Abstract
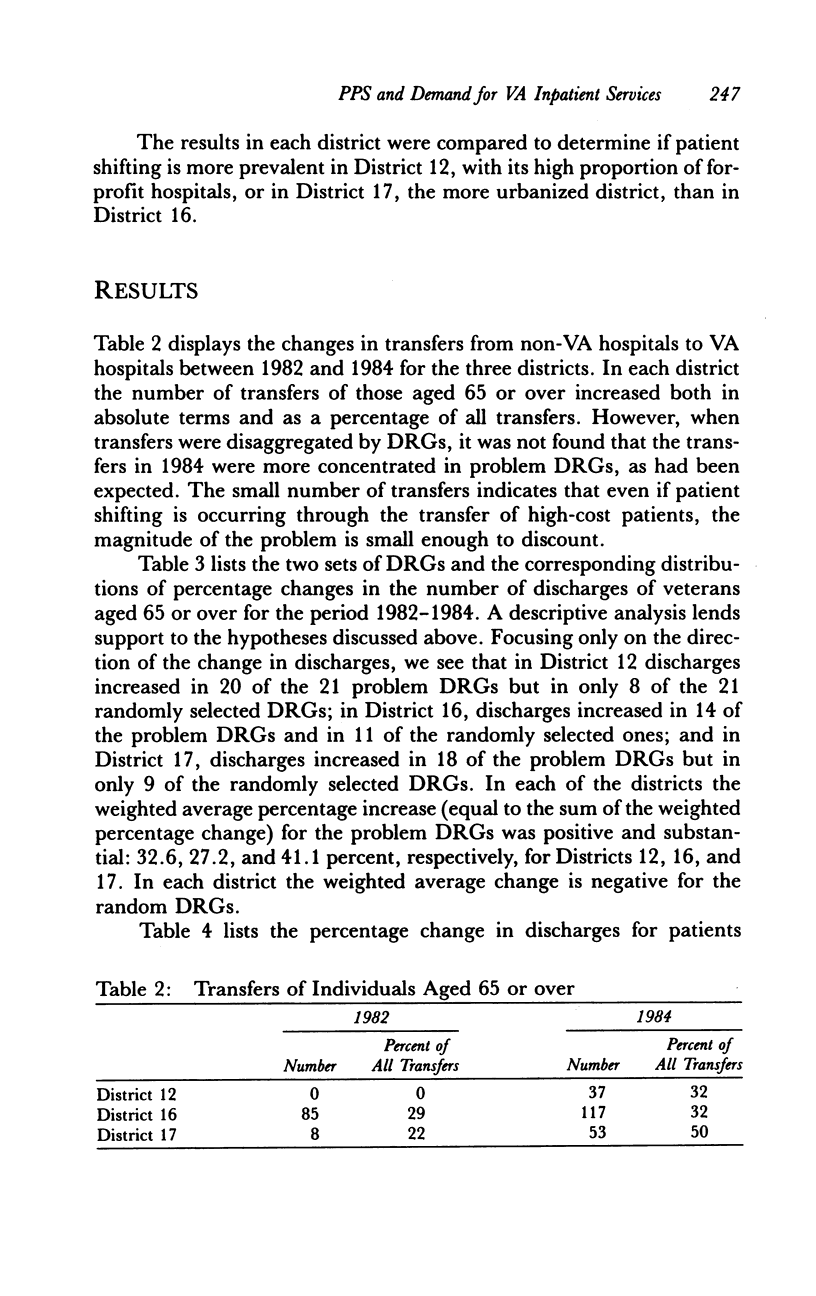
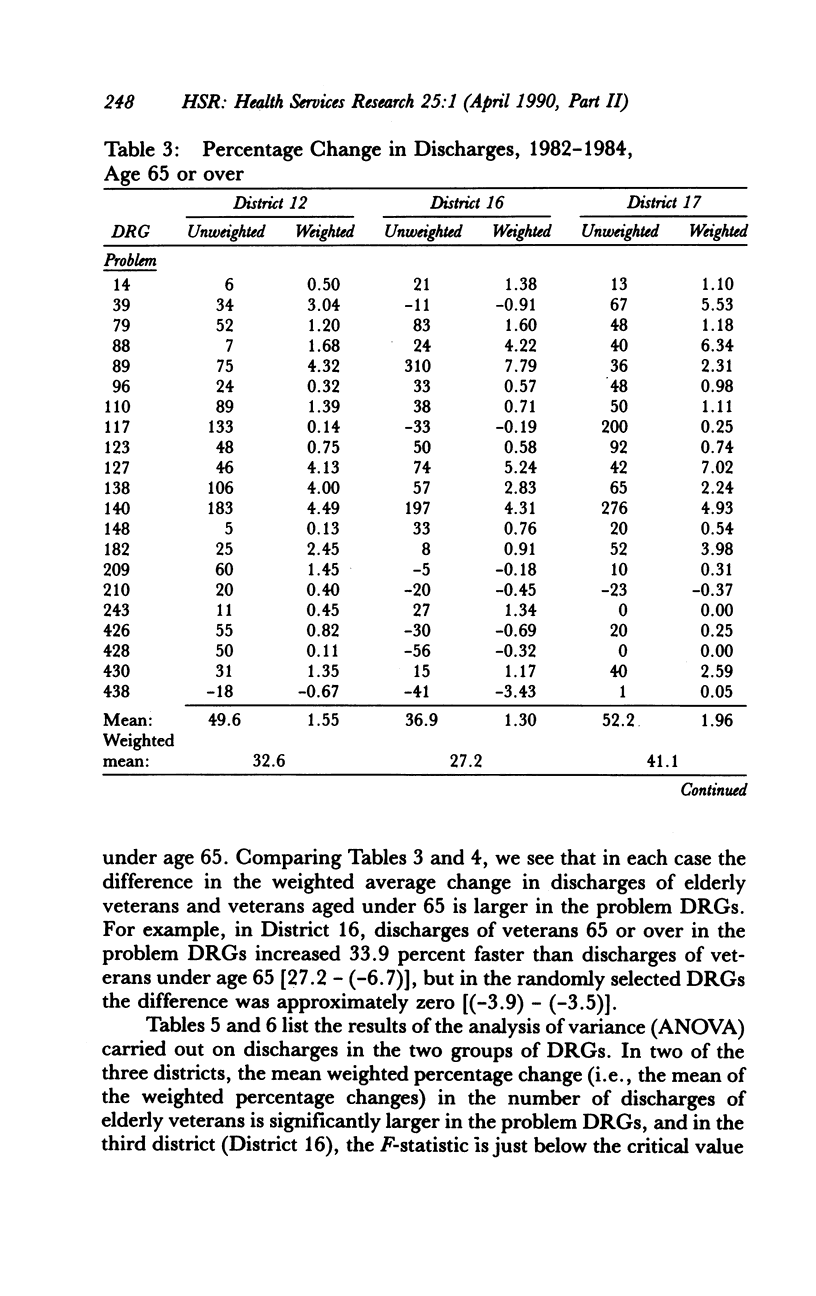
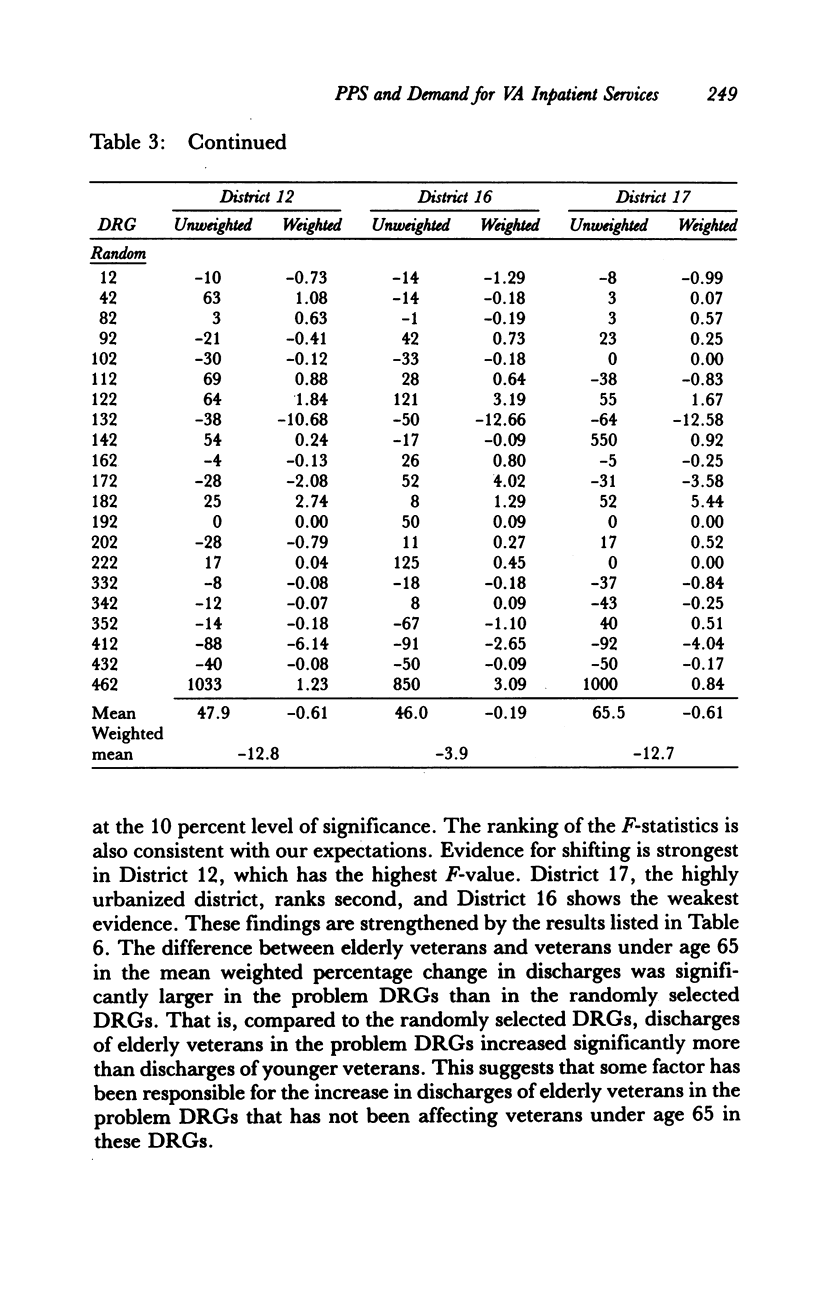
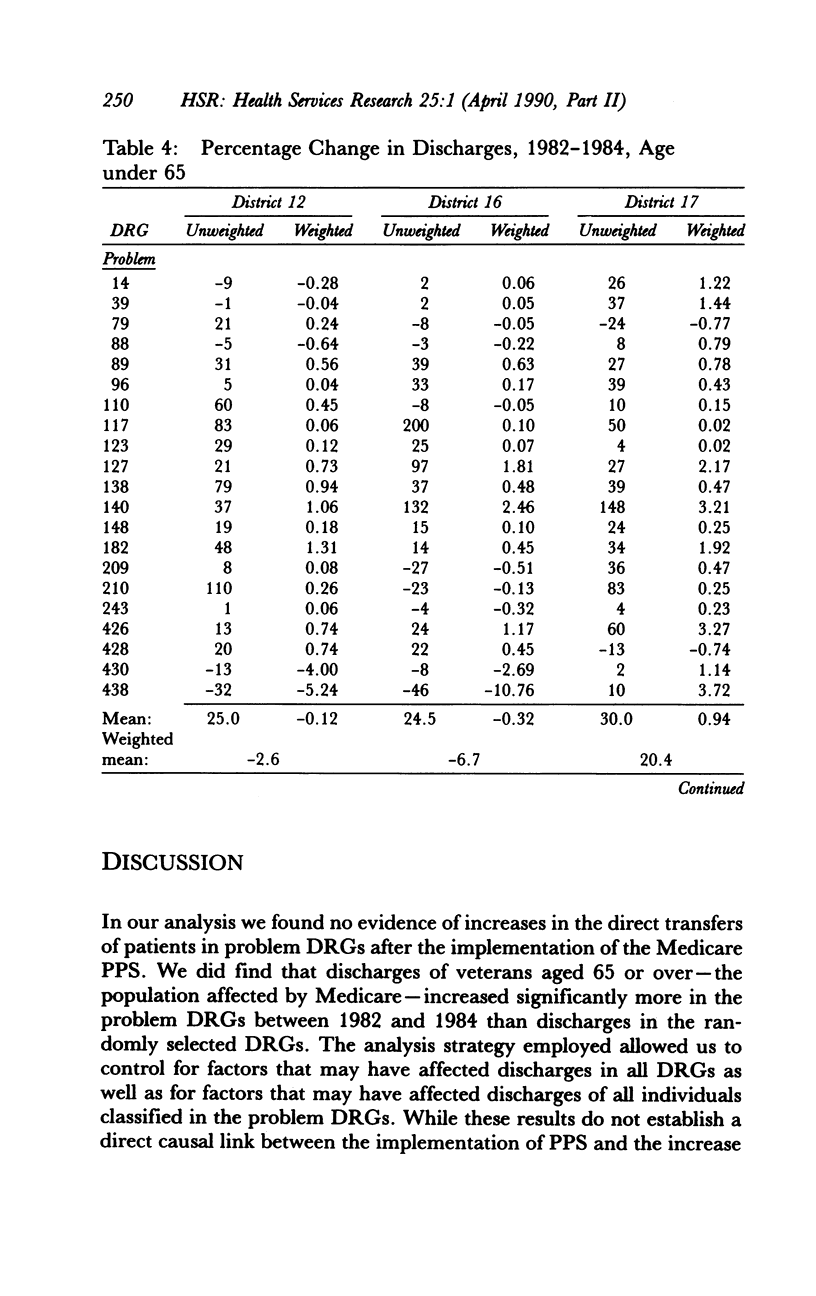
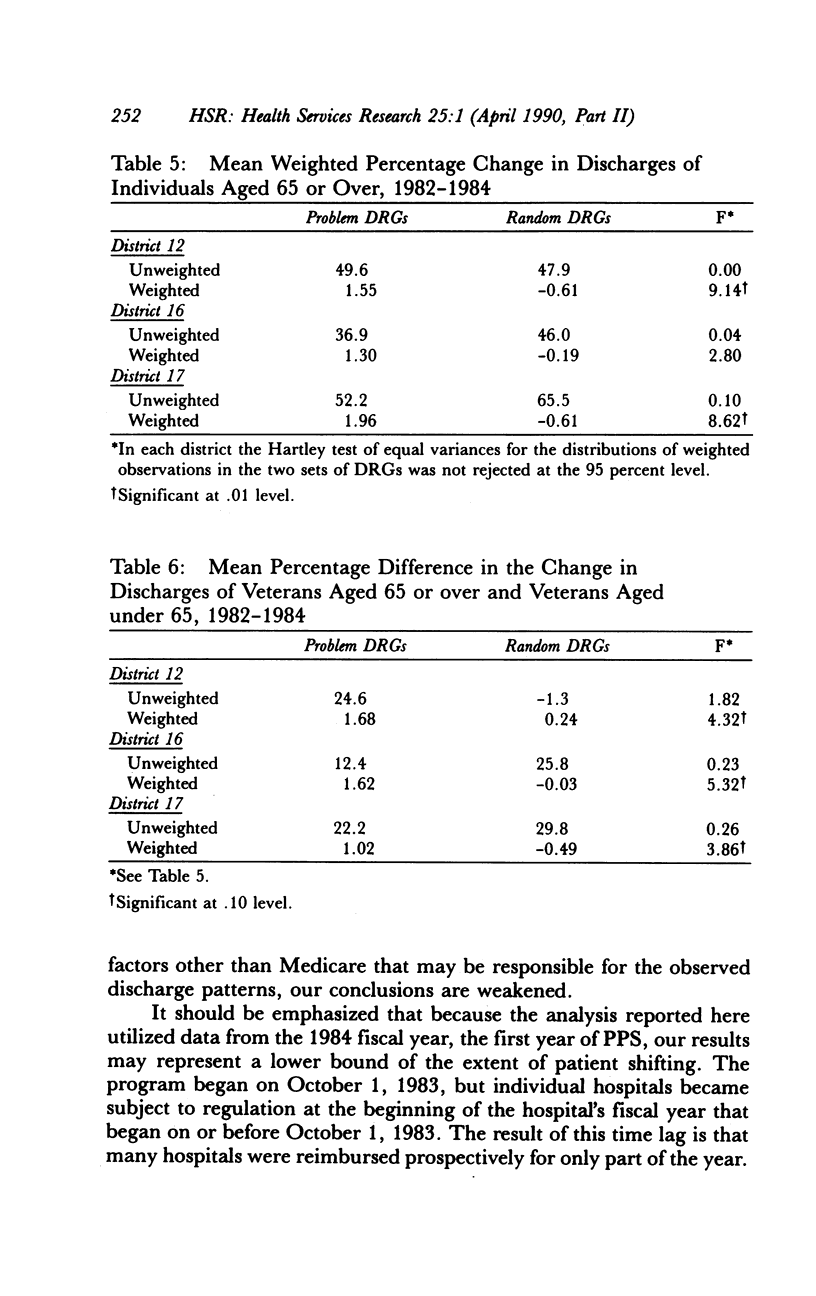
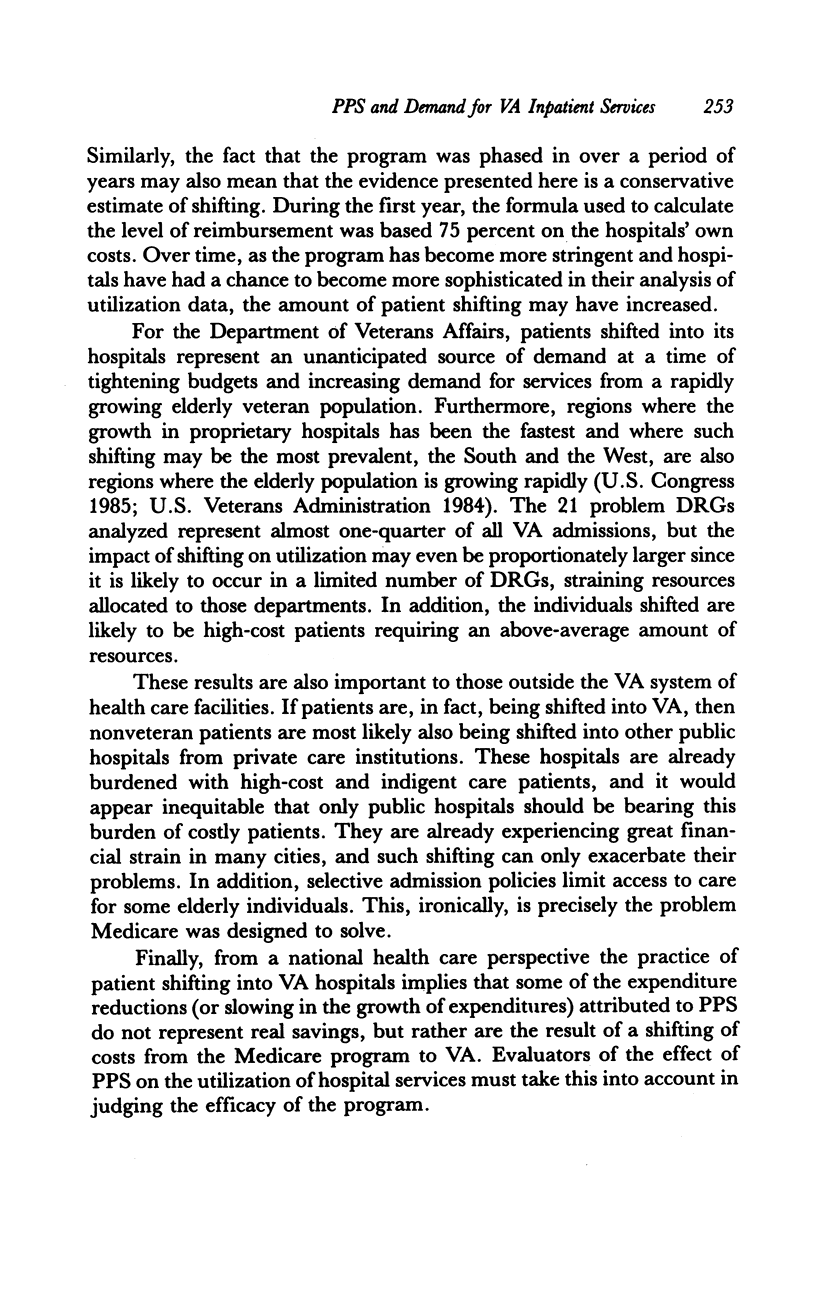
An examination of patient data from three medical districts that vary in urban/rural composition and in their proportion of proprietary hospitals was undertaken to determine if high-cost patients whose illnesses place them in "problem" DRGs (diagnosis-related groups identified as "problems" through interviews