Abstract
Objective
Physical inactivity is linked with high chronic disease risk; however, only a fraction of the global population meets the recommendations for physical activity. Stair-climbing is a simple and accessible form of physical activity that has been shown to improve cardio-metabolic outcomes in adults. The present scoping review explores the physiological and therapeutic effects of stair-climbing interventions on adult cardio-metabolic disease risk factors.
Methods
This scoping review followed the reporting guidelines of the Arksey & O'Malley framework, which collates evidence in stages. The research question was framed as “What are the effects of stair climbing on cardio-metabolic outcomes in adults?”. Eligible articles were identified through an extensive search of four electronic databases, and data from 24 research studies were charted and organized.
Results
Stair climbing improves aerobic capacity (8–33 ml kg/min) and serum biomarkers by ≈9–15 %. A minimum of 4–8 weeks are necessary to alter cardiometabolic risk. Regular stair climbing can improve cardio-metabolic risk indicators, including body composition, blood pressure, cholesterol levels, and insulin sensitivity. The research regarding inflammatory and musculoskeletal changes with stair climbing bouts is still in its infancy.
Conclusion
Stair climbing interventions are a no-cost and feasible form of physical activity for improving cardiometabolic disease risk in adults.
Keywords: Adults, Cardio-metabolic outcomes, Physical activity, Scoping review, Sedentary, Stair-climbing
الملخص
أهداف البحث
يرتبط الخمول البدني بارتفاع مخاطر الإصابة بالأمراض المزمنة؛ ومع ذلك، فإن جزءا صغيرا فقط من سكان العالم يستوفي التوصيات الخاصة بالنشاط البدني. صعود السلالم هو شكل بسيط وسهل من النشاط البدني الذي ثبت أنه يحسن نتائج القلب والأوعية الدموية لدى البالغين. يستكشف استعراض النطاق الحالي الآثار الفسيولوجية والعلاجية لتدخلات صعود السلالم على عوامل خطر الإصابة بأمراض القلب والأوعية الدموية لدى البالغين.
طرق البحث
اتبعت مراجعة النطاق هذه إرشادات الإبلاغ الخاصة بإطار عمل آركسي و أومالي، الذي يجمع الأدلة على مراحل. تم تأطير سؤال البحث على أنه "ما هي آثار صعود السلالم على نتائج القلب والأوعية الدموية لدى البالغين؟". تم تحديد المقالات المؤهلة من خلال بحث مكثف في أربع قواعد بيانات إلكترونية، وتم مراجعة وتنظيم بيانات من 24 دراسة بحثية.
النتائج
يحسن صعود السلالم القدرة الهوائية (8-33 مل كجم / دقيقة) والمؤشرات الحيوية في الدم بنسبة ≈ 9-15٪. كما أظهرت المراجعة أن ما لا يقل عن 4 - 8 أسابيع من النشاط ضرورية لتغيير مخاطر القلب والأوعية الدموية. يمكن أن يؤدي صعود السلالم المنتظم إلى تحسين مؤشرات مخاطر القلب والتمثيل الغذائي، بما في ذلك تكوين الجسم وضغط الدم ومستويات الكوليسترول وحساسية الأنسولين. لا يزال البحث المتعلق بالتغيرات الالتهابية والعضلية الهيكلية مع نوبات صعود السلالم في مهده.
الاستنتاجات
تدخلات صعود السلالم هي شكل من أشكال النشاط البدني بدون تكلفة وسهلة لتحسين مخاطر الإصابة بأمراض القلب والأوعية الدموية لدى البالغين.
الكلمات المفتاحية: البالغين, نتائج القلب والأوعية الدموية, النشاط البدني, صعود السلالم, مراجعة النطاق, الخمول البدني
Introduction
Cardiovascular diseases (CVDs) are the leading cause of death globally, with an estimated ≈ 19 million people dying from CVD, amounting to an 18.7 % mortality increase in 2020.1 Though CVD is continued to be a threat to the global economy and health, more than three-quarters of deaths due to CVDs occurred in low- and middle-income countries.2 Obesity, diabetes, hypertension, hyperlipidemia are speculated to be the precursors for both central and peripheral vascular diseases, eventually leading to coronary artery diseases and other CVD. Further cardiorespiratory fitness is a determinant of CVD risk and mortality.3 Despite medical and surgical advances, a considerable segment of the global population, particularly in low-middle income countries, lacks access to medical and surgical management. Hence the above burden has forced public health experts to design cost-effective, feasible interventions for ameliorating cardiometabolic disease risk factors, especially but not limited to high blood glucose, lipid levels, inflammation and body mass index.
Epidemiological evidence shows a strong link between physical inactivity (not able to reach the global recommendations of more than 150 min of weekly moderate to vigorous activity) and cardiometabolic risk factors.4 Optimum dose of physical activity is found to be beneficial in improving cardiometabolic risk. However, only a fraction of the global population meets the weekly recommendation for physical activity.5 Feasibility, cost and embedding physical activity modality which integrates into everybody lives and ready availability are claimed to be the challenges in administering and advocating physical activity.
Stair climbing can be a no-cost, practical, feasible form of physical activity for improving cardiovascular health and reducing the risk of cardiometabolic diseases.6, 7, 8 Accumulating evidence has shown that regular stair climbing can improve cardiometabolic risk indicators, including blood pressure, cholesterol levels, and insulin sensitivity.8, 9, 10, 11 Incorporating stair climbing into daily routines can result in significant improvements in cardiorespiratory fitness and a reduction in waist circumference.12 Emerging evidence indicate that brief stair climbing sessions (for instance, four flights of stairs per day) can yield comparable benefits in preventing cardiometabolic risks, akin to those observed in more extended periods of regular physical activity trials.13,14 However, the optimal dose, safety concerns associated with stair climbing have been overlooked.
