Abstract
The Journey of kidney transplantation began a century ago with animal experiments and xenotransplants. The initial attempts of human to human kidney transplant were made by Yuri Voronoy, Jean Hamburger and several others between 1930 and 40s, but most of these were unsuccessful. The first successful live related kidney transplant between identical twins was performed at the Brigham Hospital in Boston in December 1953, by Joseph Murray and John P. Merrill, which paved the way for future live transplants. With the gradual improvement in the understanding of immunity and tolerance, the use of immunosuppression was attempted using irradiation and steroids, which gradually evolved over the decades to include azathioprine and cyclosporine. Discoveries of human leukocyte antigen by Dausset, complement dependent cross match by Paul Terasaki, and other developments in transplant immunology improved outcomes of kidney transplant. This journey was marked by new discoveries and improvements in surgical techniques including laparoscopic and robotic transplant surgery, better and safer immunosuppression, advances in transplant immunology, advent of the concept of brain death and deceased donor transplant program, and complicated transplants like transplants in highly sensitised recipients and ABO incompatible transplants. India was not far behind the rest of the world, and after a few unsuccessful attempts, the first successful transplant was done in CMC Vellore in 1971, which was followed by advancements in kidney transplants keeping in pace with the rest of the world.
Keywords: Kidney transplant, History, Immunosuppression, Immunology, Crossmatch
Introduction
Organ transplantation has captured the imagination of mankind since ancient times. Be it the ancient Indian story of Lord Shiva transplanting the severed head of an elephant on to his son Ganesha's decapitated body and bringing him back to life, the Sphinx from the Egyptian civilization or the varied heroes and villains from Greek mythology, who were part animal and part human. All these stories of xenotransplants were usually a reference to some superhuman power endow-ed upon these people by the animal part that was attached to them.
There are several such examples in other civilizations across the world involving the use of limbs, internal organs like heart and other organs. The first written record of transplantation of a human organ to another human is the Ebers Papyrus from Egypt, which mentioned grafting of skin as a treatment of burn patients, at around 1550 BC.1 The earliest written records of such surgeries from India date to around 600 BC, when Sushruta, the father of Surgery in India, performed full-thickness skin grafts.2
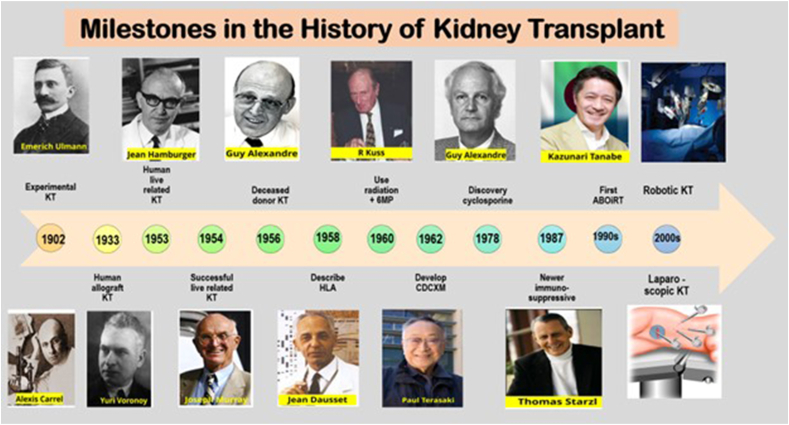
Unlike the mythological past where organ transplantation was considered a way to endow super human attributes to the recipient, organ transplantation in modern times has basically been directed towards the replacement of the function of a defective or deficient organ. Kidney transplantation has evolved over the last century. The journey which began with a few primitive animal experiments, moving on to xenotransplants, followed by attempts at human kidney transplantation, has now reached the present live related and deceased human donor transplants. Things have changed dramatically and are beginning to turn a full circle as there is new light in the xenotransplanation tunnel. This journey has been also marked by new discoveries and improvements in surgical techniques, immunosuppression, advances in transplant immunology, and many more. The important landmarks in kidney transplant are given in Fig. 1.
