Abstract
Prescription drug use has reached historic highs in the United States—a trend linked to increases in medicalization, institutional factors relating to the health care and pharmaceutical industries, and population aging and growing burdens of chronic disease. Despite the high and rising prevalence of use, no estimates exist of the total number of years Americans can expect to spend taking prescription drugs over their lifetimes. This study provides the first estimates of life course patterns of prescription drug use using data from the 1996–2019 Medical Expenditure Panel Surveys, the Human Mortality Database, and the National Center for Health Statistics. Newborns in 2019 could be expected to take prescription drugs for roughly half their lives: 47.54 years for women and 36.84 years for men. The number of years individuals can expect to take five or more drugs increased substantially. Americans also experienced particularly dramatic increases in years spent taking statins, antihypertensives, and antidepressants. There are also important differences in prescription drug use by race and ethnicity: non-Hispanic Whites take the most, Hispanics take the least, and non-Hispanic Blacks fall in between these extremes. Americans are taking drugs over a wide and expanding swathe of the life course, a testament to the centrality of prescription drugs in Americans’ lives today.
Keywords: Prescription drugs, Life course, Demography, Health care
Introduction
Prescription drug use in the United States has reached record levels, reaching 6.3 billion prescriptions—approximately 19 prescriptions for every American— filled in 2020 alone (IQVIA Institute for Human Data Science 2021). Now “the most common therapeutic intervention” (World Health Organization [WHO] 2019), the modern prescription drug only emerged around the mid-twentieth century (Tomes 2005). With few exceptions, most commonly used drugs today were developed after 1950. Beta-blockers were discovered in the mid-1960s, and statins and calcium channel blockers were not introduced until the late 1980s (Chang and Lauderdale 2009; Moser 1997). Our most frequently prescribed drugs are relatively new medical innovations that have quickly become widespread over a short time period.
Prescription drugs have become accepted as an integral part of life in the United States—just under half (45.8%) of all Americans and 85.0% of older adults (aged 60+) interviewed in 2015–2016 indicated having taken prescription drugs in the previous month (Martin et al. 2019). However, we lack a full understanding of how important a role they play over the life course. This study answers the question, How many years can Americans now expect to spend taking prescription drugs? Understanding life course patterns of prescription drug use is particularly important given the high and rising rates of use. Although prescription drugs have contributed to tremendous improvements in health and life expectancy, they are not all equally beneficial or safe. As use has increased, concerns about overutilization, increasing costs, and the potential for negative health impacts have grown.
Background
Drivers of Rising Drug Use
Several factors contribute to high and increasing levels of prescription drug use in the United States. including: population aging and rising burdens of chronic disease, medicalization (when aspects of normal life become viewed as medical conditions to be treated by drugs and other therapies; Conrad 2007), the ascendance of drugs to first-line treatment for an increasing array of medical conditions, the development of new drugs or new uses for existing drugs, and other institutional factors relating to the health care and pharmaceutical industries. Antibiotics, such as penicillin and sulfa drugs, were among the earliest drugs to be developed. As mortality from infectious diseases declined and the burden of chronic diseases rose over the course of the epidemiological transition (Horiuchi 1999; Omran 1971), efforts to treat and prevent chronic diseases, such as cardiovascular disease and cancer, and other conditions (e.g., chronic pain) spurred drug development during the twentieth century (Zajacova et al. 2021; Zimmer and Zajacova 2020).
Increasing medicalization has been the predominant trend in the United States (Conrad 2005). Numerous aspects of daily life are increasingly regarded as conditions requiring medical diagnoses and treatment, especially using prescription drugs. Medicalized phenomena include obesity, substance use, hyperactivity, loneliness, childbirth, pain, and aging (Armstrong 2003; Conrad and Schneider 1992; Owens 2020; Zajacova et al. 2021; Zimmer and Zajacova 2020). Society has come to expect and demand “a pill for every ill” (Busfield 2010: 934). Prescription drugs thus moved from the periphery to the core of medicine. Drugs have become the go-to treatment, a shift reinforced by factors relating to the culture of medicine, changing institutional constraints in health care, and health policy. Increased prescribing is spurred by physicians’ curative orientation and factors that became increasingly salient during the managed care era, including increased time constraints, the tying of physician pay to patient satisfaction, and uncertainty in clinical practice (Busfield 2010; Ho 2017, 2019; Tomes 2005). Insurance providers’ reimbursement policies also constrain treatment options. Prescription drugs, and often specific drug classes, must frequently be tried before or have higher insurance coverage than nondrug therapies. For example, insurers had more generous coverage of opioids and fewer or no requirements for approval relative to non-opioid painkillers for pain-related conditions (Thomas and Ornstein 2017).
Pharmaceutical companies contributed to increased prescribing through physician payments, sponsorship of medical conferences and educational seminars, and direct-to-consumer advertising. Between 1997 and 2016, medical marketing increased from $17.7 to $29.9 billion (Schwartz and Woloshin 2019). Prescription drug advertising was a key driver of this expansion, with 4.6 million advertisements (including 663,000 TV commercials) amounting to $6 billion spent in 2016 alone (Schwartz and Woloshin 2019). Growth of the generic drug market and policies such as Medicare Part D have also increased access to prescription drugs and their affordability (Carr 2017; Catlin et al. 2008; Qato et al. 2008).
The Changing Nature of Drug Use
Individuals increasingly take large quantities of several prescription drugs simultaneously, for long durations, and for a widening array of conditions. Polypharmacy—the concurrent use of multiple prescription drugs—is high and increasing among adults and children (Hales et al. 2018; Kantor et al. 2015; Qato et al. 2018). Older adults have the highest levels of polypharmacy: among adults aged 65+, 42% took five or more prescription drugs in 2012 (IMS Institute for Healthcare Informatics 2013). Contributing factors include high burdens of chronic disease and multimorbidity, the intensification of treatment for chronic diseases, a growing propensity to treat earlier disease stages (e.g., prediabetes), fragmentation in the health care system, and increasing use of drugs to counter side effects of other drugs.
People are taking more drugs for longer durations. The earliest drugs—antibiotics—were typically taken for short periods to treat acute infections. With the rise of chronic diseases, people began to take drugs for extended periods—often from initial diagnosis through the remainder of their lifetimes. For example, individuals with hypertension are expected to take antihypertensive medications for the rest of their lives (Lemelin 1989; van der Wardt et al. 2017). Similarly, the U.K.’s National Health Service states, “You usually have to continue taking statins for life because if you stop taking them, your cholesterol will return to a high level within a few weeks” (National Health Service 2018). Medicalization and expansions in prescription drug use mean that people are being prescribed drugs for more conditions. Antidepressant and other psychotherapeutic drug use has been rising since the 1950s, and hormone therapy for menopause began increasing in the early 1980s (Goldman 2010; López-Muñoz and Alamo 2009).
Although transitioning people off prescription drugs is not presently a routine part of medical care, efforts involving deprescribing—a patient-centered approach to reduce or stop the use of drugs entirely—have intensified (Hill et al. 2020; Rochon et al. 2021). Deprescribing often aims to address polypharmacy among older adults and decrease the use of drugs that are unnecessary, cause adverse effects, or have potential harms outweighing expected benefits (Scott et al. 2015). Evidence indicates that deprescribing interventions have successfully reduced inappropriate medication usage (Bloomfield et al. 2020).
Racial and Ethnic Differences in Drug Use
Racial and ethnic disparities in health care are a long-standing concern. Several studies have documented that racial and ethnic minorities have greater difficulty accessing care, receive lower quality of care, and are less likely to receive routine medical care (Centers for Disease Control and Prevention [CDC] 2004a; Kirby and Kaneda 2010; Schulman et al. 1999; Smedley et al. 2003). These differences persist even after accounting for socioeconomic characteristics and health status, and they contribute to racial and ethnic disparities in health and mortality (CDC 2004b; Williams and Jackson 2005). Prescription drug use is considerably lower among Blacks and Hispanics than non-Hispanic Whites (Smedley et al. 2003). This pattern applies to children and older adults, with one study finding that Black and Hispanic Medicare beneficiaries used 10% to 40% fewer drugs than White beneficiaries with the same chronic conditions (Briesacher et al. 2003; Gaskin et al. 2006; Hahn 1995; Mahmoudi and Jensen 2014). Several studies have documented racial and ethnic disparities in pain treatment and opioid prescribing (Anderson et al. 2009; Burgess et al. 2014; Pletcher et al. 2008). Blacks and Hispanics are less likely to be prescribed painkillers for acute and chronic pain in many settings, including emergency room, ambulatory care, and palliative care settings, and they also receive lower dosages (Meghani et al. 2012; Pletcher et al. 2008). Patterns of psychotropic medication use are mixed. Some studies have found that White children and adults were more likely to be prescribed such drugs than Blacks and Hispanics (Akincigil et al. 2011; Cook et al. 2016; Zito et al. 1998), but others have found that Blacks were more likely to be prescribed antipsychotics (Aggarwal et al. 2012; Segal et al. 1996). Although some studies were based on nationally representative data, others were restricted to small samples from single states, and most did not examine differences over the entire age range. One of this study’s goals is to examine the implications of these patterns for racial and ethnic differences in prescription drug use over the life course.
Although Americans are taking drugs in record quantities, no estimates exist of the total number of years individuals can expect to take prescription drugs over their lifetimes. It is critical to understand a phenomenon that occurs across so much of the life course and whose importance shows no sign of lessening, only increasing. This study provides the first estimates characterizing life course patterns of prescription drug use in the United States between 1996 and 2019. These estimates allow us to identify how much of their lives Americans now spend taking prescription drugs and how these measures have changed over time, with particular attention to differences by gender, race, and ethnicity.
Data and Methods
Data
Data on prescription drug use come from the Medical Expenditure Panel Survey (MEPS), a long-running, annual survey that is nationally representative of the U.S. civilian noninstitutionalized population (Agency for Healthcare Research and Quality 2021). Its sampling frame draws from a subsample of households interviewed in the prior year’s National Health Interview Survey. The MEPS uses a panel design consisting of five interviews covering two calendar years, with a new panel of approximately 15,000 sample households selected each year. A single household respondent provides information about each household member. Multiple panels are used to capture the household’s prescription drug use during each calendar year, but the panel structure is not used for other purposes in this study. The MEPS is the primary source of national estimates of health care use, expenditures, insurance coverage, sources of payment, and access to care (Hill et al. 2014).
The MEPS Prescribed Medicines files provide information on all prescriptions purchased by household members. The drug names and therapeutic classes are supplied by the Multum Lexicon database, which is also used by other surveys (e.g., the National Health and Nutrition Examination Survey and the Health and Retirement Study). The MEPS prescription drug information is based on household reports and, if respondents grant permission, is verified by contacting pharmacies. These reports include all medications prescribed during any health care encounter, including outpatient visits, emergency room visits, and hospital stays (Agency for Healthcare Research and Quality 2019; Hill et al. 2014). I link the Prescribed Medicines files to the MEPS Full-Year Consolidated Data files (Blewett et al. 2019), which provide key demographic characteristics, including sex, birth year, race, and ethnicity.
Advantages of the MEPS include that it is nationally representative, has a large sample size, covers the entire age range, and has high response rates. Several MEPS features give us confidence in the quality of its prescription data. First, households are interviewed in person five times within two years, resulting in an average recall period of just five months (Hill et al. 2011). This is a relatively short period compared with other surveys, which are typically fielded at least one and often multiple years apart. Shorter recall periods are associated with greater reporting accuracy (Boudreau et al. 2004). Accuracy is generally greatest for drugs used to treat chronic or serious conditions (Hill et al. 2011). The MEPS prompts respondents with lists of drugs they reported taking in prior interviews, asks them about both new prescriptions and refills, and asks about prescriptions phoned in by a doctor to a pharmacy (Hill et al. 2011). Respondents are also asked whether medicines were prescribed during specific medical encounters, including emergency room visits, dentist visits, and inpatient stays. The MEPS verifies respondent-reported information using a follow-back survey of pharmacies (Wang et al. 2008). In 2011, 69.7% of households permitted the MEPS to contact their pharmacies (Hill et al. 2014). A validation study of the MEPS data (performed by matching to a sample of Medicare claims) found that the MEPS was highly accurate, with high levels of concordance on prescription drug use (an agreement rate of .97), average number of fills (37.4 in the MEPS vs. 38.2 in the Medicare sample), and mean annual expenditures ($2,426 in the MEPS vs. $2,331 in the Medicare sample) (Hill et al. 2011). The MEPS prescription data are much more accurate than other commonly used surveys, such as the Medicare Current Beneficiary Survey and Consumer Expenditure Surveys, which have higher underreporting rates (Poisal 2003; U.S. Bureau of Labor Statistics 2023).
