Abstract
Corneal diseases are a major cause of blindness in the world. Corneal transplantation has been a cornerstone in the management of several of these advanced pathologies. This article discusses the evolution of corneal transplantation over a century, its indications, complications and briefly the various surgical techniques. Such tremendous technical improvisations from total corneal transplantation to lamellar keratoplasties have generated significant interest in the ophthalmic world and garnered momentum to the fight against blindness. Armed Forces Medical Services are also in vogue more than ever in this forward surge.
Keywords: Corneal transplantation, Descemet stripping automated endothelial keratoplasty, Deep anterior lamellar keratoplasty, Superficial anterior lamellar keratoplasty, Descemet's membrane endothelial keratoplasty
Introduction
“Netradaan mahadaan” – Donation of eye is amongst the greatest. It all started with the first attempted human corneal transplantation by Von Hippel with a rabbit cornea in 1886.1 The term “keratoplasty” was coined by Franz Reisinger and the first successful human corneal transplantation was performed by Zirm in 1905.2 Today we have reached such a stage where different layers of the 600–1200 microns thick cornea can be selectively transplanted. It is nothing short of a wonder!
There are approximately 217 million visually impaired people globally and 5 million out of them have corneal pathology. Corneal pathology is the fifth leading cause of blindness in the world following cataract, refractive error, glaucoma and age related macular degeneration.3 Corneal transplantation or keratoplasty is the replacement of the diseased cornea with a normal cornea. Keratoplasty is the most common transplant procedure done in the world annually with almost 1,85,000 surgeries, of which more than half of corneas are procured in the US and India.4 The first eye bank in India was established in 1945 at the Regional Institute of Ophthalmology, Chennai. Indian ophthalmologists perform around 15,000–30,000 surgeries per year, collating data of pre- and post COVID eras. Indian Armed Forces also contribute to this through its various State of the Art centers like Army Hospital (R & R), Armed Forces Medical college (AFMC) and various Command Hospitals. The first eye bank established in Armed Forces was at AFMC, Pune.
Corneal transplantation: evolution
Twentieth and twenty first centuries saw paradigm shift in the field of corneal transplantation. After Zirm did total corneal transplantation,2 Fuch tried lamellar keratoplasty though the success rate was debatable.5 Overtime, the techniques got refined further with the advent of various micro surgical devices and even LASER techniques to reach today's repute. The Indian Armed Forces Medical Services also keep abreast with the most advanced technologies available in its apex institutes.
Indications and types of corneal transplantation
Cornea has six layers; the epithelium, Bowman's membrane, stroma, Dua's layer, Descemet's Membrane (DM) and the endothelium. The pathologies may affect these layers separately or as a whole. Common indications of corneal transplantation include infectious keratitis, corneal degenerations and dystrophies, re-grafts, bullous keratopathy, keratoconus and ectasias, chemical injuries and mechanical traumas, various endotheliopathies, etc. As per indications, Keratoplasties can be classified into therapeutic, tectonic, optical or cosmetic. Therapeutic penetrating keratoplasty (PKs) are done in unsalvageable infected corneas, tectonic to maintain global integrity, eg. corneal perforations or melts and optical to restore optimum vision as in cases like keratoconus. Cosmetic procedures may be done to remove visible scars.
As per thickness, it can be divided into total penetrating keratoplasty (TPK) and Lamellar Keratoplasty (LK). TPK involves transplantation of full thickness cornea.
Total penetrating keratoplasty (TPK)
It is the most common type of keratoplasty where a full thickness cornea is transplanted. The surgical technique involves assessing the donor corneal extent of damage secondary to any pathology and careful excision to open sky followed by removing the adhesions and meticulously preserving the iridocorneal angle structures. The donor cornea is then trephined and sutured to the host cornea. Absolute indication of TPK is therapeutic PK due to severe infectious keratitis or corneal melt. Since it is an open sky procedure, the chances of expulsive haemorrhage and choroidal effusion is higher compared to lamellar procedures. Other complications of the procedure include suture related issues, primary graft failure, graft rejection, persistent epithelial defect microbial keratitis, astigmatism, recurrence of the original pathology etc.
