Abstract
Background
Racial and ethnic disparities in health status are pervasive at all stages of the life cycle. One approach to reducing health disparities involves mobilizing community coalitions that include representatives of target populations to plan and implement interventions for community level change. A systematic examination of coalition‐led interventions is needed to inform decision making about the use of community coalition models.
Objectives
To assess effects of community coalition‐driven interventions in improving health status or reducing health disparities among racial and ethnic minority populations.
Search methods
We searched MEDLINE, EMBASE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Central Register of Controlled Trials (CENTRAL), PsycINFO, Social Science Citation Index, Dissertation Abstracts, System for Information on Grey Literature in Europe (SIGLE) (from January 1990 through September 30, 2013), and Global Health Library (from January 1990 through March 31, 2014).
Selection criteria
Cluster‐randomized controlled trials, randomized controlled trials, quasi‐experimental designs, controlled before‐after studies, interrupted time series studies, and prospective controlled cohort studies. Only studies of community coalitions with at least one racial or ethnic minority group representing the target population and at least two community public or private organizations are included. Major outcomes of interest are direct measures of health status, as well as lifestyle factors when evidence indicates that these have an effect on the direct measures performed.
Data collection and analysis
Two review authors independently extracted data and assessed risk of bias for each study.
Main results
Fifty‐eight community coalition‐driven intervention studies were included. No study was considered to be at low risk of bias. Behavioral change outcomes and health status change outcomes were analyzed separately. Outcomes are grouped by intervention type. Pooled effects across intervention types are not presented because the diverse community coalition‐led intervention studies did not examine the same constructs or relationships, and they used dissimilar methodological designs. Broad‐scale community system level change strategies led to little or no difference in measures of health behavior or health status (very low‐certainty evidence). Broad health and social care system level strategies leds to small beneficial changes in measures of health behavior or health status in large samples of community residents (very low‐certainty evidence). Lay community health outreach worker interventions led to beneficial changes in health behavior measures of moderate magnitude in large samples of community residents (very low‐certainty evidence). Lay community health outreach worker interventions may lead to beneficial changes in health status measures in large samples of community residents; however, results were not consistent across studies (low‐certainty evidence). Group‐based health education led by professional staff resulted in moderate improvement in measures of health behavior (very low‐certainty evidence) or health status (low‐certainty evidence). Adverse outcomes of community coalition‐led interventions were not reported.
Authors' conclusions
Coalition‐led interventions are characterized by connection of multi‐sectoral networks of health and human service providers with ethnic and racial minority communities. These interventions benefit a diverse range of individual health outcomes and behaviors, as well as health and social care delivery systems. Evidence in this review shows that interventions led by community coalitions may connect health and human service providers with ethnic and racial minority communities in ways that benefit individual health outcomes and behaviors, as well as care delivery systems. However, because information on characteristics of the coalitions themselves is insufficient, evidence does not provide an explanation for the underlying mechanisms of beneficial effects. Thus, a definitive answer as to whether a coalition‐led intervention adds extra value to the types of community engagement intervention strategies described in this review remains unattainable.
Plain language summary
Community coalition‐driven interventions to improve health status and reduce disparities in racial and ethnic minority populations
Unequal health status among racial and ethnic minority populations compared with the general population is a worldwide public health problem. Decades of public health interventions have led to little success in reducing inequalities in health among racial and ethnic minorities. One approach to reducing health disparities involves using coalitions that include representatives of minority communities to create supportive community environments for healthy choices and quality of life. This review looked for evidence that interventions driven by community coalitions improve health status or reduce health disparities among racial and ethnic minority populations.
This review, which included searches of databases from January 1990 through March 31, 2014, found 58 community coalition‐driven studies, which addressed a wide array of health outcomes and risk behaviors. Only studies of community coalitions with at least one racial or ethnic minority group representing the target population and at least two community‐based public or private organizations were included. This review examined the effects of four types of strategies or interventions used by community coalitions.
Community system‐level change strategies (such as initiatives targeting physical environments like housing, green spaces, neighborhood safety, or regulatory processes and policies) have produced small inconsistent effects; broad health and social care system‐level strategies (such as programs targeting behavior of staff in a health or social care system, accessibility of services, or policies, procedures, and technologies designed to improve quality of care) have had consistently positive small effects; interventions that used lay community health outreach workers or group‐based health education led by professional staff have produced fairly consistent positive effects; and group‐based health education led by peers has had inconsistent effects.
This review shows that interventions led by community coalitions may connect health and human service providers with ethnic and racial minority communities in ways that benefit individual health outcomes and behaviors, as well as care delivery systems. However, to achieve the same levels of health across communities, regardless of race or ethnicity, we need to know specifically how a program does or does not work. This will require better information on how some programs described in this review brought about beneficial change and theresources needed, so they can be replicated. Furthermore, we need better scientific tools to improve our ability to identify effects of programs on whole community systems and to understand the leverage points that, when employed appropriately, shift the distribution of health toward equity.
Summary of findings
for the main comparison.
| Community coalition‐driven interventions to reduce health disparities in racial and ethnic minority populations | ||||
|
Population: racial and ethnic minority populations including adults and children Setting: community‐based settings, primarily in urban areas in high‐income countries Interventions: (1) broad‐scale community system level change strategies; (2) health and social care system level change strategies; (3) lay community health outreach workers; and (4) group‐based health education and support for targeted risk groups led by trained peers or by health professionals Comparision: no intervention (48 studies) or alternative intervention (10 studies) | ||||
| ||||
| Outcomes | Impact | Number of participants (studies) | Quality of the evidence (GRADE)* | Comments |
| Improvement in measures of health behavior at 24 to 48 months of follow‐up | Broad‐scale community system level change strategies lead to little or no difference in health behavior measures in large samples of community residents |
29,474 (7) | ⊝⊕⊝⊝ Very low certainty |
Studies targeted entire municipalities |
| Improvement in measures of health status at 24 to 60 months of follow‐up | Broad‐scale community system level change strategies lead to little or no difference in health status measures in large samples of community residents | 14,431 (7) | ⊝⊕⊝⊝ Very low certainty |
Studies targeted entire municipalities |
| ||||
| Improvement in measures of health behavior at 24 to 48 months of follow‐up | Broad health and social care system level strategies lead to small beneficial changes in measures of health behavior in large samples of community residents | 52,849 (4) | ⊝⊕⊝⊝ Very low certainty | Studies targeted entire municipalities |
| Improvement in measures of health status at 6 to 36 months of follow‐up | Broad health and social care system level strategies lead to small beneficial changes in measures of health status in large samples of community residents | 21,607 (3) | ⊝⊕⊕⊝ Low certainty |
Studies targeted entire municipalities |
| ||||
| Improvement in measures of health behavior at 3 to 48 months of follow‐up | Lay community health outreach worker interventions lead to beneficial changes in health behavior measures of moderate magnitude in fairly large samples of community residents |
4957 (5) | ⊝⊕⊝⊝ Very low certainty | |
| Improvement in measures of health status at 12 to 48 months of follow‐up | Lay community health outreach worker interventions may lead to beneficial change in health status measures in fairly large samples of community residents; however, results were not consistent across studies | 1833 (4) | ⊝⊕⊕⊝ Low certainty | |
| ||||
| Improvement in measures of health behavior at 4 to 36 months of follow‐up | Peer‐led health education and support to small groups yielded Inconsistent findings — either little or no effect or large effects — on health behavior measures in populations targeted for higher health risks |
4447 (9) | ⊝⊕⊝⊝ Low certainty | |
| Improvement in measures of health status at 2 to 12 months of follow‐up | Peer‐led health education and support for small groups may improve weight control outcomes | > 251 (2) | ⊝⊕⊕⊝ Low certainty | |
| ||||
| Improvement in measures of health behavior at 6 to 36 months of follow‐up | Professionally led health education and support for small groups may lead to beneficial change in measures of health behavior in populations targeted for higher health risks | 1209 (3) | ⊝⊕⊝⊝ Very low certainty | |
| Improvement in measures of health status at 12 to 40 months of follow‐up | Professionally led health education and support for small groups improve health status measures in populations targeted for higher health risks | 783 (2) | ⊝⊕⊕⊝ Low certainty | |
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
* Characteristics of the evidence base (i.e. 67% non‐randomized studies, several of which evaluated outcomes in large population‐based samples) in this review resulted in an assessment of evidence as low to quite low in certainty. Although the aim of the table is to provide transparency to review users, this method of combining internal and external validity assessments may not yield reliable predictors of the impact of further research on our confidence in the estimate of effect.
Background
Description of the condition
Unfavorable racial and ethnic disparities in health status are pervasive and can be identified at all stages of the life cycle, from birth to old age (LaVeist 2005). Socioeconomic conditions — including poverty, inadequate educational opportunities, unemployment, limited access to basic services and goods such as nutritional foods, and poor quality health care — contribute to health disparities (Marmot 2006). Some groups in society are disproportionately exposed to adverse social conditions as a consequence of differing from the predominant population (e.g. in terms of ethnic background, language, culture, religion) and experience differential treatment and discrimination (Williams 2010). One approach to reducing health disparities has been to mobilize community representatives of target populations to work collaboratively with multi‐sector public and private organizations to identify common health issues, develop program or policy interventions, and attempt to bring about community‐level change that supports health‐promoting opportunities and behaviors (Bazzoli 2003; Liao 2011; Shortell 2002). This represents a departure from a service model that views community residents as simply recipients of services and instead engages them in mobilizing resources to reduce health disparities.
Description of the intervention
Increasingly, government and private funding initiatives are promoting coalitions, collaborations, and other interorganizational approaches to address complex community health issues. Community coalitions are one strategy in the wider range of community‐based co‐operative programs that involve community members in programs to improve population health (e.g. community‐based participatory research, lay community health workers, advisory boards that include community members). Specifically, community coalitions are conglomerates of citizen groups, public and private organizations, and professions (Dluhy 1990) that are characterized by representation from multiple community sectors in bottom‐up planning and decision making. They operate through partnerships and emphasize using local assets and resources to build community capacity. The focus of a community coalition may vary depending on the sectors of the community involved (e.g. education, public safety, public health). Characteristics of these partnerships and organizational structures affect how a coalition functions and how resources are exchanged (Mizrahi 2001). Factors such as clarity of mission, coalition leadership, established governance structures, training and technical support, processes of communication, and member satisfaction can advance or impede the likelihood that a coalition can mobilize resources and implement interventions (Kadushin 2005; Mitchell 2000; Roussos 2000; Zakocs 2006). The broad cross‐sector composition and the voluntary nature of community coalitions distinguish them from other public health models.
The theory and principles behind increasing control of local communities over their affairs and using multi‐agency partnerships to bring together the resources necessary to achieve common goals have antecedents in health promotion and disease prevention coalitions (Green 1990), as well as in community development models (Chavis 1992); moreover, they draw from several theories, including social ecology, social capital, and community empowerment, as well as organizational behavior theories such as network and open‐systems theories (Kreuter 2002; Stokols 1996; Wandersman 1996). This now widely used strategy is based on the premise that health is a product of complex interactions between the individual and the social environment and thus is amenable to influence by community‐based collaborative efforts (Anderson 2003; Stokols 1992). The coalition's choice of a health improvement issue and intervention strategy is based on the shared goals and resources of member stakeholders and funders. A broad range of topics is anticipated because of the sectors involved (e.g. transportation, housing), the community population targeted (e.g. youth, seniors, high‐risk individuals), and the conditions of interest (e.g. chronic disease, substance abuse, access to care).
To summarize, this multi‐sector coalition model is a social initiative that connects a community targeted for intervention with stakeholders who share a common interest in reducing health disparities by changing community‐level structures, processes, and policies to promote the health and well‐being of local residents.
How the intervention might work
Some key assumptions underlie community‐based health programs in general, and community coalition models in particular. The focus on community stems from the recognition that "humans live in, are shaped by, and in turn shape the environment in which they live" (Nilsen 2006). Both geographic location and networks of social relationships exert influence. The notion of community participation — another key aspect — places value on members' knowledge of "what matters." Intersectoral collaboration recognizes that many factors that impact health are outside of the health field. In addition, collaboration across sectors allows pooling of local community knowledge and resources with external partners' contributions of financial and technical support to achieve common goals. Finally, the aim of community‐based strategies is to control determinants of morbidity and mortality while lessening risk across the population. Thus community‐level, rather than individual‐level, outcomes are the goal. Furthermore, long‐term, multi‐faceted intervention strategies (behavioral and structural) are needed to achieve results (Nilsen 2006).
A community coalition provides a structured arrangement for collaboration by a broad constituency of participants who represent diverse interest groups, agencies, organizations, and institutions (Butterfoss 2002). Although some coalition members can be described as interested citizens or volunteers, many members represent organizations. The logic model provided in Figure 1 depicts the program theory underlying community coalitions that was used to guide this systematic review (Butterfoss 2002). Coalitions are formed when a lead agency or a convening group takes action on a community issue (e.g. youth drug and alcohol use); they may result from an opportunity (e.g. government funding for community‐based asthma prevention) or sometimes from a mandatory requirement by the funding source (e.g. Robert Wood Johnson Foundation funding for the Fighting Back Initiative). Governments and foundations see community coalitions as a means of reducing costs and duplication of effort through blending of resources and savings of prevention programs at the local level, where they are intended to have an impact. But as policymakers look increasingly to community coalitions as a solution to complex social and public health problems, community members must understand how these social initiatives function, and when and why they do or do not work as intended.
1.
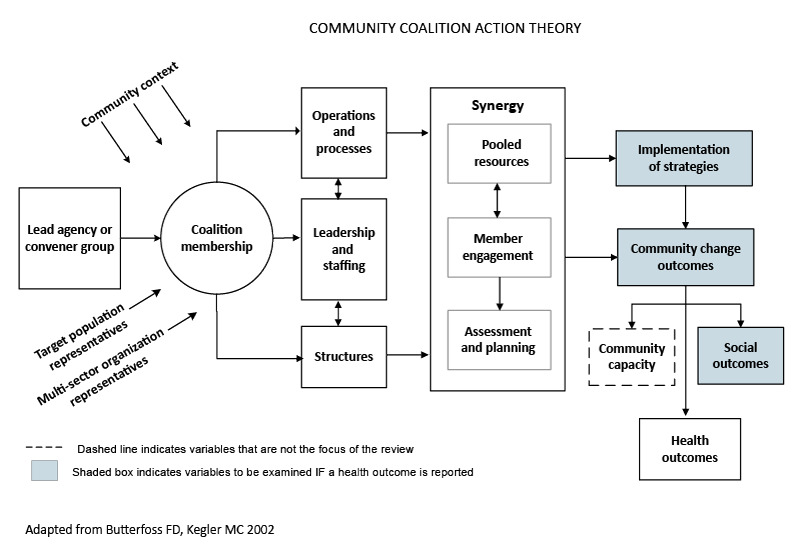
Logic model.
Why it is important to do this review
The World Health Assembly has issued a resolution on reducing health inequities through action on social determinants of health (WHO 2009). This resolution requires continued research on interventions to reduce health disparities within sectors beyond health care. Furthermore, increased emphasis has been placed on applying participatory processes to reduce health disparities. Engaging communities and civil society more inclusively and transparently in policymaking processes through meaningful collaboration in governance was a key point at the 2011 World Conference on Social Determinants of Health (WHO 2011). Closing the gap in health disparities is not just a moral imperative — it is an economic one as well. Health inequities are costly in terms of wasted human potential, lost productivity, and expensive treatment for preventable conditions. A study commissioned by the Joint Center for Political and Economic Studies in the United States provides insight into the financial burden for society imposed by racial and ethnic health disparities (LaVeist 2009). Eliminating disparities would have reduced direct medical costs by USD 229.4 billion over the four‐year period from 2003 to 2006, and indirect costs of these inequities by USD 1.24 trillion.
What is lacking is a rigorous systematic review of the literature on the effectiveness of community coalition models in reducing racial and ethnic disparities in health and well‐being. Previous literature reviews have yielded equivocal findings regarding the success of community coalitions in addressing complex health problems (Berkowitz 2001; Kreuter 2000; Roussos 2000; Wagner 2000a; Zakocs 2006). A better understanding of the types of coalition structures and processes critical for effectiveness is needed, as this approach continues to be a popular public health strategy. Information is also needed on the benefits and costs and potential adverse effects that result when community coalitions are used as a bridge between networks of service providers and community residents, especially vulnerable target populations. Systematic examination is needed of coalition organizational structures and processes likely to explain effectiveness, as well as of community contextual factors that might hinder or help the coalition accomplish its goals. Examining the types of community issues targeted, the implementation strategies employed, and the resources required can inform decision making about the use of community coalition models.
Objectives
To assess effects of community coalition‐driven interventions in improving health status or reducing health disparities among racial and ethnic minority populations.
Methods
Criteria for considering studies for this review
Types of studies
We included cluster‐randomized controlled trials, randomized controlled trials, quasi‐experimental designs (e.g. propensity score matching, regression discontinuity designs), controlled before‐after studies, interrupted time series studies (with at least three data points before and three after the intervention), and prospective controlled cohort studies.
When review authors noted that studies referred to a process evaluation or another methodologic detail that is published elsewhere in a separate paper, we obtained these additional papers and considered them as part of the included studies.
Types of participants
Community‐level coalitions are the focus of this review; we did not include state‐wide or national coalitions, which differ in purpose and stakeholder characteristics. Communities are aggregates of people who form a loosely cohesive association within a residential space or district; they represent a subpopulation of a larger unit such as a city, or they can be indigenous and ethnic groups that may not reside in immediate residential proximity but possess a common community identity. We have examined minority racial and ethnic communities, including indigenous people, who participate in community coalitions, and for whom coalitions are targeting health promotion programs and policies.
We have included only studies of community coalitions with at least one racial or ethnic minority group representing the target population, and at least two community public or private organizations.
Types of interventions
Interventions include locally recruited coalitions in racial and ethnic minority communities in partnership with social and health service agencies, schools, businesses, etc., whose role is to leverage community resources and implement community‐based programs and policies that promote health or prevent health disparities. Interventions may involve strategies that target neighborhood social conditions influencing health outcomes (e.g. access to healthy food, safe neighborhood environments) or community risk behaviors (e.g. smoking). We have included comparisons with communities that do not employ a community coalition model to promote health, as well as comparisons with communities that do not provide an intervention or use other strategies.
Types of outcome measures
We have included studies that report a health outcome and describe other determinants of health such as changes in neighborhood conditions (e.g. level of violence) or policies (e.g. access to services) implemented to promote community health improvement.
Primary outcomes
Major outcomes of interest are direct measures of health status and lifestyle factors when evidence indicates that these have an effect on those direct measures. Studies are included when data on mortality (e.g. all‐cause death within period of study, probability of survival) and morbidity (e.g. quality of life measures, incidence rates, measures of symptoms and functionality) and health behavior change measures show that interventions directly affected levels of health risk or health protection (e.g. measures of physical activity, smoking status, alcohol consumption, dietary change). Of particular interest are measures of change in health disparities among predominant populations and ethnic and racial minority populations.
Secondary outcomes
Secondary outcomes that are recorded include changes in neighborhood conditions or policies introduced to promote community health improvement (e.g. a policy establishing a farmers' market to provide access to fresh produce, a school policy opening sports fields for local resident use during non‐school periods).
We have used qualitative data and process evaluations embedded in the included studies to capture information on community context and coalition structures and mechanisms.
We have used cost data embedded in the studies to assess cost and resource use.
We have captured adverse outcomes reported qualitatively or quantitatively at community, organizational, and individual levels.
Search methods for identification of studies
We developed search strategies in conjunction with the Cochrane Public Health Group Study Search Co‐ordinator that include terms used to identify appropriate global evaluation studies, for which definitions and designations may differ. We chose the literature search period start date of 1990 because a marked rise in local community coalitions for health promotion and disease prevention began in the early 1990s (Butterfoss 2007). Furthermore, during that period, "multi‐sector" coalition models (vs a single grass‐roots advocacy group) became the predominant strategy for private foundations and government organizations that saw pooling of resources and mobilizing of talents across diverse groups as inherent to a broad‐based, social‐ecologic approach to community change (Butterfoss 2007).
Electronic searches
We provided a summary of search strategies in Appendix 1.
Health
MEDLINE, January 1990 through March 31, 2014.
EMBASE, January 1990 through March 31, 2014.
Cumulative Index to Nursing and Allied Health Literature (CINAHL), January 1990 through March 31, 2014.
Cochrane Central Register of Controlled Trials (CENTRAL), January 1990 through March 31, 2014.
PsycINFO, January 1990 through March 31, 2014.
Social science
Social Science Citation Index, January 1990 through March 31, 2014.
Grey literature
Dissertation Abstracts, January 1990 through March 31, 2014.
System for Information on Grey Literature in Europe (SIGLE), January 1990 through September 30, 2013 (we were unable to access the database for the March 2014 update).
Developing countries
Global Health Library, January 1990 through March 31, 2014.
Searching other resources
We screened reference lists of all included studies and review articles for relevant titles.
We handsearched the following four journals for the period 2000 to January 2012: Health Promotion International, Health Promotion Practice, Health Education Research, Preventive Medicine.
Data collection and analysis
Selection of studies
A research librarian (SS) conducted electronic searches of the bibliographic databases. Review authors (LA and KA) removed duplicate studies across databases and undertook initial screening of titles and abstracts to remove those clearly outside the scope of the review. We retrieved in full text papers potentially meeting inclusion criteria based on content of titles and abstracts and linked multiple publications and reports on the same study. Two independent review authors (of LA, KA, CS, and JB) screened all full‐text papers to determine eligibility for inclusion and consulted a third review author when consensus was needed to resolve disagreements. We recorded reasons for study exclusion and translated for screening purposes articles published in languages other than English. We used Reference Manager bibliographic software to manage citation records.
Data extraction and management
We extracted data from all studies that met inclusion criteria. Two review authors (of LA, KA, CS, LK, and JB) extracted study characteristics of eligible papers, details of the community coalition, details of the interventions, and outcomes data and resolved disagreements through discussion.
Review authors (LA, KA, and CS) pilot‐tested a Community Coalitions Data Extraction Form. We used this extraction form (prepared in Excel format) to collect information on citation tracking and classification, community coalition characteristics, setting and context, intervention characteristics and strategies, target population sociodemographic characteristics, outcome ascertainment characteristics, analytic methods, and results. We examined patterns within coalition structures and processes, intervention strategies, and types of outcomes for aggregation of similar groups for synthesis and interpretation. We used the program logic model presented in Figure 1 to facilitate categorization of studies.
We entered data into Review Manager for storage and analysis (RevMan 2011). When health outcomes were reported, we also collected information on changes in neighborhood structures and policies that occurred to promote change in those health outcomes. When studies reported more than one end point per outcome, we recorded all for synthesis at a similar follow‐up period across similar studies. When studies reported multiple measures of the same or similar outcomes, we recorded these.
We included qualitative data and process evaluations embedded in the primary study or related reports to capture information on community context and coalition recruitment and structures, and on decision‐making mechanisms. We collected information on country and regional influences when reported, so we could consider location when interpreting study findings. We coded data on costs and use of resources. We captured adverse outcomes reported qualitatively or quantitatively. We contacted authors of primary studies when information was missing or clarification was needed.
Assessment of risk of bias in included studies
Two review authors (LA, KA) assessed studies meeting inclusion criteria for risk of bias and resolved disagreements through discussion. We used the Cochrane Collaboration "Risk of bias" tool (Cochrane 2008) for randomized controlled trials, and the Effective Practice and Organization of Care (EPOC 2015) "Risk of bias" tool for controlled before‐after studies and for interrupted time series studies. For randomized controlled trials, controlled before‐after studies, and prospectively controlled cohort studies, we critically assessed potential for bias for random sequence generation, allocation concealment, comparability of outcome measurements at baseline, comparability of other characteristics at baseline, completeness of outcome data, blinding of participants and personnel, blinding of outcome assessment, protection against contamination, and selective reporting. For interrupted time series, we performed assessments for independence of interventions from other changes, point of analysis at point of intervention, intervention effects on data collection, blinding of outcome assessment, completeness of outcome data, and selective reporting. In each area, we appraised risk of bias as “high,” “low,” or “unclear.” We summarized risk of bias for each study and considered this information when interpreting review conclusions.
Measures of treatment effect
We used Comprehensive Meta‐Analysis 2.2 (CMA) software to calculate standardized effect sizes for health outcomes because it allowed greater flexibility in deriving and displaying forest plots; this was useful given that we do not present formal meta‐analyses of pooled effects. We reported outcomes both as differences and as ratios. We calculated a standardized mean difference effect size using CMA when outcomes were reported with sufficient data to compute the statistic. When outcome data were dichotomous (i.e. odds ratios), we transfomed them into standardized mean differences in CMA according to the method proposed by Hasselblad 1995.
Unit of analysis issues
In cluster‐randomized studies, we examined whether level of randomization was taken into account if individual participant data were analyzed, and adjusted accordingly. When cross‐over designs were used, we gathered data from the first treatment period. When multiple treatment groups were compared with a single control, we selected the most relevant treatment condition if the other groups were not applicable to the review question. When repeated measurements occurred, we used only one measurement in a single analysis.
Dealing with missing data
When important data were missing from the published report such as analytic methods used, baseline measurements, accounting for missing participants, or statistics such as variance measures, we attempted to contact the study authors via email. When we were unable to obtain missing data, we indicated this in the narrative description of that study. We considered the quantity of missing data in the overall review and discussed the potential impact on our findings and conclusions.
Assessment of heterogeneity
We did not conduct meta‐analysis to pool effects across all studies because studies included in the systematic review were variable with respect to types of participants, types of interventions, and types of outcomes. We used a random‐effects model to compute standardized mean difference effect size as the common statistic for comparison purposes. Moderate to substantial heterogeneity (I2 > 50%) in results precluded pooling of effects across studies.
Assessment of reporting biases
We used a funnel plot to investigate the impact of publication bias.
Data synthesis
We observed heterogeneity within the collection of studies on community coalitions with respect to the population targeted, the intervention strategy employed, and the health outcome targeted. We grouped studies with respect to study methods, interventions, and outcomes. When data derived from similar methods reported on similar outcomes following similar interventions, we originally planned to pool effect sizes using CMA software. However, statistical synthesis of data was not appropriate, and we synthesized study information narratively.
Differences in interventions and outcomes across the body of community coalition studies precluded preparation of a summary of results of the data synthesis using a GRADE (Grades of Recommendation, Assessment, Development, and Evaluation) approach, as suggested in Chapter 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Subgroup analysis and investigation of heterogeneity
Data were insufficient to allow subgroup analyses to examine the influence of (1) study design, (2) targeted health condition, (3) single‐setting and single‐level versus multi‐setting and multi‐level intervention strategies, (4) coalition organizational structure, and (5) community socioeconomic contextual factors, as was originally planned.
Sensitivity analysis
We did not perform sensitivity analyses comparing the results of two or more meta‐analyses calculated using different assumptions of acceptable study quality, as marked heterogeneity prohibited pooling of outcomes.
Results
Description of studies
Results of the search
Although our review had strict inclusion criteria regarding the definition of a local community coalition, with racial and ethnic minority community members represented as one of the collaborating partners, our searches cast a wide net on the range of interventions that might be expected to reduce health disparities. Literature searches identified 14,186 unique records for the period January 1, 1990, to September 27, 2011, and search updates of the same databases yielded an additional 10,655 unique records for the period September 27, 2011, to March 31, 2014. Handsearched journals and reference lists yielded 199 additional records, for a total of 25,040 unduplicated titles and abstracts for screening. Figure 2 provides the flow diagram for the literature searches. After screening titles and abstracts for clearly irrelevant records, we excluded 24,444 studies. We screened the remaining 596 articles to determine if a community coalition was present; we found that 239 were not community coalition studies and excluded them. Of 357 articles that reported on a community coalition intervention study, we identified 146 articles representing 58 unique community coalition‐driven interventions. These studies described coalitions consisting of racial and ethnic minority community organizations and community members for whom the intervention was intended, and at least two community public or private organizations, which were comparative in evaluation design (i.e. randomized or quasi‐randomized controlled trials, controlled before‐after studies, or an interrupted times series). We identified one ongoing study at the protocol stage. We excluded 187 studies because they used study designs that were not eligible (e.g. case study, single group before‐after), and 36 because no racial or ethnic minority population was represented by a community coalition.
2.
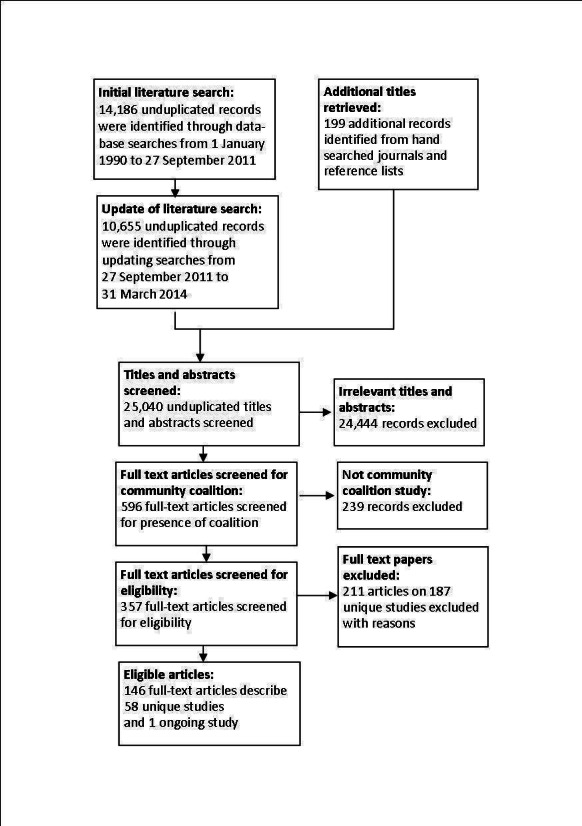
Literature flow diagram.
Included studies
The 58 studies included in the review differed in characteristics of coalitions formed and characteristics of interventions implemented (i.e. population, intervention, comparison, and outcomes), and in several other factors. This section describes these differences. Detailed information on each study is presented in the Characteristics of included studies table.
Characteristics of study methods
Thirty‐one studies used a controlled before‐after evaluation design (see cite sheet). Nineteen studies reported that they used a randomized design; of these, 11 were randomized controlled trials and eight used a cluster‐randomized design. Of the remaining studies, seven were controlled prospective cohort trials and one used a time series design. We assessed outcomes of the 58 studies by reviewing responses to questionnaires, surveys, and records for 133,852 individuals.
Publication dates for the primary studies spanned a 20‐year period from 1994 to 2014. More studies were published in the latter decade, with 41 published between 2004 and 2013, compared with 16 published between 1994 and 2003. One study was published in 2014, but the search period ended March 31, 2014.
The country of origin in 52 studies was the United States. Two studies were conducted in Australia (Kelaher 2009; Kelaher 2010), two in Canada (Dedobbeleer 2001; Paradis 2005), two in England (Melhuish 2010; Stafford 2008), and two in the Netherlands (Abbema 2004; Kloek 2006).
Characteristics of participants
Studies included in this review targeted a wide array of racial and ethnic minorities. Thirty studies included individuals who were African American, or individuals of African or Afro‐Caribbean descent (Blumenthal 2010; Brownson 1996; Brownson 2004; Burhansstipanov 2010; Cardarelli 2011; Cheadle 2001; Darrow 2011; Davidson 1994; Fisher 1998; Fisher 2004; Fuller 2007; Holder 2000; Kim 2008; Kronish 2014; Kruger 2007; Larson 2009; Levine 2003; Liao 2010b; Paine‐Andrews 1999; Parikh 2010; Parker 2008; Plescia 2008; Rothman 1999; Schorling 1997; Spencer 2011; Treno 2007; Voorhees 1996; Wagner 2000a; Wells 2013; Wilson 2008). Eighteen studies included Latino and/or Latina individuals (Burhansstipanov 2010; Darrow 2011; Davidson 1994; Holder 2000; Koniak‐Griffin 2008; Kronish 2014; Liao 2010b; Merriam 2009; Paine‐Andrews 1999; Parikh 2010; Parker 2008; Rhodes 2009; Rhodes 2011; Spencer 2011; Thompson 2006; Thompson 2008; Treno 2007; Wells 2013). Nine studies targeted individuals who were Asian or Pacific Islanders, including Hawaiian (Gotay 2000) and Hmong (Kagawa‐Singer 2009), and communities with large populations of Asian Americans (Liao 2010a; Liao 2010b), Vietnamese or Chinese‐Vietnamese (McPhee 2003; Nguyen 2006; Nguyen 2009), Samoans (Mishra 2007), and Koreans (Moskowitz 2007). Six studies targeted Native Americans or indigenous populations (Brown 2013; Burhansstipanov 2010; Kelaher 2009; Liao 2010b; Paradis 2005; Wagner 2000b). A single study included individuals of Middle Eastern descent among participants from other racial and ethnic minorities (Dedobbeleer 2001).
Residents of geographic areas defined as socioeconomically disadvantaged or ethnically diverse were the target of 10 studies (Abbema 2004; Clark 2013; Kelaher 2009; Kelaher 2010; Kloek 2006; Krieger 2000; Krieger 2005; Melhuish 2010; Saxe 2006; Stafford 2008). A single study (Thompson 2008) targeted migrant workers at risk of agricultural pesticide exposure.
In terms of age, most studies targeted adults (Blumenthal 2010; Brownson 1996; Brownson 2004; Burhansstipanov 2010; Cardarelli 2011; Darrow 2011; Fisher 1998; Gotay 2000; Holder 2000; Kagawa‐Singer 2009; Kelaher 2010; Kim 2008; Kloek 2006; Larson 2009; Levine 2003; Liao 2010a; Liao 2010b; McPhee 2003; Merriam 2009; Mishra 2007; Moskowitz 2007; Nguyen 2006; Nguyen 2009; Parikh 2010; Plescia 2008; Rhodes 2009; Rhodes 2011; Saxe 2006; Schorling 1997; Spencer 2011; Thompson 2006; Thompson 2008; Voorhees 1996; Wagner 2000a; Wilson 2008), six studies targeted adolescents (Brown 2013; Cheadle 2001; Dedobbeleer 2001; Koniak‐Griffin 2008; Paine‐Andrews 1999; Wagner 2000b), five studies targeted young children (Fisher 2004; Melhuish 2010; Paradis 2005; Rothman 1999; Thompson 2008), four studies included children and adolescent youth (Clark 2013; Davidson 1994; Krieger 2005; Parker 2008), and two studies targeted infants (Kelaher 2009; Kruger 2007). One study (Krieger 2000) targeted senior citizens, and three studies targeted the general public (Abbema 2004; Treno 2007; Wells 2013).
Nine studies targeted women (Burhansstipanov 2010; Cardarelli 2011; Gotay 2000; Kagawa‐Singer 2009; Mishra 2007; Moskowitz 2007; Nguyen 2006; Nguyen 2009; Wilson 2008). All but one study targeting women focused on screening and prevention of breast and/or cervical cancer. Koniak‐Griffin 2008 focused on human immunodeficiency virus (HIV) prevention for adolescent Latina mothers and their male partners. Two studies targeted males (Rhodes 2009; Rhodes 2011).
Nine studies included individuals according to their medical history or health risk, including children and youth with asthma (Clark 2013), minority populations with high HIV incidence (Darrow 2011), youth with asthma (Fisher 2004; Krieger 2005; Parker 2008), intravenous drug users (Fuller 2007), stroke survivors (Kronish 2014), clinic patients with hypertension (Levine 2003), and adults with pre‐diabetes (Parikh 2010).
Most studies targeted individuals in urban settings (Abbema 2004; Blumenthal 2010; Burhansstipanov 2010; Cardarelli 2011; Cheadle 2001; Clark 2013; Darrow 2011; Fisher 1998; Fisher 2004; Fuller 2007; Gotay 2000; Kagawa‐Singer 2009; Kelaher 2009; Kelaher 2010; Kloek 2006; Koniak‐Griffin 2008; Krieger 2000; Krieger 2005; Kronish 2014; Kruger 2007; Levine 2003; Liao 2010a; Liao 2010b; Merriam 2009; Mishra 2007; Moskowitz 2007; Plescia 2008; Rothman 1999; Saxe 2006; Spencer 2011; Stafford 2008; Treno 2007; Voorhees 1996; Wagner 2000a; Wells 2013; Wilson 2008). Eight studies included individuals in rural settings (Brown 2013; Brownson 1996; Brownson 2004; Kim 2008; Paradis 2005; Schorling 1997; Thompson 2006; Wagner 2000b). Participants in one study were suburban (Holder 2000) and participants in six studies were from mixed urban/suburban/rural settings (Kelaher 2009; Melhuish 2010; Paine‐Andrews 1999; Rhodes 2009; Rhodes 2011; Thompson 2008).
Characteristics of coalitions
This review includes studies of community coalitions with at least one racial or ethnic minority group representing the target population, and at least two community public or private organizations. On the basis of study author description, community coalitions were coded as one of three types: “grass roots” partnerships of predominantly community‐based organizations; academic institution partnerships with communities; or public health agency partnerships with predominantly public agencies.
Academic/community partnership was the most prevalent coalition typology and was reported in 34 studies (Blumenthal 2010; Brown 2013; Brownson 2004; Cardarelli 2011; Cheadle 2001; Clark 2013; Darrow 2011; Fisher 1998; Fisher 2004; Fuller 2007; Gotay 2000; Holder 2000; Kagawa‐Singer 2009; Kim 2008; Koniak‐Griffin 2008; Krieger 2000; Krieger 2005; Kronish 2014; Levine 2003; Merriam 2009; Mishra 2007; Moskowitz 2007; Nguyen 2006; Nguyen 2009; Parikh 2010; Parker 2008; Rothman 1999; Schorling 1997; Spencer 2011; Thompson 2008; Voorhees 1996; Wagner 2000a; Wells 2013; Wilson 2008).
Fifteen studies reported a coalition based on a partnership of public health agencies predominantly with other public agencies (Abbema 2004; Brownson 1996; Kelaher 2009; Kelaher 2010; Kloek 2006; Kruger 2007; Larson 2009; Liao 2010a; Liao 2010b; Melhuish 2010, Paradis 2005, Plescia 2008, Rhodes 2009, Rhodes 2011Wagner 2000b).
Nine studies reported a coalition based on partnership of primarily community‐based agencies (Burhansstipanov 2010; Davidson 1994; Dedobbeleer 2001; McPhee 2003; Paine‐Andrews 1999; Saxe 2006; Stafford 2008; Thompson 2006; Treno 2007).
In addition to coalition typology, and on the basis of relevant research literature, authors of this systematic review identified variables of coalition structure and process deemed salient to an understanding of the effectiveness of community coalition‐based interventions. These variables included coalition convenor, type of leadership, number of organizational groups involved, governance structure, staffing, mission statement, by‐laws, goals and objectives, funding, meeting frequency, duration of coalition, and whether or not training for coalition members, a needs assessment process, and/or work groups/subcommittees were included. In addition, review authors coded for problems noted (i.e. problems with funding, leadership, member engagement, conflict resolution, or communication) and for other problems that may impede coalition functioning. With few exceptions, included studies reported these variables in insufficient detail, if at all. A minority of studies reported in very general terms on leadership and staffing, and noted whether needs assessment was conducted. Discussion of coalition member engagement was rarely addressed and usually was limited to reports of training of peer leaders or navigators.
Congruent with the predominant academic partnership coalition typology reported, the lead sector was reported as a university in 18 studies (Brownson 2004; Cardarelli 2011; Cheadle 2001; Darrow 2011; Kim 2008; Koniak‐Griffin 2008; Kronish 2014; Levine 2003; Mishra 2007; Nguyen 2009; Parker 2008; Rhodes 2011; Rothman 1999; Schorling 1997; Thompson 2008; Treno 2007; Voorhees 1996; Wagner 2000a).
