the 809 patients (59.3% female) enrolled in this study, 591 underwent knee arthroscopy. Two hundred twenty nine of these patients identified as male and 362 (61.3%) identified as female. The other 218 shoulder arthroscopy patients were more evenly split, with 100 of these individuals identifying as male (45.9%) and 118 (54.1%) identifying as female. Nearly half of patients were older than 50 years (44.7%). No patients were precluded from the investigation because of an intraoperative decision to execute supplementary procedures addressing concomitant pathology. Patient demographics are summarized in Table 1.
Table 1.
Patient Demographics Stratified by Procedure Type
| Patient Characteristic | Overall (n, % of total) | Knee Arthroscopy (n, % of total) | Shoulder Arthroscopy (n, % of total) |
| Sex | |||
| Male | 329 (40.7%) | 229 (38.7%) | 100 (45.9%) |
| Female | 480 (59.3%) | 362 (61.3%) | 118 (54.1%) |
| Age | |||
| ≤24 | 108 (13.3%) | 82 (13.9%) | 26 (11.9%) |
| 25-35 | 102 (12.6%) | 89 (15.1%) | 13 (6.0%) |
| 36-50 | 237 (29.3%) | 197 (33.3%) | 40 (18.3%) |
| ≥51 | 362 (44.7%) | 223 (37.7%) | 139 (63.8%) |
| Body Mass Index Group | |||
| Normal weight | 231 (28.6%) | 164 (27.7%) | 67 (30.7%) |
| Overweight | 294 (36.3%) | 210 (35.5%) | 84 (38.5%) |
| Obese | 284 (35.1%) | 217 (36.7%) | 67 (30.7%) |
| Race | |||
| White | 722 (89.4%) | 518 (87.8%) | 204 (93.6%) |
| Black | 51 (6.3%) | 44 (7.5%) | 7 (3.2%) |
| Asian | 18 (2.2%) | 17 (2.9%) | 1 (0.5%) |
| Currently taking any narcotic pain medication (codeine or stronger) | |||
| No | 777 (96.0%) | 576 (97.5%) | 201 (92.2%) |
| Yes | 32 (4.0%) | 15 (2.5%) | 17 (7.8%) |
| Smoker | |||
| No | 756 (94.4%) | 558 (95.1%) | 198 (92.5%) |
| Yes | 45 (5.6%) | 29 (4.9%) | 16 (7.5%) |
| Workers’ Compensation case | |||
| No | 766 (95.3%) | 561 (95.6%) | 205 (94.5%) |
| Yes | 38 (4.7%) | 26 (4.4%) | 12 (5.5%) |
| BRS category (3-level) | |||
| Low resilience (1.00-2.99) | 35 (4.3%) | 23 (3.9%) | 12 (5.5%) |
| Normal resilience (3.00-4.3) | 536 (66.3%) | 400 (67.7%) | 136 (62.4%) |
| High resilience (4.3-5.00) | 238 (29.4%) | 168 (28.4%) | 70 (32.1%) |
Preoperative resiliency scores were determined for all 809 patients enrolled in the study with a mean score of 3.96 ± 0.62. Thirty-five patients (4%) belonged to the low-resilience category (1.00 to 2.99) while 536 patients (66%) were classified as having normal resilience (3.00 to 4.30). Finally, 238 patients (29%) scored within the range considered to be high resilience (4.31 to 5.00; Figure 2).
Figure 2.
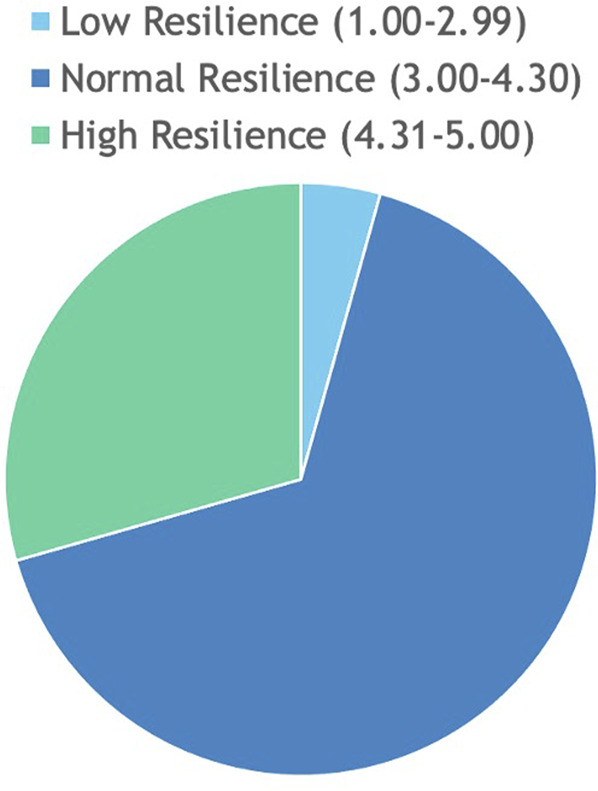
Pie chart showing the representation of patients partitioned based on Brief Resilience Score.
