This cohort study examines the risk of reoperation in children with intermittent exotropia associated with bilateral lateral rectus recession compared with unilateral lateral rectus recession with medial rectus resection.
Key Points
Question
Does the risk of reoperation differ between the surgical approaches for intermittent exotropia in children?
Findings
In this cohort study of 7482 children with intermittent exotropia who underwent horizontal muscle strabismus surgery, approximately 1 in 5 children underwent reoperation within 5 years after the initial surgery. The reoperation risk of unilateral lateral rectus recession with medial rectus resection was lower than that of bilateral lateral rectus recession.
Meaning
Results of this study suggest that children with intermittent exotropia who undergo unilateral lateral rectus recession with medial rectus resection may be less likely to require reoperation within 5 years than those who undergo bilateral lateral rectus recession.
Abstract
Importance
There is no consensus on the optimal surgical treatment for children with intermittent exotropia (IXT).
Objective
To compare the 5-year reoperation rates for children with IXT treated with horizontal muscle strabismus surgery using bilateral lateral rectus recession (BLR) vs unilateral lateral rectus recession with medial rectus resection (RR).
Design, Setting, and Participants
This cohort study examined data obtained from the Intelligent Research in Sight (IRIS) Registry on 7482 children (age, <18 years) with IXT who underwent horizontal eye muscle strabismus surgery between January 1, 2013, and December 31, 2017. Children undergoing initial surgeries involving 3 or more horizontal muscles, vertical muscles, or reoperations were excluded.
Main Outcomes and Measures
The primary outcome was the adjusted cumulative incidence of repeat horizontal muscle surgery within 5 years after the initial surgery. Reoperation risk was analyzed using adjusted hazard ratios (AHRs) derived from multivariable Cox regression models, adjusting for individual demographic and surgical factors (age, sex, race and ethnicity, US Census region, and surgeon subspecialty). Data were analyzed between January 16 and September 20, 2023.
Results
The study included 7482 children (median [IQR] age at initial surgery, 6 [4-9] years; 3945 females [53%]) with IXT treated with horizontal muscle strabismus surgery. Bilateral lateral rectus recession was performed more frequently than RR (85.3% vs 14.7%, P < .001), especially in younger children (rates of BLR vs RR by age: age 0 to ≤4 years, 88.4% vs 11.6%; age 5 to ≤11 years, 84.7% vs 15.3%; age 12 to ≤17 years, 78.1% vs 21.9%; P < 0.001). After data adjustment, the 5-year cumulative incidence of reoperation was 21.3% (95% CI, 20.1%-22.5%). The adjusted 5-year cumulative incidence of reoperation was higher for BLR than for RR (22.2% vs 17.2%; difference, 4.9%; 95% CI, 1.9%-8.0%). Unilateral lateral rectus recession with medial rectus resection was associated with a lower 5-year reoperation risk compared with BLR (AHR, 0.77; 95% CI, 0.64-0.93). Younger age at time of initial surgery was associated with a higher reoperation risk (AHR per 1-year decrease, 1.09; 95% CI, 1.07-1.11) after adjusting for all other covariates.
Conclusions and Relevance
In this nationwide registry, approximately 1 in 5 children with IXT underwent reoperation within 5 years after the initial surgery. Children treated with RR were less likely to require a reoperation within 5 years compared with those treated with BLR. Further efforts to identify modifiable risk factors for reoperation are needed to reduce the surgical burden and improve outcomes for children with IXT.
Introduction
Debate exists regarding the optimal surgical intervention for intermittent exotropia (IXT) in childhood.1 The initial surgery often involves bilateral lateral rectus recession (BLR) or unilateral lateral rectus recession with medial rectus resection (RR). A Cochrane systematic review,1 including 2 randomized controlled studies that directly compared BLR with RR, did not find sufficient evidence to support a difference in outcomes between these 2 approaches. Reoperation after strabismus surgery has been used in large database studies as a risk factor for poor surgical outcome.2,3,4 However, to our knowledge, the probability of reoperation after BLR and RR in children with IXT has not been described using a nationwide cohort. The aim of this study was to compare the 5-year reoperation rates for children with IXT who underwent BLR vs RR.