A health agency or healthcare provider was the lead sector in 13 studies (Abbema 2004; Brown 2013; Brownson 1996; Gotay 2000; Kloek 2006; Krieger 2000; Krieger 2005; Kruger 2007; Larson 2009; Merriam 2009; Moskowitz 2007; Plescia 2008; Wagner 2000b), and a not‐for‐profit community‐based organization in seven studies (Burhansstipanov 2010; Dedobbeleer 2001; Fisher 1998; Fisher 2004; McPhee 2003; Rhodes 2009; Wells 2013). Community members were identified as the lead sector in two studies (Blumenthal 2010; Thompson 2006), and government human service or social welfare agencies in two studies (Kelaher 2009; Kelaher 2010). Ten studies did not report a lead sector.
The most common type of coalition leadership, reported in 13 studies, was core group/shared leadership (Abbema 2004; Brown 2013; Burhansstipanov 2010; Fisher 1998; Fisher 2004; Krieger 2000; Krieger 2005; Kronish 2014; Nguyen 2006; Nguyen 2009; Paradis 2005; Thompson 2006; Wells 2013). Another 12 studies reported steering committee leadership (Blumenthal 2010; Cardarelli 2011; Cheadle 2001; Dedobbeleer 2001; Gotay 2000; Kelaher 2010; Kim 2008; Larson 2009; Levine 2003; Parker 2008; Treno 2007; Voorhees 1996). Three studies reported leadership by a single person co‐ordinator (Brownson 1996; Darrow 2011; Schorling 1997), and two studies reported leadership by a principal investigator (Brownson 2004; Merriam 2009).
Twenty‐six studies reported a coalition needs assessment process (Abbema 2004; Brownson 1996; Burhansstipanov 2010; Cardarelli 2011; Clark 2013; Darrow 2011; Fuller 2007; Gotay 2000; Kagawa‐Singer 2009; Kelaher 2010; Kim 2008; Kloek 2006; Larson 2009; Levine 2003; Merriam 2009; Moskowitz 2007; Nguyen 2006; Nguyen 2009; Parikh 2010; Parker 2008; Rhodes 2009; Saxe 2006; Schorling 1997; Spencer 2011; Thompson 2006; Voorhees 1996).
Twenty‐seven studies reported use of coalition work groups or subcommittees (Abbema 2004; Brownson 1996; Dedobbeleer 2001; Fisher 1998; Fisher 2004; Fuller 2007; Gotay 2000; Kelaher 2009; Kelaher 2010; Kloek 2006; Krieger 2000; Krieger 2005; Kruger 2007; Larson 2009; Levine 2003; McPhee 2003; Merriam 2009; Nguyen 2006; Nguyen 2009; Parikh 2010; Parker 2008; Rhodes 2009; Treno 2007; Voorhees 1996; Wagner 2000a; Wagner 2000b; Wells 2013).
Thirteen studies reported that training of some kind was provided to coalition members (Brown 2013; Cardarelli 2011; Dedobbeleer 2001; Fisher 2004; Gotay 2000; Holder 2000; Kronish 2014; McPhee 2003; Moskowitz 2007; Plescia 2008; Schorling 1997; Thompson 2006; Voorhees 1996).
The role of theory
Understanding or explaining why or how a coalition‐driven approach may be effective requires explicit consideration of theory and, more important, exploration of conceptual and operational links between the constructs of collaborative community coalition theory and social behavior theory. Missing from the studies included in this review is an explicit theoretical rationale for applying a coalition approach to promoting health in racial and ethnic minorities.
As suggested by the logic model on which this review is based, the theory implied by a community coalition approach to health promotion in disenfranchised or marginalized populations is social‐ecologic theory, which links the social environment to health. Nine studies in this review identified a social‐ecologic theory as the rationale for their intervention approach (Abbema 2004; Blumenthal 2010; Brownson 2004; Larson 2009; Liao 2010a; Liao 2010b; Plescia 2008; Rhodes 2009; Rhodes 2011).
Fifteen studies identified community empowerment, community organization, or community‐sensitive research as their theoretical rationale (Brownson 1996; Burhansstipanov 2010; Cheadle 2001; Kelaher 2010; Kim 2008; Kloek 2006; Mishra 2007; Parker 2008; Rhodes 2009; Rhodes 2011; Schorling 1997; Spencer 2011; Stafford 2008; Thompson 2006; Wells 2013). Eleven studies reported social cognitive theory, or social learning theory, as their rationale (Blumenthal 2010; Brownson 1996; Burhansstipanov 2010; Kagawa‐Singer 2009; Krieger 2000; Krieger 2005; Merriam 2009; Paine‐Andrews 1999; Paradis 2005; Parker 2008; Wilson 2008). Although the latter two theories incorporate social support and imply access to community networks, they do not address other health determinants of the social environment that may be influenced by interagency collaboration.
Nine studies indicated a theory of individual behavior change as their rationale, such as Health Belief (Krieger 2000; Mishra 2007), Stage Theory (Brownson 1996; Kloek 2006; Schorling 1997), Precede‐Proceed (Levine 2003; Moskowitz 2007; Paradis 2005), and Self Efficacy (Parikh 2010). Other theories identified by single studies included Appreciative Inquiry (Kronish 2014), Innovation‐Diffusion (Paine‐Andrews 1999), Gender and Power (Koniak‐Griffin 2008), and Wounded Spirit Healing (Koniak‐Griffin 2008).
Twenty studies, including three of the nine REACH (Racial and Ethnic Approaches to Community Health) studies (Kruger 2007; Nguyen 2006; Nguyen 2009), did not report an underlying theory. The REACH initiative implies a social‐ecologic approach, and four REACH studies identified this as their theoretical rationale (Larson 2009; Liao 2010a; Liao 2010b; Plescia 2008).
Characteristics of interventions
Review authors identified four core community engagement interventions utilized by the coalitions. These interventions represent a diverse set of community programs designed to improve health among racial and ethnic minority populations. Establishment of the coalition was a core component of each intervention, as it established the structure for engaging stakeholders and minority communities in collaborative decision making. Only one study (Wells 2013) explicitly tested the hypothesis that a coalition‐driven intervention provided added value, in terms of improved health status, compared with the same intervention delivered without the coalition model. The remaining studies evaluated a change in health behavior or health status resulting from the intervention strategy.
The 58 included studies evaluated behavioral change (n = 33) or health status change (n = 25) resulting from the intervention strategy. Forty‐eight studies compared the intervention group versus a control group that received no intervention or usual care. Ten studies compared the intervention group with a control group that received an alternative intervention (Blumenthal 2010; Brown 2013; Cardarelli 2011; Koniak‐Griffin 2008; Krieger 2005; Nguyen 2009; Rhodes 2011; Schorling 1997; Voorhees 1996; Wells 2013).
Thirty‐three studies measured change in health behavior as the primary outcome resulting from an intervention. Among these, 11 studies focused on cancer screening behaviors (Blumenthal 2010; Burhansstipanov 2010; Cardarelli 2011; Gotay 2000; Kagawa‐Singer 2009; Mishra 2007; Moskowitz 2007; Nguyen 2006; Nguyen 2009; Thompson 2006; Wilson 2008); eight studies evaluated changes in diet, physical activity, and other risk factors for cardiovascular disease and diabetes (Brown 2013; Brownson 1996; Brownson 2004; Kloek 2006; Larson 2009; Liao 2010b; Plescia 2008; Wagner 2000a); seven examined alcohol, drug, or tobacco use (Dedobbeleer 2001; Fisher 1998; Liao 2010a; Saxe 2006; Schorling 1997; Voorhees 1996; Wagner 2000b); four studies examined human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) risk behaviors (Fuller 2007; Koniak‐Griffin 2008; Rhodes 2009; Rhodes 2011); two evaluated changes in immunization uptake among seniors (Krieger 2000) and children (McPhee 2003); and one study reported on changes in breastfeeding behavior (Kelaher 2009).
Twenty‐five studies measured a change in health status. Four reported changes in asthma symptoms in children (Clark 2013; Fisher 2004; Krieger 2005; Parker 2008); eight reported changes in cardiovascular disease and diabetes risk factors including body weight (Kim 2008; Melhuish 2010; Paradis 2005; Parikh 2010), blood pressure (Kronish 2014; Levine 2003), and glycosylated hemoglobin (HbA1c) (Merriam 2009; Spencer 2011); four reported changes in the quality of neighborhood/community life (Abbema 2004; Cheadle 2001; Kelaher 2010; Stafford 2008); and three reported on injuries (Davidson 1994; Holder 2000; Treno 2007). The following were reported in single studies: depression (Wells 2013), HIV incidence (Darrow 2011), infant mortality rates (Kruger 2007), teen pregnancy rates (Paine‐Andrews 1999), blood lead levels in children (Rothman 1999), and exposure to pesticides (Thompson 2008).
Only a few studies reported secondary outcomes that measured changes in the social‐ecologic domain. Abbema 2004 reported changes in perceived neighborhood safety, Cheadle 2001 measured levels of community mobilization, Gotay 2000 reported changes in social support related to cancer screening norms and behavior, and Stafford 2008 reported changes in level of satisfaction with local neighborhood living conditions. One study (Nguyen 2006) reported a policy change — re‐establishment of a state cancer screening program — as an outcome of the intervention. Most studies that sought to improve the sociocultural environment used behavioral and health status measures to evaluate program impact.
Adverse outcomes resulting from coalition‐driven interventions were not reported. Some problems (e.g. power imbalance between coalition members, unequal access to information, absence of sustainable funding) were noted anecdotally in a few studies (see discussion in "Potential Harms" section).
Four core intervention strategies were selected by the coalitions: (1) broad‐scale community system‐level change (Abbema 2004; Brownson 1996; Brownson 2004; Davidson 1994; Holder 2000; Kelaher 2010; Kloek 2006; Kruger 2007; Larson 2009; Paine‐Andrews 1999; Paradis 2005; Plescia 2008; Stafford 2008; Treno 2007; Wagner 2000a; Wagner 2000b); (2) broad‐scale health or social care system‐level change (Clark 2013; Fuller 2007; Kelaher 2009; McPhee 2003; Melhuish 2010; Saxe 2006; Wells 2013); (3) lay community health outreach workers (Burhansstipanov 2010; Cheadle 2001; Fisher 1998; Fisher 2004; Kagawa‐Singer 2009; Krieger 2005; Moskowitz 2007; Nguyen 2006; Nguyen 2009; Parker 2008; Rhodes 2009; Spencer 2011; Wilson 2008); and (4) group‐based health education and support for targeted groups led by trained peers (Brown 2013; Cardarelli 2011; Gotay 2000; Kim 2008; Kronish 2014; Mishra 2007; Parikh 2010; Rhodes 2011; Schorling 1997; Thompson 2006; Thompson 2008; Voorhees 1996) or by health professionals (Blumenthal 2010; Dedobbeleer 2001; Koniak‐Griffin 2008; Levine 2003; Merriam 2009; Rothman 1999). Mass media was the core strategy in one intervention (Darrow 2011), and a patient reminder system in another (Krieger 2000). We were unable to categorize the core intervention strategy for two studies (Liao 2010a; Liao 2010b) that summarized outcomes from multiple REACH programs (Racial and Ethnic Approaches to Community Health), as each site used distinct coalition‐driven intervention approaches.
Broad‐scale community system‐level change strategies
Studies using broad‐scale community system‐level change strategies aimed to change sociocultural (e.g. public norms, regulatory processes and policies) and physical environments (e.g. housing, green spaces, neighborhood safety) to create supportive community environments for healthy choices and improved quality of life. Broad‐scale and comprehensive community initiatives typically required a longer duration than more specific programmatic efforts. In addition, it was difficult to define all of the components a priori as these programs evolved over time, and system leverage points were identified and acted on at multiple levels in the complex community system. It is not surprising that only one cluster‐randomized study was identified (Wagner 2000a), which targeted 80,953 urban Latino residents over a five‐year period to improve dietary intake for chronic disease prevention. Program components included improving grocery store options and providing community health screenings, nutrition classes, and school‐based nutrition education.
The remaining 15 studies that used broad‐scale community system‐level approaches included 11 controlled before‐after designs (Abbema 2004; Brownson 1996; Brownson 2004; Kelaher 2010; Kloek 2006; Kruger 2007; Larson 2009; Paine‐Andrews 1999; Paradis 2005; Plescia 2008), three interrupted time series (Davidson 1994; Holder 2000; Treno 2007), and one controlled prospective cohort study (Stafford 2008). Four of these consisted of multi‐component and multi‐level efforts to improve diet and physical activity among adults (Brownson 1996; Brownson 2004; Kloek 2006) and children (Paradis 2005); four studies aimed to improve resources for healthy behavior (e.g. places for recreation) and quality of community life (e.g. satisfaction with neighborhood) in socioeconomically deprived areas (Abbema 2004; Kelaher 2009; Plescia 2008; Stafford 2008); three aimed to reduce alcohol and drug risk behaviors among adults by raising awareness, altering beverage service practices in taverns, and altering law enforcement policies and practices (Holder 2000; Treno 2007), and, among Native American youth, through school‐based education, peer counseling, community education, and improved law enforcement (Wagner 2000b). The average duration of the 15 quasi‐experimental studies was 50 months.
Broad‐scale health or social care system‐level change strategies
Studies using broad‐scale health or social care system‐level strategies targeted the co‐ordinated behavior of multiple staff within a health or social care system; changed policies, procedures, and technologies to improve quality of care; and increased organizational and delivery system capacity and infrastructure to improve health outcomes among the populations served. Investigators applied complex interventions that altered the standard operating procedures of interrelated agencies in the system and changed practice protocols. We identified one cluster‐randomized controlled trial (Wells 2013) that implemented depression care quality improvement in a network of mental health and health and social care systems (primary care, substance abuse, social services, and homeless services) in the ethnically diverse South Los Angeles and Hollywood metropolitan area. Many non‐healthcare agencies were accessed by residents who also had depression, and the study aimed to establish co‐ordinated depression care across this network. Investigators compared a depression quality improvement program delivered in two ways: a coalition‐driven "community engagement" model, and a "resource support for agencies" approach without community engagement in mental health outcomes. The intervention occurred over a two‐year period and included train‐the‐trainer for quality improvement in depression care, cognitive‐behavioral therapy, and medication management, as well as development of service networks across diverse agencies.
The remaining six studies that examined broad‐scale health and social care system‐level change consisted of five controlled before‐after studies (Clark 2013; Fuller 2007; Kelaher 2009; McPhee 2003; Saxe 2006) and a prospective controlled cohort study (Melhuish 2010). Two of these studies were aimed at improving the health and development of young children in deprived areas in England through the Sure Start community‐based initiative (Melhuish 2010), and in Australia through the Best Start community initiative (Kelaher 2009). Interventions were implemented across hundreds of communities, with each program guided by a local coalition or partnership that included parents, local government, health series, education services, family support services, and community organizations such as those representing ethnic minority populations. System change strategies encompassed a range of improvements in the quality and co‐ordination of child and family support services including home visiting and outreach, childcare services, primary health care, and early childhood education and development programs. Another study, Allies Against Asthma, was a controlled before‐after evaluation of systems of asthma care for youth and adolescents in lower‐income neighborhoods of several cities (Clark 2013). Community coalitions were formed in each community with the aim of changing policies and practices regarding asthma management in minority youth by establishing asthma registries; improving reimbursement and financial incentives; improving care co‐ordination and case management; providing clinical quality improvements through provider education and use of standardized referrals, protocol, and action plans; and implementing changes in schools, childcare centers, and recreational facilities to improve asthma management. The remaining three controlled before‐after studies targeted change in systems of health and social care. One was a multi‐level intervention in Harlem, New York, that sought to increase sterile syringe access through a new policy allowing non‐prescription syringe sales in pharmacies (Fuller 2007). One study reported on the Fighting Back community initiatives implemented in several US cities, whereby multi‐sector coalitions of grass roots leaders and business and political leaders implemented a range of system level changes in prevention, treatment, and aftercare for substance abuse (Saxe 2006). One study focused on improving awareness and uptake of hepatitis B immunization for Vietnamese‐American children through community awareness and healthcare provider system changes (McPhee 2003). The average duration of these six quasi‐experimental studies was 36 months.
Lay community health outreach workers
Hiring lay health outreach workers was a strategy used in 13 studies to increase local community engagement and to reach minority community residents to facilitate health service access, increase knowledge, and promote behavior change in a culturally competent manner. Six of these studies used lay health outreach workers to contact community members, provide cancer prevention information, and facilitate access to screening services; two were randomized studies (Nguyen 2009; Wilson 2008), and four used a quasi‐experimental design (Burhansstipanov 2010; Kagawa‐Singer 2009; Moskowitz 2007; Nguyen 2006). Two randomized trials (Parker 2008; Krieger 2005) and one prospective controlled cohort study (Fisher 2004) employed lay community health workers to contact households of children with asthma and provide education, supplies, and support to reduce indoor asthma triggers. One cluster‐randomized trial paid local community organizers to raise community awareness of youth risk behaviors and to provide education about risk reduction strategies through community health fairs and other outreach venues (Cheadle 2001). One randomized controlled trial used community health workers for home visits to diagnose diabetes and teach diabetes self management (Spencer 2011). Migrant farm workers and their children at risk of pesticide exposure were the focus of a randomized trial in which "health promotoras" provided community outreach and education on abating pesticide exposure risk (Thompson 2008). One cohort study trained lay health advisors from Latino men’s soccer teams to provide HIV/AIDS prevention outreach to recent migrants in Spanish‐speaking soccer leagues (Rhodes 2009). The average duration of the 13 lay community health outreach worker interventions was 30 months.
Group‐based health education and support for targeted risk groups led by trained peers or by health professionals
Use of peer health educators to provide group‐based health education classes or workshops to targeted risk groups was the intervention strategy used in 12 studies. Four randomized studies used peer educators to reduce risk among adults of chronic disease, including cancer (Thompson 2006; Mishra 2007), cardiovascular disease (Kronish 2014), and diabetes (Parikh 2010). One randomized controlled trial trained tribal leaders to offer after‐school education to Native American youth at high risk of diabetes (Brown 2013). Two cohort studies used peer educators in church‐based settings to promote smoking cessation among African Americans (Schorling 1997; Voorhees 1996). Four controlled before‐after studies used peer health educators to increase cancer screening among Latinas (Cardarelli 2011) and Native Hawaiian women (Gotay 2000). One study (Rhodes 2011) used peer educators to reduce HIV risk and increase uptake of HIV screening among Latino men who were recent immigrants. The average duration of these peer educator interventions was five months.
Use of professional health staff to provide group‐based education and social support to targeted risk groups was evaluated in six studies. Three of these studies were randomized trials focused on chronic disease education and risk reduction for stroke survivors (Levine 2003) and people at high risk of diabetes (Merriam 2009) or cancer (Blumenthal 2010). Two studies were controlled before‐after studies evaluating group‐based health education for youth, including HIV/AIDS risk reduction (Koniak‐Griffin 2008) and risk behavior related to alcohol, drug, and tobacco use (Dedobbeleer 2001). One controlled before‐after study provided health education to the parents of children residing in low‐income neighborhoods for reducing the risk of household lead exposure (Rothman 1999). The average duration of group‐based health education programs provided by health professionals was 20 months.
Intervention costs and resources
Among the 58 studies included in this review, only eight provided information on annual costs (Brownson 1996; Clark 2013; Holder 2000; Krieger 2000; Kruger 2007; Saxe 2006; Stafford 2008; Wagner 2000a). Some studies reported the amount of grant funding the project received but provided no information beyond that.
Excluded studies
We excluded 36 studies as they had no racial or ethnic minority population, and 187 because they were not based on eligible study designs (e.g. case study, single group before‐after). See the Characteristics of excluded studies table.
Risk of bias in included studies
Of the 58 studies reporting health outcomes, most (n = 31) were described as controlled before‐after studies. The remaining studies were described as cluster‐randomized controlled trials (n = 9), randomized controlled trials (n = 11), prospectively controlled cohort studies (n = 6), and controlled interrupted time series trials (n = 1). Given the preponderance of non‐randomized study designs included in this review, we utilized the "Risk of bias" tool developed by the Cochrane Effective Practice and Organization of Care Group (EPOC 2015) to develop a checklist for appraising the methodological quality of studies.
We found that none of the randomized studies (n = 20) had uniformly low risk of bias. We found that only one study (Mishra 2007) had no areas with high risk of bias but was appraised as having “unclear” risk for four criteria Of the remaining randomized trials, two had only one area of high risk of bias, and the remaining had two or more areas of high risk of bias.
Among quasi‐experimental studies with a controlled cohort or before‐after design (n = 37), every study had at least one area with high risk of bias, and no study satisfied more than seven of the nine criteria with low risk of bias. Lack of random assignment to intervention groups in these studies meant that none could satisfy the random sequence generation or allocation concealment criteria.
We have summarized risk of bias below by study design. Figure 3 depicts the distribution of risk of bias assessments. Figure 4 presents risk of bias for individual studies.
3.
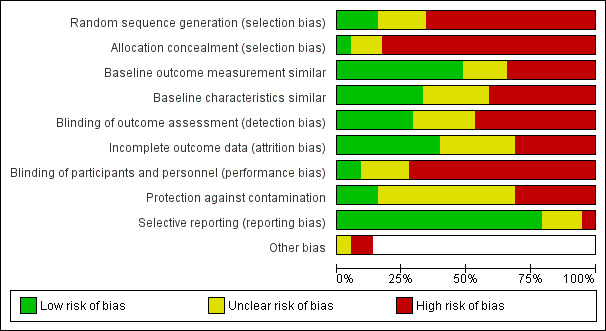
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
4.
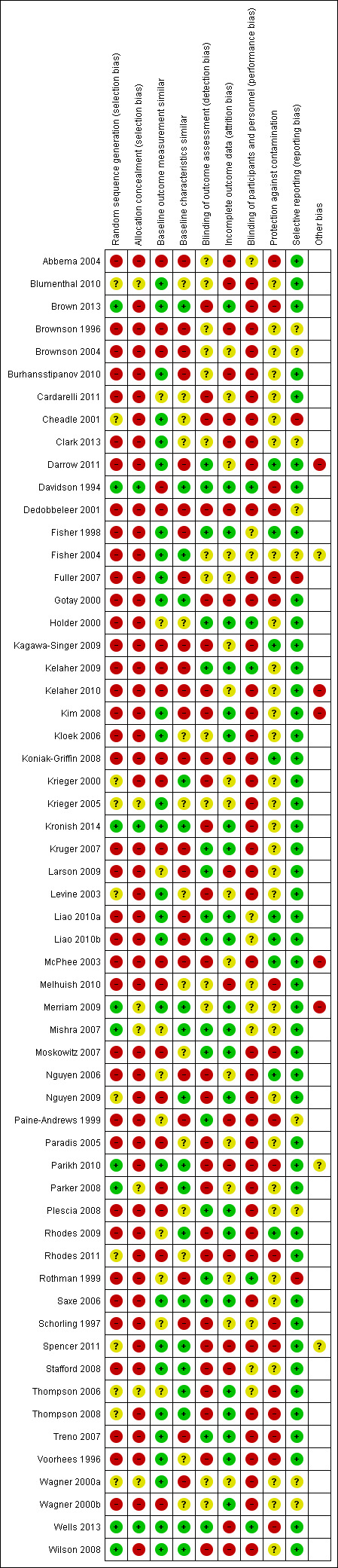
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Randomized studies
We did not completely eliminate selection bias among the randomized trials included in this review. Less than half of these trials (n = 8) described an adequate randomization procedure, and only two (Kronish 2014; Wells 2013) described the procedure in sufficient detail to ensure allocation concealment. Despite randomization, one study (Krieger 2005) had a significant imbalance in baseline measures of one of the outcomes of interest (receipt of influenza immunization); three other studies (Mishra 2007; Parker 2008; Rhodes 2011) had an unclear risk of baseline imbalance in outcome measurements. One randomized trial presented data indicating high risk of baseline differences in participant characteristics between intervention and comparison groups (Wagner 2000a), but baseline imbalances could not be completely ruled out in six studies (Blumenthal 2010; Cheadle 2001; Krieger 2005; Levine 2003; Parker 2008; Rhodes 2011), which were appraised to have unclear risk.
Non‐randomized studies
As a result of lack of random assignment to intervention groups in these studies, none could satisfy the random sequence generation or allocation concealment criteria. Selection bias was a significant risk for most of these studies. We judged both outcome measurements and other participant characteristics as adequately balanced between intervention and control groups at baseline in only four studies (Fisher 2004; Gotay 2000; Saxe 2006; Stafford 2008). However, studies frequently described only a minimal number of baseline participant characteristics, and the comparability of groups was often difficult to assess.
Blinding
Randomized studies
In light of the nature of these community‐based interventions, we judged performance and detection bias to be at high or unclear risk for most of the randomized studies, which reported no blinding of participants or study personnel. We judged only one study as having low risk of both performance and detection bias (Wells 2013), and only two studies as having low or unclear risk in both domains (Merriam 2009; Mishra 2007). The remaining 17 randomized studies were at high risk for one (n = 5) or both domains (n = 12).
Non‐randomized studies
Non‐randomized studies did not attempt to blind participants or personnel, but we characterized three studies as having low risk on this criterion because outcome measurements not susceptible to lack of blinding were used (hospital emergency department records in Holder 2000, maternal child health indicators from state records in Kelaher 2009, blood lead levels in Rothman 1999).
Incomplete outcome data
Randomized studies
We appraised seven studies as having high risk of attrition bias because a high proportion of participants were lost to follow‐up or were missing outcome measurements (Blumenthal 2010; Cheadle 2010; Parikh 2010; Rhodes 2011; Spencer 2011; Wells 2013; Wilson 2008).
Non‐randomized studies
Attrition bias due to incomplete follow‐up or other missing outcome data was a high or unclear risk for most of the cohort studies, with only one out of six studies judged to have low risk for this criterion (Voorhees 1996). Controlled before‐after studies, using independent sampling strategies at baseline and at follow‐up, were immune to individual participant attrition but still often suffered from response rates that declined over time or differed significantly between intervention and control communities.
Selective reporting
Randomized studies
Reporting bias generally was not an issue, although information was insufficient to rule out selective reporting in two studies (Parikh 2010; Wagner 2000a).
Non‐randomized studies
Reporting bias was suspected in only one study (Rothman 1999), for which the cutoff level for a positive outcome was inconsistent between publications.
Other potential sources of bias
Risk of contamination was high or unclear in most of the studies in this review — both randomized and non‐randomized — because of proximate intervention and control groups.
Effects of interventions
See: Table 1
Table 2 presents a summary of results reported in each study.
1. Findings on interventions to reduce health disparities among racial and ethnic minority populations.
| Study ID | Primary outcomes | Secondary outcomes |
| Abbema 2004 |
|
|
| Brown 2013 | Outcomes reported as between‐group difference (Tx‐Ctrl) in mean (SD) and P value, or percent and P value
|
|
| Brownson 1996 |
|
|
| Brownson 2004 |
|
|
| Burhansstipanov 2010 |
Note: 65% of intervention group dropped from study because of change in healthcare coverage law, and if counted as unscreened, the result would be 20% |
|
| Cardarelli 2011 |
|
|
| Cheadle 2001 |
|
|
| Clark 2013 |
|
|
| Darrow 2011 |
|
|
| Davidson 1994 |
|
|
| Dedobbeleer 2001 |
|
|
| Fisher 2004 |
|
|
| Fuller 2007 |
|
|
| Gotay 2000 |
|
|
| Holder 2000 |
|
|
| Kagawa‐Singer 2009 |
|
|
| Kelaher 2009 |
|
|
| Kelaher 2010 |
|
|
| Kim 2008 |
|
|
| Kloek 2006 |
|
|
| Koniak‐Griffin 2008 |
|
|
| Kronish 2014 |
|
|
| Kruger 2007 |
|
|
| Larson 2009 |
|
|
| Levine 2003 |
|
|
| Liao 2010a |
|
|
| Liao 2010b |
|
|
| McPhee 2003 |
|
|
| Melhuish 2010 |
|
|
| Merriam 2009 |
|
|
| Mishra 2007 |
|
|
| Moskowitz 2007 |
|
|
| Nguyen 2006 |
|
|
| Nguyen 2009 |
|
|
| Paine‐Andrews 1999 |
|
|
| Paradis 2005 |
|
|
| Parikh 2010 |
|
|
| Parker 2008 |
|
|
| Plescia 2008 |
|
|
| Rhodes 2009 |
|
|
| Rhodes 2011 |
|
|
| Rothman 1999 |
|
|
| Saxe 2006 |
|
|
| Schorling 1997 |
|
|
| Spencer 2011 |
|
|
| Stafford 2008 |
|
|
| Thompson 2006 |
|
|
| Thompson 2008 |
|
|
| Treno 2007 |
|
|
| Voorhees 1996 |
|
|
| Wagner 2000a |
|
|
| Wells 2013 |
|
|
| Wilson 2008 |
Note: When participants were regrouped according to self reported exposure to breast health messages at salons (10% women at control sites and 37% women at experimental sites), exposure was related to greater likelihood of self reported BSE (aOR 1.6, 95% CI 1.2 to 2.13) and was not significantly related to CBE or mammogram |
|
As described in the earlier Methods section, to present findings in a comparable statistic, we calculated the standardized mean difference (SMD) effect size. We analyzed behavioral change outcomes and health status change outcomes separately, using a random‐effects model. We used only one outcome from each study. We selected the primary outcome as reported by the study author. When more than one primary outcome was reported, we selected the outcome reported most often across studies for comparison purposes. We grouped outcomes by intervention type as follows: community system‐level change, health and social care system‐level change, lay health outreach workers, group‐based health education led by peers, and group health education led by professional staff. We would have pooled effects across each intervention type to yield a summary effect if these studies had examined the same constructs and relationships and had involved a similar methodological design. This was not the case across the diverse body of community coalition‐driven intervention studies, thus we have not presented pooled effects. However, for the purpose of synopsizing data in a manner consistent with our logic model, and in accordance with strategies that emerged from the body of research, we have presented forest plots by intervention strategy. Although heterogeneous in study design and topic content, the forest plots convey information about the impact of each intervention study in a similar metric — the standardized mean difference between intervention and control groups — using symbols whose area is proportionate to the study’s weight in the random‐effects computational method. We did not conduct subgroup analyses because we found contrasting study content in this body of research. Below we discuss study findings by intervention typology and by study design. We considered these community‐based health intervention studies — both randomized and non‐randomized — to be at moderate to high risk of bias.
Effects by intervention typology
Broad‐scale community system‐level change strategies
Seven studies (Brownson 1996; Brownson 2004; Kloek 2006; Larson 2009; Plescia 2008; Wagner 2000a; Wagner 2000b) employed broad‐scale community system‐level change strategies and showed no consistent benefit with respect to behavioral change in the intervention communities as compared with the control communities (Figure 5). Follow‐up evaluations were conducted 24 to 48 months after program implementation. Larson 2009, a controlled before‐after study, reported a significant linear decline in smoking among males only using the Behavioral Risk Factor Survey, a random‐digit dial telephone interview survey. Plescia 2008, a before‐after study, also used data from the Behavioral Risk Factory Survey and reported about a one percentage point decline in smoking prevalence in the intervention community, while the control community saw an increase of about one percentage point. Among studies that reported a change in health status, no consistent benefit was noted in the intervention communities versus the control communities (Figure 6). Of these seven studies (Abbema 2004; Holder 2000; Kelaher 2010; Paine‐Andrews 1999; Paradis 2005; Stafford 2008; Treno 2007), two non‐randomized studies reported significant benefit for intervention communities in terms of reduced alcohol‐related injuries when government data on motor vehicle accidents and injuries were examined. Health outcomes in this group of studies were ascertained 24 to 60 months after program implementation. For all 14 community system‐level change studies, the sample for outcome ascertainment, on average, included 2800 respondents.
5.
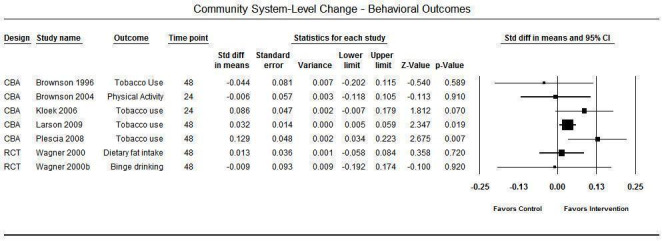
Community system level change — behavioral outcomes.
6.
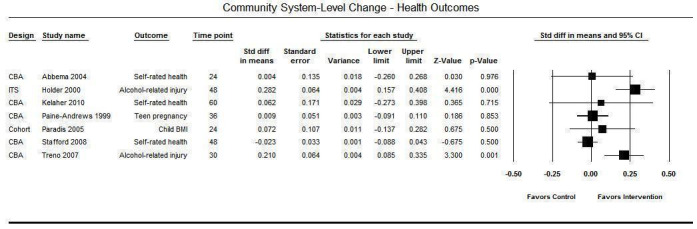
Community system level change — health outcomes.
Broad‐scale health or social care system‐level change strategies
Seven studies employed a health and social care system‐level intervention strategy and reported on resulting behavioral change (Fuller 2007; Kelaher 2009; McPhee 2003; Saxe 2006) (Figure 7) or health status change (Clark 2013; Melhuish 2010; Wells 2013) (Figure 8). This group of programs appeared to consistently result in benefit for the intervention communities across a diverse range of outcomes, including HIV risk behavior, breastfeeding behavior, immunization uptake, acute asthma symptoms, parent‐rated child health status, and mental health quality of life. An exception was Saxe 2006, a controlled before‐after study that measured illicit drug use, which reported a small (0.014 SMD) but non‐significant intervention effect at 48‐month follow‐up. Among this group of studies, Wells 2013 explicitly tested the hypothesis that community coalition‐driven interventions provided added benefit in terms of improved mental health outcomes at six‐month follow‐up, when compared with a similar depression care quality improvement intervention that was not coalition‐led. The remaining six studies measured outcomes 12 to 48 months after program implementation in a sample, on average, of 2000 respondents, except for Kelaher 2009, in which government data on 48,000 maternal‐child health records were analyzed.
7.
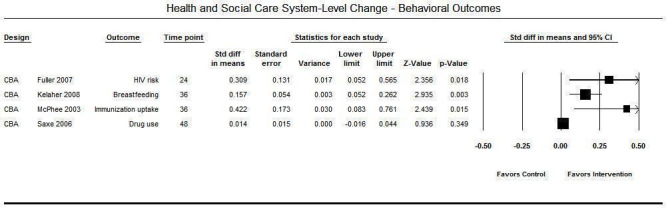
Health and social care system level change — behavioral outcomes.
8.
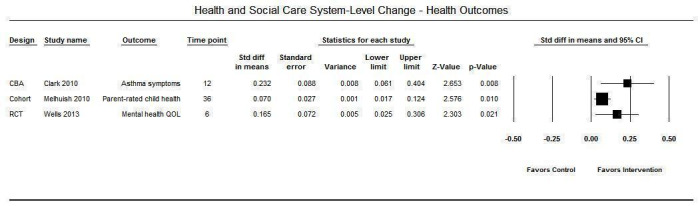
Health and social care system level change — health outcomes.
Lay community health outreach workers
Four studies (Kagawa‐Singer 2009; Nguyen 2006; Nguyen 2009; Wilson 2008) reported behavioral outcomes in studies that used lay community health workers for health education and client advocacy to increase breast and cervical cancer screening (Figure 9). All investigators reported statistically significant changes in receipt of cancer screening among the intervention community, with the exception of Wilson 2008, in which a small positive (0.047 SMD) but not significant result was observed. The remaining study that measured behavioral outcomes reported a significant increase in receipt of HIV screening among the intervention community (Rhodes 2009). Among the five studies that reported health status changes when lay community health workers were used (Figure 10), three assessed changes in asthma symptoms among children and reported mixed results (Fisher 2004; Krieger 2005; Parker 2008). One study about a diabetes control intervention reported improvement in HbA1c levels (Spencer 2011), and another study presented inconclusive findings following a lay health worker intervention provided to reduce pesticide exposure among Latino farm workers and their families (Thompson 2008). Among all 10 lay health worker interventions, outcomes were ascertained between one and 48 months following program implementation among samples that included on average 640 participants.
9.
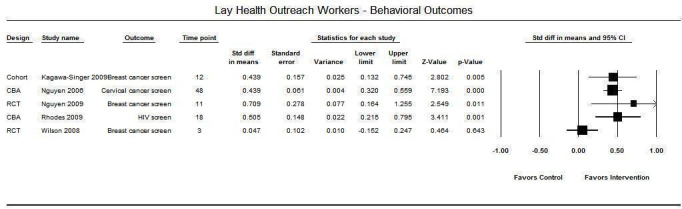
Lay health outreach workers — behavioral outcomes.
10.
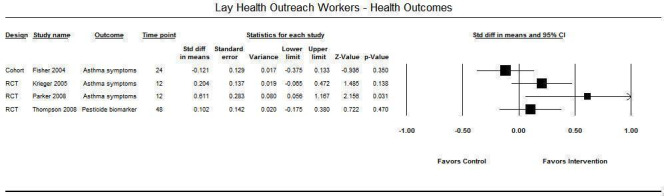
Lay health outreach workers — health outcomes.
Group‐based health education and support for targeted risk groups led by trained peers or by health professionals
The nine studies that used group‐based health education and support led by peers to change behavioral outcomes described mixed results (Figure 11). Four of these studies examined breast cancer screening behaviors, and among these, one RCT (Mishra 2007) reported a small (0.127 SMD) non‐significant effect, one RCT (Thompson 2006) reported no effect, one controlled before‐after study (Cardarelli 2011) reported a very large positive effect (1.293 SMD), and the remaining controlled before‐after study (Gotay 2000) found no significant differences between control and intervention groups. Two studies examined changes in tobacco use after peer‐led, group‐based interventions, and both reported benefit for the intervention group as compared with the control group (Fisher 1998; Schorling 1997). In an RCT evaluating dietary change among Native American youth from a program led by community tribal members trained as lifestyle educators, investigators found little difference in total calories from fat between intervention and control groups (Brown 2013). A cluster‐randomized trial of a peer‐led small group education program initiated to reduce risk of HIV transmission among recent Latino immigrant men reported a marked increase in HIV testing among those receiving the intervention (Rhodes 2011). Among the nine studies that used group‐based health education and support interventions led by peers, investigators ascertained outcomes between three and 36 months following program implementation among sample sizes that included, on average, 640 participants.
11.
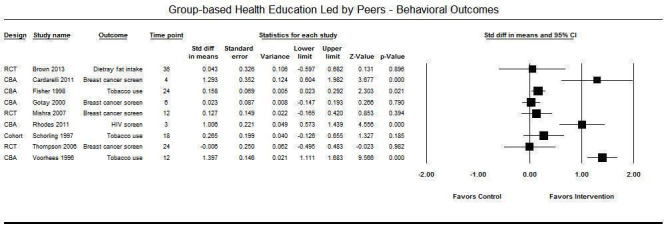
Group‐based health education led by peers — behavioral outcomes.
Two studies evaluated changes in health status following group‐based health education and support led by peers for healthy diet and physical activity (Figure 12). Both studies were conducted among African Americans in church‐based settings. One was an RCT (Parikh 2010) with weight outcomes assessed at 12 months in 72 participants, and the other a controlled before‐after study (Kim 2008) with outcomes reported at two months in 61 participants. Both studies reported moderate to large benefit for the intervention group with respect to change in body weight.
12.
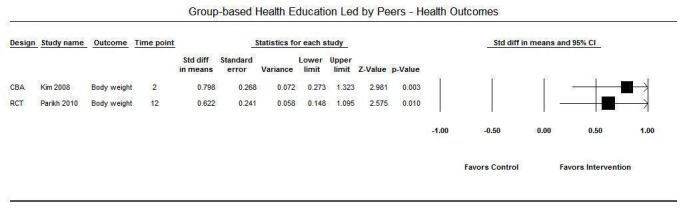
Group‐based health education led by peers — health outcomes.
Among the five studies that evaluated group‐based health education led by professional staff, all favored the intervention group and reported moderate effect sizes (Figure 13Figure 14). These five studies examined different outcomes and included three RCTs that evaluated receipt of colorectal cancer screening (Blumenthal 2010), blood pressure status (Levine 2003), and changes in body weight (Merriam 2009), and two controlled before‐after studies that evaluated alcohol use among youth (Dedobbeleer 2001) and safe sex practices among adolescents (Koniak‐Griffin 2008). Investigators explored outcomes six to 40 months after implementation of the intervention in, on average, 320 participants.