In primary graft failure, the grafted cornea has been oedematous since the surgery and has never been clear. Secondary failure is due to graft rejection. Graft rejection in TPK can be epithelial, stromal and endothelial. It is described as an immune mediated process where a corneal graft, which has been clear for at least two weeks, becomes oedematous with signs of inflammation.6, 7, 8, 9 Epithelial rejection is characterised by formation of epithelial rejection line from graft host junction. Anterior chamber inflammation is minimal. It responds well to topical steroid therapy. Stromal rejection can be acute and chronic. Both types will show subepithelial and stromal infiltrates and stromal oedema. The oedema and patchy infiltrates are more pronounced in acute rejection along with limbal vascular reaction. Stromal inflammation may be followed by vascularization of stroma, which will augment the process further. Sometimes the stromal picture may mimic corneal abscess too. Stromal rejection may need systemic steroids in addition to topical therapy based on severity. Endothelial rejection is characterised by formation of khodadoust inflammation line in the endothelium from the graft host junction, corneal edema, keratic precipitates and anterior chamber reaction. It is the most severe complication and consists of almost 50%–70% of all rejections. Treatment includes IV pulse steroid methyl prednisolone 500 mg along with oral and topical steroid follow up. There can be combined types of rejections beyond these types. The rejection in cases of multiple grafts poses a challenge to treat as the typical features cease to be evident in such cases.6,10, 11, 12 Other immunosuppressive agents include azathioprine, calcineurin inhibitors like cyclosporine A and tacrolimus, rapamycin, mycophenolate mofetil etc. Preventive administration of intrastromal anti-VEGF agents like 5 mg of 0.2 ml bevacizumab has been described for vascularised host corneas to prevent the incidence of rejection.13 Newer treatment modalities are being developed through bio engineering and gene therapy.14
Lamellar keratoplasty (LK)
In Lamellar keratoplasty (LK), the diseased partial or lamellar cornea is removed and transplanted. The obvious benefits include reduced intraoperative open sky related complications like expulsive haemorrhage and endophthalmitis, maintenance of basic structural integrity, reduced rejection probability, effective use of a single cornea and early patient recovery. It is divided into anterior and posterior LK.
Anterior lamellar keratoplasty (ALK) can be superficial (SALK) and deep (DALK). Indications include anterior stromal scars due to healed infections, trauma, dystrophies, previous surgeries etc. SALK is used in treating corneal scars or opacities involving anterior 30%–40%of the corneal thickness. Various surgical methods to achieve anterior dissection are manual, microkeratome assisted and femtosecond laser. Barraquer introduced microkeratome in 1964 initially to treat high refractive errors. Later it was modified by Kauffman et al. for ALK.15, 16, 17, 18 The microkeratome is used to excise the anterior lamella of the host cornea and similarly excised donor corneal lamella is sutured or glued to the host cornea. It is also referred to as automated anterior lamellar keratoplasty. Femtosecond laser can similarly be used for fine dissection and sutureless ALK (FALK). It is the most advanced technique, which is also available at centres like Army Hosp (R&R). Modified FALK techniques-mid stromal, with more than 250 microns of posterior residual corneal bed thickness and pre-descemet, with 50 microns of residual thickness are also described by Bonafidini et al. using Zeimer femtosecond laser.15,19
