ABSTRACT
Objectives: Immigration of Arabs to the United States has increased in recent years due to political instability and need for improved access to healthcare. Cardiovascular disease, diabetes, and obesity disproportionally affect Arab Americans. Student pharmacists are well positioned to increase health awareness by providing health screening services and education classes to the Arab immigrant community. This report will describe the development of a student-run Arab American Health Awareness Program (AAHAP) that provides culturally-sensitive community screening services targeting common health disparities seen among Arab-Americans.
Design: Data were collected on the number of patient cardiometabolic screenings, referrals for medical care, and health classes which were performed over the course of 2 years. The practice setting included community centers, faith-based centers, and grocery stores in the Chicago area participating in the AAHAP.
Results: Over the course of two years, eight cardiometabolic screenings and four community health classes were provided to the Arab-American community. Over 100 student pharmacists provided screenings to 929 patients through AAHAP. Twenty percent (n=193) of all patients screened were referred for further medical care. A total of 77% patients were within goal for blood pressure, 82.3% for blood glucose, and 39.4% for BMI. Patients with a known history of hypertension (n=83) or diabetes (n=64) were more likely to have uncontrolled blood pressure (45% vs 11%, p<0.05) or blood glucose (39% vs 14%, p<0.05) compared to patients without a history of these chronic conditions.
Conclusion: Student pharmacists can be drivers for health access through community health programs for ethnically minoritized populations. Development of a health awareness program focused on known health disparities in Arab Americans has provided student pharmacists with opportunities to deliver culturally-sensitive care and medical referral services to an underserved community.
Key words: Health access, community health, Student Pharmacists, Arab-American
Introduction
Immigrants to the U.S. often arrive with medical conditions requiring immediate care but are faced with language barriers and limited understanding of the U.S. healthcare system which can lead to health disparities and poor outcomes.1,2 Limited health literacy and cross-cultural communication breakdowns amongst immigrants can increase hospitalizations, adverse drug reactions, and incidence of preventable diseases.3 Arab-American immigrants specifically have cultural differences and differing health and religious beliefs that can influence behaviors and healthcare decisions, sometimes resulting in positive habits but in other instances limiting healthcare utilization. 45 For example, many Arab-American Muslims believe that diet and avoiding intoxicants like drugs and alcohol are important to maintaining good health but also value modesty as an Islamic mandate that can prevent Muslim women from seeking care from a provider of the opposite gender.6 Therefore, when interacting with Arab-Americans, providing the best patient care requires cultural awareness and knowledge of health disparities.
As the U.S. Census classifies Arab Americans as “White,” there is limited national health data on Arab-American populations and an absence of minority-status designation.4,5 Compared to the general population, health disparities among Arab-Americans include a higher risk of diabetes and cardiovascular disease.7 As much as 23% of the Arab-American population has diabetes and 13.4% hypertension.8,9 With a growing Arab-American population, there is a need to create healthcare interventions targeting these health disparities.
Culturally-sensitive care requires a healthcare professional to consider a patient’s beliefs, values, and linguistic preferences when interacting with patients and goes beyond having cultural competence or knowledge about certain cultural groups.13 Furthermore, a culturally-sensitive, community-based program integrates such aspects into training and addresses barriers to healthcare utilization, while also facilitating the delivery of quality healthcare to marginalized populations like Arab-Americans. In addition, such programs can define the relevant variables of acculturation, such as social support and fluency in English, which is the process by which immigrants learn and adapt to various aspects of their new country’s culture. Significant barriers to health screening include lack of knowledge, lack of access to healthcare, language barriers, and fear or embarrassment from seeking treatment.7,10 Community health screening events targeting ethnic minority communities can provide the means to overcome these barriers through promoting healthy lifestyles and early detection of certain diseases, which are shown to decrease health disparities.11,12 Health screenings also provide student pharmacists with the opportunity to become active in their communities, increase their cultural sensitivity, and apply knowledge gained in the classroom to direct patient care.
