Abstract
Introduction
Obesity is a growing and debilitating epidemic worldwide that is associated with an increased inflammation. It is often linked to rheumatic diseases and may impact negatively their natural history. The use of bariatric and metabolic surgery (BMS) has increased thanks to its positive effect on major comorbidities like diabetes type 2. This systematic review provides the most up-to-date published literature regarding the effect of BMS on outcomes in rheumatoid arthritis.
Methods
This systematic review followed the preferred reporting items for systematic reviews guidelines. Original articles from Pubmed, Embase and Cochrane, published until June 16th 2023, and tackling the effect of BMS on disease outcomes in patients with RA were included.
Results
Three studies met the inclusion criteria. They were published between 2015 and 2022. The total number of RA patients was 33193 and 6700 of them underwent BMS. Compared to non-surgical patients, weight loss after BMS was associated with lower disease activity outcomes at 12 months (p<0.05). Similarly, prior BMS in RA patients was significantly associated with reduced odds ratios for all the morbidities and in-hospital mortality compared with no prior BMS (36.5% vs 54.6%, OR = 0.45, 95% CI (0.42, 0.48), p< 0.001) and (0.4% vs 0.9%, OR = 0.41, 95% CI (0.27–0.61), p < 0.001) respectively.
Conclusion
To conclude, published data indicate that BMS seems a promising alternative in reducing RA disease activity as well as morbidity and mortality in patients with obesity.
1 Introduction
Obesity is a growing and debilitating epidemic worldwide. According to the World Health Organization, one-third of the population suffers from obesity or overweight [1]. Adipose tissue is considered as a highly dynamic organ that maintains normal metabolic function and energy homeostasis. Indeed, there is a close interaction between metabolism and immune system, and a higher body mass index (BMI) is associated with an increased inflammation [2]. More importantly, obesity is often linked to other diseases including rheumatic diseases and may impact negatively their natural history [3]. Particularly, higher levels of adiposity were associated with higher risk of developing rheumatoid arthritis (RA) (RR = 1.25, 95% CI[1.07–1.45], P <0.01) [4]. Similarly, RA patients suffering from obesity were less likely to achieve remission or low disease activity [5]. Indeed, adipocytokines produced by the adipose tissue maintain an inflammatory state in the synoviocytes which makes it difficult to achieve remission [6]. Thus, there is a need for more stringent interventions to reduce weight in this population.
The use of bariatric and metabolic surgery (BMS) has increased thanks to its positive effect on major comorbidities like diabetes type 2 [1]. It is hypothesized that weight loss is associated with a reduction of adipokine levels which improves outcomes in RA [4]. While non-surgical weight loss improved outcomes in RA, the effect of BMS in this context is not well defined [7].
For a more comprehensive assessment, we conducted this systematic review to provide the most up-to-date published literature regarding the effect of BMS on outcomes of RA including disease activity as well as RA morbidity and mortality.
2 Methods
This systematic review followed the preferred reporting items for systematic reviews guidelines. All data analyzed were extracted from published studies. For the present paper, no ethical approval or written informed consent was required. The search strategy, literature selection, and data extraction were conducted by two investigators (SM and YM) independently, then discussed, and any disagreement was resolved by consensus.
2.1 Search strategy
Eligible articles were searched in Medline, Embase, and Cochrane Library. For PubMed, the search was carried out using a strategy employing the combination of the MeSH (Medical Subject Headings) terms. The keywords used were “rheumatoid arthritis”, "Arthritis", "Inflammatory disease", "Immune-mediated rheumatic disease", "Obesity management", “bariatric surgery”, “Gastric Bypass”, “Gastroplasty”, “Patient Reported Outcome Measures”, "Blood Sedimentation", "C-Reactive Protein", “mortality” and “morbidity”. For Embase and Cochrane Library, the previous terms were searched in the article title, abstract, or keywords.
2.2 Selection criteria
A comprehensive search was conducted from inception until June 16th 2023. The inclusion criteria for the present systematic review were: 1) Patients who underwent a BMS. 2) Patients followed for RA with available data on disease outcomes before and after BMS. 3) Comparison of RA outcomes before and after surgery with or without a control group. 5) Cohort studies assessing RA outcomes over time.
