Abstract
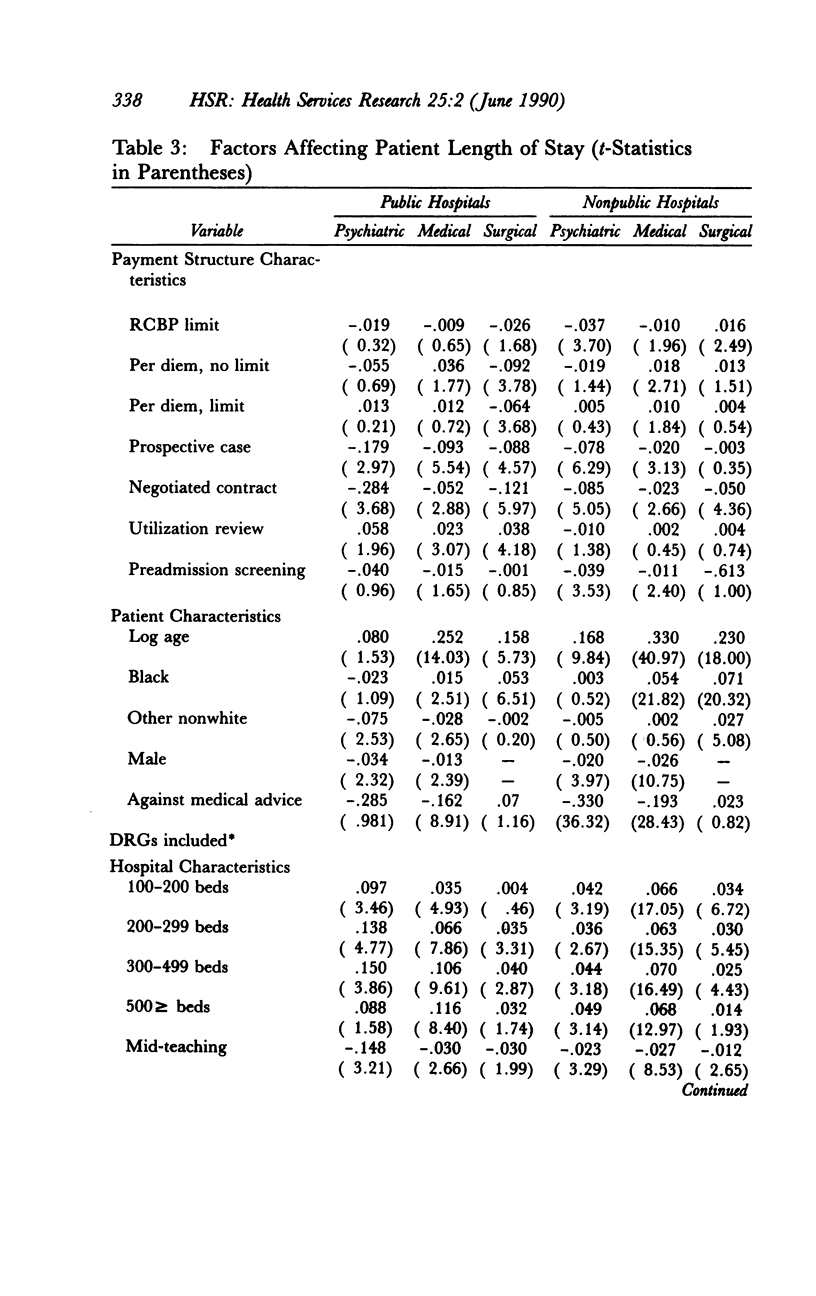
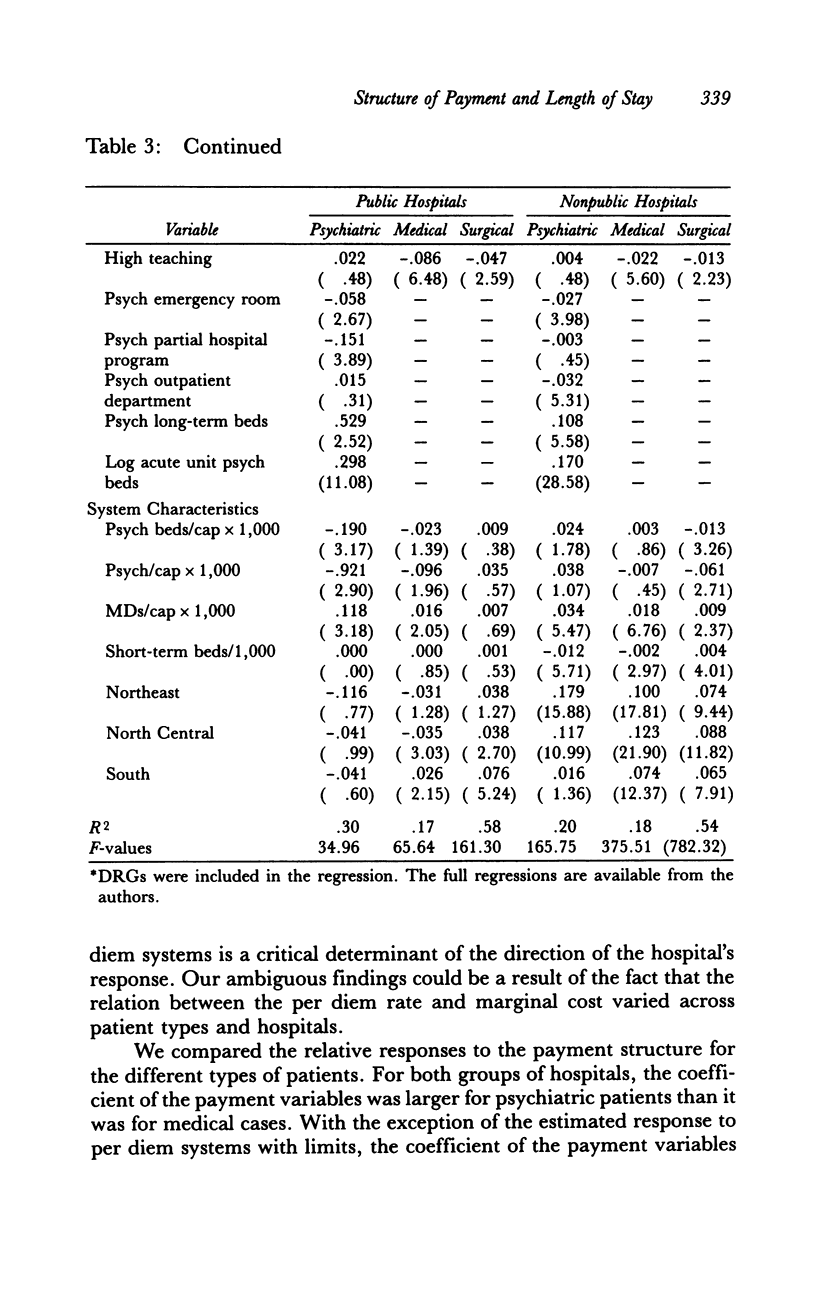
In response to rapidly rising costs, payers for health care services have made a number of changes in the way they reimburse hospitals for care. In this article we study the effect of different payment methods on the length of stay of Medicaid patients. We examine supply response by type of patient (medical, surgical, and psychiatric) and hospital ownership. We find that per case payment systems and negotiated contracts lead to significant decreases in the length of stay for all groups. Prospective per diem with limits in most cases leads to decreases in the length of stay. In general, we find that the supply response is stronger for psychiatric patients than for medical and surgical patients, and that publicly owned hospitals are more responsive to payment system incentives than are nonpublic hospitals.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