There is limited literature describing community-based programs aimed at improving health awareness of preventable disease and health access for the Arab-American population. To deliver such programs, student pharmacists must be trained to integrate clinical and cross-cultural communication skills to strengthen their patient relationships, increase engagement in the community, and improve cultural awareness. This includes interpreting differences in language or communication style and acknowledging the differences in customs, values, and lifestyles between patients and healthcare professionals. For example, in Arab culture there is often a collectivist/communal approach to health decisions versus a more individualist approach seen in Western Euro-American cultures.4 Arab-American patients are more likely to bring family and caregivers to healthcare appointments and culturally-aware providers would invite them into the conversation if the patient desires.
This report will describe the development of a student-run Arab American Health Awareness Program (AAHAP) that provides culturally-sensitive community screening services targeting commonly seen health disparities seen among Arab-Americans.
Materials and Methods
Student pharmacists participating in AAHAP established relationships with community centers, religious centers and grocery stores in neighborhoods predominantly serving Arab Americans. AAHAP services were offered in these locations to provide the general population with health education and screenings to prevent chronic health conditions. The services provided by AAHAP are outlined in figure 1.
Figure 1:
Components of the Arab-American Health Awareness Program(AAHAP)
Student pharmacists developed and delivered four interactive health awareness classes addressing disease prevention and health promotion specific to the Arab-American population. The content for the health education classes was created with faculty input and health resources from the American Heart Association and American Diabetes Association. Topics included smoking cessation, hypertension, diabetes self-care, heart-healthy diet (with examples utilizing Middle Eastern/Mediterranean cuisine), and goals for physical activity. The duration of each class was one hour and utilized Power Point presentations with interactive visuals about each topic with integrated time for questions from participants. Educational classes did not provide health screening to individual patients. Health screening services included blood pressure (BP), blood glucose (BG), and body mass index (BMI), and cholesterol screenings. Each health screening lasted between two and four hours and was provided in English and Arabic. Screenings were advertised, in both English and Arabic, to members of the community through flyers, posters, and social media posts one to two weeks prior to each event. Patients were not required to sign up in advance as each screening was offered as a walk-up service. A designated table for blood pressure, blood glucose, cholesterol, and BMI was placed at each event, with 2-3 patient stations at each. Regardless of past medical history, all adult patients over the age of 18 years were offered all screenings at their discretion. While there was no funding to hire a trained medical interpreter at each event, bilingual students and supervising pharmacists were provided with commonly used medical words in Arabic as part of training prior to each event. All educational classes and screenings were supervised by one to four supervising pharmacists, based on the number of anticipated patients. The role of the supervising pharmacists was to provide support to students as they applied their communication and clinical skills and to answer patient questions.
Providing methods for patients to be referred for future, affordable medical care without compromising the patient’s cultural needs was an essential component of AAHAP. Therefore, a mutual collaboration was started with the Chicago-based non-profit Compassion Care Network (CCN) to provide charitable, reduced-cost medical services to underserved communities. Patients without health insurance needing further medical care, regardless of immigration status and financial resources, were referred to CCN’s network of over 200 providers. AAHAP also incorporated the use of social media and technology to provide patients with reinforced health education and support following each screening. A community engagement grant from the American Heart Association supported a social media presence on Facebook and Instagram to provide health information about diabetes self-care and heart-healthy diet tips. Patients could also opt in to receiving automated text messages encouraging healthy lifestyle choices, follow up with primary care providers, and medication adherence both in English and Arabic. Students created 10 statements that were delivered bi-weekly for 5 weeks following each screening date.
Cross-Cultural Communication & Skills Training
Culturally sensitive patient care requires student pharmacists to be able to recognize and respond to differences in communication styles, customs, values, and lifestyles held by various patient populations as they engage with their health. As part of AAHAP, student pharmacist volunteers are required to participate in a two-hour-long training session led by a Middle Eastern-identifying pharmacist faculty member alongside three to five senior AAHAP student leaders to ensure proper facilitation and teaching. Attendance of at least one training session was mandatory and they were offered approximately one week prior to each health screening event. Any student pharmacist, regardless of program level, language speaking abilities, or cultural background, was invited to become a volunteer of AAHAP. Junior students who may have not had clinical skills training in the required PharmD curriculum were given extra time to practice their techniques during each training session. All students received baseline knowledge about various cross-cultural communication models and health literacy as part of the required PharmD curriculum prior to volunteering. This knowledge was augmented by training student pharmacists to understand the cultural differences and potential barriers to communication, healthcare utilization, including information on typical diets, natural remedies, and common diseases or risk factors for Arab Americans. Training sessions required every student to practice each screening on two other students and score 100% on a five-question competency-based multiple choice assessment to ensure mastery and understanding.