Only original articles written in English were considered. Publications not in compliance with this systematic review purpose as well as those not representing original research (i.e.; meta-analyses, reviews, editorials, qualitative papers, case reports, comments, and letters to editors) were excluded. Additional articles were manually retrieved based on the references of selected articles. If any study included overlapping data, the most comprehensive one was selected. After a deep analysis of titles and abstracts, articles unrelated to the inclusion criteria were excluded.
2.3 Data extraction and quality assessment
Extracted data from each study was evaluated independently by both investigators (SM and YM). A pilot-tested extraction form (Zotero) was used by both then compared between the two investigators. The extracted data included the main methodological characteristics of the articles: study data (year of publication, country, study design, number of included subjects, mean age of included subjects, inclusion and exclusion criteria, duration of the follow-up).
Our primary outcome was the evaluation of the effect of BMS on disease activity as well as on morbidity and mortality of RA patients. Furthermore, we identified potential biases of the cohort studies using the Newcastle—Ottawa Quality Assessment Scale. Only studies that met high quality belonged to our final selection.
3 Results
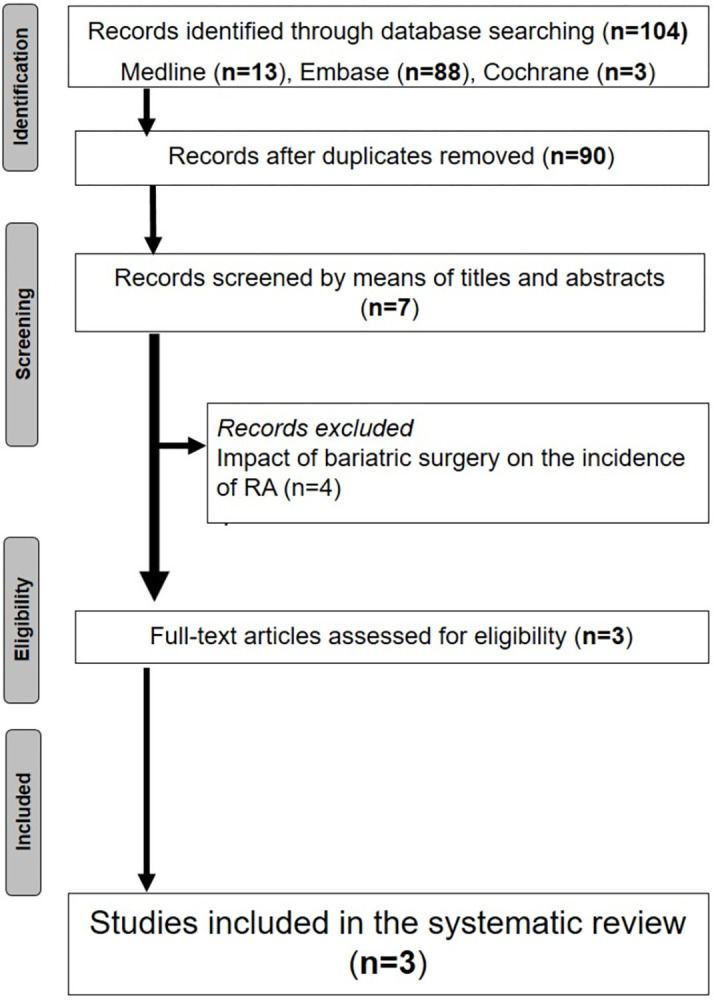
The initial search yielded 103 papers. Following duplicate elimination, we screened for 90 papers. Overall, 3 papers were finally selected for analysis. The flow chart of this systematic review is summarized in Fig 1.
Fig 1. Flow chart outlining the studied protocol.