DALK is performed when the deep corneal stroma is involved and the endothelial function is good thereby removing the corneal stroma in total or near total levels.20 The dissection can be thus descemetic or pre-descemetic. Descemet DALK is done with total removal of corneal stroma leaving behind a healthy Descemet's membrane and endothelium whereas pre-descemet is performed in thinner corneas leaving behind a minimal corneal stromal bed to prevent perforations. The different surgical techniques employed in DALK include: (i) direct open dissection described in 1976 by Anwar21 (ii) Hydro-delamination by Sugita et al. in 1997, which involves intrastromal fluid injection and seperation22 (iii) Melle's closed dissection technique described in 1999, which involves aqueous-air exchange and corneal dissection using a specially designed spatula23 (iv) Anwar's Big Bubble technique described in 2002. The trephined host cornea is dissected till 70%–80%of stroma. An air bubble is injected para centrally using a 27 or 30G needle to form a big bubble, which causes the lamellar separation and this space is further dissected and replaced by donor cornea without DM. 3 types of big bubbles (BB) are described. Type 1 where Dua's layer is separated from stroma by the bubble. This is more stable, common and preferred for DALK. Type 2 BB separates dua's layer from descemet's membrane and is less stable and has more chances of perforation. Type 3 is a mixture of both.24,25 (v) Femtosecond laser trephination of cornea initially followed by Big Bubble technique. It causes lesser post op astigmatism and better wound strength.26, 27, 28
Complications of ALK
Common complications in SALK are interface haze, dry eyes, post op astigmatism, epithelial ingrowth, recurrence of the pathology etc. Graft failure due to immunologic rejection is rare in SALK compared to DALK where graft rejection occurs and is characterised by stromal haze, oedema, infiltrates with or without neovascularisation. It can be treated by prompt identification and topical steroid therapy. Other complication is DM perforation in DALK. Rest are similar to SALK. A rare complication reported in DALK is Urrets–Zavalia syndrome where the pupil gets fixed and dilated. Later adhesions may form with lens capsule. Glaucoma and iris atrophy may ensue with or without lenticular opacities.29,30
Posterior lamellar keratoplasties (PLK)
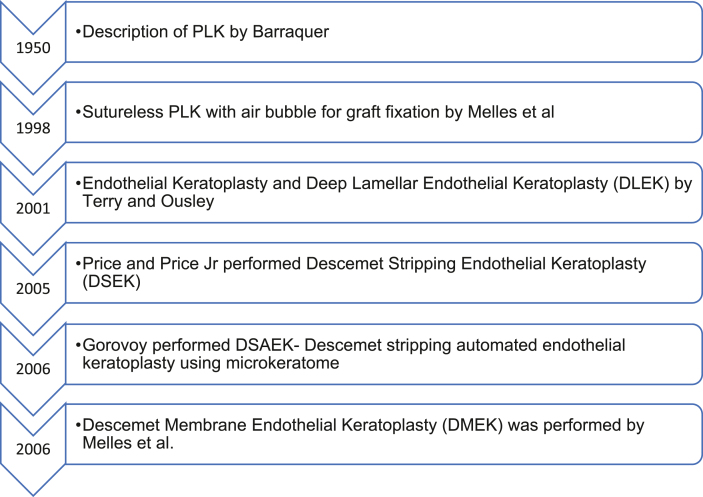
Posterior lamellar keratoplasty is performed by transplanting the posterior lamella- DM and endothelium of the cornea (Fig. 1). Indications of the surgery are endothelial disorders like Fuch's endothelial dystrophy, Bullous keratopathy, Congenital hereditary endothelial dystrophy, posterior polymorphous corneal dystrophy, iridocorneal endothelial syndrome, etc. The evolution of PLK is given below in (Figs. 2 and 3).15,31, 32, 33, 34, 35
Fig. 1.
Preoperative and postoperative photographs of different types of corneal transplants.
Fig. 2.
Types of keratoplasty.
Fig. 3.
Evolution of posterior lamellar keratoplasty.
Descemet stripping endothelial keratoplasty (DSEK)
As the name suggests, DM and endothelium of about 8 mm of the recipient is stripped first using a reverse Sinsky hook through limbal or corneoscleral incisions. This process is called “descemetorhexis.” Following which the dissected donor posterior corneal lamella is inserted into the host eye and stabilized with the help of an air bubble. The donor cornea can be dissected manually, with a microkeratome (DSAEK) or with femtosecond laser. Nowadays, precut donor tissues are also available. The donor tissue has a minimal deep stromal bed along with DM and endothelium (about 150 microns) in DSEK/DSAEK. Almost a similar technique to descemetorhexis was described in the works of a French ophthalmologist named Louis Paufique in the1950's. Complications of DSEK/DSAEK include graft dislocation (most common), primary graft failure, graft rejection, pupillary block glaucoma due to the air bubble, infections, epithelial ingrowth, endophthalmitis etc.
Descemet's membrane endothelial keratoplasty (DMEK)
DMEK is a modified EK performed by Melles et al. by using a thinner graft of about 10–15 microns. Here the donor corneal DM is removed with forceps and trephination after stained with 0.06% trypan blue. Later procedures are similar to DSEK. The graft is injected to the host eye through intraocular injectors or specialized Melles glass injector after removing the host DM.31 The donor DM is further unfolded and then air bubble is introduced to stabilize the graft. Complications include graft dislocation, graft failure, post op glaucoma etc. The incidence of complications are lesser compared to DSAEK.