Techniques taught to improve cross-cultural communication included the Listen, Explain, Acknowledge, Recommend, Negotiate (LEARN) Model.13 This model provides a framework for developing culturally sensitive treatment plans. LEARN emphasizes active listening, use of non-technical terms accounting for health literacy and cultural beliefs, acknowledging differences and similarities due to the patient’s health beliefs, recommending plans that consider those beliefs with patient-specific goals, and negotiating the final plan to integrate patient perspective. Culturally-appropriate non-verbal communication was taught using the Squarely, Open, Lean, Eye Contact, Relax (SOLER) Model, which is not meant to be specific to Arab Americans, but rather is a guideline to help healthcare professionals orient to any patient and reduce common barriers in communication.14 This teaches the healthcare professional to sit squarely on the same level as the patient, maintain an “open” body posture (e.g., avoiding crossed arms or legs), lean forward to demonstrate interest and active listening, establish culturally-appropriate eye contact, and show relaxation in body language to indicate dedicated time for the patient. When working with Arab Americans, students were taught to follow the lead of the patient as it comes to proximity, physical touch, and direct eye contact. Finally, students were encouraged to utilize open-ended Kleinman cross-cultural interview questions when appropriate.15 Example questions include: “what do you call the illness?” “what do you think caused the illness?” and “what do you fear most about the illness?” Students were also introduced to health literacy concepts that commonly impact health outcomes and adherence to treatment in the Arab-American population. Student pharmacists were encouraged to utilize the “teach-back” method to assess patient understanding and provide counseling in the patient’s preferred language. Use of translated written educational materials detailing BP, BG, and BMI goals as well as therapeutic lifestyle changes were also covered at each training event.
Training on technical and clinical skills was also conducted prior to health screening events. Training included becoming familiar with how to: 1) check a blood pressure using a cuff that inflates manually with a stethoscope, as well as with an automatic blood pressure machine; 2) measure blood glucose using a glucometer; 3) measure cholesterol using a CardioChek® point-of-care device; and 4) calculate body mass index using a scale and height. Beyond how to properly use each device, students were also taught to interpret patient-specific values through case examples and practice health counseling through role-play with peers.
Evaluation Methods
After more than two consecutive years (2017-2018), a retrospective evaluation of the program was completed to evaluate the impact on the Arab-American community by quantifying: 1) number of patients encounters achieved and 2) number of referrals made following cardiometabolic screenings and health promotional classes.
All patients over the age of 18 were eligible to be screened for BP, BG, and BMI at no cost and regardless of their health status. Patient demographics including age, gender, whether they were of Middle-Eastern decent and abbreviated past medical history were collected using a password-protected electronic form accessed on a tablet. Patients could complete any or all specific screenings. Due to the complexities of screening and interpreting results for gestational diabetes or BMI, pregnant females were excluded from being offered a blood glucose screening and were encouraged to contact their healthcare provider for a comprehensive assessment.
Blood pressure screenings were conducted in accordance with the Eighth Joint National Committee (JNC-8) guidelines.16 A systolic BP greater than 140 mmHg or a diastolic BP greater than 90 mmHg was classified as above goal. Patients were asked to be seated for 5 minutes during which time they were asked if they had caffeine or smoked that day. Blood pressures were repeated if the first reading was above goal or below 100/80 mmHg. Blood glucose screenings utilizing glucometers (OneTouch® Ultra 2) were based on the American Associated of Clinical Endocrinologists and American College of Endocrinology (AACE/ACE) guidelines.17 Patients were asked if they were fasting or post-prandial and whether they had taken their diabetes medications that day. Testing results, necessary counseling, and educational materials were provided in English or Arabic verbally and in writing. Patients with an abnormal BP or BG result were referred to the supervising pharmacist for further counseling and a recommendation to follow-up with their healthcare provider if indicated. Referral to a local emergency room was made if a patient was symptomatic with a BP ≥ 180/110 mmHg, BG > 250 mg/dL, or a BG ≤50 mg/dL with no response to glucose tablets.