For each year in 1996–2019, I combine the MEPS data with the corresponding sex-specific period U.S. life tables from the Human Mortality Database (HMD; 2021). For the analyses by race and ethnicity, I combine the MEPS data with the corresponding race-ethnicity-sex-specific period life tables from the National Center for Health Statistics (NCHS) for each year in 2006 (the earliest year they are available) through 2019 (NCHS 2022a).
Methods
The analysis examines three dimensions of prescription drug use: (1) any use versus no use, (2) the number of drugs, and (3) the class of drugs. I start with two descriptive measures: the percentage of people at each age taking any drugs and the age-standardized percentages of people taking zero, one, two, three, four, or five or more drugs. The age standard is the 2010 U.S. population (NCHS 2022b).
Estimates of the number of years individuals can be expected to take prescription drugs are produced using Sullivan’s method, the most widely used method for calculating health expectancies (Sullivan 1971). Sullivan’s method has been used to study many phenomena including disability, loneliness, and health insurance coverage (Jagger and Robine 2011; Kirby and Kaneda 2010; Raymo and Wang 2022). I combine the MEPS data with life tables from the HMD and NCHS to apportion the total number of years lived into years expected to be spent in different states (e.g., taking any prescription drugs, a certain number of drugs, or various classes of drugs). Sullivan’s estimator is consistent and unbiased, and no additional assumptions are required beyond stationarity, the standard life table assumption (Imai and Soneji 2007). In this application, the method takes into account mortality differentials between individuals taking drugs and those not taking drugs and between individuals taking different classes or numbers of drugs. The estimates are independent of population age structure, such that changes in the population age distribution will not drive estimated trends in drug use (Jagger et al. 2014; Mathers 1991).
The general procedure for calculating years of life taking prescription drugs and the share of remaining life expected to be spent taking drugs is outlined below. The measures of years of life taking prescription drugs and the share of remaining life expected to be taking drugs are calculated for the total population by sex for the period 1996–2019 and separately by race and ethnicity (for Non-Hispanic Whites, non-Hispanic Blacks, and Hispanics) and sex for the period 2006–2019. For clarity, I describe the steps for a single sex and racial or ethnic group combination. The number of years an individual surviving to age can expect to take prescription drugs (years lived taking prescription drugs [YLPD]) at ages and older is
where , is the proportion of individuals in age group to taking prescription drugs (from the MEPS), is the number of person-years lived in the age interval to (from the HMD or NCHS life tables), and is the number of survivors to exact age (from the HMD or NCHS life tables). The interpretation of in 2019 is the number of years a newborn in 2019 could expect to spend taking prescription drugs during their lifetime if, at each age, they experienced the prescription drug use prevalence and mortality rates observed in 2019.
The number of years an individual surviving to age can expect to spend not taking drugs (prescription drug-free life expectancy [PDFLE]) at ages and older is
Together, and sum to life expectancy at age .
The share of an individual’s remaining years of life expected to be spent taking prescription drugs is
where is life expectancy at age .
I use a similar approach to calculate the number of years individuals can expect to take one, two, three, four, and five or more prescription drugs. The proportion of individuals in each age group taking any prescription drugs is apportioned such that
and the expected number of years taking zero, one, two, three, four, and five or more drugs sum to overall life expectancy at age .
To investigate the number of years individuals can expect to spend taking different types of drugs, I calculate proportions specific to drug (sub)classes specified by the Multum Lexicon therapeutic classification system. Each drug is assigned to a primary therapeutic class. A consistent set of therapeutic classes is used to account for changes over time in the classification scheme. I specify 22 mutually exclusive and exhaustive classes of drugs: anti-infectives, antineoplastics, biologicals and immunologic agents, cardiovascular agents (excluding antihypertensives), antihypertensives, central nervous system (CNS) agents (excluding analgesics and opioids), analgesics (excluding opioids), opioids, coagulation modifiers, gastrointestinal agents, genitourinary tract agents, hormones and hormone modifiers, respiratory agents, psychotherapeutic agents (excluding antidepressants and antipsychotics), antidepressants, antipsychotics, metabolic agents (excluding statins), statins, topical agents, alternative medicines, nutritional products, and miscellaneous agents.1 These drug classes include the most commonly used drugs (Kantor et al. 2015), the top five classes in terms of spending (Moeller et al. 2004), and the ones most commonly implicated in adverse drug events (CDC 2023; Shehab et al. 2016). I also examine a subset of drugs referred to as “key prescription drugs” expected to be used over the longer term or for more severe or chronic conditions: antineoplastics, biologicals and immunologic agents, cardiovascular agents (excluding antihypertensives), antihypertensives, CNS agents (excluding analgesics and opioids), non-opioid analgesics, opioids, coagulation modifiers, gastrointestinal agents, genitourinary tract agents, hormones and hormone modifiers, respiratory agents, psychotherapeutic agents (excluding antidepressants and antipsychotics), antidepressants, antipsychotics, metabolic agents (excluding statins), and statins. In these analyses, I use an approach similar to the one described previously, using the proportion of individuals in each age group taking each class of drugs.
I conducted all analyses using Stata version 16.1 and used MEPS-provided weights to account for complex survey design.
Results
Expected Years and Share of the Life Course Spent Taking Drugs
Prescription drug use has reached very high levels, with more than half of all men (52.2%) and women (62.0%) taking prescription drugs in 2019 (percentages are age-standardized). For the subset of key drugs, these figures remain fairly high, at 43.8% and 53.0% for men and women, respectively. Use is strongly patterned by age and sex (panel a, Figure 1). Among men, use decreases between childhood and young adulthood (between ages 1–4 and 20–24) and increases from age 25 onward. In contrast, use increases nearly continuously among women from age 5 onward. At all ages above 40, more than half of men take prescription drugs. Women cross the 50% threshold much earlier: at all ages above 15, the majority of women take prescription drugs.2 These gender differences are partly related to women’s 12% to 24% greater use at reproductive ages. Appendix Figure A1 (shown in the online appendix, along with all other figures and tables designated with an “A”) shows that if hormonal contraceptives were excluded, gender differences would be smaller but would not disappear; at reproductive ages, the reduction in the gender gap would be roughly one third. Other important contributors to gender differences include other hormones, analgesics, and psychotherapeutics.
Fig. 1.
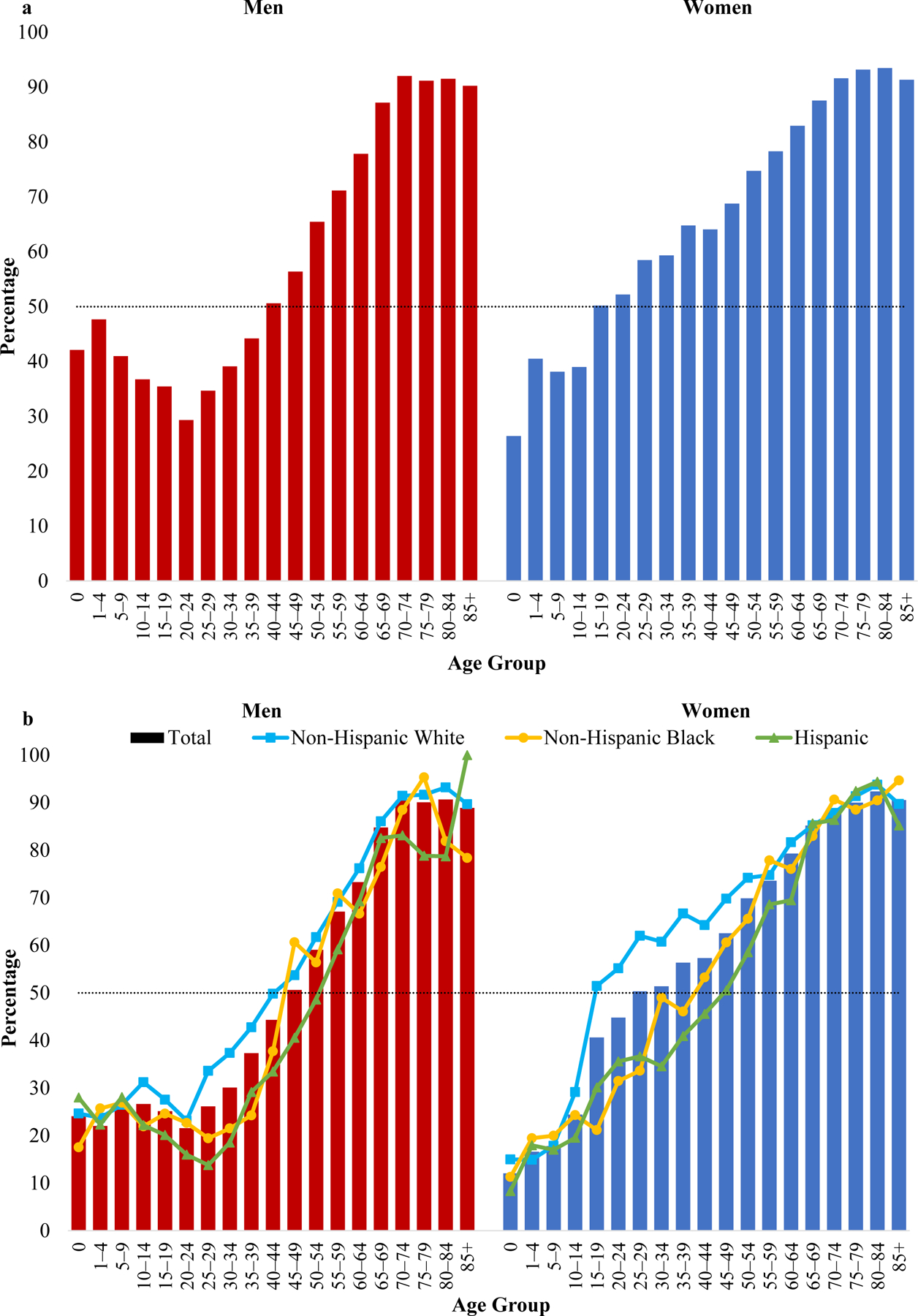
Percentage of Americans taking (a) any prescription drugs by age and sex and (b) key prescription drugs by age, sex, race, and ethnicity in 2019. The key prescription drugs are antineoplastics, biologicals and immunologic agents, cardiovascular agents, CNS agents, coagulation modifiers, gastrointestinal agents, genitourinary tract agents, hormones and hormone modifiers, respiratory agents, psychotherapeutic agents, and metabolic agents. The dashed horizontal line indicates the point at which more than 50% of the population in that age group is taking prescription drugs. Source: Author’s analysis of data from the MEPS, 2019.
Large differences across racial and ethnic groups exist (panel b of Figure 1), with use ramping up at much earlier ages for non-Hispanic Whites than for non-Hispanic Blacks and Hispanics. The age above which the majority of men take prescription drugs is 40 for Whites, 45 for Blacks, and 55 for Hispanics. For women, these disparities are even greater. More than half of all White women older than 15 take drugs, whereas Black and Hispanic women do not reach this rate until they are much older (40 and 45, respectively). Large gaps in use occur between Whites and the two other groups at young and prime adult ages. The percentage of White men taking drugs is an average of 11% to 12% higher at ages 10–44 and 10–84 than for Black and Hispanic men, respectively. The pattern for women is similar, although the differences are larger (at 16% to 18%, on average), and convergence occurs at age 50 for Black women and 65 for Hispanic women.
The percentages shown in Figure 1 translate to a considerable number of years that individuals can be expected to take drugs (Table 1). For example, life expectancy for a newborn boy in 2019 was 76.59 years. Of those years, he could expect to take prescription drugs for 36.84 years (48% of his life) and not to take drugs for the remaining 39.75 years (52% of his life). A newborn girl in 2019, with a life expectancy of 81.72 years, could expect to take prescription drugs for many more years (47.54 years, nearly 60% of her life). The number of years U.S. men and women can expect to spend taking drugs has generally increased at every age during 1996–2019 (the exceptions are for women at ages 0 and 1).
Table 1.