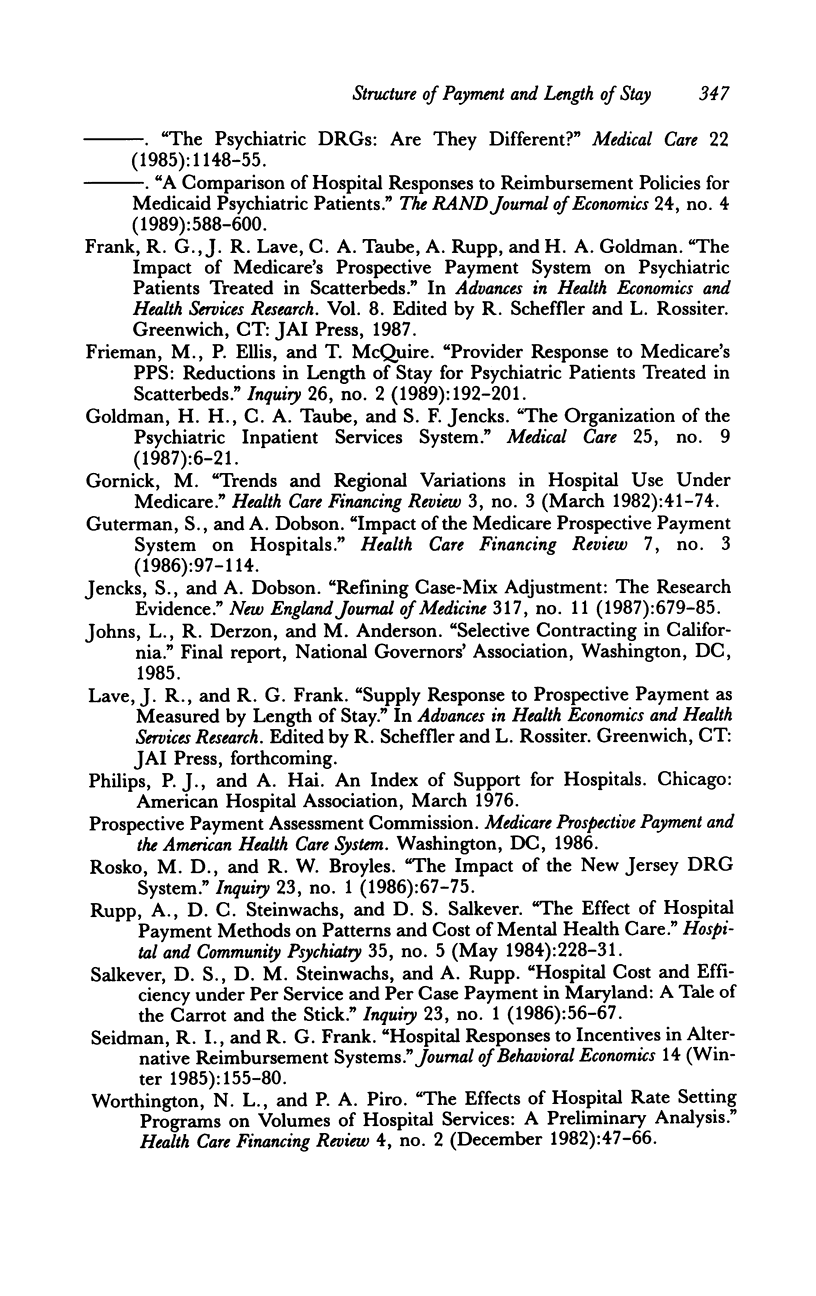
- Ellis R. P., McGuire T. G. Provider behavior under prospective reimbursement. Cost sharing and supply. J Health Econ. 1986 Jun;5(2):129–151. doi: 10.1016/0167-6296(86)90002-0. [DOI] [PubMed] [Google Scholar]
- Feder J., Hadley J., Zuckerman S. How did Medicare's prospective payment system affect hospitals? N Engl J Med. 1987 Oct 1;317(14):867–873. doi: 10.1056/NEJM198710013171405. [DOI] [PubMed] [Google Scholar]
- Freiman M. P., Ellis R. P., McGuire T. G. Provider response to Medicare's PPS: reductions in length of stay for psychiatric patients treated in scatter beds. Inquiry. 1989 Summer;26(2):192–201. [PubMed] [Google Scholar]
- Gornick M. Trends and regional variations in hospital use under Medicare. Health Care Financ Rev. 1982 Mar;3(3):41–73. [PMC free article] [PubMed] [Google Scholar]
- Guterman S., Dobson A. Impact of the Medicare prospective payment system for hospitals. Health Care Financ Rev. 1986 Spring;7(3):97–114. [PMC free article] [PubMed] [Google Scholar]
- Jencks S. F., Dobson A. Refining case-mix adjustment. The research evidence. N Engl J Med. 1987 Sep 10;317(11):679–686. doi: 10.1056/NEJM198709103171106. [DOI] [PubMed] [Google Scholar]
- Rosko M. D., Broyles R. W. The impact of the New Jersey all-payer DRG system. Inquiry. 1986 Spring;23(1):67–75. [PubMed] [Google Scholar]
- Salkever D. S., Steinwachs D. M., Rupp A. Hospital cost and efficiency under per service and per case payment in Maryland: a tale of the carrot and the stick. Inquiry. 1986 Spring;23(1):56–66. [PubMed] [Google Scholar]
- Worthington N. L., Piro P. A. The effects of hospital rate-setting programs on volumes of hospital services: a preliminary analysis. Health Care Financ Rev. 1982 Dec;4(2):47–66. [PMC free article] [PubMed] [Google Scholar]