13.
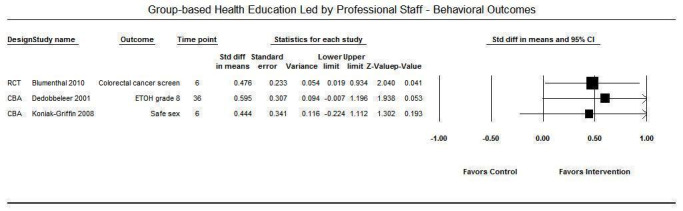
Group‐based health education led by professional staff — behavioral outcomes. (Note: ETOH — alcohol use.)
14.
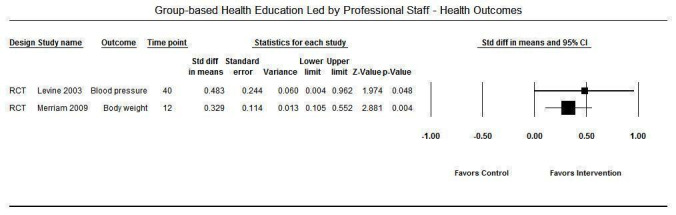
Group‐based health education led by professional staff — health outcomes.
Of the 11 studies in our review that were not presented in the discussion above or in the forest plots depicted in Figures 5 through 14, two did not fall into any of the intervention typologies. These include a study of a client reminder system for African American senior citizens conducted to promote flu and pneumococcal immunization uptake (Krieger 2000), and a study on use of a community mass media strategy to reduce HIV risk among African Americans and Latinos (Darrow 2011). Two studies presented aggregated results from several REACH community studies, each with unique coalitions and intervention strategies, and thus could not be categorized (Liao 2010a; Liao 2010b). One study did not report changes in health behaviors or in health status but measured levels of community mobilization (Cheadle 2001). Data provided in the remaining studies (Burhansstipanov 2010; Davidson 1994; Kronish 2014; Kruger 2007; Moskowitz 2007; Rothman 1999) did not allow computation of SMD effect sizes. Details on outcomes in these studies are presented in Table 2.
Level of measurement
This review attempts to synthesize behavioral and health outcomes collected from individuals who participated in programs (e.g. group‐based health education) and had outcomes assessed by questionnaire or interview or clinical measurement (e.g. HbA1c). It includes behavioral and health outcomes ascertained through population‐based surveys (household and telephone) in areas targeted for intervention or through public databases (e.g. health department records on child blood lead levels) that may be representative samples or universal records but do not signify exposure to an intervention. For coherence and simplicity in presenting effects by intervention typology, we did not stratify by level of measurement. However, because of measurement‐level differences among the studies, effect magnitudes may differ, and residual heterogeneity may exist. It is likely, however, that measurement‐level differences would not influence the direction of effect and thus our conclusions about intervention effectiveness.
Discussion
The community coalition‐driven intervention studies included in this review are heterogeneous in terms of program constructs and relationships evaluated, as well as methods used to do so. Thus, we could not pool individual study data to yield summary effects across intervention typologies. To present data on the impact of each intervention in a similar metric, we computed standardized mean differences between intervention and control groups using a random‐effects model.
Summary of main results
Evaluation of the magnitude and direction of effects across community coalition‐driven intervention typologies revealed that broad community system‐level change strategies (n = 14) produced small and inconsistent results in large samples at 24‐ to 60‐month follow‐up; broad health and social care system‐level approaches (n = 7) produced consistently positive small effects in large samples at six‐ to 48‐month follow‐up; lay community health outreach worker interventions (n = 10) produced fairly consistent positive effects of moderate magnitude in fairly large samples at three‐ to 48‐month follow‐up; group‐based health education led by peers (n = 11) produced inconsistent effects of inconsistent magnitude at three‐ to 36‐month follow‐up; and group‐based health education led by professional staff (n = 5) produced consistently positive effects of moderate magnitude at six‐ to 40‐month follow‐up. These findings provide evidence that community coalition‐driven interventions can benefit minority populations.
Overall completeness and applicability of evidence
In this review, we focused on local community‐based coalitions with representation from a variety of sectors, including the racial and ethnic community that was targeted for intervention. Such coalitions are characterized by shared planning and decision making. Searching the literature for evaluations of coalition‐driven interventions was not a simple task. Terms that might capture studies regarding coalition models are broad and include "partnerships," "alliances," "networks," and "consortia." In addition, health conditions and outcomes of interest included wide‐ranging measures of morbidity, mortality, quality of life, and behaviors empirically linked to health outcomes. As a consequence, we screened a very large quantity of literature to find the studies included in this review. How well we constructed a "representative sample" of coalitions is difficult to determine, as the universe of coalitions is not easily defined, and what gets published may not be representative (Berkowitz 2001). We did note a paucity of grassroots coalition typologies compared with academic‐community partnerships, and we identified few studies from low‐ and middle‐income countries. However, we also noted that the number of articles referring to community coalitions in the past decade was considerably greater than the number in the first decade of our searches, suggesting that our focus on more recent literature (i.e. 1990 forward) was reasonable. However, publication bias in the body of studies was clearly present, as is shown in Figure 15.
15.
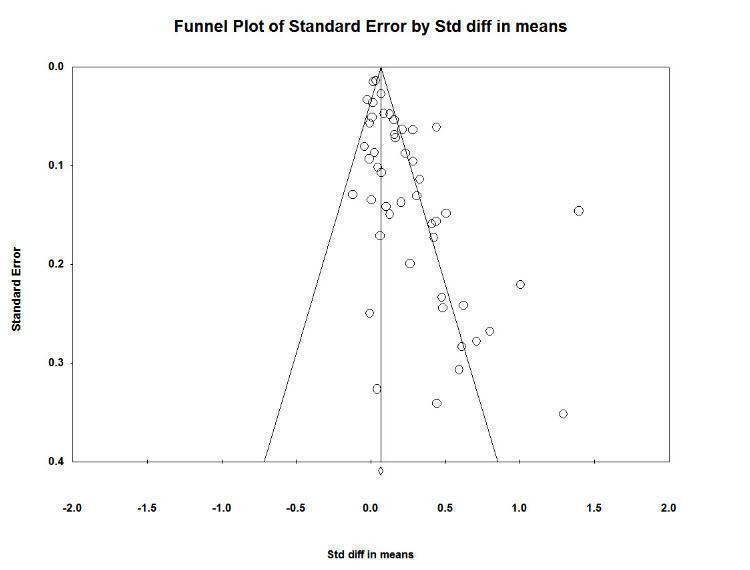
Funnel plot of standard error by standardized difference in means.
A recent systematic review on community engagement to reduce inequalities in health (O'Mara‐Eves 2013) had some common characteristics with our review, in that it examined a broader category of interventions described as “community partnerships, community coalitions, or a community task force.” The O'Mara‐Eves review identified 57 studies in this category, and although our criteria for a community coalition were more specific (i.e. a local community coalition with racial and ethnic minority coalition members involved in decision making), we noted that 16 of those studies were included in both reviews, 24 did not meet inclusion criteria for this review, and 13 were excluded from our review at later stages of screening. Only one study (Dedobbeleer 2001) was found that met our inclusion criteria, but it was missed in our literature searches and was added to our review. This strengthened confidence in the overall completeness of our evidence base.
In assessing applicability of findings, we noted that only high‐income countries are represented, and within high‐income countries the evidence base was restricted to racial and ethnic minority communities. We were unable to describe contextual factors (e.g. coalition organizational contexts, political environments, prevailing priorities) that influence the outcomes of coalition‐driven intervention programs. Financial costs and other resource requirements to support such interventions were not reported, and thus the feasibility of implementing and sustaining community coalition‐driven models is not clear.
Quality of the evidence
Overall, the evidence shows moderate to high risk of bias, particularly in the area of selection bias. This is not surprising in light of the complex and often evolving nature of community‐based health intervention research. In addition, publication bias is a matter of concern, as studies are more likely to be published if effects are large and statistically significant. Our funnel plot suggests that this is the case, as it shows an absence of smaller studies that report null or negative effects.
Potential biases in the review process
We screened a very large quantity of literature to find studies evaluating the effects of community coalition‐driven interventions provided to reduce health disparities in racial and ethnic minority populations. How well we constructed a representative sample of coalitions is difficult to determine.
Agreements and disagreements with other studies or reviews
We found a large body of literature considering the effects of coalitions, community partnerships, and/or collaboration on health promotion and chronic disease outcomes, but we found that until recently, no reviews had examined coalition‐driven interventions specifically targeting racial and ethnic minorities. Congruent with results of this review, findings have been inconsistent and the evidence base is weak as a result of inadequate reporting and insufficient studies with rigorous design.
O'Mara‐Eves 2013 conducted a systematic review, meta‐analysis, and economic analysis of community engagement to reduce inequalities in health in 131 studies. They defined community engagement as “involving communities in decision making and in the planning, design, governance and delivery of services.” They categorized coalitions as a strategy for community engagement. We noted considerable overlap between their review of "community empowerment" interventions and our review of coalition‐led interventions to reduce health disparities. The review authors categorized 57 studies as "community partnerships, community coalitions, community task forces," 17 of which are included in both reviews; 24 of those studies did not meet inclusion criteria for this review, and 13 studies were excluded from this review at later stages of screening. Their overall conclusion was that public health interventions for disadvantaged groups using community engagement strategies are effective in terms of health behaviors, health consequences, self efficacy, and perceived social support across various conditions. Interventions that engage community members exclusively in delivery of the intervention tended to be more effective in improving health behaviors than interventions that empower the community or involve members in the design of the intervention. As with this current review, because of insufficient data and inadequate reporting, review authors were unable to test the hypothesis that community engagement interventions can reduce health inequalities through their impact on social inequalities. Evidence was insufficient to show whether one particular model of community engagement is likely to be more effective than another. Weak evidence from effectiveness and process evaluations suggests that certain implementation factors may affect intervention success. Greater effectiveness of peer/lay‐delivered interventions in health behaviors was noted, as compared with interventions that take a community empowerment approach, or those that involve community members in design of the intervention.
A systematic review by Hayes 2012 examined the effects of interagency collaboration by local health departments and local government agencies on individual health outcomes in several health domains, including mental health, chronic disease management, and lifestyle improvement. This review failed to find evidence that collaborative partnerships made a difference in health outcomes compared with standard services; methodological flaws made it difficult to determine whether limited and inconsistent positive trends observed might be attributable simply to increased funding rather than to collaboration.
In a systematic review commissioned by the US Agency for Health Research and Quality, Viswanathan 2004 examined evidence from community‐based participatory research (CBPR) programs to inform funders about the state of the methodological quality of CBPR efforts and the resources required to promote successful collaborative research. These research authors concluded that although many CBPR studies described strong community‐institutional collaboration, few combined this type of collaboration with robust research methodology. They determined that given the long‐term nature of CBPR efforts, individual and community capacity‐building efforts ultimately may result in positive health outcomes that have little or nothing to do with those targeted in the initial study. This review found no studies that could predict the long‐term and indirect potential benefits of CBPR.
Roussos 2000 reviewed the effects of collaborative partnerships in 34 studies addressing a wide variety of community health concerns. They found 10 studies presenting population‐level outcomes with some improvements that potentially could be attributed to the activities of the partnership. Most of those studies were case studies, and the more methodologically rigorous studies had weak outcomes, contradictory results, or null effects. Nevertheless, the review found evidence of environmental, community, and systems changes.
Litt 2013 studied compositional and stakeholder engagement correlates of group effectiveness in 59 collaboratives promoting physical activity in 22 states. Results from multi‐variate models indicate that engagement in media communication and advocacy was correlated with higher levels of environmental improvement, and groups that frequently solicited endorsement from community leaders and offered testimony in policy or legal hearings reported significantly greater policy change.
Authors' conclusions
Implications for practice.
Evidence found in this review indicates that coalition‐led interventions can connect multi‐sectoral networks of health and human service providers with ethnic and racial minority communities in ways that benefit not only individual health outcomes and behaviors, but also health and social care delivery systems, through collective action and empowerment strategies. This is compelling in light of the fact that after decades of public health interventions to reduce health disparities, little success in closing the gap has been reported (Bleich 2012; Mackenbach 2008; Voelker 2008). For example, the US Agency for Healthcare Research and Quality reported that, compared with whites, significantly more new AIDS cases and pediatric asthma hospitalizations were reported among blacks; American Indian and Alaskan Native women were less likely to receive prenatal care; and Asian women had significantly lower rates of mammography (US AHRQ 2007). Use of a coalition‐driven model may increase the likelihood of adoption of community engagement strategies shown in this review to yield beneficial effects: broad health and social care systems changes that reflect and incorporate community perspectives, use of lay community health workers, group‐based health education and support led by peers, and group‐based health education and support led by professional staff. An array of public health issues, including cancer screening, HIV risk behavior, breastfeeding behavior, immunization uptake, asthma symptoms, parent‐rated child health status, mental health quality of life, diabetes control, blood pressure control, tobacco use, alcohol use in adolescents, and injury prevention, were shown in this review to be amenable to the positive effects of coalition‐driven community engagement strategies. Strategies that engage members of a minority community for whom the intervention is targeted not only may serve as a way to “do public health better” but can be a “source of health for the community” because they allow community members to gain greater control over their health and the conditions that influence it (South 2014).
Potential harms
Social‐ecologic theory suggests that coalition‐driven interventions generate community empowerment and build social capital by expanding and diversifying social networks that lead to greater trust and shared norms. However, qualitative evidence from studies included in this review and from other research suggests that a collaborative community engagement process may have unintended negative consequences, including furthering alienation and disenfranchisement, and inhibition of innovative change.
We coded studies in this review for problems or challenges reported by study authors, and several issues emerged relevant to potential harm. Differences in the fund of knowledge between lay community members and scientific, academic, or professional partners sometimes led to confusion and/or conflict. When these differences were combined with inequity of power in decision making and control of funds, whether real or perceived, a sense of disempowerment resulted. This may have contributed to difficulties noted by some in retaining commitment and engagement by community members. In addition, inadequate funding for implementation and sustainability described by some could lead to stalling or failure of nascent efforts, and may contribute to a community sense of abandonment and alienation.
England’s New Deal for Communities Programme (Lawless 2012), an area‐based regeneration program founded on principles of collaborative community engagement, which included changes in self rated health status, concluded that community engagement produced fewer benefits and proved more problematic than anticipated. That study, which targeted 9800 people within 39 deprived areas between 1998 and 2011, indicated that conflicts related to knowledge gaps and incorrect assumptions by community participants inhibited adoption of evidence‐based strategies and innovative change. It was also noted that as central government priorities shifted over the decade, interest waned and the focus moved to regional strategies — not local strategies — thus marginalizing the importance of local community control.
These potential harms might be mitigated by recruitment practices, by a collaborative governance structure, by training of coalition members that promotes parity, and by assurance of meaningful roles in planning, decision making, implementation, and evaluation of coalition processes.
Implications for research.
Although the evidence in this review provides some support for use of coalition‐driven interventions to improve health and reduce disparities among racial and ethnic minorities, it does not reveal a beneficial effect for broad community system‐level change, it does not provide an explanation for the underlying mechanisms of beneficial effects on health and social care systems, and it does not provide a definitive answer as to whether a coalition‐led intervention adds value to other community engagement intervention strategies. Several factors have contributed to these deficits, with implications for future research.
Coalition structure and processes are integral to the theory‐derived logic model informing this review and to the review process. Reporting of coalition factors was largely inadequate in the studies reviewed, leaving salient questions unexamined: Is one type of coalition structure (community‐based organization partnership, academic‐community partnership, public health agency/government‐community partnership) more effective than others? How is coalition effectiveness impacted by the specific partners included? Who provides leadership? What is the role of professional staff, of volunteers, and of coalition members, if any, in assessment, planning, and implementation? What kind of training, if any, was provided for coalition members? What is the duration and quality of a coalition’s experiences? Is a coalition‐led intervention more likely to choose community engagement strategies? Such details of coalition structure, process, and evaluation would allow analysis to improve our understanding and explanation of the utility of coalition‐driven interventions.
Published community coalition research literature uses an abundance of study designs that are not comparative and/or lack methodological rigor. This review found only one high‐quality study — a cluster‐randomized trial — that specifically evaluated the added value of a community engagement and planning intervention (i.e. a coalition‐led intervention) over and above resource enhancement and community outreach (Wells 2013). That study found added benefit of a coalition‐driven intervention for improved mental health among African Americans. Additional studies of this quality and with this specific focus would allow meaningful meta‐analysis, which was not possible with the studies included in this review. Despite a wide‐ranging search process of international published research, middle‐ and low‐income countries were underrepresented in the search results. In addition to resource limitations, this may represent cultural barriers that inhibit such initiatives. Additional studies from those countries would enhance understanding of the benefits and harms of a community coalition‐led approach for disadvantaged populations.
It is widely acknowledged that methodological challenges may hinder measurement of effects of multi‐level public health interventions embedded in complex systems (Anderson 2013; Barile 2012; Noyes 2013; Schensul 2009; South 2014), and this certainly is relevant in examination of coalition‐driven interventions. The myriad of contextual factors bearing on coalition outcomes is difficult to specify and is heterogeneous across communities. Although it may be true that the evidence in this review supports a null hypothesis for beneficial effects of coalition‐driven interventions on broad community system level change, it may also be true that ability to detect a beneficial effect is hampered by the measures used (or not used) and by inadequate analytic methods. Important questions to be addressed in future research include the following: Are valid measures available for use at the coalition level that can be used across coalitions to measure effectiveness? Do intervention level outcomes (e.g. cancer screening) capture coalition effectiveness? What social indicators, such as community cohesion and resilience, might show linkages between mechanisms of local capacity building and levels of health? The ability to apply multi‐level analytic techniques will be affected by the completeness of data reported in research studies.
Finally, because the research objective of this review was limited to coalition‐driven interventions for racial and ethnic minorities, a large volume of research literature on coalition‐led interventions for general populations was excluded. The comprehensive database generated by the search process includes more than 200 studies of community coalitions excluded from this review because they were not focused on a racial or ethnic community, or because they were not comparative evaluations. It may be true that examination of that body of research would facilitate detection of effects and would provide a better understanding of the underlying mechanisms of coalition‐driven interventions.
Acknowledgements
The review author team is grateful for guidance provided by our Community Coalitions Review Advisory Group — a group of individuals recruited specifically to this project to ensure that the review parameters reflected an international focus. Advisory group members are named here.
Anthony Morgan, National Institute for Health and Clinical Excellence, London, UK.
Hilary Thomson, Medical Research Council, Glasgow, UK.
Louise Potvin, University of Montreal, Montreal, Canada.
Linda Burhansstipanov, Native American Cancer Initiative, Pine, CO, USA.
Shelley Cooper‐Ashford, Center for Multicultural Health, Seattle, WA, USA.
David Hawkins, University of Washington, Seattle, WA, USA.
Mindy Fullilove, Columbia University, New York, NY, USA.
Corey Nunlist, formerly with the Washington State Institute for Public Policy, provided assistance with study retrieval and database management, and contacted study authors for additional information. J Shayne Zhang of the Public Health Review Group provided assistance in handsearching journals.
We also would like to thank our external referees, Professor John Toumbourou of Deakin Univerity and Sari Huttunen, for their insightful comments. In particular, we greatly appreciate the guidance of our Contact Editor, Dr Jonathan Shepherd, from the University of Southampton.
Appendices
Appendix 1. Search strategies
Community Coalitions Search Strategies (2014)
The search strategy was initially developed in Medline, and then adapted for each additional database and website.
========================================================
Database: Medline & Medline in Process (Ebsco interface) covers dates January 1990 ‐ March 31, 2014.
1.
MH medically underserved area OR MH poverty areas OR MH vulnerable populations OR MH minority groups OR MH health status disparities OR MH ethnic groups+ OR MH culture OR MH continental population groups+ OR MH population groups OR MH socioeconomic factors+ OR MH developing countries OR MH refugees OR MH social environment
2.
(health OR social OR disease* OR morbidit* OR mortalit* OR racial OR ethnic) n5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage* OR gradient*)
3.
((disadvant* OR low income or marginali* OR underserved OR under served OR depriv* OR poverty OR impoverish* OR minorit* OR racial OR ethnic*) n5 (population OR group OR communit* OR neighbo#rhood*)) OR (school* n5 community)
4.
(low pay OR low paid OR unemploy* OR depriv* OR financial hardship OR benefit recipient* OR social position* OR social class* OR socioeconomic OR social status OR poverty OR impoverish*) n5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*)
5.
(illitera* OR education* attainment* OR education* level# OR education* status OR low education OR education* achievement* OR school leaver*) n5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*)
6.
(single parent* OR lone parent* OR rural OR refugee* OR immigrant* OR ethnic minorit* OR ethnic group* OR racial group* OR indigenous) n5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*)
7.
(gender OR women) n5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*) OR school n5 children OR pacific islander* OR African American OR Hispanic* OR latino OR latina OR Asian American OR Alaska* native* OR American Indians
8. OR 1‐7 (population)
9.
(communit* OR civic OR neighbo#r* OR public OR village* OR city OR cities OR town OR citizen* OR local people* OR resident# OR stakeholder*) n5 (coalition# OR partnership* OR collaborat* OR participat* OR engage* OR combin* OR share* OR sharing OR union* OR alliance* OR associat* OR federation* OR joint ventur* OR pool* OR resource* OR cooperat* OR champion# OR involv* OR empower* OR panel# OR forum# OR jury OR juries OR council# OR mobilis* OR mobiliz* OR consortium* OR empower* OR network*)
10.
MH health care coalitions OR MH healthy people programs OR MH community health services/og OR MH community networks OR MH community institutional relations OR MH consumer participation+ OR MH community health planning
11.
Cherokee choices OR REACH program* OR "communities that care" OR culturally appropriate OR community develop* OR citizen cent* government* OR "racial and ethnic approaches to community health" OR community n5 coalition*
12. OR 9‐11 ‐ intervention terms
13.
PT randomized controlled trial OR PT controlled clinical trial OR PT clinical trial OR PT comparative study OR PT evaluation studies OR PT support of research OR MH cohort studies+ OR MH intervention studies OR MH program evaluation+ OR MH random allocation OR MH clinical trials as topic+ OR MH single‐blind method OR MH double‐blind method OR MH control groups OR TX randomized OR TX randomised OR TX placebo* OR TX randomly OR TX groups OR TX trial OR TX time series OR TX quasi‐experiment* OR TX pre test OR TX pretest OR TX pre‐intervention OR TX post‐intervention OR TX posttest OR TX post test OR TX "controlled before" OR TX "before and after stud*" OR TX follow‐up assessment OR TX program OR TX programme OR TX secondary anal* OR TX impact evaluation OR TX regression OR TX propensity match* OR TX propensity scor* OR TX matched comparison OR TX discontinuity anal*
OR MH "outcome assessment (health care)*"
14.
(evaluat* OR intervention OR interventional OR treatment* OR educate) AND (control OR controlled OR study OR program* OR comparison OR "before and after" OR comparative OR health promot*)
15.
((intervention* OR process OR program) n8 (evaluat* OR effect* OR outcome*)) OR "racial and ethnic approaches to community health" OR rapid review OR community n5 coalition*
16. S13 OR S14 OR S15 ‐ study design filter
17. S8 AND S12 AND S16
==============================================================================================================
CINAHL (Ebsco interface) January 1990 ‐ March 31, 2014.
1.
MH medically underserved area OR MH orphans and orphanages OR MH poverty areas OR MH special populations OR MH minority groups OR MH ethnic groups+ OR MH culture OR MH immigrants OR MH socioeconomic factors+ OR MH developing countries OR MH refugees OR MH social environment+ OR MH social problems+
2.
(health OR social OR disease* OR morbidit* OR mortalit* OR racial OR ethnic) n5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage* OR gradient*)
3.
((disadvant* OR low income or marginali* OR underserved OR under served OR depriv* OR poverty OR impoverish* OR minorit* OR racial OR ethnic*) n5 (population OR group OR communit* OR neighbo#rhood*)) OR (school* n5 community)
4.
(low pay OR low paid OR unemploy* OR depriv* OR financial hardship OR benefit recipient* OR social position* OR social class* OR socioeconomic OR social status OR poverty OR impoverish*) n5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*)
5.
(illitera* OR education* attainment* OR education* level# OR education* status OR low education OR education* achievement* OR school leaver*) n5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*)
6.
(single parent* OR lone parent* OR rural OR refugee* OR immigrant* OR ethnic minorit* OR ethnic group* OR racial group* OR indigenous) n5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*)
7.
(gender OR women) n5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*) OR school n5 children OR pacific islander* OR African American OR Hispanic* OR latino OR latina OR Asian American OR Alaska* native* OR American Indians
8. OR 1‐7 (population)
9.
(communit* OR civic OR neighbo#r* OR public OR village* OR city OR cities OR town OR citizen* OR local people* OR resident# OR stakeholder*) n5 (coalition# OR partnership* OR collaborat* OR participat* OR engage* OR combin* OR share* OR sharing OR union* OR alliance* OR associat* OR federation* OR joint ventur* OR pool* OR resource* OR cooperat* OR champion# OR involv* OR empower* OR panel# OR forum# OR jury OR juries OR council# OR mobilis* OR mobiliz* OR consortium* OR empower* OR network*)
10.
MH health care coalitions OR MH healthy people programs OR MH community health services/og OR MH community networks OR MH community institutional relations OR MH consumer participation+ OR MH community health planning
11.
Cherokee choices OR REACH program* OR "communities that care" OR culturally appropriate OR community develop* OR citizen cent* government* OR "racial and ethnic approaches to community health" OR community n5 coalition*
12. OR 9‐11 ‐ intervention terms
13.
PT randomized controlled trial OR PT clinical trial OR MH clinical trials OR MH comparative studies OR MH evaluation research OR MH prospective studies+ OR MH experimental studies+ OR MH program evaluation OR MH random sample+ OR MH control group OR TX randomized OR TX randomised OR TX placebo* OR TX randomly OR TX groups OR TX trial OR TX time series OR TX quasi‐experiment* OR TX pre test OR TX pretest OR TX pre‐intervention OR TX post‐intervention OR TX posttest OR TX post test OR TX "controlled before" OR TX "before and after stud*" OR TX follow‐up assessment OR TX program OR TX programme OR TX secondary anal* OR TX impact evaluation OR TX regression OR TX propensity match* OR TX propensity scor* OR TX matched comparison OR TX discontinuity anal*
OR MH "outcomes (health care)+"
14.
(evaluat* OR intervention OR interventional OR treatment* OR educate) AND (control OR controlled OR study OR program* OR comparison OR "before and after" OR comparative OR health promot*)
15.
((intervention* OR process OR program) n8 (evaluat* OR effect* OR outcome*)) OR "racial and ethnic approaches to community health" OR rapid review OR community n5 coalition*
16. S13 OR S14 OR S15 ‐ study design filter
17. S8 AND S12 AND S16
===============================================================================================================
Database: Cochrane Central Register of Controlled Trials (Wiley interface) January 1990 ‐ March 31, 2014.
1.
("medically underserved" OR orphan* OR "poverty area*" OR "special population*" OR "minority group*" OR "ethnic group*" OR immigrant* OR "socioeconomic factor*” OR refugee* OR "social environment" OR "social problem*")
OR
((health OR disease* OR morbidit* OR mortalit* OR racial OR ethnic) AND (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage* OR gradient*))
OR
((disadvantage* OR "low income" OR marginalize* OR marginalise* OR underserved OR "under served" OR depriv* OR poverty OR impoverish* OR minority) AND (population OR group* OR communit* OR neighborhood* OR neighbourhood*))
OR
(("low pay" OR "low paid" OR unemployed OR depriv* OR "financial hardship" OR "benefit recipient" OR "benefit recipients" OR "social position" OR "social class" OR socioeconomic OR "social status" OR poverty OR impoverish*) AND (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*))
OR
((illiterate OR "educational attainment" OR "educational attainments" OR "educational level" OR "educational status" OR "low education" OR "educational achievement" OR "school leaver" OR "school leavers") AND (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*))
OR
(("single parent" OR "lone parent" OR rural OR refugee OR immigrant OR "ethnic minority" OR "ethnic minorities" OR "ethnic group" OR "ethnic groups" OR "racial group" OR "racial groups" OR indigenous OR gender OR women) AND (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*))
2.
((community OR civic OR neighbor* OR neighbour* OR village* OR city OR cities OR town* OR citizen* OR "local people" OR resident* OR stakeholder*) AND (coalition* OR partnership* OR participat* OR engage OR engagement OR combined OR combination OR share OR union OR alliance* OR associate OR federation* OR "joint venture" OR "joint ventures" OR pool OR resource* OR cooperat* OR collaborat* OR champion* OR involve* OR empower* OR panel OR forum OR jury OR council OR mobilize* OR mobilise* OR consortium OR empower* OR network))
3. 1 AND 2
=========================================================================================================================
Database: Dissertation Abstracts (Proquest interface) January 1990 ‐ March 31, 2014.
Proquest Dissertation Abstracts
search strategy
1.
AB,TI("medically underserved" or orphan* or "poverty area*" or "special population*" or "minority group*" or "ethnic group*" or immigrant* or "socioeconomic factors" or refugee* or "social environment" or "social problem*" or "pacific islander*" OR "African American*" OR Hispanic* OR latino* OR latina* OR "Asian American" OR "Alaska* native*" OR "American indian*")
OR
2.
AB,TI(health or disease* or morbidit* or mortalit* or racial or ethnic or unemployed or "benefit recipient*" or poverty or impoverish* OR "social class" OR socioeconomic* OR "social status" or "low paid" or deprived or illiterate or "educational status" or "school leaver*" or "single parent" OR "lone parent" or rural or "ethnic minorit*" or "racial group*" or indigenous or gender or women) AND AB,TI(inequalit* or inequit* or disparit* or equit* or disadvantage* or gradient*)
3. 1 OR 2
4.
AB,TI(community or civic or neighbor* or neighbour* or village or city or cities or town* or citizen* or "local people" or resident or residents or stakeholder*) AND AB,TI(coalition* or partnership* or collaborat* or participat* or engage* or combined or combination or share or union* or alliance* or associat* or federation* or "joint ventur*" or pool or resource* or cooperat* or collaborat* or champion* or involve* or empower* or panel or forum or jury or council* or mobilize* or mobilise* or consortium or network*)
5.
3 AND 4
6.
AB,TI(randomized or randomised or "controlled trial*" or "clinical trial*" or "comparative stud*" or "evaluation stud*" or "support of research" or "cohort stud*" or "intervention stud*" or "program evaluation*" or "random allocation" or "single‐blind method*" or "double‐blind method*" or "control group*" or placebo* or "time series" or "quasi‐experiment*" or "pre test" or pretest or "pre‐intervention" or "post‐intervention" or posttest or "post test" or "controlled before" or "before and after stud*" or "follow‐up assessment*" or program or programme or "secondary anal*" or "impact evaluation*" or regression or "propensity match*" or "propensity scor*" or "matched comparison*" or "discontinuity anal*" or "outcome assessment*" or "rapid review" or "process outcome")
7.
AB,TI(evaluat* or intervention or interventional or treatment* or educate) AND AB,TI(control or controlled or study or program* or comparison or "before and after" or comparative or health promot*)
8. 6 OR 7
9. 5 AND 8
10.
AB,TI("Cherokee choices" or "REACH program*" or "communities that care" or "racial and ethnic approaches to community health" or "health care coalition*" or "healthy people program*" or "community coalition*")
11. 9 OR 10
========================================================
Database: Embase (Embase.com interface) January 1990 ‐ March 31, 2014.
1.
'medically underserved area':ab,ti OR 'medically underserved areas':ab,ti OR poverty:de OR 'vulnerable population':de OR 'minority group':de OR 'health disparity':de OR 'ethnic or racial aspects':de OR 'ethnic group'/exp OR 'cultural anthropology':de OR socioeconomics/exp OR 'developing country':de OR refugee:de OR 'social environment'/exp
2.
(health OR social OR diseas* OR morbidit* OR mortalit* OR racial OR ethnic) NEAR/5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage* OR gradient*)
3.
(disadvant* OR 'low income' OR marginali* OR underserved OR 'under served' OR depriv* OR poverty OR impoverish* OR minorit* OR racial OR ethnic) NEAR/5 (population OR group OR communit* OR neighbor?rhood*)
4.
('low pay' OR 'low paying' OR 'low paid' OR unemploy* OR depriv* OR 'financial hardship' OR 'benefit recipient' OR 'benefit recipients' OR 'social position' OR 'social positions' OR 'social class' OR 'social classes' OR socioeconomic* OR 'social status' OR poverty OR impoverish*) NEAR/5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*)
5.
(illitera* OR 'educational attainment' OR 'educational attainments' OR 'educational level' OR 'education levels' OR 'educational level' OR 'educational levels' OR 'education status' OR 'low education' OR 'educational achievement' OR 'educational achievements' OR 'school leaver' OR 'school leavers') NEAR/5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*)
6.
('single parent' OR 'single parents' OR 'lone parent' OR 'lone parents' OR rural OR refugee* OR immigrant* OR 'ethnic minority' OR 'ethnic minorities' OR 'ethnic group' OR 'ethnic groups' OR 'racial group' OR 'racial groups' OR indigenous) NEAR/5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*)
7.
(gender OR women) NEAR/5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*) OR school n5 children OR pacific islander* OR African American OR Hispanic* OR latino OR latina OR Asian American OR 'Alaska native?' OR 'native alaskan?' OR 'American indian?'
8. OR 1‐7 (population)
9.
(communit* OR civic) NEAR/5 (coalition? OR partnership* OR collaborat* OR participat* OR engage* OR combin* OR share* OR sharing OR union* OR alliance* OR associat* OR federation* OR 'joint venture' OR 'joint ventures' OR pool* OR resource* OR cooperat* OR collaborat* OR champion? OR involv* OR empower* OR panel? OR forum? OR jury OR juries OR council? OR mobilis* OR mobiliz* OR consortium* OR empower* OR network*)
10.
neighbo?r* NEAR/5 (coalition? OR partnership* OR collaborat* OR participat* OR engage* OR combin* OR share* OR sharing OR union* OR alliance* OR associat* OR federation* OR 'joint venture' OR 'joint ventures' OR pool* OR resource* OR cooperat* OR collaborat* OR champion? OR involv* OR empower* OR panel? OR forum? OR jury OR juries OR council? OR mobilis* OR mobiliz* OR consortium* OR empower* OR network*)
11.
public NEAR/5 (coalition? OR partnership* OR collaborat* OR participat* OR engage* OR combin* OR share* OR sharing OR union* OR alliance* OR associat* OR federation* OR 'joint venture' OR 'joint ventures' OR pool* OR resource* OR cooperat* OR collaborat* OR champion? OR involv* OR empower* OR panel? OR forum? OR jury OR juries OR council? OR mobilis* OR mobiliz* OR consortium* OR empower* OR network*)
12.
(village* OR city OR cities OR town*) NEAR/5 (coalition? OR partnership* OR collaborat* OR participat* OR engage* OR combin* OR share* OR sharing OR union* OR alliance* OR associat* OR federation* OR 'joint venture' OR 'joint ventures' OR pool* OR resource* OR cooperat* OR collaborat* OR champion? OR involv* OR empower* OR panel? OR forum? OR jury OR juries OR council? OR mobilis* OR mobiliz* OR consortium* OR empower* OR network*)
13.
(citizen OR 'local people' OR 'local peoples' OR resident? OR stakeholder*) NEAR/2 (coalition? OR partnership* OR collaborat* OR participat* OR engage* OR combin* OR share* OR sharing OR union* OR alliance* OR associat* OR federation* OR 'joint venture' OR 'joint ventures' OR pool* OR resource* OR cooperat* OR collaborat* OR champion? OR involv* OR empower* OR panel? OR forum? OR jury OR juries OR council? OR mobilis* OR mobiliz* OR consortium* OR empower* OR network*)
14.
'health care coalition':ti OR 'health care coalitions':ti OR 'healthy people program':ti OR 'healthy people programs':ti OR 'community care':de OR 'community networks':ab,ti OR 'community network':ab,ti OR 'public relations':de
15.
'Cherokee choices' OR 'REACH program' OR 'REACH programs' OR 'communities that care' OR 'culturally appropriate' OR 'community development' OR 'citizen centered government' OR 'citizen centered governments' OR 'racial and ethnic approaches to community health' OR (community NEAR/5 coalition)
16. OR 9‐15 ‐ intervention terms
17.
[randomized controlled trial]/lim OR [controlled clinical trial]/lim OR 'clinical trial'/exp OR 'comparative study':de OR evaluation:de OR 'evaluation research':de OR 'cohort analysis':de OR 'intervention study':de OR 'health care quality'/exp OR randomization:de OR 'clinical trial (topic)'/exp OR 'single blind procedure':de OR 'double blind procedure':de OR 'control group':de OR randomized:ab,ti OR randomized:ab,ti OR placebo*:ab,ti OR randomly:ab,ti OR groups:ab,ti OR trial:ab,ti OR time series:ab,ti OR 'quasi‐experimental':ab,ti OR 'pre test':ab,ti OR pretest:ab,ti OR 'pre‐intervention':ab,ti OR 'post‐intervention':ab,ti OR posttest:ab,ti OR 'post test':ab,ti OR 'controlled before':ab,ti OR 'before and after study':ab,ti OR 'before and after studies':ab,ti OR 'follow‐up assessment':ab,ti OR program:ab,ti OR programme:ab,ti OR 'secondary analysis':ab,ti OR 'secondary analyses':ab,ti OR 'impact evaluation':ab,ti OR regression:ab,ti OR 'propensity match':ab,ti OR 'propensity matched':ab,ti OR 'propensity matching':ab,ti OR 'propensity score':ab,ti OR 'propensity scores':ab,ti OR 'propensity scored':ab,ti OR 'propensity scoring':ab,ti OR 'matched comparison':ab,ti OR 'discontinuity analysis':ab,ti OR 'discontinuity analyses':ab,ti OR 'treatment outcome'/exp
18.
(evaluat*:ab,ti OR intervention:ab,ti OR interventional:ab,ti OR treatment*:ab,ti OR educate:ab,ti) AND (control:ab,ti OR controlled:ab,ti OR study:ab,ti OR program*:ab,ti OR comparison:ab,ti OR 'before and after':ab,ti OR comparative:ab,ti OR 'health promotion':ab,ti)
19.
intervention* NEAR/8 evaluat* OR intervention* NEAR/8 effect* OR intervention* NEAR/8 outcome* OR process NEAR/8 evaluat* OR process NEAR/8 effect* OR process NEAR/8 outcome* OR program NEAR/8 evaluat* OR program NEAR/8 effect* OR program NEAR/8 outcome* OR 'racial and ethnic approaches to community health' OR 'rapid review':ab,ti OR community NEAR/5 coalition*
20. #17 OR #18 OR #19 ‐ study design filter
21. #8 AND #16 AND #20
=========================================================================================
Database: New York Academy of Medicine's Grey Literature Collection (http://www.nyam.org/library/online‐resources/grey‐literature‐report/). Search performed December 19, 2011.
(("medically underserved" OR orphanages OR "poverty areas" OR "special populations" OR "minority groups" OR "ethnic groups" OR immigrants OR "socioeconomic factors" OR refugee* OR "social environment" OR "social problem*" OR "pacific islanders" OR "African Americans" OR Hispanics OR latinos OR latinas OR "Asian Americans" OR "Alaska natives" OR "American indians" OR "ethnic minority" OR "ethnic minorities" OR "racial minorities" OR "racial groups") AND ((community OR civic OR neigborhood OR neighbourhood OR resident OR "local people) AND (coalition* OR partnership* OR collaboration* OR participation OR engagement OR combined OR combination OR share OR union OR alliance OR associate OR federation OR "joint venture" OR pool OR resource OR cooperate OR collaborate OR champion* OR involve OR empower OR panel OR forum OR jury OR council* OR mobilize OR mobilise OR consortium OR network)) AND (trial OR trials OR study OR studies OR evaluation* OR intervention* OR "control group" OR analysis OR assessment OR outcome OR review))
=========================================================================================
Database: OpenGrey (SIGLE) (http://www.opengrey.eu/). Search performed December 19, 2011.