Methods
This retrospective cohort study used data from the Intelligent Research in Sight (IRIS) Registry, a deidentified database of more than 70 million patients treated by more than 13 000 clinicians in ophthalmology practices in the US,5 to compare the probability of reoperation between BLR and RR surgical approaches in children with IXT. The study was approved by the Mass General Brigham Institutional Review Board, which waived informed consent given the use of deidentified data. We adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
We included all patients younger than 18 years with IXT who underwent strabismus surgery between January 1, 2013, and December 31, 2017. Patients were identified using International Classification of Diseases, Ninth Revision; International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; and Current Procedural Terminology codes (eTable 1 in Supplement 2). All patients in whom the initial surgery involved horizontal eye muscles were included. Children with an initial surgery involving 3 or more horizontal muscles, vertical muscles, or reoperation were excluded. There was no minimum follow-up period in this time-to-event analysis.
The primary outcome was repeat horizontal muscle surgery within 5 years after initial surgery. The initial surgical approach was categorized as RR or BLR. Data were collected on patient age at the time of initial surgery, sex, race and ethnicity, US Census region, and surgeon subspecialty. Age was analyzed as a continuous and categorical variable stratified into early childhood (0 to ≤4 years), middle childhood (5 to ≤11 years), and adolescence (12 to ≤17 years). Race and ethnicity were categorized into non-Hispanic Black, Hispanic, non-Hispanic White, other (including Asian, Native American or Alaska Native, and Native Hawaiian or Other Pacific Islander), and unknown. Data on race and ethnicity were collected to adjust for sociodemographic factors that could be associated with access to care. Geographic region was categorized according to US Census regions (Northeast, Midwest, South, and West). Surgeon subspecialty was dichotomized into pediatric vs other specialty.
Multivariable Cox proportional hazards regression models adjusted for age as a continuous variable and including all other covariates as potential confounders were used to describe the association between surgical approach and reoperation risk. Adjusted cumulative incidence curves were generated and used to estimate the 5-year cumulative incidence of reoperation. Data were analyzed between January 16 and September 20, 2023, using R, version 4.2.0 (R Foundation for Statistical Computing) with 2-sided tests and no adjustment for multiple comparisons. A P value <.05 was considered statistically significant.
