Abstract
Purpose
To review the different types of ganglion cysts surrounding the proximal tibio-fibular joint, their management options, outcomes, and recurrence.
Design
Descriptive analytical review.
Results
7 case series consisting of a total of 159 patients and 61 case reports consisting of 80 patients (with three patients having bilateral pathology) were included in this review. (Total cysts 159 + 83 = 242). The mean age was 41 years, and 71 % of the patients were males. 96.5 % of the cases were managed operatively, out of which 98 % of patients felt improvement in local symptoms and 71.5 % had improvement in neurological symptoms. Complete excision of the cyst is the primary mode of operative management. Many added procedures with complete excision are to mitigate the risk of recurrence. The recurrence rate of aspiration, simple excision alone, simple excision with recurrent articular branch neurectomy, and simple excision with PTFJ procedures were 77 %, 56 %, 11.5 %, and 0 %, respectively. Outcomes beyond recurrence were poorly reported.
Conclusion
There is not enough literature regarding the topic from which any formal systematic review can be done. Our summary suggests that aspiration alone or with steroid injection is associated with the highest recurrence rates among all the procedures. Complete excision with recurrent articular branch neurectomy should be the primary management. Revision cyst excision in isolation is an inadequate treatment option, therefore should be done in conjunction with PTFJ arthrodesis, which reduces the recurrence rates. Better quality studies are needed that report patient-centered outcomes and morbidities following PTFJ procedures.
Keywords: Proximal tibiofibular joint, Ganglion cyst
1. Introduction
Cyst around the joint is common in an orthopedic outpatient department clinic. It may be a ganglion cyst, synovial cyst, or degenerative myxoid cyst. A ganglion cyst can be differentiated from a synovial cyst in terms of compressibility, lining of the cavity, and types of fluid it contains. It is less compressible, lined by connective tissue capsules without any mesothelial cells, and contains gelatinous materials.1,2 A synovial cyst is more compressible, lined by mesothelial cells, and contains clear or xanthochromic fluid. The myxoid cysts are small benign lumps mostly seen in the digits and toes, also known as mucous cysts.3
Although the ganglionic cyst is rare around the proximal tibiofibular joint, it is quite a common site in the lower limb per se.4 An average of 15–20 % of all ganglion cysts occur on the lower limb, with 33 % involving the knee.5 The articular theory proposes that all ganglion cysts, including extra neural and intra-neural, originate from the synovial joint.6,7 Due to the rarity of this entity, literature on this topic is scarce. This article aims to review the different types of ganglion cysts surrounding the proximal tibiofibular joint regarding their presentation, management options, results, and complications.
2. Method
2.1. Literature search and study selection process
The following electronic databases were searched for this review article: Google Scholar, Medline (PubMed), PMC, and ScienceDirect. We searched the literature from the inception to December 2021, published in the English language in peer-reviewed journals reporting incidence, surgical methods, approaches, and outcomes in terms of complications and recurrence with regard to the ganglionic cyst of PTFJ. The search strategy included a combination of the following terms, along with the Boolean operators (OR; AND): ‘proximal tibiofibular joint’, ‘ganglion cyst’, ‘non-operative’, ‘conservative’, ‘operative’, ‘outcomes’, ‘synovial cyst’. The authors independently reviewed the abstract of each publication to establish its suitability for inclusion in the review. A flowchart (Fig. 1) showing how articles are chosen for the review is given below. The inclusion criteria for studies were as follows:
Fig. 1.
Flowchart of the selection process of the articles.
The inclusion criteria for studies were as follows.
-
●
Ganglionic cyst or synovial cyst around the PTFJ
-
●
Case series, Case reports, Non Randomized or Randomized controlled trials
-
●
Surgical methods and approaches for ganglion cysts around PTFJ
-
●
Outcomes, recurrence rate, post-op complications
-
●
Peer-reviewed journals
-
●
English language
Animal studies and those published in languages other than English were excluded. If the abstract failed to include the study, the full text was examined to confirm the eligibility. Further studies were also included while reviewing the reference lists of selected articles. The compilation of chosen case series34, 35, 36, 37, 38, 39, 40 and case reports41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101 pertinent to this review can be found enumerated in the references section of this article.
2.2. Data extraction
Patient demographics, symptoms, type of ganglion, operative and non-operative management, clinical and functional outcomes, improvement in neural symptoms, recurrence of the cyst, and post-op complications were included in the review database.
3. Results
We have described our result groups A and B as case series' and case reports’ summaries, respectively. Then, we have described the combined results of both groups. Patient demography, types of the ganglion cyst, biopsy confirmation, prior history of trauma, and tinel sign are described in tabulate format in Table 1. It suggests that.
-
●
This entity is more common in middle-aged males. (Avg age is 41 years), but has been reported as early as in 4-year-old child and as late as 74 year old male.
-
●
Three patients in our case report summary described the bilateral ganglion cyst near PTFJ. So, we added those three cases separately.
-
●
Intra neural cyst is the most common, followed by Extraneural, Combined Intra and Extra neural, and Simple ganglionic cysts.
-
●
Prior history of trauma is present in 15.5 % of cases, and Tinel sign is present in 13 % of cases only.
-
●Local presenting symptoms like swelling and pain are common in typical presentation, Nerve involvement shows symptoms of motor and sensory deficit. The detailed analysis of neurological symptoms of group B (case reports summary) suggested the following things.
-
1.There is no case with only lateral compartment involvement. It is always associated with the involvement of the anterior compartment.
-
2.The anterior compartment has no case with only extensors (EHL, EDL) involvement. They are always associated with dorsiflexor (TA) involvement.
-
1.
Table 1.
Demographics, types, Prior history of trauma and tinel sign analysis.
| Group A (Case series summary) | Group B (Case reports summary) | Combined result | ||
|---|---|---|---|---|
| Males | 118 (74.2 %) | 52 (66 %) | 170 (71 %) | |
| Females | 41 (25.8 %) | 26 (33 %) | 67 (29 %) | |
| Male to female ratio | 11/4 = 2.75 | 3/2 = 1.5 | 5/2 = 2.5 | |
| Mean Age | 43.05 years | 40.1 (4 years–74 years) | 41 years | |
| Total patients | 159 | 78 (Total ganglion studied = 83 as three patient had recurrence, two case report had 2 patients) | 242 | |
| Types of the ganglion cyst | Simple ganglion cyst | 20 (12 %) | 9 (11 %) | 29 (12 %) |
| Intraneural ganglion cyst | 62 (39 %) | 32 (38 %) | 94 (39 %) | |
| Extraneural ganglion cyst | 36 (23 %) | 28 (34 %) | 64 (26 %) | |
| Combined intra and extra neural ganglion cyst | 35 (26 %) | – | 35 (15 %) | |
| Intra osseous ganglion | 6 (4 %) | 3 (4 %) | 9 (4 %) | |
| No diagnosis described | – | 11 (14 %) | 11 (4 %) | |
| Biopsy confirmation of the lesion by histopathological examination | 65 (40.8 %) | 65 (82 %) | 130 (55 %) | |
| Prior history of trauma | Present | Not described by authors except only RJ spinner et al.38 it has described 17 out of 24 (71 %) cases had history of prior trauma | 14 (17 %) | 31 (12.5 %) |
| Absent | 29 (36.5 %) | 36 (15 %) | ||
| Not specified by authors | 40 (46.5 %) | 175 (72.5 %) | ||
| Tinel sign | Present | Not described by authors except only RJ spinner et al.38 it has described 20 out of 24 (83 %) cases had tinel sign | 11 (14 %) | 31 (13 %) |
| Absent | 8 (7.5 %) | 12 (4.2 %) | ||
| Not specified by authors | 64 (78.5 %) | 199 (82.8 %) | ||
Various types of procedures, along with associated recurrence rate and Post-op improvement in the symptoms, are analyzed in Table 2, Table 3, respectively. Certain analyses are not feasible for tabulate format, therefore have been described below.
