Abstract
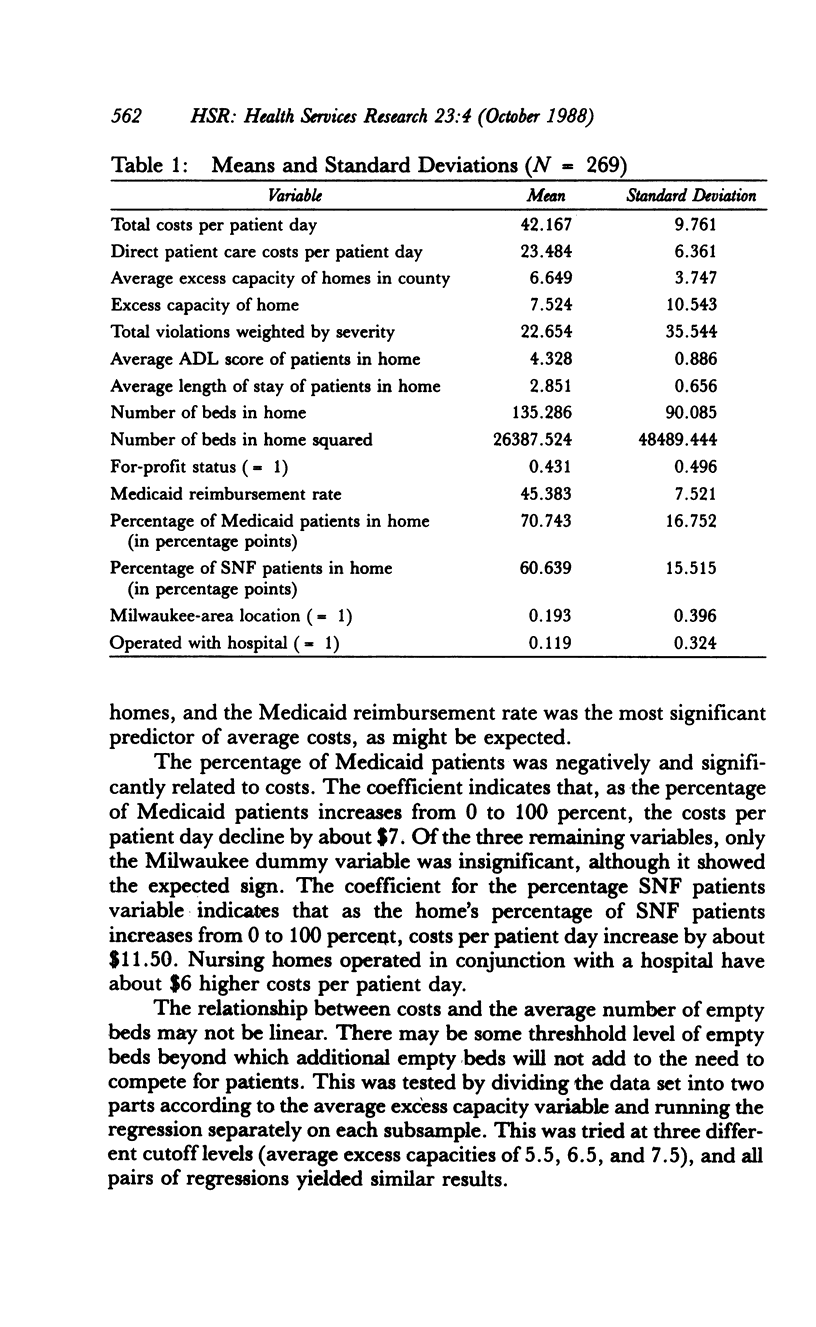
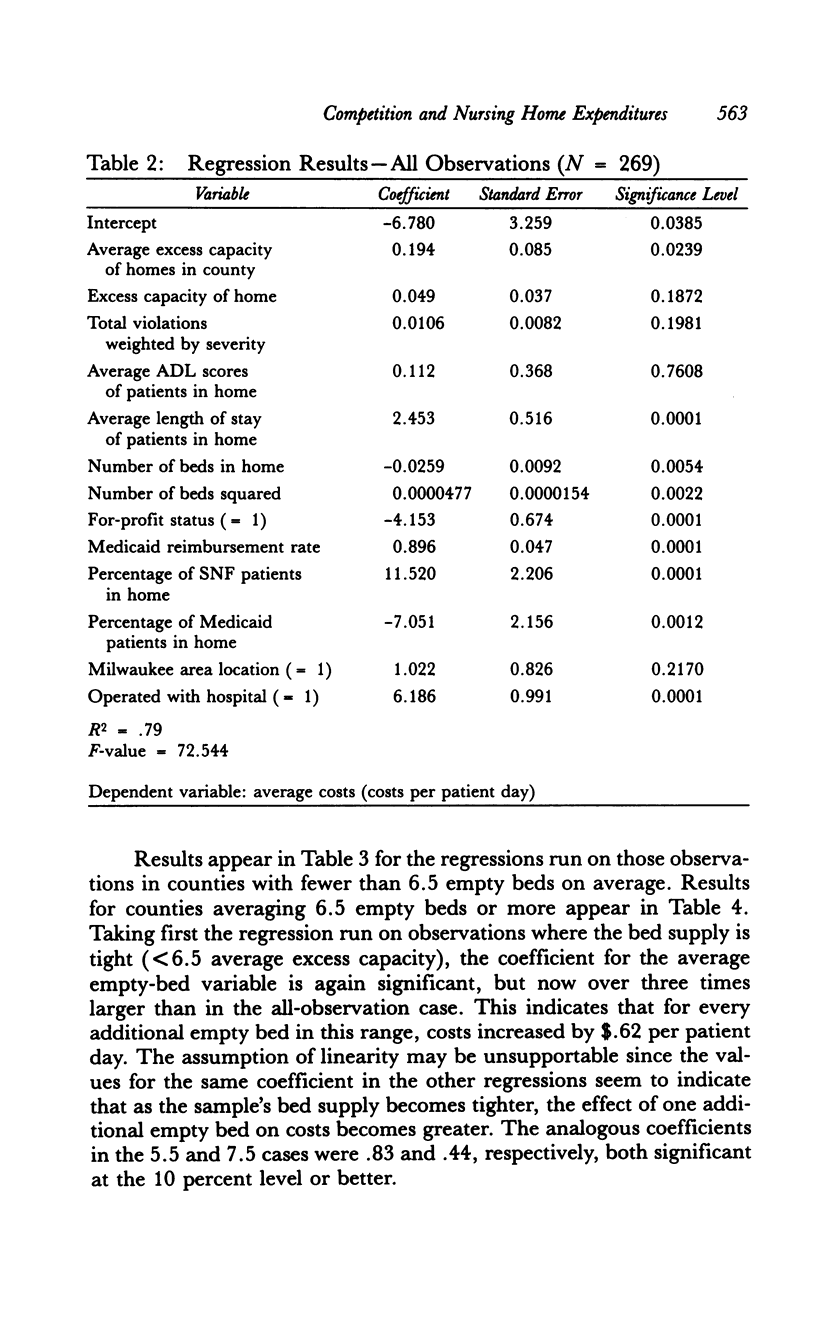
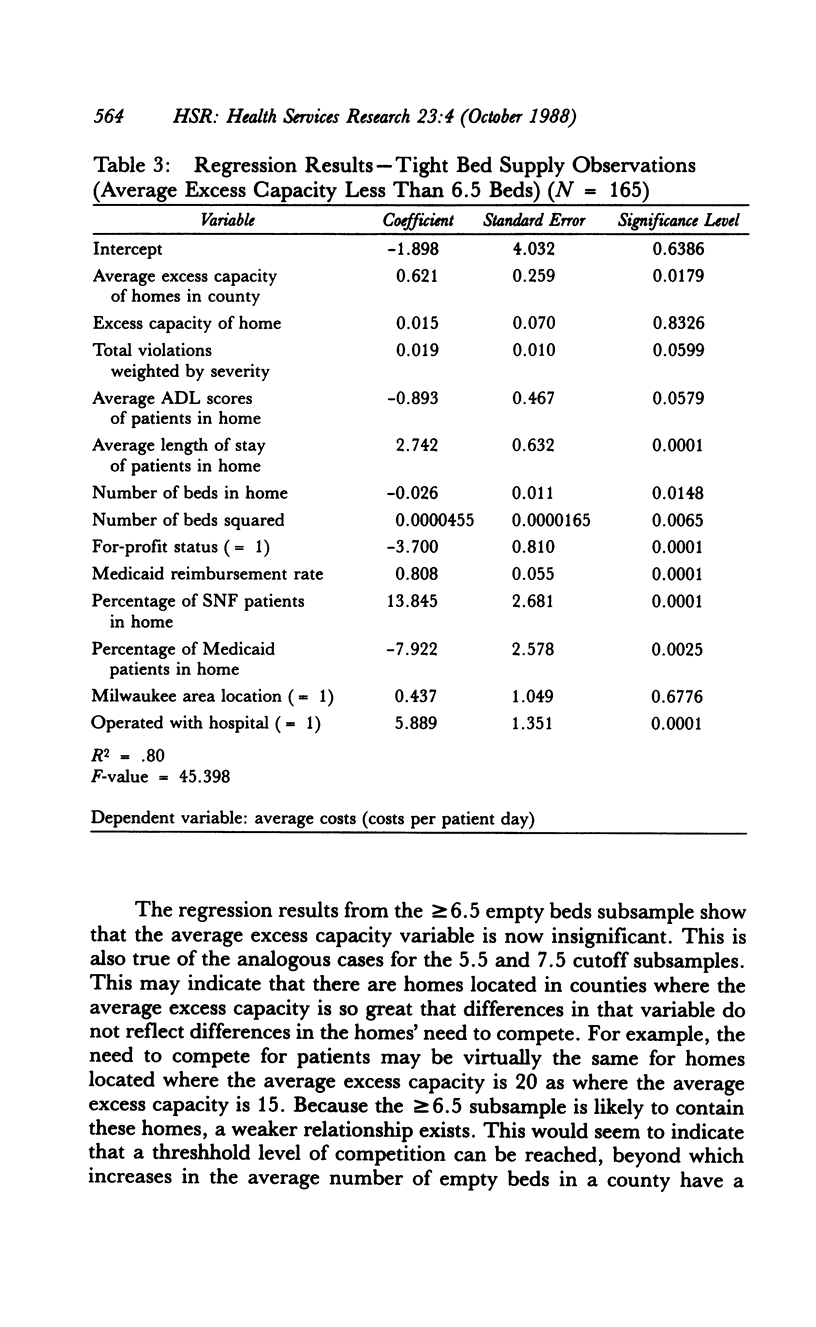
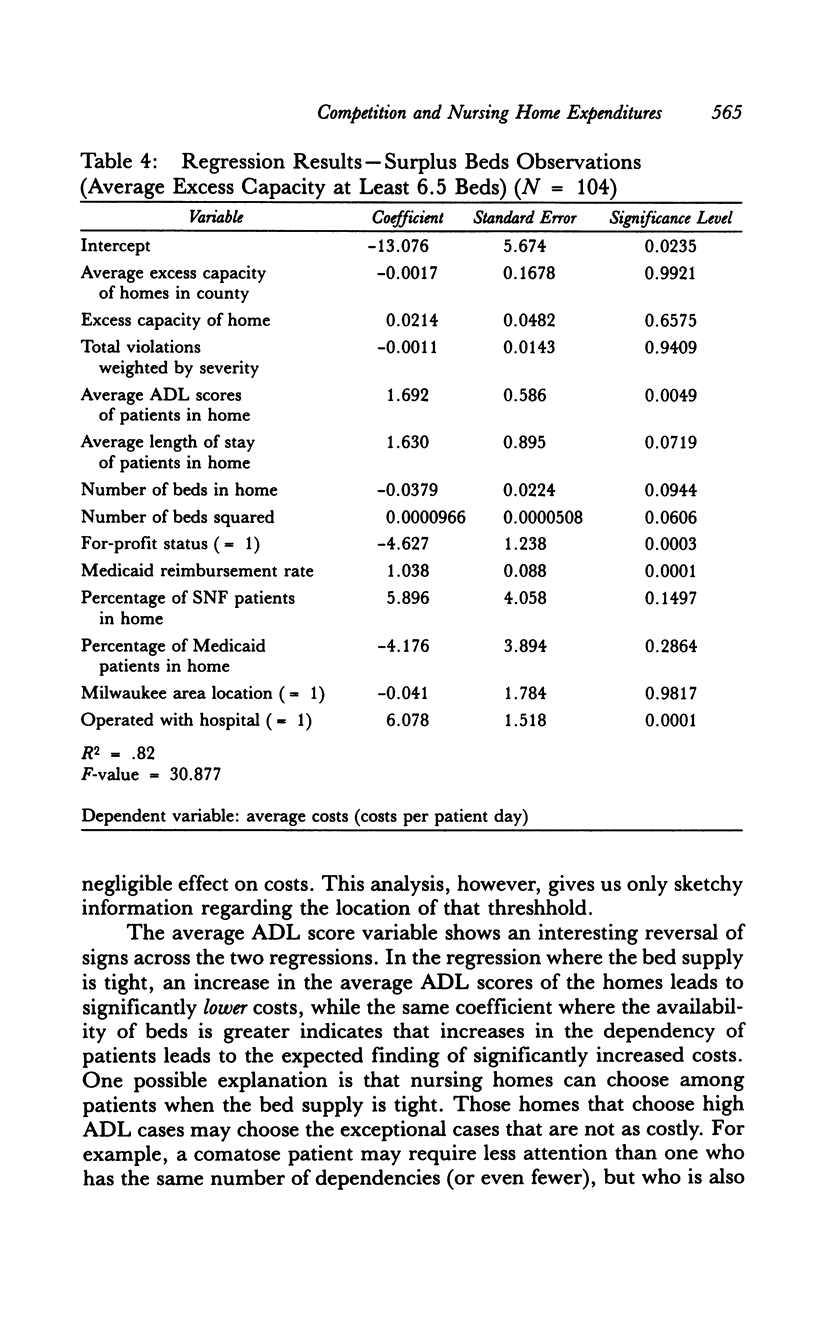
The for-profit nursing home's incentive to minimize costs has been maligned as a major cause of the quality problems that have traditionally plagued the nursing home care industry. Yet, profit-maximizing firms in other industries are able to produce products of adequate quality. In most other industries, however, firms are constrained from reducing costs to the point where quality suffers by the threat of losing business to competing firms. In the nursing home industry, competition for patients often does not exist because of the shortage of nursing home beds. As a result, one would expect that nursing homes located in areas where there is excess demand would spend less on patient care than homes located where the bed