Fig. 1.
Milestones in the history of kidney transplant (Picture courtesy Vineet Behera).
Experimental transplants
The initial attempts to transplant a kidney began in the 19th century with many failed experiments in animals. The first successful attempt of kidney transplant was reported by Austrian doctor, Emerich Ullmann in 1902, who performed an auto-transplant in a dog, by removing the kidney from its original position and transplanting it in the neck, by anastomosing it to the neck vessels, which successfully produced urine for some time, but the animal died soon after.3 There were similar attempts in animals with variable benefit. Alexis Carrel, a surgeon from the United States, did seminal work on organ grafting by performing several kidney autografts in cats and dogs, during which he pioneered various concepts of vascular anastomoses. He received the Nobel Prize in 1912 for his path-breaking work on vascular suturing and tissue matching.4 After performing about 100 experimental kidney transplants, in 1909 Ernst Unger transplanted the kidneys from a fox terrier to a boxer dog, which worked well and produced urine for 14 days.5 These early experiments established the technical feasibility of kidney transplantation.
However, assessment of transplant function was difficult in those days as the methods of studying renal functions were primitive and there were no radiological methods to visualize the kidney within the body of the animal. These, coupled with the risk of possible episodes of rejection led to a reduced interest in organ transplantation over the next few decades. The World Wars I and II were a stagnant period in the history of modern organ transplantation, with no major advances as the focus of surgery moved towards battle injuries and blood transfusion.6
Kidney transplant in humans
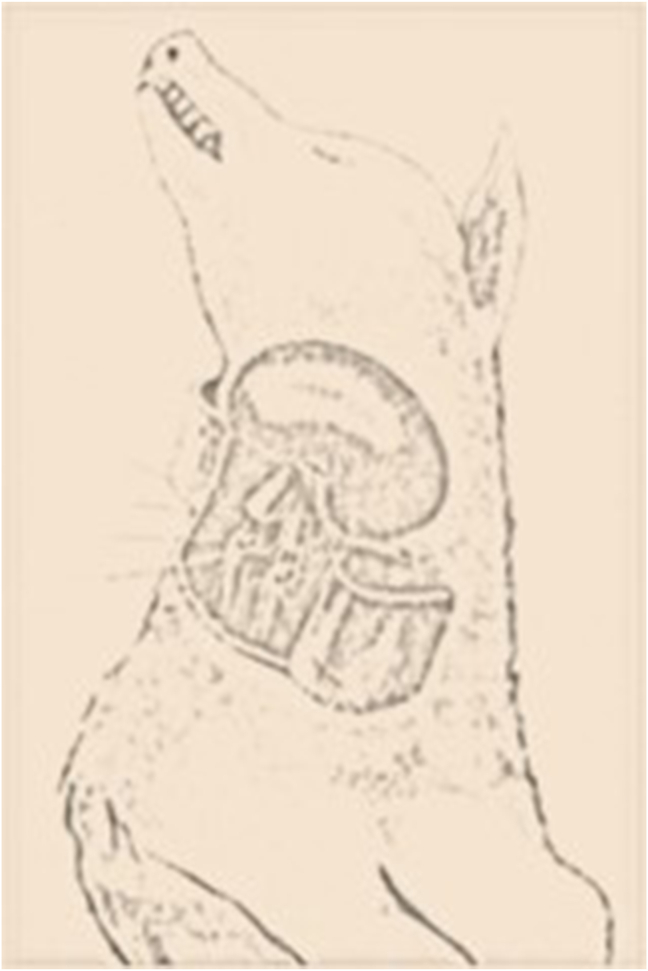
In 1933, a Ukrainian surgeon, Yuri Voronoy from the Kharkov Medical Institute in Kherson, in the erstwhile USSR, who had performed kidney transplants in dogs (Fig. 2), transplanted a human kidney from a deceased donor (blood group B) who had died due to severe head injury, to a 26 year old girl with O blood group, who suffered acute renal failure following consumption of mercuric chloride in an attempt to commit suicide.7 The donor nephrectomy was done nearly 6 h after death, and transplanted to the thigh of the recipient under local anesthesia. Though the patient showed an initial improvement in the first post operative day, the kidney never worked, and she died on the second day. Voronoy did a few similar transplants, but did not achieve substantial benefit in any.8
Fig. 2.