Table 2.
Analysis of Various management options with recurrence rate.
| Management options | Types | Group A |
Group B |
||||
|---|---|---|---|---|---|---|---|
| No of patients | Recurrence rate | No of patients | Recurrence rate | ||||
| Conservative | Mindful observation | 1 | – | 2 | – | ||
| Aspiration | – | 8a | 6 | 2 | |||
| Operative management | Primary procedure | Added procedures | |||||
| Complete excision of cyst only | – | – | 42 | 9 + 29a | 48 | 12 | |
| Complete excision | PTFJ excision | – | – | – | 1 | – | |
| Complete excision | RAN | – | 38 | 6 | 17 | – | |
| Complete excision | RAN | PTFJ excision | – | – | 1 | – | |
| Complete excision | RAN | PTFJ fusion | – | – | 1 | – | |
| Complete excision | RAN | PTFJ resection | – | – | 5 | – | |
| Complete excision | PTFJ arthrodesis | – | 57 | – | – | – | |
| Complete excision | PTFJ arthrodesis | Partial fibular excision | 2 | – | – | – | |
| Complete excision | Tendon transfer for foot drop | – | 7 | – | – | – | |
| Complete excision | Curettage and bone grafting of the bone defect | – | 1 | – | – | – | |
| Complete excision | TKA | – | 1 | – | – | – | |
| Complete excision | Arthroscopic resection | – | 1 | – | – | – | |
| TKA | Fibula head resection | – | 9 | – | 2 | – | |
RAN = Recurrent articular branch neurectomy.
= no of cases that had been previously managed by respective procedure and came with recurrence to that respective author.
Table 3.
Post-op status analysis.
| Group A (Case series summary) | Group B (Case reports summary) | Combined result | ||
|---|---|---|---|---|
| Post-op improvements of local symptoms | Present | 105 (100 %) | 61 (95 %) | 166 (99 %) |
| Absent | 0 | 3 (5 %) | 3 (1 %) | |
| In Group A, Only 105 cases out of 159 had local symptoms, and all had improvements, Group B, 64 out of 83 cases had local symptoms. Among them, 61 had improvements. | ||||
| Post-op neurological symptoms | Complete recovery | 74 (66.3 %) | 29 (40 %) | 103 (55 %) |
| Residual motor symptoms | 11 (10 %) | 25 (34.5%) | 36 (19 %) | |
| Residual sensory symptoms | 3 (2.7 %) | 4 (5.5%) | 7 (4.5 %) | |
| Residual motor and sensory both | 23 (21 %) | 10 (13%) | 33 (18.5 %) | |
| No data specified by author | 0 | 5 (7 %) | 5 (3 %) | |
| In Group A, Only 111 cases out of 159 had neurological symptoms and Group B, 73 out of 83 cases had neurological symptoms. | ||||
3.1. Pre-operative investigations
3.1.1. MRI
MRI can help to gather information regarding the cyst, such as type, size, the extension of the cyst, communication with the PTFJ, homo or heterogeneous and septate or without septa, etc. The combined results of groups A and B show that 220 out of 242 ganglion cysts (90.9 %) were diagnosed on the MRI, rest were diagnosed by clinical examination or USG.
3.1.2. -NCV
For Group A - Only four authors (Damron TA et al.,34 RJ Spinner et al.,35 TJ Wilson et al.,39 Papanastassiou et al.40) out of 7 in our case series described the electro-diagnostic study as a pre-op investigation which also helped to confirm and to measure the amplitude of neurological involvement. So, a total of 130 (81.7 %) out of 159 cases underwent EMG NCV investigation.
For Group B–As described above, 73 out of 83 (87 %) had neurological involvement. 40 of those 73 (55 %) case reports had a description of EMG-NCV.
Combined results showed that 170 ganglion cysts out of 242 (70.8 %) underwent EMG-NCV examination.
3.2. Type of the operative procedure
The main surgical procedure for a ganglion cyst would be complete excision with the help of the loupe magnification in case of open dissection or with the help of the arthroscope if the cyst has an intra-articular extension. But due to the high recurrence rate, excision of the cyst is followed by various other procedures such as (1) Neurectomy of the recurrent articular branch, (2) PTFJ excision, (3) PTFJ arthrodesis, (4) Partial fibula head excision.
For management of the intraosseous extension, Curettage and bone graft are used to address the cortical bone defect. Old presentation with foot drop could be managed with tendon transfer and the cyst's excision. To add to that, a few exceptions in Group B are described below.
-
1.
C. L. Herndon et al.95 described TKA (total knee arthroplasty) along with the partial fibular excision to justify the primary complaint of the patient, which was related to osteoarthritis knee.
-
2.
An Alsahhaf et al.82 described minimal invasive surgical interventions like computed tomography (CT) guided cyst fenestration, and pulsed radiofrequency modulation followed by steroid injection.
3.3. Post-op improvement after the operative management
The analysis of the Post-op Symptoms improvements is depicted in tabulated form (Table 3). Local symptoms get complete improvement after the cyst excision, which is very plausible, but symptoms may persist if the excision is incomplete or partial. In our summary, 98 % of cases have the complete improvement of local symptoms, but 3 case reports have described partial improvement only.
Neurological symptoms after the excision might not completely be recovered. We observed 55 % of cases with complete motor and sensory recoveries, but 19 % of cases have residual motor symptoms, and 4.5 % had residual sensory involvements, 18.5 % had both motor and sensory residual symptoms. Five case reports didn't specify this. Duration of the motor and sensory symptoms has a positive correlation with the postoperative outcome.
Therefore, operative decompression will improve neurological and local symptoms, but a complete motor recovery is the most arduous.
3.4. Recurrence rate and duration of development
For Group A - In the case of series analysis, 42 (26.4 %) patients went through only complete excision, and among them, 9 cases (21 %) showed recurrence. TJ Wilson et al.39 described the 6 recurrence cases among 11 cases that underwent excision and recurrent articular branch neurectomy. The mean duration for the development of the recurrence described by six studies was 56 months, compared to the median value of 15 months described by TJ Wilson et al.39
We reported 8 cases with a history of prior aspiration and 29 cases with a history of prior complete excision managed by somewhere else before presenting to respective authors.
For Group B–In the case reports’ summary, 13 (16.8 %) cases of recurrence out of 83 cases were reported. All 13 cases prior went through only one procedure i.e., excision of the cyst, except one case, which was described by A Vatansever et al.59 in which only aspiration was done prior.
These 13 cases also included those 3 cases (P J O'Rourke et al.,47 C Pagnoux et al.,52 F Aymen et al.90) in which subtotal or partial excision of the cyst was performed. The median value of duration for the development of the recurrence, in group B was 6 months with a minimum of 3 months to a maximum of 5 years. Procedures like excision of the PTFJ joint and its arthrodesis didn't show any recurrence. Combined results showed in Table 4, with a detailed explanation of the calculation.
Table 4.