The emerging scientific knowledge regarding the effectiveness of stair-climbing interventions remains unconsolidated. The consolidated findings may equip public health experts, behavioral scientists and policy makers in adapting feasible movement interventions and townplanning strategies for effective physical activity promotion. The present review may provide a breadth of knowledge about the effectiveness of stair climb interventions as stair climbing can be a practical, convenient form of exercise and also an effective way to accumulate physical activity throughout the day, especially for individuals who may not have the time or resources to engage in structured exercise.
Materials and Methods
The scoping review serves two purposes: (1) rapid assessment of emerging evidence and (2) identifying research gaps and paying the way for future systematic reviews. The present review followed the reporting guidelines of Arksey & O'Malley framework, which collates the evidence in stages: (1) Identifying the research question; (2) Identifying relevant studies, (3) Study selection, (4) Charting the data, (5) Collating, summarizing, and reporting the results.
Identification of research question
The review's primary aim is to explore stair climbing's physiological effects on the cardiometabolic disease risk factors in adults. To serve the above purpose, the following question was framed ‘What are the effects of stair climbing on cardio-metabolic outcomes in adults?’. We framed the study question based on the population, intervention or exposure, comparison and outcomes (PI(E)CO) format (Table 1). The studies to be included should have involved a target population of adults between the age of 18–65 years. It should have administered stair-climbing interventions in the lab or natural setting. The study included should have assessed any one of the following cardiometabolic risk outcomes, including but not limited to serum glucose, insulin, inflammatory markers, anthropometry – body mass, circumference, aerobic capacity, vascular compliance, heart rate recovery, heart rate variability and cardiac contractility functions. Table 1 shows the PICO format administered in the review for eligibility of the potential studies to be included.
Table 1.
Population, Intervention (exposure), Comparison and Outcomes (PI(E)CO) framework.
| PICO | Eligibility criteria |
|---|---|
| Population | Adults, aged 18–65 years |
| Intervention/Exposure | Stair climbing, stair, stair use, stair climbing intervention |
| Comparison | Any physical intervention other than stair climbing or no intervention |
| Outcome | Cardiovascular diseases (ischemic heart disease, artery disease), cardiometabolic risk, BMI, blood biomarkers (glucose, lipid, lipoprotein, fasting glucose, insulin, cholesterol, triglyceride, nitric oxide), inflammation, ventilation (maximum oxygen uptake, aerobic capacity and metabolism), functional status, diseases (diabetes and cancer). |
| Exclusion criteria | |
| Population | Children |
| Interventions | Lifestyle interventions other than stair climbing, studies administer interventions to promote stair climbing alone |
| Outcome | Outcomes other than cardiometabolic risk |
| Language | Other than English |
| Publication | Abstracts and conference proceedings without full text |
Identification of relevant studies
A systematic search was performed on four databases (Embase, Cumulative Index to Nursing and Allied Health Literature, Web of Science and Scopus) to find potential studies for this review. The keyword search string was as follows: “stair-climbing”, “stair”, “stair use”, “cardiovascular disease”, “ischemic heart disease”, “artery disease”, “cardiometabolic risk”, “body mass”, “obes∗”, “fat”, “glucose”, “lipid”, “lipoprotein”, “fasting glucose”, “insulin”, “cholesterol”, “triglyceride”, “inflammatory”, “nitric oxide”, “maximum oxygen uptake”, “aerobic metabolism”, “aerobic capacity”, “functional status”, “diabetes”, “cancer”, “adult”, “male”, “female” appropriately combined by Boolean operators “AND” “OR”. The first search was conducted on 24th January 2023. The final search was updated on 14th April 2023.
Study selection
The citations retrieved from the databases were uploaded to Endnote online, and duplicates were removed. After duplicate removal, the citations were screened at the title and abstract level based on the priori set eligibility criteria (Table 1). After the abstract screening, potential studies to be included were downloaded as full text and screened by two independent researchers (AM, BC). The reason for exclusion also was documented, and any disagreements were resolved by consensus.
Charting of obtained data
The data obtained from the citations were organized in a tabular form with the following components: author, year, country of origin, study design, population of study, interventions, outcomes and key findings. Table 2 illustrates the study characteristics of the included studies. Gender, number, and baseline characteristics described the population, while interventions were explained in terms of the frequency and duration of the stair-climbing interventions. The outcomes were explained based on method and frequency of measurement. The key findings were explained in terms of mean change in the measures and authors' point of view in the inferences.
Table 2.
Characteristics of the included studies.