(("medically underserved" OR orphanages OR "poverty areas" OR "special populations" OR "minority groups" OR "ethnic groups" OR immigrants OR "socioeconomic factors" OR refugee* OR "social environment" OR "social problem*" OR "pacific islanders" OR "African Americans" OR Hispanics OR latinos OR latinas OR "Asian Americans" OR "Alaska natives" OR "American indians" OR "ethnic minority" OR "ethnic minorities" OR "racial minorities" OR "racial groups") AND ((community OR civic OR neigborhood OR neighbourhood OR resident OR "local people) AND (coalition* OR partnership* OR collaboration* OR participation OR engagement OR combined OR combination OR share OR union OR alliance OR associate OR federation OR "joint venture" OR pool OR resource OR cooperate OR collaborate OR champion* OR involve OR empower OR panel OR forum OR jury OR council* OR mobilize OR mobilise OR consortium OR network)) AND (trial OR trials OR study OR studies OR evaluation* OR intervention* OR "control group" OR analysis OR assessment OR outcome OR review))
=========================================================================================
Database: PsycInfo (Ebsco interface) January 1990 ‐ March 31, 2014.
1.
DE poverty areas OR DE social environments+ OR DE social deprivation+ OR DE ghettoes OR DE minority groups OR DE health disparities OR DE racial and ethnic groups+ OR DE race and ethnic discrimination OR DE indigenous populations+ OR DE disadvantaged OR DE homeless+ OR DE poverty OR DE cultural deprivation OR DE sociocultural factors+ OR DE socioeconomic status+ OR DE developing countries OR DE refugees
2.
(health OR social OR disease* OR morbidit* OR mortalit* OR racial OR ethnic) n5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage* OR gradient*)
3.
((disadvant* OR low income or marginali* OR underserved OR under served OR depriv* OR poverty OR impoverish* OR minorit* OR racial OR ethnic*) n5 (population OR group OR communit* OR neighbo#rhood*)) OR (school* n5 community)
4.
(low pay OR low paid OR unemploy* OR depriv* OR financial hardship OR benefit recipient* OR social position* OR social class* OR socioeconomic OR social status OR poverty OR impoverish*) n5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*)
5.
(illitera* OR education* attainment* OR education* level# OR education* status OR low education OR education* achievement* OR school leaver*) n5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*)
6.
(single parent* OR lone parent* OR rural OR refugee* OR immigrant* OR ethnic minorit* OR ethnic group* OR racial group* OR indigenous) n5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*)
7.
(gender OR women) n5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*) OR school n5 children OR pacific islander* OR African American OR Hispanic* OR latino OR latina OR Asian American OR Alaska* native* OR American Indians
8. OR 1‐7 (population)
9.
(communit* OR civic OR neighbo#r* OR public OR village* OR city OR cities OR town OR citizen* OR local people* OR resident# OR stakeholder*) n5 (coalition# OR partnership* OR collaborat* OR participat* OR engage* OR combin* OR share* OR sharing OR union* OR alliance* OR associat* OR federation* OR joint ventur* OR pool* OR resource* OR cooperat* OR champion# OR involv* OR empower* OR panel# OR forum# OR jury OR juries OR council# OR mobilis* OR mobiliz* OR consortium* OR empower* OR network*)
10.
MH health care coalitions OR MH healthy people programs OR MH community health services/og OR MH community networks OR MH community institutional relations OR MH consumer participation+ OR MH community health planning
11.
Cherokee choices OR REACH program* OR "communities that care" OR culturally appropriate OR community develop* OR citizen cent* government* OR "racial and ethnic approaches to community health" OR community n5 coalition*
12.
DE coalition formation OR DE community involvement
13. OR 9‐12 ‐ intervention terms
14.
randomized OR randomised OR placebo* OR randomly OR groups OR trial OR time series OR quasi‐experiment* OR pre test OR pretest OR pre‐intervention OR post‐intervention OR posttest OR post test OR "controlled before" OR "before and after stud*" OR follow‐up assessment OR outcome assessment OR program OR programme OR secondary anal* OR impact evaluation OR regression OR propensity match* OR propensity scor* OR matched comparison OR discontinuity anal*
15.
evaluat* OR intervention OR interventional OR treatment* OR TX educate) AND (control OR controlled OR study OR program* OR comparison OR "before and after" OR comparative OR health promot*
16.
((intervention* OR process OR program) n8 (evaluat* OR effect* OR outcome*)) OR "racial and ethnic approaches to community health" OR rapid review OR community n5 coalition*
17. S14 OR S15 OR S16 ‐ study design filter
21. S8 AND S13 AND S17
========================================================================================================
Database: Social Sciences Citation Index (SSCI) (ISI Web of Science interface) January 1990 ‐ March 31, 2014.
1.
"medically underserved area" OR orphan* OR "poverty area*” OR "special population*" OR "minority group*" OR "ethnic group*" OR culture* OR "immigrant*" OR "socioeconomic factor*" OR "developing countries" OR refugee* OR "social environment*" OR "social problems"
2.
(health OR social OR disease* OR morbidit* OR mortalit* OR racial OR ethnic) NEAR/5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage* OR gradient*)
3.
((disadvant* OR low income or marginali* OR underserved OR under served OR depriv* OR poverty OR impoverish* OR minorit* OR racial OR ethnic*) NEAR/5 (population OR group OR communit* OR neighbo#rhood*)) OR (school* NEAR/5 community)
4.
(low pay OR low paid OR unemploy* OR depriv* OR financial hardship OR benefit recipient* OR social position* OR social class* OR socioeconomic OR social status OR poverty OR impoverish*) NEAR/5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*)
5.
(illitera* OR education* attainment* OR education* level# OR education* status OR low education OR education* achievement* OR school leaver*) NEAR/5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*)
6.
(single parent* OR lone parent* OR rural OR refugee* OR immigrant* OR ethnic minorit* OR ethnic group* OR racial group* OR indigenous) NEAR/5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*)
7.
(gender OR women) NEAR/5 (inequalit* OR inequit* OR disparit* OR equit* OR disadvantage*) OR school NEAR/5 children OR pacific islander* OR African American OR Hispanic* OR latino OR latina OR Asian American OR Alaska* native* OR American Indians
8. OR 1‐7 (population)
9.
(communit* OR civic OR neighbo?r* OR public OR village* OR city OR cities OR town OR citizen* OR local people* OR resident? OR stakeholder*) NEAR/5 (coalition? OR partnership* OR collaborat* OR participat* OR engage* OR combin* OR share* OR sharing OR union* OR alliance* OR associat* OR federation* OR joint ventur* OR pool* OR resource* OR cooperat* OR champion? OR involv* OR empower* OR panel? OR forum? OR jury OR juries OR council? OR mobilis* OR mobiliz* OR consortium* OR empower* OR network*)
10.
“health care coalition*” OR “healthy people program*” OR "community health services" OR "community network*” OR "community institutional relations" OR "consumer participation" OR “community health planning” OR “Cherokee choices” OR “REACH program*” OR "communities that care" OR “culturally appropriate” OR “community develop*” OR “citizen cent* government*” OR "racial and ethnic approaches to community health" OR community NEAR/5 coalition*
11. OR 9‐10 ‐ intervention terms
12.
"randomized controlled trial*" OR "clinical trial?" OR "comparative studies" OR "comparative study" OR "evaluation research" OR "prospective study" OR "prospective studies" OR "experimental studies" OR "program evaluation*" OR "random sampl*" OR "control group*" OR randomized OR randomized OR randomly OR placebo* OR groups OR trial OR "time series" OR quasi‐experiment* OR "pre test" OR pretest OR pre‐intervention OR "post‐intervention" OR posttest OR "post test" OR "controlled before" OR "before and after stud*" OR "follow‐up assessment" OR program OR programme OR "secondary anal*" OR "impact evaluation" OR regression OR "propensity match*" OR "propensity scor*" OR "matched comparison") OR "discontinuity anal*"
13.
(evaluat* OR intervention* OR treatment* OR educate) AND (control OR controlled OR study OR program* OR comparison OR "before and after" OR comparative OR “health promot*”)
14.
((intervention* OR process OR program) NEAR/8 (evaluat* OR effect* OR outcome*)) OR "racial and ethnic approaches to community health" OR “rapid review” OR community NEAR/5 coalition*
15. #12 OR #13 OR #14 ‐ study design filter
16. #8 AND #11 AND #15
=================================================================================
Database: World Health Organization (WHO) Global Health Library Regional Indexes. (http://www.globalhealthlibrary.net/php/index.php). 2001‐2014.
(("medically underserved" OR orphan OR orphanages OR "poverty area*" OR "special population*" OR "minority group*" OR "ethnic group*" OR immigrant OR "socioeconomic factors" OR refugee OR "social environment" OR "social problem*")
OR
((health OR disease OR morbidity OR mortality OR racial OR ethnic) AND (inequality OR inequity OR disparity OR equity OR disadvantage OR gradient))
OR
((disadvantage OR "low income" OR marginalize OR marginalise OR underserved OR "under served" OR deprive OR poverty OR impoverish OR minority) AND (population OR group OR community OR neighborhood OR neighbourhood))
OR
(("low pay" OR "low paid" OR unemployed OR deprive OR "financial hardship" OR "benefit recipient" OR "benefit recipients" OR "social position" OR "social class" OR socioeconomic OR "social status" OR poverty OR impoverish) AND (inequality OR inequity OR disparity OR equity OR disadvantage))
OR
((illiterate OR "educational attainment" OR "educational attainments" OR "educational level" OR "educational status" OR "low education" OR "educational achievement" OR "school leaver" OR "school leavers") AND (inequality OR inequity OR disparity OR equity OR disadvantage))
OR
(("single parent" OR "lone parent" OR rural OR refugee OR immigrant OR "ethnic minority" OR "ethnic minorities" OR "ethnic group" OR "ethnic groups" OR "racial group" OR "racial groups" OR indigenous OR gender OR women) AND (inequality OR inequity OR disparity OR equity OR disadvantage)))
AND
(((communit* OR civic OR neighbor* OR neighbour* OR public OR village* OR city OR cities OR town OR towns OR citizen* OR "local people*” OR resident OR residents OR stakeholder*) AND (coalition* OR partnership* OR collaborat* OR participat* OR engage* OR combine* OR combination OR share* OR sharing OR union* OR alliance* OR associat* OR federation* OR "joint venture” OR "joint ventures" OR pool OR resource* OR cooperat* OR collaborat* OR champion OR champions OR involv* OR empower* OR panel OR panels OR forum OR forums OR jury OR juries OR council OR councils OR mobiliz* OR mobilis* OR consortium OR empower* OR network*)))
================================================================
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abbema 2004.
| Methods |
Study design: controlled before‐after (independent samples) Sampling frame: districts in the City of Arnhem, Netherlands Sampling method: convenience Collection method: mail survey to random sample obtained from population register of residents > 14 years of age Description of the community coalition: The Regional Health Authority and the Local Social Service Institute initiated the community project Arnhemse Broek, Healthy and Well, in a deprived area of the city of Arnhem in which professionals from 20 organizations (police, environmental and public works services, social services, and youth services) formed committees to address stress, physical inactivity, unemployment, and safety through a comprehensive, multi‐level, multi‐strategy community intervention. A needs assessment and priority setting process involved community members. Over a 2‐year action period, the multi‐sector group provided 54 community‐based programs and activities targeting these conditions |
|
| Participants |
Communities: deprived districts of the city of Arnhem; 1 intervention and 2 control sites Country: Netherlands Ages included in assessment: 14 and older Reasons provided for selection of intervention community: deprived area; aim of intervention was to reduce health inequalities Intervention community (population size): Arnhemse (5000) Comparison community (population size): districts of Arnheim (7000, 9500) |
|
| Interventions |
Name of intervention: Arnhemse Broek, Healthy and Well Theory: Lalonde's Health Determinants Framework Aim: to reduce socioeconomic health inequalities Description of costs and resources: ‘seed money’ provided to initiate activities but no other funding Components of the intervention: provision of information, behavioral change strategies, increased police services, environmental change, regulatory change Start date: June 1998 Duration: 2 years |
|
| Outcomes |
Outcomes and measures: self reported health status, self reported physical activity level Time points: baseline and 24 months |
|
| Notes | Outcomes measured at the population level by mail survey Source of funding: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐experimental controlled before‐after study with 1 intervention and 2 control districts within the same city |
| Allocation concealment (selection bias) | High risk | Allocation not concealed |
| Baseline outcome measurement similar | High risk | Baseline difference in control community 2: physical activity level lower |
| Baseline characteristics similar | High risk | Baseline differences in control area 2: older, less educated, more immigrants |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Differential response rates at follow‐up between intervention and control area 2: 58.8%, 73.2% |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding of participants not reported. |
| Protection against contamination | High risk | Intervention community and control area 1 were adjacent |
| Selective reporting (reporting bias) | Low risk | Questionnaire items described In detail |
Blumenthal 2010.
| Methods |
Study design: cluster RCT Sampling frame: African Americans over age 49, no history of colorectal cancer (CRC), and no previous CRC screening within the recommended time interval Sampling method: random Collection method: telephone interview Description of the community coalition: The Community Coalition Board of the Morehouse School of Medicine Preventive Research Center comprised representatives from the medical school, 2 other academic institutions, and 6 local agencies (the health department, public schools, public housing authority, local community health center, area health education center, the Empowerment Zone Corporation), and from each of the 8 neighborhoods of Neighborhood Planning Unit Y of Atlanta, plus some adjoining neighborhoods. Community members held most of the positions as well as the chair. The Board served in a governance rather than advisory capacity as a senior partner with the medical school, established the research agenda for the PRC, reviewed all research protocols, and participated in study recruitment |
|
| Participants |
Communities: all participants (n = 369) recruited from 4 counties of the Atlanta metropolitan area (DeKalb, Fulton, Cobb, Clayton) Country: USA Ages included in assessment: 50+ (mean age 68) Reasons provided for selection of intervention community: none stated Intervention community (population size): Atlanta metro area (not stated) Comparison community (population size): Atlanta metro area (not stated) |
|
| Interventions |
Name of intervention: Colorectal Cancer Screening Intervention Trial (CCSIT) Theory: Social‐Ecologic Theory, Social Cognitive Theory Aim: to test 3 interventions to increase colorectal cancer screening rates among African Americans. These interventions also addressed gaps in the evidence as summarized in the Guide to Community Preventive Services; each approach is considered by the Guide to have "insufficient evidence" on which to base a recommendation Description of costs and resources: not reported Components of the intervention: 3‐arm trial:
Start date: January 2003 Duration: up to 4 weeks |
|
| Outcomes |
Outcomes and measures: Primary: receipt of colorectal cancer screening test (self report, not defined) Secondary: CRC knowledge (7‐item questionnaire) Time points: baseline and follow‐up (3 months, 6 months) |
|
| Notes | Participants were randomly assigned to intervention or control arm by recruitment site; controls received educational materials at introductory session. Participants who withdrew after randomization but before intervention were not included in the analysis. 30% of participants were lost to follow‐up and were considered unscreened Source of funding: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not specified |
| Allocation concealment (selection bias) | Unclear risk | Not specified |
| Baseline outcome measurement similar | Low risk | None of the participants had been screened at baseline |
| Baseline characteristics similar | Unclear risk | Baseline characteristics of groups similar, except participants in financial support arm were more likely to have private insurance |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 40% of participants withdrew after randomization or were lost to follow‐up after intervention. Study completers tended to be better educated than non‐completers |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | Unclear risk | Participants cluster‐randomized by recruitment site to minimize contamination; no information provided about relationships or social cross‐over among sites |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes are reported |
Brown 2013.
| Methods |
Study design: RCT Sampling frame: school rosters Sampling method: Rosters were blocked by site and grade and were randomly ordered within blocks for recruitment Description of the community coalition: The community‐academic partnership started in 2004 with a qualitative study of barriers to and facilitators of healthy eating among Native youth. This provided the basis for the design of the Journey to Native Youth Health intervention for healthy weight maintenance, lower fat intake, and increased physical activity. The collaborative partnership consisted of tribal health center staff, tribal health board, and council members of 2 Northern Plains Indian reservations, as well as University of Montana academic researchers. Together they prepared a grant for funding and modified an existing diabetes prevention program to make it developmentally and culturally appropriate for Native youth at high risk of diabetes. Collaboration oversaw implementation and evaluation of the program |
|
| Participants |
Communities: 2 Northern Plains Indian reservations in Montana Country: USA Ages included in assessment: 10 to 14 years Reasons provided for selection of intervention community: high risk of diabetes among Native youth Intervention community (population size): 9570 Comparison community (population size): same |
|
| Interventions |
Name of intervention: Journey to Native Youth Health was a youth diabetes prevention program. This 3‐month program trained tribal health representatives who offered the after‐school behavioral change program to 8 youth groups age 10 to 14 (n = 76), who were randomly assigned to the diabetes prevention intervention or to a control group that received substance abuse prevention information Theory: none stated Aim: healthy weight maintenance, lower fat intake, and greater physical activity Description of costs and resources: no program cost data provided. 2 tribal representatives received intense 2‐week training. Incentives of approximately $175 in sports clothing and equipment and cash for healthy food were provided per participant Components of the intervention: individual and family education Start date: 2010 Duration: 3 months |
|
| Outcomes |
Outcomes and measures (follow‐up months):
Date (year) of pre and post measurements: 2010/2011 to 2011/2012 |
|
| Notes | Study authors describe this as a pilot study to test program feasibility and acceptability and confirm that the study duration was too short to measure change in BMI | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | School rosters were blocked by site and grade and were randomly ordered within blocks for recruitment |
| Allocation concealment (selection bias) | High risk | Neither participants nor implementers were blinded |
| Baseline outcome measurement similar | Low risk | No differences in measurements |
| Baseline characteristics similar | Low risk | Similar baseline characteristics reported |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 84% retention; similar loss to f/u in each group |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Neither blinded |
| Protection against contamination | High risk | Interventions for treatment and control were offered in each small community |
| Selective reporting (reporting bias) | Low risk | Primary outcomes were reported |
Brownson 1996.
| Methods |
Study design: controlled before‐after study (independent samples) Sampling frame: non‐institutionalized adults with telephones Sampling method: at baseline, random‐digit dialing; at follow‐up, RDD in entire intervention area for first 1000 respondents, then RDD in communities with > 20% black population for next 500 Collection method: telephone interviews (n = 1510) Description of the community coalition: The Missouri Southeastern District Health Office hired a full‐time project co‐ordinator to form and oversee 6 county coalitions comprising representatives from the community, municipal government, a citizen advocacy agency, religious organizations, university staff, and local and state health departments. County coalitions had full control over selection and implementation of interventions |
|
| Participants |
Communities: 6 rural counties in the southeastern Missouri Bootheel region compared with the rest of rural Missouri Country: USA Ages included in assessment: 18+ Reasons provided for selection of intervention community: The Bootheel region displayed significantly high rates of death from coronary heart and cerebrovascular disease, as well as the largest minority population in Missouri, and high rates of poverty, unemployment, and medical underservice Intervention community (population size): 6 rural counties in the southeastern Missouri Bootheel region (approximately 160,000) Comparison community (population size): the rest of rural Missouri (not reported) |
|
| Interventions |
Name of intervention: Bootheel Heart Health Project Theory: Social Learning Theory, Stage Theory of Innovation Aim: to assess whether a community‐based risk reduction project reduces major modifiable risk factors for cardiovascular disease Description of costs and resources: each county coalition given $5,000 to 8,000 per year to implement intervention activities Components of the intervention: Intervention activities included blood pressure and cholesterol screenings, walking groups, exercise and cooking/nutrition classes, parties, pageants, and anti‐smoking campaigns and contests Start date: September 1990 Duration: 4 years |
|
| Outcomes |
Outcomes and measures:
Time points: baseline (1990) and follow‐up (1994) |
|
| Notes | Fifth outcome reported in study (cholesterol checked in past 2 years) not included in review because comparison community data collected 1 year earlier. Comparison between “coalition present” and “coalition absent” communities within the Bootheel 6‐county region not included in this review Outcomes measured at the population level by telephone surveys Source of funding: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Intervention was not randomly assigned |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | High risk | Baseline rates of physical activity significantly different even after adjustment for demographic factors by analysis of covariance (43.1% in intervention group vs 29.0% in control group) |
| Baseline characteristics similar | High risk | Allocation by region; intervention and comparison populations are not comparable |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Sampling strategy was changed between baseline and follow‐up in the intervention group. Response rate declined over time in the intervention group and was not stated for the control group. Proportion of study sample without telephone not stated for control population |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | Unclear risk | No statement regarding contamination |
| Selective reporting (reporting bias) | Unclear risk | Only 5 risk factors reported out of 87+ BRFSS questions |
Brownson 2004.
| Methods |
Study design: controlled before‐after study (independent samples) Sampling frame: non‐institutionalized adults with working telephone Sampling method: random‐digit dialing Collection method: telephone interviews (n = 1233) Description of the community coalition: An academic team was formed to work with the Bootheel Heart Health coalitions and local governments to develop walking trails and to promote physical activity in 6 Missouri communities. The Bootheel Heart Health coalitions were 6 county‐wide groups originally comprising representatives from the community, municipal government, a citizen advocacy agency, religious organizations, university staff, and local and state health departments (see Brownson 1996; no updated coalition membership provided for this later intervention) |
|
| Participants |
Communities: rural communities Country: USA Ages included in assessment: 18+ Reasons provided for selection of intervention community: Bootheel region has more poverty, is medically underserved, and has lower education levels; age‐adjusted death rates for heart disease are significantly higher than in the rest of the state Intervention community (population size): 6 rural communities in the southeastern Missouri Bootheel region with population range of 2399 to 17,642 Comparison community (population size): 6 communities in Arkansas and Tennessee with population range of 2399 to 17,642 |
|
| Interventions |
Name of intervention: Bootheel Walking Promotion Project Theory: Multi‐Level Ecologic Model Aim: to increase physical activity (walking) at the community level Description of costs and resources: none provided Components of the intervention: development of walking trails, tailored newsletters, walking clubs Start date: December 2000 Duration: 1.5 years |
|
| Outcomes |
Outcomes and measures:
Time points: baseline (December 2000 to May 2001) and follow‐up (June to August 2002) |
|
| Notes | Walking trails appear to have been developed between 1975 and 1997. Additionally, the Bootheel Heart Health coalition had been actively promoting physical activity in the area since 1990 Outcomes measured at the population level by telephone surveys Source of funding: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Intervention was not randomly assigned |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | High risk | Baseline rates of physical activity significantly different even after adjustment for demographic factors by analysis of co‐variance (43.1% in intervention group vs 29.0% in control group) |
| Baseline characteristics similar | High risk | Allocation is by region, and intervention and comparison populations are not comparable |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Sampling strategy was changed between baseline and follow‐up in the intervention group. Response rate declined over time in intervention group and was not stated for control group. Proportion of study sample without telephone not stated for control population |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | Unclear risk | No statement regarding contamination |
| Selective reporting (reporting bias) | Unclear risk | Only 5 risk factors reported out of 87+ BRFSS questions |
Burhansstipanov 2010.
| Methods |
Study design: controlled before‐after (independent samples) Sampling frame: Denver, Colorado; low‐income minority women including Native American, Latina, and African American Sampling method: convenience Collection method: telephone or in‐person interview Description of the community coalition: A coalition of 3 organizations serving low‐income minority women (Native American Cancer Research, La Clinica Tepeyac, and Exempla Saint Joseph Hospital) was formed to implement “Increasing Mammography Adherence among Medically Underserved Women‐MUP,” a National Cancer Institute‐funded project. Data collected before the intervention by the Susan Komen Foundation and the University of Colorado Cancer Center indicated the need for culturally relevant patient navigator support for low‐income minority and white women to increase mammography rescreening among women > 40 years of age. A statewide network, the “Partnership in Cancer Control Among Underserved Populations,” served as the advisory committee for the project. A patient navigator model of care was selected on the basis of previous effectiveness in 2 Native American breast cancer screening studies |
|
| Participants |
Communities: Denver, Colorado Country: USA Ages included in assessment: women > 39 years, mean age 52.9 years Reasons provided for selection of intervention community: Data (not reported in paper) gathered by the Susan Komen Foundation and the University of Colorado Cancer Center indicated the need Intervention group: (n = 316) women recruited through outreach at 3 coalition settings and community cultural events Comparison group: (n = 200) women in the Colorado Mammography Advocacy Program of similar demographics |
|
| Interventions |
Name of intervention: Increasing Mammography Adherence among Medically Underserved Women (MUP) Theory: Social Learning Theory Aim: to increase regular mammography rescreening among medically underserved women > 39 years of age Description of costs and resources: Patient navigators were hired and were provided 80 hours of training on patient support and education, breast cancer, cancer screening, and intervention for abnormal mammograms. Each of the 3 coalition organizations hired navigators for patient outreach and follow‐up. Number of patient navigators is not provided and costs are not mentioned Components of the intervention: Culturally appropriate education session, assistance with scheduling mammogram, and follow‐up by phone or visit to document screening were provided; assistance was provided with follow‐up appointment if result was abnormal. Patient navigators followed checklist to document implantation of program components. Control group received usual care Start date: 2001 Duration: 5 years |
|
| Outcomes |
Outcomes and measures: self report of receipt of mammogram Time points: not reported |
|
| Notes | High attrition in intervention group due to change in Colorado law disallowing publicly funded services to undocumented Latinas Source of funding: agencies within the coalition |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Convenience sample |
| Allocation concealment (selection bias) | High risk | Allocation not concealed |
| Baseline outcome measurement similar | Low risk | Only enrolled women who had never received repeat screening |
| Baseline characteristics similar | High risk | Baseline data not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Proportion of missing data higher among intervention group |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded |
| Protection against contamination | Unclear risk | Potential for contamination not described |
| Selective reporting (reporting bias) | Low risk | Relevant outcome reported |
Cardarelli 2011.
| Methods |
Study design: controlled before‐after study Sampling frame: women age 40 and older residing in 2 specific Dallas neighborhoods with no personal history of breast cancer Sampling method: random; multiple modalities including door‐to‐door recruitment, referrals, and flyers Description of the community coalition: The Dallas Cancer Disparities Community Research Coalition was created by academic investigators and community partners in 2007 to address disparities in cancer mortality in the South Dallas area. 10 diverse community members on a Community Advisory Board led the coalition |
|
| Participants |
Communities: Dallas, Texas Country: USA Ages included in assessment: 40+ (n = 119) Reasons provided for selection of intervention community: Residents of South Dallas experience higher breast cancer mortality compared with county averages Intervention community (population size): Frazier Courts neighborhood of South Dallas (not provided) Comparison community (population size): unnamed neighborhood of West Dallas (not provided) |
|
| Interventions |
Name of intervention: not provided, but based on the Forsyth County Cancer Screening Project intervention Theory: Health Belief Model, Social Cognitive Theory Aim: to assess the efficacy of an intervention designed to promote increased knowledge about the importance of early detection for reducing breast cancer mortality and for increasing uptake of breast cancer screening practices Description of costs and resources: not provided Components of the intervention: a series of eight 1.5‐hour breast health education classes delivered by volunteers and a mobile mammography unit brought to the neighborhood during the intervention period Start date: not provided Duration: 8 weeks |
|
| Outcomes |
Outcomes and measures (follow‐up months):
Years of pre and post measurements: not provided |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | No randomization |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | Unclear risk | Baseline rates of self examination not presented; baseline rates of clinical examination differed and baseline rates of mammography did not differ |
| Baseline characteristics similar | Unclear risk | Participant characteristics appear similar, but intervention was not randomly assigned |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Rates of loss to follow‐up similar for intervention and control groups, but relatively high (22%) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | Unclear risk | Distinct Dallas communities (but still in the same city) were chosen to minimize contamination |
| Selective reporting (reporting bias) | Low risk | Main outcome measures reported |
Cheadle 2001.
| Methods |
Study design: cluster RCT Sampling frame:low‐income minority neighborhoods in Seattle Sampling method: random Collection method: school‐based student and parent interviews, key informant interviews among civic leaders Description of the community coalition: Minority Youth Health Project was launched in a partnership between University of Washington, Seattle Minority Health Coalition, Seattle King County Public Health Department, Group Health Cooperative of Puget Sound, and Harborview Medical Center. 4 neighborhoods randomly selected; each formed a Community Action Board consisting of residents and a paid staff co‐ordinator and was given an $8000 annual budget to implement projects of their choosing to improve youth health and social opportunities and to increase neighborhood co‐operation. Limited information on coalition formal governance structures and processes or how they interacted with partnership agencies |
|
| Participants |
Communities: Seattle minority communities Country: USA Ages included in assessment: youth 11 to 13 and their parents Reasons provided for selection of intervention community: higher youth risks Intervention community (population size): 42,100 |
|
| Interventions |
Name of intervention: Seattle Minority Youth Health Project Theory: Community Empowerment Aim: to promote community mobilization and youth development strategies to prevent drug use, violence, and risky sexual activity Description of costs and resources: 4 paid community organizers at the 4 intervention sites. Salary amount not reported. Each of the 4 Community Action Boards received $8,000 to support community health promotion activities. Total federal funding received for the program reported Components of the intervention: Neighborhood projects included health fairs and community festivals, workshops, and training n deduction programs. About 2000 youth and adults participated in the projects across the 4 neighborhoods Start date: 1994 Duration: 50 months |
|
| Outcomes |
Outcomes and measures: measures of community mobilization and satisfaction with neighborhood. Researchers did not report health outcomes in this paper, and no further publications with health outcome data Time points: baseline and follow‐up (student and parent surveys 1994 and 1997) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not specified |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | Low risk | Similar baseline outcome measurement |
| Baseline characteristics similar | Unclear risk | Baseline characteristics of groups not reported separately |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 30% attrition |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | Unclear risk | Neighborhoods were in close proximity |
| Selective reporting (reporting bias) | High risk | Only community mobilization outcomes reported |
Clark 2013.
| Methods |
Study design: controlled before‐after (independent samples) Sampling frame: lower‐income areas in the US cities of Washington, DC; Hampton Roads, VA; San Juan, PR; Milwaukee, WI; Seattle, WA; Long Beach, CA; and Philadelphia, PA, with high asthma prevalence Sampling method: convenience Collection method: in‐person interviews with parents or guardians of children Description of the community coalition: The Robert Wood Johnson Foundation funded coalitions in 7 regions of the USA with the goal of changing policies and practices regarding asthma management in low‐income communities of color. The University of Michigan Center for Managing Chronic Disease served as the national program office. At each site, a coalition was formed comprising stakeholders including local healthcare providers, schools and day care centers, community advocacy groups, businesses, local government organizations, academic institutions, parent groups, and other community‐based organizations. Community contexts and coalition processes and structures differed at each site, but a common core of process and outcome evaluations were applied |
|
| Participants |
Communities: Washington, DC; Hampton Roads, VA; San Juan, PR; Milwaukee, WI; Seattle, WA; Long Beach, CA; Philadelphia, PA Country: USA Ages included in assessment: 0 to 17 years Reasons provided for selection of intervention community: communities of color with high asthma prevalence Intervention community (population size): approximately 75,000 across sites Comparison community (population size): similar but actual number not given |
|
| Interventions |
Name of intervention: Allies Against Asthma Theory: not reported Aim: to create population‐wide, macro‐level changes in asthma management practices and policies Description of costs and resources: Each site received up to $1.3 million per year Components of the intervention: education in homes, at community sites and for providers; changes in schools, child care centers, and recreation facilities to improve asthma management; care co‐ordination and case management; clinical quality improvement including standardized referrals, protocols, and action plans; establishment of registries; improved reimbursement and financial incentives; and policy change initiatives enacted. Each site employed a combination of most of these components Start date: 2000 Duration: 5 years |
|
| Outcomes |
Outcomes and measures: comparative data on parent reported asthma symptoms; parental quality of life. Descriptive data on coalition characteristics and policy and systems change Time points: baseline and 12 months |
|
| Notes | Funding source: government | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Controlled before‐after study with convenience sampling |
| Allocation concealment (selection bias) | High risk | Allocation not concealed |
| Baseline outcome measurement similar | Low risk | Baseline measurements reported were similar |
| Baseline characteristics similar | Unclear risk | Adjusted for baseline differences in race and age groups |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition 36% |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants not reported |
| Protection against contamination | Unclear risk | Description of control recruitment not detailed; however, state they were recruited in areas where coalition activity was limited or absent |
| Selective reporting (reporting bias) | Unclear risk | All outcomes collected were not specified in paper |
Darrow 2011.
| Methods |
Study design: controlled before‐after cross‐sectional study Sampling frame: Florida adults Collection method: State of Florida HIV incidence data Description of the community coalition: Florida International University and 3 community‐based organizations that served African American, Hispanic, Haitian, and Afro‐Caribbean communities formed a coalition in response to REACH 2010 funding with the aim of reducing disparities in HIV among minority young adults through community awareness and education. The University served as the lead agency and contracted with the CBOs annually to provide educational outreach |
|
| Participants |
Communities: Broward County, Florida Country: USA Ages included in assessment: adults Reasons provided for selection of intervention community: minority population with high HIV/AIDS rates Intervention community (population size): South Florida counties of Broward, Palm Beach, and Miami‐Dade (population size not provided) Comparison community (population size): North Florida counties of Duval, Hillsborough, and Orange (population size not provided) |
|
| Interventions |
Name of intervention: Broward County REACH HIV Prevention Theory: none reported Aim: to improve levels of awareness of the HIV/AIDS problems among minority young adults, to increase perceptions of the seriousness of the local AIDS problem, and to stimulate action to reduce HIV/AIDS in minority communities Description of costs and resources: 6 community health outreach workers, graduate students, and other university staff delivered interventions. US$103,500 provided annually to 3 CBOs; funding amount to University not reported Components of the intervention: educational materials in the form of posters, pamphlets, bus advertisements, newspaper articles, and radio and television public service announcements, as well as community health fairs and poetry competitions Start date: 2000 Duration: 4 years |
|
| Outcomes |
Outcomes and measures: annual HIV incidence rates per 100,000 Time points: 1998 to 2006 |
|
| Notes | Outcomes measured at population level using state HIV incidence data Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized |
| Allocation concealment (selection bias) | High risk | Non‐randomized |
| Baseline outcome measurement similar | Low risk | Statewide HIV surveillance data |
| Baseline characteristics similar | High risk | Baseline differences in HIV incidence between intervention and control |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Statewide HIV surveillance data |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Statewide surveillance system data |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Non‐randomized |
| Protection against contamination | Low risk | Counties not adjacent |
| Selective reporting (reporting bias) | Low risk | Statewide HIV surveillance data |
| Other bias | High risk | Included counties in the intervention group that received community outreach |
Davidson 1994.
| Methods |
Study design: interrupted time series with control group Sampling frame: Central Harlem, NYC, USA Sampling method: entire population (5‐ through 16‐year‐olds) Collection method: hospital and death records Description of the community coalition: The Safe Kids/Healthy Neighborhoods Coalition was initiated by the Harlem Hospital Injury Prevention Program in response to a request from parents and educators for a program in playground safety. The original coalition consisted of hospital, public health, public school, law enforcement, fire and emergency medical service, municipal government, parents, and community volunteers. Initial funding for the coalition was received from Robert Wood Johnson |
|
| Participants |
Communities: low‐income, predominantly African American Central Harlem and predominantly Hispanic Washington Heights Districts of New York City Country: USA Ages included in assessment: 5 through 16 Reasons provided for selection of intervention community: high risk of serious injury for youth in Central Harlem Intervention community (population size): 19,254 (5 to 16 years —1990 census) Comparison community (population size): 44,535 (5 to 16 years — 1990 census) |
|
| Interventions |
Name of intervention: Safe Kids/Healthy Neighborhoods Theory: not reported Aim: to reduce the rate of serious injury for 5‐ to 16‐year‐olds Description of costs and resources: cost unknown, funding from RWJ, CDC, and municipal government Components of the intervention: improvement to parks and playgrounds, playground supervision, traffic and bicycle safety education, bicycle helmets, activities for youth including sports, arts, and dance Start date: 1989 Duration: 36 months |
|
| Outcomes |
Outcomes and measures: risk ratio for serious injury after intervention compared with before the intervention Time points: pre‐intervention (1983 to 1988), intervention (1989 to 1991) |
|
| Notes | Outcomes measured at population level using vital statistics records and hospital records Funding source: Robert Wood Johnson Foundation, Centers for Disease Ccontrol and Prevention, and municipal government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | |
| Allocation concealment (selection bias) | Low risk | |
| Baseline outcome measurement similar | High risk | EPOC criteria for ITS study designs Independent of other change: High‐risk injury defines trends at both intervention and control sites |
| Baseline characteristics similar | Low risk | Point of analysis at intervention: low risk — annual surveillance data collected |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Intervention effect on data collection: low risk — population‐based injury surveillance system |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Incomplete outcome data: low risk — population‐based injury surveillance system |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Intervention effect on data collection: low risk — population‐based injury surveillance system |
| Protection against contamination | High risk | Independent of other change: high risk — injury defines trends at both intervention and control sites |
| Selective reporting (reporting bias) | Low risk | Selective reporting: low risk — population‐based injury surveillance system |
Dedobbeleer 2001.
| Methods |
Study design: controlled before‐after Sampling frame: St‐Croix School District in St‐Laurent City, Montreal, Quebec Sampling method: schools matched by urban, public, French‐speaking, and multi‐ethnic Description of the community coalition: A coalition of 15 partners, including public health organizations, community organizations (e.g. YMCA, St‐Laurent Youth Resources), schools, police, St‐Laurent City, parents, and youth representatives developed the project Coalition for Youth Quality of Life Project in St‐Laurent City, an industrial area on the west side of the Island of Montreal, Quebec, Canada, which has a large, multi‐ethnic immigrant population from Asia, North African, and Middle East. Training on intersectorial collaboration, youth development, and substance abuse was provided by professionals in partner organizations |
|
| Participants |
Communities: St‐Laurent City, an industrial area on the west side of the Island of Montreal, Quebec Country: Canada Ages included in assessment: 791 students in 6th grade and 8th grade cohorts Reasons provided for selection of intervention community: higher‐risk, multi‐ethnic population of recent immigrants Intervention community (population size): St‐Laurent City (67,000) Comparison community (population size): same |
|
| Interventions |
Name of intervention: Coalition for Youth Quality of Life Project Theory: Ecologic Participatory Framework, PROCEED Aim: to reduce alcohol and other drug use Description of costs and resources: Professionals from partner organization trained coalition members. Information on youth development, drug resistance, self esteem, and parent‐child communication was provided in a school setting Components of the intervention: skills development, parent education, competence enhancement, and youth mobilization Start date: coalition formed in 1990. Intervention in 1992 to 1993, 1993 to 1994 Duration: 2 school years (18 months) |
|
| Outcomes |
Outcomes and measures (follow‐up months): Follow at 30 months:
Date (year) of pre and post measurements Pre‐test 1992 Post‐test 1995 |
|
| Notes | Only 40% follow‐up at 30 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not randomized |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | High risk | Frequency of alcohol consumption and amount of alcohol consumed differed at baseline |
| Baseline characteristics similar | High risk | Significant difference in age of 6th grade cohort at baseline |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only 40% follow‐up at 30‐month measurement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel not blinded |
| Protection against contamination | High risk | Intervention and control student cohorts in the same school district |
| Selective reporting (reporting bias) | Unclear risk | Alcohol use and amount of alcohol consumed were primary outcomes. Drug use was of low prevalence at baseline and was not reported at follow‐up |
Fisher 1998.