Results
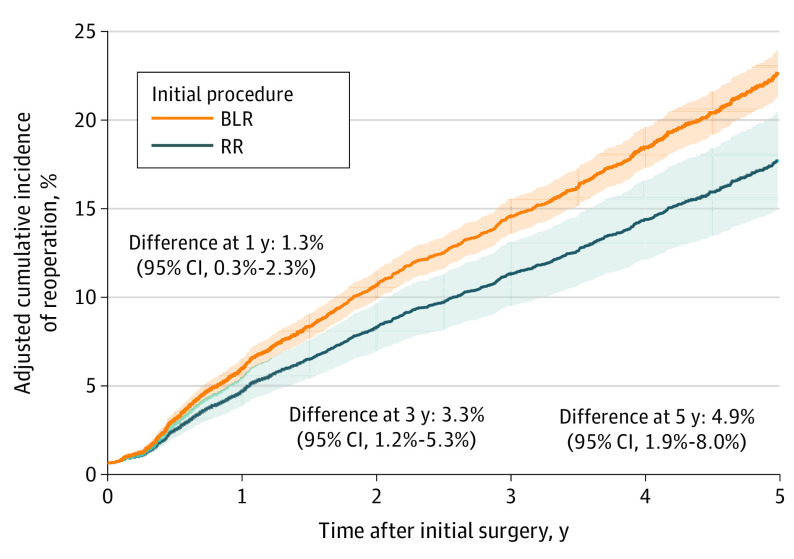
The study included 7482 children with IXT (median [IQR] age, 6 [4-9] years; 3945 females [53%] and 3525 males [47%]; 816 Black individuals [11%], 1018 Hispanic individuals [14%], 4265 White individuals [57%], 292 individuals [4%] of other race or ethnicity, and 1091 individuals [15%] with unknown race and ethnicity) who underwent horizontal muscle strabismus surgery. Bilateral lateral rectus recession was performed more frequently than RR (85.3% vs 14.7%, P < .001), especially in younger children (rates of BLR vs RR by age: age 0 to ≤4 years, 88.4% vs 11.6%; age 5 to ≤11 years, 84.7% vs 15.3%; age 12 to ≤17 years, 78.1% vs 21.9%; P < 0.001) (eTable 2 in Supplement 2). The adjusted 5-year cumulative incidence of reoperation was 21.3% (95% CI, 20.1%-22.5%). After adjusting for all covariates, BLR had a higher cumulative incidence of reoperation than RR at 1 year (5.4% vs 4.1%; difference, 1.3%; 95% CI, 0.3% to 2.3%), 3 years (14.0% vs 10.7%; difference, 3.3%; 95% CI, 1.2%-5.3%), and 5 years (22.2% vs 17.2%; difference, 4.9%; 95% CI, 1.9%-8.0%) after the initial surgery (Figure). Children aged 0 to 4 years or younger were more likely to undergo reoperation compared with children aged 12 to 17 years or younger (28.0% vs 16.9%; difference, 11.0%; 95% CI, 7.2%-14.9%), but the adjusted cumulative incidence of reoperation did not differ by region or surgeon specialty (Table).
Figure. Adjusted Cumulative Incidence of Reoperation After Horizontal Muscle Surgery in Children With Intermittent Exotropia Stratified by Surgical Approach.
Shaded areas represent 95% CIs. Data were adjusted for age, sex, race and ethnicity, US Census region, and surgeon subspecialty. BLR indicates bilateral lateral rectus recession; RR, unilateral lateral rectus recession with medial rectus resection.
Table. Adjusted Cumulative Incidence of Reoperation and Associated Risk Factors for Children With Intermittent Exotropia in the Intelligent Research in Sight Registry.
| Covariate | Patients, No. (%)a | Adjusted cumulative incidence of reoperation, % (95% CI) | Adjusted HR (95% CI)b | P value | |||
|---|---|---|---|---|---|---|---|
| 1 y | Difference | 5 y | Difference | ||||
| Surgical approach | |||||||
| BLR | 6379 (85) | 5.4 (4.8 to 5.9) | [Reference] | 22.2 (20.9 to 23.5) | [Reference] | 1 [Reference] | .008 |
| RR | 1103 (15) | 4.1 (3.3 to 4.8) | −1.3 (−2.3 to −0.3) | 17.2 (14.5 to 20.0) | −4.9 (−8.0 to −1.9) | 0.77 (0.64 to 0.93) | |
| Age, yc | |||||||
| 12 to ≤17 | 912 (12) | 4.0 (3.0 to 4.9) | [Reference] | 16.9 (13.6 to 20.2) | [Reference] | 1 [Reference] | <.001 |