| Author year | Country | Design | Objective | Population | Intervention | Outcomes | Key findings |
|---|---|---|---|---|---|---|---|
| Andersen, 201316 | Denmark | Randomised controlled trial | To explore the effects of email prompts on stair climbing on CVD risk | 160 office workers (125 F, aged 42 yrs, 90 % of work hours in sitting) |
(2) control group: pursued usual work |
|
|
| Azmi, 202211 | United Kingdom | Quasi experimental study | To investigate the stair climbing effects on glucose and lipid profiles |
|
|
|
|
| Boreham, 200517 | Ireland | Non-randomised controlled trial | To investigate the effects of stair climbing on VO2max, blood lipids, and homocysteine levels among sedentary and healthy young women |
|
randomly assigned to 8 weeks (1) Intervention group: progressive stair climb. 2 bouts of climb every day, 5 days, increasing one climb every two week (2) control group |
|
|
| Cabral-Santos, 202118 | Netherlands | Randomized controlled study | to determine whether breaking up prolonged sitting with stair climbing bouts with or without high carb diet alter acute inflammatory response. | 40 [10 lean males, 10 overweight/obese (OW) males; 10 lean females. 10 OW females] | Four interventions: control group with 9 h sitting with (1) low carbohydrate or (2) high carbohydrate snack; and stair climbing intervention (15–30 s × 8) with (3) low carbohydrate and (4) high carbohydrate snacks |
|
|
| Chen, 201719 | Taiwan | Quasi randomised experimental study | To compare effects on BMD, lipid profile, insulin sensitivity and physical fitness between DSE and ASE individuals. |
|
|
|
|
| Cho, 202020 | South Korea | Randomised cross over study design | To explore the acute effects of stair climbing interruptions during prolonged sitting on vascular and metabolic function after a high-fat meal | 12 healthy adults (age: 23.5 ± 2.9 years) | Two interventions 1) a 4-h uninterrupted sitting (sitting trial) or 2) a 4-h sitting interrupted with a 5-min stair climbing (66 % of HRR) every hour after a high fat meal |
|
|
| Chow, 202021 | China | Randomized controlled study | To examine the effects of stair exercise on cardiometabolic risk in young obese Chinese females | 36 inactive female college students with body fat percentage >30 %, no exercise, no chronic diseases |
|
|
|
| Donath, 201422 | Switzerland | Non-randomised controlled study | To investigate the effects of two 8-week stair-climbing interventions on balance, gait, strength, and endurance in healthy seniors. | 48 enrolled but 39 elderly (22 F) completed Aged 61–83 years, BMI 25.08 |
|
|
|
| Gay, 201823 | United states | Cross-over trial | To determine the effects of 2-min and 4-min bouts of vigorous-intensity stair climbing on glucose levels. | 9 overweight/obese adults ranging between ages of 40–64 years with prediabetes and HbA1C levels ranging between 5.7% and 6.4 % | Three interventions: (1) control group; (2) stair-climbing in bouts of 2 min, every hour for 8 h; (3) stair-climbing in bouts of 4 min, followed in every 2 h for 8-h duration. |
|
|
| Jenkins, 201924 | Canada | Randomised controlled trial | To explore the effect of stair climbing exercise “snacks” on peak oxygen uptake |
|
|
|
|
| Kennedy, 200725 | United Kingdom | Parallel group trial | To investigate the effects of accumulated bouts of stair walking on CRF, BMI and blood lipids in sedentary office workers |
|
|
|
|
| Lim, 202014 | Canada | Non-blinded parallel group | To compare the effects of 12 wk of usual and stair climbing– based HIIT program on skeletal muscle phenotype in individuals with CAD. |
|
Randomised to either usual cardiac rehab (30 min at 60%–80% of peak heart rate) or STAIR (three bouts of one flight (12 steps), 3–6 flights/day for 12 wk. 4 weeks of supervised and 8 weeks of unsupervised |
|
|
| McCulley, 199426 | United states | Non-randomised controlled trial | to determine the efficacy of stair climb compared with walk/run training, for improving CRF and reducing adiposity |
• 19 sedentary, middle-aged male volunteers (40–65 years old) • Free from diseases • 12 for walk or stair while 7 chosen as sedentary controls |
|
|
|
| Meyer, 201027 | Switzerland | Single group experimental trial | to evaluate impact of a worksite-based promotional campaign of stair use on cardiometabolic risk in apparently healthy adults |
|
|
|
|
| Michael, 20217 | Cyprus | Randomized controlled study | To test the effects of walking up and down stairs at home on a range of CVD and MetS risk factors | 52 sedentary females (18–45 years) from four different Cyprus companies |
|
|
|