Statistical analyses of the community health data were performed using SPSS 22, (IBM; Chicago, Illinois). Descriptive data were summarized with means for quantitative variables, including knowledge scores. Multivariate analysis was conducted via simultaneous estimation techniques, including multiple regression and multiple logistic regression. The institutional review board at Midwestern University approved this project.
Results
Community screenings
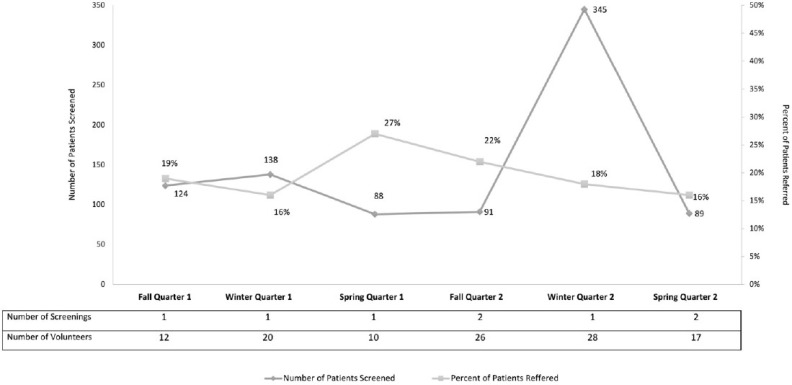
A total of 8 health screenings were conducted over the course of two calendar years. The location of the events included grocery stores (n=2), faith-based centers (n=3), community centers (n=2), and a local convention center (n=1). The mean cost per health screening event was $105 to cover cost of supplies. Over 85% of patients elected to have both their BP and BG screened at each event. Nine-hundred and twenty-nine patient encounters were provided with screenings for BP, BG, and BMI by over 100 student pharmacists (Figure 2).
Figure 2:
Patient screenings and referrals per quarterly event
Table 1 describes the demographic characteristics of study participants and factors specific for each condition, including a history of disease and the presence of cardiovascular risk factors. Data for cholesterol screenings were not collected, as it was only offered for one screening event due to supply issues. Females represented more than half of the patient encounters screened for BP, BG, and BMI. Mean readings for the entire population included systolic BP of 125.1 ± 21.4 mmHg, diastolic BP of 72.3 mmHg, typically post-prandial BG of 115.9 ± 48.1 mg/dL, and BMI of 26.3 ± 5.4. Of participants screened for BP, 20.5% (n=83) had a prior diagnosis of hypertension and 8.2% (n=33) reported currently using tobacco products. Forty-four percent (n=178) of participants screened for BP had additional CV risk factors, including a history of stroke, myocardial infarct, obesity, or family history of CV disease. Patients with a known history of hypertension or diabetes were more likely to have uncontrolled BP (45% vs 11%, p<0.05) or BG (39% vs 14%, p<0.05) compared to patients without a history of these chronic conditions. Of the participants screened for BG, 14.1% (n=64) were previously diagnosed with diabetes. A total of 56.3% of patients screened for BMI were found to be overweight, defined by BMI > 25 kg/m2.
Table 1.
Demographic Characteristics and Screening Results
| N (%) | |
|---|---|
| Blood Pressure Screening Participants, n= 404 a | |
| Age, years (mean ± SD) | 42.8 (15.1) |
| Gender, Male | 162 (40.1) |
| Previous diagnosis of HTN | 83 (20.5) |
| Currently use tobacco | 33 (8.2) |
| Presence of CV risk factorsb | 178 (44.1) |
| Above goal | 86 (21.3) |
| Blood Glucose Screening Participants, n= 454 a | |
| Age, years (mean ± SD) | 41.8 (16.3) |
| Gender, Male | 170 (37.4) |
| Previous diagnosis of DM | 64 (14.1) |
| Fasting, | 43 (9.5) |
| Above goal | 67 (14.8) |
| Body Mass Index Screening, n= 71 | |
| Age, years (mean± SD) | 37.5 (14.6) |
| Gender, Male | 29 (40.8) |
| BMI (mean ± SD) | 26.3 (5.4) |
| Underweight (<18.5) | 3 (4.2) |
| Normal (18.5-24.9) | 28 (39.4) |
| Overweight (25-29.9; above goal) | 21 (29.6) |
| Obese (≥30; above goal) | 19 (26.8) |
Abbreviations used: HTN=Hypertension; DM=Diabetes Mellitus; BMI=Body Mass Index; CV=Cardiovascular
Data was not recorded by student pharmacists.
