Abstract
Key Clinical Message
Impacted maxillary central incisors represent a relatively infrequent occurrence. This condition significantly impacts the patient's self‐esteem and aesthetic concerns. Effective resolution is achievable through a combined strategy involving surgical exposure, bracket attachment, and subsequent orthodontic extrusion. The Surgical orthodontic approach is the optimal strategy for addressing impacted maxillary central incisors.
Abstract
Central incisor is rarely impacted teeth often associated with supernumerary teeth. This case series includes three cases of central incisor impaction presented with complaints of missing teeth, unesthetic appearance, and unclear speech. All the cases were managed with surgical exposure followed by traction by orthodontic force, restoring smile aesthetics.
Keywords: case series, incisor, orthodontic extrusion, tooth impacted, tooth supernumerary, traction
1. INTRODUCTION
An impacted tooth refers to a tooth that does not emerge through the gum within the expected timeframe of normal development. 1 Among impacted teeth, the maxillary canine is the most commonly impacted tooth after third molars and central incisor impaction is rare, accounting for around 0.06%–0.2% of all cases. 2 , 3
Central incisor impaction can be attributed to a range of causative factors, including abnormal tooth dilaceration, fusion of tooth roots, disruptions in the normal eruption mechanisms, the presence of tumors, and underlying systemic conditions such as hormonal imbalances, vitamin deficiencies, or genetic predisposition. 4 However, it is crucial to emphasize that the predominant and primary cause is the existence of a physical barrier that impedes the proper eruption of the tooth. Remarkably, in approximately 56%–60% of cases, the impaction is directly associated with the presence of supernumerary teeth, which serve as obstructive elements that disrupt the normal tooth eruption process. 5 , 6
The absence of a central incisor not only affects one's appearance but also has negative impacts on self‐esteem, functionality, and social interactions. Therefore, it is crucial to diagnose and address this issue at an early stage. 7
Orthodontists often face a dilemma when deciding whether to remove the impacted tooth or guide it into its correct position. In cases where the central incisor is ankylosed to the surrounding bone, positioned unfavorably, or severely curved, extraction is usually recommended. 8 However, for cases where the tooth's alignment is favorable but it fails to emerge naturally, a combination of surgical exposure and orthodontic treatment is necessary to bring the tooth into the correct position within the dental arch. 9
We report a case series documenting the successful management of impacted central incisors through a coordinated approach involving surgical procedures and orthodontic interventions.
2. MANAGEMENT OF IMPACTED MAXILLARY CENTRAL INCISORS
2.1. Case 1
2.1.1. Case history/examination
A 10‐year‐old male patient presented with a chief complaint of missing upper front teeth for the past year, which had caused difficulties in biting food and impaired his ability to smile. There was no noteworthy medical history, and the patient's height and weight were within the normal range. The patient was in a late mixed dentition stage and had a missing permanent maxillary left central incisor. The retained deciduous central incisor, which was also carious, remained in place without any mobility.
2.1.2. Differential diagnosis, investigations, and treatment
Cone beam computed tomography (CBCT) imaging revealed that the maxillary left central incisor was impacted on the labial side, and there were supernumerary teeth positioned palatally in the same region. The position of the impacted central incisor was found to be favorable both in relation to the mid‐sagittal plane and the vertical alignment in relation to the adjacent tooth. The treatment plan involved a surgical procedure to remove the supernumerary teeth and an orthodontic approach to guide the impacted tooth into proper occlusion.
To commence the orthodontic treatment, we affixed 0.022″ MBT pre‐adjusted edgewise appliance (PEA) brackets, (Sapphire™ True Twin MIM Metal bracket system manufactured by Modern Orthodontics India) to the maxillary teeth. This was done with the aim of achieving alignment and leveling. Anchorage augmentation techniques were employed to ensure proper tooth movement. The orthodontic wire was sequentially progressed to 019″ × 025″ stainless steel wire, beginning with alignment and leveling procedures. A loop was incorporated into the center of the wire to accommodate the attachment of active components for the impacted tooth.
Under local anesthesia, a surgical procedure was performed to expose the impacted tooth, and the supernumerary tooth was removed. Begg's brackets were affixed, and a monkey chain was connected from the impacted tooth to the base archwire, which was then ligated. The patient's progress was closely monitored, and the appliance was adjusted at 3‐week intervals.