with private hospital administrators and from information published by the Wisconsin Hospital Association) are being shifted from non-Department of Veterans Affairs (non-VA) hospitals to VA hospitals. Two outcome measures were employed to detect shifting: patient transfers between non-VA and VA hospitals and discharges of veterans in a sample of DRGs identified as unprofitable by private hospitals. A comparison of patient transfers for fiscal year 1982 and fiscal year 1984 (pre- and post-DRG implementation) revealed substantial increases in the number of transfers, but there appeared to be no concentration of transfers in particular DRGs. An examination of discharges for FY 1982 and FY 1984 within 21 problem DRGs showed average increases ranging from 27 percent to 41 percent among patients aged 65 years or older. A comparison of discharges within a sample of 21 randomly selected DRGs showed either no increase or small decreases in discharges from FY 1982 to FY 1984. The possibility is discussed that some of the cost reductions (or slowing of the rise in costs) attributed to the prospective payment system are merely phantom savings. Hospitals may simply be shifting costs from Medicare to the VA system.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berki S. E., Ashcraft M. L., Newbrander W. C. Length-of-stay variations within ICDA-8 diagnosis-related groups. Med Care. 1984 Feb;22(2):126–142. doi: 10.1097/00005650-198402000-00004. [DOI] [PubMed] [Google Scholar]
- Horn S. D. Does severity of illness make a difference in prospective payment? Healthc Financ Manage. 1983 May;37(5):49–53. [PubMed] [Google Scholar]