Analysis of recurrence rate according to procedure.
| Recurrence rate | Data analysis | Explanation | |
|---|---|---|---|
| Simple aspiration | 77 % |
|
It is observed repeatedly that aspiration of the ganglionic cyst is associated with a high recurrence rate, and it also has a scientifically plausible explanation. So to make the calculation more realistic, we included 8 cases from group A in the equation (as a recurrent and presenting case both). We also excluded 2 cases from group B as they either lacked follow-up data or were managed with Radiofrequency ablation along with aspiration. |
| Complete excision | 56 % | In group A, we had 29 cases that underwent prior complete excision somewhere else. Nine cases show recurrence even after complete excision. Hence, 50 recurrences in 89 cases. | We included 29 cases in our recurrence rate calculation same as above. |
| Complete excision + Recurrent articular branch neurectomy | 11.5 % | In group A, we had 6 extra neural recurrent cases operated earlier for intraneural ganglion cysts. Hence, 6 recurrence cases in 52 cases. | This method has 0 % recurrence for intraneural ganglion cysts, but the risk of extraneural ganglion cyst after excision of the intraneural cyst is 11.5 %. |
4. Discussion
4.1. Prevalence and presentation
Ganglionic cyst, although a rare entity considering the prevalence of cystic mass around the knee, but if it is present in the lower limb, then the most common site of it is around PTFJ.8, 9, 10 Most commonly, it affects the CPN at the fibula neck, less likely tibial nerves also get involved.10 The first case report regarding Intra neural ganglion cysts in CPN was published in 1931 b y Wadstein et al.11 OA Ilahi et al.,13 described the prevalence of PTFJ ganglionic cyst, which is 0.76 % (95 % confidence interval CI = 0.1 %–1.4 %). Most of the patients described by OA Ilahi et al.13 had no clinical symptoms. Because of such a small prevalence, we only found case series, case reports, and descriptive narrative reviews in our literature search.
4.2. Types of ganglion cysts
There are a majority of 5 types of ganglionic cysts related to PTFJ joints we have found. That is described in detail in Fig. 2.
Fig. 2.
Flowchart of types and etiopathogenesis of the various ganglion cysts.
4.3. Atypical presentation
Ozden et al.73 described intermittent claudication as presenting a complaint of the PTFJ ganglionic cyst. S H Park et al.,89 J Sim et al.,94 MA Hersekli et al.,56 and F Aymen et al.90 described low back pain with radiculopathy and foot drop as the initial presentation. Rubin et al.57 described a patient with sudden onset of deep peroneal neuropathy in the midst of golfing, the reason for that was unclear. Streib et al.14 described 3 patients with sudden onset of deep peroneal neuropathies after minor athletic trauma and suggested that minor or sudden stretch or traction injuries of the peroneal nerve could occur with some athletic maneuvers. All were later on diagnosed as PTFJ ganglion cysts.
Ganglion cysts may present as compartment syndrome. R D Muckart et al.15 described eight cases of the PTFJ ganglionic cyst that presented as anterior and lateral compartment syndrome. Ward WG et al.9 described anterior compartment syndrome later reported as a rupture of the ganglion cyst. Maheshwari et al.64 presented a rare case of a PTFJ ganglion association with a TKA and unusual features, including aggressive intra-osseous extension, cortical thinning, pathological fracture, and soft tissue extension. Barrie et al.16 reported three different cases of ganglionic cysts that involved the peroneal nerve, peroneal tendon, and fibular head, respectively. They concluded that ganglion cysts might migrate in various directions and named them ganglion migrants. S M Mortazavi et al.60 reviewed the extension of the synovial cyst arising from the PTFJ and found that extensions were subcutaneous in 23, intramuscular in 7, inter-muscular in 2, and intra-osseous in 2 cases.
4.4. Etiopathogenesis
4.4.1. General ganglion cyst
Controversy exists concerning the pathogenesis of PTFJ ganglion cysts. The main theory is the synovial theory which describes that ganglion cyst derives from articular and periarticular tissues.17 Other supportive theories have been described in Fig. 2.
4.4.2. For intraneural ganglion cysts
The articular theory, which is widely accepted compared to degenerative theory,12,18 is based on synovial fluid migration from an adjacent joint via an articular branch of the nerve. This was later modified as the Unifying articular theory presented by RJ Spinner et al.19, 20, 21, 22 His first two papers published in 2007 and 2008, thoroughly examined cadaveric experiments by injecting the dye into the outer epifascicular epineurium of the fibular and the tibial nerves and described the extension of the ganglionic cyst in the form of phases 1,2 and 3. There was a proposed mechanism for the formation of the fibular or tibial intra-neural ganglion cyst, derived from the superior tibiofibular joint that may extend proximally into the sciatic nerve (Phase I), cross over (Phase II), and descend down the terminal branches (Phase III). The articular branch led the cyst from the origin joint up to a larger parent nerve (primary ascent) through a capsular rent confirmed in arthrography. It allows communication between the injected joint and the cyst in various studies.20 The cyst followed the path of least resistance within the epineurium that might be influenced by native internal and external anatomy and pathology (e.g., postoperative scarring). This theory would apply directly to the peroneal nerve but could be extrapolated to other nerves at other sites as well.26 RJ Spinner et al.25 extrapolated these principles of the articular theory to the axial spine, demonstrating its versatility in explaining extra neural and intra-neural cysts. In fact, Nonaka et al.23 described hypoglossal cysts with atlanto-occipital joint connection.
4.5. Investigation and differential diagnosis
4.5.1. USG
In USG, The use of a high-frequency 17.5-MHz small footprint “hockey stick” transducer is necessary to achieve the appropriate resolution that requires seeing small joint connections, but it, unfortunately, results in a limited field of view, which may preclude visualization of the full extent of the cyst.46 As a simple and cheap technique, sonographic control for the follow-up is of crucial importance.
4.5.2. MRI
MRI is the standard investigation for any type of cystic lesion around the knee joint. Bassett27 described the characteristics of ganglia on MRI. On T1-weighted images, the signal density shows low, whereas on T2-weighted images, the signal density shows high, and appears homogeneous. Contrast should be used in every instance to confirm the cystic nature of the lesion, which may otherwise mimic solid lesions such as a benign neurogenic tumor or even a malignant tumor such as a synovial sarcoma.25 For intra-neural ganglion cysts, MRI signs of all phases, including ascent, crossover, and descent for Intra neural ganglion cyst, have also been described by RJ spinner et al.22 in different papers. The combination of these MRI features i.e., the signet ring sign, traverse limb, tail sign, and denervation changes, are essentially pathognomonic of an intra-neural cyst arising from the superior tibiofibular joint dedicated in Fig. 3. Preop imaging of intraneural ganglion cyst has been systematically reviewed by K A Lenartowicz et al.32 and concluded that preop MRI is the most sensitive and specific investigation to find the joint connection of the ganglion cyst.
Fig. 3.
MRI signs according to the intra-neural ganglion cyst extension (Red arrow suggests pathway pf intra-neural cyst extension and signs accordingly).
4.5.3. EMG-NCV
EMG-NCV can be helpful for locating the compressive lesion and provide information regarding the severity of the neuropathy, which can determine the neurological and functional prognosis.82 In addition, EMG can exclude other peripheral nerve lesions, including plexopathy or radiculopathy. Response on EMG NCV was used to evaluate the early recovery changes after decompression along with clinical MRC grade.
4.6. Management
Earlier treatment recommendations have been based largely on anecdotes rather than a comprehensive understanding of the mechanism of cyst formation. In this paper, we have tried to summarise the treatment for various ganglion cysts comprehensively. There is a minimal role of conservative management when there is a proven Ganglionic cyst around PTFJ.