| Mir, 201728 | Malaysia | Non-randomised controlled study | To compare the effectiveness of 4 weeks stair climbing intervention with walking on cardiometabolic outcomes |
|
|
|
|
| Ozaki, 201929 | Japan | Experimental study | To explore the additive effects of stair-climb to routine walk program on muscle thickness and strength. |
|
|
|
|
| Paschalis, 201330 | Cyprus | Parallel group controlled trial | To compare the effect of two sessions of stair descending versus stair ascending exercise on muscle performance and health-related parameters in young healthy men |
|
|
|
|
| Rafiei, 202031 | Canada | Randomised cross over study | to investigate brief stair climbing exercise “snacks” could lower postprandial insulin, glucose, and free fatty acids responses during prolonged sitting |
N = 22 (12 healthy weight, 11 overweight) | completed two interventions: 1) sedentary (9-h sitting) and 2) stair climbing snacks (8 × 15–30 s once per hour). |
|
Healthy weight
|
| Takaishi, 201232 | Japan | Non-randomised cross over study | To explore the effectiveness of stair climb interventions on postprandial glucose in glucose impaired participants | 11 healthy participants. Not engaging in regular and strenuous ex. |
Two visits: (1) STAIR: stair climbing visit: 80–110 steps/min (moderate intensity corresponding to 60 % HRR and 13 RPE); (2) WALK: self selected walk speed on 650 m course for 2 h for 6 min at 90th min |
|
|
| Takaishi, 201415 | Japan | Narrative review | To summarize the studies that have investigated the effects of stair-ascending exercise |
Inference
|
|||
| Takaishi, 201733 | Japan | Experimental cross over trial | to confirm acute effect of stair exercise on postprandial hyperglycaemia by comparing it cycle exercise performed at the same workload |
|
Two visits: (1) ST-EX: descending stair (60–65 % HRR, RPE – 13–14), 21 steps, 8–10 reps; STEP RATE – 80–110 (2) Bi-EX: 50–60 reps/minute progressing to predetermined workload |
|
|
| Whittaker AC, 20218 | Netherlands | Secondary analysis study | to explore the association between stair climbing and the metabolic syndrome. |
|
Nurses enquired the exposure of “Do you climb stairs daily?’ (yes/no)” |
|
|
| Yamaji, 202134 | Japan | Cross sectional study | To explore the relation between daily stair climbing activity and vascular function |
|
Three groups based on their daily stair climbing habit: no stairs group, climbing stairs to the 2nd-floor group, and climbing stairs to the ≥3rd-floor group |
|
|
Abbreviations: ASE, ascending stair exercise; AUC, area under curve; BMI, body mass index; BMD, bone mineral density; BP, blood pressure; CK, creatinine kinase; CRF, cardiorespiratory fitness; CVD, cardiovascular disease; DEXA, dual X-ray absorptiometry; DOMS, delayed onset muscle soreness; DSE, descending stair exercise; F, female; FMD, flow mediated dilation; HbA1C, glycated haemoglobin; HDL-C, high density lipoprotein cholesterol; HOMA, IR, insulin resistance; HR, heart rate; IL, interleukin; LDL-C, low density lipoprotein cholesterol; M, male; MVC, maximal voluntary contraction; NEFA, non-esterified fatty acids; NID, nitro-glycerine induced dilation; OR, odds ratio; OW, overweight; ROM, range of motion; TG, triglycerides; TC, total cholesterol; TNF, α, tumor necrosis factor; VAS, visual analogue scale; VO2 max, maximal oxygen consumption.
Results
Characteristics of included studies
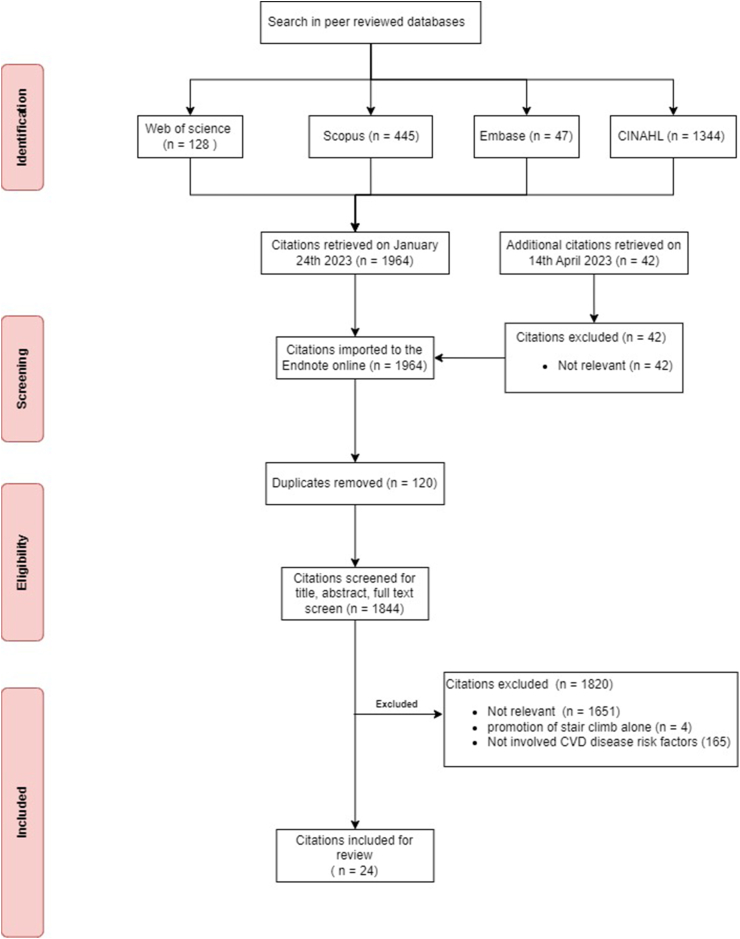
Of the four databases searched with the above search criteria, 1844 citations were deemed eligible for screening after the removal of duplicates. Most of the studies were irrelevant (N = 1651, 90 %), and few citations were excluded based on the criteria (N = 169, 9 %). Only a few studies were included (N = 24, 1.3 %). Figure 1 shows the studies screened and included in the scoping review.
Figure 1.
Flowchart showing the screening and inclusion of the eligible articles.
Nature of the studies
Most of the 24 studies included are interventional studies (N = 21, 88 %). In comparison, two studies are observational, and one is narrative synthesis.15 All the included studies originate from high-income countries (Japan - 5, United Kingdom - 2, Canada - 2, united states - 2, Cyprus - 2 followed by Taiwan, China, Denmark, South Korea and Malaysia, each contributing one). No published research has explored the effects in lower-income countries. Almost half of the studies (N = 11, 45 %) have been administered in the past four years (2019–2022). Table 2 demonstrates the studies' characteristics and critical findings consolidated for the scoping review.