3.1 Characteristics of the studies
The main characteristics of the 3 studies selected in this systematic review are represented in S1 Table [7–9]. Three studies published between 2015 [7] and 2022 [8] included RA patients who underwent BMS. The studies were conducted in China [9], Boston [7] and Taiwan [8]. Both were cohort studies [7, 9] and the other one a case control study [8]. The control group included patients with obesity who did not receive any intervention. The exclusion criteria were mentioned in only 2 studies. A history of malignancy or problems contraindicating BMS and secondary obesity were cited in the study of Fang et al. [9]. In the study of Sparks and Lin et al., only subjects who had adequate clinical data available before and after BMS were included in the study [7, 8].
3.2 Characteristics of the patients
Overall, 33193 patients were included and the sample sizes varied from 53 [7] to 33,075 [8]. The mean age was 52.1 years. Extremes were mentioned only in one study [8]. The mean number of RA patient who underwent BS was 6700 [32–6617] [8, 9]. The mean disease duration of RA before BS was 9 years with extremes ranging between 8.5 and 10.3 years [7, 9]. The diagnosis criteria applied in the studies were 1987 American College of Rheumatology RA [7], the Classification of Diseases (ICD) codes for RA [8] and the 2010 ACR/EULAR classification criteria [9].
All the selected patients were obese. Anthropometric data was available in two studies. The mean BMI at inclusion and after BS was 43.1 kg/m2 and 29.7 kg/m2 respectively [7, 9], with a mean loss change estimated at -34.2 (p = 0.01).
3.3 The effect of bariatric surgery on disease activity
3.3.1 Inflammatory markers and disease activity outcomes
The effect of BMS on disease activity was reported in two studies [7, 9]. Disease activity was evaluated at 4, 6, 8,12 months all studies combined. The used scores were DAS28 ESR, DAS28 CRP, CDAI and ACR responses [9]. In the study by Sparks et al., validated measures were unavailable in most patients; assessment was based on an agreed upon a priori protocol [7]. Compared to non-surgical patients, weight loss after BMS was associated with lower disease activity. At 12 months post-surgery, 68% of subjects were in remission compared to 26% at baseline (p<0.001) [7]. An ACR20, 50 and 70 response rate were observed in 75.0%, 53.1% and 31.3% in the BMS compared to 51.5%, 39.4%, 21.2% in the non-surgery group (p < 0.01, p < 0.01, p < 0.01) respectively [9]. Regarding acute phase reactants, CRP and ESR were significantly lower at 12 months post-surgery (5.9 mg/L (SD 8.2), 26.1 mm/hr (SD 2.0)) compared to baseline (26.1 mg/L (SD 20.9), 45.7 mm/hr (SD 26.2)), (p<0.05, p<0.001) respectively [7]. In the study by Fang et al., the improvement in PhGA, EGP, CRP and ESR were not precised. The distribution of the different disease activity measures is represented in Table 1.
Table 1. The distribution of disease activity measures at baseline and at follow-up before and after bariatric and metabolic surgery.
| Baseline | 4M | 6M | 8M | 12M | Most recent follow-up (mean 69.6 M) | |||
|---|---|---|---|---|---|---|---|---|
| Fang et al. (2020) | DAS28-ESR (S/NS) mean (SD) | 6.3 (1.4)/ 6.2 (1.0)* | 3.1 (1.2)/4.1 (1.3) * | - | 2.0 (1.5)/ 2.8 (1.1)* | 1.5 (0.9)/ 2.4 (1.4)* | - | |
| DAS28-CRP (S/NS) mean (SD) | 6.6 (3.7)/ 5.8 (2.9)* | 2.9 (2.1)/ 3.8 (1.2)* | - | 1.7 (1.4)/ 2.7 (1.8)* | 1.2 (0.9)/ 2.2 (1.7)* | - | ||
| CDAI (S/NS) mean (SD) | 38.9(24.5)/37.5(21.0)* | 21.4(18.3)/25.3(17.5)* | - | 14.5(8.9)/20.3(14.2)* | 9.5(6.8)/15.8(12.5)* | - | ||
| Weight, kg | 111.8 (11.8) | 92.8 (19.3)** | - | 86.2 (23.7)** | 78.2 (25.6)** | - | ||
| BMI, Kg/m2 | 38.4 (4.8) | 31.9 (10.2)** | - | 29.6 (11.9)** | 26.9 (13.5)** | - | ||
| Sparks et al. (2015) | RA disease activity (%) § | Remission | 26 | - | 72** | - | 68** | 74** |
| Low | 17 | - | 23** | - | 17** | 23** | ||
| Moderate | 51 | - | 4** | - | 6** | 2** | ||
| High | 6 | - | 2** | - | 0** | 0** | ||
| Weight, kg | 128.2 (24.1) | 95.8 (22.0)** | 87.7 (20.0)** | 93.2 (24.0)** | ||||
| BMI, Kg/m2 | 47.8 (7.7) | 35.7 (6.9)** | 32.6 (7.0)** | 34.6 (8.0)** | ||||
*p<0.05
**p<0.01, DAS28: 28-joint count disease activity score; ESR: erythrocyte sedimentation rate, CRP: C-reactive protein, CDAI: clinical disease activity index, S:surgery, NS: non-surgery, M = months, SD: standard deviation.