Schematic diagram of dog experiment like transplanting the kidney to neck vessels done by Yuri Voronoy (Picture courtesy Vineet Behera).
In 1946, Hufnagel, Hume, and Landsteiner transplanted a human allograft kidney to the arm vessels at the Peter Bent Brigham Hospital in Boston, which worked for some time, and helped the patient to recover from acute renal failure.9 This revived global interest in renal transplantation. Thereafter, Simonsen from Denmark, and Dempster from London independently found that transplanting the kidney to the pelvic position was preferable to a superficial site for transplant. They also realized that an immunologic mechanism was at play which caused the failure of these transplants.10
In 1950, a Chicago surgeon Richard Lawler, performed the first successful kidney allograft transplant in the intraabdominal position on Ms Ruth Tucker, a 44 year old lady with polycystic kidney disease, using a kidney from a deceased donor at the Mary Hospital in Illinois. The allograft functioned successfully for ten months.11 The recipient survived for five more years thereafter, finally succumbing to a cardiac event.
The first live-related kidney transplant by placing the graft kidney in the pelvic position was done in 1952 in Paris by nephrologist Jean Hamburger and his surgical team, in which a mother donated her kidney to her son who damaged his solitary kidney following a fall from height. The kidney initially functioned well, but developed acute rejection abruptly on the 22nd day.12 Similar attempts at transplant were reported from Chicago, Toronto, and Cleveland in the early 1950s, but none achieved good sustained function.
First successful live-related kidney transplant
In Boston, on December 23, 1954, the first successful transplant of a kidney from one identical twin (Ronald Herrick) to the other with renal failure (Richard Herrick) was performed at Brigham Hospital, by Joseph Murray, J. Hartwell Harrison, and John P. Merrill.13 In order to reduce the risk for rejection, the doctors first had to prove that the two were actually identical twins. This was done using fingerprinting technology and thereafter performing skin grafts. The transplant was successful and Richard Herrick lived a normal life for eight years before dying due to causes unrelated to the transplant. Joseph Murray was awarded the Nobel Prize for Medicine in 1990, for this achievement. The donor Ronald, lived a full life till the age of 79 years and died on 29 Dec 2010 of complications following cardiac surgery. This paved the way for many transplantations which were performed successfully in Boston and worldwide.
The first deceased donor transplant was performed in 1955 by Charles Rob and William James Dempster in London, but this was unsuccessful. The concept of brain death was introduced in 1959 by Guy Alexandre, a Belgian surgeon, in his work coma depasse, which could be made possible by continuing artificial ventilation allowing oxygenation to organs in patients with no brain function, thus preserving them for transplant.14 Thereafter, Fred Peter Raper performed the first successful deceased donor transplant from a “beating-heart donor” in 1959.
Tolerance
Transplant tolerance is a state of when the graft continues to function well in the absence of immunosuppressives, despite an intact immune system of the recipient. In 1945, Ray Owen did immunology studies in cattle to discover that fraternal cattle twins often had two types of red blood cell (RBC), hinting at an exchange of blood happening between them in utero. He hypothesized that the chimeric RBC could persist in adults, because of the intrauterine transfer of both RBCs and stem cells, that had perpetuated the RBCs.15 Billingham and Medawar added to this concept to state that this intra-uterine exchange of stem cells possibly occured for both RBCs and leucocytes. They felt that, this could be the possible reason for acceptance of skin grafts in these calves. They also attempted animal experiments in mice to induce chimerism and acceptance of graft by inoculating splenic cells of donor to intrauterine fetuses.16 This concept of induction of chimerism to prevent graft rejection was the foundation for present day tolerance, and Medawar was awarded the Nobel Prize in 1966 for this work.