4.6.1. Aspiration
Either USG-guided or mini-open aspiration has been described in the literature. It is commonly performed if the patient is asymptomatic and denies any kind of open surgery. Cyst recurrence has been reported in up to 13 % of cases after aspiration.29,61 Sometimes aspiration may be followed by corticosteroid injection inside the cyst that prevents recurrence, but there is no concrete evidence in the literature to prove that claim.49
4.6.2. Excision of the cyst
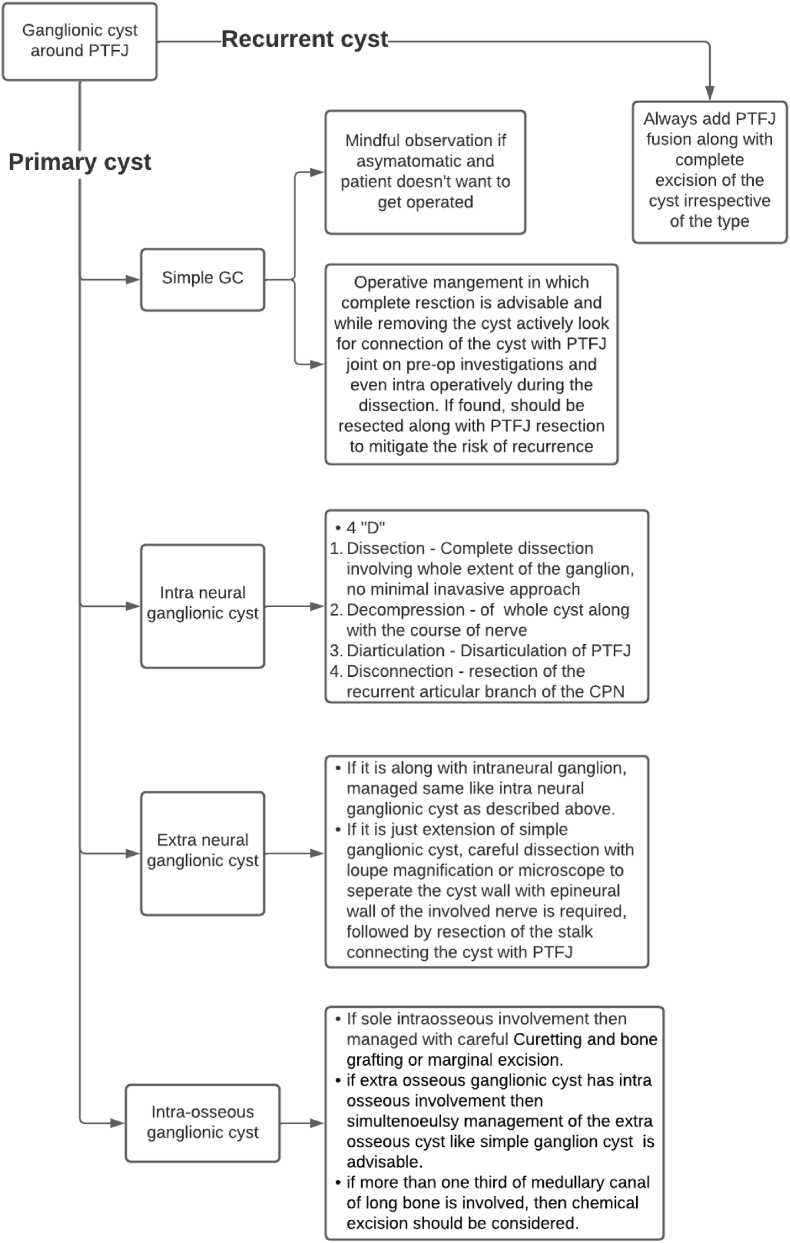
Primary surgical management of the ganglionic cyst is complete excision, irrespective of the type. In order to treat intra-neural ganglion cysts effectively, RJ spinner et al.28 described detailed management of the intra-neural ganglion cyst, which involves 4 “D” - Dissection, Decompression, Disconnection, Disarticulation. According to our summary, we have modified that table for every type of cyst. (Table 5).
Tables 5.
4 “D″of ganglion cyst management.
| Technique | Pitfall | |
|---|---|---|
| Dissection |
|
|
| Decompression (Only for intra-neural types) |
|
|
| Disconnection |
|
|
| Disarticulation |
|
|
| Closure |
|
|
It also involves complications such as vessel injury, infection, perineural fibrosis, traction injuries, and sometimes complete nerve transection resulting in loss of function that may occur due to the proximity of the peroneal nerve to the origin of ganglion cysts within the proximal tibiofibular joint.65,89 Postoperatively, Gentle, early motion of the knee is encouraged because it permits gliding of the peroneal nerve.31 Follow-Up Evaluation by serial clinical and Electromyographic examination may be helpful, especially several months after surgery, to demonstrate recovery. Postoperative MR imaging and long-term follow-up (at least several years) are necessary to document the outcome and identify subclinical recurrent cysts.
4.6.3. For intraosseous ganglion cysts
Curettage and bone grafting or marginal excision have been recommended for the treatment of extensive proximal fibular intraosseous ganglia.24 Bone grafting prevents recurrence and mitigates the risk of collapsing fracture.
Our proposed algorithm for the management of the PTFJ ganglionic cyst is illustrated in Fig. 4.
Fig. 4.
Flowchart of management of ganglion cyst.
4.7. Prognosis
All the cases that are managed with operative management have significant improvement in their local and neurological symptoms. Clinical features are similar in adults and in children, except for the outcome, which is better in children.78 Even in recurrent cases, excellent operative outcomes can be achieved.
Motor recovery following an operation for peroneal intraneural ganglia was less predictable. And depends on many factors such as duration of symptoms; extent of the compression; length of the cyst; and neural anatomy of the tibialis anterior muscle, specifically whether a tibialis anterior branch is derived directly from the articular branch or main trunk.30
4.8. Recurrences
The most important step of the intervention to avoid recurrences seems to be the complete resection of the ganglion stem and its connecting stalk with PTFJ, along with the resection of PTFJ.5 During managing intra-neural ganglion cysts, resection of the recurrent articular branch holds the same importance. Extraneural cyst recurrence may occur if subtotal joint resection is performed. It is often subclinical and rarely leads to extrinsic nerve compression. Intraosseous recurrences usually have a large central cavity and frequently, small satellites or daughter cysts are scattered in the previous surgery's scar. In these instances, it may be advisable to perform an intralesional procedure to alleviate the risk of recurrence. Miskovsky et al.36 found 100% repeat recurrence if only simple excision is repeated as a second intervention. Hence, a second intervention, as only complete excision, is not advisable in recurred cases. If simple cyst excision fails, two alternative treatment options have been described; first, resection arthroplasty of the fibula and the second, fusion of the proximal tibiofibular joint fusion.39 Kapoor et al.55 resected the proximal tibiofibular joint in two recurrent cases and showed a good prognosis. Now, resection of the PTFJ is advised to perform in the management of the primary cyst to decrease the chance of subsequent recurrence. Recurrence is advisable to manage with PTFJ fusion. L S Huntigton et al.33 did systematic review of the PTFJ ganglion cyst of 101 knees and concluded recurrence rates of cyst aspiration, cyst excision, PTFJ hemi resection and PTFJ arthrodesis were 81.8 %, 27.4 %, 8.3 % and 0 %, respectively. Our review included 242 knees and our recurrence rates of cyst aspiration, simple excision alone, simple excision with recurrent articular branch neurectomy, and simple excision with PTFJ procedures were 77 %, 56 %, 11.5 %, and 0 %, respectively.
5. Conclusion
Due to low prevalence, there is a lack of higher evidence studies like RCTs and cohort studies that describe ganglion cysts around the PTFJ. Case series and case reports have been included in this review, showing the following findings.
-
1.
Any type of ganglionic cyst around the PTFJ should be thoroughly investigated to find its connection with PTFJ.
-
2.
Every primary ganglionic cyst should be managed with an open procedure that includes complete excision, resection of the connecting stalk to the joint, and resection of the PTFJ (4 ‘D’ = see Table 5).
-
3.
Every primary intra-neural ganglion cyst should be managed with resection of the recurrent articular branch of the PTFJ as an additional procedure (RJ spinner et al.28)
-
4.
The recurrent cyst should be managed with repeat excision and PTFJ fusion or resection. High-quality studies are needed to evaluate the outcome and complications of it.
Funding (information that explains whether and by whom the research was supported)
Not Applicable.
Conflicts of interest/competing interests (include appropriate disclosures)
Not Applicable.