Expected years and percentage of remaining life expectancy taking key prescription drugsa for survivors to each age, by sex and year
| Expected Years Taking Prescription Drugs |
Percentage of Remaining Life Expectancy Taking Prescription Drugs |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men |
Women |
Men |
Women |
|||||||||
| Age | 1996 | 2019 | Changeb | 1996 | 2019 | Changeb | 1996 | 2019 | Changeb | 1996 | 2019 | Changeb |
| 0 | 34.89 | 36.84 | 1.95 | 48.01 | 47.54 | −0.46 | 47.7 | 48.1 | 0.4 | 60.6 | 58.2 | −2.4 |
| 1 | 34.94 | 36.83 | 1.89 | 48.05 | 47.66 | −0.39 | 48.1 | 48.4 | 0.3 | 61.0 | 58.8 | −2.2 |
| 5 | 33.45 | 35.98 | 2.53 | 46.90 | 47.04 | 0.13 | 48.6 | 49.9 | 1.3 | 62.6 | 60.9 | −1.7 |
| 10 | 32.02 | 34.70 | 2.68 | 45.87 | 46.17 | 0.30 | 50.1 | 51.7 | 1.5 | 65.6 | 63.9 | −1.7 |
| 15 | 30.54 | 33.40 | 2.86 | 44.71 | 44.98 | 0.27 | 51.8 | 53.7 | 1.9 | 68.8 | 66.9 | −1.9 |
| 20 | 29.26 | 32.25 | 2.99 | 42.86 | 43.01 | 0.15 | 53.9 | 56.2 | 2.2 | 71.3 | 69.0 | −2.3 |
| 25 | 28.09 | 31.38 | 3.29 | 40.26 | 40.87 | 0.61 | 56.6 | 59.4 | 2.9 | 72.8 | 71.1 | −1.8 |
| 30 | 26.72 | 30.33 | 3.60 | 37.29 | 38.48 | 1.20 | 59.4 | 62.9 | 3.5 | 73.9 | 73.0 | −0.9 |
| 35 | 25.05 | 29.11 | 4.05 | 34.51 | 36.09 | 1.58 | 62.0 | 66.7 | 4.7 | 75.6 | 75.3 | −0.3 |
| 40 | 23.56 | 27.57 | 4.01 | 31.73 | 33.48 | 1.75 | 65.6 | 70.5 | 4.8 | 77.6 | 77.5 | −0.1 |
| 45 | 21.84 | 25.73 | 3.90 | 29.09 | 30.88 | 1.79 | 69.4 | 74.3 | 4.9 | 80.3 | 80.1 | −0.2 |
| 50 | 19.69 | 23.68 | 3.99 | 26.02 | 28.10 | 2.07 | 72.4 | 78.2 | 5.7 | 82.2 | 82.7 | 0.5 |
| 55 | 17.55 | 21.39 | 3.84 | 22.62 | 25.07 | 2.45 | 76.2 | 81.9 | 5.7 | 83.1 | 84.9 | 1.8 |
| 60 | 15.22 | 18.95 | 3.73 | 19.23 | 22.03 | 2.80 | 79.4 | 85.3 | 5.9 | 83.5 | 87.2 | 3.7 |
| 65 | 12.74 | 16.46 | 3.71 | 16.00 | 18.88 | 2.88 | 81.5 | 88.7 | 7.2 | 83.8 | 89.1 | 5.3 |
| 70 | 10.28 | 13.60 | 3.33 | 12.84 | 15.59 | 2.74 | 82.6 | 90.0 | 7.4 | 83.3 | 90.2 | 7.0 |
| 75 | 7.89 | 10.67 | 2.78 | 10.16 | 12.39 | 2.23 | 82.1 | 89.9 | 7.8 | 84.1 | 90.9 | 6.8 |
| 80 | 5.74 | 8.10 | 2.36 | 7.77 | 9.46 | 1.69 | 80.6 | 89.8 | 9.2 | 85.8 | 91.3 | 5.5 |
| 85 | 4.12 | 5.90 | 1.78 | 5.67 | 6.86 | 1.18 | 79.2 | 88.9 | 9.7 | 86.4 | 90.5 | 4.2 |
Source: Data are from the author’s calculations based on the MEPS and the HMD, 1996 and 2019.
Key prescription drugs are antineoplastics, biologicals and immunologic agents, cardiovascular agents, CNS agents, coagulation modifiers, gastrointestinal agents, genitourinary tract agents, hormones and hormone modifiers, respiratory agents, psychotherapeutic agents, and metabolic agents.
Change is calculated as expected years (or percentage of remaining life expectancy) taking prescription drugs in 2019 – expected years (or percentage of remaining life expectancy) taking prescription drugs in 1996.
The share of remaining life expectancy spent taking drugs also increased with age. For example, 25-year-old men and women in 2019 could expect to take prescription drugs for, respectively, 59.4% and 71.1% of their remaining years. For 65-year-old men and women, this share approached 90%. Between 1996 and 2019, the share of remaining life expectancy spent taking drugs increased at every age among men. Among women, it decreased slightly at ages below 50 and increased at ages above 50.
Compared with Whites, Blacks and Hispanics can expect to take prescription drugs for far fewer years (appendix Table A2). For example, in 2019, newborn boys in these groups could expect to take drugs for 39.01, 30.83, and 33.99 years, respectively. The corresponding figures for newborn girls were 50.99, 41.34, and 43.80 years. These differences partly reflect differences in life expectancy. Comparing the proportion of remaining life expectancy spent taking drugs helps account for those differences. Using this metric, I find that Black and Hispanic newborn boys could be expected to spend 43% of their lives taking drugs compared with 51% for White boys in 2019. In 2019, newborn Black and Hispanic girls could be expected to spend roughly 10% less of their lives (53% and 52%, respectively) taking drugs than newborn White girls (63%). These patterns hold through much of the age range, with convergence occurring at roughly age 65 for women and 80 for men.
Trends in the Use of Multiple Drugs
Figure 2 shows trends in the age-standardized percentages of people taking zero, one, two, three, four, and five or more prescription drugs. Most of the change has occurred at the extremes. Declines in the percentage of Americans taking only one drug have been matched by concomitant rises in the percentage taking five or more drugs (panel a, Figure 2). In the mid-1990s, among people taking any drugs, taking only one drug was the modal category. Within a decade, the percentages of people taking one and five or more prescription drugs had converged and remained fairly similar for both men and women through 2019, when they reached, respectively, 14% and 13% for men and 15% and 16% for women. In contrast, the percentages for the intermediate categories (i.e., taking two, three, or four drugs) were fairly stable over time.
Fig. 2.
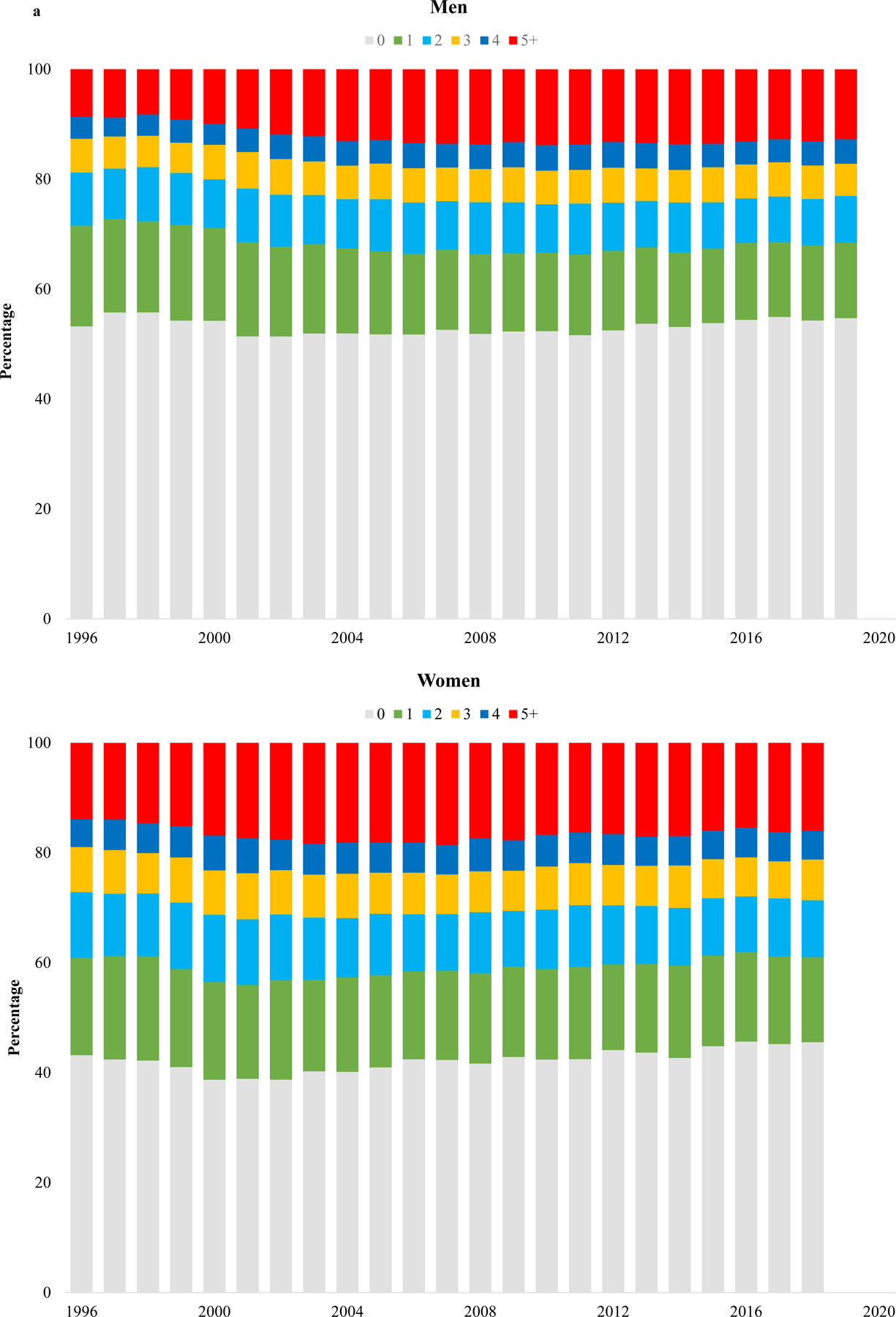
Age-standardized percentage of U.S. men and women taking zero, one, two, three, four, and five or more key prescription drugs (a) for the total population in 1996–2019 and (b) by race and ethnicity in 2006–2019. The key prescription drugs are antineoplastics, biologicals and immunologic agents, cardiovascular agents, CNS agents, coagulation modifiers, gastrointestinal agents, genitourinary tract agents, hormones and hormone modifiers, respiratory agents, psychotherapeutic agents, and metabolic agents. Source: Author’s analysis of data from the MEPS, 1996–2019.
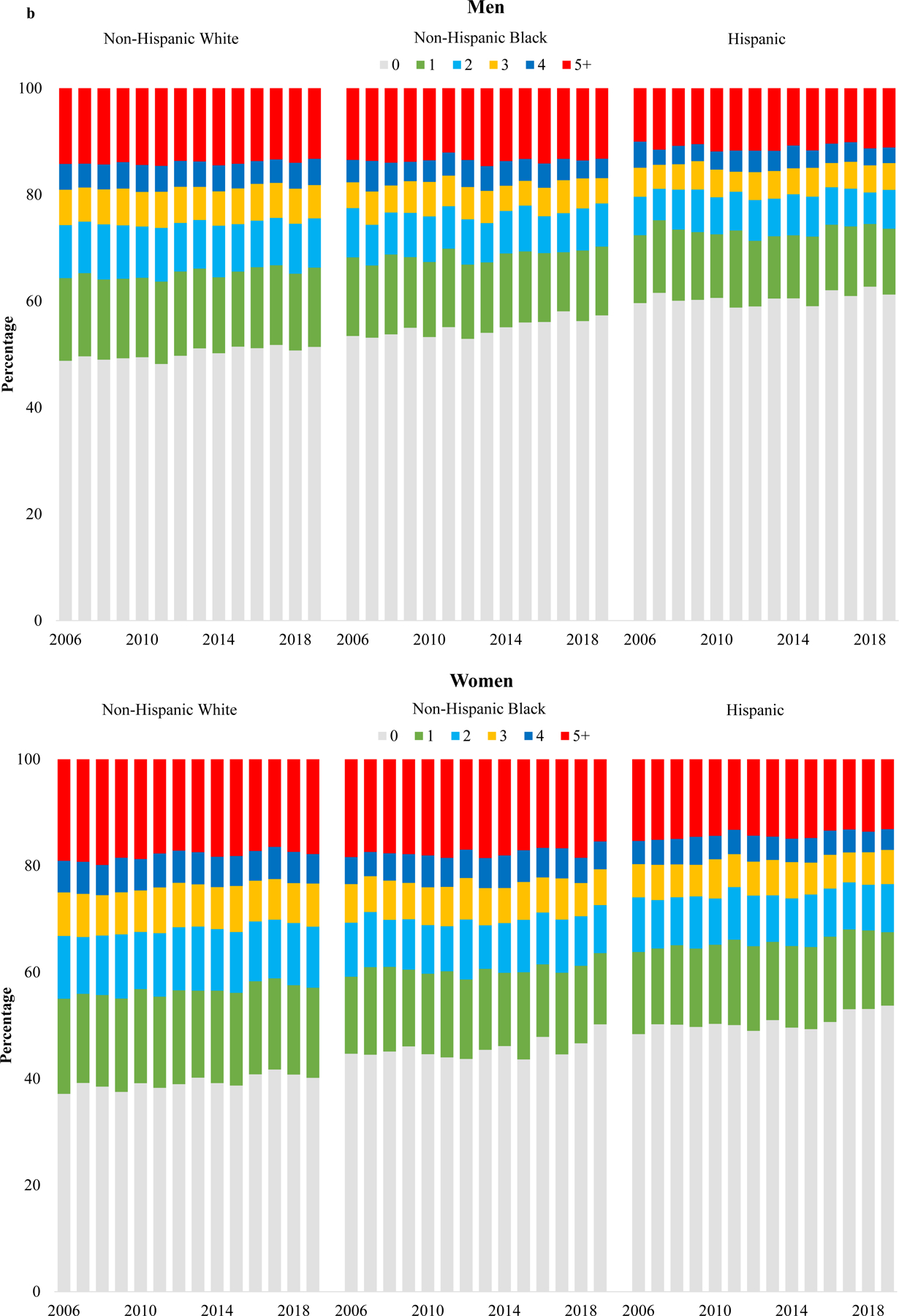
These trends translate into large expansions in the share of life people take large numbers of prescription drugs. Figure 3 shows the years that individuals could expect to take zero, one, two, three, four, and five or more drugs at various ages in 1996 and 2019. With increasing age, many fewer years of remaining life are expected to be spent taking no drugs. The most dramatic change between 1996 and 2019 was the substantial increase in years of taking five or more drugs (red bars) that have occurred at each age. By 2019, the share of Americans’ lives spent taking large numbers of drugs was nontrivial. A newborn boy in 2019 could expect to take five or more drugs for 11.56 years (or 15% of his life), compared with 16.29 years (a fifth of her life) for a newborn girl in 2019. These figures were considerably lower (9% and 16%, respectively) in 1996. Among 85-year-olds in 2019, men and women could expect to take five or more drugs for more than half (52% and 58%, respectively) of their remaining lives, up from 28% and 35%, respectively, in 1996.