Immunosuppression
In the initial trials of transplantation, no immunosuppression was used. David Hume realized the importance of immunological mechanisms at play and used small doses of adrenocorticotropic hormone or cortisone to obtain modest unexpected survival of the graft kidney.17 Medawar tried to suppress the immune system by using total body irradiation.18 These irradiation based regimens were risky, difficult to control and were associated with graft-versus-host disease. Schwartz and Dameshek used 6-mercaptopurine (6-MP) or methotrexate as immunosuppression in their transplant patients.19 In 1960 Roy Calne developed BW57-322 (later known as azathioprine), a new derivative of 6-MP which was more effective with lesser side effects as compared to 6-MP, which paved the path for the use of Azathioprine in transplants.20
In 1960 in Paris, Küss and his team successfully used a combination of 6-MP and intermittent prednisone, after an initial dose of irradiation. This case was the first successful use of chemical immunosuppression.21 The physicians realized that steroids combined with azathioprine had a synergistic immunosuppressive effect, which introduced this combination as a standard immunosuppressive regimen in renal transplantation.22
Woodruff and Medawar attempted to use many agents for induction immunosuppression. In 1971, they developed antilymphocyte serum, which was a powerful immunosuppressant and was successful in inducing initial immunosuppression. This product followed by its better monoclonal antibody versions, later became an important component of induction in transplant.23 Despite many claims of optimal immunosuppression, based on trials utilizing splenectomy, thymectomy, thoracic duct drainage and cyclophosphamide, no agent except anti thymocyte globulin survived the test of time. In the 1970s, Cyclosporine was discovered as a powerful immunosuppressive agent by Borel.24 Cyclosporine entered immunosuppression practice, and became the dominant agent in use, till the 1990s. Starzl et al first used Tacrolimus in1989, realizing its greater potential compared to Cyclosporine, and today Tacrolimus has replaced Cyclosporine.25 Mycophenolate which was discovered much earlier in the 20th century was also used for kidney transplants and was found to be an extremely effective drug. This paved the way for the present triple drug immunosuppression utilizing steroids, tacrolimus and mycophenolate, which remains the standard of care in renal transplantation world-wide.
Immunological methods
The role of immunity in the survival of the transplanted kidneys began to be understood early in the course of modern transplantation, when organs which were well perfused and seemingly well preserved would rapidly cease functioning. The path breaking discovery of human leukocyte antigen (HLA)26 in 1958 by Jean Dausset paved the way for further immunological research. There were attempts to identify anti-HLA antibodies by tissue-typing methods in 1962. These anti-HLA antibodies were first identified by Rose Payne in patients with prior sensitization including those who received multiple transfusions or underwent multiple pregnancies.27
In 1965, Paul Terasaki and colleagues developed the first test to detect these anti HLA antibodies associates. They did a crossmatch between donor cells and recipient sera using lymphocytotoxicity which later popularly came to be known as the complement dependent cytotoxicity (CDC) cross match, that has become the first step of pre-transplant immunological testing.28 Kissmeyer-Nielsen refined the crossmatch methods in the pre-transplant setting and used it successfully to reduce the episodes of hyperacute rejection.29 The same concept was also proved by Terasaki that a recipient with a positive cross-match test against a particular donor, had a high risk of hyperacute rejection post-transplant. He also used crossmatch to find the most appropriate and safe donor amongst all potential donors.30 The detailed HLA-DR concept of HLA and matching was reported by Ting and Morris.31
Evolution of transplant
With the advent of renal transplantation, transplantation groups and societies were set up. Parallel advances in dialysis technology increased the life span of patients, improving their health and opening the option of kidney transplant in these patients. With the advent of better transplant care and safer immunosuppressives, management of patients improved with reduced risks.32,33
The advantages of cooling the donor organs and perfusion fluids was gradually recognized. Collins et al, in 1969 did landmark work on perfusion fluids and started a simple flush and chill technique of perfusion, to allow longer storage of donor organ.34 With the advent of transport of organs between centers, perfusion pumps were designed and developed to increase the life of harvested donor organs.