§ validated measures were unavailable in most patients, assessment was based on an agreed upon a priori protocol
3.3.2 Medication tapering
Medication tapering was reported in two studies [7, 9]. In the study by Fang et al., there was a significant reduction in the use of NSAIDs, Leflunomide, biologics and combination treatment in both surgery and non-surgery groups at 12 months compared to baseline (p < 0.01) (Table 2) [9]. This reduction did not concern corticosteroids, Methotrexate and Sulfasalazine use. Similarly, medication tapering in the bariatric group was not superior to that in non-surgical patients (p>0.05) [9]. In contrast, a significant decrease in the use of NSAIDs, glucocorticoids CsDMARDS and biologics was noted in the study by Sparks et al. [7]. Only one patient was in remission on no RA-related medications at baseline compared to 12 (23%), however this was not statistically significant (p = 0.28) at 12 months. Medication tapering in the different studies is represented in Table 2.
Table 2. Characteristics of patients’ medication at baseline and at 12 months post surgery.
| Fang et al. (M0(%)/M12(%)) | Sparks (M0(%)/M12(%)) | |||
|---|---|---|---|---|
| Surgery | Non surgery | Surgery | Non surgery | |
| CSDMARDs | 96.9/ 88.5 | 93.9/75.0 | 93/59** | - |
| Methotrexate | 87.5 /59.4 | 81.8/71.4 | - | - |
| Sulfasalazine | 15.6/9.4 | 12.1/7.1 | - | - |
| Leflunomide | 56.3/ 19.2** | 45.5/17.9* | - | - |
| Combination | 65.6/28.1* | 57.6 /28.6* | 70/43* | - |
| Biological agents | 43.8/15.6* | 30.3/21.4 | 51/36** | - |
| Glucocrticoids | 12.5/0 | 15.2/ 3.6 | 17/9* | - |
| NSAIDs | 50.0/6.3** | 51.5/25.0* | 45/15* | - |
*P < 0.05 and
**P < 0.01, csDMARDs: conventional disease-modifying anti-rheumatic drug, NSAIDs: non-steroidal anti-inflammatory drugs, M:months
3.4 The effect of bariatric surgery on disease activity on morbidity and mortality
Only the study of Lin et al. assessed this particular aspect [8]. The multivariate analysis of this study showed that prior BMS in RA patients was significantly and independently associated with reduced odds ratios for all the morbidities compared with no prior BMS (OR = 36.5% vs 54.6%, OR = 0.45, 95% CI (0.42, 0.48), p< 0.001)). Similarly, this also concerned in-hospital mortality (0.4% vs 0.9%, OR = 0.41, 95% CI (0.27–0.61), p < 0.001)) [8].
4 Discussion
This systematic review investigated the impact of BS on clinical outcomes such as disease activity, morbidity and mortality in RA patients. The anti-inflammatory role was investigated in other diseases such as systemic lupus erythematosus and multiple sclerosis. Prior BMS was associated with an improvement in clinical course and in-hospitals outcomes compared to non-surgery [10, 11].