| 5 to ≤11 | 3819 (51) | 4.2 (3.6 to 4.7) | 0.2 (−0.8 to 1.3) | 17.8 (16.3 to 19.3) | 0.9 (−2.8 to 4.5) | 1.00 (0.81 to 1.23) | |
| 0 to ≤4 | 2751 (37) | 6.9 (6.1 to 7.7) | 3.0 (1.7 to 4.2) | 28.0 (26.0 to 30.0) | 11.0 (7.2 to 14.9) | 1.62 (1.32 to 1.99) | |
| Per 1-y decrease | NA | NA | NA | NA | NA | 1.09 (1.07 to 1.11) | |
| Sex | |||||||
| Male | 3525 (47) | 4.9 (4.3 to 5.5) | [Reference] | 20.5 (18.9 to 22.2) | [Reference] | 1 [Reference] | .11 |
| Female | 3945 (53) | 5.4 (4.8 to 6.0) | 0.5 (−0.4 to 1.4) | 22.3 (20.7 to 24.0) | 1.8 (−0.5 to 4.1) | 1.10 (0.98 to 1.25) | |
| Race and ethnicity | |||||||
| Black non-Hispanic | 816 (11) | 4.6 (3.6 to 5.5) | −1.0 (−2.2 to 0.1) | 19.3 (15.9 to 22.6) | −3.9 (−7.6 to −0.2) | 0.81 (0.65 to 1.00) | .02 |
| Hispanic | 1018 (14) | 4.4 (3.6 to 5.3) | −1.2 (−2.3 to −0.1) | 18.7 (15.8 to 21.7) | −4.4 (−7.8 to −1.1) | 0.78 (0.64 to 0.95) | |
| White non-Hispanic | 4265 (57) | 5.6 (5.0 to 6.2) | [Reference] | 23.2 (21.6 to 24.7) | [Reference] | 1 [Reference] | |
| Otherd | 292 (4) | 4.0 (2.6 to 5.5) | −1.6 (−3.1 to −0.0) | 17.2 (11.8 to 22.6) | −5.9 (−11.6 to −0.3) | 0.72 (0.50 to 1.03) | |
| Unknown | 1091 (15) | 4.8 (3.9 to 5.8) | −0.8 (−1.9 to 0.3) | 20.3 (17.1 to 23.4) | −2.9 (−6.6 to 0.6) | 0.86 (0.71 to 1.04) | |
| US Census region | |||||||
| Midwest | 1814 (24) | 5.0 (4.3 to 5.7) | [Reference] | 20.9 (18.6 to 23.1) | [Reference] | 1 [Reference] | .32 |
| Northeast | 1606 (22) | 5.0 (4.2 to 5.8) | 0.0 (−1.1 to 1.1) | 20.9 (18.5 to 23.2) | 0.0 (−3.3 to 3.3) | 1.01 (0.84 to 1.20) | |
| South | 3283 (44) | 5.5 (4.8 to 6.2) | 0.5 (−0.5 to 1.5) | 22.7 (20.9 to 24.5) | 1.8 (−1.1 to 4.7) | 1.11 (0.95 to 1.29) | |
| West | 731 (10) | 4.5 (3.6 to 5.5) | −0.5 (−1.7 to 0.7) | 19.0 (15.5 to 22.5) | −1.9 (−6.0 to 2.3) | 0.90 (0.70 to 1.14) | |
| Surgeon subspecialty | |||||||
| Pediatric | 6293 (84) | 5.2 (4.6 to 5.7) | [Reference] | 21.5 (20.2 to 22.8) | [Reference] | 1 [Reference] | .91 |
| Other | 1189 (16) | 5.1 (4.2 to 5.9) | −0.1 (−1.1 to 0.9) | 21.2 (18.3 to 24.1) | −0.3 (−3.5 to 2.8) | 0.99 (0.84 to 1.17) | |
Abbreviations: BLR, bilateral lateral rectus recession; HR, hazard ratio; NA, not applicable; RR, unilateral lateral rectus recession with medial rectus resection.
Percentages may not sum to 100 due to rounding.
The multivariable model includes age as a continuous variable and all other covariates listed in the Table. Sensitivity analysis with categorical age in the multivariable model yielded similar estimates for all covariates.
Adjusted HR for continuous age in multivariable model reflects the change per 1-y decrease.
Other race and ethnicity includes Asian, Native American or Alaska Native, and Native Hawaiian or Other Pacific Islander.