Fig. 3.
Expected years taking zero, one, two, three, four, and five or more key prescription drugs at selected ages by sex for the total population in 1996 and 2019. The key prescription drugs are antineoplastics, biologicals and immunologic agents, cardiovascular agents, CNS agents, coagulation modifiers, gastrointestinal agents, genitourinary tract agents, hormones and hormone modifiers, respiratory agents, psychotherapeutic agents, and metabolic agents. Source: Author’s analysis of data from the MEPS and the HMD, 1996 and 2019.
There are important differences in the number of drugs taken across racial and ethnic groups (panel b of Figure 2). Between 2006 and 2019, the percentage taking no prescription drugs was consistently highest among Hispanics, intermediate for Blacks, and lowest for Whites. Correspondingly, the inverse of this pattern was generally replicated across each of the other categories (i.e., Whites had the highest percentages taking one, two, three, and four drugs, followed by Blacks and then Hispanics). Levels of polypharmacy (five or more drugs) were lowest for Hispanics but were very similar for Blacks and Whites. Over this period, the share of Black and White men taking five or more drugs was 14%, compared with 11% for Hispanic men. The corresponding figures for women were 18% and 14%, respectively.
These patterns are reflected in racial and ethnic differences in the proportions of remaining life expectancy expected to be spent taking prescription drugs (appendix Figure A2). Whites could expect not to take drugs for the smallest shares of their lives, whereas Blacks and Hispanics experienced similarly larger shares. For example, among newborns in 2019, White boys could expect not to take drugs for roughly half (49%) their lives, compared with 57% for Black and Hispanic boys. These differences were even larger for women. White newborn girls could expect not to take drugs for only a third (34%) of their lives, compared with 47% and 48% for Black and Hispanic girls, respectively. Similar patterns are observed at age 65, although the magnitudes of the differences are smaller given the racial and ethnic convergence in drug use with age. Interestingly, the distribution across the number of drugs among those taking any drugs is highly similar across racial and ethnic groups. In other words, much of difference across racial and ethnic groups is driven by the larger proportions of Blacks and Hispanics taking no drugs.
Trends in Types of Drugs Used
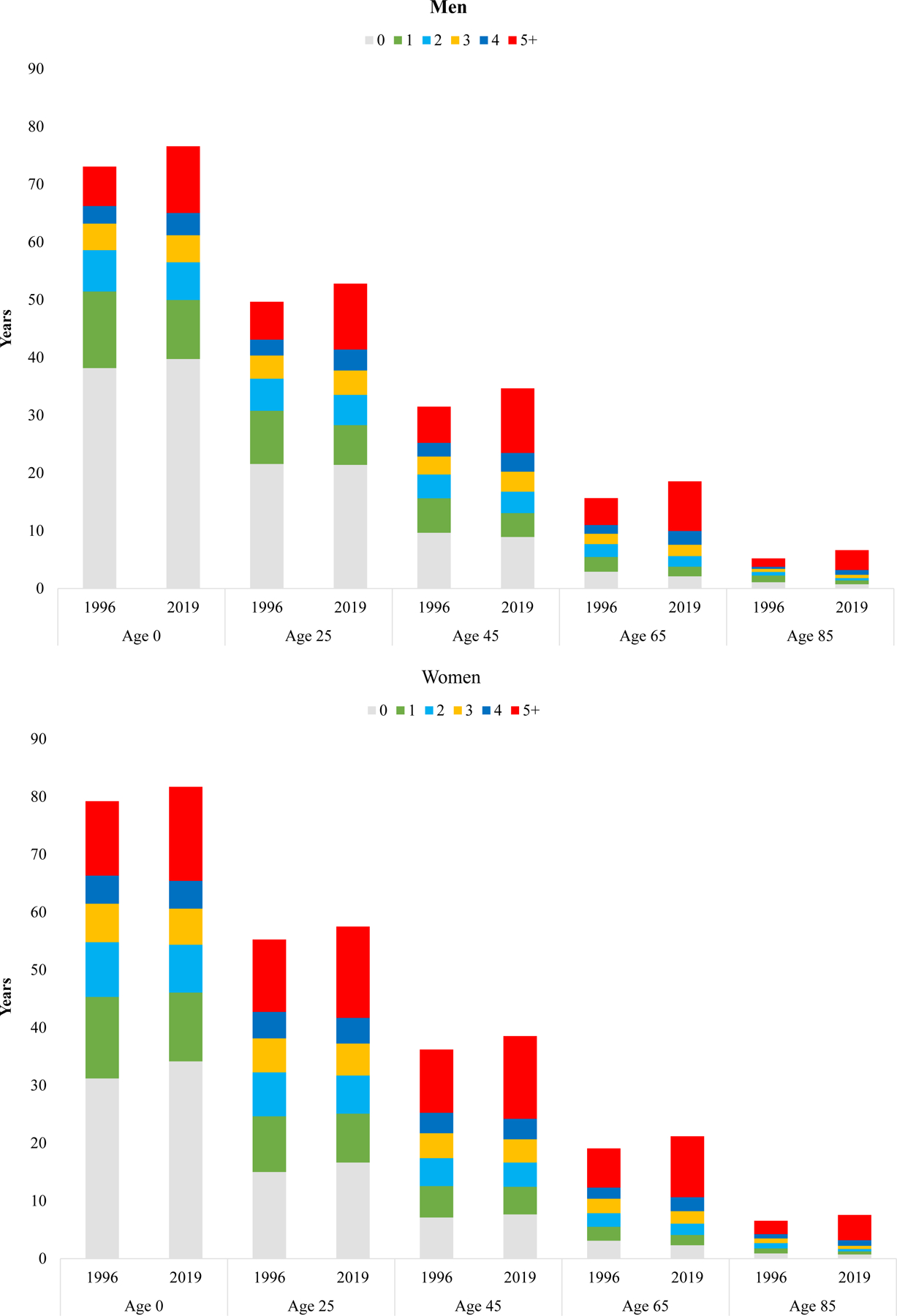
Figure 4 (panels a and b) shows trends in the number of years expected to be spent taking eight common classes of drugs (see also Table 2 and appendix Figures A4–A6). Among these classes, newborns could expect to be taking antihypertensives for the most years, followed by analgesics (through the early 2000s) or statins for men and CNS agents (post-2003) for women. Among 65-year-olds, antihypertensives are taken the most years, followed by statins (since the mid-2000s). Among men, antihypertensive drug use increased tremendously over the period studied. Newborn boys in 1996 could expect to take antihypertensives for 10.14 years; by 2019, this figure reached 17.21 years. Among men aged 65, this figure nearly doubled from 6.67 to 12.18 years. Women experienced large increases in antidepressant use. A newborn girl in 1996 could expect to take antidepressants for 5.55 years; by 2019, this figure more than doubled to 12.52 years. Antidepressant use among older women also grew substantially, from 1.89 to 5.13 years. Men could expect to spend many fewer years taking antidepressants than women—5.42 years for newborn boys (vs. 12.52 years for girls) and 2.29 years for men aged 65 (vs. 5.13 years for women aged 65) in 2019. Use of statins, CNS agents, and other metabolic agents also increased substantially over time. In contrast, years taking other cardiovascular agents remained fairly stable over time among men and decreased among women.
Fig. 4.
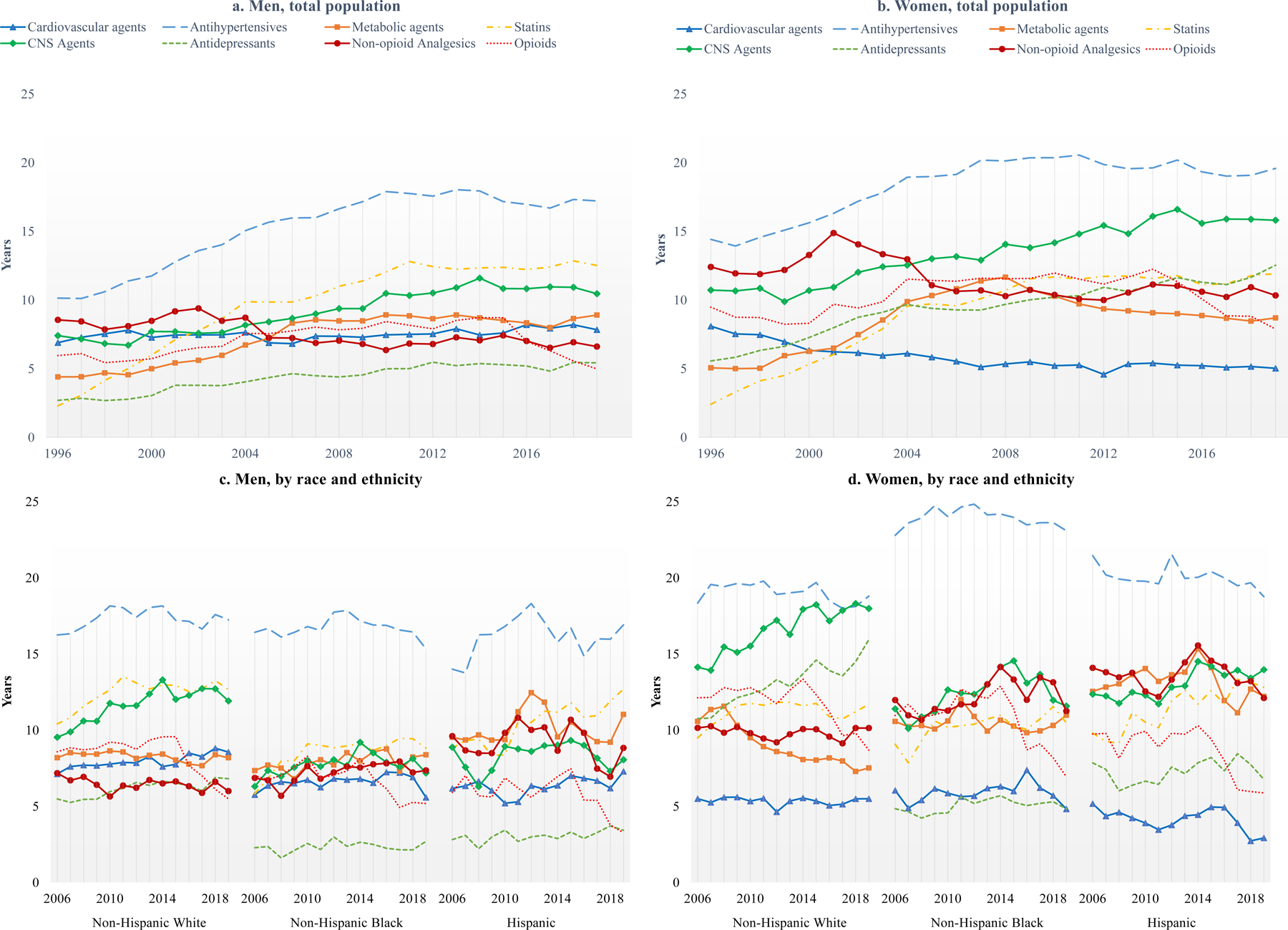
Expected years spent taking common classes of prescription drugs at age 0 by sex (a) for the total population between 1996 and 2019 and (b) by race and ethnicity between 2006 and 2019. Source: Author’s analysis of data from the MEPS, the HMD, and the NCHS, 1996–2019.
Table 2.
