Abstract
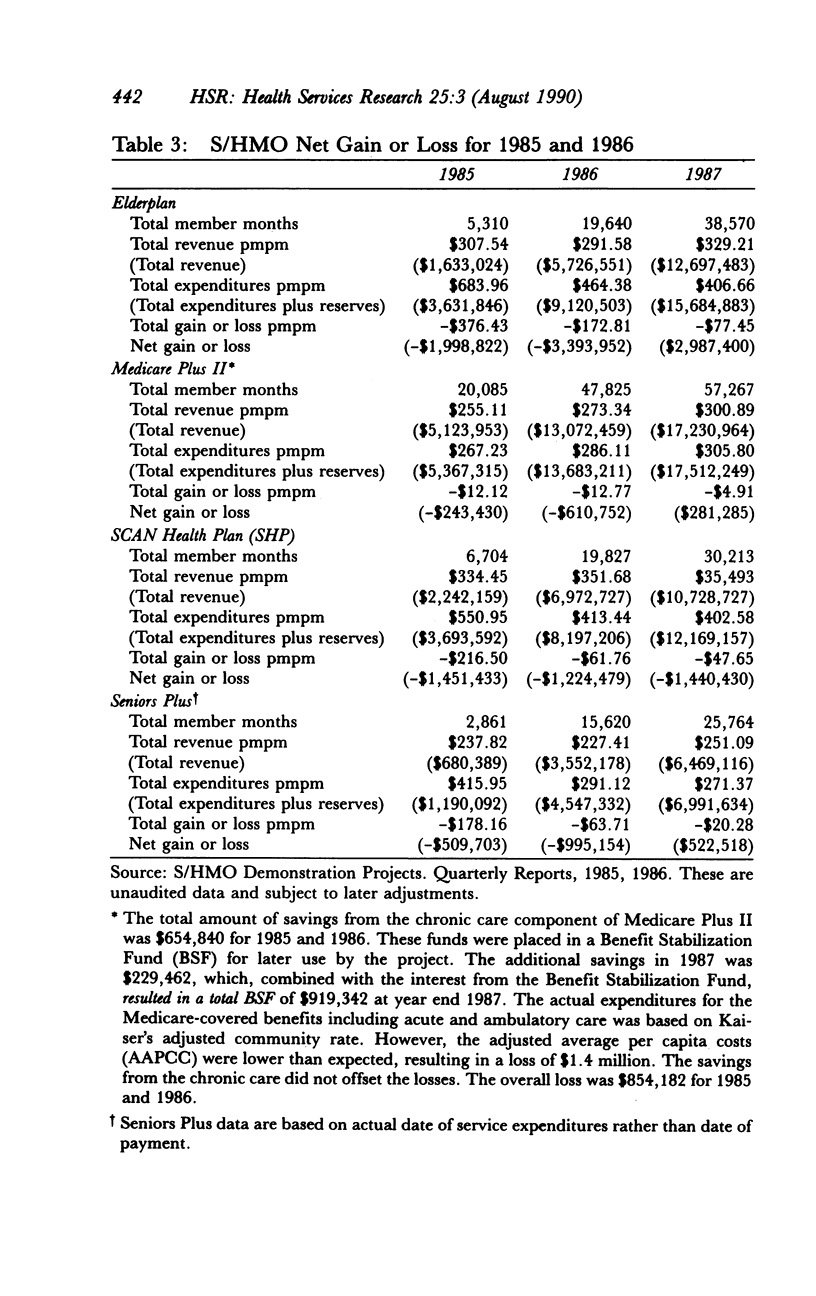
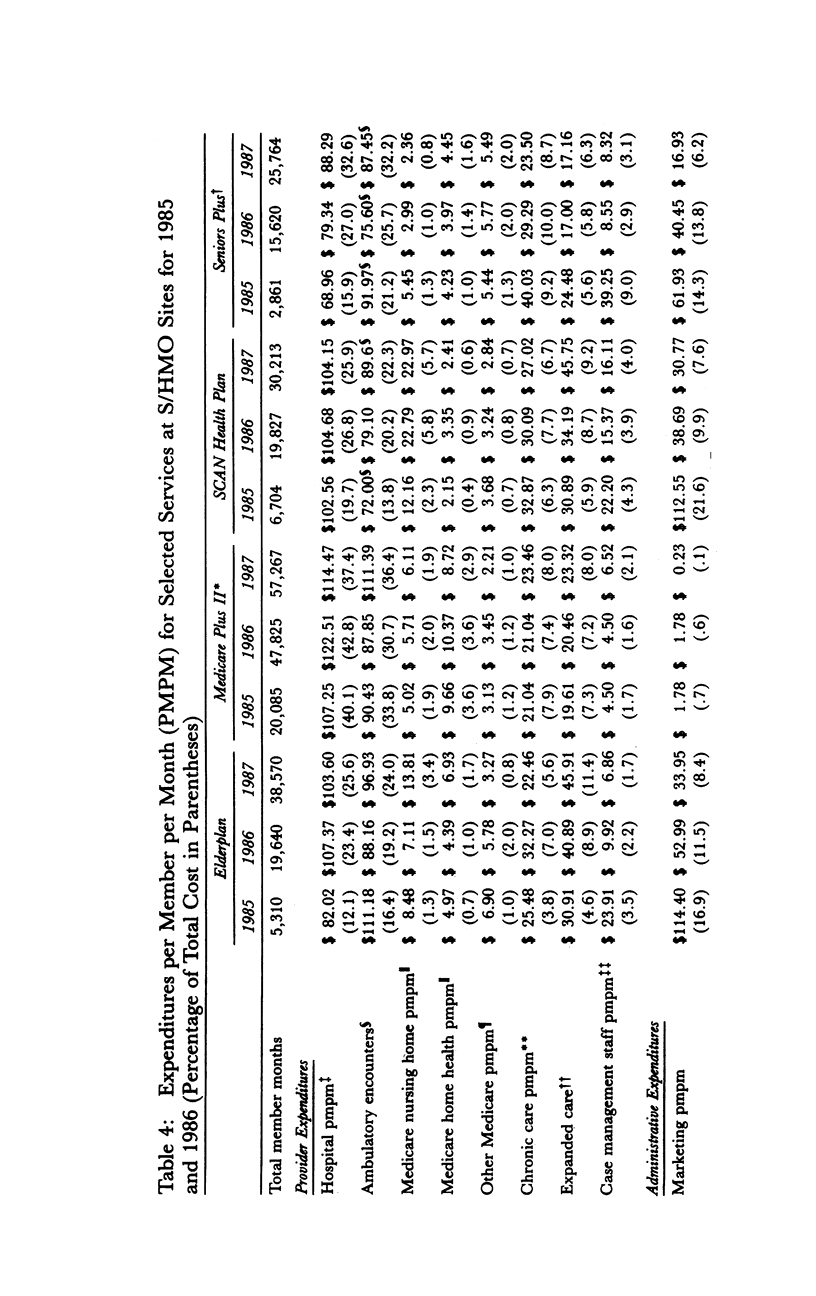
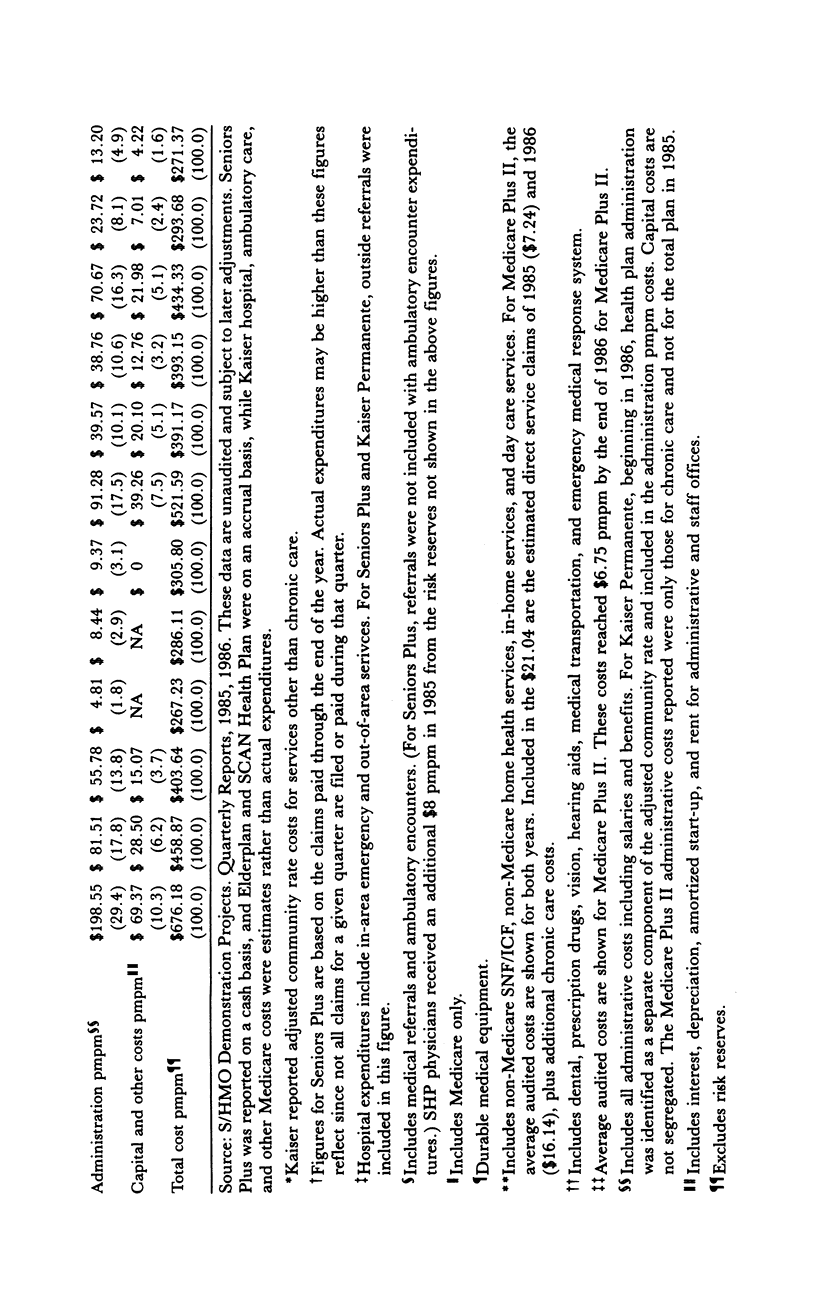
The Social/Health Maintenance Organization (S/HMO) is a four-site national demonstration. This program combines Medicare Part A and B coverage, with various extended and chronic care benefits, into an integrated health plan. The provision of these services extends both the traditional roles of HMOs and that of long-term care community-service case management systems. During the initial 30 months of operation the four S/HMOs shared financial risk with the Health Care Financing Administration. This article reports on this developmental period. During this phase the S/HMOs had lower-than-expected enrollment levels due in part to market competition, underfunding of marketing efforts, the limited geographic area served, and an inability to differentiate the S/HMO product from that of other Medicare HMOs. The S/HMOs were allowed to conduct health screening of applicants prior