In the multivariable regression model, RR was associated with a lower 5-year reoperation risk compared with BLR (adjusted hazard ratio, 0.77; 95% CI, 0.64-0.93). Younger age at time of initial surgery was associated with a higher reoperation risk (adjusted hazard ratio per 1-year decrease, 1.09; 95% CI, 1.07-1.11) (Table).
Discussion
In this cohort study using data from a nationwide registry of children with IXT who underwent RR or BLR, approximately 1 in 5 children underwent reoperation within 5 years after initial surgery. The 1-year reoperation estimates of 4.1% for RR and 5.4% for BLR are comparable with those in previous studies of pediatric cohorts using large databases.2,3 Using IRIS Registry data (2013-2015), Repka et al2 reported a 1-year reoperation rate of 3.9% to 5.1% for patients younger than 20 years (17 243) with any strabismus diagnosis. Using data from the IBM MarketScan database (2007-2013), Leffler et al3 found a 1-year reoperation rate of 7.7% for children younger than 18 years with all forms of strabismus (11 115). Our study inclusion criteria (IXT diagnosis) and outcome definition (reoperations involving horizontal rectus muscles) may contribute to the slight differences in estimates between these studies.
We found that BLR was associated with a higher 5-year risk of reoperation compared with RR. These findings support results from the Pediatric Eye Disease Investigator Group (PEDIG) multicenter randomized clinical trial (n = 197), which reported on reoperations within 3 years after initial surgery in 9 patients (10%) who underwent BLR and 4 patients (5%) who underwent RR and a cumulative incidence of reoperation of 30% for BLR and 11% for RR (difference, 19%; 95% CI, 2%-36%; P = .049) at 8 years after the initial surgery.6,7 However, the cumulative incidence of suboptimal surgical outcome in the PEDIG study did not differ substantially between BLR and RR.7
There is also a lack of consensus on the optimal timing for surgery in children with IXT.1 Repka et al8 reported that children who underwent surgery at ages 3 to younger than 5 years had fewer suboptimal outcomes compared with children who underwent surgery at ages 5 to younger than 11 years. Some surgeons recommend early intervention to minimize suppression and maximize the probability of success,9,10,11 whereas others support delaying surgery until the child is older when measurements are more precise and there is a lower chance of permanent loss of binocular vision after overcorrection.12
Limitations
This study has several limitations. First, there may be confounding factors affecting surgeon choice between BLR and RR that are unavailable in the IRIS Registry (eg, type, magnitude, and duration of misalignment). For instance, certain types of pattern strabismus may be approached with a preference of bilateral surgery with a vertical transposition. Second, the decision to perform a reoperation may be affected by unmeasured confounders (eg, unilateral poor vision among children undergoing RR). Third, we were unable to identify the indications for reoperation (eg, overcorrection, undercorrection, and recurrence) using this data set, which may have been associated with the timing of reoperation. Fourth, short follow-up intervals may have played a role in the wide CIs in our estimates. Finally, the 5-year follow-up period may not have captured the long-term stability of alignment of the surgical approaches.
Conclusions
This registry-based cohort study of more than 7000 children with IXT who underwent strabismus surgery found an increased 5-year reoperation risk for BLR compared with RR. Although the magnitude of the difference in the cumulative incidence of reoperation between procedures was small, this difference may have implications at the population level, since BLR is the predominant surgical approach for children with IXT in the US. Preference for bilateral surgery that avoids lateral incomitance induced by unilateral surgery should be balanced with potential increased risk of reoperation. Given the high incidence of reoperation in this population, these findings support the need for further investigation into modifiable factors that may reduce the surgical burden and improve outcomes for children with IXT.