Ethics approval (include appropriate approvals or waivers)
Not Applicable.
Consent to participate (include appropriate statements)
Not Applicable.
Consent for publication (include appropriate statements)
Not Applicable.
Availability of data and material (data transparency)
The data extraction file is available in the link below. https://drive.google.com/drive/folders/1RQsSHfvZnjTYvbJZxXo1FDORuvyvU3Bj.
Authors' contributions
NM, DM, and AN have conceptualized and designed the article along with all the acquisition of data and its analysis. DS and SD supervised the whole process and did the proofreading. The conflict of selection of the disputed study was sorted by senior authors (DS and SD) according to the description in the manuscript.
Declaration of competing interest
None.
Contributor Information
Nirav Mungalpara, Email: nirav.orthodoc@gmail.com.
Dhyey Mungalpara, Email: dkmungalpara3102@gmail.com.
Aarjav Naik, Email: naikaarjav@gmail.com.
Daivesh Shah, Email: dr.daivesh@gmail.com.
Shaival Dalal, Email: Shaival_dalal@yahoo.co.in.
References
- 1.Giard M.C., Pineda C. Ganglion cyst versus synovial cyst? Ultrasound characteristics through a review of the literature. Rheumatol Int. 2015;35:597–605. doi: 10.1007/s00296-014-3120-1. [DOI] [PubMed] [Google Scholar]
- 2.Kao Chun C., Winkler Stefan S., Turner J Harvey. Synovial cyst of spinal facet. Case report. J Neurosurg. 1974;41 3:372–376. doi: 10.3171/jns.1974.41.3.0372. [DOI] [PubMed] [Google Scholar]
- 3.Li Kayi, Barankin Benjamin. Digital mucous cysts. J Cutan Med Surg. 2010;14:199–206. doi: 10.2310/7750.2010.09058. [DOI] [PubMed] [Google Scholar]
- 4.Lateur G., Pailhé R., Refaie R., et al. Ganglion cysts of the proximal tibiofibular articulation: the role of arthrodesis and combined partial fibula excision. Int Orthop. 2018;42(6):1233–1239. doi: 10.1007/s00264-017-3542-y. [DOI] [PubMed] [Google Scholar]
- 5.Rozbruch S.R., Chang V., Bohne W.H., et al. Gangalionic cysts of the lower extremity: an analysis of 54 cases and review of the literature. Orthopedics. 1998;21:141–148. doi: 10.3928/0147-7447-19980201-07. [DOI] [PubMed] [Google Scholar]
- 6.Spinner R.J., Atkinson J.L., Tiel R.L. Peroneal intraneural ganglia: the importance of the articular branch. A unifying theory. J Neurosurg. 2003;99(2):330–343. doi: 10.3171/jns.2003.99.2.0330. [DOI] [PubMed] [Google Scholar]
- 7.Spinner R.J., Desy N.M., Amrami K.K. The unifying articular (synovial) origin for intraneural ganglion cysts: moving beyond a theory. J Hand Surg. 2016;41(7):e223–e224. doi: 10.1016/j.jhsa.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 8.Stack R.E., Bianco A.J., MacCarty C.S. Compression of the peroneal nerve by ganglion cysts: report of nine cases. J. Bone Joint Surg. Br. 1965;47:773–778. [PubMed] [Google Scholar]
- 9.Ward W.G., Eckardt D.L. Ganglion cyst of the proximal tibiofibular joint causing anterior compartment syndrome: a case report and anatomic study. J. Bone Joint Surg. Am. 1994;76:1561–1564. doi: 10.2106/00004623-199410000-00018. [DOI] [PubMed] [Google Scholar]
- 10.Mahaley M.S., Jr. Ganglion of the posterior tibial nerve. J Neurosurg. 1974;40:120–124. doi: 10.3171/jns.1974.40.1.0120. [DOI] [PubMed] [Google Scholar]
- 11.Wadstein Torsten. Two cases of ganglia in the sheath of the peroneal nerve. Acta Orthop Scand. 1932;2(1-4):221–231. doi: 10.3109/17453673208991232. [DOI] [Google Scholar]
- 12.Spinner R.J., Hebert-Blouin M.N., Amrami K.K. A complex cyst characterized into its individual components: a shared pathogenesis from the superior tibiofibular joint. J Surg Orthop Adv. 2010;19(3):143–148. [PubMed] [Google Scholar]
- 13.Ilahi O.A., Younas S.A., Labbe M.R., Edson S.B. Prevalence of ganglion cysts originating from the proximal tibiofibular joint: a magnetic resonance imaging study. Arthroscopy. 2003;19(2):150–153. doi: 10.1053/jars.2003.50007. [DOI] [PubMed] [Google Scholar]
- 14.Streib E.W., Sun S.F., Pfeiffer R.F. Toe extensor weakness resulting from trivial athletic trauma. Am J Sports Med. 1982;10:311–313. doi: 10.1177/036354658201000510. [DOI] [PubMed] [Google Scholar]
- 15.Muckart R.D. Compression of the common peroneal nerve by intramuscular ganglion from the superior tibio-fibular joint. J. Bone Joint Surg. Br. 1976;58(2):241–244. doi: 10.1302/0301-620X.58B2.932088. [DOI] [PubMed] [Google Scholar]
- 16.Barrie H.J., Barrington T.W., Colwill J.C., Simmons E.H. Ganglion migrans of the proximal tibiofibular joint causing lesions in the subcutaneous tissue, muscle, bone, or peroneal nerve: report of three cases and review of the literature. Clin Orthop Relat Res. 1980;149:211–215. [PubMed] [Google Scholar]
- 17.Robert R., Resche F., Lajat Y., et al. Kyste synovial intraneu- ral du sciatique poplite externe. A propos d’un cas. Neurochirurgie. 1980;26:135–143. [PubMed] [Google Scholar]
- 18.Scherman B., Bilbao J., Hudson A., Briggs S. Intraneural ganglion: a case report with electron microscopic observations. Neurosurgery. 1981;8:487–490. doi: 10.1227/00006123-198104000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Spinner R.J., Wang H., Carmichael S.W., Amrami K.K., Scheithauer B.W. Epineurial compartments and their role in intraneural ganglion cyst propagation: an experimental study. Clin Anat. 2007;20(7):826–833. doi: 10.1002/ca.20509. [DOI] [PubMed] [Google Scholar]
- 20.Spinner R.J., Carmichael S.W., Wang H., Parisi T.J., Skinner J.A., Amrami K.K. Patterns of intraneural ganglion cyst descent. Clin Anat. 2008;21 doi: 10.1002/ca.20614. [DOI] [PubMed] [Google Scholar]
- 21.Spinner R.J., Desy N.M., Amrami K.K. Cystic transverse limb of thearticular branch: a pathognomonic sign for peroneal intraneuralganglia at the superior tibiofibular joint. Neurosurgery. 2006;59:157–166. doi: 10.1227/01.NEU.0000219820.31012.22. [DOI] [PubMed] [Google Scholar]
- 22.Spinner Robert J., Atkinson John L.D., Maus Timothy P. Letter to the editor. J. Neurosurg. JNS. 2010;113(6):1331–1332. doi: 10.3171/2010.7.JNS101025. [DOI] [PubMed] [Google Scholar]
- 23.Nonaka Y., Grossi P.M., Filomena C.A., Friedman A.H., Fukush- ima T. Unilateral hypoglossal nerve palsy caused by an intra- neural ganglion cyst. Case report. J Neurosurg. 2010;113:380–383. doi: 10.3171/2010.1.JNS091526. [DOI] [PubMed] [Google Scholar]
- 24.Schajowicz F., Clavel Sainz M., Slullitel J.A. Juxta‐articular bone cysts (intra‐osseous ganglia): a clinicopathological study of eighty‐eight cases. J. Bone Joint Surg. Br. 1979;61:107–116. doi: 10.1302/0301-620X.61B1.422629. [DOI] [PubMed] [Google Scholar]