| Methods |
Study design: controlled before‐after (independent samples) Sampling frame: non‐institutionalized adults residing within block boundaries of intervention neighborhoods or within zip code boundaries of control areas with a working telephone Sampling method: random‐digit dialing, then individuals selected at random within the household based on the number and sex of adult members of the household and the last digit of the telephone number Collection method: telephone interview (n = 1491) Description of the community coalition: Neighbors for a Smoke Free North Side was initiated by a partnership between Washington University and Grace Hill Neighborhood Services in conjunction with neighborhood steering committees composed of 10 to 15 volunteer community members and 1 Grace Hill staff person to serve as a facilitator. A "Nuts and Bolts" committee comprising representatives from Washington University and Grace Hill and the facilitator from each neighborhood committee performed central planning of project activities. Neighborhood committees were responsible for approving and carrying out all activities. In addition, a city‐wide advisory council with representatives from major corporate, medical, religious, and community groups, most of whom were African American, met monthly to provide resources and advice |
|
| Participants |
Communities: urban neighborhoods in St Louis and Kansas City Country: USA Ages included in assessment: 18+ Reasons provided for selection of intervention community: historically underserved, low income, urban settings Intervention community (population size): 3 neighborhoods of St Louis, MO (38,000) Comparison community (population size): 4 zip codes of Kansas City, MO (256,500) |
|
| Interventions |
Name of intervention: Neighbors for a Smoke Free North Side Theory: not reported Aim: to evaluate a community organization approach to smoking cessation among African Americans Description of costs and resources: not reported Components of the intervention: Intervention activities included smoking cessation classes, billboards, door‐to‐door campaigns, and a “gospelfest” Start date: April 1990 Duration: 24 months |
|
| Outcomes |
Outcomes and measures: smoking prevalence (self report) Time points: baseline (1990) and follow‐up (1992) |
|
| Notes | Outcomes measured at population level by telephone survey Source of funding: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Intervention not randomly assigned |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | Low risk | Smoking prevalence exactly the same between intervention and control groups at baseline |
| Baseline characteristics similar | High risk | Intervention and control groups differed on many demographic characteristics |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Population‐based telephone survey |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Independent samples lower the risk of incomplete outcome data |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No blinding was performed; unclear whether this would have any effect on self reported smoking status |
| Protection against contamination | Low risk | No protection against contamination noted; groups resided in different cities |
| Selective reporting (reporting bias) | Low risk | Main outcome reported |
Fisher 2004.
| Methods |
Study design: prospectively controlled cohort Sampling frame: African American children age 5 to 14 who had a physician diagnosis of asthma and at least 1 incident of acute care (seen in the emergency department or hospitalized for treatment of asthma at St Louis Children’s Hospital) and who lived in 1 of the intervention or control neighborhoods (n = 345) Sampling method: Parents of all eligible children were contacted for recruitment into the study Collection method: telephone interview and hospital records Description of the community coalition: The coalition was a continuation of the partnership between Washington University and Grace Hill Neighborhood Services that was initiated during the Neighbors for a Smoke Free North Side intervention project (Fisher 1998). The partnership worked in conjunction with 4 neighborhood steering committees, or “Wellness Councils.” The Wellness Councils are part of a larger Wellness Initiative, which also co‐ordinates other programs for the Grace Hill neighborhoods. Paid staff from the target neighborhoods serve as executive secretaries for the councils. Subcommittees of the all‐site Wellness Council, with representation from each of the 4 neighborhoods, handle different planning aspects of program activities. Additionally, a Physician Advisory Board was established by a co‐principal investigator to meet regularly with community practitioners to inform them about coalition activities, encourage referrals, and receive feedback |
|
| Participants |
Communities: 8 urban neighborhoods in St Louis, Missouri Country: USA Ages included in assessment: 5 to 14 Reasons provided for selection of intervention community: predominantly low income and African American with high numbers of Medicaid‐eligible children. Partnership and neighborhood committees already existed from previous smoking cessation project. Asthma morbidity and mortality due to deficits in basic care described as an issue for the target population Intervention community (population size): 4 St Louis neighborhoods served by Grace Hill Neighborhood Services (60,700) Comparison community (population size): 4 other St Louis neighborhoods in the same general area with similar demographic characteristics (population size not reported) |
|
| Interventions |
Name of intervention: Neighborhood Asthma Coalition (NAC) Theory: not reported Aim: to promote basic understanding of asthma, encourage improved management, and reduce the need for acute care within low‐income, predominantly African American neighborhoods Description of costs and resources: educational and training materials developed, residents hired to serve as "asthma advocates," no costs described Components of the intervention: promotional campaigns, training neighborhood residents as support workers for asthmatic children and their caregivers (“neighbor‐to‐neighbor support”), a neighborhood summer day camp and activities throughout the year for asthmatic children, their families and friends, asthma management curriculum offered through community settings, and activities in neighborhood schools Start date: 1992 Duration: 24 to 36 months, depending on when participant was recruited |
|
| Outcomes |
Outcomes and measures: acute care utilization related to asthma (reported by caregivers plus emergency department and hospital records); asthma management practices (score based on how caregivers reported they would respond to asthma symptoms) Time points: baseline (12 months before study enrollment for acute care visits, and initial study interview for asthma management score) and follow‐up (last 12 months of participation and final study interview, 2 to 3 years later, depending on timing of recruitment) |
|
| Notes | Losses to follow‐up were not included in analyses. The second outcome (asthma management practices) relates indirectly to the target population via their caregivers Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Intervention not randomly assigned |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | Low risk | Rates of acute care utilization in the year before enrollment and baseline asthma management scores were similar |
| Baseline characteristics similar | Low risk | Groups appear to be similar on key characteristics |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | “Lost to follow‐up” rates differed between intervention (29%) and control (10%) groups, but all lost participants were dropped from analysis |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated whether interviewers were blinded to participant groups, or if control and “low‐participation” intervention participants were aware of community‐wide intervention |
| Protection against contamination | Unclear risk | Control and intervention areas were located near one another. Control participants who reported participating in intervention activities were dropped from analysis Physicians involved in advisory board may have promoted intervention to control participants |
| Selective reporting (reporting bias) | Unclear risk | No relevant outcomes are omitted, but groups were re‐allocated on the basis of level of exposure to the intervention in secondary analyses |
| Other bias | Unclear risk | Response rates to initial recruitment call (69%) not presented by study group |
Fuller 2007.
| Methods |
Study design: controlled before‐after study Sampling frame: participants in pre‐existing studies of injection drug users (IDUs) Sampling method: convenience sample; participants were recruited at community research sites within target community using targeted and respondent‐driven sampling methods (n = 728) Collection method: survey/self report Description of the community coalition: Established in 1999, the Harlem Community and Academic Partnership is composed of 30 community‐based organizations in Harlem, 4 academic institutions, and the local health department. The partnership focuses on community‐based participatory research; members actively participate in needs assessment, issue identification, and priority setting |
|
| Participants |
Communities: IDUs in the community of Harlem, New York Country: USA Ages included in assessment: > 18 years of age Reasons provided for selection of intervention community: Partnership initially was created in Harlem to increase community participation in research. Early data indicate that IDUs in the intervention community had low levels of participation in the Expanded Syringe Access Demonstration Program (ESAP) Intervention community (population size): Harlem, NY (not reported) Comparison community (population size): South Bronx, NY (not reported) |
|
| Interventions |
Name of intervention: Harlem Expanded Syringe Access Program (ESAP) Intervention Project Theory: not reported Aim: to determine whether a multi‐level intervention would increase sterile syringe access through a new policy allowing non‐prescription syringe sales in pharmacies Description of costs and resources: not reported Components of the intervention: multi‐level, multi‐component intervention including 1‐on‐1 education, workshops/small groups/trainings, presentations and community events, and dissemination of educational materials. Target populations included community residents, pharmacists, and IDUs Start date: July 1, 2002 Duration: 1 year |
|
| Outcomes |
Outcomes and measures: utilization of new or previously used syringe at last injection, utilization of pharmacy to obtain new syringes within last 6 months Time points: Pre‐intervention data were collected from January 1, 2001, to June 31, 2002; post‐intervention data were collected from July 1, 2002, to September 1, 2004 |
|
| Notes | Intervention outreach activities were targeted to community residents, pharmacists, and IDUs. Pre‐ and post‐intervention evaluations to assess awareness, attitudes and perceptions of community members and pharmacists were also collected and reported Funding source: government and Robert Wood Johnson Foundation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized |
| Allocation concealment (selection bias) | High risk | Allocation not concealed |
| Baseline outcome measurement similar | Low risk | No statistical examination of differences between intervention and control communities was provided. However, baseline outcomes measurements appear to be similar |
| Baseline characteristics similar | High risk | No statistical examination of differences between intervention and control communities was provided. Significant differences reported in pre and post samples for age, gender, and ethnic composition. Study authors did not report that results were controlled for these baseline differences |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Independent samples immune to attrition. Pre‐ and post‐intervention response rates not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not reported |
| Protection against contamination | High risk | Contamination effect possible |
| Selective reporting (reporting bias) | High risk | Some reported questionnaire items and analysis plans not presented |
Gotay 2000.
| Methods |
Study design: controlled before‐after study Sampling frame: women age 18 or older of Hawaiian or part‐Hawaiian ancestry with a working telephone Sampling method: select every nth number with last 2 digits reversed Collection method: telephone interview (n = 678) Description of the community coalition: The Wai'anae Cancer Research Project emerged from a research collaboration between the University of Hawaii and the Wai'anae Coast Comprehensive Health Center, a community health center serving the target population. The study was headed by the medical director of the WCCHC with a policy‐making steering committee comprising representatives from the WHCHC, the University, and the Native Hawaiian community. An advisory committee of community members was formed to participate in the project |
|
| Participants |
Communities: Oahu neighborhoods with high proportion of Native Hawaiians Country: USA Ages included in assessment: 18+ Reasons provided for selection of intervention community: Native Hawaiian women had the highest mortality and lowest screening rates for breast and cervical cancer among all ethnic groups in Hawaii Intervention community (population size): Wai’anae Coast (45,000; 18,000 are Native Hawaiians) Comparison community (population size): other Oahu neighborhoods with similar proportion of Native Hawaiians (unknown) |
|
| Interventions |
Name of intervention: Wai’anae Cancer Research Project Theory: not reported Aim: to test the effectiveness of a culturally appropriate, community‐driven intervention as a means of increasing breast and cervical cancer screening practices among Native Hawaiian women Description of costs and resources: lay health educators hired, educational materials and health care vouchers provided to participants. Costs not reported Components of the intervention: 65 health‐activated support groups of 2 to 19 women; each delivered information and facilitated interaction and experience via traditional Native Hawaiian “talk story” format. Educational materials and vouchers for free mammograms and Pap tests distributed. Support group for cancer patients and a designated women’s clinic at the health center were also initiated in the intervention community during the project Start date: 1990 (funding initiated) Duration: Most support groups met twice over 2 weeks. Length of time between baseline and follow‐up survey: 3 years |
|
| Outcomes |
Outcomes and measures:
Time points: baseline (before intervention implementation) and follow‐up (3 years later) |
|
| Notes | Lay health educators were trained to provide group support and education to family and community members via “Kokua Groups” Funding source: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Intervention not randomly assigned |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | Low risk | Intervention and comparison communities displayed similar screening histories at baseline |
| Baseline characteristics similar | Low risk | Intervention community participants somewhat more likely to be married and less likely to have higher education, otherwise similar to comparison community on demographic characteristics |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 46% of women who participated in baseline survey were lost to follow‐up. Participants retained in the study tended to be older, better educated, employed, married, and in compliance with mammography screening recommendations at baseline |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | High risk | Intervention and comparison communities located on same small island (Oahu); intervention involved encouragement to share information and screening vouchers with friends |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported |
Holder 2000.
| Methods |
Study design: controlled before‐after study Sampling frame: adult population Sampling method: random‐digit dialing telephone survey Collection method: phone interviews, police incidence reports, and emergency services records Description of the community coalition: Coalition included local law enforcement officers, medical service providers, alcohol‐beverage control agents, CBO staff, community activists, parents, and youth |
|
| Participants |
Communities: 2 California communities and 1 South Carolina community, compared with similar communities that did not receive the intervention Country: USA Ages included in assessment: general public Reasons provided for selection of intervention community: Intervention sites had existing community coalitions through which the intervention could be implemented Intervention community (population size): approximately 100,000 at each site Comparison community (population size): approximately 100,000 at each site |
|
| Interventions |
Name of intervention: Community Trials Project Theory: not reported Aim: to reduce excessive drinking and related injury and violence problems Description of costs and resources: not reported Components of the intervention: (1) community mobilization; (2) community awareness; (3) responsible beverage service; (4) underage‐access law enforcement; and (5) intoxicated‐patron law enforcement Start date: 1992 Duration: 48 months |
|
| Outcomes |
Outcomes and measures: alcohol‐related traffic accidents and assaults with emergency services events Time points: time series accident data from 1988 to 1997, hospital discharge data from 1991 to 1997 |
|
| Notes | Outcomes measured at population level Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not randomly assigned communities |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | Unclear risk | Matched comparison communities |
| Baseline characteristics similar | Unclear risk | Matched comparison communities |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Data collected from state records and hospital emergency services records |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data collected from state records and hospital emergency services records |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Change in outcome assessed by population survey and public records |
| Protection against contamination | Unclear risk | Do not describe geographic proximity of control communities |
| Selective reporting (reporting bias) | Low risk | Relevant outcome data were reported |
Kagawa‐Singer 2009.
| Methods |
Study design: prospectively controlled cohort study Sampling frame: Eligible housing units were identified in neighborhood blocks or housing complexes with highest concentrations of Hmong women age 30 years and older. Every third apartment unit or house was approached Sampling method: cohort of Hmong women age 40 and older recruited by community health workers via door‐to‐door recruitment (n = 434) Collection method: in‐person survey Description of the community coalition: collaborative partnership between 4 community‐based organizations (in 4 cities) and 2 universities (California State University, Fullerton, and the University of California, Los Angeles). Participatory approach; project management position shared between 2 university and 3 community partners |
|
| Participants |
Communities: low‐income Hmong communities in urban areas of central and southern California Country: USA Ages included in assessment: women 40+ years old Reasons provided for selection of intervention community: Needs assessment found low rates of breast cancer screening knowledge among Hmong women in these cities Intervention community (population size): Fresno and San Diego, CA (not reported) Comparison community (population size): Long Beach, CA (not reported) |
|
| Interventions |
Name of intervention: Life Is Precious Theory: grounded in Social Learning Theory, behavioral skills development through modeling, and Social Support Theory Aim: to increase rates of breast cancer screening among Hmong women using a culturally and linguistically appropriate educational intervention Description of costs and resources: not reported Components of the intervention: education sessions conducted by trained Hmong health educators in culturally acceptable locations. Educational materials were prepared in Hmong language Start date: October 2000 Duration: 12 months |
|
| Outcomes |
Outcomes and measures: ever had breast self examination, clinical breast examination, or mammogram Time points: assessed at baseline and 1 year post intervention |
|
| Notes | Knowledge and attitudes were also assessed and were improved between baseline and follow‐up for both intervention and control communities Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐experimental cohort study conducted in 2 intervention cities and 1 control city, no randomization |
| Allocation concealment (selection bias) | High risk | Allocation not concealed |
| Baseline outcome measurement similar | High risk | Intervention and control groups differed in baseline rates of breast self examination, clinical breast examination, and mammogram utilization |
| Baseline characteristics similar | High risk | Significant differences in intervention and control groups for marital status, age, ability to read Hmong, ability to speak English, health insurance status |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Follow‐up of 78.6% not reported by treatment group |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants not reported |
| Protection against contamination | Low risk | Communities were located in geographically distinct areas. Control community received a similar (non‐culturally tailored educational) intervention; as such, likelihood of contamination is low |
| Selective reporting (reporting bias) | Low risk | Questionnaire described in detail |
Kelaher 2009.
| Methods |
Study design: controlled before‐after study (independent samples) Sampling frame: all children 1 to 2 years in Victoria with active maternal and child health records for breastfeeding (n = 48,533) or age 3 for MCH visit outcome Sampling method: all eligible persons included Collection method: routinely collected by maternal and child health clinics Description of the community coalition: Best Start is an area‐based initiative that provides funding to engage and support families, local services, and local government in a local partnership responsible for overseeing all phases of the project. Partnerships vary by site but must include representation of 6 essential partner groups: parents/elders, local government, health services, education services, family/community support services, and community organizations. Additional partners may include representatives from housing, law enforcement, and specialist services. Partnership must be representative of key stakeholders within the community, including Aboriginal networks and ethnic organizations where applicable. Agencies are nominated as the facilitating partner and the fund holder; a community facilitator is appointed to manage administration of the project on behalf of the partnership. The partnership is expected to establish subcommittees to accomplish its action plan |
|
| Participants |
Communities: urban and rural regions of Victoria Country: Australia Ages included in assessment: 0 to 4 Reasons provided for selection of intervention community: Sites were selected by the Department of Human Services on the basis of social and health disadvantages and lack of existing partnerships Intervention community (population size): Best Start sites (1,117,511) Comparison community (population size): the remainder of Victoria (3,536,269) |
|
| Interventions |
Name of intervention: Best Start Theory: not reported Aim: to improve the health, development, learning, and well‐being of all Victorian children age 0 to 8 years through better access to child and family support, health services, and early education; improvements in parents’ capacity, confidence, and enjoyment of family life; and communities that are more child and family friendly Description of costs and resources: Costs and resources vary by site Components of the intervention: Components of intervention vary by site and may include community outreach, peer support, education for health professionals, and established evidence‐based initiatives Start date: 2002 Duration: ongoing |
|
| Outcomes |
Outcomes and measures:
Time points: pre‐intervention (2001 to 2002) and during intervention (2004 to 2005) |
|
| Notes | Outcomes measured at the population level Funding source: Victorian government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Intervention not randomly assigned |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | High risk | Intervention sites selected for poor outcomes relative to comparison group at baseline |
| Baseline characteristics similar | High risk | Intervention sites selected for disadvantaged status relative to comparison group at baseline |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Statewide maternal child health records |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcomes derived from independent samples, statewide records |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Outcomes derived from statewide records, probably not susceptible to lack of blinding |
| Protection against contamination | Unclear risk | Comparison sites proximate to intervention sites, no protection from contamination |
| Selective reporting (reporting bias) | Low risk | Main outcomes reported |
Kelaher 2010.
| Methods |
Study design: controlled before‐after (independent samples) Sampling frame: residents of defined intervention and control areas age 18 and older Sampling method: quota samples in some areas, random in others Collection method: Peer interviewers administered in‐person surveys to intervention sample participants at community‐based sites or at home (n = 1510). Control groups were administered a truncated version of the survey over the telephone by a market research company (n = 750) Description of the community coalition: Neighbourhood Renewal (NR) is described as a complex area‐based initiative, sponsored by the Victorian Department of Human Services, in which community and local stakeholders work with the government to prepare an area‐based local action plan and oversee its implementation. At the time of the evaluation, 19 NR sites were located within Victoria’s most disadvantaged neighborhoods. Each project site is staffed by a Place Manager, a Community Development Worker, and an Employment and Learning Co‐ordinator, who guide the governing Steering Committee, a coalition of local organizations and community members with 50% resident membership. Steering committee composition varies by site and may include, for example, representatives of local schools, businesses, municipal government, non‐profit agencies, community health centers, and housing authorities |
|
| Participants |
Communities: disadvantaged and nearby neighborhoods from metropolitan regions in Victoria, Australia Country: Australia Ages included in assessment: 18+ Reasons provided for selection of intervention community: Sites were selected for intervention because when matched against the Victorian average, they showed poor performance on a range of indicators, including official unemployment rate, welfare status, average income, education, single‐parent families, crime rate, emergency admissions, child protection notifications, and concentration of public housing Intervention community (population size): 5 metropolitan NR sites in Victoria, Australia (target site populations range from 1000 to 20,000) Comparison community (population size): census districts proximate to NR sites and within the same local government area (population size not reported) |
|
| Interventions |
Name of intervention: Neighbourhood Renewal Theory: described as “top‐down resource allocation and bottom‐up decision making” Aim: to reduce inequalities between the most disadvantaged neighborhoods and the rest of the state across a range of social, educational, and health outcomes through 6 action areas: (1) increasing community pride and participation, (2) enhancing housing and environment, (3) improving employment, learning, and local economic activity, (4) decreasing crime, (5) improving health and well‐being, and (6) increasing access to services Description of costs and resources: not reported Components of the intervention: Intervention activities vary by site. Health promotion projects have included community kitchens, support groups, community gardens, park redevelopment, walking groups, school obesity prevention programs, health fairs, and oral health initiatives for young children Start date: 2001 Duration: 8 years |
|
| Outcomes |
Outcomes and measures: (1) self‐rated health (self‐reported); and (2) life satisfaction (self reported) Time points: first round (year 2 of intervention) and second round (year 4 to 5 of intervention) |
|
| Notes | Although described as a “before‐after” study, lacks true baseline measures. A larger‐scale evaluation including 15/19 Neighborhood Renewal sites has been published but lacks detailed results from each population regarding health outcomes Outcomes measured at population level Funding source: Victorian Department of Human Services |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Intervention not randomly assigned |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | High risk | “Round 1” measures of self rated health and life satisfaction higher in control than intervention sample |
| Baseline characteristics similar | High risk | Intervention samples were significantly different from control samples on all counts reported: older, more likely to be male, unemployed, with a disability, living in public housing, and with a higher proportion of migrants from non‐English speaking countries than control samples |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Independent samples ensure no “loss to follow‐up.” Response rates not reported. Methods of collecting outcome data differed between intervention and control samples |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | Unclear risk | Not commented on, but intervention and control areas were proximal |
| Selective reporting (reporting bias) | Low risk | Main outcomes reported |
| Other bias | High risk | Methods of collecting outcome data differed between intervention and control samples |
Kim 2008.
| Methods |
Study design: controlled before‐after Sampling frame: 4 rural African American Churches Sampling method: non‐random (2 churches assigned to treatment) Collection method: physical measurement Description of the community coalition: Coalition included 4 churches, non‐profit community‐based organizations, and University of North Carolina investigators |
|
| Participants |
Communities: rural North Carolina Country: USA Ages included in assessment: mean age 56 (SD 15.8) Reasons provided for selection of intervention community: rural African American at‐risk population Intervention community (population size): unknown Comparison community (population size): unknown |
|
| Interventions |
Name of intervention: Wholeness, Oneness, Righteousness, Deliverance (WORD) Theory: Stages of Change, Social Cognitive Theory, Social Support Aim: weight loss Description of costs and resources: not reported Components of the intervention: trained lay health leader in four 2.5‐hour training sessions to lead weekly small group sessions over 8 weeks as treatment (n = 61) Start date: unknown Duration: 2 months |
|
| Outcomes |
Outcomes and measures: mean weight loss (standard error) controlling for baseline BMI, education, and age Time points: baseline and 2‐month follow‐up |
|
| Notes | Funding source: coalition partners | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not randomly assigned |
| Allocation concealment (selection bias) | High risk | Not randomly assigned |
| Baseline outcome measurement similar | Low risk | Physical measurement |
| Baseline characteristics similar | High risk | Reported differences at baseline |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 20% attrition |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not randomly assigned |
| Protection against contamination | Unclear risk | Possibility of contamination not described |
| Selective reporting (reporting bias) | Low risk | Relevant outcome reported |
| Other bias | High risk | Small sample size, short follow‐up period |
Kloek 2006.
| Methods |
Study design: controlled before‐after (independent samples) Sampling frame: adults (18 to 65) residing in deprived Eindhoven neighborhoods Sampling method: random Collection method: postal survey Description of the community coalition: to tackle health inequalities in urban areas, 3 out of 10 deprived neighborhoods in Eindhoven were assigned to receive a community coalition‐led program to improve health‐related behaviors; 3 similarly deprived neighborhoods served as controls. The program Wijkgezondheidswerk (Working on Healthy Neighborhoods) was led by Municipal Health Services and included sectors from social work, social welfare, city development department, neighborhood organizations, health providers, and researchers on the coalitions. Coalitions conducted a local needs assessment, chose intervention goals, and established a neighborhood action plan that focused on healthy nutrition and physical activity, smoking cessation, and reduction of excessive alcohol consumption. 43 community activities were implemented over a 24‐month period; most health activities were led by Municipal Health Services |
|
| Participants |
Communities: Eindhoven Country: Netherlands Ages included in assessment: 18 to 65 Reasons provided for selection of intervention community: socially and economically deprived neighborhoods. Intervention community (population size): unknown Comparison community (population size): unknown |
|
| Interventions |
Name of intervention: Wijkgezondheidswerk (Working on Healthy Neighborhoods) Theory: Community Organization Theory, Transtheoretical Model of Change Aim: to reduce socioeconomic inequalities in health Description of costs and resources: Cost data were not provided. Participating organization provided staff to implement activities, and volunteers were involved in about 30% of the activities implemented Components of the intervention: nutrition projects in primary schools; information on health, nutrition, and lifestyle for adults; collaboration with the greengrocer’s shop, neighborhood walking tours, gymnastic classes, quit smoking courses, annual large community events related to health, and a monthly mailed newsletter Start date: 2000 Duration: 24 months |
|
| Outcomes |
Outcomes and measures: self‐reported daily fruit consumption, daily vegetable consumption, physical activity level, current smoking Time points: baseline and 24 months |
|
| Notes | Outcomes measured at population level Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized |
| Allocation concealment (selection bias) | High risk | Non‐randomized |
| Baseline outcome measurement similar | Low risk | Similar baseline measurements |
| Baseline characteristics similar | Unclear risk | Some significant baseline differences but adjusted in analysis |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Postal survey |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Similar attrition of 30% among intervention and control |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded |
| Protection against contamination | Unclear risk | Districts were in same city but were not adjacent |
| Selective reporting (reporting bias) | Low risk | Questionnaire items clearly described |
Koniak‐Griffin 2008.
| Methods |
Study design: control before‐after study Sampling frame: adolescent Latino couples in Los Angeles, CA Sampling method: non‐random assignment Collection method: self report questionnaire (n = 49) Description of the community coalition: University of California Los Angeles School of Nursing, in collaboration with a community–based organization (CBO) already successful in providing innovative services to adolescent fathers (the Bienvenidos Family Services National Latino Fatherhood and Family Institute (NLFFI)), developed and pilot–tested a culturally based HIV prevention program for young couples; funded by the California Collaborative Research Initiative of the University‐wide AIDS Research Program |
|
| Participants |
Communities: Los Angeles Country: USA Ages included in assessment: 14 to 23 years old Reasons provided for selection of intervention community: high proportion of Latino couples at risk for HIV/AIDS Intervention community (population size): unknown Comparison community (population size): unknown |
|
| Interventions |
Name of intervention: HIV Risk Reduction for Latino Adolescents Theory: Healing the Wounded Spirit (Tello 1998) and Gender and Power (Amaro 1995) Aim: to reduce unprotected sex among adolescent Latino couples Description of costs and resources: unknown Components of the intervention: small group sessions with HIV/AIDS education and counseling Start date: unknown Duration: 12 hours of content provided in 6 sessions |
|
| Outcomes |
Outcomes and measures: self report of rate of unprotected sex (questionnaire) Time points: baseline, follow‐up at 3 months and 6 months post intervention |
|
| Notes | Funding source: University of California | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐random assignment |
| Allocation concealment (selection bias) | High risk | Non‐random assignment |
| Baseline outcome measurement similar | High risk | Baseline risk among females lower in control group |
| Baseline characteristics similar | High risk | Differences in sociodemographic characteristics at baseline |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High number of participants not included in follow‐up data analysis |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | Low risk | Intervention offered in small groups |
| Selective reporting (reporting bias) | Low risk | Outcomes of interest described |
Krieger 2000.
| Methods |
Study design: randomized controlled trial Sampling frame: participants age 65+ with residence in targeted zip code areas Sampling method: mail recruitment from senior center membership and a marketing database Collection method: mailed surveys with telephone follow‐up for non‐respondents (n = 1083) Description of the community coalition: The Seattle Partners for Healthy Communities was established in 1995 as a Centers for Disease Control funded Urban Research Center. This was a multi‐disciplinary collaboration of community agencies, community activists, public health professionals, academics, and health providers, which had a mission to improve the health of urban, marginalized Seattle communities by conducting community‐based collaborative research. The Seattle Partners was guided by a policy‐making Board, which comprised representatives from each of the partner organizations involved and unaffiliated community residents. 12 staff persons (2 full‐time) supported the coalition. |
|
| Participants |
Communities: Central Seattle Country: USA Ages included in assessment: 65+ Reasons provided for selection of intervention community: coalition established to serve a specific racially and ethnically diverse urban community of concentrated disadvantage. Seniors targeted for low immunization rates and the importance of immunization in reducing illness, hospitalization, and death in the elderly Intervention community (population size): 5 zip codes served by Central Area Senior Center in Seattle Comparison community (population size): same |
|
| Interventions |
Name of intervention: Seattle Senior Immunization Project Theory: Health Belief Model, Social Learning Theory Aim: to test the effectiveness of a reminder and tracking system in increasing pneumococcal and influenza immunization rates among an urban senior population Description of costs and resources: Cost to senior center reported to be $14,106 for 622 members of intervention group, covering value of time for senior center staff, computer services, software, copying, and mailing. Costs did not include the value of volunteer time or of Medicare‐provided vaccines Components of the intervention: Participants received an educational brochure in the mail with a reply card to note immunization status. If card indicated no immunization, or no card was returned, participants received a call from a volunteer senior center member to encourage receipt of immunizations and to address specific barriers to immunization (peer‐to‐peer outreach) Start date: 1996 Duration: 6 weeks |
|
| Outcomes |
Outcomes and measures
Time points: baseline (September 1996) and follow‐up (March 1997) |
|
| Notes | Funding source: government | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Group assigned by systematic allocation of alternative respondents to control or intervention |
| Allocation concealment (selection bias) | High risk | Allocation determined by order of participant response, not concealed |
| Baseline outcome measurement similar | High risk | Intervention group significantly less likely to report having received an influenza vaccine the previous year (78.3% vs 83.0%) |
| Baseline characteristics similar | Low risk | Groups similar with respect to gender, age, race, education, income, and general health status. However, participants lost to follow‐up were more commonly female, with lower SES and lacking a usual source of care |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Only 23% of individuals invited to participate completed baseline survey. Approximately 13% of participants lost to follow‐up; similar loss in intervention and control groups. No intention‐to‐treat analysis performed |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to intervention group. Not stated whether interviewers were blinded to participant status |
| Protection against contamination | Unclear risk | Participants recruited from same neighborhood and senior center, with no attempt to prevent contamination |
| Selective reporting (reporting bias) | Low risk | All targeted outcomes reported |
Krieger 2005.
| Methods |
Study design: randomized controlled trial Sampling frame: Households with a child age 4 to 12 with diagnosed persistent asthma who spent at least 50% of nights there, with income below 200% of 1996 poverty threshold or child enrolled in Medicaid, English‐, Spanish‐, or Vietnamese‐speaking caregiver, in King County Sampling method: participants recruited from community and public health clinics, local hospitals and emergency departments, and referrals from community residents and agencies Collection method: in‐home interview |
|
| Participants |
Communities: King County, Washington Country: USA Ages included in assessment: 4 to 12 years Reasons provided for selection of intervention community: coalition established to serve a specific racially and ethnically diverse urban community of concentrated disadvantage Intervention community (population size): King County, WA (not stated) |
|
| Interventions |
Name of intervention: Seattle‐King County Healthy Homes Project Theory: Social Cognitive Theory and Transtheoretical Stages of Change Model Aim: to assess the effectiveness of a community health worker intervention focused on reducing exposure to indoor asthma triggers Description of costs and resources: Estimated marginal cost of high‐intensity intervention relative to low‐intensity intervention was $124,000. Hoover provided vacuums at cost, Group Health Co‐operative donated free enrollment in tobacco cessation program, and the local hazardous waste management program donated green cleaning kits and pails Components of the intervention: “high‐intensity intervention”: A community health worker conducted an initial home environmental assessment, provided individualized action plans, and made additional visits over a 12‐month period to provide education, support, materials such as low‐emission vacuums and bedding encasements), assistance with roach and rodent eradication, and advocacy for improved housing conditions. “Low‐intensity intervention”: received the initial assessment, home action plan, limited education, and bedding encasements. Start date: 1999 |
|
| Outcomes | Outcomes and measures: 1. Days with asthma symptoms/2 weeks (reported by caregiver) 2. Urgent health services use for asthma/2 months (reported by caregiver) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomization not stated |
| Allocation concealment (selection bias) | Unclear risk | Method of allocation concealment not specified |
| Baseline outcome measurement similar | Low risk | Baseline outcome measurements similar between 2 groups |
| Baseline characteristics similar | Unclear risk | Baseline characteristics similar on most factors, except high‐intensity intervention group tended to have more severe asthma than low‐intensity group |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Study group was revealed to some interviewers at exit interview |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 12% lost to follow‐up, proportion lost similar between 2 groups, and study authors state that completers were similar at baseline across intervention groups. Primary analysis included only study completers; intention‐to‐treat analysis presented in text for only 1 of 2 main outcomes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel not blinded |
| Protection against contamination | Unclear risk | None reported, unclear whether study participants from the same county would have interaction with one another |
| Selective reporting (reporting bias) | Low risk | Main study outcomes reported |
Kronish 2014.
| Methods |
Study design: RCT Sampling frame: stroke survivors receiving Visiting Nurse care or clinic‐based care, and community‐dwelling residents Sampling method: record of diagnosis of stroke or TIA in Visiting Nurse or clinic records, or community residents with self report of stroke. These were randomly assigned to treatment or wait‐list control Description of the community coalition: The East and Central Harlem Health Outcomes Community Action Board was a community‐academic partnership with a history of working together for a decade or longer. Members included community residents, stroke survivors, and community educators. Little description was provided about coalition structure, processes, or partner members beyond affiliations of study authors with Mt Sinai School of Medicine and Columbia University Medical Center. Community residents were involved in the design of PRAISE, a tailored version of Stanford University's Chronic Disease Self Management Program, and implementation of the intervention as peer educators |
|
| Participants |
Communities: Harlem and Bronx areas of New York Country: USA Ages included in assessment: adults Reasons provided for selection of intervention community: minority populations — African American and Latino — at high risk for recurrent stroke Intervention community (population size): Harlem and Bronx, population size not reported Comparison community (population size): Harlem and Bronx, population size not reported |
|
| Interventions |
Name of intervention: PRAISE (Prevent Recurrence of All Inner‐City Strokes Through Education) Theory: Appreciative Inquiry (Suchman AL 2004) Aim: "to increase the proportion of stroke and TIA survivors who achieve control of B/P, lipids, and adherence to antithrombotic medication" Description of costs and resources: no cost data provided. Study authors did state that a week‐long training course was provided to peer educators, and that they were reimbursed for providing the 6 intervention workshops (amount not disclosed) Components of the intervention: 6 workshops on stroke and risk prevention related to B/P, lipids, and medication Start date: 2009 Duration: 6 weeks with one 90‐minute session per week |
|
| Outcomes |
Outcomes and measures (follow‐up months): control of 3 stroke risk factors: B/P, lipids (LDL), and medication adherence Date (year) of pre and post measurements: Between 2009 and 2012, study participants were recruited, baseline measurements were taken, and participants were randomly assigned to treatment or wait‐list control. Intervention duration was 6 weeks. Follow‐up measurements were taken at 6 months |
|
| Notes | 301 allocated to peer education intervention 299 allocated to wait‐list control 85% f/u at 6 months Study authors state that more than half of the treatment group participated in at least 50% of the program workshops |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | After baseline measurements, participants were randomly assigned to treatment or wait‐list control |
| Allocation concealment (selection bias) | Low risk | Allocation concealed by blinded third party |
| Baseline outcome measurement similar | Low risk | No differences noted in baseline outcome measures |
| Baseline characteristics similar | Low risk | Baseline characteristics similar |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 85% follow‐up at 6‐month measurement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not reported |
| Protection against contamination | Unclear risk | Unlikely but not described |
| Selective reporting (reporting bias) | Low risk | Primary outcomes were reported |
Kruger 2007.
| Methods |
Study design: controlled before‐after cross‐sectional study (multiple time points) Sampling frame: Michigan state vital statistics Sampling method: All recorded infant mortality outcomes Collection method: state records Description of the community coalition: The Genesee County REACH 2010 partnership was established in the early 1990s with private foundation funding and continued without outside financial assistance for 3 years until Prevention Research Center and REACH 2010 grants were awarded in 1998. Partnership included the local medical center, health department, and university, and multiple community‐based organizations |
|
| Participants |
Communities: 5 Michigan counties Country: USA Ages included in assessment: infants Reasons provided for selection of intervention community: Partnership was already established in the community Intervention community (population size): Genesee County (436,000) Comparison community (population size): 4 comparison groups: Saginaw, Berrien, Oakland, Wayne Counties (population sizes not reported) |
|
| Interventions |
Name of intervention: Genesee County REACH Initiative Theory: not reported Aim: to effect community and systems change sufficient to improve local infant mortality problem, particularly the disparity in rates between African Americans and European Americans Description of costs and resources: funded at $988,968 for first year of implementation and $912,062 for subsequent years Components of the intervention: included community dialogue sessions, “Undoing Racism” workshops, university course in cultural competency, maternal/infant health advocates, and a community media campaign Start date: 2000 Duration: ongoing |
|
| Outcomes |
Outcomes and measures: infant mortality rate as measured by vital statistics data Time points: pre‐intervention (1999) and follow‐up (2005) |
|
| Notes | Funding source: government | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Intervention not randomly assigned |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | High risk | Intervention county had poorer outcomes relative to comparison counties at baseline |
| Baseline characteristics similar | High risk | Intervention county selected for disadvantaged status relative to comparison county at baseline |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | State vital statistics records |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | State vital statistics data |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | Unclear risk | Did not discuss proximity of counties |
| Selective reporting (reporting bias) | Low risk | Main outcomes reported |
Larson 2009.
| Methods |
Study design: controlled before‐after study (independent samples, multiple time points) Sampling frame: adult residents of Tennessee with working telephone Sampling method: random‐digit dial Collection method: telephone interview (n = 21,064) Description of the community coalition: The Nashville Health Disparities Coalition was formed in response to CDC's REACH 2010 funding. The lead agency was a local comprehensive health center, and other coalition organizations included local universities, county hospital, public health department, grassroots organizations, ministers, faith‐based organizations, and concerned citizens. The first 10 community members recruited became the Community Action Plan Committee, which would develop the mission and vision for the group, create bylaws, and elect officers. 4 strategy teams were created to focus on tobacco use, obesity, screening, and access to health care. Each team was staffed by a community health educator and a community outreach worker |
|
| Participants |
Communities: all Tennessee communities included in analysis, with North Nashville community as intervention group Country: USA Ages included in assessment: 18+ Reasons provided for selection of intervention community: decision based on data indicating that African American residents had significantly higher age‐adjusted death rates due to cardiovascular disease and diabetes compared with whites in the same county Intervention community (population size): North Nashville (42,000) Comparison community (population size): Tennessee State (not reported) |
|
| Interventions |
Name of intervention: Nashville REACH 2010 Initiative Theory: Social‐Ecologic Model Aim: to reduce disparities in heart disease and diabetes among African Americans in North Nashville, TN Description of costs and resources: not reported Components of the intervention: Hundreds of community actions were documented during the initiative, including changes in infrastructure such as expanded clinic hours, educational campaigns, smoking cessation classes and support groups, advocacy training to help volunteers impact smoking policy at the organizational level, health screenings, and activities to promote healthy eating and exercise Start date: 2001 Duration: 5 years |
|
| Outcomes |
Outcomes and measures
Time points: baseline (2001) and annually thereafter (2002 to 2005) |
|
| Notes | Results from the latter outcome group have not yet been published in manuscript form, and lack detailed descriptions of Methods and Results Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Intervention was not randomly assigned |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | Unclear risk | Age‐standardized proportions of smokers similar between target population and other Tennessee African Americans. No baseline data are presented for analyses of body mass index, physical activity, eating behaviors, diabetes, or heart disease |
| Baseline characteristics similar | High risk | Age and gender distributions differed significantly between target group and other Tennessee African Americans. No other characteristics compared |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Population‐based telephone survey |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Response rates declined over time(from 68% to 46%) in target population; no response rates presented for comparison group |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding reported |
| Protection against contamination | Unclear risk | No efforts to protect against contamination reported. Intervention and comparison groups within the same state |
| Selective reporting (reporting bias) | Low risk | Main outcomes are reported |
Levine 2003.