Nonauthor Contributors.
eTable 1. International Classification of Disease (ICD-9/10) and Current Procedural Terminology (CPT) Codes Used to Identify Children With Intermittent Exotropia and the Type of Strabismus Surgery
eTable 2. Baseline Demographics of Children Undergoing Horizontal Muscle Surgery for Intermittent Exotropia Stratified by Surgical Approach
Data Sharing Statement
References
- 1.Pang Y, Gnanaraj L, Gayleard J, Han G, Hatt SR. Interventions for intermittent exotropia. Cochrane Database Syst Rev. 2021;9(9):CD003737.doi: 10.1002/14651858.CD003737.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Repka MX, Lum F, Burugapalli B. Strabismus, strabismus surgery, and reoperation rate in the United States: analysis from the IRIS Registry. Ophthalmology. 2018;125(10):1646-1653. doi: 10.1016/j.ophtha.2018.04.024 [DOI] [PubMed] [Google Scholar]
- 3.Leffler CT, Vaziri K, Schwartz SG, et al. Rates of reoperation and abnormal binocularity following strabismus surgery in children. Am J Ophthalmol. 2016;162:159-166.e9. doi: 10.1016/j.ajo.2015.10.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oke I, Hall N, Elze T, Miller JW, Lorch AC, Hunter DG; IRIS Data Analytics Committees . Adjustable suture technique is associated with fewer strabismus reoperations in the Intelligent Research in Sight Registry. Ophthalmology. 2022;129(9):1028-1033. doi: 10.1016/j.ophtha.2022.04.021 [DOI] [PubMed] [Google Scholar]
- 5.IRIS Registry data analysis. American Academy of Ophthalmology. Accessed October 5, 2023. https://www.aao.org/iris-registry/data-analysis/requirements
- 6.Donahue SP, Chandler DL, Holmes JM, et al. ; Pediatric Eye Disease Investigator Group; Writing Committee . A randomized trial comparing bilateral lateral rectus recession versus unilateral recess and resect for basic-type intermittent exotropia. Ophthalmology. 2019;126(2):305-317. doi: 10.1016/j.ophtha.2018.08.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donahue SP, Chandler DL, Wu R, et al. ; Pediatric Eye Disease Investigator Group; Pediatric Eye Disease Investigator Group . 8-Year outcomes of bilateral lateral rectus recessions versus unilateral recess-resect in childhood basic-type intermittent exotropia. Ophthalmology. 2023;S0161-6420(23)00630-9. doi: 10.1016/j.ophtha.2023.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Repka MX, Chandler DL, Holmes JM, et al. ; Pediatric Eye Disease Investigator Group . The relationship of age and other baseline factors to outcome of initial surgery for intermittent exotropia. Am J Ophthalmol. 2020;212:153-161. doi: 10.1016/j.ajo.2019.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Asjes-Tydeman WL, Groenewoud H, van der Wilt GJ. Timing of surgery for primary exotropia in children. Strabismus. 2006;14(4):191-197. doi: 10.1080/09273970601026193 [DOI] [PubMed] [Google Scholar]
- 10.Abroms AD, Mohney BG, Rush DP, Parks MM, Tong PY. Timely surgery in intermittent and constant exotropia for superior sensory outcome. Am J Ophthalmol. 2001;131(1):111-116. doi: 10.1016/S0002-9394(00)00623-1 [DOI] [PubMed] [Google Scholar]
- 11.Saunders RA, Rogers GL. Superior oblique transposition for third nerve palsy. Ophthalmology. 1982;89(4):310-316. doi: 10.1016/S0161-6420(82)34786-7 [DOI] [PubMed] [Google Scholar]
- 12.Edelman PM, Brown MH, Murphree AL, Wright KW. Consecutive esodeviation… then what? Am Orthopt J. 1988;38:111-116. doi: 10.1080/0065955X.1988.11981779 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Nonauthor Contributors.
eTable 1. International Classification of Disease (ICD-9/10) and Current Procedural Terminology (CPT) Codes Used to Identify Children With Intermittent Exotropia and the Type of Strabismus Surgery
eTable 2. Baseline Demographics of Children Undergoing Horizontal Muscle Surgery for Intermittent Exotropia Stratified by Surgical Approach
Data Sharing Statement