Compared to DSAEK, DMEK has superior visual outcome and early patient recovery at 6 months evaluation. The endothelial density also is found to be better compared to DSAEK. The minor hyperopic shift is about +0.74D compared to +1-1.5D in DSAEK. The incidence of graft failure and dislocation is also lesser. Post op glaucoma rates are also lesser.36, 37, 38
TPK vs LK
The trends are changing with the advantages of LK. LK avoids the ill effects of open sky procedures as described above. The post op recovery of patients are faster along with lesser post op astigmatism and faster visual rehabilitation. The chances of rejection are less with LK; DMEK having the least. Further a single cornea can be used in multiple patients with various levels of pathologies in LK whereas in TPK a single cornea is entirely used in one patient. In sutureless LKs, the complications related to sutures are also avoided. Post op glaucoma and adhesions are also less compared to TPK. The availability of precut cornea for LK is also a motivating factor for surgeons.39, 40, 41
Recent advances and future
As of now, DMEK is considered the gold standard in EK. There are newer techniques tried like descemet's membrane stripping only (DSO) or descemetorhexis without endothelial keratoplasty (DWEK) where the host descemtorrhexis is done without placing a graft. But it is used in only mild cases of Fuch's endotheliopathy, as healthy peripheral endothelial cells are required to migrate centrally for a successful procedure. There are attempts to combine the procedure with rho kinase inhibitors. Rho kinase inhibitors have profound pro endothelial properties for which they are used in nascent research activities in the field of intracameral endothelial cell injection therapies.42 A similar alteration is employed in descemet's membrane endothelial transfer (DMET). The donor draft is introduced into anterior chamber after host DM removal but is left detached and floating. The host cornea gradually clears over 3 months to optimum clarity in DMET. Other tissue-saving alterations are Quarter and Hemi DMEK, where one cornea can be used in four and two recipients, respectively. In quarter- DMEK, four pie shaped DM endothelial grafts are prepared from single host tissue and in hemi- DMEK, two semi circular grafts from a single donor cornea.
N-DSEK is another modification where no host DM stripping is done prior to insertion of donor lamella. Ultra-thin DSAEK (UT DSAEK) is a new technique where thickness of the graft (less then 100 microns) is more than DMEK (10–15 microns) but less than DSAEK (150 microns). DMEK- S is a hybrid technique, which combines the lamellar properties of DSAEK and DMEK. The thicker periphery of the graft has the deep stroma, DM and endothelium similar to DSAEK and thinner central part only has DM like that of DMEK, thus DMEK- S (peripheral Stromal Support).
Another spin in keratoplasty was the application of femtosecond laser in transplant procedures. It can be used for both TPK and LK. The accurate honed and smooth cuts with precision in donor and host corneas made the graft host alignment flawless leading to reduced astigmatism, wound leaks and better healing. The chances of eccentric grafts are also less. The better graft host apposition strengthens the recovery and reduces the chances of dehiscence besides minimizing the loss of endothelium during the surgery. While microkeratome can be used to dissect out a pre-determined depth of the tissue (like in M-DMEK), femtosecond can be used to modify the depths of incision and dissection during the surgery, which led to revamping techniques like femtosecond laser enabled descemetorrhexis DMEK or FE DMEK.19,27,28,43 Recent development is femtosecond and excimer laser- assisted endothelial keratoplasty (FELEK) where excimer photoablation is also used for refinement of donor-recipient corneal interface.
The arrival of intra-operative optical coherence tomography (iOCT) has again been a boon. iOCT helps in the intraoperative accurate measurement of corneal thickness of host and donor corneas and assessment of opacities. It is also useful to gauge the planes of dissection and thus control the procedures precisely and thereby reducing complications like eccentric dissection and DM perforation. In PLKs, the real time apposition can be evaluated and adjusted accordingly. The overall visual recovery is positively impacted with the use of iOCT.18,44
Bioengineered corneal implantation is a neoteric development. The Nature journal has published an article in August 2022 by Rafat et al. regarding the implantation of bioengineered corneal tissue for advanced keratoconus patients.45 They described the tissue as “cell-free engineered corneal tissue, bioengineered porcine construct, double crosslinked” or BPCDX, in a minimally invasive technique to implant it. The pilot studies were conducted in India and Iran in 20 patients of advanced keratoconus and found significant improvement in visual acuity, corneal thickness and keratometric values. The study also claims the procedure to be simpler than donor corneal transplantation. The corneal implant was developed from medical grade purified type I porcine collagen, which is double linked. No viable biological material including cells are present in BPCDX but it mimics properties of natural human cornea. The surgical technique requires creation of an intrastromal pocket and placing the implant without any sutures.