- 25.Spinner R.J., Desy N.M., Rock M.G., Amrami K.K. Peroneal intraneural ganglia. Part I. Techniques for successful diagnosis and treatment. Neurosurg Focus. 2007;22(6):E16. Published 2007 Jun 15. [PubMed] [Google Scholar]
- 26.Takagishi K., Maeda K., Ikeda T., Itoman M., Yamamoto M. Ganglion causing paralysis of the suprascapular nerve. Diagnosis by MRI and ultrasonography. Acta Orthop Scand. 1991;62:391–393. doi: 10.3109/17453679108994480. [DOI] [PubMed] [Google Scholar]
- 27.Seegar L.L., Bassett L.W. In: MRI: Atlas of Muscu- Loskeletal System. Bassett L.W., Gold R.H., Seegar L.L., editors. Martin Dunitz; London: 1989. Tumour and tumour like conditions; p. 319. [Google Scholar]
- 28.Spinner R.J., Carmichael S.W., Wang H., Parisi T.J., Skinner J.A., Amrami K.K. Patterns of intraneural ganglion cyst descent. Clin Anat. 2008;21 doi: 10.1002/ca.20614. [DOI] [PubMed] [Google Scholar]
- 29.Spinner R., Edwards P., Amrami K. Application of three-dimensional rendering in joint-related ganglion cysts. 2022. https://onlinelibrary.wiley.com/doi/10.1002/ca.20292 Published. [DOI] [PubMed]
- 30.Spinner R.J., Desy N.M., Rock M.G., Amrami K.K. Peroneal intraneural ganglia. Part II. Lessons learned and pitfalls to avoid for successful diagnosis and treatment. Neurosurg Focus. 2007;22(6):E27. Published 2007 Jun 15. [PubMed] [Google Scholar]
- 31.Desy N.M., Lipinski L.J., Tanaka S., et al. Recurrent intraneural ganglion cysts: pathoanatomic patterns and treatment implications. Clin Anat. 2015;28:1058–1069. doi: 10.1002/ca.22615. [DOI] [PubMed] [Google Scholar]
- 32.Lenartowicz K.A., Wolf A.S., Desy N.M., Strakowski J.A., Amrami K.K., Spinner R.J. Preoperative imaging of intraneural ganglion cysts: a critical systematic analysis of the world literature. World Neurosurg. 2022;166:e968–e979. doi: 10.1016/j.wneu.2022.08.005. [DOI] [PubMed] [Google Scholar]
- 33.Huntington L.S., Talia A., Devitt B.M., Batty L. Management and outcomes of proximal tibiofibular joint ganglion cysts: a systematic review. Knee. 2022;37:60–70. doi: 10.1016/j.knee.2022.05.009. [DOI] [PubMed] [Google Scholar]
References
- 34.Damron T.A., Rock M.G. Unusual manifestations of proximal tibiofibular joint synovial cysts. Orthopedics. 1997 Mar;20(3):225–230. doi: 10.3928/0147-7447-19970301-07. PMID: 9088016. [DOI] [PubMed] [Google Scholar]
- 35.Spinner R.J., Atkinson J.L., Scheithauer B.W., et al. Peroneal intraneural ganglia: the importance of the articular branch. Clin. Ser. J. Neurosurg. 2003;99(2):319–329. doi: 10.3171/jns.2003.99.2.0319. [DOI] [PubMed] [Google Scholar]
- 36.Miskovsky S., Kaeding C., Weis L. Proximal tibiofibular joint ganglion cysts: excision, recurrence, and joint arthrodesis. Am J Sports Med. 2004;32(4):1022–1028. doi: 10.1177/0363546503258706. [DOI] [PubMed] [Google Scholar]
- 37.Gulati A., Lechler P., Steffen R., et al. Surgical treatment of recurrent proximal tibio-fibular joint ganglion cysts. Knee. 2014;21(5):932–935. doi: 10.1016/j.knee.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 38.Lateur G., Pailhé R., Refaie R., et al. Ganglion cysts of the proximal tibiofibular articulation: the role of arthrodesis and combined partial fibula excision. Int Orthop. 2018;42:1233–1239. doi: 10.1007/s00264-017-3542-y. [DOI] [PubMed] [Google Scholar]
- 39.Wilson T.J., Mauermann M.L., Rock M.G., Spinner R.J. Outcomes following surgery for peroneal intraneural ganglion cysts. Muscle Nerve. 2018;57(6):989–993. doi: 10.1002/mus.26062. [DOI] [PubMed] [Google Scholar]
- 40.Papanastassiou I.D., Tolis K., Savvidou O., Fandridis E., Papagelopoulos P., Spyridonos S. Ganglion cysts of the proximal tibiofibular joint: low risk of recurrence after total cyst excision. Clin Orthop Relat Res. 2021;479(3):534–542. doi: 10.1097/CORR.0000000000001329. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 41.Clark K. Ganglion of the lateral popliteal nerve. J. Bone and Joint Surg.-Br. 1961;ume:778–783. doi: 10.1302/0301-620X.43B4.784. [DOI] [PubMed] [Google Scholar]
- 42.Katz M. Richard, Lenobel Milton I. Intraneural ganglionic cyst of the peroneal nerve. J Neurosurg. 1970;32(6):692–694. doi: 10.3171/jns.1970.32.6.0692. [DOI] [PubMed] [Google Scholar]
- 43.Cobb Cully A., III, Moiel Richard H. Ganglion of the peroneal nerve. J Neurosurg. 1974;41(2):255–259. doi: 10.3171/jns.1974.41.2.0255. [DOI] [PubMed] [Google Scholar]
- 44.Nucci F., Artico M., Santoro A., et al. Intraneural synovial cyst of the peroneal nerve: report of two cases and review of the literature. Neurosurgery. 1990;26(2):339–344. doi: 10.1097/00006123-199002000-00028. [DOI] [PubMed] [Google Scholar]
- 45.Evans J.D., Neumann L., Frostick S.P. Compression neuropathy of the common peroneal nerve caused by a ganglion. Microsurgery. 1994;15(3):193–195. doi: 10.1002/micr.1920150310. [DOI] [PubMed] [Google Scholar]
- 46.Nicholson T.R., Cohen R.C., Grattan-Smith P.J. Intraneural ganglion of the common peroneal nerve in a 4-year-old boy. J Child Neurol. 1995;10(3):213–215. doi: 10.1177/088307389501000310. [DOI] [PubMed] [Google Scholar]
- 47.O'Rourke P., Byrne John J. Giant ganglion of the proximal tibiofibular joint: a case report. Ir J Med Sci. 1995;164:295–296. doi: 10.1007/BF02967209. [DOI] [PubMed] [Google Scholar]
- 48.Dubuisson A.S., Stevenaert A. Recurrent ganglion cyst of the peroneal nerve: radiological and operative observations. Case report. J Neurosurg. 1996;84(2):280–283. doi: 10.3171/jns.1996.84.2.0280. [DOI] [PubMed] [Google Scholar]
- 49.Kelm J., Ames M., Weissenbach P., Engel C. A ganglion of the superior tibiofibular joint as a mucoid-cystic degeneration of unusual localization. A case report and review of the literature. Knee Surg Sports Traumatol Arthrosc. 1998;6(1):62–66. doi: 10.1007/s001670050073. [DOI] [PubMed] [Google Scholar]
- 50.Fansa H., Plogmeier K., Gonschorek A., Feistner H. Common peroneal nerve palsy caused by a ganglion. Case report. Scand J Plast ReConstr Surg Hand Surg. 1998;32(4):425–427. doi: 10.1080/02844319850158525. [DOI] [PubMed] [Google Scholar]
- 51.Coleman S.H., Beredjeklian P.K., Weiland A.J. Intraneural ganglion cyst of the peroneal nerve accompanied by complete foot drop. A case report. Am J Sports Med. 2001;29(2):238–241. doi: 10.1177/03635465010290022101. [DOI] [PubMed] [Google Scholar]