Share of remaining life expectancy taking specific classes of prescription drugs at ages 0, 25, 45, 65, and 85 for men and women in 1996 and 2019: Percentages
| Age 0 |
Age 25 |
Age 45 |
Age 65 |
Age 85 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Men | 1996 | 2019 | 1996 | 2019 | 1996 | 2019 | 1996 | 2019 | 1996 | 2019 |
| Cardiometabolic Agents | 21 | 31 | 31 | 44 | 46 | 63 | 61 | 82 | 58 | 80 |
| Cardiovascular agents | 9 | 10 | 14 | 14 | 21 | 21 | 35 | 32 | 42 | 38 |
| Antihypertensives | 14 | 22 | 21 | 33 | 31 | 48 | 43 | 66 | 39 | 65 |
| Metabolic agents | 6 | 12 | 9 | 17 | 14 | 25 | 19 | 33 | 21 | 33 |
| Statins | 3 | 16 | 5 | 24 | 7 | 37 | 8 | 51 | 0 | 52 |
| Psychotherapeutic (total) | 13 | 18 | 15 | 21 | 18 | 25 | 25 | 31 | 37 | 34 |
| CNS agents | 10 | 14 | 12 | 16 | 14 | 20 | 19 | 24 | 26 | 23 |
| Psychotherapeutic agents | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 1 |
| Antidepressants | 4 | 7 | 5 | 9 | 6 | 11 | 8 | 12 | 9 | 13 |
| Antipsychotics | 1 | 1 | 1 | 2 | 1 | 2 | 1 | 2 | 3 | 3 |
| Hormones/Hormone Modifiers | 6 | 9 | 8 | 12 | 10 | 17 | 14 | 24 | 17 | 35 |
| Coagulation Modifiers | 3 | 5 | 4 | 8 | 7 | 12 | 12 | 21 | 14 | 30 |
| Gastrointestinal Agents | 8 | 9 | 11 | 12 | 15 | 17 | 20 | 22 | 21 | 19 |
| Anti-infectives | 28 | 18 | 26 | 19 | 29 | 21 | 33 | 24 | 24 | 20 |
| Respiratory Agents | 16 | 10 | 15 | 10 | 18 | 13 | 19 | 16 | 16 | 18 |
| Non-opioid Analgesics | 12 | 9 | 15 | 11 | 18 | 13 | 18 | 14 | 10 | 13 |
| Opioids | 8 | 7 | 10 | 9 | 11 | 11 | 12 | 12 | 17 | 7 |
| Topical Agents | 20 | 12 | 21 | 14 | 24 | 18 | 33 | 25 | 33 | 26 |
| Nutritional Products | 4 | 4 | 5 | 6 | 7 | 9 | 12 | 13 | 14 | 12 |
| Genitourinary Tract Agents | 1 | 1 | 1 | 1 | 2 | 2 | 2 | 3 | 3 | 2 |
| Biologicals and Immunologic Agents | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 2 | 0 | 2 |
| Antineoplastics | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 2 | 0 | 1 |
| Alternative Medicines | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 |
| Miscellaneous | 0 | 2 | 1 | 3 | 1 | 3 | 1 | 3 | 0 | 2 |
|
| ||||||||||
| Age 0 |
Age 25 |
Age 45 |
Age 65 |
Age 85 |
||||||
| Women | 1996 | 2019 | 1996 | 2019 | 1996 | 2019 | 1996 | 2019 | 1996 | 2019 |
|
| ||||||||||
| Cardiometabolic Agents | 25 | 32 | 35 | 44 | 50 | 60 | 66 | 78 | 78 | 88 |
| Cardiovascular agents | 10 | 6 | 15 | 8 | 21 | 11 | 32 | 16 | 45 | 21 |
| Antihypertensives | 18 | 24 | 26 | 34 | 37 | 48 | 51 | 66 | 60 | 80 |
| Metabolic agents | 6 | 11 | 9 | 15 | 13 | 21 | 18 | 27 | 15 | 25 |
| Statins | 3 | 15 | 4 | 21 | 7 | 31 | 8 | 44 | 3 | 44 |
| Psychotherapeutic (total) | 19 | 27 | 24 | 34 | 27 | 39 | 29 | 42 | 28 | 39 |
| CNS agents | 14 | 19 | 17 | 25 | 20 | 28 | 21 | 32 | 20 | 30 |
| Psychotherapeutic agents | 2 | 1 | 2 | 1 | 2 | 1 | 2 | 0 | 1 | 0 |
| Antidepressants | 7 | 15 | 10 | 20 | 10 | 22 | 10 | 24 | 10 | 22 |
| Antipsychotics | 1 | 2 | 1 | 2 | 1 | 2 | 2 | 2 | 3 | 1 |
| Hormones/Hormone Modifiers | 20 | 17 | 28 | 23 | 38 | 29 | 32 | 32 | 24 | 29 |
| Coagulation Modifiers | 2 | 4 | 3 | 6 | 5 | 9 | 9 | 15 | 11 | 21 |
| Gastrointestinal Agents | 9 | 13 | 13 | 17 | 16 | 23 | 20 | 29 | 18 | 33 |
| Anti-infectives | 34 | 25 | 33 | 26 | 32 | 28 | 30 | 29 | 28 | 25 |
| Respiratory Agents | 20 | 14 | 22 | 15 | 23 | 18 | 20 | 19 | 12 | 18 |
| Non-opioid Analgesics | 16 | 13 | 20 | 16 | 22 | 18 | 21 | 17 | 22 | 18 |
| Opioids | 12 | 10 | 15 | 13 | 15 | 15 | 16 | 18 | 18 | 22 |
| Topical Agents | 25 | 17 | 27 | 20 | 30 | 24 | 32 | 30 | 35 | 31 |
| Nutritional Products | 9 | 8 | 10 | 10 | 11 | 13 | 16 | 17 | 22 | 22 |
| Genitourinary Tract Agents | 1 | 2 | 2 | 3 | 2 | 4 | 2 | 6 | 1 | 6 |
| Biologicals and Immunologic Agents | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 0 |
| Antineoplastics | 5 | 2 | 7 | 3 | 9 | 3 | 6 | 4 | 3 | 3 |
| Alternative Medicines | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 2 | 0 | 5 |
| Miscellaneous | 1 | 3 | 1 | 4 | 1 | 4 | 1 | 3 | 1 | 2 |
Note: Main (nonindented) categories are mutually exclusive and exhaustive.
Source: Data are from the author’s calculations based on the MEPS and the HMD, 1996 and 2019.
Disaggregating patterns by race and ethnicity reveals some similarities but also key differences (Figure 4, panels c and d). Members of all racial and ethnic groups could expect to spend the most years taking antihypertensives. In 2019, years taking antihypertensives were similar among men (with large increases occurring among Hispanics between 2006 and 2019), but Black and Hispanic women actually took antihypertensives for more years than White women. Among men, Whites took cardiovascular agents, CNS agents, and antidepressants for many more years than Blacks and Hispanics. Among women, Whites took cardiovascular agents, CNS agents, antidepressants, and opioids for more years. The discrepancies in antidepressant use are particularly large, amounting to roughly 10-year differences. In 2019, Black and Hispanic women could expect to take antidepressants for 4.83 and 6.76 years, respectively, compared with 15.94 years among White women. Black men and women took statins for the fewest years, but years of statin use were similar for White and Hispanic men and women in 2019.
Trends in opioid use are of interest, given the ongoing drug overdose epidemic and recommendations to reduce opioid prescribing. Although attention surrounding drug overdose increased in the 2000s, culminating in restrictions on opioid prescribing and a shift from prescribed to illicit drugs (Ho 2019; Rudd et al. 2016), the expected number of years spent taking opioids continued to rise through 2015 (Figure 4). Despite subsequent declines in years of life expected to be taking opioids among newborns between 1996 and 2019, expected years of taking opioids remained higher for men and women aged 65 in 2019 than in 1996. Years taking opioids declined from their peak for all racial and ethnic groups. Among men, declines were largest for Hispanics, followed by Whites and then Blacks. Among women, Blacks experienced the largest declines, followed by Hispanics and then Whites.
Figure 5 shows the share of remaining life expectancy at ages 0 and 65 spent taking specific classes of drugs for the total population. (appendix Figure A7 shows the corresponding information by race and ethnicity, with patterns highly similar to those described here.) These classes account for the largest shares of drug use over individuals’ lifetimes (see Table 2 for all drug classes). Individuals can expect to take cardiometabolic drugs, anti-infectives, and psychotherapeutics for the largest shares of their lives. For most of these drugs, the share of remaining life expectancy taking these drugs increases with age. Among men, shares of remaining life expected to be spent taking cardiometabolic drugs, psychotherapeutics, gastrointestinal agents, and coagulation modifiers increased between 1996 and 2019. The share of remaining life expected to be spent taking anti-infectives, topical agents, respiratory agents, and opioids decreased. Similar patterns are observed for women. The share of remaining years taking hormones and hormone modifiers increased for men but decreased for women at ages 0 and 65. Compared with men, women took several types of drugs for considerably greater shares of their lives. For example, women aged 65 and 85 in 2019 could expect to take antidepressants for, respectively, 24% and 22% of their remaining lives. Men could expect to take antidepressants for many fewer years than women: the shares of their lives spent taking antidepressants were roughly half those of women at ages below 85 in 2019. In 1996, a woman aged 85 could expect to take cardiometabolic drugs for 78% of her remaining years, compared with only 58% for a man aged 85. In 2019, a woman aged 45 could expect to take psychotherapeutics for 39% of her remaining lifetime, compared with only 25% for her male counterpart.
Fig. 5.
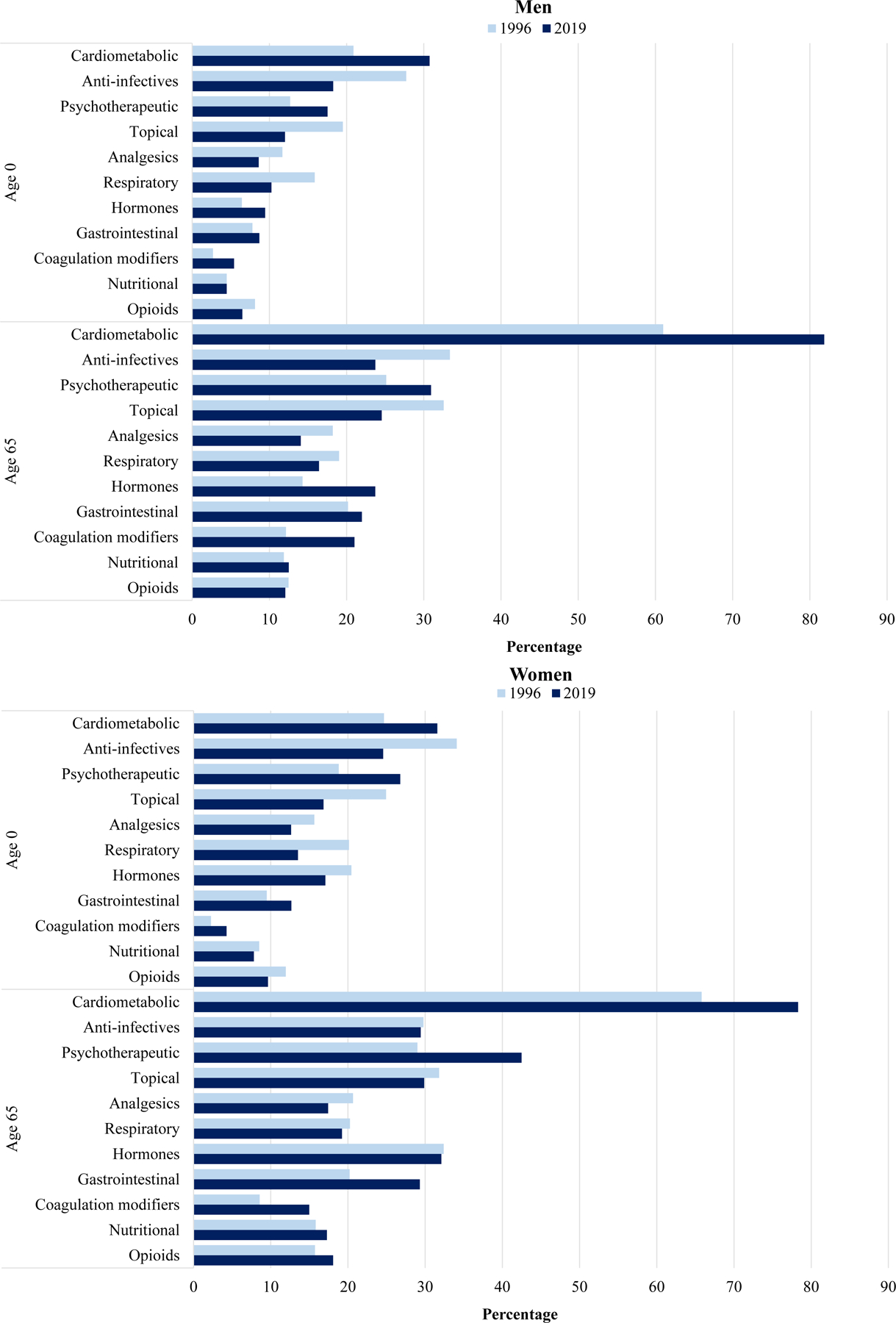
Share of remaining life expectancy spent taking specific classes of prescription drugs at ages 0 and 65 for men and women in 1996 and 2019. Source: Author’s analysis of data from the MEPS and the HMD, 1996 and 2019.