Population
The total number of participants in the included studies is 1792. Most of the studies have been administered to healthy, while few explored the effects on the clinical population.30, 31, 32 Few studies have looked explicitly at the favourable effects of stair climbing in office workers,7,11,16,25,27 obese,18,19,23 hypertension,34 type 2 diabetes mellitus (T2DM),33 elderly22,29 and coronary artery diseases.14 Diet and sleep were standardized in a few studies.31
Interventions
Most of the studies administered stair climbing intervention as a stand-alone intervention, while only a few administered it as an adjunct to exercise training.29 The climb involves 140–300 steps per day with a vertical displacement of ≈17–23 m.11,17,25 Stair climb is identified as moderate intensity (≈13 of RPE scale 6–20) on the self-paced climb. Studies have administered stair climbing interventions using both self and externally paced stair climbing velocity using both low cadence (60–75 steps/min) and high cadence rate (80–110 steps/min).20,25 Randomization of interventions was seldom mentioned.31 Majority studies explored the effects of stair climbing in the long term (> four weeks) while few studies administered in the short term (<1 day).18,20,31
Outcome
Several studies have focussed on examining serological markers (serum TG, TC, LDL, VLD, HDL)8,11,17,20,25,28,31 and cardiorespiratory fitness as outcomes.7,28 Almost all the studies have administered venous samples and assessed through immunoassays.20,25 Body composition measures such as body mass index was routinely administered while reliable sources of fat percentages such as underwater weighing,26 bioelectric impedance,25,27 skin fold7 were rarely administered.
Most studies have found significant changes in cardiometabolic risks ranging from body mass to serum biomarkers (glucose and lipid profile) with stair climb interventions, whether sporadic or continuous bouts. The favourable cardiometabolic effects are higher in the supervised exercise sessions than in home-based stair-climbing interventions.
-
i.
Cardiorespiratory fitness: Most studies have found a significant increase in the VO2 max (2–5 ml/kg/min) after the stair climb interventions of >8 weeks duration7,17 while few failed to observe the change. Stair climbers demonstrated 1.9 L/min higher absolute VO2 and 9 % higher relative VO2 max than the control group.24,25 However, McCulley 1994 could establish a higher absolute VO2 in stair climbing intervention than controls.26
-
ii.
Metabolic fitness markers: Significant reduction in glucose was observed, especially in people with prediabetes or T2DM.23 Healthy individuals, too, benefited from the hypoglycaemic effects of stair climb interventions.32 Insulin sensitivity improved with stair climbing interventions by 24 % compared to walk interventions.19,21 Area under the curve for insulin and non-esterified fatty acids were found to be reduced by 16 % and 21 % with stair climb interventions. At the same time, no significant difference in glucose was observed.31
-
iii.
Body composition changes: Most studies found no changes in the body weight or mass with the stair climb interventions.16,17,19 Significant fat mass changes were observed with stair climb interventions similar to walk interventions.21
-
iv.
Inflammation: Two studies have explored the inflammatory changes with the stair climbing intervention.17,18 Interleukins were found to be reduced with stair climbing interventions in obese populations however remained inert in normal-weight individuals and failed to observe changes with TNF-α. However, Chow 2020 found that TNF-α reduced by 40 % after 12 weeks of stair interventions.21 Further salivary immunoglobulin was found to be high in the active group. No significant changes in homocysteine were found.18
-
v.
Vascular functions: Blood pressure was significantly lower (−8%) with stair climb interventions.19 Cho 2020 demonstrated that stair climbing bouts can mitigate a reduction in flow-mediated dilation associated with prolonged sitting, and popliteal shear rate improved in stair climbing interventions.20 These findings were further strengthened by Yamaji (2021), who found a 3.3 % increase in flow-mediated dilation with stair-climbing interventions. Vasodilator such as e-NOS improved from the 4th week of the training.14
-
vi.
Skeletal muscle functions: Mixed evidence exists with muscle strength improvements with stair climbing. Chen (2017) found no changes in the maximal voluntary contraction or muscle soreness.19 Though no change in strength, maximal explosive power and gait parameters were observed, the balance was found to be improved after stair climb interventions.22 Further, no change can be seen in the fibre type after stair training in coronary artery disease patients was observed. Satellite cells improved in number after stair training compared to controls.14 Countermovement jump height was found to improve after stair climb.7 Thigh muscle thickness was found to be improved with stair climb interventions, while no significant changes were noted in lower leg muscle morphology.29 While contemporary studies favour muscle changes with stair climbing, one study observed muscle damage and soreness after one bout of stair climbing. However, successive stair-climbing training sessions make this muscle damage and soreness insignificant.30
Discussion
The present scoping review aimed to provide a breadth of knowledge on the effects of stair climbing on cardiometabolic disease risk. Whether administered as a continuous, sporadic or bouted, the stair climbing interventions are shown to be beneficial and identified as single ammunition to multifaceted cardiometabolic disease risk. Stair climbing interventions appear to improve cardiorespiratory fitness, glycaemic and lipid profiles, regulate energy expenditure and vascular functions.