Recipients of kidney transplants lived longed and lived normal lives as any other individual. They took up jobs and had successful careers, besides doing well in their personal lives. The age cut-offs for donor and recipients widened and kidney transplants were also done successfully in children. Patients went on to receive a second or third transplant after the earlier graft failed.
Deceased donor transplant programs flourished with increase in availability of organs because of better awareness of medical professionals and common population. Hospitals also adopted better resuscitation and brain death protocols, increasing the availability of deceased donor organs. But this supply of deceased donor organs has not been able to catch up with the steadily increasing number of patients needing organ transplants.35
Kidney transplant in India
The kidney transplant program in India progressed keeping in pace with the rest of the world. Kidney transplant was first attempted in animals in India, in King Edward Memorial (KEM) Hospital Mumbai in 1950, where Dr PK Sen and his team attempted liver and kidney transplants in dogs.36 KEM hospital, Mumbai performed the first human kidney transplant in India in May 1965, by transplanting a cadaveric donor kidney to a patient with hypernephroma. The graft functioned well, but unfortunately, the patient succumbed after ten days due to a sudden myocardial infarction. Thereafter, another deceased donor transplant was carried out after a year at the KEM hospital in 1966, but even this patient died on the third day post transplant due to bilateral pneumonia and sepsis. Banaras Hindu University, Varanasi also performed deceased donor kidney transplant led by Udupa and his team.37
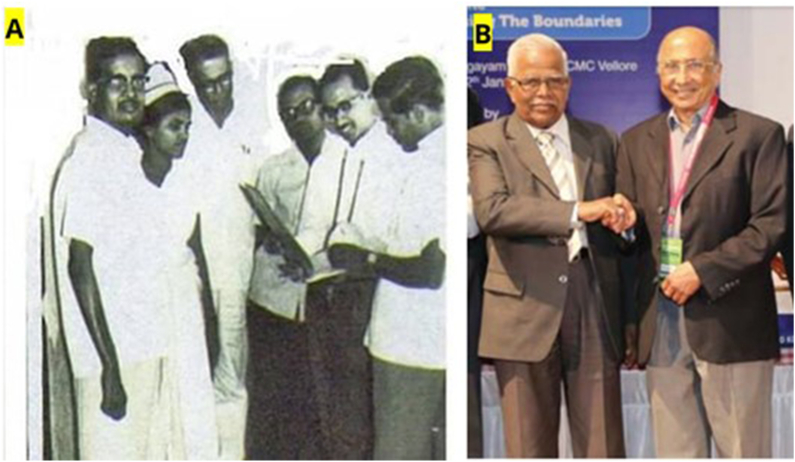
After these unsuccessful attempts, the first successful living donor kidney transplant of the country was performed at the Christian Medical College (CMC), Vellore on 02 Feb 1971, by Mohan Rao and Kaivilayil V Johny (who established the transplant centre at the hospital after their training from Australia) (Fig. 3).
Fig. 3.
The first successful live donor renal transplant done in CMC Vellore in 1971 with the transplant team Dr Martin Isaac, Dr HS Bhat, transplant nurse and the patient Shanmugham (A). The pioneers of the first transplant Dr Mohan Rao (left) and Dr Kaivilayil Johny (right) seen together(B). (Picture courtesy CMC Vellore).