Discussion
Prescription drug use has become a highly central, prevalent, and expanding part of the life course in the United States. However, for a phenomenon that occurs across so much of the life course and has enormous potential to affect health, well-being, and other outcomes, it remains surprisingly understudied. This study finds that newborn girls and boys in 2019 can now expect to spend more than or close to half their lives—47.54 and 36.84 years, respectively—taking prescription drugs. In other words, a newborn girl in 2019 can be expected not to take drugs for only approximately 40% of her life. Even as life expectancy has increased—albeit much more slowly since 2010 than in earlier decades (Ho and Hendi 2018)—the share of Americans’ lives spent taking drugs increased at all ages for men and at all ages above 50 for women between 1996 and 2019. The years Americans can expect to spend taking drugs increased at most ages (except below age 5 for women); the number of years expected to be spent not taking any drugs also increased in some of the younger age groups. With future life expectancy increases, it will be interesting to observe whether those additional years are spent taking or not taking prescription drugs.
High levels of use begin early in the life course. The majority of women older than 15 take prescription drugs; the corresponding age for men is 40. This study also finds that the nature of drug use has shifted considerably over time. The share of Americans’ lives spent simultaneously taking large numbers of drugs is substantial and expanded dramatically over time. In 1996, no men at any age could expect to take five or more drugs for more than a third of their remaining life expectancy. By 2019, men in all age groups above 50 could expect to take five or more drugs for 36% to 53% of their remaining life expectancy. Among women, the maximum share of remaining life taking five or more drugs was 38% in 1996. By 2019, women in all age groups above 50 could expect to take five or more drugs for 40% to 58% of their remaining years.
Americans are taking statins, antihypertensives, and antidepressants for large and growing portions of their lives. In 2019, newborns could be expected to take antihypertensives for nearly a quarter of their lives, compared with two thirds for 65-year-olds. The share of remaining years Americans could be expected to take statins increased more than fourfold at every age, compared with 30% to 68% for antihypertensives. These trends are likely related to several factors, including the growing burden of obesity, longer survival with chronic conditions, and the intensification of treatment of high blood pressure and cholesterol. The rising and potentially unnecessary use of psychotherapeutics, particularly among adolescents, is of growing concern (Richtel 2022). This study finds that the share of newborns’ lives expected to be spent taking antidepressants roughly doubled between 1996 and 2019.
This article documents striking gender differences. At every age, women have much higher rates of prescription drug use than men: women can expect to take drugs for more years and for a greater share of their remaining lifetimes and to take five or more drugs for a greater proportion of their lives. Men and women also take different types of drugs. Large gender differences in the number of years newborns in 2019 could expect to take drugs were observed for psychotherapeutics (8.45 years), particularly antidepressants (7.11 years); hormones and hormone modifiers (6.72 years); anti-infectives (6.09 years); and painkillers (3.73 years) (appendix Table A5). Gender differences in drug use are multifaceted and related to many factors, including the fact that contraceptives remain largely targeted toward women. These patterns also reflect physicians’ long-standing tendencies to prescribe psychotherapeutics (particularly tranquilizers) to women since the late 1800s and early 1900s, Valium in the 1960s and 1970s, and benzodiazepines in recent decades (Courtwright 1982; Herzberg 2006; Olfson et al. 2015). Other factors include gender differences in health care access and utilization, norms relating to care seeking and symptom presentation (especially related to pain relief), and morbidity (e.g., women experience a higher burden of pain-related chronic conditions, such as rheumatoid arthritis, migraines, and fibromyalgia) (Case and Paxson 2005; Ho 2020; Roe et al. 2002). However, there is one class of drugs women take for fewer years of their lives than men: drugs to treat cardiovascular disease. Interestingly, these differences widened, rather than narrowed, over time (appendix Table A5). This widening is concerning in light of prior assessments that gender differences in prescribing may not be evidence-based and studies finding that women are more likely to be prescribed drugs for the management of depression, migraines, thyroid disorders, and other chronic conditions but less likely to be prescribed drugs for cardiovascular disease prevention (Rochon et al. 2021).
This study also reveals complex patterns of racial and ethnic differences in prescription drug use. Use starts much earlier among Whites than among Blacks and Hispanics, with particularly large gaps at the young and middle adult ages among women before convergence at the older ages. As a result, for most of the age range (below ages 65 and 80 for women and men, respectively), Blacks and Hispanics can expect to take no prescription drugs for higher proportions of their remaining lifetimes than Whites. This finding is unlikely to be due to better health among Blacks and Hispanics, given that both groups experience higher mortality than Whites at these ages (Cunningham et al. 2017; Fenelon et al. 2017). Instead, this difference likely reflects inequality across racial and ethnic groups in access to care or receipt of prescriptions. Some phenomena are shared across racial and ethnic groups, including greater levels of use among women than men, high polypharmacy levels, and high rates of antihypertensive use. However, we also observe key racial and ethnic differences in the proportions of life people can expect to spend taking certain classes of drugs (appendix Tables A3 and A4). Use of cardiometabolic drugs generally converged among women but remained lower for Black and Hispanic men than White men, particularly at young and middle adult ages. Black men can be expected to take statins for 4% to 14% less of their lives than White men, which is concerning given Black men’s high rates of cardiovascular disease mortality and that these gaps did not narrow appreciably between 2006 and 2019. Opioid use was similar among Black and White men but lower among Hispanic men. Among women, who take opioids for greater shares of their lives than men, Blacks and Hispanics can generally be expected to take opioids for lower proportions of their lives than Whites. The most sizable differences are observed for psychotherapeutics. For example, newborn White girls in 2019 could be expected to take such drugs for nearly a third (32%) of their lives, compared with 18% and 20% for Black and Hispanic girls, respectively. The magnitudes of these differences are fairly stable over the life course. The patterns for newborn boys in 2019 are similar, although the differences are slightly smaller (e.g., 8% vs. 12–14%).
The study results have implications for health care spending. Prescription drug expenditures are high, reaching $335.0 billion—roughly a tenth of national health expenditures—in 2018 (Centers for Medicare & Medicaid Services 2020; Hartman et al. 2020). Per capita drug spending is higher in the United States than in all other high-income countries (Kesselheim et al. 2016; OECD 2023; Sarnak et al. 2017). Trends in drug use may have outsized impacts on specific programs. Medicare and Medicaid are among the largest payers for prescriptions, which accounted for nearly a fifth of Medicare spending in 2016 (Kaiser Family Foundation 2019). The finding that men and women aged 65 in 2019 could expect to take prescription drugs for an additional 16.46 and 18.88 years—up from 12.74 and 16.00 years in 1996, respectively—is particularly salient for Medicare. For more than half of those 16.46 and 18.88 years, men and women can be expected to take five or more drugs. Out-of-pocket expenditures are also significant, accounting for 14% of drug spending. Not only are current levels of drug spending high, but they are projected to be the fastest-growing category of health care spending in the coming decade (Centers for Medicare & Medicaid Services 2020; Cuckler et al. 2018; Hartman et al. 2020). By 2026, prescription spending is projected to increase to $875 billion, or 15.4% of national health expenditures (Roehrig 2018).
In addition to their fiscal impacts, trends in prescription drug use exert complex influences on health and mortality. On the one hand, prescription drugs are a cornerstone of disease management and contributed to health and life expectancy improvements over the past several decades. On the other hand, the opioid epidemic, which has resulted in over 1 million (1,082,050) drug overdose deaths as of 2021, constitutes one of the starkest manifestations of the unintended consequences of use (CDC 2021a, 2021b). The risks of drug–drug interactions and adverse drug events increase with the number of drugs taken. Each year, adverse drug events result in approximately 1.3 million emergency department visits, with blood thinners, diabetes medications, heart medications, seizure medications, and opioid painkillers most commonly implicated in these events (CDC 2023). Rises in polypharmacy are particularly impactful for older adults, who are at the greatest risk of experiencing negative effects due to their greater likelihood of taking more drugs; metabolic changes associated with aging, including decreased renal and hepatic function; body composition (e.g., lower lean body mass); and higher prevalence of impaired cognition and mobility (IMS Institute for Healthcare Informatics 2013; Masnoon et al. 2017). Polypharmacy increases the risk of falls, hospitalization, cognitive impairment, lower quality of life, and mortality (Maher et al. 2014; Masnoon et al. 2017; WHO 2019). Deprescribing, as mentioned earlier, is an approach that seeks to reduce polypharmacy and inappropriate prescribing. Both domestic (e.g., US Deprescribing Research Network) and international (e.g., International Group for Reducing Inappropriate Medication Use & Polypharmacy) networks provide information and coordinate efforts relating to deprescribing. Several frameworks or decision algorithms have been developed to identify inappropriate medication use and implement deprescribing (Curtin et al. 2021; Farrell et al. 2016; Rochon et al. 2021; Scott et al. 2015). As such efforts become more widespread and accepted, adverse impacts associated with drug use might be reduced (Reeve et al. 2017). Given the high prevalence and initiation of use at younger ages, extending deprescribing efforts beyond older adults may be beneficial.
The environmental impacts of prescription drug use pose additional concerns. The first reports documenting that heart medications, analgesics, contraceptives, and other pharmaceuticals were present in wastewater and other water resources in the United States date from the 1970s (Caban and Stepnowski 2021). One study estimated that 80% of 139 streams sampled in 30 states contained pharmaceuticals in 1999–2000 (Kolpin et al. 2002). Pharmaceutical ingredients have been detected in water supplies worldwide (WHO 2012; Wilkinson et al. 2022). Prescription drugs can make their way into the environment through manufacturing, sewage and wastewater systems from residential areas and health care facilities, and improper disposal of unused or expired medicines (Boxall 2004; WHO 2012). Because wastewater treatment plants do not entirely eliminate pharmaceuticals, people can be exposed to residues in drinking water and food (OECD 2019). Growing antibiotic resistance is also a concern. Studies indicate that the levels present in the environment are below the thresholds that would pose health risks to humans (Boxall 2004; WHO 2012). However, these studies generally study one substance at a time rather than capturing joint or interactive impacts of exposure, are typically of short duration, and rarely examine the effects of long-term, low-level exposure. Furthermore, several commonly used drugs (e.g., beta-blockers, antidepressants, analgesics, and anti-inflammatory drugs) have been found to negatively impact aquatic species and ecosystems (Boxall 2004; Kusturica et al. 2022).
The present study’s limitations include that the MEPS sample is restricted to the noninstitutionalized population and the potential for underreporting in the survey. Because the institutionalized population likely has higher levels of drug use, the estimates produced in these analyses should be conservative. The MEPS attempts to address potential underreporting of prescription drug use by following up with pharmacies, using multiple prompts to elicit information about prescription drug use (including asking respondents to bring medication containers to the interview), and using multiple rounds within each survey wave to enable shorter recall periods that improve reporting accuracy (Boudreau et al. 2004; Hill et al. 2011; Nahin et al. 2019). The MEPS also prompts respondents by asking whether medicines are prescribed during various health care events, including emergency room visits, dentist visits, and inpatient stays (Hill et al. 2014). A validation study of the MEPS based on matching the MEPS to Medicare claims data found the MEPS data to be highly accurate (Hill et al. 2011). Furthermore, accuracy was highest for maintenance drugs and for drugs for serious conditions, which are the categories this study is most interested in capturing. One limitation of Sullivan’s method is that it may underestimate or overestimate health expectancies when transition rates between health states are changing rapidly. Because drug use has been increasing over time, the estimates produced in these analyses are expected to be conservative (Mathers and Robine 1997). Another potential concern is that short-term drug use may inflate estimates of lifetime drug use. However, this concern is somewhat mitigated because most prescription drug use is expected to be permanent rather than transient (Lemelin 1989; National Health Service 2018; van der Wardt et al. 2017). Finally, this article focuses exclusively on prescription drugs, even though over-the-counter medications are also an important feature of medication use.
Over the past several decades, prescription drug use has become a highly central, prevalent, and expanding part of the life course in the United States. Americans today can expect to spend more than or close to half their lives taking prescription drugs. This is more than the share of their lives expected to be spent completing formal education, in a first marriage (Hendi 2019), and perhaps even in the labor force. We are just beginning to be able to observe cohorts of older adults who experienced high, sustained levels of prescription drug use over several decades of their lives, but these conditions are likely to characterize all subsequent cohorts going forward. It will therefore be important to gain a full understanding of how sustained use of high levels of prescription drugs over decades of people’s lives impacts health and well-being over the long run.