Challenges
The procurement of cornea itself is a major challenge. The transplant volunteers are much less compared to the demand of corneas. The government, National Eye Bank, Eye Bank Association of India and many NGOs are all in the forefront to motivate people and spread awareness. Measures to bridge the gap may include educating the public through effective use of social media, intense participation of medical and paramedical staff including students, campaigns with more counselors and involvement of religious leaders and social activists in such campaigns. Sometimes the socio-cultural environment itself is the challenge. Worthwhile positive legal actions include reintroduction of cornea as a tissue rather than an organ through the Gazette notification of “Transplantation of Human Organs and Tissues Rules” in 2014 and the introduction of “Hospital Cornea Retrieval Programme” (HRCP). These have markedly increased the donor cornea availability and cornea counselors, though still inadequate.18
Conclusion
Corneal transplantation has come a long way since its inception. The research and advent of new technology has advanced the pace of its improvisation and techniques. Global media has made it possible to share such phenomenal developments and knowledge thus augmenting the fight against blindness. The Indian Armed Forces Medical Services also is a proud partaker thus helping people to the door of vision. And finally “Tamasoma jyothirgamaya”; lets walk towards the light of vision from darkness.
Disclosure of competing interest
All authors have none to declare.
References
- 1.Von Hippel A. Eine neue methode der hornhauttransplantation. Arch Ophthalmol. 1888;34:108–130. [Google Scholar]
- 2.Zirm E.K. Eine erfolgreiche totale Keratoplastik (A successful total keratoplasty) Refract Corneal Surg. 1989;5:258–261. 1906. [PubMed] [Google Scholar]
- 3.Mathews P.M., Lindsley K., Aldave A.J., Akpek E.K. Etiology of global corneal blindness and current practices of corneal transplantation: a focused review. Cornea. 2018;37(9):1198–1203. doi: 10.1097/ICO.0000000000001666. [DOI] [PubMed] [Google Scholar]
- 4.Gain P., Jullienne R., He Z., et al. Global survey of corneal transplantation and eye banking. JAMA Ophthalmol. 2016 Feb;134(2):167–173. doi: 10.1001/jamaophthalmol.2015.4776. [DOI] [PubMed] [Google Scholar]
- 5.Trevor Roper P.D. In: Corneal Grafting. Casey T.A., editor. Butterwork; London: 1972. The history of corneal grafting; pp. 1–5. [Google Scholar]
- 6.Panda A., Vanathi M., Kumar A., Dash Y., Priya S. Corneal graft rejection. Surv Ophthalmol. 2007;52(4):375–396. doi: 10.1016/j.survophthal.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 7.Koay P.Y., Lee W.H., Figueiredo F.C., et al. Opinions on risk factors and management of corneal graft rejection in the United Kingdom. Cornea. 2005;24:292–296. doi: 10.1097/01.ico.0000138841.44926.f8. [DOI] [PubMed] [Google Scholar]
- 8.Miedziak A.I., Tambasco F.P., Lucas-Glass T.C., et al. Evaluation of triggers for corneal graft rejection. Ophthalmic Surg Laser. 1999;30:133–139. [PubMed] [Google Scholar]
- 9.Prendergast D.G., Easty D.L. Immunological aspects of corneal graft rejection. Immunol Lett. 1991;29:73–76. doi: 10.1016/0165-2478(91)90203-m. [DOI] [PubMed] [Google Scholar]
- 10.Teichmann K.D. Randomised controlled trial of corticosteroid regimens in endothelial corneal allograft rejection. Br J Ophthalmol. 2000;84:1083. doi: 10.1136/bjo.84.9.1083a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khodadoust A.A., Silverstein A.M. Transplantation and rejection of individual cell layers of the cornea. Invest Ophthalmol. 1969;8:180–195. [PubMed] [Google Scholar]
- 12.Shapiro M.B., Mandel M.R., Krachmer J.H. In: Corneal Surgery, Theory, Technique and Tissues. ed 2. Bright B., editor. CV Mosby Company; St Louis: 1997. Rejection; pp. 254–268. [Google Scholar]