The two take-home messages derived from this systematic review are the following: i) Weight loss from BMS was associated with an improvement in disease activity outcomes in RA patients compared with no intervention. ii) RA patients with prior BMS were less likely to develop major morbidities and have a decreased in-hospital mortality compared to RA patients with obesity.
The achievement of an inactive disease state, or at least low disease activity, is the ultimate goal for patients with RA [12]. In addition to medication, non-pharmacological measures including weight loss are also at the core of the management of the disease. Previous studies have demonstrated that obesity decreases the likelihood of achieving a sustained remission despite adequate treatment [13–15]. Indeed, a recent meta-analysis revealed that odds of achieving a sustained remission were reduced by 51% when comparing RA patients with and without obesity [12]. However, results on whether obesity increase the incidence of RA are still conflicting and paradoxal [1, 5, 16–18]. This was particularly debated for the entity seronegative RA and obesity [1]. This may be explained by the marginal role of adipokines in the pathogenesis of RA as evidenced in the study by Qin et al. [4]. Surprisingly, BS seems to be a cause of developing RA.
Only few studies evaluated the role of non-surgical weight loss on RA outcomes [19, 20]. This review highlighted the important role of BMS on reducing serum inflammatory markers and disease activity. Beyond the weight loss itself, BMS seemed to reduce the inflammatory pathway. This was supported by the fact that the adipose tissue produce adipocytokines and inflammatory cytokines, which maintain an inflammatory state in the synoviocytes [6]. Another hypothesis included alterations in the microbiome and hormones, particularly glucagon-like peptide-1, which modulate inflammation in RA disease activity [21].
Similarly, current evidence seems to show improved outcomes in obese patients with other rheumatic disorders after bariatric surgery such as psoriatic arthritis, systemic lupus erythematosus (SLE) and gout [1, 22]. The positive effect was also was extended to a reduction in the use of corticosteroids as well as DMARDs. It is not clear whether the observed medication reduction is due to perioperative medication adjustments to avoid complications or to the bariatric surgery itself. However, 23% remained free of all RA medication one year after BMS in the study by Sparks et al. [7]. This contrasts with prior studies in which only 12% of RA patients remained free of medication two years after clinical remission without any BS [23].
As another highlight of our review, we focused on the effect of BMS on reducing morbidity and mortality of RA patients. The results of the study of Lin et al. including 6615 RA patients were unanimous [8]. BS could be a promising alternative in reducing comorbidities.
To the best of the authors’ knowledge, this is the first systematic review to investigate the effect of BS on different aspects of RA including not only disease activity but also morbidity and mortality. Besides, our systematic review focused also on medication tapering after BS as part of disease activity evaluation.
However, some limitations should be addressed for this review. On the one hand, the number of the investigated studies was limited in the literature. More importantly, such interventions are not risk-free and are not performed as frequently as intended to conduct sufficient trials. Despite that, this review included an adequate number of patients to make statistically significant results and the quality of the studies was rated as high according to the NOS. On the other hand, diagnosis criteria and disease activity outcomes regarding RA varied according to authors. Consequently, comparison and interpretation of the results were difficult. Another potential limitation is the lack of a comparison group that utilized data collected in routine medical care, the non-randomized design as well as the short-term follow-up. Similarly, the doctors and patients were not blinded to the therapeutic strategy.
Finally, some factors such as dietary intake and physical activity were not collected, which might confound the efficacy of BS on disease activity. More importantly, these results should be interpreted with caution. Indeed, some authors showed that bariatric procedures were sometimes associated with an excessive weight loss and therefore an increased risk of death as well as a deleterious effect on bone [1, 24, 25].
Hopefully, future trials should tackle these particular issues. These studies should include more cases and control subjects to ascertain the specific implication of each subset for a better holistic approach.
4.1 Conclusion
Current evidence seems to show improved outcomes in RA patients with obesity one year after BMS. More rigorous prospective controlled studies with long follow-up are needed to ascertain the beneficial effect of such interventions.