CV risk factors included history of stroke, myocardial infarct, obesity, family history of CV disease.
Discussion
This study is the first to evaluate a student pharmacist-led health education and screening program targeting an Arab-American community living in the United States. The evaluation highlighted student-driven methods to improve health awareness for Arab Americans by providing free, accessible, culturally-sensitive health education as a means to minimize barriers and facilitate access. The impact of student-led programs providing services to underserved populations has been previously published, but not in an Arab-American population. In 2013, Rebholz et al. described the role of 4 student-run, disease-specific clinics for underserved populations in New Orleans.18 A similar program established a smoking cessation clinic in the housing insecure population of Phoenix by providing education and resources to a smoking quitline, resulting in 13.7% of patients reporting an increase in confidence, knowledge, and willingness to quit.20 Similarly, AAHAP was able to provide screening, education, and referral to Arab American patients with a goal to change health behaviors and outcomes. Student-run programs also provide health professional students with the opportunity to better understand the medical and social barriers for underserved populations seeking healthcare in the U.S. AAHAP also supported several key elements of the Accreditation Council for Pharmacy Education (ACPE) Standards 2 and 3 by teaching student pharmacists the importance of health, wellness, and population-based care as well as patient education, advocacy, communication, and cultural sensitivity.19
This study demonstrated the substantial impact that student pharmacists can make to bridge the gap in health access in Arab-American immigrants. AAHAP services aimed to address commonly noted cardiometabolic health disparities among Arab- Americans through student-directed community health screenings and education. Hypertension, diabetes, tobacco use, and cardiovascular disease continue to disproportionally affect Arab-Americans in the U.S.7 Our results align with previously published rates of 4.8-23% diabetes and 13.4% of hypertension.8,9 The success of the program was measured primarily by the over 900 patients who participated and secondarily by the referrals made to medical care. A total of 20% of patients screened were referred for additional medical attention due to uncontrolled BP and BG values. Maintaining sustainable care for vulnerable populations depends on collaborating with others who value and support a program’s mission. Partnership with organizations like CCN allowed patients to receive additional care from a team of physicians, specialists, pharmacies, and home-health agencies they otherwise would have been unaware of had they not taken part in the screenings. By focusing on community-based services, the program targeted healthcare access gaps in the Arab-American community.
While not formally evaluated with qualitative analyses, student pharmacists were surveyed after participating in the program. A total of 40 students provided feedback, reflection, and valuable insights about the program. Twenty-two (55%) who participated in previous screenings and 18 (45%) who had never participated in a previous health screening answered the survey. One student stated, “This put me outside my comfort zone but it was a rewarding experience to work with patients who are from a culturally different background then myself.” Another noted, “I’m glad I got the chance to apply my cultural care skills, like addressing health literacy with a non-native English speaker, which we don’t often get to do in our classes at school.” Among those who had never participated in similar events (n=18), students were most encouraged to take part in AAHAP and become more engaged in their local community (40%) and improve their cross-cultural clinical skills (20%). Students who had already participated in previous screenings (n=22) felt they improved their technique measuring BG and BP (41%), counseling skills (9%), and providing culturally sensitive care to individuals from the Arab-American community (50%). Hesitations students had to participate in AAHAP often stemmed from the possibility of a language barrier (40%), lack of prior experience with community health outreach (18%), and lack of free time outside of school or work obligations (23%). Following the first screening event, the number of student pharmacists increased in number. Student pharmacists also reported that utilization of the Kleinman cross-cultural interview questions often revealed beliefs that may be more common in the Arab-American community. For example, in response to the question, “what do you call your diabetes?” a patient replied, “I call it my sugar.” When asked, “what kind of treatment do you need for your blood pressure?” another responded, “I need to pray more for Allah to help me stay healthy.” And in response to, “what kind of treatment do you need for your diabetes?” another said, “I need to eat more walnuts and not eat desserts.”