In 1972, Inder Dhawan performed a renal transplant at the All India Institute of Medical Sciences, New Delhi. The Father of Nephrology in India, KL Chugh and Rajveer Yadav started the kidney transplant program at the Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh in 1974. Jaslok Hospital in Mumbai also started to do live donor kidney transplants in 1974. The cadaver program in the country, got a boost when Samuel Kountz and TK Sreepada Rao from the Downstate Medical Centre in Brooklyn, New York, got two cadaver kidneys from the United States to India by air, and performed kidney transplantation in two patients on December 27, 1977 in Jaslok Hospital in Mumbai.38
The advent of kidney transplants led to few unfortunate cases of illegal transplants and donor exploitation in the country. This paved the way for various legislations to stop the same, and ultimately the “Transplantation of Human Organs Act (THOA)” came into existence in the year 1995, to streamline the process of organ transplant, lay down requisite rules for the same, and avoid illegal transplants or financial dealings in respect of donor organs. The Act was amended in 2011 and is presently called the Transplantation of Human Organs and Tissues Act (THOTA).
Kidney transplantation in the Indian Armed Forces
The journey of the Armed Forces Medical Services (AFMS) of India, in the field of kidney transplantation began in February 1991, when the first transplant was done in INHS Asvini, Mumbai, with a live related kidney transplant performed by Vinod Kumar Saxena (then Surgeon Commander) (transplant surgeon) and Raman Malik (then Surgeon Commander) (Nephrologist), as shown in Fig. 4. This was immediately followed by a kidney transplant at the Army Hospital Delhi (presently Army Hospital Research and Referral) (AH R&R), when a serving Air Force personnel received a kidney allograft from his wife, with the team comprising of nephrologists Akhil Mishra (then Colonel), Yashpal (then Colonel), and urologists Madhusoodanan P (then Lieutenant Colonel) and Hardev Singh Bhatyal (then Lieutenant Colonel). This was soon followed by kidney transplants at other service hospitals like Command Hospital Pune, Command Hospital Calcutta, and Command Hospital Bangalore. The first deceased donor renal transplant was done in AHRR in August, 1998. The AFMS has thereafter kept pace with the latest developments in the world, doing its first ABO incompatible renal transplant in 2013 and the first swap transplant in 2021, both at the AHRR, New Delhi.
Fig. 4.
Transplant surgery being performed at INHS Asvini, which was the first AFMS centre to perform a transplant. (Picture courtesy Surg VAdm VK Saxena [Retd]).
Conclusion
Renal transplantation has come a long way since the first successful live transplant done in Boston, in December 1953. Despite its initial successes, the transplant community is faced with many challenges, of which, improving graft life and recipient survival, bridging the ever-increasing supply-demand gap and immune tolerance are the main ones. Though deceased donor organ harvesting addressed the initial shortage of donor organs, the recent attempts of xenotransplantation of kidneys and a heart from genetically modified pigs has lit a ray of hope of a possible limitless source of donor organs for human beings in the future. Of course, surmounting the immune system and ensuring graft tolerance continues to be the elusive holy grail for all transplant physicians and surgeons.
Discloser of competing interest
The authors have none to declare.