to enrolling them. The number of nursing home-certifiable enrollees was controlled through this mechanism, but waiting lists were never very long. Persons joining S/HMOs and other Medicare HMOs during this period were generally aware of the alternatives available. S/HMO enrollees favored the more extensive benefits; HMO enrollees considerations of cost. The S/HMOs compare both newly formed HMOs and established HMOs. On the basis of administrator cost, it is more efficient to add chronic care benefits to an HMO than to add an HMO component to a community care provider. All plans had expenses greater than their revenues during the start-up period, but they were generally able to keep service expenditures within planned levels.
Full text
PDF

























Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Capitman J. A., Haskins B., Bernstein J. Case management approaches in coordinated community-oriented long-term care demonstrations. Gerontologist. 1986 Aug;26(4):398–404. doi: 10.1093/geront/26.4.398. [DOI] [PubMed] [Google Scholar]
- Kemper P., Applebaum R., Harrigan M. Community care demonstrations: what have we learned? Health Care Financ Rev. 1987 Summer;8(4):87–100. [PMC free article] [PubMed] [Google Scholar]
- Weissert W. G. Seven reasons why it is so difficult to make community-based long-term care cost-effective. Health Serv Res. 1985 Oct;20(4):423–433. [PMC free article] [PubMed] [Google Scholar]
- Yordi C. L., Waldman J. A consolidated model of long-term care: service utilization and cost impacts. Gerontologist. 1985 Aug;25(4):389–397. doi: 10.1093/geront/25.4.389. [DOI] [PubMed] [Google Scholar]
- Zawadski R. T., Ansak M. L. Consolidating community-based long-term care: early returns from the On Lok demonstration. Gerontologist. 1983 Aug;23(4):364–369. doi: 10.1093/geront/23.4.364. [DOI] [PubMed] [Google Scholar]
- Zawadski R. T., Eng C. Case management in capitated long-term care. Health Care Financ Rev. 1988 Dec;Spec No:75–81. [PMC free article] [PubMed] [Google Scholar]