Supporting information
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
Registration and protocol: The study is registered (PROSPERO) CRD42023437401
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Lespessailles E, Hammoud E, Toumi H, Ibrahim-Nasser N. Consequences of bariatric surgery on outcomes in rheumatic diseases. Arthritis Res Ther. déc 2019;21(1):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Müller-Ladner U, Frommer K, Karrasch T, Neumann E, Schäffler A. Der Einfluss von Adipositas auf die Krankheitsaktivität bei entzündlich rheumatischen Erkrankungen. Z Rheumatol. mai 2021;80(4):353–61. [DOI] [PubMed] [Google Scholar]
- 3.Gómez R, Conde J, Scotece M, Gómez-Reino JJ, Lago F, Gualillo O. What’s new in our understanding of the role of adipokines in rheumatic diseases? Nat Rev Rheumatol. sept 2011;7(9):528–36. doi: 10.1038/nrrheum.2011.107 [DOI] [PubMed] [Google Scholar]
- 4.Qin B, Yang M, Fu H, Ma N, Wei T, Tang Q, et al. Body mass index and the risk of rheumatoid arthritis: a systematic review and dose-response meta-analysis. Arthritis Res Ther. déc 2015;17(1):86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Linauskas A, Overvad K, Symmons D, Johansen MB, Stengaard‐Pedersen K, Thurah A. Body Fat Percentage, Waist Circumference, and Obesity As Risk Factors for Rheumatoid Arthritis: A Danish Cohort Study. Arthritis Care Res. juin 2019;71(6):777–86. [DOI] [PubMed] [Google Scholar]
- 6.Tolusso B, Alivernini S, Gigante MR, Ferraccioli G, Gremese E. Biomolecular features of inflammation in obese rheumatoid arthritis patients: management considerations. Expert Review of Clinical Immunology. 2 juill 2016;12(7):751–62. [DOI] [PubMed] [Google Scholar]
- 7.Sparks JA, Halperin F, Karlson JC, Karlson EW, Bermas BL. Impact of Bariatric Surgery on Patients With Rheumatoid Arthritis: Bariatric Surgery and RA. Arthritis Care & Research. déc 2015;67(12):1619–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin IC, Liu H. Impact of Bariatric Surgery on Outcomes of Patients with Rheumatoid Arthritis: a Propensity Score–Matched Analysis of US Nationwide Inpatient Sample, 2005–2018. OBES SURG. sept 2022;32(9):2966–74. doi: 10.1007/s11695-022-06177-8 [DOI] [PubMed] [Google Scholar]
- 9.Xu F, Yu C, Li DG, Yan Q, Zhang SX, Yang XD, et al. The outcomes of bariatric surgery on rheumatoid arthritis disease activity: a prospective cohort study. Sci Rep. 21 févr 2020;10(1):3167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang PC, Ho KC, Ko WC, Lin WN. Impact of prior bariatric surgery on outcomes of hospitalized patients with systemic lupus erythematosus: a propensity score-matched analysis of the U.S. nationwide inpatient sample. Surgery for Obesity and Related Diseases. juin 2023;S1550728923005798. doi: 10.1016/j.soard.2023.06.006 [DOI] [PubMed] [Google Scholar]
- 11.Shahsavan M, Amr B, Chiappetta S, Kermansaravi M. Effect of Metabolic and Bariatric Surgery on the Clinical Course of Multiple Sclerosis in Patients with Severe Obesity: a Systematic Review. OBES SURG. juill 2023;33(7):2219–28. doi: 10.1007/s11695-023-06633-z [DOI] [PubMed] [Google Scholar]
- 12.Liu Y, Hazlewood GS, Kaplan GG, Eksteen B, Barnabe C. Impact of Obesity on Remission and Disease Activity in Rheumatoid Arthritis: A Systematic Review and Meta-Analysis: Obesity and RA Outcomes. Arthritis Care & Research. févr 2017;69(2):157–65. [DOI] [PubMed] [Google Scholar]