Even though approximately half of the student pharmacists identified as Arab-Americans, they were still exposed to a community of patients with differing views on healthcare than their own, as there are subcultural differences across the Arab world. This allowed for an expansion in their worldview. In addition to providing students with hands-on cultural encounters, it promoted their cultural knowledge and understanding of the impact of social determinants of health impacting the Arab-American communities in a metropolitan area. Via culturally sensitive interviews, students became acquainted with behaviors, places of work, educational influences, and environmental barriers. This enabled them to provide comprehensive, appropriate assessments and recommendations. A future goal is to complete a more comprehensive qualitative study of student involvement in the program.
AAHAP came with limitations to the program itself and evaluation of the program. While several of the student pharmacist volunteers were able to communicate with patients in Arabic, which provided an advantage to building trust and rapport with Arab-American patients, there was no formal medical interpreter on site. A future step would be to include use of interpreters and to track the frequency of using linguistic interpreters at each event. Limitation to how the program was evaluated included that student pharmacists may not have documented all pertinent information, including demographics and social and medical history for each patient encounter, resulting in incomplete data collection and exclusion from analysis. This also limited the evaluation of components to a patient’s history that would contribute to their BP, BG, or BMI to be above goal. Another future step is to ask patients if they have attended a previous AAHAP health screening during the initial interview, to assess the impact of referrals on patient health outcomes and after each screening event. By adding this interview question, we ensure patient confidentiality and still keep patient data unidentified. Furthermore, since the health screening events are open to all community members to participate in, we did not formally track who self-identified as Arab.
The student-led program described is still in existence. There has been increased interest by pharmacists to serve as supervising preceptors for AAHAP health screening events. Additional non-profit health organizations in the Chicago area have been approached to discuss further outreach into different Arab-American communities and provide further volunteer opportunities for student pharmacists as part of co-curricular training. Based on these changes, a future goal is to formally measure sustainability of the program by tracking influx of patients, student volunteers, and pharmacist preceptors. In addition, further expansion of community partnerships and funding for screening supplies are needed to produce lasting health outcomes in the Arab American community that is being served.
Conclusion
Student pharmacists can be drivers for health access through community health programs for ethnically-minoritized populations. Development of a health awareness program focused on previously documented health disparities seen in Arab Americans has provided student pharmacists with opportunities to deliver culturally-sensitive care and medical referral services to an underserved community.
The opinions expressed in this paper are those of the author(s).
Acknowledgments
Acknowledgement: “The authors would like to acknowledge Milena Murray, PharmD, MSc, BCIDP, AAHIVP, FCCP, Associate Professor of Pharmacy Practice, Midwestern University College of Pharmacy (Downers Grove) for her support in statistical analyses and manuscript review”
Funding: Supplies for health screening services were provided by a grant from the American Heart Association.
Conflicts of Interest: We declare no conflicts of interest or financial interests that the authors or members of their immediate families have in any product or service discussed in the manuscript, including grants (pending or received), employment, gifts, stock holdings or options, honoraria, consultancies, expert testimony, patents, and royalties.