| Methods |
Study design: controlled before‐after study Sampling frame: clinic patients with hypertension Sampling method: random assignment Collection method: review of records Description of the community coalition: Sandtown‐Winchester High Blood Pressure Control Program. Johns Hopkins University and Hospital led a coalition composed of city health department, city schools, district mayor’s office, recreation, social welfare sectors, and community churches in East Baltimore, MD, USA. A needs assessment was conducted using Maryland Department of Health data, hospital discharge data, community household survey, and interviews of community leaders to establish goals and objectives |
|
| Participants |
Communities: urban, low income, 82% African American with a median age of 30, East Baltimore, MD Country: USA Ages included in assessment: adults Reason provided for selection of intervention community: high risk, African American population Intervention community (population size): 120,000 Comparison community (population size): 120,000 |
|
| Interventions |
Name of intervention: Sandtown‐Winchester High Blood Pressure Control Program Theory: Precede‐Proceed Model Aim: to control hypertension Description of costs and resources: unknown Components of the intervention: (1) information provided to the patient to clarify and reinforce components of treatment (15 min); (2) family and peer education to enhance social support (2 hours); and (3) a small group approach to enhance motivation and commitment (three 2‐hour sessions) Start date: unknown Duration: 48 months |
|
| Outcomes |
Outcomes and measures: review of health records, % with high blood pressure under control (BP < 140/90) Time points: baseline and 60 months |
|
| Notes | Source of funding: government | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Study authors state that patients were randomly assigned to treatment and control groups but do not explain the method of randomization |
| Allocation concealment (selection bias) | High risk | Allocation not concealed |
| Baseline outcome measurement similar | Low risk | At baseline, % in control of high blood pressure was similar for treatment and control groups (38% vs 41%) |
| Baseline characteristics similar | Unclear risk | Study authors do not report characteristics separately for the 2 groups |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Treatment group attrition 16% and control group attrition 30% |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding reported |
| Protection against contamination | Unclear risk | None reported |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported |
Liao 2010a.
| Methods |
Study design: controlled before‐after Sampling frame: combination of banks of telephone numbers and listed telephones (target group surnames) Sampling method: random digit Collection method: telephone survey (in‐person survey in Lowell, MA) (n = 98,206) Description of the community coalition: Study authors state that each coalition comprised a community‐based organization and at least 3 other organizations, of which 1 was a local or state health department, university, or research organization |
|
| Participants |
Communities: Los Angeles County and Orange County, CA; Santa Clara County, CA; Lowell, MA; and King County, WA Country: USA Ages included in assessment: 18 and older Reasons provided for selection of intervention community: communities with large populations of Asian Americans Intervention community (population size): unknown Comparison community (population size): unknown |
|
| Interventions |
Name of intervention: Racial and Ethnic Approaches to Community Health (REACH) Theory: Social‐Ecologic Model Aim: to reduce health disparities among targeted groups (reduction of prevalence of current smoking) Description of costs and resources: unknown Components of the intervention: Interventions included health communications campaigns and health education and promotion programs and varied among communities Start date: 2002 Duration: 60 months |
|
| Outcomes |
Outcomes and measures: prevalence of current smoking from survey data (logistic regression used to examine trends) Time points: annual risk factor surveys (2002 to 2006) |
|
| Notes | Funding source: government | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not randomized |
| Allocation concealment (selection bias) | High risk | Not randomized |
| Baseline outcome measurement similar | Low risk | Same survey |
| Baseline characteristics similar | High risk | Baseline differences noted |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Population‐based survey |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Adequately reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Telephone survey respondents were not necessarily aware of intervention, but data collectors were aware |
| Protection against contamination | Low risk | Intervention sites in different cities |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported |
Liao 2010b.
| Methods |
Study design: controlled before‐after Sampling frame: combination of banks of telephone numbers and listed telephones (target group surnames) Sampling method: random‐digit telephone survey Collection method: telephone survey (or in‐person survey in some communities) (n = 221,256) Description of the community coalition: Study authors state that each coalition comprised a community‐based organization and at least 3 other organizations, of which 1 was a local or state health department, university, or research organization |
|
| Participants |
Communities: 22 communities in 16 states Country: USA Ages included in assessment: 18 and older Reasons provided for selection of intervention community: communities focusing on cardiovascular disease or diabetes with targeted racial/ethnic groups (black, Hispanic, Asian, and American Indian/Alaskan Native) Intervention community (population size): unknown Comparison community (population size): unknown |
|
| Interventions |
Name of intervention: Racial and Ethnic Approaches to Community Health (REACH) Theory: Social‐Ecologic Model Aim: to reduce health disparities among targeted groups (increase prevalence of blood cholesterol screening) Description of costs and resources: unknown Components of the intervention: Interventions included health communication campaigns and health education and promotion programs and varied among communities Start date: 2002 Duration: 60 months |
|
| Outcomes |
Outcomes and measures: prevalence of blood cholesterol screening from survey data and relative disparity ratios compared with general population Time points: annual risk factor surveys (2002 to 2006) |
|
| Notes | Funding source: government funding | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not randomized |
| Allocation concealment (selection bias) | High risk | Not randomized |
| Baseline outcome measurement similar | Low risk | Same survey |
| Baseline characteristics similar | High risk | Baseline characteristics differed |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Population‐based telephone survey |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Population‐based telephone survey |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Telephone survey respondents not necessarily aware of intervention |
| Protection against contamination | Low risk | Interventions occurred in different cities |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported |
McPhee 2003.
| Methods |
Study design: controlled before‐after study (independent samples) Sampling frame: Vietnamese or Chinese‐Vietnamese adults age 18+ and parent of at least 1 child age 3 to 18 living in the same household Sampling method: telephone numbers of individuals with Vietnamese surnames randomly selected from area telephone books Collection method: physician or county health department contact via mail or telephone, or in person, to obtain verification of immunization status (n = 784) Description of the community coalition: Community mobilization campaign was sponsored by the Vietnamese Community Health Promotion Project, which subcontracted with the East Dallas Counseling Center to form a coalition of Vietnamese groups in Dallas. The 19 coalition members consisted of physicians, dentists, pharmacists, city and county department of public health and education officials, business leaders, veterans, seniors, teachers, researchers, parents, grandparents, homemakers, newspaper editors, and community‐based organization representatives. The coalition employed a program co‐ordinator and worked through 3 committees: advisory, planning, and outreach |
|
| Participants |
Communities: metropolitan areas Country: USA Ages included in assessment: 3 to 16 at pre‐intervention, 5 to 18 at post intervention Reasons provided for selection of intervention community: large Vietnamese‐American population that had not received interventions for hepatitis B vaccination Intervention community (population size): Dallas/Fort Worth metropolitan area (41,591 Vietnamese‐Americans) Comparison community (population size): Washington, DC, metropolitan area (38,796 Vietnamese‐Americans) |
|
| Interventions |
Name of intervention: not reported Theory: not reported Aim: to promote awareness of and responsibility for hepatitis B vaccinations of Vietnamese‐American children through families, healthcare providers, and community organizations Description of costs and resources: Costs included direct intervention costs (personnel, volunteers’ time, other operating expenses) plus vaccination costs. Prizes for children receiving vaccines and media publicity were donated Components of the intervention: The coalition promoted physicians’ registration as Vaccines for Children providers, distributed referral lists of vaccine providers and educational materials, conducted health fairs, sent targeted mailings, gave educational presentations, conducted home visits for new immigrants, worked at 2 weekly community clinics to translate and help children receive vaccines, and utilized free local media publicity. Estimated cost‐benefit ratio was 4.47:1 Start date: April 1998 Duration: 2 years |
|
| Outcomes |
Outcomes and measures: proportion of Vietnamese‐American children who had received 3 doses of HepB (%) Time points: pre‐intervention (1998) and post‐intervention (2000) |
|
| Notes | This study also included a media intervention arm in the Houston metropolitan area that was not coalition‐driven, and was not included in this review Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Intervention not randomly assigned |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | High risk | At pre‐intervention, children in the control population reported significantly higher levels of HepB immunization than children in the intervention group; baseline levels were not taken into account in the main results |
| Baseline characteristics similar | High risk | Parents of children in the control group were more likely to speak English, have more education, higher income level, health insurance, and a Vietnamese healthcare provider than parents of children in the intervention group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Independent samples were measured pre‐intervention and post intervention, and response rates were similar (93% and 92.5%. respectively). However, HepB status was reported in only 44% to 61% of each sample. The main study analysis excludes respondents with missing outcome data, and a secondary analysis codes these individuals as unvaccinated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | Low risk | No protection against contamination is noted, but study sites were separated by a large distance |
| Selective reporting (reporting bias) | Low risk | All intended outcomes appear to have been reported |
| Other bias | High risk | Characteristics of participants sampled within each group appear to vary considerably between pre‐intervention and post intervention with regard to income, insurance status, and provider ethnicity for the intervention group, and with regard to education, employment status, and provider ethnicity for the control group |
Melhuish 2010.
| Methods |
Study design: controlled prospective cohort study Sampling frame: Child Benefit Register used to identify participants in Sure Start areas, and Millennium Cohort Study used to identify controls in non‐Sure Start areas Sampling method: propensity score matched Collection method: home interviews Description of the community coalition: Sure Start partnerships were formed in response to national government funding starting in 1998 to enhance the health and development of children younger than 4 years of age and their families who live in socially deprived communities in England. These area‐based initiatives had populations, on average, of about 13,000 residents and now number over 500 sites. Sure Start guidance required programs to be planned and run by partnerships of parents, local people, voluntary and community organizations, representatives from health and local government, and others involved in improving services for young children and families. Every partnership had a lead partner acceptable to the members and accountable to receive Sure Start moneys on behalf of the partnership. Most included parents, but numbers varied and partnerships commonly included two or three parents. The size of the partnership also varied widely. Partnerships drew statutory representatives from agencies (typically practitioners) and voluntary members. Lead partners were not chosen by formal process but emerged during the planning stage. Partnerships were required to consult about the content of the Sure Start program at all stages of the planning process and throughout implementation and delivery of the plan. A program manager was appointed to see that plans were completed. Sites were given flexibility in implementing the program. Statutory agencies sometimes dominated the partnership |
|
| Participants |
Communities: targeted 20% of the most deprived areas in England (n > 500 sites) Country: England Ages included in assessment: 5‐year‐old children and parents or guardians Reasons provided for selection of intervention community: to prevent health inequalities, poverty, school failure, and social exclusion Intervention community (population size): Sure Start Local Programme areas (approximately 13,000 per site) Comparison community (population size): Millennium Cohort Study areas (similar) |
|
| Interventions |
Name of intervention: Sure Start Local Programmes Theory: not reported Aim: to enhance the health and development of children younger than 4 years of age and their families who live in socially deprived communities in England Description of costs and resources: not reported Components of the intervention: Core services consisted of outreach or home visiting; family support; support for good quality play, learning, and childcare experiences; primary and community health care; advice about child and family health and development; and support for people with special needs, including help in accessing specialized services Start date: 1999 Duration: ongoing |
|
| Outcomes |
Outcomes and measures: child BMI, child health, teacher‐rated child development, maternal depression Time points: child age 5 (some measures also completed at age 3) |
|
| Notes | Data collection for intervention and control groups not concurrent: Sure Start data were collected between June 2007 and June 2009. Millemium Cohort Study data were collected from January 2006 to March 2007. Mean differences in outcome measures were calculated as an average from 3 separate analyses, 2 with imputed missing data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | No randomization. Study used propensity score matching procedures |
| Allocation concealment (selection bias) | High risk | Allocation not concealed. Study used propensity score matching procedures |
| Baseline outcome measurement similar | High risk | Sure Start data collected from June 2007 to June 2009. Millenium Cohort data collected from January 2006 to March 2007. Outcomes not measured concurrently. Change scores incorporating baseline measures not presented for most outcomes |
| Baseline characteristics similar | Unclear risk | Propensity score matched, but groups still differed significantly with respect to race, spoken language, and household deprivation |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Study used propensity score matching procedures |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 30% of sample interviewed when participants were 3 years old were missing at 5‐year‐old assessment, but effects were averaged across 3 analyses with imputed data. Outcomes were measured by different research teams for intervention and comparison groups |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Study used propensity score matching procedures |
| Protection against contamination | High risk | Communities could be contiguous |
| Selective reporting (reporting bias) | Low risk | Protocols well documented |
Merriam 2009.
| Methods |
Study design: randomized controlled trial Sampling frame: Latino clients of Greater Lawrence Family Health Center Sampling method: randomization at household level Collection method: recruitment letter with telephone follow‐up; supplementary outreach via public access TV, Spanish radio, and bilingual newspapers. Clinic visits for anthropometric measures and blood draws for lab values; oral surveys in Spanish for diet intake, physical activity, and depression Description of the community coalition: Greater Lawrence Family Health Center (GLFHC) serving 80% of local Latino population houses a REACH diabetes project. Collaborators in study plan and implementation included family health center, Latina PI (physician at GLFHC), and Latina co‐PI from U Mass medical school, local Council on Aging/Senior Center, YWCA, and Mayor's health task force. Community co‐ordinators of project came from Lawrence Council on Aging and YWCA |
|
| Participants |
Communities: Greater Lawrence, MA area (urban) Country: USA Ages included in assessment: 25 and older Reasons provided for selection of intervention community: diabetes prevalence estimated at 11.8% among Lawrence Latino adults vs 6.4% among non‐Hispanics statewide; population of target community ˜60% Latino; target community also with high rates of poverty and limited resources Intervention community (population size): population of community not reported. Study completed 9959 telephone screening invitation calls, 2638 completed screening calls. 949 Latino clients of GLFHC assessed for eligibility, 312 enrolled, and 162 allocated to intervention Comparison community (population size): See above — 150 allocated to usual care |
|
| Interventions |
Name of intervention: Lawrence Latino Diabetes Prevention Project (LLDPP); similar to Centers for Disease Control Diabetes Prevention Program Theory: Social Cognitive Theory, Patient‐Centered Counseling Aim: To reduce risk factors for type 2 diabetes among high‐risk Latinos (those with > 30% risk of developing diabetes in next 7.5 years) Description of costs and resources: REACH project funded by CDC. First‐year costs per participant $661 Components of the intervention: provision of information in Spanish via multiple formats in 13 group sessions, provision of pedometers, 3 individual home visits for monitoring progress, cash incentives, and transportation support Start date: October 2004 Duration: 1 year |
|
| Outcomes |
Outcomes and measures: weight change, HgA1, physical activity Time points: baseline, 6 months, 1‐year follow‐up |
|
| Notes | To address low English fluency/low Spanish literacy, information presentations included video novellas, colorful food photo cards, and cooking demonstrations adapting culturally familiar foods. Significant family members were welcome to attend group sessions. Intervention fidelity was promoted through extensive training by PIs of 3 Spanish‐speaking community individuals who implemented intervention components. Study authors note that they successfully reduced the costs of the model Diabetes Prevention Program by modifying the number of sessions from 20 to 13 and by substituting less costly screening methods for glucose testing Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomized block design (at household level) |
| Allocation concealment (selection bias) | Unclear risk | Not described or stated |
| Baseline outcome measurement similar | Low risk | No significant differences |
| Baseline characteristics similar | Low risk | No significant differences |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Only blood pressure and dietary intake recall described as measured "by personnel blinded to study condition" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 94% completion rate, no significant differences between groups |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Protection against contamination | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Low risk | Main study outcomes reported |
| Other bias | High risk | Intervention "dose": Attendance at group sessions was low, dropped from 60% at 1st session to 20% at last session |
Mishra 2007.
| Methods |
Study design: cluster‐randomized controlled trial Sampling frame: women from 68 Samoan‐speaking churches in 2 southern California counties, aged > 42, who had not had a mammogram in preceding 2 years Sampling method: screening interviews by trained bilingual Samoan interviewers Collection method: pre‐test and post‐test survey (n = 776) Description of the community coalition: Coalition described as collaborative effort between National Office of Samoan Affairs and University of California at Irvine and at Los Angeles |
|
| Participants |
Communities: Samoan women in Los Angeles and Orange County, California Country: USA Ages included in assessment: women > age 42 Reasons provided for selection of intervention community: Breast cancer is the most common cancer among Samoan women; it accounts for 22% to 27% of cancers among Samoan women in Los Angeles County and Hawaii. Regional surveys show that a high percentage of Samoan women have never heard of mammography Intervention community (population size): 32 churches from sample; general population not reported; ˜45,000 Samoans reside in the 2 counties Comparison community (population size): 29 churches from sample |
|
| Interventions |
Name of intervention: Breast Cancer Education Program for Samoan Women Theory: Health Behavior Framework, Freire's Empowerment Pedagogy Aim: to increase mammogram usage among Samoan women Description of costs and resources: not reported Components of the intervention: Intervention included 3 components: culturally tailored educational booklets, skill building and behavioral exercises, and interactive group discussions led by trained bilingual Samoan lay health educators. Culturally appropriate breast cancer education booklets in English and Samoan language. Session held in churches, at Pacific Islander festival, or in private residence. Cash incentive for completing each survey Start date: July 1998 Duration: study conducted July 1998 to June 2001; recruitment, intervention, and follow‐up occurred between March 1999 and October 2000 |
|
| Outcomes |
Outcomes and measures: self reported mammogram use Time points: baseline pre‐test and 8‐month follow‐up |
|
| Notes | Funding source: government | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Churches stratified on denomination and congregation size, then randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not described |
| Baseline outcome measurement similar | Unclear risk | Baseline rates of mammogram receipt not presented for intervention or control |
| Baseline characteristics similar | Low risk | Study authors state in text:that control and intervention groups were similar on demographics and on all HBF constructs at pre‐test; data not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Interviewers were blind to study group status |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 96% of participants completed study |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Protection against contamination | Unclear risk | Not described |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported |
Moskowitz 2007.
| Methods |
Study design: controlled before‐after study (propensity score adjusted) Sampling frame: Korean surname‐based telephone lists Sampling Method: random; women age > 50 years oversampled during phase 2 Collection method: random telephone surveys in Korean and English administered by trained bilingual Korean American interviewers Description of the community coalition: collaboration between UC Berkeley Center for Family and Community Health, which is a CDC Prevention Research Center, Asian Health Services (AHS), a community clinic that provides primary care to indigent, limited‐English‐proficient Asian‐American immigrants who reside in the county, and the local Korean American Community Advisory Board (KCAB), which comprises members and leaders of the community |
|
| Participants |
Communities: women affiliated with Korean churches in Alameda County and Santa Clara County, California Country: USA Ages included in assessment: women > 18 years old (n = 876); for mammogram assessment women > 50 years old (n = 419) Reasons provided for selection of intervention community: low rates of Pap screening and mammography use among Asian Pacific Islander women in California Intervention community (population size): Alameda County (Korean American population: 14,200 in 2000) Comparison community (population size): Santa Clara County (Korean American population: 21,600 in 2000) |
|
| Interventions |
Name of intervention: Health Is Strength Theory: Precede‐Proceed model, Community Sensitive Research Aim: to improve breast and cervical cancer screening among Korean American women Components of the intervention: educational workshops; materials in Korean language, delivered by Korean American social worker and nurse; adaptation of American Cancer Society “Tell a Friend” program; financial incentives; volunteer Korean lay health advisors/church members used for recruitment and monitoring/reinforcement of health behaviors. Brochure and access‐resource lists distributed, targeted media campaign Start date: 1994 Duration: 48 months — see notes |
|
| Outcomes |
Outcomes and measures: self reported breast and cervical cancer screening change over time: Pap test, breast self exam, mammogram, clinical breast exam Time points: pre‐intervention (1994) and post intervention (2002) |
|
| Notes | Intervention duration calculated as the sum of 3 separate phases, which occurred between March 1996 and January 2002 Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | No randomization |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | High risk | Mammogram and clinical breast exam rates significantly higher in intervention group at baseline after propensity score adjustment for other characteristics; change scores compared |
| Baseline characteristics similar | Unclear risk | At pre‐intervention, “women in the two counties differed significantly on 6 of 12 sociodemographic and health care access measures”; adjustments made through propensity score analysis |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Random‐digit telephone survey |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Independent samples, response rate similar over time |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding reported, exposure to intervention assessed |
| Protection against contamination | High risk | Study authors state: “by 2002, 36% of the comparison community had some awareness of, or participation in, our community intervention” |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported |
Nguyen 2006.
| Methods |
Study design: controlled before‐after study (independent samples) Sampling frame: self identified Vietnamese, non‐institutionalized adult women with working telephone Sampling method: random samples of listed telephone numbers with 37 Vietnamese surnames Collection method: computer‐assisted telephone interview Description of the community coalition: The Vietnamese REACH for Health Initiative Coalition was convened in 1999 by the Vietnamese Community Health Promotion Project, a community–academic research organization. Original coalition members included multiple local Asian community‐based organizations, a health insurance plan, a large healthcare maintenance organization, a consortium of non‐profit community‐based health clinics, the county health department, and a society of Vietnamese physicians. One staff member from each organization attended coalition meetings, each had 1 vote, and the majority ruled |
|
| Participants |
Communities: 2 metropolitan counties with large Vietnamese communities Country: USA Ages included in assessment: 18+ (n = 2009) Reasons provided for selection of intervention community: Community‐academic partnership targeting Vietnamese population already existed in intervention county; baseline community‐wide survey of Vietnamese‐American women showed lower rates of Pap testing Intervention community (population size): Santa Clara County, CA (Vietnamese population 102,841) Comparison community (population size): Harris County, TX (Vietnamese population 58,248) |
|
| Interventions |
Name of intervention: Vietnamese REACH for Health Initiative Theory: not reported Aim: to promote cervical cancer screening among Vietnamese‐American women in Santa Clara County, CA Description of costs and resources: paid coalition members, hired lay health workers, educational materials, Vietnamese television, radio and newspaper advertising Components of the intervention: media campaign, lay health worker outreach, continuing medical education, restoration of Breast and Cervical Cancer Control Program, weekly Vietnamese Pap clinic with a patient navigator, Pap registry/reminder system Start date: 2000 Duration: 4 years |
|
| Outcomes |
Outcomes and measures: receipt of Pap test; measures: (1) ever had a Pap test, (2) had a Pap test in last year Time points: pre‐intervention (2000) and post intervention (2004) |
|
| Notes | Independent studies assessed the impact of individual intervention components (media education, lay health worker intervention) and are not included in this review Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Intervention not randomized |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | Unclear risk | Intervention population somewhat more likely to report Pap test history than control participants at baseline |
| Baseline characteristics similar | High risk | Study populations similar with respect to age, marital status, English‐speaking ability, and self reported health status. Control county participants more likely to be below poverty level and without health insurance or a regular healthcare provider. Multivariate analysis included |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No loss to follow‐up (independent samples). Lower response rate in control county at both time points |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding of participants or personnel reported. Participants asked about exposure to intervention activities during outcome assessment |
| Protection against contamination | Low risk | Study groups in different states to protect against media contamination. Participants questioned about study component exposure |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes were reported |
Nguyen 2009.
| Methods |
Study design: randomized controlled trial Sampling frame: Vietnamese American women ≥ 40 years Sampling method: random assignment Collection method: self report via telephone interview Description of the community coalition: Vietnamese REACH for Health Initiative (VRHI) coalition was led by the Vietnamese Community Health Promotion Project (VCHPP) at the University of California, San Francisco (UCSF). The other 12 members included healthcare organizations, religious organizations, and CBOs in the Vietnamese American community of Santa Clara County, California. Needs assessment was conducted, and the coalition developed a community action plan |
|
| Participants |
Communities: suburban; high concentration of Vietnamese Americans in Santa Clara County, CA Country: USA Ages included in assessment: women ≥ 40 (n = 1100) Reasons provided for selection of intervention community: Vietnamese American population with health disparities Intervention community (population size): 102,841 Comparison community (population size): 102,841 |
|
| Interventions |
Name of intervention: Lay Health Worker Outreach (LHWO) Theory: not reported Aim: to increase mammography screenings and clinical breast examinations among targeted group Description of costs and resources: Costs include media education campaign, stipends ($1500) for 50 lay health workers, and incentives ($30) for 1100 participants Components of the intervention: comparison of media education and lay health workers; both groups were exposed to targeted media education. Intervention group received 2 small group education sessions led by LHWs and 2 follow‐up telephone calls Start date: September 2004 Duration: 11 months |
|
| Outcomes |
Outcomes and measures: self report of mammography or CBE within past 2 years Time points: baseline and follow‐up at 11 months |
|
| Notes | Funding source: government | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Names of participants drawn randomly and assigned in alternating fashion to intervention or control |
| Allocation concealment (selection bias) | High risk | No concealment |
| Baseline outcome measurement similar | High risk | Intervention group had a lower baseline rate for having ever received a mammogram (84.1% vs 89.6%) and for having had 1 in the past 2 years (64.7% vs 74%) |
| Baseline characteristics similar | Low risk | No significant differences reported for baseline characteristics of groups |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Small numbers lost to follow‐up in both groups (T = 7, C = 4) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | Unclear risk | Potential for contamination not described |
| Selective reporting (reporting bias) | Low risk | Survey items clearly described and relevant outcomes reported |
Paine‐Andrews 1999.
| Methods |
Study design: controlled before‐after study Sampling frame: cross‐sectional design; behavioral change collected by school‐based survey; pregnancy data collected from state health department Sampling method: convenience Collection method: questionnaire (Adolescent Curriculum Evaluation, Youth Risk Behavior Survey), archival records from state health department Description of the community coalition: Geary County: county school district in affiliation with community mobilizers, student interns from nearby university. Coalition included advisory board, financial sustainability committee. Franklin County: satellite office for regional drug and alcohol prevention center, community mobilizers, advisory board. Wichita: grassroots community organization (Wichita Metropolitan Family Preservation), high schools, community mobilizers, advisory board |
|
| Participants |
Communities: 3 communities in Kansas: Geary County, Franklin County, and Wichita County: USA Ages included in assessment: questionnaire(s) administered to 7th graders; state health department data for teens age 14 to 17 (n = 1769) Reasons provided for selection of intervention community: communities chosen on the basis of minority populations, SES, and high teen pregnancy rates Intervention community (population size): Franklin County (22,000), Geary County (30,353), Wichita County (304,000) Comparison community (population size): similar Kansas county |
|
| Interventions |
Name of intervention: School/Community Sexual Risk Reduction Replication Initiative (replication of the School/Community Model for Preventing Adolescent Pregnancy) Theory: Social Learning Theory, Innovation Diffusion Theory Aim: to determine effects of a comprehensive multi‐component school‐ and community‐based intervention on unintended pregnancy among never‐married teens and pre‐teens by promoting abstinence, postponing age of first intercourse, and promoting effective contraceptive use Description of costs and resources: Kansas Health Foundation; 3‐year grants of $150,000 per year for 3 communities Components of the intervention: enhancing sexuality education (for teachers, community members, parents, clergy), implementing age‐appropriate comprehensive K‐12 sexuality education, increasing access to health services and contraceptives, using mass media to increase awareness and involvement, providing peer support and education, and establishing linkages with communities and religious organizations Start date: 1993 Duration: 4 years |
|
| Outcomes |
Outcomes and measures: proportion of adolescents having sex, condom use, pregnancy rate, birth rate Time points: pre‐intervention data: 1991 to 1993; intervention data: 1994 to 1996 |
|
| Notes | Funding source: Kansas Health Foundation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomization not performed |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | Unclear risk | Process used to select counties or zip codes with similar pregnancy rates using 5‐year estimated pregnancy rates |
| Baseline characteristics similar | High risk | Variation between target areas described, but not in detail |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | School‐wide surveys and state vital statistical data |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Response rates to ACE and YRBS surveys between 68% and 73% |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding reported |
| Protection against contamination | High risk | Intervention and comparison target areas were geographically close. Given community‐level interventions, contamination is possible/likely |
| Selective reporting (reporting bias) | Unclear risk | Study authors report specific outcomes from large behavioral risk survey |
Paradis 2005.
| Methods |
Study design: prospectively controlled cohort Sampling frame: all elementary school children in study communities in grades 1 through 4 at baseline Sampling method: All children with written consent from parent/guardian were included Collection method: anthropomorphic measurements and run/walk tests administered by researchers; lifestyle questionnaires filled out by parents for participants in grades 1 through 3 and self administered for participants in grades 4 through 6 Description of the community coalition: The Kahnawake Schools Diabetes Prevention Project (KSDPP) was initiated by community leaders and was described as a partnership of the Kanien’keha:ka (Mohawk) community of Kahnawake with community‐based researchers and academic researchers working co‐operatively and collaboratively in the design, implementation, analysis, interpretation, conclusion, reporting, and publication of experiences of the project. During phase 1 of the project, the partnership included KSDPP staff (diabetes prevention facilitators and trainers, secretarial and administrative support staff, and researchers from the community or outside the community), a Community Advisory Board, academic researchers, and community researchers. The Community Advisory Board consisted of 40 members from the health, educational, political, recreational, social, spiritual, economic, and private sectors. KSDPP decisions were supported by a collective decision‐making process that involved representation from multiple partner groups |
|
| Participants |
Communities: 2 native Mohawk territories southwest of Montreal Country: Canada Ages included in assessment: 6 to 11 years of age (n = 641) Reasons provided for selection of intervention community: Community leaders and elders requested a prevention program to address high observed rates of NIDDM and complications in adults, as well as a perceived increase in obesity among children Intervention community (population size): Kahnawake (6746) Comparison community (population size): Tyendinaga (2200) |
|
| Interventions |
Name of intervention: Kahnawake Schools Diabetes Prevention Project (KSDPP) Theory: Social Learning Theory, Precede‐Proceed model Aim: to decrease the incidence of NIDDM by increasing physical activity and healthy eating and reducing obesity among children age 6 to 12 years, while incorporating Mohawk traditions and fostering community empowerment and ownership Description of costs and resources: not provided Components of the intervention: A culturally appropriate elementary school‐based health education program with complementary school and community activities, such as school walking programs, nutrition policy promotion, parent‐sponsored dining events, media campaigns, and a 2‐day community diabetes conference. Altogether more than 60 activities aimed at children, teachers, families, and the community were implemented during phase 1 Start date: 1994 Duration: 24 months |
|
| Outcomes |
Outcomes and measures
Time points: baseline (1994) and follow‐up (1996) |
|
| Notes | Ownership of KSDPP has evolved over time, but the description of the coalition herein refers to the project as organized in phase 1 (1994 to 1997), during the comparative evaluation time frame Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | No randomization performed |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | High risk | At baseline, intervention group had somewhat lower measures of body fatness and higher measures of physical activity; nutrition indices were similar |
| Baseline characteristics similar | Unclear risk | Agreement with participating nations stipulated that no direct comparisons of raw data would be made; no baseline characteristics were reported |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Numbers of participants and losses to follow‐up not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | Unclear risk | Communities were 200 miles apart, but no other reported attempt was made to prevent contamination |
| Selective reporting (reporting bias) | Low risk | Range of body composition, nutrition, and physical fitness results presented |
Parikh 2010.
| Methods |
Study design: randomized controlled trial Sampling frame: community members with pre‐diabetes referred from primary care clinicians and recruited at community organizations Sampling method: participants randomly assigned to intervention or delayed intervention (control) arm via blocked randomization (n = 178) Collection method: biometric data, questionnaires, self report of behavior change Description of the community coalition: Community Action Board, composed of 20 leaders, activists, and residents of East Harlem |
|
| Participants |
Communities: East Harlem, NY Country: USA Ages included in assessment: > 18 Reasons provided for selection of intervention community: East Harlem comprises the poorest and most obese population in Manhattan; this population has the highest prevalence of diabetes and mortality rates in the city Intervention community (population size): not reported Comparison community (population size): same |
|
| Interventions |
Name of intervention: Project HEED (Help Educate to Eliminate Diabetes) Theory: Self Efficacy Theory Aim: to measure the effectiveness of a peer‐led lifestyle intervention in promoting weight loss among overweight adults with pre‐diabetes in East Harlem Description of costs and resources: not reported. Components of the intervention: peer‐led intervention to promote weight loss and prevent diabetes; social marketing Start date: July 2007 Duration: February 2008 |
|
| Outcomes |
Outcomes and measures: weight, blood pressure, health behaviors Time points: baseline (intervention n = 50, control n = 49), 3, 6, 12 months (12‐month intervention: n = 35; control: n = 37) |
|
| Notes |
Funder: National Center on Minority Health and Health Disparities and the New York State Department of Health Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants randomly assigned using blocked randomization |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | Low risk | No statistically significant differences between groups for anthropometric measures or behaviors |
| Baseline characteristics similar | Low risk | No statistically significant differences between groups for demographic characteristics |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition: 23 of 83 participants lost to follow‐up at 12 months; employed last‐observation‐carried‐forward strategy to impute missing weights at follow‐up |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding reported |
| Protection against contamination | High risk | Likelihood of contamination high; participants in intervention and control groups live in same community |
| Selective reporting (reporting bias) | Low risk | Primary outcome of weight loss was reported |
| Other bias | Unclear risk | Not powered to detect changes in diet or physical activity as measured by questionnaire&& |
Parker 2008.
| Methods |
Study design: randomized controlled trial Sampling frame: households in southwest or eastside Detroit with children age 7 to 11 with persistent asthma Sampling method: questionnaires mailed to all caregivers of children age 7 to 11 who attended 1 of 44 elementary schools in neighborhoods; for households with more than 1 eligible child, the child with the most severe symptoms was chosen. Participants participating in baseline assessment were randomly assigned to intervention or control group Collection method: asthma screening questionnaire, measurements of lung function Description of the community coalition: partnership with Detroit Community‐Academic Urban Research Center (URC); community‐based participatory research (CBPR) with steering committee composed of representatives of 8 community‐based organizations, a health service agency, a state agency, an academic institution, and community members |
|
| Participants |
Communities: eastside and southwest Detroit, MI Country: USA Ages included in assessment: children age 7 to 11 (n = 298) Reasons provided for selection of intervention community: high rates of African American and Latino residents; statistics demonstrating high rates of asthma hospitalization, high rates of poverty, pre‐existing efforts to address health concerns, and pre‐existing relationships Intervention community (population size): 165,000 Comparison community (population size): same |
|
| Interventions |
Name of intervention: Community Action Against Asthma (CAAS) Theory: Empowerment and Social Cognitive Theory Aim: to improve children’s asthma‐related health by reducing household environmental triggers for asthma through activities delivered by community health workers (CHWs) Description of costs and resources: not provided Components of the intervention: community health worker home visits (> 9/y). CHWs provided tailored information, strategies, methods, and materials to reduce environmental triggers, as well as referral to medical treatment and/or other social services (e.g. food bank) (intervention group: n = 162; control group: n = 166) Start date: 2000 Duration: 12 months |
|
| Outcomes |
Outcomes and measures: lung function (daily nadir forced expiratory volume, daily nadir peak flow), asthma symptoms (cough that will not go away, coughing with exercise), unscheduled medical visits, use of asthma controller medications Time points: 1‐year follow‐up |
|
| Notes |
Funder: National Institute for Environmental Health Sciences and the US Environmental Protection Agency Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator used for randomization |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Baseline outcome measurement similar | High risk | Unscheduled medical care and uncontrolled symptoms higher in intervention group at baseline; P values not provided |
| Baseline characteristics similar | Low risk | Intervention and control groups showed no significant differences with regard to baseline characteristics |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 25% attrition rates did not differ between intervention and control |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding performed |
| Protection against contamination | Unclear risk | Cases and controls lived in close geographic proximity and attended the same schools |
| Selective reporting (reporting bias) | Low risk | Main outcomes reported |
Plescia 2008.
| Methods |
Study design: controlled before‐after study Sampling frame: residents of 14 neighborhoods in Charlotte, NC Sampling method: random samples of intervention and control populations Collection method: behavioral risk factor survey Description of the community coalition: The Charlotte REACH coalition grew out of a national funding program (REACH 2010) to address health disparities in minority communities. The Charlotte REACH coalition included community members, community grassroots organizations, community health center, neighborhood association, county health department, a community‐based substance abuse program, and other community service providers. Health disparities were identified, and cardiovascular disease and diabetes were identified as priorities. Decisions were made by consensus, with an external consultant providing mediation |
|
| Participants |
Communities: 14 neighborhoods in Charlotte, NC Country: USA Ages included in assessment: adults (n = 3738) Reasons provided for selection of intervention community: predominantly urban, low‐income African American communities with high risk for cardiovascular disease and diabetes Intervention community (population size): 19,670 Comparison community (population size): not reported |
|
| Interventions |
Name of intervention: Charlotte REACH Theory: Social‐Ecologic Model Aim: to reduce behavioral risk factors for cardiovascular disease and diabetes Description of costs and resources: not described Components of the intervention: (1) increasing community resources to remove barriers to healthy behavior; (2) improving quality of care at health center; (3) initiating campaign to change social norms; and (4) engaging in political advocacy for evidence‐based policy interventions Start date: 2001 Duration: 60 months |
|
| Outcomes |
Outcomes and measures
Time points: 2001 (baseline) and 2005 (follow‐up) |
|
| Notes | Funding source: government | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | No randomization |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | High risk | Intervention group less likely to be physically active and more likely to be smokers at baseline |
| Baseline characteristics similar | Unclear risk | Women and older age groups better represented in intervention group |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Population‐based survey |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Independent samples imply no attrition; response rates stable over time (63% to 69%) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | Unclear risk | Contamination not addressed; intervention and control within same state |
| Selective reporting (reporting bias) | Unclear risk | Unclear how 3 outcomes were chosen from 60 survey questions |
Rhodes 2009.
| Methods |
Study design: controlled before‐after study Sampling frame: 30 Latino soccer teams in central North Carolina Sampling method: data collected from random sample of teammates from intervention and control teams Collection method: questionnaire administered by staff member Description of the community coalition: Chatham Communities In Action (CCIA) is a partnership between the local Latino community, local health organizations, religious organizations, Latino‐serving CBOs, advocacy groups, the local public health department, and academic institutions conducting community‐based participatory research |
|
| Participants |
Communities: 30 Latino soccer teams in central North Carolina Country: USA Ages included in assessment: > 18 years of age (n = 222) Reasons provided for selection of intervention community: population of recently arrived, non‐English‐speaking Latino men in central North Carolina, a region of the USA with a quickly growing Latino population and disproportionately high rates of HIV and STD infection Intervention community (population size): Chatham County — 55,000 Comparison community (population size): not reported |
|
| Interventions |
Name of intervention: HoMBRes (Hombres Manteniendo Bienestar y Relaciones Saludables) Theory: Social Cognitive and Empowerment Theory Aim: to reduce risk of HIV and STD infection among Latino migrant and seasonal farmworkers through increased condom use and increased counseling, testing, and treatment for HIV and STDs Description of costs and resources: not reported Components of the intervention: selection and training of members of local soccer teams as pilot lay health advisors (LHAs) to reduce HIV and STD infection among recently arrived, non‐English‐speaking Latino men; creation of HoMBRes training and resources manuals Start date: October 2003 Duration: 18 months |
|
| Outcomes |
Outcomes and measures: condom use, HIV testing, behavior, knowledge of HIV transmission Time points: baseline, 18‐month post‐Navegante training |
|
| Notes | Members of control teams were offered intervention when study was completed Funder: US Centers for Disease Control and Prevention Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | No randomization |
| Allocation concealment (selection bias) | High risk | Allocation concealment not reported |
| Baseline outcome measurement similar | Unclear risk | Baseline measurement not reported separately for intervention and control groups |
| Baseline characteristics similar | Low risk | No statistically significant differences between intervention and control participants’ sociodemographic characteristics (P > 0.05 for all) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Independent samples imply no attrition |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not reported |
| Protection against contamination | Low risk | Teams chosen from geographically and socially distinct areas to minimize contamination |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported |
Rhodes 2011.