- 13.Fasciani R., Mosca L., Giannico M.I., Ambrogio S.A., Balestrazzi E. Subconjunctival and/or intrastromal bevacizumab injections as preconditioning therapy to promote corneal graft survival. Int Ophthalmol. 2014;35(2):221–227. doi: 10.1007/s10792-014-9938-4. [DOI] [PubMed] [Google Scholar]
- 14.Ma D., Mellon J., Niederkorn J.Y. Oral immunisation as a strategy for enhancing corneal allograft survival. Br J Ophthalmol. 1997;81:778–784. doi: 10.1136/bjo.81.9.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Espandar L., Carlson A.N. Lamellar keratoplasty: a literature review. J Ophthalmol. 2013;2013 doi: 10.1155/2013/894319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barraquer J.I. Lamellar keratoplasty. (Special techniques) Ann Ophthalmol. 1972;4:437–469. [PubMed] [Google Scholar]
- 17.Kaufman H.E., Insler M.S., Ibrahim-Elzembely H.A., Kaufman S.C. Human fibrin tissue adhesive for sutureless lamellar keratoplasty and scleral patch adhesion: a pilot study. Ophthalmology. 2003;110:2168–2172. doi: 10.1016/S0161-6420(03)00832-7. [DOI] [PubMed] [Google Scholar]
- 18.Singh R., Gupta N., Vanathi M., Tandon R. Corneal transplantation in the modern era. Indian J Med Res. 2019 Jul;150(1):7–22. doi: 10.4103/ijmr.IJMR_141_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bonfadini G., Moreira H., Jun A.S., et al. Modified femtosecond laser-assisted autureless anterior lamellar keratoplasty. Cornea. 2013;32(4):533–537. doi: 10.1097/ICO.0b013e31826e828c. [DOI] [PubMed] [Google Scholar]
- 20.Pannu A., Sati A., Mishra S.K. An inadvertent usage of the deep stromal lenticule in anterior lamellar keratoplasty - an emancipator technique. Indian J Ophthalmol. 2022 Sep;70(9):3409–3411. doi: 10.4103/ijo.IJO_190_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anwar M. Dissection technique in lamellar keratoplasty. Br J Ophthalmol. 1972;56(9):711–713. doi: 10.1136/bjo.56.9.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sugita J., Kondo J. Deep lamellar keratoplasty with com- plete removal of pathological stroma for vision improvement. Br J Ophthalmol. 1997;81(3):184–188. doi: 10.1136/bjo.81.3.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Melles G.R., Rietveld F.J.R., Beekhuis W.H., Binder andP.S. A technique to visualize corneal incision and lamellar dissection depth during surgery. Cornea. 1999;18(1):80–86. [PubMed] [Google Scholar]
- 24.Dua H.S., Katamish T., Said D.G., Faraj L.A. Differentiating type 1 from type 2 big bubbles in deep anterior lamellar keratoplasty. Clin Ophthalmol. 2015 Jun 26;9:1155–1157. doi: 10.2147/OPTH.S81089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anwar M., Teichmann K.D. Deep lamellar keratoplasty: surgical techniques for anterior lamellar keratoplasty with and without baring of Descemet's membrane. Cornea. 2002;21(4):374–383. doi: 10.1097/00003226-200205000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Suwan-Apichon O., Reyes J.M., Griffin N.B., Barker J., Gore P., Chuck R.S. Microkeratome versus femtosecond laser predissection of corneal grafts for anterior and posterior lamellar keratoplasty. Cornea. 2006;25(8):966–968. doi: 10.1097/01.ico.0000226360.34301.29. [DOI] [PubMed] [Google Scholar]
- 27.Price F.W., Jr., Price M.O., Grandin J.C., Kwon R. Deep anterior lamellar keratoplasty with femtosecond-laser zigzag incisions. J Cataract Refract Surg. 2009;35(5):804–808. doi: 10.1016/j.jcrs.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 28.Farid M., Steinert R.F. Deep anterior lamellar keratoplasty performed with the femtosecond laser zigzag incision for the treatment of stromal corneal pathology and ectatic disease. J Cataract Refract Surg. 2007;35(5):809–813. doi: 10.1016/j.jcrs.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 29.Olson E.A., Tu E.Y., Basti S. Stromal rejection following deep anterior lamellar keratoplasty: implications for postoper- ative care. Cornea. 2012;31(9):969–973. doi: 10.1097/ICO.0b013e31823f8a99. [DOI] [PubMed] [Google Scholar]