Table 2 analyzes preoperative patient demographics and associates them with patient resilience as measured by the BRS. When looking at age adjusted by sex, female patients 24 years or younger were used as the reference group because this group had the lowest mean BRS score.
Table 2.
Adjusted Association Between Continuous BRS and Demographic Characteristics
| Patient Factors | Categories | Knee | Shoulder | Overall |
| Mean difference (95% Cl) of BRS | Mean difference (95% Cl) of BRS | Mean difference (95% Cl) of BRS | ||
| Sex and age group | 1. Male </=24 | −0.05 (−0.34, 0.24) | −0.14 (−0.64,0.37) | −0.08 (−0.32, 0.16) |
| 2. Male, 24-35 | −0.36 (−0.63, −0.10) | −0.61 (−1.24, 0.03) | −0.40 (−0.64, −0.16) | |
| 3. Male, 36-50 | −0.25 (−0.46, −0.04) | −0.27 (−0.79, 0.26) | −0.25 (−0.44, −0.06) | |
| 4. Male, 51+ | −0.43 (−0.63, −0.22) | −0.35 (−0.77, 0.07) | −0.39 (−0.57, −0.21) | |
| 5. Female, </=24 | Reference | Reference | Reference | |
| 6. Female, 25-35 | −0.29 (−0.52, −0.06) | −0.10 (−0.72, 0.52) | −0.27 (−0.48, −0.06) | |
| 7. Female, 36-50 | −0.26 (−0.46, −0.07) | −0.52 (−0.98, −0.06) | −0.31 (−0.49, −0.13) | |
| 8. Female, 51+ | −0.25 (−0.44, −0.06) P=0.0049 | −0.23 (−0.65, 0.19) P=0.1971 | −0.24 (−0.41, −0.07) P=0.0008 | |
| Preoperative opioid use | 1. No | 0.23 (−0.09, 0.54) | 0.22 (−0.10, 0.55) | 0.25 (0.02, 0.47) |
| 2. Yes | Reference P=0.1636 | Reference P=0.1755 | Reference P=0.0301 | |
| Workers' Compensation | 1. No | 0.37 (0.12, 0.62) reference | 0.37 (−0.02, 0.75) reference | 0.37 (0.17, 0.58) reference |
| 2. Yes | P=0.0035 | P=0.0619 | P=0.0004 | |
| Current smoker | 1. No | 0.13 (−0.10, 0.37) reference | 0.13 (−0.21, 0.47) reference | 0.13(-0.06, 0.32) reference |
| 2. Yes | P=0.2606 | P=0.4526 | P=0.0004 |
Sex by Age Interaction
Compared with female patients younger than 24 years, older age and male patients had significantly higher resiliency in the overall cohort (P = 0.0008). Trends were generally similar in the knee and shoulder cohorts (Table 2).
Preoperative Opioid Use
Patients who used opioids preoperatively had lower average BRS scores in the overall cohort (P = 0.0301; Table 2). Trends were similar although not statistically significant in the knee and shoulder cohorts.
Smoking Status
No significant association was observed between smoking status and resilience in the knee (P = 0.2606), shoulder (P = 0.4526), or overall (P = 0.1867; Table 2) cohorts.
Workers' Compensation
Although this group only represented 4.7% of the cohort (38 patients), there is a strong association between low resiliency and Workers’ Compensation cases in the knee (P = 0.0035), shoulder (P = 0.0619), and overall (P = 0.0004; Table 2) cohorts. Trends were similar across the two cohorts, with Workers’ Compensation cases on average reporting resilience 0.37 points lower than non–Workers’ Compensation cases.