supply is relatively abundant. This hypothesis is tested using Wisconsin data from 1983. It is found that, in counties with relatively tight bed supplies, an additional empty bed in all the homes in the county will force each home to increase expenditures by $.62 per day for each patient in the home. Overall, the average nursing home located in underbedded markets would spend $5.12 more per patient day or about $240,000 more annually (in 1983 dollars) if it were located in a market where it was forced to compete for patients. The implications for public policy are discussed.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Birnbaum H., Bishop C., Lee A. J., Jensen G. Why do nursing home costs vary? The determinants of nursing home costs. Med Care. 1981 Nov;19(11):1095–1107. doi: 10.1097/00005650-198111000-00004. [DOI] [PubMed] [Google Scholar]
- Caswell R. J., Cleverley W. O. Cost analysis of the Ohio nursing home industry. Health Serv Res. 1983 Fall;18(3):359–382. [PMC free article] [PubMed] [Google Scholar]
- Christianson J. B. Long-term care standards: enforcement and compliance. J Health Polit Policy Law. 1979 Fall;4(3):414–434. doi: 10.1215/03616878-4-3-414. [DOI] [PubMed] [Google Scholar]
- Lee A. J., Birnbaum H. The determinants of nursing home operating costs in New York State. Health Serv Res. 1983 Summer;18(2 Pt 2):285–308. [PMC free article] [PubMed] [Google Scholar]
- Meiners M. R. An econometric analysis of the major determinants of nursing home costs in the United States. Soc Sci Med. 1982;16(8):887–898. doi: 10.1016/0277-9536(82)90208-8. [DOI] [PubMed] [Google Scholar]
- Palm D. W., Nelson S. The determinants of nursing home costs in Nebraska's proprietary nursing homes. Socioecon Plann Sci. 1984;18(3):171–177. doi: 10.1016/0038-0121(84)90016-8. [DOI] [PubMed] [Google Scholar]
- Ruchlin H. S., Levey S. Nursing home cost analysis: a case study. Inquiry. 1972 Sep;9(3):3–15. [PubMed] [Google Scholar]
- Schlenker R. E. Case mix reimbursement for nursing homes. J Health Polit Policy Law. 1986 Fall;11(3):445–461. doi: 10.1215/03616878-11-3-445. [DOI] [PubMed] [Google Scholar]
- Schlenker R. E., Shaughessy P. W. Case mix, quality, and cost relationships in Colorado nursing homes. Health Care Financ Rev. 1984 Winter;6(2):61–71. [PMC free article] [PubMed] [Google Scholar]
- Smith H. L., Fottler M. D., Saxberg B. O. Does prospective payment encourage nursing home efficiency? Eval Health Prof. 1985 Jun;8(2):209–221. doi: 10.1177/016327878500800206. [DOI] [PubMed] [Google Scholar]
- Ullmann S. G. Cost analysis and facility reimbursement in the long-term health care industry. Health Serv Res. 1984 Apr;19(1):83–102. [PMC free article] [PubMed] [Google Scholar]