REFERENCES
- 1.Sastre L, Haldeman L. Environmental, Nutrition and Health Issues in a US Refugee Resettlement Community. MEDICC Rev. Oct 2015;17(4):18–24. doi:10.37757/MR2015.V17.N4.5 [DOI] [PubMed] [Google Scholar]
- 2.Morris MD, Popper ST, Rodwell TC, Brodine SK, Brouwer KC. Healthcare barriers of refugees post-resettlement. J Community Health. Dec 2009;34(6):529–38. doi:10.1007/s10900-009-9175-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prescott GM, Dascanio SA, Klosko R, Shogan M. Development of a medication health literacy program for refugees. J Am Pharm Assoc (2003). Nov - Dec 2018;58(6):673–678. doi:10.1016/j.japh.2018.08.009 [DOI] [PubMed] [Google Scholar]
- 4. Prevention CfDCa. Immigrant, Refugee, and Migrant Health. cdc.gov/immigrantrefugeehealth/
- 5.Mokdad AH, Forouzanfar MH, Daoud F, et al. Health in times of uncertainty in the eastern Mediterranean region, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Glob Health. Oct 2016;4(10):e704–13. doi:10.1016/S2214-109X(16)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yosef AR. Health beliefs, practice, and priorities for health care of Arab Muslims in the United States. J Transcult Nurs. Jul 2008;19(3):284–91. doi:10.1177/1043659608317450 [DOI] [PubMed] [Google Scholar]
- 7.Abuelezam NN, El-Sayed AM, Galea S. The Health of Arab Americans in the United States: An Updated Comprehensive Literature Review. Front Public Health. 2018;6:262. doi:10.3389/fpubh.2018.00262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jaber LA, Brown MB, Hammad A, et al. Epidemiology of diabetes among Arab Americans. Diabetes Care. Feb 2003;26(2):308–13. doi:10.2337/diacare.26.2.308 [DOI] [PubMed] [Google Scholar]
- 9.Dallo FJ, Borrell LN. Self-reported diabetes and hypertension among Arab Americans in the United States. Ethn Dis. Summer 2006;16(3):699–705. [PubMed] [Google Scholar]
- 10.Elmubarak E, Bromfield E, Bovell-Benjamin AC. Focused interviews with Sudanese Americans: perceptions about diet, nutrition, and cancer. Prev Med. May 2005;40(5):502–9. doi:10.1016/j.ypmed.2004.09.021 [DOI] [PubMed] [Google Scholar]
- 11.Vicini FA, Shah C, Wallace M, et al. Strategies for reducing cancer incidence and mortality in African American and Arab American and Chaldean communities in the Detroit metropolitan area. Am J Clin Oncol. Aug 2012;35(4):316–21. doi:10.1097/COC.0b013e318210f9b5 [DOI] [PubMed] [Google Scholar]
- 12.Weinstein JN, Geller A, Negussie Y, Baciu A, National Academies of Sciences Engineering and Medicine (U.S.). Committee on Community-Based Solutions to Promote Health Equity in the United States. Communities in action : pathways to health equity. The National Academies Press; 2017:xxiv, 557 pages. [PubMed] [Google Scholar]
- 13.Berlin EA, Fowkes WC, Jr. A teaching framework for cross-cultural health care. Application in family practice. West J Med. Dec 1983;139(6):934–8. [PMC free article] [PubMed] [Google Scholar]
- 14.Egan G. The skilled helper : a problem-management and opportunity-development approach to helping. 10th ed. Brooks/Cole, Cengage Learning; 2014:xv, 464 p. [Google Scholar]
- 15.Kleinman A, Eisenberg L, Culture Good B., illness, and care: clinical lessons from anthropologic and cross-cultural research. Ann Intern Med. Feb 1978;88(2):251–8. doi:10.7326/0003-4819-88-2-251 [DOI] [PubMed] [Google Scholar]
- 16.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. Feb 5 2014;311(5):507–20. doi:10.1001/jama.2013.284427 [DOI] [PubMed] [Google Scholar]
- 17.Garber AJ, Handelsman Y, Grunberger G, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm - 2020 Executive Summary. Endocr Pract. Jan 2020;26(1):107–139. doi:10.4158/CS-2019-0472 [DOI] [PubMed] [Google Scholar]
- 18.Rebholz CM, Macomber MW, Althoff MD, et al. Integrated models of education and service involving community-based health care for underserved populations: Tulane student-run free clinics. South Med J. Mar 2013;106(3):217–23. doi:10.1097/SMJ.0b013e318287fe9a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Education ACfP. Accreditation standards and key elements for the professional program in pharmacy leading to the doctor of pharmacy degree. Chicago, Illinois: Accreditation Counsel for Pharmacy Education; 2015. [Google Scholar]
- 20.Buckley K, Tsu L, Hormann S, et al. A health sciences student-run smoking cessation clinic experience within a homeless population. J Am Pharm Assoc (2003). Jan - Feb 2017;57(1):109–115 e3. doi:10.1016/j.japh.2016.09.008 [DOI] [PubMed] [Google Scholar]