World Health Organisation recommends a weekly dose of 150 min of moderate-intensity or 75 min of vigorous-intensity physical activity for achieving health benefits, including protection against cardiometabolic disease risk.35 Despite these recommendations, a substantial portion of the global population (1 in 4 adults and 3 in 4 adolescents) does not meet the activity recommendations, with an increased risk of cardiovascular disease and economic burden.36 Public health experts recommend feasible, familiarised and economically viable activity strategies that could be easily integrated into daily lives and reduce the cardiometabolic disease risk. One such intervention is stair climbing.15
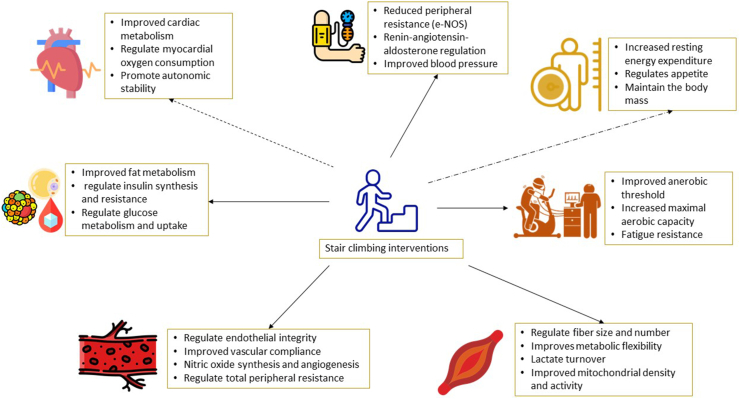
The studies included in this review consistently reported significant improvements in various risk factors associated with cardiovascular diseases, including blood pressure, cholesterol levels, insulin sensitivity, and body mass. Furthermore, incorporating stair-climbing into daily routines has significantly improved cardiorespiratory fitness. However, the emerging evidence regarding the efficacy of inflammatory markers or body fat percentages is promising. Still, there are no studies yet to explore the effects of stair climbing on cardiac remodelling and dynamics which could further reinforce the need for physical activity in these clinical populations. Figure 2 consolidates the potential favourable physiological effects of stair climbing interventions reviewed from the available literature.
Figure 2.
Potential favorable physiological benefits associated with the stair climbing interventions.  denotes proven positive effects whereas
denotes proven positive effects whereas  denotes proven equivocal effects and
denotes proven equivocal effects and  yet to be proved physiological effects.
yet to be proved physiological effects.
While the majority of studies included in this review found significant changes in cardiometabolic risk factors with stair-climbing interventions, it is worth noting that supervised exercise sessions were found to be more effective than home-based interventions. This suggests that support from trained professionals may benefit individuals looking to incorporate stair-climbing into their exercise routine.
For efficient cardiorespiratory conditioning, short bouts of vigorous-intensity aerobic exercise are speculated to have equal benefits to continuous low-moderate intensity exercise.37 Stair climbing is a practically feasible, no-cost and familiar intervention that could be integrated into daily life to reap health benefits. Takaishi 2014 claims “net energy cost of stair climbing was similar to 26 % of upslope walking and pedalling bicycle ergometer".15 In sedentary individuals, even a lesser intensity volume of activity could bring appreciable health benefits, however, to a lesser degree than the bouted moderate–vigorous activity.
Compared to interventions involving walking (≈30 min), similar cardiometabolic health benefits can be reaped from the shorter stair climbing interventions (≈5–6 min).25 Majority of the studies demonstrated the beneficial effects of stair climbing in multifaceted components of cardiometabolic disease risk in a short period.15
Acute intense stair climbing was shown to have minimal adverse effects, such as acute muscle damage and the flare-up of arthritis. In contrast, successive stair climb bouts or training diminish these adverse effects.30 The stair climbing bouts should be of less volume while initiating the training program (1–2 flight/climb, 1–2 climbs/day, 150 steps) and progressing 1 flight every week) should be a safe zone for healthy sedentary individuals, while the clinical population would benefit from an even lesser dose. Adequate familiarisation, stair height <18 cm, preparticipation risk screening before stair climb interventions would reduce the fall risks or cardiac or musculoskeletal loading associated with stair climbing.
Implications for practice
Due to computerization, manual labour is significantly reduced, and sedentary behaviour and physical inactivity become inevitable in modern society, posing a high risk for cardiometabolic diseases. Public health experts recommend regular physical activity of 30 min daily to mitigate the cardiometabolic disease risk; however, only a fraction of the global population meets the recommended dose of weekly physical activity of 150 min. The challenges in achieving the weekly target of physical activity are attributed to various factors, such as limited access to high-quality gym and fitness centers, the expenses involved in accessing equipment and facilities, the requirement for expert guidance to use fitness equipment and techniques, and difficulties in managing time and travel. These factors collectively make it nearly impractical for individuals to meet their physical activity goals. Workplaces and educational institutions often have staircases, which can serve as a viable and superior alternative for promoting moderate to vigorous physical activity. Our review highlights the potential benefits of stair climbing in ameliorating cardiometabolic disease risk, feasibility and accessibility to the community, making stair climbing an impending fitness source. Our review may aid public health experts, behavioural scientists and policymakers in designing, implementing and advocating stair climbing to reduce society's cardiometabolic disease risk. Further designing and implementing appropriate town planning strategies, such as appealing staircases and implementing optimum stairwell use at public health buildings (malls, worship places) and educational institutions, is the need of the hour.
Recommendations
From the findings of the present scoping review, we reckon further studies to investigate the effects of stair-climbing interventions on specific populations, such as older adults, individuals with chronic diseases, and those with disabilities. Further, sparse studies explored the optimal duration, frequency, and intensity of stair-climbing interventions needed to improve cardio-metabolic outcomes significantly. We recommend future studies that could examine the long-term effects of stair-climbing interventions on cardio-metabolic outcomes and other health-related outcomes. Also, further studies are warranted exploring the potential barriers and facilitators to implementing stair-climbing interventions in community and organizational settings.
Conclusion
Our scoping review provides evidence that stair-climbing interventions have the potential to be a low-cost, feasible, and effective form of physical activity for improving cardio-metabolic health outcomes in adults. While supervised exercise sessions are found to be more effective than home-based interventions overall, the feasibility and accessibility of stair-climbing interventions make them an attractive option for individuals looking to improve their cardiovascular health without requiring access to specialized equipment or facilities. These findings suggest that stair-climbing interventions have great potential as a simple yet effective strategy for reducing the risk factors associated with cardiovascular diseases. Further research is needed to explore these interventions' long-term effects and identify specific populations or settings where they may be especially beneficial.