- 30.Maurino V., Allan B.D., Stevens J.D., Tuft S.J. Fixed dilated pupil (urrets-zavalia syndrome) after air/gas injection after deep lamellar keratoplasty for keratoconus. Am J Ophthalmol. 2002;133(2):266–268. doi: 10.1016/s0002-9394(01)01308-3. [DOI] [PubMed] [Google Scholar]
- 31.Melles G.R., Eggink F.A., Landeretal F. A surgical technique for posterior lameliar keratoplasty. Cornea. 1998;17(6):618–626. doi: 10.1097/00003226-199811000-00010. [DOI] [PubMed] [Google Scholar]
- 32.Terry M.A., Ousley P.J. Deep lamellar endothelial keratoplasty in the first United States patients. Cornea. 2001;20(3):239–243. doi: 10.1097/00003226-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 33.Price F.W., Jr., Price M.O. Descemet's stripping with endothelial keratoplasty in 50 eyes: a refractive neutral corneal transplant. J Refract Surg. 2005;21(4):339–345. doi: 10.3928/1081-597X-20050701-07. [DOI] [PubMed] [Google Scholar]
- 34.Gorovoy M.S. Descemet-stripping automated endothelial keratoplasty. Cornea. 2006;25(8):886–889. doi: 10.1097/01.ico.0000214224.90743.01. [DOI] [PubMed] [Google Scholar]
- 35.Melles G.R., Ong T.S., Ververs B., van der Wees J. Descemet membrane endothelial keratoplasty (DMEK) Cornea. 2006;25(8):987–990. doi: 10.1097/01.ico.0000248385.16896.34. [DOI] [PubMed] [Google Scholar]
- 36.Tourtas T., Laaser K., Bachmann B.O., Cursiefen C., Kruse F.E. Descemet membrane endothelial keratoplasty versus Descemet stripping automated endothelial keratoplasty. Am J Ophthalmol. 2016;153(6):1082–1090.e2. doi: 10.1016/j.ajo.2011.12.012. [DOI] [PubMed] [Google Scholar]
- 37.Guerra F.P., Anshu A., Price M.O., Price andF.W. Endothelial keratoplasty: fellow eyes comparison of Descemet stripping automated endothelial keratoplasty and Descemet membrane endothelial keratoplasty. Cornea. 2011;30(12):1382–1386. doi: 10.1097/ICO.0b013e31821ddd25. [DOI] [PubMed] [Google Scholar]
- 38.Parker J., Dirisamer M., Naveiras M., et al. Outcomes of Descemet membrane endothelial keratoplasty in phakic eyes. J Cataract Refract Surg. 2012;38(5):871–877. doi: 10.1016/j.jcrs.2011.11.038. [DOI] [PubMed] [Google Scholar]
- 39.Röck T., Landenberger J., Bramkamp M., Bartz-Schmidt K.U., Röck D. The evolution of corneal transplantation. Ann Transplant. 2017;22:749–754. doi: 10.12659/AOT.905498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang A.Q., Rubenstein D., Price A.J., et al. Evolving surgical techniques of and indications for corneal transplantation in Ontario: 2000-2012. Can J Ophthalmol. 2013;48:153–159. doi: 10.1016/j.jcjo.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 41.Zare M., Javadi M.A., Einollahi B., et al. Changing indications and surgical techniques for corneal transplantation between 2004 and 2009 at a tertiary referral center. Middle East Afr J Ophthalmol. 2012;19:323–329. doi: 10.4103/0974-9233.97941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kinoshita S., Koizumi N., Ueno M., et al. Injection of cultured cells with a ROCK inhibitor for bullous keratopathy. N Engl J Med. 2018;378:995–1003. doi: 10.1056/NEJMoa1712770. [DOI] [PubMed] [Google Scholar]
- 43.Shousha M.A., Yoo S.H., Kymionis G.D., et al. Long-term results of femtosecond laser-assisted sutureless anterior lamellar keratoplasty. Ophthalmology. 2011;118:315–323. doi: 10.1016/j.ophtha.2010.06.037. [DOI] [PubMed] [Google Scholar]
- 44.Juthani V.V., Goshe J.M., Srivastava S.K., Ehlers J.P. Association between transient interface fluid on intraoperative OCT and textural interface opacity after DSAEK surgery in the PIONEER study. Cornea. 2014;33:887–892. doi: 10.1097/ICO.0000000000000209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rafat M., Jabbarvand M., Sharma N., et al. Bioengineered corneal tissue for minimally invasive vision restoration in advanced keratoconus in two clinical cohorts. Nat Biotechnol. 2023;41:70–81. doi: 10.1038/s41587-022-01408-w. [DOI] [PMC free article] [PubMed] [Google Scholar]