Supplementary Material
Acknowledgments
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number R03AG073081. The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Some common examples include amoxicillin (anti-infective), used to treat bacterial infections like pneumonia; digoxin (cardiovascular agent), used to regulate heart rhythms; amlodipine (antihypertensive), used to treat high blood pressure; diazepam (e.g., brand name Valium) and alprazolam (Xanax), which are CNS agents used to treat anxiety, seizures, and panic disorders; naproxen (e.g., Aleve), a non-opioid analgesic, and oxycodone (e.g., OxyContin), an opioid analgesic, used for pain relief; warfarin (coagulation modifier), used to treat and prevent blood clots; omeprazole (e.g., Prilosec), a gastrointestinal agent used for heartburn; oxybutynin (e.g., Oxytrol), a genitourinary tract agent used for overactive bladder; contraceptives containing estrogen or progesterone and corticosteroids, examples of hormones; albuterol (respiratory agent), a bronchodilator used to treat asthma, bronchitis, and chronic obstructive pulmonary lung disease; sertraline (e.g., Zoloft), an antidepressant used for depression, posttraumatic stress disorder, and panic attacks; metformin (metabolic agent), used to treat type 2 diabetes; and atorvastatin (e.g., Lipitor), a statin used for high cholesterol.
This finding holds for the subset of key drugs (panel b of Figure 1). The age at which the majority of the population takes drugs is slightly older (at 45–49 for men and 25–29 for women) but still encompasses a substantial swathe of the life course.
References
- Agency for Healthcare Research and Quality. (2019). MEPS HC-197A: 2017 Prescribed medicines [Dataset documentation] Retrieved from https://meps.ahrq.gov//data_stats/download_data/pufs/h197a/h197adoc.shtml
- Agency for Healthcare Research and Quality. (2021). Medical Expenditure Panel Survey (MEPS) [Data set] Retrieved from https://meps.ahrq.gov/mepsweb/
- Aggarwal NK, Rosenheck RA, Woods SW, & Sernyak MJ (2012). Race and long-acting antipsychotic prescription at a community mental health center: A retrospective chart review. Journal of Clinical Psychiatry, 73, 513–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akincigil A, Olfson M, Siegel M, Zurlo KA, Walkup JT, & Crystal S (2011). Racial and ethnic disparities in depression care in community-dwelling elderly in the United States. American Journal of Public Health, 102, 319–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson KO, Green CR, & Payne R (2009). Racial and ethnic disparities in pain: Causes and consequences of unequal care. Journal of Pain, 10, 1187–1204. [DOI] [PubMed] [Google Scholar]
- Armstrong EM (2003). Conceiving risk, bearing responsibility: Fetal alcohol syndrome and the diagnosis of moral disorder Baltimore, MD: Johns Hopkins University Press. [Google Scholar]
- Blewett LA, Drew JAR, Griffin R, & Williams KCW (2019). IPUMS Health Surveys: Medical Expenditure Panel Survey, Version 1.1 [Data set] Minneapolis, MN: IPUMS. 10.18128/D071.V1.1 [DOI] [Google Scholar]
- Bloomfield HE, Greer N, Linsky AM, Bolduc J, Naidl T, Vardeny O, … Wilt TJ (2020). Deprescribing for community-dwelling older adults: A systematic review and meta-analysis. Journal of General Internal Medicine, 35, 3323–3332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boudreau DM, Daling JR, Malone KE, Gardner JS, Blough DK, & Heckbert SR (2004). A validation study of patient interview data and pharmacy records for antihypertensive, statin, and antidepressant medication use among older women. American Journal of Epidemiology, 159, 308–317. [DOI] [PubMed] [Google Scholar]
- Boxall ABA (2004). The environmental side effects of medication. EMBO Reports, 5, 1110–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briesacher B, Limcangco R, & Gaskin D (2003). Racial and ethnic disparities in prescription coverage and medication use. Health Care Financing Review, 25(2), 63–76. [PMC free article] [PubMed] [Google Scholar]
- Burgess DJ, Nelson DB, Gravely AA, Bair MJ, Kerns RD, Higgins DM, … Partin MR (2014). Racial differences in prescription of opioid analgesics for chronic noncancer pain in a national sample of veterans. Journal of Pain, 15, 447–455. [DOI] [PubMed] [Google Scholar]
- Busfield J (2010). ‘A pill for every ill’: Explaining the expansion in medicine use. Social Science & Medicine, 70, 934–941. [DOI] [PubMed] [Google Scholar]
- Caban M, & Stepnowski P (2021). How to decrease pharmaceuticals in the environment? A review. Environmental Chemistry Letters, 19, 3115–3138. [Google Scholar]
- Carr T (2017, August 3). Too many meds? America’s love affair with prescription medication. Consumer Reports Retrieved from https://www.consumerreports.org/prescription-drugs/too-many-meds-americas-love-affair-with-prescription-medication/
- Case A, & Paxson C (2005). Sex differences in morbidity and mortality. Demography, 42, 189–214. [DOI] [PubMed] [Google Scholar]
- Catlin A, Cowan C, Hartman M, & Heffler S (2008). National health spending in 2006: A year of change for prescription drugs. Health Affairs, 27, 14–29. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2004a). Access to health-care and preventive services among Hispanics and non-Hispanics—United States, 2001–2002. Morbidity and Mortality Weekly Report, 53, 937–941. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2004b). Health disparities experienced by Hispanics—United States. Morbidity and Mortality Weekly Report, 53, 935–937. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2023). Adverse drug events in adults Retrieved from https://www.cdc.gov/medicationsafety/adult_adversedrugevents.html#print
- Centers for Disease Control and Prevention. (2021a). Compressed mortality file 1979–1998 [CDC WONDER Data set] Hyattsville, MD: National Center for Health Statistics. Retrieved from https://wonder.cdc.gov/wonder/help/cmf.html# [Google Scholar]
- Centers for Disease Control and Prevention. (2021b). Underlying cause of death 1999–2020 [CDC WONDER Data set] Hyattsville, MD: National Center for Health Statistics. Retrieved from https://wonder.cdc.gov/ucd-icd10.html [Google Scholar]
- Centers for Medicare & Medicaid Services. (2020, December 31). NHE fact sheet U.S. Department of Health and Human Services. Retrieved from https://www.hhs.gov/guidance/document/national-health-expenditure-nhe-fact-sheet [Google Scholar]
- Chang VW, & Lauderdale DS (2009). Fundamental cause theory, technological innovation, and health disparities: The case of cholesterol in the era of statins. Journal of Health and Social Behavior, 50, 245–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conrad P (2005). The shifting engines of medicalization. Journal of Health and Social Behavior, 46, 3–14. [DOI] [PubMed] [Google Scholar]
- Conrad P (2007). The medicalization of society: On the transformation of human conditions into treatable disorders Baltimore, MD: Johns Hopkins University Press. [Google Scholar]
- Conrad P, & Schneider JW (1992). Deviance and medicalization: From badness to sickness Philadelphia, PA: Temple University Press. [Google Scholar]
- Cook BL, Trinh N-H, Li Z, Hou SS-Y, & Progovac AM (2016). Trends in racial-ethnic disparities in access to mental health care, 2004–2012. Psychiatric Services, 68, 9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtwright DT (1982). Dark paradise: Opium addiction in America before 1940 Cambridge, MA: Harvard University Press. [Google Scholar]
- Cuckler GA, Sisko AM, Poisal JA, Keehan SP, Smith SD, Madison AJ, … Hardesty JC (2018). National health expenditure projections, 2017–26: Despite uncertainty, fundamentals primarily drive spending growth. Health Affairs, 37, 482–492. [DOI] [PubMed] [Google Scholar]
- Cunningham TJ, Croft JB, Liu Y, Lu H, Eke PI, & Giles WH (2017). Vital signs: Racial disparities in age-specific mortality among Blacks or African Americans—United States, 1999–2015. Morbidity and Mortality Weekly Report, 66, 444–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtin D, Gallagher P, & O’Mahony D (2021). Deprescribing in older people approaching end-of-life: Development and validation of STOPPFrail version 2. Age and Ageing, 50, 465–471. [DOI] [PubMed] [Google Scholar]
- Farrell B, Pottie K, Rojas-Fernandez CH, Bjerre LM, Thompson W, & Welch V (2016). Methodology for developing deprescribing guidelines: Using evidence and GRADE to guide recommendations for deprescribing. PLoS One, 11, e0161248. 10.1371/journal.pone.0161248 [AU: FYI...Per style, for journals, we insert doi numbers for those articles that appear solely online—hence the change here and elsewhere.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenelon A, Chinn JJ, & Anderson RN (2017). A comprehensive analysis of the mortality experience of Hispanic subgroups in the United States: Variation by age, country of origin, and nativity. SSM—Population Health, 3, 245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaskin DJ, Briesacher BA, Limcangco R, & Brigantti BL (2006). Exploring racial and ethnic disparities in prescription drug spending and use among Medicare beneficiaries. American Journal of Geriatric Pharmacotherapy, 4, 96–111. [DOI] [PubMed] [Google Scholar]
- Goldman N (2010). Can hormone therapy account for American women’s survival disadvantage? In Crimmins EM, Preston SH, & Cohen B (Eds.), International differences in mortality at older ages: Dimensions and sources (pp. 299–311). Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Hahn BA (1995). Children’s health: Racial and ethnic differences in the use of prescription medications. Pediatrics, 95, 727–732. [PubMed] [Google Scholar]
- Hales CM, Kit BK, Gu Q, & Ogden CL (2018). Trends in prescription medication use among children and adolescents—United States, 1999–2014. JAMA, 319, 2009–2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman M, Martin AB, Benson J, Catlin A, & National Health Expenditure Accounts Team. (2020). National health care spending in 2018: Growth driven by accelerations in Medicare and private insurance spending. Health Affairs, 39, 8–17. [DOI] [PubMed] [Google Scholar]
- Hendi AS (2019). Proximate sources of change in trajectories of first marriage in the United States, 1960–2010. Demography, 56, 835–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herzberg D (2006). “The pill you love can turn on you”: Feminism, tranquilizers, and the valium panic of the 1970s. American Quarterly, 58, 79–103. [Google Scholar]
- Hill L, Prager Geller T, Baruah R, Beattie JM, Boyne J, de Stoutz N, … Jaarsma T (2020). Integration of a palliative approach into heart failure care: A European Society of Cardiology Heart Failure Association position paper. European Journal of Heart Failure, 22, 2327–2339. [DOI] [PubMed] [Google Scholar]
- Hill SC, Roemer M, & Stagnitti MN (2014). Outpatient prescription drugs: Data collection and editing in the 2011 Medical Expenditure Panel Survey (MEPS Methodology Report, No. 29) Rockville, MD: Agency for Healthcare Research and Quality. Retrieved from https://meps.ahrq.gov//data_files/publications/mr29/mr29.shtml [Google Scholar]
- Hill SC, Zuvekas SH, & Zodet MW (2011). Implications of the accuracy of MEPS prescription drug data for health services research. Inquiry, 48, 242–259. [DOI] [PubMed] [Google Scholar]
- Ho JY (2017). The contribution of drug overdose to educational gradients in life expectancy in the United States, 1992–2011. Demography, 54, 1175–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho JY (2019). The contemporary American drug overdose epidemic in international perspective. Population and Development Review, 45, 7–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho JY (2020). Cycles of gender convergence and divergence in drug overdose mortality. Population and Development Review, 46, 443–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho JY, & Hendi AS (2018). Recent trends in life expectancy across high income countries: Retrospective observational study. BMJ, 362, k2562. 10.1136/bmj.k2562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horiuchi S (1999). Epidemiological transitions in human history. In Chamie J (Ed.), Health and mortality: Issues of global concern (pp. 54–71). New York, NY: United Nations. [Google Scholar]
- Human Mortality Database. (2021). Berkeley, CA (USA): University of California, Berkeley; Rostock, Germany: Max Planck Institute for Demographic Research. Available from www.mortality.org [Google Scholar]
- Imai K, & Soneji S (2007). On the estimation of disability-free life expectancy: Sullivan’s method and its extension. Journal of the American Statistical Association, 102, 1199–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IMS Institute for Healthcare Informatics. (2013). Avoidable costs in U.S. healthcare: The $200 billion opportunity from using medicines more responsibly (Report) Parsippany, NJ: IMS Institute for Healthcare Informatics. Retrieved from https://offers.premierinc.com/rs/381-NBB-525/images/Avoidable_Costs_in%20_US_Healthcare-IHII_AvoidableCosts_2013%5B1%5D.pdf [Google Scholar]