2.1.3. Outcome and follow‐up
After 8 months of treatment, the impacted tooth had been successfully guided into proper occlusion. Further adjustments were made by applying individual palatal root torque to the 0.019″ × 0.025″ stainless steel wire and securing it with ligatures. As a result of this comprehensive treatment approach, the patient achieved an aesthetically pleasing smile with a healthy periodontal condition. Upon evaluating the lateral cephalogram, it was observed that the patient presented with a skeletal Class II malocclusion and a vertical growth pattern. Consequently, we devised a plan to incorporate myofunctional therapy as part of the treatment approach (Figure 1).
FIGURE 1.

(A) Pretreatment frontal intraoral photograph revealing retained carious tooth 61 and missing tooth 21. (B) 3‐D CBCT image revealing impacted tooth 21, impacted supernumerary tooth present palatally and retained tooth 61. (C) Sagittal section of CBCT image revealing horizontally impacted tooth 21, horizontally impacted supernumerary tooth present palatally and retained tooth 61. (D) Surgical exposure of impacted tooth 21 and impacted supernumerary tooth. (E) Surgical site revealing Begg's bracket bonded to impacted tooth 21 with a monkey chain and extraction socket of supernumerary tooth. (F) Post‐treatment frontal intraoral photograph showing orthodontically extruded and aligned tooth 21.
2.2. Case 2
2.2.1. Case history/examination
A 12‐year‐old male patient presented with a non‐eruption of his upper front tooth persisting for 3 years. The patient exhibits introverted tendencies and expressed experiencing embarrassment at school due to the absence of that tooth. He had no significant medical or dental history. Intraoral examination revealed a permanent dentition period with a bilateral Class I molar relationship. However, the upper right central incisor (tooth 11) was missing. The upper right central incisor was palpable in the labial vestibule.
2.2.2. Differential diagnosis, investigations, and treatment
To confirm the findings, an orthopantomogram (OPG) was taken, which revealed that tooth 11 was slightly rotated, and an impacted supernumerary tooth was also identified adjacent to it. The treatment plan involved a series of steps: surgical exposure, extraction of the supernumerary tooth, and orthodontic extrusion of tooth 11. The treatment commenced with the placement of orthodontic bands on teeth 16 and 26. Subsequently, a full arch bonding procedure was performed using 0.022″ MBT pre‐adjusted edgewise appliance (PEA) brackets (Sapphire™ True Twin MIM Metal bracket system by Modern Orthodontics, India). The alignment process utilized a sequence of wires, starting with 0.012″, 0.014″, 0.016″, and 0.018″ NiTi wires, and finally transitioning to 0.017 × 0.025″ stainless steel wire.
During the surgical exposure procedure conducted under local anesthesia, a flap was raised to expose the tooth surface. Additionally, a lower central incisor bracket was bonded to the impacted central incisor, and an active attachment was ligated from the bracket to the loop on the base archwire. This attachment facilitated the controlled movement of the tooth. Activation of this attachment was performed every 15 days. Once the coronal portion of the tooth was sufficiently visible, a 0.014″ NiTi wire was ligated in place. This wire progression continued until the central incisor (tooth 11) was properly aligned within the dental arch.
2.2.3. Outcome and follow‐up
The treatment outcome resulted in achieving aesthetic harmony, functional balance, and a healthy periodontal condition. The comprehensive approach successfully addressed impacted and rotated tooth 11 and the presence of the impacted supernumerary tooth (Figure 2).
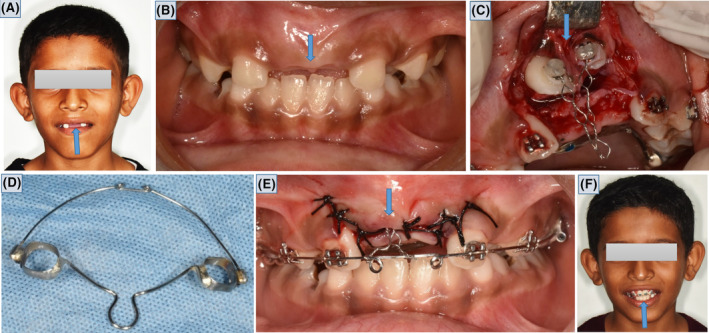
FIGURE 2.