- 13.Vidal C, Barnetche T, Morel J, Combe B, Daïen C. Association of Body Mass Index Categories with Disease Activity and Radiographic Joint Damage in Rheumatoid Arthritis: A Systematic Review and Metaanalysis. J Rheumatol. déc 2015;42(12):2261–9. doi: 10.3899/jrheum.150224 [DOI] [PubMed] [Google Scholar]
- 14.Schulman E, Bartlett SJ, Schieir O, Andersen KM, Boire G, Pope JE, et al. Overweight, Obesity, and the Likelihood of Achieving Sustained Remission in Early Rheumatoid Arthritis: Results From a Multicenter Prospective Cohort Study. Arthritis Care Res. août 2018;70(8):1185–91. doi: 10.1002/acr.23457 [DOI] [PubMed] [Google Scholar]
- 15.Sandberg MEC, Bengtsson C, Källberg H, Wesley A, Klareskog L, Alfredsson L, et al. Overweight decreases the chance of achieving good response and low disease activity in early rheumatoid arthritis. Ann Rheum Dis. nov 2014;73(11):2029–33. doi: 10.1136/annrheumdis-2013-205094 [DOI] [PubMed] [Google Scholar]
- 16.Maglio C, Zhang Y, Peltonen M, Andersson-Assarsson J, Svensson PA, Herder C, et al. Bariatric surgery and the incidence of rheumatoid arthritis–a Swedish Obese Subjects study. Rheumatology. 1 févr 2020;59(2):303–9. doi: 10.1093/rheumatology/kez275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ljung L, Rantapää-Dahlqvist S. Abdominal obesity, gender and the risk of rheumatoid arthritis–a nested case–control study. Arthritis Res Ther. déc 2016;18(1):277. doi: 10.1186/s13075-016-1171-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ohno T, Aune D, Heath AK. Adiposity and the risk of rheumatoid arthritis: a systematic review and meta-analysis of cohort studies. Sci Rep. 29 sept 2020;10(1):16006. doi: 10.1038/s41598-020-71676-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Engelhart M, Kondrup J, Høie LH, Andersen V, Kristensen JH, Heitmann BL. Weight reduction in obese patients with rheumatoid arthritis, with preservation of body cell mass and improvement of physical fitness. Clin Exp Rheumatol. 1996;14(3):289–93. [PubMed] [Google Scholar]
- 20.Sadeghi A, Tabatabaiee M, Mousavi MA, Mousavi SN, Abdollahi Sabet S, Jalili N. Dietary Pattern or Weight Loss: Which One Is More Important to Reduce Disease Activity Score in Patients with Rheumatoid Arthritis? A Randomized Feeding Trial. Laranjo M, éditeur. International Journal of Clinical Practice. 29 avr 2022;2022:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen CY, Tsai CY. From endocrine to rheumatism: do gut hormones play roles in rheumatoid arthritis? Rheumatology. 1 févr 2014;53(2):205–12. doi: 10.1093/rheumatology/ket255 [DOI] [PubMed] [Google Scholar]
- 22.Gallo G, Candilio G, De Luca E, Iannicelli A, Sciaudone G, Pellino G, et al. Bariatric Surgery and Rheumatic Diseases: A Literature Review. RRCT. 1 août 2018;13(3):176–83. [DOI] [PubMed] [Google Scholar]
- 23.van den Broek M, Huizinga TW, Dijkmans BA, Allaart CF. Drug-free remission: is it already possible? Current Opinion in Rheumatology. mai 2011;23(3):266–72. doi: 10.1097/BOR.0b013e32834563e3 [DOI] [PubMed] [Google Scholar]
- 24.Baker JF, England BR, Mikuls TR, Sayles H, Cannon GW, Sauer BC, et al. Obesity, Weight Loss, and Progression of Disability in Rheumatoid Arthritis. Arthritis Care Res. déc 2018;70(12):1740–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baker JF, Billig E, Michaud K, Ibrahim S, Caplan L, Cannon GW, et al. Weight Loss, the Obesity Paradox, and the Risk of Death in Rheumatoid Arthritis: WEIGHT LOSS AS A PREDICTOR OF DEATH IN RA. Arthritis & Rheumatology. juill 2015;67(7):1711–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