- IQVIA Institute for Human Data Science. (2021). The use of medicines in the U.S.: Spending and usage trends and outlook to 2025 (Institute report) Durham, NC: IQVIA. [Google Scholar]
- Jagger C, & Robine J-M (2011). Healthy life expectancy. In Rogers RG & Crimmins EM (Eds.), International handbooks of population: Vol. 2. International handbook of adult mortality (pp. 551–568). Dordrecht, the Netherlands: Springer Science+Business Media. [Google Scholar]
- Jagger C, Van Oyen H, & Robine JM (2014). Health expectancy calculation by the Sullivan method: A practical guide (Report, 4th ed.) Retrieved from http://www.eurohex.eu/pdf/Sullivan_guide_pre%20final_oct%202014.pdf
- Kaiser Family Foundation. (2019, January 29). 10 essential facts about Medicare and prescription drug spending Retrieved from https://www.kff.org/infographic/10-essential-facts-about-medicare-and-prescription-drug-spending/
- Kantor ED, Rehm CD, Haas JS, Chan AT, & Giovannucci EL (2015). Trends in prescription drug use among adults in the United States from 1999–2012. JAMA, 314, 1818–1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kesselheim AS, Avorn J, & Sarpatwari A (2016). The high cost of prescription drugs in the United States: Origins and prospects for reform. JAMA, 316, 858–871. [DOI] [PubMed] [Google Scholar]
- Kirby JB, & Kaneda T (2010). Unhealthy and uninsured: Exploring racial differences in health and health insurance coverage using a life table approach. Demography, 47, 1035–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolpin DW, Furlong ET, Meyer MT, Thurman EM, Zaugg SD, Barber LB, & Buxton HT (2002). Pharmaceuticals, hormones, and other organic wastewater contaminants in U.S. streams, 1999−2000: A national reconnaissance. Environmental Science & Technology, 36, 1202–1211. [DOI] [PubMed] [Google Scholar]
- Kusturica MP, Jevtic M, & Ristovski JT (2022). Minimizing the environmental impact of unused pharmaceuticals: Review focused on prevention. Frontiers in Environmental Science, 10. 10.3389/fenvs.2022.1077974 [DOI] [Google Scholar]
- Lemelin J (1989). Does antihypertensive therapy need to be life-long? Canadian Family Physician / Medecin de Famille Canadien, 35, 1829–1831. [PMC free article] [PubMed] [Google Scholar]
- López-Muñoz F, & Alamo C (2009). Monoaminergic neurotransmission: The history of the discovery of antidepressants from 1950s until today. Current Pharmaceutical Design, 15, 1563–1586. [DOI] [PubMed] [Google Scholar]
- Maher RL, Hanlon J, & Hajjar ER (2014). Clinical consequences of polypharmacy in elderly. Expert Opinion on Drug Safety, 13, 57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmoudi E, & Jensen GA (2014). Has Medicare Part D reduced racial/ethnic disparities in prescription drug use and spending? Health Services Research, 49, 502–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin CB, Hales CM, Gu Q, & Ogden CL (2019). Prescription drug use in the United States, 2015–2016 (NCHS Data Brief, No. 334) Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Masnoon N, Shakib S, Kalisch-Ellett L, & Caughey GE (2017). What is polypharmacy? A systematic review of definitions. BMC Geriatrics, 17, 230. 10.1186/s12877-017-0621-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathers C (1991). Health expectancies in Australia 1981 and 1988 Canberra: Australian Government Publishing Service. [Google Scholar]
- Mathers CD, & Robine JM (1997). How good is Sullivan’s method for monitoring changes in population health expectancies? Journal of Epidemiology and Community Health, 51, 80–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meghani SH, Byun E, & Gallagher RM (2012). Time to take stock: A meta-analysis and systematic review of analgesic treatment disparities for pain in the United States. Pain Medicine, 13, 150–174. [DOI] [PubMed] [Google Scholar]
- Moeller JF, Miller GE, & Banthin JS (2004). Looking inside the nation’s medicine cabinet: Trends in outpatient drug spending by Medicare beneficiaries, 1997 and 2001. Health Affairs, 23, 217–225. [DOI] [PubMed] [Google Scholar]
- Moser M (1997). Evolution of the treatment of hypertension from the 1940s to JNC V. American Journal of Hypertension, 10(S1), 2S–8S. [DOI] [PubMed] [Google Scholar]
- Nahin RL, Sayer B, Stussman BJ, & Feinberg TM (2019). Eighteen-year trends in the prevalence of, and health care use for, noncancer pain in the United States: Data from the Medical Expenditure Panel Survey. Journal of Pain, 20, 796–809. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. (2022a). Life tables Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/nchs/products/life_tables.htm [Google Scholar]
- National Center for Health Statistics. (2022b). Vintage 2020 postcensal estimates of the resident population of the United States (April 1, 2010, July 1, 2010–July 1, 2020), by year, county, single-year of age (0, 1, 2, .., 85 years and over), bridged race, Hispanic origin, and sex [Data set] Centers for Disease control and prevention. Available from: https://www.cdc.gov/nchs/nvss/bridged_race.htm [Google Scholar]
- National Health Service (UK)(2018). Statins Retrieved from https://www.nhs.uk/conditions/statins/
- OECD. (2019). Pharmaceutical residues in freshwater: Hazards and policy responses (OECD Studies on Water report) Paris, France: OECD Publishing. 10.1787/c936f42d-en [DOI] [Google Scholar]
- OECD. (2023). Pharmaceutical spending [Indicator] Retrieved from https://data.oecd.org/healthres/pharmaceutical-spending.htm
- Olfson M, King M, & Schoenbaum M (2015). Benzodiazepine use in the United States. JAMA Psychiatry, 72, 136–142. [DOI] [PubMed] [Google Scholar]
- Omran AR (1971). The epidemiologic transition: A theory of the epidemiology of population change. Milbank Memorial Fund Quarterly, 49, 509–538. [PubMed] [Google Scholar]
- Owens J (2020). Social class, diagnoses of attention-deficit/hyperactivity disorder, and child well-being. Journal of Health and Social Behavior, 61, 134–152. [DOI] [PubMed] [Google Scholar]
- Pletcher MJ, Kertesz SG, Kohn MA, & Gonzales R (2008). Trends in opioid prescribing by race/ethnicity for patients seeking care in U.S. emergency departments. JAMA, 299, 70–78. [DOI] [PubMed] [Google Scholar]
- Poisal JA (2003). Reporting of drug expenditures in the MCBS. Health Care Financing Review, 25(2), 23–36. [PMC free article] [PubMed] [Google Scholar]
- Qato DM, Alexander GC, Conti RM, Johnson M, Schumm P, & Lindau ST (2008). Use of prescription and over-the-counter medications and dietary supplements among older adults in the United States. JAMA, 300, 2867–2878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qato DM, Alexander GC, Guadamuz JS, & Lindau ST (2018). Prescription medication use among children and adolescents in the United States. Pediatrics, 142, e20181042. 10.1542/peds.2018-1042 [DOI] [PubMed] [Google Scholar]
- Raymo JM, & Wang J (2022). Loneliness at older ages in the United States: Lonely life expectancy and the role of loneliness in health disparities. Demography, 59, 921–947. 10.1215/00703370-9937606 [DOI] [PubMed] [Google Scholar]
- Reeve E, Thompson W, & Farrell B (2017). Deprescribing: A narrative review of the evidence and practical recommendations for recognizing opportunities and taking action. European Journal of Internal Medicine, 38, 3–11. [DOI] [PubMed] [Google Scholar]
- Richtel M (2022, August 27). This teen was prescribed 10 psychiatric drugs. She’s not alone The New York Times. Retrieved from https://www.nytimes.com/2022/08/27/health/teens-psychiatric-drugs.html [Google Scholar]
- Rochon PA, Petrovic M, Cherubini A, Onder G, O’Mahony D, Sternberg SA, … Gurwitz JH (2021). Polypharmacy, inappropriate prescribing, and deprescribing in older people: Through a sex and gender lens. Lancet Healthy Longevity, 2, e290–e300. 10.1016/S2666-7568(21)00054-4 [DOI] [PubMed] [Google Scholar]
- Roe CM, McNamara AM, & Motheral BR (2002). Gender- and age-related prescription drug use patterns. Annals of Pharmacotherapy, 36, 30–39. [DOI] [PubMed] [Google Scholar]
- Roehrig C (2018). Projections of the prescription drug share of national health expenditures including non-retail (Research brief) Altarum. Retrieved from https://altarum.org/publications/projections-prescription-drug-share-national-health-expenditures-including-non-retail
- Rudd RA, Aleshire N, Zibbell JE, & Gladden RM (2016). Increases in drug and opioid overdose deaths—United States, 2000–2014. Morbidity and Mortality Weekly Report, 64, 1378–1382. [DOI] [PubMed] [Google Scholar]
- Sarnak DO, Squires D, Kuzmak G, & Bishop S (2017). Paying for prescription drugs around the world: Why is the U.S. an outlier? (Issue brief) Commonwealth Fund. Retrieved from https://www.commonwealthfund.org/sites/default/files/documents/___media_files_publications_issue_brief_2017_oct_sarnak_paying_for_rx_ib_v2.pdf [PubMed] [Google Scholar]
- Schulman KA, Berlin JA, Harless W, Kerner JF, Sistrunk S, Gersh BJ, … Escarce JJ (1999). The effect of race and sex on physicians’ recommendations for cardiac catheterization. New England Journal of Medicine, 340, 618–626. [DOI] [PubMed] [Google Scholar]
- Schwartz LM, & Woloshin S (2019). Medical marketing in the United States, 1997–2016. JAMA, 321, 80–96. [DOI] [PubMed] [Google Scholar]
- Scott IA, Hilmer SN, Reeve E, Potter E, Le Couteur D, Rigby D, … Martin JH (2015). Reducing inappropriate polypharmacy: The process of deprescribing. JAMA Internal Medicine, 175, 827–834. [DOI] [PubMed] [Google Scholar]
- Segal SP, Bola JR, & Watson MA (1996). Race, quality of care, and antipsychotic prescribing practices in psychiatric emergency services. Psychiatric Services, 47, 282–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shehab N, Lovegrove MC, Geller AI, Rose KO, Weidle NJ, & Budnitz DS (2016). U.S. emergency department visits for outpatient adverse drug events, 2013–2014. JAMA, 316, 2115–2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, & Nelson AR (Eds.). (2003). Unequal treatment: Confronting racial and ethnic disparities in health care Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Sullivan DF (1971). A single index of mortality and morbidity. HSMHA Health Reports, 86, 347–354. [PMC free article] [PubMed] [Google Scholar]
- Thomas K, & Ornstein C (2017, September 17). Amid opioid crisis, insurers restrict pricey, less addictive painkillers The New York Times. Retrieved from https://www.nytimes.com/2017/09/17/health/opioid-painkillers-insurance-companies.html?smid=url-share [Google Scholar]
- Tomes N (2005). The great American medicine show revisited. Bulletin of the History of Medicine, 79, 627–663. [DOI] [PubMed] [Google Scholar]
- U.S. Bureau of Labor Statistics. (2023). Medical Expenditure Panel Survey Retrieved from https://www.bls.gov/cex/cecomparison/meps_profile.htm
- van der Wardt V, Harrison JK, Welsh T, Conroy S, & Gladman J (2017). Withdrawal of antihypertensive medication: A systematic review. Journal of Hypertension, 35, 1742–1749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Mullins CD, Zuckerman IH, Walker GD, Suda KJ, Yang Y, & White-Means SI (2008). Medical Expenditure Panel Survey: A valuable database for studying racial and ethnic disparities in prescription drug use. Research in Social Administrative Pharmacy, 4, 206–217. [DOI] [PubMed] [Google Scholar]
- Wilkinson JL, Boxall ABA, Kolpin DW, Leung KMY, Lai RWS, Galbán-Malagón C, … Teta C (2022). Pharmaceutical pollution of the world’s rivers. Proceedings of the National Academy of Sciences, 119, e2113947119. 10.1073/pnas.211394711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Jackson PB (2005). Social sources of racial disparities in health. Health Affairs, 24, 325–334. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2012). Pharmaceuticals in drinking-water (Report) Geneva, Switzerland: World Health Organization. [Google Scholar]
- World Health Organization. (2019). Medication safety in polypharmacy (Technical Report, No. WHO-UHC-SDS-2019.11) Geneva, Switzerland: World Health Organization. [Google Scholar]
- Zajacova A, Grol-Prokopczyk H, & Zimmer Z (2021). Pain trends among American adults, 2002–2018: Patterns, disparities, and correlates. Demography, 58, 711–738. 10.1215/00703370-8977691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmer Z, & Zajacova A (2020). Persistent, consistent, and extensive: The trend of increasing pain prevalence in older Americans. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75, 436–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zito JM, Safer DJ, Dosreis S, & Riddle MA (1998). Racial disparity in psychotropic medications prescribed for youths with Medicaid insurance in Maryland. Journal of the American Academy of Child & Adolescent Psychiatry, 37, 179–184. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