| Methods |
Study design: cluster RCT Sampling frame: adult Latino males in rural central North Carolina Sampling method: random; participants recruited from community locations frequented by Latinos Description of the community coalition: community‐based participatory research partnership of more than 50 members located mainly in northwest and central North Carolina. Members represent the lay community, including African American/black, Latino, and white gay men; organizational representatives; and academic researchers. Partnership has numerous studies ongoing |
|
| Participants |
Communities: rural central North Carolina Country: USA Ages included in assessment: 18+ (n = 139) Reasons provided for selection of intervention community: Latinos in USA disproportionately affected by HIV/AIDS, North Carolina has one of the fastest growing Latino populations Intervention community (population size): rural central North Carolina (unknown) Comparison community (population size): rural central North Carolina (unknown) |
|
| Interventions |
Name of intervention: HoMBReS‐2 (Hombres Manteniendo Bienestar y Relaciones Saludables‐2) Theory: Social Cognitive and Education Empowerment Aim: to test the efficacy of a small‐group HIV prevention intervention regarding condom use and HIV testing behavior Description of costs and resources: not provided Components of the intervention: 2 small group sessions involving trust‐building activities, didactic teaching, DVD modules, role plays, and group discussion, as well as skills building, practice, and feedback Start date: not provided Duration: 2 sessions |
|
| Outcomes |
Outcomes and measures (follow‐up months)
Years of pre and post measurements: not provided |
|
| Notes | Participants entered the study and were randomly assigned in waves to avoid delays between recruitment and intervention delivery. Unclear why missing outcome data appear extensive | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization occurred in waves; each participant selected an envelope from a discrete pool of assignments during each wave |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | High risk | Consistent condom use much greater in intervention group (34.7%) than in control group (21.4%) at baseline |
| Baseline characteristics similar | Unclear risk | Intervention group significantly younger; all other presented characteristics appeared similar |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Very low rate of loss to follow‐up reported, but final outcome measures show extensive missing observations |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | High risk | No protection against contamination was detailed; 6 participants attended the incorrect intervention arm |
| Selective reporting (reporting bias) | Low risk | Main outcomes reported |
Rothman 1999.
| Methods |
Study design: controlled before‐after study (independent samples) Sampling frame: children age 6 years of age and younger living in predominantly African American census tracts in Philadelphia Sampling method: not clearly stated, but appears to be associated with where children were brought for blood lead level testing (self selection). Control census tracts matched by demographics and housing older than 1950 Collection method: elevated blood lead levels reported to the City of Phildelphia Description of the community coalition: The coalition was formed to address lead awareness in North Central Philadelphia; it originated from a pre‐existing community‐academic partnership. The group was convened by the City Lead Poisoning Prevention Program and the Temple Health Connection, a community‐based academic nursing practice, and included the Department of Health, a university, the local housing authority, community residents, the Salvation Army, and other grassroots community‐based organizations |
|
| Participants |
Communities: Philadelphia neighborhoods with a high proportion of residents who were African American and below the poverty level, with a high proportion of housing built before 1950 Country: USA Ages included in assessment: ≤ 6 years old (n = 890) Reasons provided for selection of intervention community: Targeted neighborhood was economically disadvantaged, underserved, and at risk because of lead in the environment Intervention community (population size): 4 census tracts of North Central Philadelphia (population size not reported) Comparison community (population size): 4 additional census tracts within Philadelphia that matched as closely as possible the experimental population on % housing built before 1950, % African American, and % below poverty level (population size not reported) |
|
| Interventions |
Name of intervention: Lead Awareness: North Philly Style Theory: not reported Aim: to implement and evaluate community‐developed, community‐based strategies that address childhood lead poisoning Description of costs and resources: after‐school and camp programs with a focus on lead education provided for children through participating agencies. ‘Block captains’ who were residents of the targeted community invited neighbors to block parties and provided educational materials, lead remediation materials, and gifts. Cost data not reported Components of the intervention: educational after‐school programs and camps for children; informational “block parties” in local churches and recreation centers for adults, with educational materials and free lead‐remediation materials Start date: 1997 Duration: 3 years |
|
| Outcomes |
Outcomes and measures: change in elevated blood lead levels (> 10 micrograms/Dl) in children (proportion of blood lead levels over certain thresholds) (f/u intervention: n = 360; comparison: n = 530) Time points: baseline (1997) and follow‐up (3 years later) |
|
| Notes |
Funder: US National Institute for Nursing Research Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Intervention not randomly assigned |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | Unclear risk | Outcome (proportion above lead level cutoff) shifted during study and baseline levels not presented with final results |
| Baseline characteristics similar | High risk | Control census tracts matched on housing built before 1950, % African American, and poverty, with some differences evident |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Mandatory reporting of elevated blood lead levels to City of Phildelphia. Objectively measured outcome should not be affected by lack of blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Completeness of reporting elevated blood lead levels to City of Phildelphia not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Objectively measured outcome should not be affected by lack of blinding |
| Protection against contamination | Unclear risk | No statement regarding protection against contamination. Proximity of experimental and control census tracts unclear |
| Selective reporting (reporting bias) | High risk | Exact results for blood lead level ≥ 20 described in initial paper as main outcome variable reported only in brief; no statistical testing provided |
Saxe 2006.
| Methods |
Study design: controlled cross‐sectional before‐after study Sampling frame: adults age 16 to 44 years and living in experimental and control communities Sampling method: random‐digit dial population survey Collection method: telephone interview Description of the community coalition: Robert Wood Johnson Foundation’s Fighting Back program to prevent and control drug and alcohol abuse. Community coalitions were established at each site and involved local political, business, and grassroots leaders. Community leaders chose, developed, and implemented strategies with autonomy, thus sites differed in their approaches |
|
| Participants |
Communities: 41 communities in sections of the following US cities: Washington, DC, Santa Barbara, Vallejo, Little Rock, New Haven, San Antonio, Kansas City, Milwaukee, Columbia, Charlotte, Newark, and Worcester. On average, sites were more urban, more African American, and poorer than the USA at large Country: USA Ages included in assessment: 16 to 44 years old (n = 2804) Reasons provided for selection of intervention community: Targeted neighborhoods were economically disadvantaged with higher rates of drug and alcohol problems Intervention community (population size): Area represented by each coalition ranged from 100,000 to 250,000 residents, typically portions of cities Comparison community (population size): communities similar in size and demographics within the same city as the intervention community |
|
| Interventions |
Name of intervention: Fighting Back Theory: not reported Aim: to develop a comprehensive system of prevention, treatment, and aftercare for substance abuse Description of costs and resources: Communities received, on average, US $3 million over a 5‐year implementation period to bring coalition groups together, hire staff, and develop a plan for interventions Components of the intervention: broad‐based community initiatives, including public awareness, prevention targeted at youth, early identification of substance abuse problems, and treatment and relapse prevention Start date: 1995 Duration: 4 years |
|
| Outcomes |
Outcomes and measures: use of any illicit drug, heroin use within 12 months, daily marijuana use Time points: baseline (1995) and follow‐up (4 years later) |
|
| Notes | Funding source: government | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Intervention was not randomly assigned |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | Low risk | Baseline measures were similar in control and intervention groups |
| Baseline characteristics similar | Low risk | Reported baseline characteristics were similar in control and intervention groups |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Population‐based telephone survey |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Random‐digit dial population survey with large sample size |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | Unclear risk | No statement regarding possibility for contamination |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported |
Schorling 1997.
| Methods |
Study design: prospective controlled cohort Sampling frame: Street segments were identified from US Census blocks with at least 50% African American residents and at least 10 African American adults Sampling method: Every household on identified street segments was screened for the presence of 1 or more black adults and was rostered for denominator data on smoking prevalence Collection method: in‐person interview Description of the community coalition: The Buckingham Health Education Board was assembled by a county co‐ordinator hired by the academic researchers. Coalition members were African American and included both volunteer lay persons and clergy. Assistance was offered to the coalition to deal with any health issues of concern, with the provision that smoking cessation must be included |
|
| Participants |
Communities: 2 rural Virginia counties Country: USA Ages included in assessment: 18+ (n = 452) Reasons provided for selection of intervention community: African Americans have higher smoking‐attributable morbidity and mortality than Caucasians, despite data suggesting higher attempted quit rates. In the rural South, a high percentage of the population is African American, and services for smoking cessation are scarce Intervention community (population size): Buckingham County, VA (11,926) Comparison community (population size): Louisa County, VA (20,325) |
|
| Interventions |
Name of intervention: Alliance of Black Churches Health Project Theory: Community Empowerment and Transtheoretical Stages of Change Model Aim: to determine if smoking cessation interventions delivered through a coalition of black churches would increase the smoking cessation rate of church members exposed to the intervention and among African Americans community‐wide Description of costs and resources: none stated Components of the intervention: Smoking cessation counselors were trained by participating churches to deliver advice and counseling to individuals interested in quitting. Smoking cessation devotional booklets were distributed through churches, county‐wide Gospel Quit Nights were held every 6 months, and annual county‐wide smoking cessation contests and in‐school poster and essay contests were held Start date: 1991 Duration: 18 months |
|
| Outcomes |
Outcomes and measures: smoking cessation. Measure: self reported continuous abstinence (zero cigarettes smoked in the past month) ascertained by in‐person household survey Time points: baseline: n = 648; follow‐up (18 months later): n = 453 |
|
| Notes | A separate coalition was organized in the control to address hypertension, diet, and exercise. Smoking was not addressed by any coalition activities in this county Funder: US National Heart, Lung, and Blood Institute Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | From 2 pre‐selected counties, selection of a county to receive smoking cessation intervention was “arbitrary” |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | Unclear risk | After standardization for age distribution, gender‐specific smoking prevalence was similar between intervention and control counties, but no statistical testing was reported |
| Baseline characteristics similar | High risk | Most participants in intervention and control counties were similar at baseline, but those in the intervention county started to smoke at a significantly younger age on average than participants in the control county |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blinded. Presumably, study interviewers were aware of intervention allocation, as it was determined by place of residence |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Thirty percent of participants were lost to follow‐up, and these individuals exhibited significant differences from those remaining in the study. However, the attrition rate was similar between study groups, and, according to study authors, no significant between‐county differences were observed in the characteristics of retained study participants. Study author performed secondary analysis with conservative assumption for losses to follow‐up |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants were not necessarily aware of the coalition intervention |
| Protection against contamination | High risk | Intervention and control counties were in relatively close proximity. 9.4% of control population reported hearing about the intervention program |
| Selective reporting (reporting bias) | Low risk | Relevant outcome was reported |
Spencer 2011.
| Methods |
Study design: randomized controlled trial Sampling frame: medical facility records of physician‐diagnosed type 2 diabetes, self identified as African American or Latino, living in target zip codes Sampling method: medical record review Collection method: laboratory data, survey Description of the community coalition: REACH Detroit Steering Committee. Composed of community health leaders, clinical providers, researchers, and REACH Detroit staff |
|
| Participants |
Communities: southwest Detroit, eastside Detroit Country: USA Ages included in assessment: > 18 years old (n = 164) Reasons provided for selection of intervention community: communities with predominantly Latino or African American populations with low average income who are historically underserved Intervention community (population size): not reported Comparison community (population size): not reported |
|
| Interventions |
Name of intervention: REACH (Racial and Ethnic Approaches to Community Health) Detroit Initiative Theory: Empowerment Theory Aim: to determine whether a culturally tailored community health worker (CHW) intervention for diabetes self management improves HbA1c levels, blood pressure, lipid levels, diabetes knowledge, diabetes self management behavior, and diabetes‐related distress amongst low‐income, inner city African Americans and Latinos with diabetes Description of costs and resources: cost information not provided Components of the intervention: trained community health workers (“family health" advocates) conducted diabetes education classes and tailored home visits and a clinic visit with patient and care provider; both intervention and control groups had access to REACH community activities (healthy eating, physical fitness, farmers' markets) and received health care at facilities with trained REACH healthcare providers Start date: September 2004 Duration: 22 months |
|
| Outcomes |
Outcomes and measures: physiological measures (HbA1c, LDL, BP), self management knowledge, diabetes self efficacy, physical activity, dietary practices Time points: baseline and 6 months (f/u intervention: n = 58; control: n = 69) |
|
| Notes |
Funder: US Centers for Disease Control and Prevention Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random sequence generation not reported |
| Allocation concealment (selection bias) | High risk | Allocation concealment not described |
| Baseline outcome measurement similar | Low risk | Baseline HbA1c similar |
| Baseline characteristics similar | Low risk | Intervention group was significantly younger than control; this was controlled for in the data analysis |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | All measured outcomes appear to be reported. Laboratory data were not available for a significant percentage of those initially enrolled. However, ITT analysis was performed |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding reported |
| Protection against contamination | High risk | Not stated. Because interventions occurred in the same communities, likelihood of contamination is high |
| Selective reporting (reporting bias) | Low risk | All measured outcomes appear to be reported |
| Other bias | Unclear risk | Modest sample size may limit power; laboratory test results obtained through medical chart reviews |
Stafford 2008.
| Methods |
Study design: prospective controlled cohort Sampling frame: residents age 16 or older in 39 New Deal community areas in England, and residents in comparator areas matched on deprivation score and local authority Sampling method: random sample household survey of residents of New Deal communities age 16 or older. A similar household survey was carried out in deprived but not New Deal neighborhoods. At 2‐year follow‐up, surveys were repeated and a longitudinal panel of respondents resulted. In total, 10,390 previously interviewed New Deal site respondents were interviewed again in 2004 (73%). Among residents surveyed in comparison communities, 977 (72% of baseline) were interviewed Collection method: in‐person interview Description of the community coalition: New Deal program was launched in 1998 with the aim of reducing the gap between deprived neighborhoods and the rest of England through community‐led partnerships in 39 neighborhoods. Partnerships received about £50 million over 10 years. Each partnership had to create its own operating and governance procedures and systems for financial management and monitoring; also had to hire staff, decide on the role and composition of multi‐sector boards, and appoint or elect boards. Many were incorporated as companies |
|
| Participants |
Communities: 39 deprived neighborhoods in London, in Birmingham, and across England Country: England Ages included in assessment: 16+ (n = 11,367) Reasons provided for selection of intervention community: areas of high socioeconomic deprivation Intervention community (population size): Each New Deal site had a population of approximately 9800 residents Comparison community (population size): similar size |
|
| Interventions |
Name of intervention: New Deal for Communities Program Theory: area‐based regeneration Aim: to reduce gaps between the poorest neighborhoods and the rest of the country through a 10‐year strategic transformation of neighborhoods and local agencies Description of costs and resources: £50 million over 10 years per site Components of the intervention: Each New Deal site chose its own 10‐year targets and delivered a different set of interventions aimed at improving the environment, crime, education, employment, and health Start date: 1998 Duration: 10 years |
|
| Outcomes |
Outcomes and measures: self rated health status, SF‐36 mental health, smoking status, satisfaction with local area Time points: baseline (2002) and follow‐up (2004) |
|
| Notes | Funding source: government | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not randomized |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | Low risk | Similar baseline outcome measures |
| Baseline characteristics similar | Low risk | Participants in intervention and control areas similar |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Study interviewers were aware of intervention allocation, as it was determined by place of residence |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 30% of longitudinal cohort members lost to follow‐up in consecutive surveys |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants were not necessarily aware of the coalition intervention |
| Protection against contamination | Unclear risk | Intervention and control communities were in relatively close proximity |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes were reported |
Thompson 2006.
| Methods |
Study design: cluster‐randomized trial Sampling frame: residents of 20 communities in Yakima Valley Sampling method: census data used to over‐sample Hispanic households; every household in small census group was sampled; otherwise households were randomly selected Collection method: cross‐sectional survey, in‐person interviews by trained bilingual project staff Description of the community coalition: Community Advisory Boards were recruited from each of the 10 intervention sites to run projects (content of questionnaires, types of activities that would be done, staff to be hired, types of screening to target, cultural appropriateness of different intervention activities, implementation of activities). CABs consisted of 18 to 24 Hispanic and non‐Hispanic white community members representing a like number of organizations |
|
| Participants |
Communities: rural agricultural communities in Yakima Valley, Eastern Washington Country: USA Ages included in assessment: adults > 18 years (n = 916), except women > 40 for mammogram (n = 103); adults 50 years or over for colorectal screening (n = 180) Reasons provided for selection of intervention community: increased risk of cancer among Hispanics due to smoking and dietary intake; higher cancer mortality due to screening behaviors Intervention community (population size): 10 Yakima Valley communities (ranging in population from 300 to 7000 each) Comparison community (population size): 10 matched Yakima Valley communities plus 3 Columbia Basin communities (ranging in population from 300 to 7000 each) |
|
| Interventions |
Name of intervention: Celebremos La Salud Theory: Community Organization Aim: to increase cancer prevention activities including screening behaviors, dietary intake, and smoking cessation among Hispanic and non‐Hispanic residents of Yakima Valley Description of costs and resources: not reported Components of the intervention: comprehensive multi‐level intervention including distribution of informational materials at community events, worksites, and clinics; group education sessions; home “health parties” with project interventionist; wellness van; free or reduced screenings at local clinics; use of trained volunteer “promotoras” to discuss cash incentives for participation Start date: March 2003 Duration: 30 months |
|
| Outcomes |
Outcomes and measures: cancer screening behaviors; % compliant with screening recommendations (Pap smear, mammogram, fecal occult blood, colonoscopy); dietary intake (fruit and vegetables, fat); smoking (current, ever, never) Time points: baseline and post intervention (timing unclear) |
|
| Notes | Results stratified by ethnicity, shown for Hispanic only. Separate cohort of 823 individuals > 50 years of age, non‐compliant with colorectal screening at baseline, re‐interviewed at final survey — cohort members in intervention communities no more likely than those in control communities to have ever had or recently had screening Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of within‐pair randomization not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Baseline outcome measurement similar | Unclear risk | Not presented, but final rates adjusted for baseline |
| Baseline characteristics similar | Low risk | Study authors state: “at baseline, there were no significant differences between communities by treatment arm” |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Independent samples; high response rates |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Protection against contamination | High risk | Some contamination measured |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported |
Thompson 2008.
| Methods |
Study design: cluster‐randomized trial Sampling frame: Participants were recruited through 3 approaches: (1) participants in previous research study in same area; (2) additional households identified in 16 communities with high rates of Hispanic agricultural workers, and (3) households in labor camps Sampling method: All previous participants and households from labor camps were contacted; additional households in 16 communities were randomly sampled Collection method: in‐person interview, urine samples of farmworkers and children age 2 to 6, environmental sampling (house and vehicle dust) Description of the community coalition: Community Planning Group, consisting of 18 individuals from 16 diverse organizations, including farmworkers, growers, health department, regulatory agencies, farmworker clinics, advocates, and local media |
|
| Participants |
Communities: 16 communities and 8 labor camps in Yakima Valley, Washington Country: USA Ages included in assessment: adult farmworkers (n = 213) and their children age 2 to 6 (n = 211) Reasons provided for selection of intervention community: Agricultural communities in Yakima Valley of Washington State have a high percentage of Hispanic agricultural workers, many of whom work with organophosphates. 24 communities were randomly assigned to intervention or control condition Intervention community (population size): 300 to 11,000 Comparison community (population size): 300 to 11,000 |
|
| Interventions |
Name of intervention: Para Niños Saludables Theory: not reported Aim: to reduce pesticide exposure among farmworkers and their children via a community‐based intervention trial Description of costs and resources: not reported Components of the intervention: Comprehensive intervention included activities at community (health fairs, festivals), organizational (schools and preschools, churches, English language and citizenship classes, orchards, farms), small group (lay health promotoras, home health parties), and individual (promotoras conducted individual outreach at community sites) levels. Main activities included information provision and education, distribution of educational materials, and media advocacy Start date: 1999 Duration: 2 years |
|
| Outcomes |
Outcomes and measures: farmworkers’ and children’s urinary metabolite levels of pesticides (organophosphates) Time points: baseline (year 1) and follow‐up (year 4) |
|
| Notes | No information provided regarding intervention and control community characteristics. Urinary metabolite concentrations were increased in both intervention and control communities Funder: National Institute for Environmental Health Sciences and US Environmental Protection Agency Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | High risk | Allocation not concealed |
| Baseline outcome measurement similar | Low risk | No P values reported, but for urinary metabolites baseline measurements appear to be similar |
| Baseline characteristics similar | Low risk | Study authors report no differences between intervention and control communities |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | High response rates, independent samples |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not reported |
| Protection against contamination | High risk | Contamination was monitored by including questions in a final survey regarding awareness of and participation in intervention activities; estimated to be ˜20% |
| Selective reporting (reporting bias) | Low risk | Questionnaire described in detail |
Treno 2007.
| Methods |
Study design: controlled before‐after Sampling frame: 2 low‐income, predominantly ethnic minority neighborhoods in Sacramento, CA, compared with the other neighborhoods of Sacramento, CA Sampling method: not reported Collection method: police incidence reports and emergency services records Description of the community coalition: Coalition included local law enforcement officers, medical service providers, alcohol‐beverage control agents, CBO staff, community activists, parents, and youth |
|
| Participants |
Communities: 2 neighborhoods in Sacramento, CA Country: USA Ages included in assessment: general public in 37 intervention census blocks (North and South Sacramento); 243 remaining Sacramento census blocks served as the control Reasons provided for selection of intervention community: predominantly low‐income, ethnic minority neighborhoods with high risk for alcohol‐related violence and injuries Intervention community (population size): not reported Comparison community (population size): not reported |
|
| Interventions |
Name of intervention: Sacramento Neighborhood Alcohol Prevention Project (SNAPP) Theory: not reported Aim: to test the effectiveness of neighborhood‐based interventions in reducing alcohol access and drinking and related problems Description of costs and resources: unknown Components of the intervention: (1) community mobilization; (2) community awareness; (3) responsible beverage service; (4) underage‐access law enforcement; and (5) intoxicated‐patron law enforcement Start date: July 2000 Duration: 30 months |
|
| Outcomes |
Outcomes and measures: assaults and emergency services events (Chi2 and effect sizes) Time points: baseline (July 2000) and follow‐up (2002 and 2003) |
|
| Notes | Funding source: government | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not randomized |
| Allocation concealment (selection bias) | High risk | Not randomized |
| Baseline outcome measurement similar | Low risk | Similar data collected before and after intervention |
| Baseline characteristics similar | High risk | Social and demographic characteristics of North and South sites differ from Sacramento at large |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Police incidence reports and data from emergency service events |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Used public surveillance data |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded |
| Protection against contamination | High risk | Sites followed same municipal services and policies |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported |
Voorhees 1996.
| Methods |
Study design: controlled before‐after Sampling frame: 21 African American churches in East Baltimore Sampling method: non‐random (churches assigned to treatment and comparison conditions); participants were smokers Collection method: self report; validated with physical measurement (saliva cotinine and exhaled carbon monoxide levels) Description of the community coalition: Coalition included churches, clergy organization, non‐profit CBOs, and Johns Hopkins investigators |
|
| Participants |
Communities: East Baltimore, MD Country: USA Ages included in assessment: ≥ 18 (n = 292) Reasons provided for selection of intervention community: African American at‐risk population in Baltimore, MD Intervention community (population size): 71,291 Comparison community (population size): same |
|
| Interventions |
Name of intervention: Heart, Body, and Soul Theory: not reported Aim: smoking cessation Description of costs and resources: not reported Components of the intervention: church‐based educational information, sermons, lay health workers, smoking cessation counseling, support groups Start date: not reported Duration: 11 months |
|
| Outcomes |
Outcomes and measures: smoking quit rates Time points: baseline and 12‐month follow‐up |
|
| Notes | Funding source: government | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not reported |
| Allocation concealment (selection bias) | High risk | No allocation concealment reported |
| Baseline outcome measurement similar | Low risk | Similar smoking levels in intervention and comparison groups |
| Baseline characteristics similar | Unclear risk | Significantly different educational levels between groups |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding reported |
| Protection against contamination | High risk | Comparison community was same as intervention community |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported |
Wagner 2000a.
| Methods |
Study design: cluster‐randomized controlled trial (independent samples) Sampling frame: non‐institutionalized adults age 18+ with working telephones residing in intervention or control communities Sampling method: Waksberg method random‐digit dialing Collection method: telephone interview Description of the community coalition: The 11 grantees of the Community Health Promotion Grant Program were expected to establish coalitions that encompassed a broad spectrum of community agencies and organizations. Sponsoring agency for the coalition at this site (“Community G”) was a university; no further site‐specific information on coalition composition or structure is reported |
|
| Participants |
Communities: urban communities in Western USA (no further location reported) Country: USA Ages included in assessment: 18+ Reasons provided for selection of intervention community: not reported Intervention community (population size): “Community G”: urban community with large Hispanic population in Western USA (80,953) Comparison community (population size): 4 urban communities (population size not reported) |
|
| Interventions |
Name of intervention: Henry J. Kaiser Family Foundation’s Community Health Promotion Grants Program Theory: not reported Aim: to address nutrition problems and increased risk of cancer and cardiovascular disease in the local Hispanic community Description of costs and resources: $150,000 per year from Kaiser Family Foundation plus any external funding or in‐kind donations the program could obtain (total funding not reported by community; overall average = $237,000 per year per site total) Components of the intervention: community health screenings, school‐based nutrition education, grocery store interventions, community nutrition classes Start date: 1987 Duration: 5 years |
|
| Outcomes |
Outcomes and measures: nutrition (self reported): (1) percent calories from fat; (2) days eating red meat as main meal; (3) percent who drink low‐fat milk; and (4) fruit and vegetable intake Time points: baseline (1988) and follow‐up (1992) |
|
| Notes | Because the 11 grantee communities had different populations, interventions, and evaluation study designs, and because the evaluation was stratified by site, the 2 communities with a minority target group and complete evaluation results are presented as separate studies (see Wagner 2000b) Source of funding: Kaiser Foundation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Applicants for funding were stratified by urbanicity, then were randomly divided into intervention and control groups by the “finite selection model” to ensure the desired mix of health problems, minority target populations, and geographic locations |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Baseline outcome measurement similar | Low risk | Similar rates of CVD/cancer at baseline; similar with respect to diet outcomes, except intervention community more likely to drink low‐fat milk |
| Baseline characteristics similar | High risk | 3 of 4 control communities had significantly different racial composition; 2 of 4 control communities had significantly lower poverty levels |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Cross‐sectional surveys unlikely to be the subject of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Independent cross‐sectional samples imply no attrition; overall response rate of 50% did not differ between intervention and control |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | Unclear risk | Intervention and control site proximity not reported |
| Selective reporting (reporting bias) | Unclear risk | Presented outcomes were selected on the basis of hypothesized intervention effects |
Wagner 2000b.
| Methods |
Study design: controlled before‐after study (independent samples) Sampling frame: ninth and twelfth graders from public and private schools where at least 50% of enrolled students resided in the community Sampling method: all available students from schools implementing the intervention Collection method: school‐based self administered questionnaire Description of the community coalition: The 11 grantees of the Community Health Promotion Grant Program were expected to establish coalitions that encompassed a broad spectrum of community agencies and organizations. Sponsoring agency for the coalition at this site (“Community I”) was a county mental health center; no further site‐specific information on coalition composition or structure is reported |
|
| Participants |
Communities: Native American reservation Country: USA Ages included in assessment: adolescents (age range not provided) Reasons provided for selection of intervention community: not reported Intervention community (population size): Native American reservation (4149) Comparison community (population size): Native American reservation plus 2 other rural communities (population size not reported) |
|
| Interventions |
Name of intervention: Henry J. Kaiser Family Foundation’s Community Health Promotion Grants Program Theory: not reported Aim: to address suicide and substance abuse among Native American teens Description of costs and resources: $150,000 per year from Kaiser Family Foundation plus any external funding or in‐kind donations the program could obtain (total funding not reported by community; overall average = $237,000 per year per site total) Components of the intervention: school‐based training; peer counseling programs; drug‐free activities; family resource center; community education activities; improvement in law enforcement Start date: 1987 Duration: 5 years |
|
| Outcomes |
Outcomes and measures
Time points: baseline (1988) and follow‐up (1992) |
|
| Notes | Because the 11 grantee communities had different populations, interventions, and evaluation study designs, and because the evaluation was stratified by site, the 2 communities with a minority target group and complete evaluation results are presented as separate studies (see Wagner 2000a) Funding source: Kaiser Foundation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not randomized |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | High risk | Baseline rates of substance abuse much higher in intervention community |
| Baseline characteristics similar | Unclear risk | Baseline characteristics not presented |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | School‐based surveys in 9th and 12th grades |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Independent cross‐sectional samples imply no attrition; response rates not given by site or survey time |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | Unclear risk | Portion of control population drawn from same area as target population, but different ethnic group |
| Selective reporting (reporting bias) | Unclear risk | Only 2 major substance abuse outcomes reported |
Wells 2013.
| Methods |
Study design: cluster RCT Sampling frame: lists of health and social service agencies in targeted geographic area plus agencies identified by Community Partners in Care Council Sampling method: random Description of the community coalition: Los Angeles Community Health Improvement Collaborative involves Healthy African American Families, University of California Los Angeles, Charles Drew University, RAND, Queens Care Health and Faith Partnership, Los Angeles County Health Department, Veterans Affairs Greater Los Angeles Healthcare System, and others. These groups have worked together for 15 years in partnership efforts. They formed Community Partners In Care (CPIC), a participatory research initiative, to improve depression services in Los Angeles for diverse populations in under‐resourced communities. CPIC was designed and implemented by a council of 35 leaders from 3 academic and 24 community‐based agencies, using principles of equal authority of community and academic partners and 2‐way knowledge exchange. The CPIC Council oversaw implementation and evaluation of the program |
|
| Participants |
Communities: For the cluster RCT, a frame of 94 organizations in the South Los Angeles and Hollywood metro areas was generated from comprehensive lists of service agencies coupled with recommendations from lead community partners in mental health, substance abuse, primary care, social service, and homeless and other community agencies Country: USA Ages included in assessment: general population Reasons provided for selection of intervention community: ethnically diverse population with higher rates of depression Intervention community (population size): South Los Angeles and Hollywood metro (2 million) Comparison community (population size): same areas |
|
| Interventions |
Name of intervention: Community Partners in Care (CPIC) Theory: Community Engagement, Cognitive‐Behavioral Therapy (CBT) for Depression Aim: The CPIC program initiated by the Council was based on the idea that non‐healthcare settings can play a role in serving depressed clients, and that most people have some access to primary care services that can co‐ordinate depression services across various social service sectors. The Council developed depression care quality improvement strategies for use by diverse agencies. A randomized trial of "community engagement to activate multiple‐agency networks" compared with "resource support for agencies" to implement depression care quality improvement tested whether the community engagement process added extra value Description of costs and resources: costs not provided, several professional trainers used Components of the intervention: train‐the‐trainer for quality improvement (QI) in depression care, CBT, medication management; developed service networks across agencies. Start date: 2009 Duration: 20 months |
|
| Outcomes |
Outcomes and measures (at 6‐month follow‐up) Primary
Secondary
Dates (years) of pre and post measurements: 2009 through 2011 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization was conducted by a statistician uninvolved in recruitment. Council members produced seed numbers for randomization |
| Allocation concealment (selection bias) | Low risk | Recruiters were blinded to assignment |
| Baseline outcome measurement similar | Low risk | No differences by intervention status |
| Baseline characteristics similar | Low risk | No significant differences in baseline characteristics |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded to condition |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 60% follow‐up rate |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and personnel were blinded to condition |
| Protection against contamination | High risk | Treatment and control conditions were implemented in the same communities |
| Selective reporting (reporting bias) | Low risk | Primary outcomes reported |
Wilson 2008.
| Methods |
Study design: cluster‐randomized trial (independent samples) Sampling frame: female clients receiving services at 1 of 40 experimental/control salons participating in the study Sampling method: listed all salons in target neighborhood using telephone directories and Internet sources by target ZIP codes Collection method: not reported for baseline assessment; self administered questionnaire for follow‐up Description of the community coalition: The Arthur Ashe Institute for Urban Health, faculty at the State University of New York Downstate Medical Center, and members of the Health and Beauty Council advisory group (consisting of local community health leaders, including salon owners, breast cancer survivors, and other healthcare advocates; leaders of local media outlets and foundations; and academic partners) worked together to develop, oversee, and interpret results of the intervention |
|
| Participants |
Communities: salons in Brooklyn, New York Country: USA Ages included in assessment: range not reported; mean age 38 (n = 1210) Reasons provided for selection of intervention community: Residents are predominantly racial/ethnic minority group members, of low income, and presumably less likely to adhere to breast cancer screening guidelines Intervention community (population size): 5 neighborhoods in Brooklyn, NY (population size not reported) Comparison community (population size): same as above |
|
| Interventions |
Name of intervention: Soul Sense of Beauty Theory: Social Cognitive Theory Aim: to promote customer screening practices by fostering the ability and motivation of stylists to deliver theoretically based and culturally appropriate breast health messages Description of costs and resources: not reported Components of the intervention: Stylist training included two 2‐hour workshops, a reference handbook, written materials provided to clients, and ongoing support from Institute staff Start date: 2002 Duration: 3 months (implemented in waves by salon) |
|
| Outcomes |
Outcomes and measures: salon customer survey of breast cancer screening measures completed for the prior 3 months
Time points: baseline and follow‐up (1 to 3 months later) |
|
| Notes | Only 16% of all salons approached agreed to participate Intended to follow‐up a cohort of clients, but because of attrition, only the results of 2 cross‐sectional surveys were presented Funder: National Cancer Institute Funding source: government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Salons randomly assigned by random number generator |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Baseline outcome measurement similar | Low risk | Baseline rates of recent breast health practices similar between salon client groups |
| Baseline characteristics similar | Low risk | Salon client groups similar at baseline with regard to age, race, and family history of breast cancer |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Cohort follow‐up dropped because of 80% attrition; response rates for baseline and follow‐up surveys not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Protection against contamination | Unclear risk | Some contamination measured by asking participants about exposure to breast health messages in salons; analyses re‐grouped to test effectiveness by receipt of health promotion message |
| Selective reporting (reporting bias) | Low risk | Main outcomes reported |
AIDS: acquired immunodeficiency syndrome.
BMI: body mass index.
BP: blood pressure.
CBO: community‐based organization.
CDC: Centers for Disease Control and Prevention.
CHW: community health worker.
CI: confidence interval.
CRC: colorectal cancer.
EPOC: Effective Practice and Organization of Care.
HbA1c: glycosylated hemoglobin.
HIV: human immunodeficiency virus.
ITS: interrupted time series.
ITT: intention‐to‐treat.
LDL: low‐density lipoprotein.
OR: odds ratio.
PRC: Preventive Research Center.
RCT: randomized controlled trial.
RDD: random‐digit dialing.
REACH: Racial and Ethnic Approaches to Community Health.
RWJ: Robert Wood Johnson.