- 52.Pagnoux C., Lhotellier L., Marek J.J., Ballard M., Chazerain P., Ziza J.M. Synovial cysts of the proximal tibiofibular joint: three case reports. Joint Bone Spine. 2002;69(3):331–333. doi: 10.1016/s1297-319x(02)00403-7. [DOI] [PubMed] [Google Scholar]
- 53.Rawal A., Ratnam K.R., Yin Q., Sinopidis C., Frostick S.P. Compression neuropathy of common peroneal nerve caused by an extraneural ganglion: a report of two cases. Microsurgery. 2004;24(1):63–66. doi: 10.1002/micr.10203. [DOI] [PubMed] [Google Scholar]
- 54.Kili S., Perkins R.D. Common peroneal nerve ganglion following trauma. Injury. 2004;35(9):938–939. doi: 10.1016/S0020-1383(02)00383-2. [DOI] [PubMed] [Google Scholar]
- 55.Kapoor V., Theruvil B., Britton J.M. Excision arthroplasty of superior tibiofibular joint for recurrent proximal tibiofibular cyst. A report of two cases. Joint Bone Spine. 2004;71(5):427–429. doi: 10.1016/j.jbspin.2003.07.011. [DOI] [PubMed] [Google Scholar]
- 56.Hersekli M.A., Akpinar S., Demirors H., et al. Synovial cysts of proximal tibiofibular joint causing peroneal nerve palsy: report of three cases and review of the literature. Arch Orthop Trauma Surg. 2004;124(10):711–714. doi: 10.1007/s00402-004-0717-y. [DOI] [PubMed] [Google Scholar]
- 57.Rubin D.I., Nottmeier E., Blasser K.E., Peterson J.J., Kennelly K. Acute onset of deep peroneal neuropathy during a golf game resulting from a ganglion cyst. J Clin Neuromuscul Dis. 2004;6(2):49–53. doi: 10.1097/00131402-200412000-00001. [DOI] [PubMed] [Google Scholar]
- 58.Bonar S.F., Viglione W., Schatz J., Scolyer R.A., McCarthy S.W. An unusual variant of intraneural ganglion of the common peroneal nerve. Skeletal Radiol. 2006;35(3):165–171. doi: 10.1007/s00256-005-0031-y. [DOI] [PubMed] [Google Scholar]
- 59.Vatansever A., Bal E., Okcu G. Ganglion cysts of the proximal tibiofibular joint review of literature with three case reports. Arch Orthop Trauma Surg. 2006;126(9):637–640. doi: 10.1007/s00402-005-0084-3. [DOI] [PubMed] [Google Scholar]
- 60.Mortazavi S.M.J., Farzan M., Asadollahi S. Proximal tibiofibular joint synovial cyst—one pathology with three different presentations. Knee Surg Sports Traumatol Arthrosc. 2006;14:875–879. doi: 10.1007/s00167-005-0021-6. [DOI] [PubMed] [Google Scholar]
- 61.Aprin H., Weinberg J., Lustrin E.S., Abrutyn D. Peroneal nerve palsy due to an intraneural ganglion: a case report of a 4 1/2-year-old boy. Am J Orthoped. 2007 March;36(3):40–42. [PubMed] [Google Scholar]
- 62.Johnston J.A., Lyne D.E. Intraneural ganglion cyst of the peroneal nerve in a four-year-old girl: a case report. J Pediatr Orthop. 2007;27(8):944–946. doi: 10.1097/BPO.0b013e3181558c05. [DOI] [PubMed] [Google Scholar]
- 63.Dragoni S., Giombini A., Di Cesare A., Ripani M. A synovial ganglion of the knee: two cases in athletes. Int J Sports Med. 2008;29(8):692–695. doi: 10.1055/s-2007-989440. [DOI] [PubMed] [Google Scholar]
- 64.Maheshwari A.V., Muro-Cacho C.A., Temple H.T. Aggressive proximal tibio-fibular joint ganglion cyst after a total knee arthroplasty--a case report. Knee. 2008;15(5):411–415. doi: 10.1016/j.knee.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 65.Greer-Bayramoglu R.J., Nimigan A.S., Gan B.S. Compression neuropathy of the peroneal nerve secondary to a ganglion cyst. Can J Plast Surg. 2008;16(3):181–183. doi: 10.1177/229255030801600307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Waldschmidt U., Slongo T. An unusual cause of paralysis of the peroneal nerve-a case report. J Pediatr Surg. 2010;45(1):259–261. doi: 10.1016/j.jpedsurg.2009.09.039. [DOI] [PubMed] [Google Scholar]
- 67.Stamatis E.D., Manidakis N.E., Patouras P.P. Intraneural ganglion of the superficial peroneal nerve: a case report. J Foot Ankle Surg. 2010;49(4) doi: 10.1053/j.jfas.2010.04.012. 400.e1-400.e4004. [DOI] [PubMed] [Google Scholar]
- 68.Al Mufargi Y.S., Mouch C.A., Ziebarth K., Joeris A., Slongo T. An unusual cause of paralysis of the peroneal nerve: a report of 3 cases [retracted in: hensinger RN, Thompson GH. J Pediatr Orthop. 2012 Oct-Nov;32(7):748] J Pediatr Orthop. 2011;31(5):e50–e52. doi: 10.1097/BPO.0b013e31821f50cb. [DOI] [PubMed] [Google Scholar]
- 69.Spinner R.J., Ibrahim Elshiekh M.A., Tubbs R.S., Turner N.S., 3rd, Amrami K.K. Posttraumatic torsional injury as an indirect cause of fibular intraneural ganglion cysts: case illustrations and potential mechanisms. Clin Anat. 2012;25(5):641–646. doi: 10.1002/ca.21290. [DOI] [PubMed] [Google Scholar]
- 70.Lee Y.S., Kim J.E., Kwak J.H., Wang I.W., Lee B.K. Foot drop secondary to peroneal intraneural cyst arising from tibiofibular joint. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):2063–2065. doi: 10.1007/s00167-012-2194-0. [DOI] [PubMed] [Google Scholar]
- 71.Erdil M., Ozkan K., Ozkan F.U., et al. A rare cause of deep peroneal nerve palsy due to compression of synovial cyst - case report. Int. J. Surg. Case Rep. 2013;4(5):515–517. doi: 10.1016/j.ijscr.2012.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mulligan E.P., McCain K. Common fibular (peroneal) neuropathy as the result of a ganglion cyst. J Orthop Sports Phys Ther. 2012;42(12):1051. doi: 10.2519/jospt.2012.0421. [DOI] [PubMed] [Google Scholar]
- 73.Ozden R., Uruc V., Kalacı A., Dogramacı Y. Compression of common peroneal nerve caused by an extraneural ganglion cyst mimicking intermittent claudication. J Brachial Plexus Peripher Nerve Inj. 2013;8(1):5. doi: 10.1186/1749-7221-8-5. Published 2013 May 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Muramatsu K., Hashimoto T., Tominaga Y., Tamura K., Taguchi T. Unusual peroneal nerve palsy caused by intraneural ganglion cyst: pathological mechanism and appropriate treatment. Acta Neurochir. 2013;155(9):1757–1761. doi: 10.1007/s00701-013-1768-z. [DOI] [PubMed] [Google Scholar]
- 75.Nikolopoulos D., Safos G., Sergides N., Safos P. Deep peroneal nerve palsy caused by an extraneural ganglion cyst: a rare case. Case Rep. Orthop. 2015;2015 doi: 10.1155/2015/861697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kukreja M.M., Telang V.G. Common peroneal nerve palsy secondary to a proximal tibi- ofibular joint “ganglion cyst”—a case report and review of literature. Open J Orthoped. 2015;5:369–377. doi: 10.4236/ojo.2015.511050. [DOI] [Google Scholar]
- 77.Prasad N.K., Desy N.M., Howe B.M., Amrami K.K., Spinner R.J. Subparaneurial ganglion cysts of the fibular and tibial nerves: a new variant of intraneural ganglion cysts. Clin Anat. 2016;29(4):530–537. doi: 10.1002/ca.22671. [DOI] [PubMed] [Google Scholar]