Availability of the data
All the available data was presented in the study. The main data will be available on reasonable request to the corresponding author.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
As a scoping review, this work did not require ethical approval.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Author contributions
BC conceived and designed the scoping review. AM and BC searched and collated the citations. BC analyzed and interpreted the data. AM wrote the initial manuscript draft, and BC provided critical input and shaped the manuscript in its current form. All authors critically reviewed and approved the final draft. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Acknowledgment
The authors would like to thank Manipal Academy of Higher Education for the knowledge and research support for the completion of the review.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Tsao C.W., Aday A.W., Almarzooq Z.I., et al. Heart disease and stroke statistics-2022 update: a report from the american heart association. Circulation. 2022;145:e153–e639. doi: 10.1161/CIR.0000000000001052. [DOI] [PubMed] [Google Scholar]
- 2.Amini M., Zayeri F., Salehi M. Trend analysis of cardiovascular disease mortality, incidence, and mortality-to-incidence ratio: results from global burden of disease study 2017. BMC Publ Health. 2021;21:401. doi: 10.1186/s12889-021-10429-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khan H., Kunutsor S., Rauramaa R., et al. Cardiorespiratory fitness and risk of heart failure: a population-based follow-up study. Eur J Heart Fail. 2014;16:180–188. doi: 10.1111/ejhf.37. [DOI] [PubMed] [Google Scholar]
- 4.Mora S., Cook N., Buring J.E., Ridker P.M., Lee I.M. Physical activity and reduced risk of cardiovascular events: potential mediating mechanisms. Circulation. 2007;116:2110–2118. doi: 10.1161/CIRCULATIONAHA.107.729939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Napolitano M.A., Tjaden A.H., Bailey C.P., DiPietro L., Rimal R. What moves young people? Applying the risk perception attitude framework to physical activity behavior and cardiometabolic risk. Transl Behav Med. 2022;12:742–751. doi: 10.1093/tbm/ibac012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sanchez-Lastra M.A., Ding D., Dalene K.E., del Pozo Cruz B., Ekelund U., Tarp J. Stair climbing and mortality: a prospective cohort study from the UK biobank. Journal of Cachexia, Sarcopenia and Muscle. 2021;12:298–307. doi: 10.1002/jcsm.12679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Michael E., White M.J., Eves F.F. Home-based stair climbing as an intervention for disease risk in adult females; a controlled study. Int J Environ Res Publ Health. 2021;18:1–14. doi: 10.3390/ijerph18020603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whittaker A.C., Eves F.F., Carroll D., et al. Daily stair climbing is associated with decreased risk for the metabolic syndrome. BMC Publ Health. 2021;21:923. doi: 10.1186/s12889-021-10965-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu Y., Luo M., Tan X., Chen L. Stair climbing, genetic predisposition, and the risk of incident type 2 diabetes: a large population-based prospective cohort study. J Sport Health Sci. 2022;12:158–166. doi: 10.1016/j.jshs.2022.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Allison M.K., Baglole J.H., Martin B.J., MacInnis M.J., Gurd B.J., Gibala M.J. Brief intense stair climbing improves cardiorespiratory fitness. Med Sci Sports Exerc. 2017;49:298–307. doi: 10.1249/MSS.0000000000001188. [DOI] [PubMed] [Google Scholar]
- 11.Mat Azmi I.S.M., Wallis G.A., White M.J., Puig-Ribera A., Eves F.F. Desk based prompts to replace workplace sitting with stair climbing; a pilot study of acceptability, effects on behaviour and disease risk factors. BMC Publ Health. 2022;22:1–9. doi: 10.1186/s12889-022-14393-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hongu N., Shimada M., Miyake R., Nakajima Y., Nakajima I., Yoshitake Y. Promoting stair climbing as an exercise routine among healthy older adults attending a community-based physical activity program. Sports (Basel) 2019;7 doi: 10.3390/sports7010023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dunford E.C., Valentino S.E., Dubberley J., et al. Brief vigorous stair climbing effectively improves cardiorespiratory fitness in patients with coronary artery disease: a randomized trial. Front Sports Act Living. 2021;3 doi: 10.3389/fspor.2021.630912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lim C., Dunford E.C., Valentino S.E., et al. Both traditional and stair climbing-based hiit cardiac rehabilitation induce beneficial muscle adaptations. Med Sci Sports Exerc. 2021;53:1114–1124. doi: 10.1249/MSS.0000000000002573. [DOI] [PubMed] [Google Scholar]
- 15.Takaishi T., Ishihara K., Shima N., Hayashi T. Health promotion with stair exercise. The Journal of Physical Fitness and Sports Medicine. 2014;3:173–179. [Google Scholar]
- 16.Andersen L.L., Sundstrup E., Boysen M., Jakobsen M.D., Mortensen O.S., Persson R. Cardiovascular health effects of internet-based encouragements to do daily workplace stair-walks: randomized controlled trial. J Med Internet Res. 2013;15:e127–e. doi: 10.2196/jmir.2340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boreham C.A., Wallace W.F., Nevill A. Training effects of accumulated daily stair-climbing exercise in previously sedentary young women. Prev Med. 2000;30:277–281. doi: 10.1006/pmed.2000.0634. [DOI] [PubMed] [Google Scholar]