- Horn S. D., Sharkey P. D. Measuring severity of illness to predict patient resource use within DRGs. Inquiry. 1983 Winter;20(4):314–321. [PubMed] [Google Scholar]
- Matsui R. T. Medicare payment policy needs corrections. JAMA. 1985 Nov 1;254(17):2454–2455. [PubMed] [Google Scholar]
- Mendenhall S. DRG winners and losers affect profits under prospective payment. Healthc Financ Manage. 1985 Jul;39(7):62–68. [PubMed] [Google Scholar]
- Newhouse J. P. Two prospective difficulties with prospective payment of hospitals, or, it's better to be a resident than a patient with a complex problem. J Health Econ. 1983 Dec;2(3):269–274. doi: 10.1016/0167-6296(83)90020-6. [DOI] [PubMed] [Google Scholar]
- Smits H. L., Fetter R. B., McMahon L. F., Jr Variation in resource use within diagnosis-related groups: the severity issue. Health Care Financ Rev. 1984;Suppl:71–78. [PMC free article] [PubMed] [Google Scholar]
- Stern R. S., Epstein A. M. Institutional responses to prospective payment based on diagnosis-related groups. Implications for cost, quality, and access. N Engl J Med. 1985 Mar 7;312(10):621–627. doi: 10.1056/NEJM198503073121005. [DOI] [PubMed] [Google Scholar]