References
- 1.Paul C.N. Skin grafting in burns. Wounds. 2008 Jul;20(7):199–202. [PubMed] [Google Scholar]
- 2.Singh V. Sushruta: the father of surgery. Natl J Maxillofac Surg. 2017 Jan-Jun;8(1):1–3. doi: 10.4103/njms.NJMS_33_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ullman E. Experimentelle Nierentransplantation. 1902 [experimental kidney transplantation. 1902] Wien Klin Wochenschr. 2002 Feb 28;114(4):126–127. [German] [PubMed] [Google Scholar]
- 4.Hamilton D. World Scientific; Singapore: 2017. The First Transplant Surgeon: The Flawed Genius of Nobel Prize Winner, Alexis Carrel. [Google Scholar]
- 5.Unger E. Nierentransplantation. Berl Klin Wochenschr. 1909;1:1057. [Google Scholar]
- 6.Hamilton D. Kidney transplantation: A history. Kidney Trans: Principles and Practice. 2008;4:1–7. [Google Scholar]
- 7.Matevossian E., Kern H., Hüser N., et al. Surgeon Yurii Voronoy - a pioneer in the history of clinical transplantation: in memoriam at the 75th anniversary of the first human kidney transplantation. Transpl Int. 2009 Dec;22(12):1132–1139. doi: 10.1111/j.1432-2277.2009.00986.x. [DOI] [PubMed] [Google Scholar]
- 8.Dubost C., Oeconomos N., Vaysse J., et al. Resultats d’une tentative de greffe rénale. Bull Soc Med Hop Paris. 1951;67:1372. [PubMed] [Google Scholar]
- 9.Moore F.D. WB Saunders; Philadelphia: 1964. Give and Take: The Development of Tissue Transplantation. [Google Scholar]
- 10.Dempster W.J. Kidney homotransplantation. Br J Surg. 1953 Mar;40(163):447–465. doi: 10.1002/bjs.18004016309. [DOI] [PubMed] [Google Scholar]
- 11.Medicine's living history: Dr. Richard H. Lawler recalls the first successful kidney transplant. Medical World News, April. 1972;14:57. [Google Scholar]
- 12.Michon L., Hamburger J., Oeconomos N., et al. Une tentative de transplantation rénale chez l'homme: aspects médicauxét biologiques [An attempted kidney transplantation in man: medical and biological aspects] Presse Med. 1893;61(70):1419–1423. 1953 Nov 4. [PubMed] [Google Scholar]
- 13.Murray J.E., Merrill J.P., Harrison J.H. Kidney transplantation between seven pairs of identical twins. Ann Surg. 1958 Sep;148(3):343–359. doi: 10.1097/00000658-195809000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mollaret P., Goulon M. [The depassed coma (preliminary memoir)] Rev Neurol (Paris) 1959 Jul;101:3–15. [French] [PubMed] [Google Scholar]
- 15.Owen R.D. Immunogenetic consequences of vascular anastomoses between bovine twins. Science. 1945 Oct 19;102(2651):400–401. doi: 10.1126/science.102.2651.400. [DOI] [PubMed] [Google Scholar]
- 16.Medawar P.B. Vol. 52. Academic Press; New York: 1958. The immunology of transplantation; pp. 144–176. (Harvey Lecture Series, 1956–1957). [Google Scholar]
- 17.Hume D.M., Merill J.P., Miller B.F., Thorn G.W. Experiences with renal homotransplantation in the human: report of nine cases. J Clin Invest. 1955 Feb;34(2):327–382. doi: 10.1172/JCI103085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murray J.E., Merrill J.P., Dammin G.J., et al. Study on transplantation immunity after total body irradiation: clinical and experimental investigation. Surgery. 1960 Jul;48:272–284. [PubMed] [Google Scholar]
- 19.Schwartz R.S. In: Design and Achievements in Chemotherapy. Hitchings G.H., editor. Burroughs Wellcome; Durham, NC: 1976. Perspectives on immunosuppression; pp. 39–41. [Google Scholar]
- 20.Calne R.Y. The development of immunosuppressive therapy. Transplant Proc. 1981 Mar;13(1 Suppl 1):44–49. [PubMed] [Google Scholar]