Psychosocial Factors
Additional associations were explored concerning the BRS score and psychosocial factors. Patients with positive psychosocial factors (possessing a confident preoperative mental state) obtained high BRS mean scores in the overall cohort. For example, preoperatively, the group of patients who were confident they could accomplish all their goals despite their current level of pain had a higher BRS mean score in the overall cohort compared with the group of patients who were not at all confident. Furthermore, patients who asserted they expected an improvement in motion and strength had a higher BRS mean score in the overall cohort compared with those who did not expect an improvement. Logically, these trends validate the resilience score because the scale is designed to determine how well patients can bounce back from a physical trauma based on their preoperative and postoperative mental status.
VR-12 Mental Health Component Score
Finally, the team analyzed correlations between preoperative patient-reported outcomes and the BRS. Through utilization of the VR-12 Mental Health Component Score, high resilience was associated with strong mental health in both the knee [Pearson correlation (95%CI): 0.38 (0.30,0.44)] and shoulder [Pearson correlation (95%CI): 0.39 (0.27,0.50)] cohorts.
Discussion
The main findings of this study are that preoperative resilience scores are higher in male and older patients undergoing both arthroscopic knee and shoulder procedures. This claim is supported by a retrospective study by Haffar et al (2021) who followed 86 patients who underwent primary unilateral total knee arthroplasty. Haffar et al10 asserted that resilience significantly correlated with male sex (P = 0.031) along with preoperative VR-12 MCSs. Furthermore, this study's discovery that high preoperative resilience scores correlate with older patients is supported by Otlans et al11 (2021), who asserted that adults are more likely to obtain increased resilience scores compared with younger patients because of their greater experience with stress and trauma.
The BRS was established to assess an individual's ability to bounce back from a stressful psychological and physical circumstance. Currently, within the medical community and subsequent literature, the BRS is most used to measure an individual's psychological strength as it allows them the ability to recover. A specific example of the BRS used to assess operative outcomes can be seen in the study by Silverman et al7 (2020). This prospective cohort study followed 40 individuals who were undergoing hip arthroscopy operations from a single surgeon. After conducting a comparative analysis between low and high-resilience patients, a strong correlation was determined between preoperative and postoperative patient-reported outcomes. Patients with high resilience were able to return to sport earlier and had lower preoperative depression/anxiety.
The analysis of this current study further revealed an association between resilience and mental health. Patients with strong mental health had high resilience scores. By correlating preoperative PROMs with the BRS, an association was discovered between high resiliency and the VR-12 Mental Score revealing that high resilience scores were associated with strong mental health in both the knee and shoulder cohorts. These findings are supported by DiSilvestro et al12 This study evaluated 95 individuals undergoing a lumbar spinal fusion with the stipulation that each patient complete the BRS. Researchers concluded that preoperative resilience is associated with mental health quality in lumbar spinal fusion patients. Understanding a patient's resiliency can provide insight into their mental health and allow surgeons to make more informed decisions on determining best treatment options and rehabilitation for each individual patient.
Limitations of this study include sampling bias because the investigation was restricted to a group of patients from a single institution. Furthermore, this study incorporated a sports medicine population with a limited number of patients with low resilience along with a minimal number of Workers' Compensation cases and patients with a positive smoking status. An additional limitation might include the Hawthorne effect because patients sampled were informed of their participation in this study before initial engagement. Moreover, the BRS was originally developed for a psychiatric population and, therefore, the norms of a sports medicine population may not be the same. In addition, this study declined to incorporate and report postoperative BRS; however, Drayer et al13 showed notable differences between preoperative and postoperative BRSs.
Additional research should be conducted to examine the BRS and overall outcomes. Drayer et al (2020) showed notable differences in the Knee Injury and Osteoarthritis Outcome Score, PROMIS-43, and International Knee Documentation Committee. Tokish et al14 showed that resilience (BRS) was a major predictor of postoperative outcomes after total shoulder arthroplasty, with low-resilience patients reporting markedly lower PROM scores postoperatively. Furthermore, Tokish et al14 revealed that lower resilience patients had markedly lower Penn and Single Assessment Numerical Evaluation scores.
Conclusion
This study provides evidence that preoperative resilience score, as measured by the BRS, is associated with age, sex, preoperative opioid use, Workers’ Compensation, and smoking status of patients undergoing knee and shoulder arthroscopy.