- 18.Cabral-Santos C., Rafiei H., Lira F.S., Little J.P. 1288-pub: acute inflammatory response of breaking up prolonged sitting with stair climbing exercise snacks. Diabetes. 2021;70:1288. doi: 10.1249/MSS.0000000000002431. PUB. [DOI] [PubMed] [Google Scholar]
- 19.Chen T.C., Chung-Chan H., Kuo-Wei T., Chih-Chiao H., Kazunori N. Effects of descending stair walking on health and fitness of elderly obese women. Med Sci Sports Exerc. 2017;49:1614–1622. doi: 10.1249/MSS.0000000000001267. [DOI] [PubMed] [Google Scholar]
- 20.Cho M.J., Bunsawat K., Kim H.J., Yoon E.S., Jae S.Y. The acute effects of interrupting prolonged sitting with stair climbing on vascular and metabolic function after a high-fat meal. Eur J Appl Physiol. 2020;120:829–839. doi: 10.1007/s00421-020-04321-9. [DOI] [PubMed] [Google Scholar]
- 21.Chow B.C., Li S., Zhu X., et al. Effects of descending or ascending stair exercise on body composition, insulin sensitivity, and inflammatory markers in young Chinese women with obesity: a randomized controlled trial. J Sports Sci. 2021;39:496–502. doi: 10.1080/02640414.2020.1829362. [DOI] [PubMed] [Google Scholar]
- 22.Donath L., Faude O., Roth R., Zahner L. Effects of stair- climbing on balance, gait, strength, resting heart rate, and submaximal endurance in healthy seniors. Scand J Med Sci Sports. 2014;24:E93–E101. doi: 10.1111/sms.12113. [DOI] [PubMed] [Google Scholar]
- 23.Gay J.L., Buchner D.M., Erickson M.L., Lauture A. Effect of short bouts of high intensity activity on glucose among adults with prediabetes: a pilot randomized crossover study. Diabetes Res Clin Pract. 2018;141:168–174. doi: 10.1016/j.diabres.2018.04.045. [DOI] [PubMed] [Google Scholar]
- 24.Jenkins E.M., Nairn L.N., Skelly L.E., Little J.P., Gibala M.J. Do stair climbing exercise "Snacks" Improve cardiorespiratory fitness? Appl Physiol Nutr Metabol. 2019;44:681–684. doi: 10.1139/apnm-2018-0675. [DOI] [PubMed] [Google Scholar]
- 25.Kennedy R.A., Boreham C.A., Murphy M.H., Young I.S., Mutrie N. Evaluating the effects of a low volume stairclimbing programme on measures of health-related fitness in sedentary office workers. J Sports Sci Med. 2007;6:448–454. [PMC free article] [PubMed] [Google Scholar]
- 26.McCulley C., Houmard J.A., Bruner R.K., McCammon M.R., Hortobagyi T., Israel R.G. Comparison of stair-step ergometry and walk/run training. Sports Med Train Rehabil. 1994;5:107–114. [Google Scholar]
- 27.Meyer P., Kayser B., Kossovsky M.P., et al. Stairs instead of elevators at workplace: cardioprotective effects of a pragmatic intervention. Eur J Cardiovasc Prev Rehabil. 2010;17:569–575. doi: 10.1097/HJR.0b013e328338a4dd. [DOI] [PubMed] [Google Scholar]
- 28.Mir I.A., Yu V.L.K., Jia F.S., Bhat A.H. Comparison between stair climbing and 1 mile walking in relation to cardiorespiratory fitness among sedentary adults. IFMBE Proceedings. 2017;58:14–18. [Google Scholar]
- 29.Ozaki H., Nakagata T., Yoshihara T., et al. Effects of progressive walking and stair-climbing training program on muscle size and strength of the lower body in untrained older adults. J Sports Sci Med. 2019;18:722–728. [PMC free article] [PubMed] [Google Scholar]
- 30.Paschalis V., Theodorou A.A., Panayiotou G., et al. Stair descending exercise using a novel automatic escalator: effects on muscle performance and health-related parameters. PLoS One. 2013;8 doi: 10.1371/journal.pone.0056218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rafiei H., Omidian K., É Myette-CÔTÉ., Little J.P. Metabolic effect of breaking up prolonged sitting with stair climbing exercise snacks. Med Sci Sports Exerc. 2021;53:150–158. doi: 10.1249/MSS.0000000000002431. [DOI] [PubMed] [Google Scholar]
- 32.Takaishi T., Hayashi T. A short bout of stair climbing-descending exercise ameliorates postprandial hyperglycemia more efficiently than a bicycle exercise. Diabetes. 2012;61:A184–A185. [Google Scholar]
- 33.Takaishi T., Hayashi T. Stair ascending–descending exercise accelerates the decrease in postprandial hyperglycemia more efficiently than bicycle exercise. BMJ Open Diabetes Research and Care. 2017;5 doi: 10.1136/bmjdrc-2017-000428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yamaji T., Harada T., Hashimoto Y., et al. Stair climbing activity and vascular function in patients with hypertension. Hypertens Res. 2021;44:1274–1282. doi: 10.1038/s41440-021-00697-z. [DOI] [PubMed] [Google Scholar]
- 35.Bull F.C., Al-Ansari S.S., Biddle S., et al. World health organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Amini H., Habibi S., Islamoglu A.H., Isanejad E., Uz C., Daniyari H. Covid-19 pandemic-induced physical inactivity: the necessity of updating the global action plan on physical activity 2018-2030. Environ Health Prev Med. 2021;26:32. doi: 10.1186/s12199-021-00955-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Garber C.E., Blissmer B., Deschenes M.R., et al. American college of sports medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]