- 21.Kuss R., Legrain M., Mathe G., Nedey R., Camey M. Homologous human kidney transplantation. Experience with six patients. Postgrad Med J. 1962 Sep;38(443):528–531. doi: 10.1136/pgmj.38.443.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murray J.E., Merrill J.P., Harrison J.H., Wilson R.E., Dammin G.J. Prolonged survival of human-kidney homografts by immunosuppressive drug therapy. N Engl J Med. 1963 Jun 13;268:1315–1323. doi: 10.1056/NEJM196306132682401. [DOI] [PubMed] [Google Scholar]
- 23.Wolstenholme G.E.W., O'Connor M., editors. Antilymphocytic Serum. J&A Churchill; London: 1967. [Google Scholar]
- 24.Calne R.Y., White D.J., Thiru S., et al. Cyclosporin A in patients receiving renal allografts from cadaver donors. Lancet. 1978 Dec 23-30;2(8104-5):1323–1327. doi: 10.1016/s0140-6736(78)91970-0. [DOI] [PubMed] [Google Scholar]
- 25.Starzl T.E., Todo S., Fung J., Demetris A.J., Venkataramman R., Jain A.F.K. 506 for liver, kidney, and pancreas transplantation. Lancet. 1989 Oct 28;2(8670):1000–1004. doi: 10.1016/s0140-6736(89)91014-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dausset J. Iso-leuco-anticorps [Iso-leuko-antibodies] Acta Haematol. 1958 Jul-Oct;20(1-4):156–166. doi: 10.1159/000205478. French. [DOI] [PubMed] [Google Scholar]
- 27.Dausset J. The challenge of the early days of human histocompatibility. Immunogenetics. 1980;10(1):1–5. doi: 10.1007/BF01561547. [DOI] [PubMed] [Google Scholar]
- 28.Terasaki P.I., Marchioro T.L., Starzl T.E. In: Histocompatibility Testing. Amos D.B., van Rood J.J., editors. National Academy of Sciences; Washington, DC: 1965. p. 83. [Google Scholar]
- 29.Williams G.M., Hume D.M., Hudson R.P., Jr., Morris P.J., Kano K., Milgrom F. "Hyperacute" renal-homograft rejection in man. N Engl J Med. 1968 Sep 19;279(12):611–618. doi: 10.1056/NEJM196809192791201. [DOI] [PubMed] [Google Scholar]
- 30.Terasaki P.I., Mcclelland J.D. Microdroplet assay of human serum cytotoxins. Nature. 1964 Dec 5;204:998–1000. doi: 10.1038/204998b0. [DOI] [PubMed] [Google Scholar]
- 31.Jager M.J., Brand A., Claas F.H.J., Jon van Rood The pioneer and his personal view on the early developments of HLA and immunogenetics. Transpl Immunol. 2019 Feb;52:1–26. doi: 10.1016/j.trim.2018.12.006. [DOI] [PubMed] [Google Scholar]
- 32.Ting A., Morris P.J. Matching for B-cell antigens of the HLA-DR series in cadaver renal transplantation. Lancet. 1978 Mar 18;1(8064):575–577. doi: 10.1016/s0140-6736(78)91025-5. [DOI] [PubMed] [Google Scholar]
- 33.Starzl T.E. Personal reflections in transplantation. Surg Clin North Am. 1978 Oct;58(5):879–893. doi: 10.1016/s0039-6109(16)41629-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Collins G.M., Bravo-Shugarman M., Terasaki P.I. Kidney preservation for transportation. Initial perfusion and 30 hours' ice storage. Lancet. 1969 Dec 6;2(7632):1219–1222. doi: 10.1016/s0140-6736(69)90753-3. [DOI] [PubMed] [Google Scholar]
- 35.Burdick J.F., DeMeester J., Koyama I. In: Ginns LC. Cosimi A.B., Morris P.J., editors. Blackwell; Boston: 1999. Understanding organ procurement and the transplant bureaucracy; pp. 875–894. (Transplantation). [Google Scholar]
- 36.Trivedi H.L. Nephrology and kidney transplantation in India: past, present and future. Indian Journal of Transplantation. 2014;8:S10–S13. doi: 10.1016/j.ijt.2014.01.006. [DOI] [Google Scholar]
- 37.Acharya V.N. Status of renal transplant in India--May 1994. J Postgrad Med. 1994;40(3):158–161. [PubMed] [Google Scholar]
- 38.Chugh K.S. Five decades of Indian nephrology: a personal journey. Am J Kidney Dis. 2009;54(4):753–763. doi: 10.1053/j.ajkd.2009.06.027. [DOI] [PubMed] [Google Scholar]