Footnotes
Dr. Matzkin or an immediate family member has received nonincome support (such as equipmentor services), commercially derived honoraria, or other non-research–related funding (such as paid travel) from Arthrex, Inc. Editorial or governing board: Arthroscopy. None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Ms. Mazzocca, Ms. Lowenstein, Mr. Crutchfield, and Dr. Collins.
Contributor Information
Jillian L. Mazzocca, Email: jmazzocca@bwh.harvard.edu.
Natalie A. Lowenstein, Email: nlowenstein@bwh.harvard.edu.
Connor R. Crutchfield, Email: Connor.Crutchfield@students.jefferson.edu.
Jamie E. Collins, Email: jcollins@bwh.harvard.edu.
References
- 1.Furstova J, Kascakova N, Polackova Solcova I, Hasto J, Tavel P: How czecho-Slovakia bounces back: Population-based validation of the brief resilience scale in two central European countries. Psychol Rep 2022;125:2807-2827. [DOI] [PubMed] [Google Scholar]
- 2.Rodríguez-Rey R, Alonso-Tapia J, Hernansaiz-Garrido H: Reliability and validity of the brief resilience scale (BRS) Spanish version. Psychol Assess 2016;28:e101-e110. [DOI] [PubMed] [Google Scholar]
- 3.Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J: The brief resilience scale: Assessing the ability to bounce back. Int J Behav Med 2008;15:194-200. [DOI] [PubMed] [Google Scholar]
- 4.Fung SF: Validity of the brief resilience scale and brief resilient coping scale in a Chinese sample. Int J Environ Res Public Health 2020;17:1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zabat MA, Lygrisse KA, Sicat CS, Pope C, Schwarzkopf R, Slover JD: The impact of patient resilience on discharge after total hip arthroplasty. J Arthroplasty 2022;37:S493-S497. [DOI] [PubMed] [Google Scholar]
- 6.Chavez TJ, Garvey KD, Collins JE, Lowenstein NA, Matzkin EG: Resilience as a predictor of patient satisfaction with nonopioid pain management and patient-reported outcome measures after knee arthroscopy. Arthroscopy 2020;36:2195-2201. [DOI] [PubMed] [Google Scholar]
- 7.Silverman AR, DeFroda SF, Cohen BH, Quinn MS, Tabaddor RR: The brief resilience scale is associated with pre- and short-term postoperative outcomes following hip arthroscopy. Hip Int 2022;32:641-647. [DOI] [PubMed] [Google Scholar]
- 8.Trinh JQ, Carender CN, An Q, Noiseux NO, Otero JE, Brown TS: Resilience and depression influence clinical outcomes following primary total joint arthroplasty. J Arthroplasty 2021;36:1520-1526. [DOI] [PubMed] [Google Scholar]
- 9.Magaldi RJ, Staff I, Stovall AE, Stohler SA, Lewis CG: Impact of resilience on outcomes of total knee arthroplasty. J Arthroplasty 2019;34:2620-2623.e1. [DOI] [PubMed] [Google Scholar]
- 10.Haffar A, Bryan S, Harwood M, Lonner JH: Patient resilience has moderate correlation with functional outcomes, but not satisfaction, after primary unilateral total knee arthroplasty. Arthroplast Today 2021;10:123-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Otlans PT, Szukics PF, Bryan ST, Tjoumakaris FP, Freedman KB: Resilience in the orthopaedic patient. J Bone Joint Surg Am 2021;103:549-559. [DOI] [PubMed] [Google Scholar]
- 12.DiSilvestro KJ, Bond D, Alsoof D, et al. : Preoperative resilience and early postoperative outcomes following lumbar spinal fusion. World Neurosurg 2022;163:e573-e578. [DOI] [PubMed] [Google Scholar]
- 13.Drayer NJ, Wallace CS, Yu HH, et al. : High resiliency linked to short-term patient reported outcomes and return to duty following arthroscopic knee surgery. Mil Med 2020;185:112-116. [DOI] [PubMed] [Google Scholar]
- 14.Tokish JM, Kissenberth MJ, Tolan SJ, et al. : Resilience correlates with outcomes after total shoulder arthroplasty. J Shoulder Elbow Surg 2017;26:752-756. [DOI] [PubMed] [Google Scholar]