(A) Pretreatment extraoral photograph showing missing tooth 11. (B) Pretreatment frontal intraoral photograph revealing missing tooth 11. (C) Bracket bonded to tooth 11 with monkey chain. (D) Tooth 11 ligated to the base archwire with 0.012 NiTi wire. (E) Post‐treatment frontal intraoral photograph showing orthodontically extruded and aligned tooth 11. (F) Post‐treatment extraoral photograph showing orthodontically extruded and aligned tooth 11.
2.3. Case 3
2.3.1. Case history/examination
An 11‐year‐old male patient presented with an aesthetically unpleasing smile due to the absence of eruption of his upper front teeth for 2 years. He expressed concerns regarding his speech clarity. His parents also noted inadequate physical growth compared to his age. Upon evaluation, no significant medical issues were identified. Intraoral examination revealed that he was in a mixed dentition stage with a bilateral Class I molar relationship. Teeth 11 and 21 were missing, leading to a noticeable bulge in the incisor region, which could be felt high in the labial vestibule. Upon further clinical assessment, it was confirmed that teeth 11 and 21 were situated labially above the marginal gingiva.
2.3.2. Differential diagnosis, investigations, and treatment
Given the patient's mixed dentition status and the absence of suitable teeth for adequate anchorage, a specialized appliance was designed. This appliance featured a rigid wire framework incorporating a Nance palatal arch positioned palatally for anchorage. A labial 0.019 × 0.025″ stainless steel wire with two anterior loops was fabricated to provide the necessary support.
The treatment strategy encompassed the application of bands on teeth 16 and 26, followed by bonding to achieve leveling on teeth 12, 22, 14, and 24. This was carried out using 0.022″ MBT pre‐adjusted edgewise appliance (PEA) brackets (Sapphire™ True Twin MIM Metal bracket system by Modern Orthodontics, India). The wire framework was securely cemented and ligated into position. Under local anesthesia, a surgical procedure was performed, which included raising a flap and exposing the tooth surface. The upper central incisor bracket was then bonded, and an active attachment was ligated from the bracket to the loop on the base archwire. Activation of this attachment was carried out every 15 days. Following a month and a half, a 0.014″ NiTi wire was ligated, allowing for the continued progression of the wire until the impacted central incisors (teeth 11 and 21) were properly aligned within the dental arch.
2.3.3. Outcome and follow‐up
Upon examination of the periodontal condition, a slight increase in crown length and irregular gingival contour related to tooth 21 were noted. To address this issue and enhance the periodontal health of the exposed teeth, the patient was advised to undergo flap surgery. However, the patient's parents declined this recommendation, expressing their contentment with the treatment outcomes achieved. The patient was scheduled for regular follow‐up appointments to assess the eruption progress of the canine and to monitor the periodontal condition of tooth 21.
The comprehensive treatment approach successfully addressed the lack of tooth eruption and improved the patient's smile aesthetics, despite the minor periodontal concerns that were presented (Figure 3).
FIGURE 3.
(A) Pretreatment extraoral photograph showing missing teeth 11 and 21. (B) Pre‐treatment frontal intraoral photograph revealing missing teeth 11 and 21. (C) Surgical exposure of teeth 11 and 21 and attachment of orthodontic appliances. (D) Appliance design for anchorage. (E) Cemented anchorage device and ligation of impacted teeth to base wire. (F) Post‐treatment extraoral photograph showing orthodontically extruded and aligned teeth 11 and 21.
3. DISCUSSION
Impacted central incisors are a relatively uncommon occurrence in routine pediatric dental examinations. In the two previously discussed cases, the patients presented with the failure of eruption in one central incisor, while the counterpart incisor was present. In contrast, the third case involved the absence of both central incisors.
Among the various potential causes of impaction, cases 1 and 2 were linked to the presence of supernumerary teeth, which acted as barriers hindering the eruption process, as suggested by supporting evidence. 10
In contrast, case 3 did not exhibit any local barriers as a causative factor. However, it is important to consider that insufficient physical growth and suboptimal nutritional status may contribute to this case.
Surgical orthodontic procedures can be a viable option for treating dental impaction, ensuring both good aesthetics and functionality.