- 78.Consales A., Pacetti M., Imperato A., Valle M., Cama A. Intraneural ganglia of the common peroneal nerve in children: case report and review of the literature. World Neurosurg. 2016;86 doi: 10.1016/j.wneu.2015.10.023. 510.e11-510.e5.1E17. [DOI] [PubMed] [Google Scholar]
- 79.Zumrut M., Demirayak M., Kucukapan A. An unusual cause of foot drop: peroneal extraneural ganglion cyst. Pakistan J Med Sci. 2016;32(4):1047–1050. doi: 10.12669/pjms.324.9998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sevimli R., Karakaplan M., Korkmaz M.F., Salih A.H. Drop foot developed secondary to peroneal nerve located intraneural ganglion caused by proximal tibiofibular joint: case report. Gavin J. Case Rep. 2016. 2016:10–12. [Google Scholar]
- 81.Yan X., Zhang Z., Lin N., Xie T., Ye Z. Fibular juxta-articular ganglion: a rare case report and literature review. Mol. Clin Oncol. 2016;5(5):590–592. doi: 10.3892/mco.2016.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Alsahhaf A., Renno W. Ganglion cyst at the proximal tibiofibular joint in a patient with painless foot drop. Pain Physician. 2016;19(8):E1147–E1160. [PubMed] [Google Scholar]
- 83.Ratanshi I., Clark T.A., Giuffre J.L. Immediate nerve transfer for treatment of peroneal nerve palsy secondary to an intraneural ganglion: case report and review. Plast Surg (Oakv). 2018;26(2):80–84. doi: 10.1177/2292550317747844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kara A., Yalçın S., Çelik H., Kuyucu E., Şeker A. Compression neuropathy of the common peroneal nerve caused by an intraosseous ganglion cyst of fibula. Int. J. Surg. Case Rep. 2017;40:10–12. doi: 10.1016/j.ijscr.2017.08.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Schmidt I. Common peroneal nerve palsy caused by an initially misdiagnosed extraneural and intraneural benign ganglion cyst of the peroneal nerve in a 11-year-old child: a rare but severe condition. Int J Case Rep Images. 2017;8(9):623–626. [Google Scholar]
- 86.Keser N., Akpinar P., Is M., Aktas I. Irreversible footdrop as a consequence of neglected knee pain in an adolescent with a peroneal intraneural ganglion cyst. World Neurosurg. 2018;111:307–310. doi: 10.1016/j.wneu.2017.12.168. [DOI] [PubMed] [Google Scholar]
- 87.Kruspi S.M., Dietrich M. Peroneal nerve palsy caused by a synovial cyst of the proximal tibiofibular joint: a case report. Case Stud Surg. 2018;4(2):11–14. [Google Scholar]
- 88.Adil Abrar, Basener Clint, Checketts Jake. Intraneural synovial cyst of the common peroneal nerve: an unusual cause of foot drop with four-year follow-up. Case Rep. Orthopedics. 2019 doi: 10.1155/2019/8045252. 4 pages, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Park S.H., Do H.K., Jo G.Y. Compressive peroneal neuropathy by an intraneural ganglion cyst combined with L5 radiculopathy: a case report. Medicine (Baltim) 2019;98(44) doi: 10.1097/MD.0000000000017865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Aymen F., Jacem S., Youssef O., Issam A., Abderrazek A. Peroneal nerve palsy caused by a synovial cyst of the proximal tibiofibular joint: a report of two cases and review of the literature. Pan Afr. Med. J. 2019;34(115) doi: 10.11604/pamj.2019.34.115.18339. Published 2019 Oct 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Apel P.J., Zielinski J.A., Grider D.J., Brown R.D., Orfield N.J. Intraneural peroneal ganglion cyst excision in a pediatric patient: a case report. JBJS Case Connect. 2020;10(1) doi: 10.2106/JBJS.CC.19.00272. [DOI] [PubMed] [Google Scholar]
- 92.Stamiris S., Stamiris D., Sarridimitriou A., Anestiadou E., Karampalis C., Vrangalas V. Acute complete foot drop caused by intraneural ganglion cyst without a prior traumatic event. Case Rep. Orthop. 2020;2020 doi: 10.1155/2020/1904595. Published 2020 Mar 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Singh S., Singh R., Tanwar M., Kaur K. Giant ganglion cyst of the proximal tibiofibular joint with peroneal nerve palsy: a case report. J Orthop Case Rep. 2020;10(2):5–8. doi: 10.13107/jocr.2020.v10.i02.1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sim J., Kwak H., Lee S., Min K. Peroneal neuropathy caused by an extraneural ganglion cyst in the supracondylar area of the femur: a case report. Medicine (Baltim) 2020;99(37) doi: 10.1097/MD.0000000000022123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Herndon C.L., Alonge T., McDermott Nance E., Cooper H.J. Concurrent surgical management of advanced osteoarthritis of the knee and proximal tibiofibular joint with compressive peroneal neuropathy: 3-year follow-up on a complex case. Arthroplast Today. 2020;6(4):993–997. doi: 10.1016/j.artd.2020.09.009. Published 2020 Dec 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Khan G., Kazmi Z., Khan B., Khan N., Datta S. Ganglion cyst at the proximal tibiofibular joint - a rare cause of compression neuropathy of the peroneal nerve. Radiol. Case Rep. 2021;17(1):99–102. doi: 10.1016/j.radcr.2021.10.004. Published 2021 Nov 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Thalla N., White W.D., Mansfield J.T., Souza J.M., Miller M.E. Spontaneous proximal tibiofibular joint ganglion cyst as a rare cause of acute foot drop: a case report. J. Musculoskelet Disord. Treat. 2021;7 doi: 10.23937/2572-3243.1510095. 095. [DOI] [Google Scholar]
- 98.Broekx S., Van Der Straeten R., D'Haen B., Vandevenne J., Ernon L., Weyns F. Intraneural ganglion cyst of the common peroneal nerve causing foot drop in a 12-year old child. Clin Neurol Neurosurg. 2021;209 doi: 10.1016/j.clineuro.2021.106915. [DOI] [PubMed] [Google Scholar]
- 99.Marathe A., Song B., Sulapas I., Jayaram P. Doppler ultrasound utility in intraneural ganglion cyst diagnosis. Am J Phys Med Rehabil. 2022;101(5) doi: 10.1097/PHM.0000000000001967. [DOI] [PubMed] [Google Scholar]
- 100.Bucher F., Maerz V., Obed D., Vogt P.M., Weyand B. Intraneural ganglion of the peroneal nerve-A rare cause of pediatric peroneal nerve palsy: a case report. Eur J Pediatr Surg Rep. 2022;10(1):e33–e36. doi: 10.1055/s-0042-1742608. Published 2022 Mar 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Won K.H., Kang E.Y. Differential diagnosis and treatment of foot drop caused by an extraneural ganglion cyst above the knee: a case report. World J. Clin. Cases. 2022;10(21):7539–7544. doi: 10.12998/wjcc.v10.i21.7539. [DOI] [PMC free article] [PubMed] [Google Scholar]