To diagnose impacted teeth properly, a comprehensive approach involving patient history, visual examination, palpation, and essential radiographic imaging like intraoral periapical radiographs (IOPAR), orthopantomograms (OPG), and cone beam computed tomography (CBCT) should be employed. OPG is considered the standard radiograph for assessing the dental status, position, depth, and angulation of impacted teeth. 10 , 11
In all three cases, the central incisor was detected in the labial vestibule, indicative of labial impaction.
In Case 1, a CBCT scan was conducted to assess various factors, including the presence of associated supernumerary teeth, root dilacerations, or any underlying pathology. This was necessary as a deciduous central incisor remained in place, and the impacted incisor was palpable in a high position within the vestibule.
In Case 2, an OPG revealed the presence of supernumerary teeth situated palatally, along with a rotated central incisor. Additionally, the OPG facilitated the diagnosis of the impacted incisor's status, root development, and allowed for a space analysis to determine the alignment feasibility of impacted teeth within the dental arch.
In Case 3, both central incisors were palpated just above the alveolus, and adequate space was observed for the alignment of the incisors.
To evaluate the favorability of addressing the impacted central incisor, several criteria were employed, including measuring the angle between its long axis and the mid‐sagittal plane using Bryan et al.'s method, 12 assessing the vertical position of the impacted permanent incisors in relation to the contralateral erupted central incisor following Smailiene et al.'s approach, 13 and determining the maturity of unerupted incisors through Cvek's classification. 14
Case 1 posed challenges in terms of favorability as the impacted central incisor exhibited an angle of more than 30 degrees to the mid‐sagittal plane and was positioned at the level of the apical one‐third of the contralateral central incisor. Conversely, Case 2 and Case 3 displayed a more favorable outlook for traction and alignment within the dental arch.
Impacted teeth that fails to erupt even after removable of etiology may require surgical exposure followed by orthodontic traction for eruption. Surgical exposure techniques can include circular incisions, apically positioned flaps (raising a flap that includes attached gingiva over the impacted tooth), or the closed eruption technique (raising a flap with attached gingiva and fully replacing it after bonding an attachment to the impacted tooth). Closed eruption is often preferred for better aesthetics and periodontal health. 15 The closed eruption technique was consistently employed in all three cases to improve aesthetic outcomes and promote optimal periodontal health.
When bone covers the tooth's surface, it is advisable to remove as little bone as possible to attach the traction device, reducing the risk of root resorption, trauma to neighboring teeth, and interference with the natural eruption process. Various attachments, such as crowns, wire ligatures, chain links, bands, and directly bonded brackets, can be used to apply traction forces to impacted teeth. In general, mini brackets, buttons, or Begg's brackets are preferred to minimize bone removal from the tooth's surface. 16 In the initial case, Begg's brackets were utilized, while mini brackets were employed in the second and third cases. Bonding should be done during the ongoing surgical procedure, using a hemostatic agent and a specialized bonding technique. The bracket should be secured with a steel ligature to the base archwire. In the case of labial impaction of the central incisor described in this case series, the monkey chain was ligated and activated over the desired period. Subsequently, once the tooth became visible in the oral cavity, the previous bracket was replaced with PEA brackets, and further leveling and alignment procedures were carried out. The goal should be to achieve proper positioning of impacted teeth, including tip and torque adjustments, ensuring good periodontal health and stability.
4. CONCLUSION
Impacted central incisor teeth represent a relatively infrequent occurrence and can manifest due to a variety of factors, frequently impacting both aesthetic appearance and functional aspects. Consequently, this condition necessitates a comprehensive diagnostic approach and precise management strategies. Surgical orthodontic interventions can play a crucial role in guiding these impacted teeth into their rightful position within a normal occlusion.
4.1. Patient's perspective
All three patients expressed a high level of satisfaction as a result of the successful treatment, which was accomplished without any complications.
AUTHOR CONTRIBUTIONS
Kanistika Jha: Conceptualization; investigation; methodology; resources; supervision; validation; visualization; writing – original draft; writing – review and editing. Manoj Adhikari: Conceptualization; investigation; methodology; supervision; validation; visualization; writing – original draft; writing – review and editing.
FUNDING INFORMATION
The present case study has received no financial aid.
CONFLICT OF INTEREST STATEMENT
Authors have stated explicitly that no potential conflict of interest has been reported in connection with this article.
ETHICS STATEMENT
It is our routine standard surgical procedure, so ethical clearance was not required.
CONSENT
Written informed consent was obtained from the patient to publish this case series in accordance with the journal's patient consent policy.
Jha K, Adhikari M. Surgical orthodontic intervention for impacted maxillary permanent central incisors: A case series. Clin Case Rep. 2023;11:e8199. doi: 10.1002/ccr3.8199
Contributor Information
Kanistika Jha, Email: Kanu.jha01@gmail.com.
Manoj Adhikari, Email: manojadhikari@naihs.edu.np, Email: adhikarimanoj2007@gmail.com.
DATA AVAILABILITY STATEMENT
No data was generated or analyzed in the present research.
REFERENCES
- 1. Santosh P. Impacted mandibular third molars: review of literature and a proposal of a combined clinical and radiological classification. Ann Med Health Sci Res. 2015;5(4):229‐234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cruz RM. Orthodontic traction of impacted canines: concepts and clinical application. Dental Press J Orthod. 2019;24:74‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Al‐Zoubi H, Alharbi AA, Ferguson DJ, Zafar MS. Frequency of impacted teeth and categorization of impacted canines: a retrospective radiographic study using orthopantomograms. Eur J Dent. 2017;11(1):117‐121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jain S, Raza M, Sharma P, Kumar P. Unraveling impacted maxillary incisors: the why, when, and how. Int J Clin Pediatr Dent. 2021;14(1):149‐157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chaushu S, Becker T, Becker A. Impacted central incisors: factors affecting prognosis and treatment duration. Am J Orthod Dentofacial Orthop. 2015;147(3):355‐362. [DOI] [PubMed] [Google Scholar]
- 6. Kafle D, Shrestha S, Acharya N, Agarwal A. Prevalence of maxillary central incisor impaction and supernumerary teeth among Nepalese orthodontic patients. Orthod J Nepal. 2015;5(2):14‐16. [Google Scholar]
- 7. Seehra J, DiBiase AT, Patel S, et al. Study protocol for the management of impacted maxillary central incisors: a multicentre randomised clinical trial: the iMAC trial. Trials. 2022;23(1):787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Singh H, Kapoor P, Sharma P, Dudeja P, Maurya RK, Thakkar S. Interdisciplinary management of an impacted dilacerated maxillary central incisor. Dental Press J Orthod. 2018;23:37‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chan CH, Chou ST, Tseng YC, Pan CY, Chang HP, Wu CW. Orthodontic‐surgical management of a horizontally impacted maxillary incisor − a case report. Taiwan J Orthod. 2015;26(4):8. [Google Scholar]
- 10. Kjær I. Mechanism of human tooth eruption: review article including a new theory for future studies on the eruption process. Scientifica. 2014;2014:1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chaushu S, Chaushu G, Becker A. The role of digital volume tomography in the imaging of impacted teeth. World J Orthod. 2004;5(2):120‐132. [PubMed] [Google Scholar]
- 12. Mockutė G, Klimaitė G, Smailienė D. The morphology of impacted maxillary central incisors: a systematic review. Medicina. 2022;58(4):462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Seehra J, Mortaja K, Wazwaz F, Papageorgiou SN, Newton JT, Cobourne MT. Interventions to facilitate the successful eruption of impacted maxillary incisor teeth due to the presence of a supernumerary: a systematic review and meta‐analysis. Am J Orthod Dentofacial Orthop. 2023;163:594‐608. [DOI] [PubMed] [Google Scholar]
- 14. Alsweed AA, Al‐Sughier Z. Surgical management of unerupted permanent maxillary central incisors due to presence of two supernumerary teeth. Int J Clin Pediatr Dent. 2020;13(4):421‐424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Marek I, Janková A, Starosta M, Novosad M, Kučera J. Comparison of spontaneous eruption and modified closed eruption technique with palatal traction in alignment of impacted maxillary central incisor teeth. Prog Orthod. 2023;24(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Vashi N, Vashi B. Eruption and alignment of impacted teeth with multi‐purpose attachments. J Clin Orthod. 2012;46(8):486‐490. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data was generated or analyzed in the present research.