STD: sexually transmitted disease.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aguilar 2010 | Not a comparative study/ineligible methods |
| Ambrose 2009 | Not a comparative study/ineligible methods |
| Anaya 2010 | No minority population |
| Anderson 2006 | Not a comparative study/ineligible methods |
| Angell 2003 | No minority population |
| Arcury 1999 | Not a comparative study/ineligible methods |
| Arthur 2010 | No minority population |
| Atkinson 2011 | Not a comparative study/ineligible methods |
| Babu 2006 | Not a comparative study/ineligible methods |
| Bachar 2006 | Not a comparative study/ineligible methods |
| Bailey 2011 | Not a comparative study/ineligible methods |
| Baker 1997 | Not a comparative study/ineligible methods |
| Baker 2007 | Not a comparative study/ineligible methods |
| Balcazar 2012 | Not a comparative study/ineligible methods |
| Baldwin 1999 | Not a comparative study/ineligible methods |
| Barnes 2000 | Not a comparative study/ineligible methods |
| Bazzoli 1997 | Not a comparative study/ineligible methods |
| Begley 2009 | Not a comparative study/ineligible methods |
| Biel 2009 | Not a comparative study/ineligible methods |
| Bluthenthal 2006 | Not a comparative study/ineligible methods |
| Boettcher 2008 | No minority population |
| Brown 1991 | Not a comparative study/ineligible methods |
| Brown 2010 | No minority population |
| Buchanan 1993 | Not a comparative study/ineligible methods |
| CADCA 2004 | Not a comparative study/ineligible methods |
| Calman 2005 | Not a comparative study/ineligible methods |
| Case 2003 | Not a comparative study/ineligible methods |
| Cheadle 2010 | Not a comparative study/ineligible methods |
| Cheadle 2011 | Not a comparative study/ineligible methods |
| Cheadle 2012 | Not a comparative study/ineligible methods |
| Chinman 1990 | Not a comparative study/ineligible methods |
| Chou 2008 | Not a comparative study/ineligible methods |
| Clark 2009 | Not a comparative study/ineligible methods |
| Claus 2012 | Not a comparative study/ineligible methods |
| Collie‐Akers 2007 | Not a comparative study/ineligible methods |
| Conrad 2003 | Not a comparative study/ineligible methods |
| Cornell 2009 | Not a comparative study/ineligible methods |
| Cox 2010 | Not a comparative study/ineligible methods |
| Cramer 2003 | Not a comparative study/ineligible methods |
| Crow 2006 | Not a comparative study/ineligible methods |
| Cummings 1999 | Not a comparative study/ineligible methods |
| Dal Conte 2011 | Not a comparative study/ineligible methods |
| Daniel 1995 | Not a comparative study/ineligible methods |
| Darrow 2010 | Not a comparative study/ineligible methods |
| Delp 2005 | Not a comparative study/ineligible methods |
| Dulin 2011 | Not a comparative study/ineligible methods |
| Eaker 2001 | No minority population |
| Ehlers 2005 | Not a comparative study/ineligible methods |
| Eisen 1994 | Not a comparative study/ineligible methods |
| Elder 2013 | Not a comparative study/ineligible methods |
| Ellis 2003 | Not a comparative study/ineligible methods |
| English 2008 | Not a comparative study/ineligible methods |
| Fawcett 1997 | Not a comparative study/ineligible methods |
| Feinberg 2005 | No minority population |
| Ferdinand 1995 | Not a comparative study/ineligible methods |
| Ferdinand 2013 | Not a comparative study/ineligible methods |
| Findley 2004 | Not a comparative study/ineligible methods |
| Flewelling 2005 | No minority population |
| Flynn 2006 | Not a comparative study/ineligible methods |
| Forti 2002 | Not a comparative study/ineligible methods |
| Fouad 2004 | Not a comparative study/ineligible methods |
| Fox 2012 | Not a comparative study/ineligible methods |
| Friedman 2014 | Not a comparative study/ineligible methods |
| Furlong 1997 | Not a comparative study/ineligible methods |
| Garvin 2004 | Not a comparative study/ineligible methods |
| Garza 2009 | Not a comparative study/ineligible methods |
| Giachello 2003 | Not a comparative study/ineligible methods |
| Glasser 2003 | Not a comparative study/ineligible methods |
| Godley 1998 | Not a comparative study/ineligible methods |
| Goodman 1996 | Not a comparative study/ineligible methods |
| Greenberg 2007 | No minority population |
| Griffin 2006 | Not a comparative study/ineligible methods |
| Grigg‐Saito 2008 | Not a comparative study/ineligible methods |
| Gutierrez 2014 | Not a comparative study/ineligible methods |
| Hamamoto 2009 | Not a comparative study/ineligible methods |
| Hannon 2006 | Not a comparative study/ineligible methods |
| Harachi 1996 | Not a comparative study/ineligible methods |
| Hawkes 2007 | Not a comparative study/ineligible methods |
| Hawkins 2012 | No minority population |
| Helitzer 2009 | Not a comparative study/ineligible methods |
| Higginbotham 1999 | No minority population |
| Higgins 2005 | Not a comparative study/ineligible methods |
| Hingson 1996 | No minority population |
| Hinton 2005 | Not a comparative study/ineligible methods |
| Holliday 2008 | Not a comparative study/ineligible methods |
| Horen 2003 | Not a comparative study/ineligible methods |
| Hull 2010 | Not a comparative study/ineligible methods |
| Hunte 2004 | Not a comparative study/ineligible methods |
| Hussein 2014 | Not a comparative study/ineligible methods |
| Jenkins 2004 | Not a comparative study/ineligible methods |
| Jernigan 2012 | Not a comparative study/ineligible methods |
| Kaufman 1994 | No minority population |
| Kegler 1998 | Not a comparative study/ineligible methods |
| Kegler 2003 | Not a comparative study/ineligible methods |
| Keys 2001 | Not a comparative study/ineligible methods |
| Kieffer 2004 | Not a comparative study/ineligible methods |
| Klerman 2005 | Not a comparative study/ineligible methods |
| Klevens 2008 | No minority population |
| Komro 2001 | No minority population |
| Krishnan 2011 | Not a comparative study/ineligible methods |
| Lara 2009 | Not a comparative study/ineligible methods |
| Lee 2008 | Not a comparative study/ineligible methods |
| Leviton 2006 | Not a comparative study/ineligible methods |
| Lewis 1996 | No minority population |
| Lewis 1999 | No minority population |
| Lewis 2005 | Not a comparative study/ineligible methods |
| Li 2007 | Not a comparative study/ineligible methods |
| Lisovicz 2006 | Not a comparative study/ineligible methods |
| Lohrmann 2005 | Not a comparative study/ineligible methods |
| Lyon 2009 | Not a comparative study/ineligible methods |
| Ma 2004 | Not a comparative study/ineligible methods |
| Ma'at 2001 | Not a comparative study/ineligible methods |
| Maciak 1998 | Not a comparative study/ineligible methods |
| Marcus 2004 | Not a comparative study/ineligible methods |
| Martinez 2014 | Not a comparative study/ineligible methods |
| McCloskey 2011 | Not a comparative study/ineligible methods |
| McElmurry 2009 | Not a comparative study/ineligible methods |
| McFarlane 1994 | Not a comparative study/ineligible methods |
| McKay 2004 | Not a comparative study/ineligible methods |
| McKeever 2004 | Not a comparative study/ineligible methods |
| Miao 2011 | Not a comparative study/ineligible methods |
| Michelen 2006 | Not a comparative study/ineligible methods |
| Minkler 2006 | Not a comparative study/ineligible methods |
| Minkler 2010 | Not a comparative study/ineligible methods |
| Mishra 2009 | No minority population |
| Monks 2010 | Not a comparative study/ineligible methods |
| Moore 2010 | Not a comparative study/ineligible methods |
| Morita 2006 | Not a comparative study/ineligible methods |
| Nargiso 2013 | Not a comparative study/ineligible methods |
| Nelson 2005 | No minority population |
| Nicholas 2005 | Not a comparative study/ineligible methods |
| Northridge 2000 | Not a comparative study/ineligible methods |
| Okafor 2003 | Not a comparative study/ineligible methods |
| Okwumabua 1997 | Not a comparative study/ineligible methods |
| Olaseha 2006 | Not a comparative study/ineligible methods |
| Operario 2005 | Not a comparative study/ineligible methods |
| Paine‐Andrews 1997 | No minority population |
| Painter 2001 | Not a comparative study/ineligible methods |
| Pargee 1999 | Not a comparative study/ineligible methods |
| Pazoki 2007 | No minority population |
| Perera 2002 | Not a comparative study/ineligible methods |
| Perry 1996 | No minority population |
| Person 1996 | Not a comparative study/ineligible methods |
| Plochg 2013 | Not a comparative study/ineligible methods |
| Pullen‐Smith 2008 | Not a comparative study/ineligible methods |
| Quandt 2001 | Not a comparative study/ineligible methods |
| Quigley 2000 | Not a comparative study/ineligible methods |
| Raphael 2003 | Not a comparative study/ineligible methods |
| Rapkin 2006 | Not a comparative study/ineligible methods |
| Redmond 2009 | No minority population |
| Reifsnider 2010 | Not a comparative study/ineligible methods |
| Rodriguez 1993 | Not a comparative study/ineligible methods |
| Rohrbach 1997 | Not a comparative study/ineligible methods |
| Rowe 1997 | Not a comparative study/ineligible methods |
| Saewyc 2008 | Not a comparative study/ineligible methods |
| Sanigorski 2008 | No minority population |
| Schensul 1999 | Not a comparative study/ineligible methods |
| Schulz 2001 | Not a comparative study/ineligible methods |
| Schwarte 2010 | Not a comparative study/ineligible methods |
| Serpas 2013 | Not a comparative study/ineligible methods |
| Shaw 1997 | Not a comparative study/ineligible methods |
| Shearer 2005 | Not a comparative study/ineligible methods |
| Shortell 2002b | Not a comparative study/ineligible methods |
| Sloane 2003 | Not a comparative study/ineligible methods |
| Solomon 2012 | No minority population |
| Somerville 2012 | Not a comparative study/ineligible methods |
| Sorkin 2013 | Not a comparative study/ineligible methods |
| Spielman 2006 | Not a comparative study/ineligible methods |
| Splett 2006 | No minority population |
| Spoth 2004 | No minority population |
| Spoth 2011 (2) | No minority population |
| Steckler 1992 | Not a comparative study/ineligible methods |
| Stevens 2003 | Not a comparative study/ineligible methods |
| Tate 2003 | No minority population |
| TenBrink 2009 | Not a comparative study/ineligible methods |
| Tsui 2012 | Not a comparative study/ineligible methods |
| Turner 1995 | Not a comparative study/ineligible methods |
| Two Feathers 2005 | Not a comparative study/ineligible methods |
| Urban 1995 | No minority population |
| Watson‐Thompson 2008 | Not a comparative study/ineligible methods |
| Williams 1999 | Not a comparative study/ineligible methods |
| Wynn 2006 | Not a comparative study/ineligible methods |
| Yancey 2004 | Not a comparative study/ineligible methods |
| Yassi 2003 | No minority population |
| Ytterstad 2003 | Not a comparative study/ineligible methods |
| Ziegahn 2013 | Not a comparative study/ineligible methods |
| Zoellner 2013 | Not a comparative study/ineligible methods |
Characteristics of ongoing studies [ordered by study ID]
Smith 2013.
| Trial name or title | Educational program to increase colorectal cancer screening (EPICS) |
| Methods | Cluster‐randomized controlled trial |
| Participants | African Americans 50 to 74 years of age |
| Interventions | 4‐Arm cluster‐randomized trial compares the following implementation strategies: passive arms: (1) web access to facilitator training materials and toolkits without technical assistance (TA); and (2) web access to facilitator training materials with TA active arms; active arms: (3) in‐person access to facilitator training materials and toolkits without TA; and (4) in‐person access with TA |
| Outcomes | Primary outcomes: reach (proportions of representative community coalitions and individuals participating), efficacy (post‐intervention changes in colorectal cancer screening rates) Secondary outcomes: adoption (percentage of community coalitions implementing EPICS sessions), implementation (quality and consistency of intervention delivery) |
| Starting date | May 2013 |
| Contact information | Selina A Smith; ssmith@msm.edu |
| Notes |
Differences between protocol and review
None.
Contributions of authors
Laurie Anderson (LA), Kathryn Adeney (KA), Carolynne Shinn (CS), and L. Kendall Krause (LK) drafted the protocol with input from the Review Advisory Group. Sarah Safranek (SS) developed the search strategy in conjunction with Ruth Turley (RT), the Public Health Review Group Trials Search Co‐ordinator. LA, KA, CS, LK, and Joyce Buckner‐Brown (JB) screened papers and extracted data. LA and CS analyzed data. LA, CS, and JB wrote the report.
Sources of support
Internal sources
No sources of support supplied
External sources
International Union for Health Promotion and Education, Other.
Declarations of interest
None declared.
New
References
References to studies included in this review
Abbema 2004 {published data only}
- Abbema EA, Assema P, Kok J, Leeuw E, Vries NK. Effect evaluation of a comprehensive community intervention aimed at reducing socioeconomic health inequalities in the Netherlands. Health Promotion International 2004;19(2):141‐56. [DOI] [PubMed] [Google Scholar]
Blumenthal 2010 {published data only}
- Blumenthal DS. A community coalition board creates a set of values for community‐based research. Preventing Chronic Disease 2006;3(1):A16. [PMC free article] [PubMed] [Google Scholar]
- Blumenthal DS, Smith SA, Majett CD, Alema‐Mensah E. A trial of three interventions to promote colorectal cancer screening in African Americans. Cancer 2010;116(4):922‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brown 2013 {published data only}
- Brown B, Noonan C, Harris KJ, Parker M, Gaskill S, RIcci C, et al. Developing and piloting the Journey to Native Youth Health program in Northern Plains Indian communities. The Diabetes Educator 2013;39(1):109‐18. [DOI] [PubMed] [Google Scholar]
- Brown BD, Harris KJ, Harris JL, Parker M, Ricci C, Noonan C. Translating the diabetes prevention program for Northern Plains Indian youth through community‐based participatory research methods. The Diabetes Educator 2010;36(6):924‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brownson 1996 {published data only}
- Brownson CA, Dean C, Dabney S, Brownson RC. Cardiovascular risk reduction in rural minority communities: the Bootheel Heart Health Project. Journal of Health Education 1998;29(3):158‐65. [Google Scholar]
- Brownson RC, Smith CA, Jorge N, Deprima L, Dean CG, Cates R. The role of data‐driven planning and coalition development in preventing cardiovascular disease. Public Health Reports 1992;107(1):32‐7. [PMC free article] [PubMed] [Google Scholar]
- Brownson RC, Smith CA, Pratt M, Mack NE, Jackson‐Thompson J, Dean CG, et al. Preventing cardiovascular disease through community‐based risk reduction: the Bootheel Heart Health Project. American Journal of Public Health 1996;86(2):206‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mack NE, Brownson RC, Pratt M, Brownson CA, Dean C, Dabney SC. Cardiovascular disease control efforts among local health departments in Missouri: four‐year trends and policy implications. Journal of Public Health Management and Practice 1997;3(2):71. [DOI] [PubMed] [Google Scholar]
Brownson 2004 {published data only}
- Brownson RC, Baker EA, Boyd RL, Caito NM, Duggan K, Housemann RA, et al. A community‐based approach to promoting walking in rural areas. American Journal of Preventive Medicine 2004;27(1):28‐34. [DOI] [PubMed] [Google Scholar]
- Brownson RC, Housemann RA, Brown DR, Jackson‐Thompson J, King AC, Malone BR, et al. Promoting physical activity in rural communities: walking trail access, use, and effects. American Journal of Preventive Medicine 2000;18(3):235‐41. [DOI] [PubMed] [Google Scholar]
Burhansstipanov 2010 {published data only}
- Burhansstipanov L, Dignan MB, Schumacher A, Krebs LU, Alfonsi G, Apodaca CC. Breast screening navigator programs within three settings that assist underserved women. Journal of Cancer Education 2010;25(2):247‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cardarelli 2011 {published data only}
- Cardarelli K, Jackson R, Martin M, Linnear K, Lopez R, Senteio C, et al. Community‐based participatory approach to reduce breast cancer disparities in South Dallas. Progress in Community Health Partnerships: Research, Education and Action 2011;5(4):375‐85. [PMC free article] [PubMed] [Google Scholar]
Cheadle 2001 {published data only}
- *Cheadle A, Wagner E, Walls M, Diehr P, Bell M, Anderman C, et al. The effect of neighborhood‐based community organizing: results from the Seattle Minority Youth Health Project. Health Services Research 2001;36(4):671‐89. [PMC free article] [PubMed] [Google Scholar]
Clark 2013 {published data only}
- Butterfoss FD, Gilmore LA, Krieger JW, Lachance LL, Lara M, Meurer JR, et al. From formation to action: how Allies Against Asthma coalitions are getting the job done. Health Promotion Practice 2006;7(2 Suppl):34S‐43S. [DOI] [PubMed] [Google Scholar]
- Clark NM. Community‐based approaches to controlling childhood asthma. Annual Review of Public Health 2012;33:193‐208. [DOI] [PubMed] [Google Scholar]
- Clark NM, Doctor LJ, Friedman AR, Lachance LL, Houle CR, Geng X, et al. Community coalitions to control chronic disease: Allies Against Asthma as a model and case study. Health Promotion Practice 2006;7(2 Suppl):14S‐22S. [DOI] [PubMed] [Google Scholar]
- Clark NM, Lachance L, Doctor LJ, Gilmore L, Kelly C, Krieger J, et al. Policy and system change and community coalitions: outcomes from Allies Against Asthma. American Journal of Public Health 2010;100(5):904‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark NM, Lachance LL, Benedict MB, et al. Improvements in health care use associated with community coalitions: long‐term results of the Allies Against Asthma initiative. American Journal of Public Health 2013;103:1124‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachance LL, Houle CR, Cassidy EF, Bourcier E, Cohn JH, Orians CE, et al. Collaborative design and implementation of a multisite community coalition evaluation. Health Promotion Practice 2006;7(2 Suppl):44S‐55S. [DOI] [PubMed] [Google Scholar]
Darrow 2011 {published data only}
- Darrow WW, Montanea JE, Fernandez PB, Zucker UF, Stephens DP, Gladwin H. Eliminating disparities in HIV disease: community mobilization to prevent HIV transmission among Black and Hispanic young adults in Broward County, Florida. Ethnicity & Disease 2004;14(Suppl 1):S108‐16. [PubMed] [Google Scholar]
- Darrow WW, Montanea JE, Uribe CL, Sánchez‐Braña E, Gladwin H. Summative evaluation of a community mobilization program to eliminate racial and ethnic disparities in HIV disease. International Public Health Journal 2010;2(3):301‐11. [Google Scholar]
Davidson 1994 {published data only}
- Davidson LL, Barlow B, Thompkins T, Bey‐Grecia A, Weeks S, Laraque D, et al. Beyond the hospital's ivory tower: from research to action for a safer city for children. Child 1994;11:3‐5. [Google Scholar]
- Davidson LL, Durkin MS, Kuhn L, O'Connor P, Barlow B, Heagarty MC. The impact of the Safe Kids/Healthy Neighborhoods Injury Prevention Program in Harlem, 1988 through 1991. American Journal of Public Health 1994;84(4):580‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkin MS, Kuhn L, Davidson LL, Laraque D, Barlow B. Epidemiology and prevention of severe assault and gun injuries to children in an urban community. The Journal of Trauma 1996;41(4):667‐73. [DOI] [PubMed] [Google Scholar]
- Durkin MS, Laraque D, Lubman I, Barlow B. Epidemiology and prevention of traffic injuries to urban children and adolescents. Pediatrics 1999;103(6):e74. [DOI] [PubMed] [Google Scholar]
- Kuhn L, Davidson LL, Durkin MS. Use of Poisson regression and time series analysis for detecting changes over time in rates of child injury following a prevention program. American Journal of Epidemiology 1994;140(10):943‐55. [DOI] [PubMed] [Google Scholar]
- Laraque D, Barlow B, Durkin M, Heagarty M. Injury prevention in an urban setting: challenges and successes. Bulletin of the New York Academy of Medicine 1995;72(1):16‐30. [PMC free article] [PubMed] [Google Scholar]
- Pressley JC, Barlow B, Durkin M, Jacko SA, Dominguez DLR, Johnson L. A national program for injury prevention in children and adolescents: the Injury Free Coalition for Kids. Journal of Urban Health 2005;82(3):389‐402. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dedobbeleer 2001 {published data only}
- Dedobbeleer N, Desjardins S. Outcomes of an ecological and participatory approach to prevent alcohol and other drug abuse among multiethnic adolescents. Substance Abuse & Misuse 2001;36(13):1959‐91. [DOI] [PubMed] [Google Scholar]
Fisher 1998 {published data only}
- Fisher EB, Auslander W, Sussman L, Owens N, Jackson‐Thompson J. Community organization and health promotion in minority neighborhoods. Ethnicity & Disease 1992;2(3):252‐72. [PubMed] [Google Scholar]
- Fisher EB, Auslander WF, Munro JF, Arfken CL, Brownson RC, Owens NW. Neighbors for a Smoke Free North Side: evaluation of a community organization approach to promoting smoking cessation among African Americans. American Journal of Public Health 1998;88(11):1658‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fisher 2004 {published data only}
- Fisher EB, Auslander W, Sussman L, Owens N, Jackson‐Thompson J. Community organization and health promotion in minority neighborhoods. Ethnicity & Disease 1992;2(3):252‐72. [PubMed] [Google Scholar]
- Fisher EB, Strunk RC, Sussman LK, Arfken C, Sykes RK, Munro JM, et al. Acceptability and feasibility of a community approach to asthma management: the Neighborhood Asthma Coalition (NAC). Journal of Asthma 1996;33(6):367‐83. [DOI] [PubMed] [Google Scholar]
- Fisher EB, Strunk RC, Sussman LK, Sykes RK, Walker MS. Community organization to reduce the need for acute care for asthma among African American children in low‐income neighborhoods: the Neighborhood Asthma Coalition. Pediatrics 2004;114(1):116‐23. [DOI] [PubMed] [Google Scholar]
- Fisher EB, Sussman LK, Arfken C, Harrison D, Munro J, Sykes RK, et al. Targeting high risk groups. Neighborhood organization for pediatric asthma management in the Neighborhood Asthma Coalition. Chest 1994;106(4 Suppl):248S‐59S. [DOI] [PubMed] [Google Scholar]
Fuller 2007 {published data only}
- Fuller CM, Galea S, Caceres W, Blaney S, Sisco S, Vlahov D. Multilevel community‐based intervention to increase access to sterile syringes among injection drug users through pharmacy sales in New York City. American Journal of Public Health 2007;97(1):117‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Factor SH, Bonner S, Foley M, Freudenberg N, Latka M, et al. Collaboration among community members, local health service providers, and researchers in an urban research center in Harlem, New York. Public Health Reports 2001;116(6):530‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israel BA, Krieger J, Vlahov D, Ciske S, Foley M, Fortin P, et al. Challenges and facilitating factors in sustaining community‐based participatory research partnerships: lessons learned from the Detroit, New York City and Seattle Urban Research Centers. Journal of Urban Health 2006;83(6):1022‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gotay 2000 {published data only}
- Banner RO, DeCambra H, Enos R, Gotay C, Hammond OW, Hedlund N, et al. A breast and cervical cancer project in a native Hawaiian community: Wai'anae cancer research project. Preventive Medicine 1995;24(5):447‐53. [DOI] [PubMed] [Google Scholar]
- DeCambra H, Enos R, Matsunaga DS, Hammond OW. Community involvement in minority health research: participatory research in a native Hawaiian community. Cancer Control Research Report on Public Health 1992;7(Suppl):2‐9. [Google Scholar]
- Gotay CC, Banner RO, Matsunaga DS, Hedlund N, Enos R, Issell BF, et al. Impact of a culturally appropriate intervention on breast and cervical screening among native Hawaiian women. Preventive Medicine 2000;31(5):529‐37. [DOI] [PubMed] [Google Scholar]
- Matsunaga DS, Enos R, Gotay CC, Banner RO, DeCambra H, Hammond OW, et al. Participatory research in a native Hawaiian community: the Wai'anae Cancer Research Project. Cancer 1996;78(S7):1582‐6. [PubMed] [Google Scholar]
Holder 2000 {published data only}
- Grube JW. Preventing sales of alcohol to minors: results from a community trial. Addiction 1997;92(Suppl 2):S251‐60. [PubMed] [Google Scholar]
- Holder HD. Community prevention of alcohol problems. Addictive Behaviors 2000;25(6):843‐59. [DOI] [PubMed] [Google Scholar]
- Holder HD, Gruenewald PJ, Ponicki WR, Treno AJ, Grube JW, Saltz RF, et al. Effect of community‐based interventions on high‐risk drinking and alcohol‐related injuries. Journal of the American Medical Association 2000;284(18):2341‐7. [DOI] [PubMed] [Google Scholar]
- Holder HD, Reynolds RI. Application of local policy to prevent alcohol problems: experiences from a community trial. Addiction 1997;92(6s1):285‐92. [PubMed] [Google Scholar]
- Treno AJ, Holder HD. Evaluating efforts to reduce community‐level problems through structural rather than individual change. Evaluation Review 1997;21(2):133‐9. [DOI] [PubMed] [Google Scholar]
- Voas RB, Holder HD, Gruenewald PJ. The effect of drinking and driving interventions on alcohol‐involved traffic crashes within a comprehensive community trial. Addiction 1997;92:S221‐36. [PubMed] [Google Scholar]
Kagawa‐Singer 2009 {published data only}
- Kagawa‐Singer M, Tanjasiri SP, Valdez A, Yu H, Foo MA. Outcomes of a breast health project for Hmong women and men in California. American Journal of Public Health 2009;99(S2):S467‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanjasiri SP, Kagawa‐Singer M, Foo MA, Chao M, Linayao‐Putman I, Nguyen J, et al. Designing culturally and linguistically appropriate health interventions: the 'Life Is Precious' Hmong breast cancer study. Health Education & Behavior 2007;34(1):140‐53. [DOI] [PubMed] [Google Scholar]
Kelaher 2009 {published data only}
- Kelaher M, Dunt D, Feldman P, Nolan A, Raban B. The effect of an area‐based intervention on breastfeeding rates in Victoria, Australia. Health Policy 2009;90(1):89‐93. [DOI] [PubMed] [Google Scholar]
- Kelaher M, Dunt D, Feldman P, Nolan A, Raban B. The effects of an area‐based intervention on the uptake of maternal and child health assessments in Australia: a community trial. BMC Health Services Research 2009;9(1):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raban B, Victoria Department of Human Services, Victoria Department of Education and Training, Victoria.Community, University of Melbourne. Statewide evaluation of Best Start: final report. Department of Human Services 2006.
- Victorian Government Department of Human Services. Best Start in action: project guidelines. Victorian Government Department of Human Services 2005.
Kelaher 2010 {published data only}
- Kelaher M, Warr DJ, Tacticos T. Evaluating health impacts: results from the Neighbourhood Renewal strategy in Victoria, Australia. Health & Place 2010;16(5):861‐7. [DOI] [PubMed] [Google Scholar]
- Victoria Department of Human Services. Neighborhood Renewal evaluation report 2008. Victoria State Government Department of Human Services 2009.
- Victoria Department of Human Services. Neighbourhood Renewal evaluation framework. Victoria State Government Department of Human Services 2009.
Kim 2008 {published data only}
- Kim KH, Linnan L, Campbell MK, Brooks C, Koenig HG, Wiesen C. The WORD (Wholeness, Oneness, Righteousness, Deliverance): a faith‐based weight‐loss program utilizing a community‐based participatory research approach. Health Education & Behavior 2008;35(5):634‐50. [DOI] [PubMed] [Google Scholar]
Kloek 2006 {published data only}
- Kloek GC, Lenthe FJ, Nierop PWM, Koelen MA, Mackenbach JP. Impact evaluation of a Dutch community intervention to improve health‐related behaviour in deprived neighbourhoods. Health & Place 2006;12(4):665‐77. [DOI] [PubMed] [Google Scholar]
Koniak‐Griffin 2008 {published data only}
- Koniak‐Griffin D, Lesser J, Henneman T, Huang R, Huang X, Tello J, et al. HIV prevention for Latino adolescent mothers and their partners. Western Journal of Nursing Research 2008;30(6):724‐42. [DOI] [PubMed] [Google Scholar]
- Lesser J, Koniak‐Griffin D, Gonzalez‐Figueroa E, Huang R, Cumberland WG. Childhood abuse history and risk behaviors among teen parents in a culturally rooted, couple‐focused HIV prevention program. Journal of the Association of Nurses in AIDS Care 2007;18(2):18‐27. [DOI] [PubMed] [Google Scholar]
- Lesser J, Verdugo RL, Koniak‐Griffin D, Tello J, Kappos B, Cumberland WG. Respecting and protecting our relationships: a community research HIV prevention program for teen fathers and mothers. AIDS Education & Prevention 2005;17(4):347‐60. [DOI] [PubMed] [Google Scholar]
Krieger 2000 {published data only}
- Eisinger A, Senturia K. Doing community‐driven research: a description of Seattle Partners for Healthy Communities. Journal of Urban Health 2001;78(3):519‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israel BA, Krieger J, Vlahov D, Ciske S, Foley M, Fortin P, et al. Challenges and facilitating factors in sustaining community‐based participatory research partnerships: lessons learned from the Detroit, New York City and Seattle Urban Research Centers. Journal of Urban Health 2006;83(6):1022‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger JW, Castorina JS, Walls ML, Weaver MR, Ciske S. Increasing influenza and pneumococcal immunization rates: a randomized controlled study of a senior center‐based intervention. American Journal of Preventive Medicine 2000;18(2):123‐31. [DOI] [PubMed] [Google Scholar]
Krieger 2005 {published data only}
- Israel BA, Krieger J, Vlahov D, Ciske S, Foley M, Fortin P, et al. Challenges and facilitating factors in sustaining community‐based participatory research partnerships: lessons learned from the Detroit, New York City and Seattle Urban Research Centers. Journal of Urban Health 2006;83(6):1022‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger J, Allen C, Cheadle A, Ciske S, Schier JK, Senturia K, Sullivan M. Using community‐based participatory research to address social determinants of health: lessons learned from Seattle Partners for Healthy Communities. Health Education & Behavior 2002;29(2):361‐82. [DOI] [PubMed] [Google Scholar]
- Krieger J, Takaro T, Song L, Weaver M. The Seattle‐King County Healthy Homes project: a randomized controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. American Journal of Public Health 2005;95(4):652‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger J, Takaro TK, Allen C, Song L, Weaver M, Chai S, et al. The Seattle‐King County Healthy Homes project: implementation of a comprehensive approach to improving indoor environmental quality for low‐income children with asthma. Environmental Health Perspectives 2002;110(Suppl 2):311‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kronish 2014 {published data only}
- Goldfinger JZ, Kronish IM, Kezhen F, Graciani A, Rosenfeld P, Lorig K, et al. Peer education for secondary stroke prevention in inner‐city minorities: design and methods of the prevent recurrence of all inner‐city strokes through education randomized controlled trial. Contemporary Clinical Trials 2012;33:1065‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronish IM, Goldfinger JZ, Negron R, Fei K, Tuhrim S, Arniella G, et al. Effect of peer education on stroke prevention: the prevent recurrence of all inner‐city strokes through education randomized controlled trial. Stroke 2014;45(11):3330‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kruger 2007 {published data only}
- Kruger DJ. Documenting effectiveness in a successful infant mortality reduction program. APHA 135th Annual Meeting and Expo. 2007.
- Kruger DJ, French‐Turner T, Brownlee S. REACH windshield tours: enhancing health professionals understanding of community conditions that influence infant mortality. Journal of Primary Prevention 2013;34:163‐72. [DOI] [PubMed] [Google Scholar]
- McKellar JD, French‐Turner TM, Kruger DJ. REACH (Racial and Ethnic Approaches to Community Health) 2010: the Genesee County (Michigan) infant mortality disparity reduction initiative. NACCHO Exchange 2008;7(4):21‐3. [Google Scholar]
- Pestronk RM, Franks ML, Team R, Team HS, Team P. A partnership to reduce African American infant mortality in Genesee County, Michigan. Public Health Reports 2003;118(4):324‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Larson 2009 {published data only}
- Larson CO, Schlundt DG, Patel K, Wang H, Beard K, Hargreaves MK. Trends in smoking among African‐Americans: a description of Nashville's REACH 2010 initiative. Journal of Community Health 2009;34(4):311‐20. [DOI] [PubMed] [Google Scholar]
- McClellan L, Schlundt D. Overview of Nashville REACH 2010's approach to eliminating disparities in diabetes and cardiovascular disease. The Journal of Ambulatory Care Management 2006;29(2):106. [DOI] [PubMed] [Google Scholar]
- Miller ST, Schlundt DG, Larson C, Reid R, Pichert JW, Hargreaves M, et al. Exploring ethnic disparities in diabetes, diabetes care, and lifestyle behaviors: the Nashville REACH 2010 community baseline survey. Ethnicity & Disease 2004;14(3 Suppl 1):1‐38. [PubMed] [Google Scholar]
- Schlundt DG, Greene C, Reid R, McClellan L, Dowling L, Sheats JL, et al. An evaluation of the Nashville REACH 2010 community health screening strategy. The Journal of Ambulatory Care Management 2006;29(2):151‐61. [DOI] [PubMed] [Google Scholar]
- Schlundt DG, Larson C, Patel K, Beard K, Hargreaves MK. Nashville REACH 2010: Association of community health promotion with population prevalence estimates of BMI, physical activity, and eating behaviors. 69th Scientific Session of the American Diabetes Association. 2012.
- Schlundt DG, Mushi C, Larson CO, Marrs M. Use of innovative technologies in the evaluation of Nashville's REACH 2010 community action plan: reducing disparities in cardiovascular disease and diabetes in the African American community. The Journal of Ambulatory Care Management 2001;24(3):51. [DOI] [PubMed] [Google Scholar]
- Schlundt DG, Niebler S, Brown A, Pichert JW, McClellan L, Carpenter D, et al. Disparities in smoking: data from the Nashville REACH 2010 project. The Journal of Ambulatory Care Management 2007;30(2):150. [DOI] [PubMed] [Google Scholar]
- Schlundt DG, Patel K, Larson C, Beard K, Hargreaves MK. Nashville REACH 2010: Association of health screening with population prevalence estimates of diabetes and hypertension. 69th Scientific Session of the American Diabetes Association. 2012.
Levine 2003 {published data only}
- Levine DM, Bone LR, Hill MN, Stallings R, Gelber AC, Barker A, et al. The effectiveness of a community/academic health center partnership in decreasing the level of blood pressure in an urban African‐American population. Ethnicity & Disease 2003;13(3):354‐61. [PubMed] [Google Scholar]
Liao 2010a {published data only}
- Liao Y, Tsoh JY, Chen R, Foo MA, Garvin CC, Grigg‐Saito D, et al. Decreases in smoking prevalence in Asian communities served by the Racial and Ethnic Approaches to Community Health (REACH) Project. American Journal of Public Health 2010;100(5):853‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liao 2010b {published data only}
- Liao Y, Tucker P, Siegel P, Liburd L, Giles WH. Decreasing disparity in cholesterol screening in minority communities: findings from the Racial and Ethnic Approaches to Community Health 2010. Journal of Epidemiology and Community Health 2010;64(4):292‐9. [DOI] [PubMed] [Google Scholar]
McPhee 2003 {published data only}
- Jenkins CNH, McPhee SJ, Wong C, Nguyen T, Euler GL. Hepatitis B immunization coverage among Vietnamese‐American children 3 to 18 years old. Pediatrics 2000;106(6):e78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPhee SJ, Nguyen T, Euler GL, Mock J, Wong C, Lam T, et al. Successful promotion of hepatitis B vaccinations among Vietnamese‐American children ages 3 to 18: results of a controlled trial. Pediatrics 2003;111(6):1278‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou F, Euler GL, McPhee SJ, Nguyen T, Lam T, Wong C, et al. Economic analysis of promotion of hepatitis B vaccinations among Vietnamese‐American children and adolescents in Houston and Dallas. Pediatrics 2003;111(6):1289‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Melhuish 2010 {published data only}
- Belsky J, Melhuish E, Barnes J, Leyland AH, Romaniuk H. Effects of Sure Start Local Programmes on children and families: early findings from a quasi‐experimental, cross sectional study. British Medical Journal 2006;332(7556):1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latham P, Kapoor S, Myers P, Barnes J, Institute for the Study of Children, Families, Social Issues. Breastfeeding, Weaning and Health Eating: A Synthesis of Sure Start Local Programme Evaluation Findings. Birkbeck: Institute for the Study of Children, Families & Social Issues 2006.
- Melhuish E, Belsky J, Leyland AH. The National Evaluation of Sure Start (NESS) Team: the impact of Sure Start Local Programmes on five year olds and their families. Research report DFE‐RR067. London: Birkbeck University Department of Education; 2010.
- Melhuish E, Belsky J, Leyland AH, Barnes J. Effects of fully‐established Sure Start Local Programmes on 3‐year‐old children and their families living in England: a quasi‐experimental observational study. The Lancet 2008;372(9650):1641‐7. [DOI] [PubMed] [Google Scholar]
Merriam 2009 {published data only}
- Merriam P, Tellez T, Rosal M, Olendzki B, Ma Y, Pagoto S, et al. Methodology of a diabetes prevention translational research project utilizing a community‐academic partnership for implementation in an underserved Latino community. BMC Medical Research Methodology 2009;9(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ockene IS, Tellez TL, Rosal MC, Reed GW, Mordes J, Merriam PA, et al. Outcomes of a Latino community‐based intervention for the prevention of diabetes: the Lawrence Latino Diabetes Prevention Project. American Journal of Public Health 2012;102(2):336‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mishra 2007 {published data only}
- Mishra SI, Bastani R, Crespi CM, Chang LC, Luce PH, Baquet CR. Results of a randomized trial to increase mammogram usage among Samoan women. Cancer Epidemiology Biomarkers & Prevention 2007;16(12):2594‐604. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moskowitz 2007 {published data only}
- Chen AM, Wismer BA, Lew R, Kang SH, Min K, Moskowitz JM, et al. " Health is strength": a research collaboration involving Korean Americans in Alameda County. American Journal of Preventive Medicine 1997;13(6 Suppl):93. [PubMed] [Google Scholar]
- Moskowitz JM, Kazinets G, Wong JM, Tager IB. 'Health Is Strength': a community health education program to improve breast and cervical cancer screening among Korean American Women in Alameda County, California. Cancer Detection and Prevention 2007;31(2):173‐83. [DOI] [PubMed] [Google Scholar]
- Wismer BA, Moskowitz JM, Min K, Chen AM, Ahn Y, Cho S, et al. Interim assessment of a community intervention to improve breast and cervical cancer screening among Korean American women. Journal of Public Health Management and Practice 2001;7(2):61‐70. [DOI] [PubMed] [Google Scholar]
Nguyen 2006 {published data only}
- Lam TK, Phee SJ, Mock J, Wong C, Doan HT, Nguyen T, et al. Encouraging Vietnamese‐American women to obtain Pap tests through lay health worker outreach and media education. Journal of General Internal Medicine 2003;18(7):516‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mock J, McPhee SJ, Nguyen T, Wong C, Doan H, Lai KQ, et al. Effective lay health worker outreach and media‐based education for promoting cervical cancer screening among Vietnamese American women. American Journal of Public Health 2007;97(9):1693‐700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mock J, Nguyen T, Nguyen KH, Bui‐Tong N, McPhee SJ. Processes and capacity‐building benefits of lay health worker outreach focused on preventing cervical cancer among Vietnamese. Health Promotion Practice 2006;7(3 Suppl):223S‐32S. [DOI] [PubMed] [Google Scholar]
- Nguyen TT, McPhee SJ, Bui‐Tong N, Luong TN, Ha‐Iaconis T, Nguyen T, et al. Community‐based participatory research increases cervical cancer screening among Vietnamese‐Americans. Journal of Health Care for the Poor and Underserved 2006;17(2):31‐54. [DOI] [PubMed] [Google Scholar]
- Nguyen TT, McPhee SJ, Gildengorin G, Nguyen T, Wong C, Lai KQ, et al. Papanicolaou testing among Vietnamese Americans: results of a multifaceted intervention. American Journal of Preventive Medicine 2006;31(1):1‐9. [DOI] [PubMed] [Google Scholar]
Nguyen 2009 {published data only}
- Nguyen TT, Le G, Nguyen T, Le K, Lai K, Gildengorin G, et al. Breast cancer screening among Vietnamese Americans: a randomized controlled trial of lay health worker outreach. American Journal of Preventive Medicine 2009;37(4):306‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Paine‐Andrews 1999 {published data only}
- Paine‐Andrews A, Fisher JL, Patton JB, Fawcett SB, Williams EL, Lewis RK, et al. Analyzing the contribution of community change to population health outcomes in an adolescent pregnancy prevention initiative. Health Education & Behavior 2002;29(2):183‐93. [DOI] [PubMed] [Google Scholar]
- Paine‐Andrews A, Harris KJ, Fisher JL, Lewis RK, Williams EL, Fawcett SB, et al. Effects of a replication of a multicomponent model for preventing adolescent pregnancy in three Kansas communities. Family Planning Perspectives 1999;31(4):182‐9. [PubMed] [Google Scholar]
- Paine‐Andrews A, Vincent ML, Fawcett SB, Campuzano MK, Harris KJ, Lewis RK, et al. Replicating a community initiative for preventing adolescent pregnancy: from South Carolina to Kansas. Family and Community Health 1996;19(1):14‐30. [Google Scholar]
Paradis 2005 {published data only}
- Cargo M, Lavesque L, Macaulay AC, McComber A, Desrosiers S, Delormier T, et al. Community governance of the Kahnawake Schools Diabetes Prevention Project, Kahnawake Territory, Mohawk Nation, Canada. Health Promotion International 2003;18(3):177‐87. [DOI] [PubMed] [Google Scholar]
- Cargo MD, Delormier T, Lavesque L, McComber AM, Macaulay AC. Community capacity as an “inside job”: evolution of perceived ownership within a university‐Aboriginal community partnership. American Journal of Health Promotion 2011;26(2):96‐100. [DOI] [PubMed] [Google Scholar]
- Macaulay AC, Paradis G, Potvin L, Cross EJ, Saad‐Haddad C, McComber A, et al. The Kahnawake Schools Diabetes Prevention Project: intervention, evaluation, and baseline results of a diabetes primary prevention program with a native community in Canada. Preventive Medicine 1997;26(6):779‐90. [DOI] [PubMed] [Google Scholar]
- Paradis G, Levesque L, Macaulay AC, Cargo M, McComber A, Kirby R, et al. Impact of a diabetes prevention program on body size, physical activity, and diet among Kanien'keha: ka (Mohawk) children 6 to 11 years old: 8‐year results from the Kahnawake Schools Diabetes Prevention Project. Pediatrics 2005;115(2):333‐9. [DOI] [PubMed] [Google Scholar]
- Potvin L, Cargo M, McComber AM, Delormier T, Macaulay AC. Implementing participatory intervention and research in communities: lessons from the Kahnawake Schools Diabetes Prevention Project in Canada. Social Science & Medicine 2003;56(6):1295‐305. [DOI] [PubMed] [Google Scholar]
Parikh 2010 {published data only}
- Horowitz C, Vasquez C. Relevance and rigor: community‐based diabetes prevention. 4th International Congress on Prediabetes and Metabolic Syndrome. 2011.
- Parikh P, Simon EP, Fei K, Looker H, Goytia C, Horowitz CR. Results of a pilot diabetes prevention intervention in East Harlem, New York City: Project HEED. American Journal of Public Health 2010;100(S1):S232‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Parker 2008 {published data only}
- Edgren KK, Parker EA, Israel BA, Lewis TC, Salinas MA, Robins TG, et al. Community involvement in the conduct of a health education intervention and research project: Community Action Against Asthma. Health Promotion Practice 2005;6(3):263‐9. [DOI] [PubMed] [Google Scholar]
- Israel BA, Krieger J, Vlahov D, Ciske S, Foley M, Fortin P, et al. Challenges and facilitating factors in sustaining community‐based participatory research partnerships: lessons learned from the Detroit, New York City and Seattle Urban Research Centers. Journal of Urban Health 2006;83(6):1022‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israel BA, Lichtenstein R, Lantz P, McGranaghan R, Allen A, Guzman JR, et al. The Detroit community‐academic urban research center: development, implementation, and evaluation. Journal of Public Health Management and Practice 2001;7(5):1‐19. [DOI] [PubMed] [Google Scholar]
- Lantz PM, Viruell‐Fuentes E, Israel BA, Softley D, Guzman R. Can communities and academia work together on public health research? Evaluation results from a community‐based participatory research partnership in Detroit. Journal of Urban Health 2001;78(3):495‐507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker EA, Israel BA, Robins TG, Mentz G, Lin X, Brakefield‐Caldwell W, et al. Evaluation of Community Action Against Asthma: a community health worker intervention to improve children's asthma‐related health by reducing household environmental triggers for asthma. Health Education & Behavior 2008;35(3):376‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker EA, Israel BA, Williams M, Brakefield‐Caldwell W, Lewis TC, Robins T, et al. Community Action Against Asthma. Journal of General Internal Medicine 2003;18(7):558‐67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Plescia 2008 {published data only}
- Plescia M, Herrick H, Chavis LT. Improving health behaviors in an African American community: the Charlotte Racial and Ethnic Approaches to Community Health project. American Journal of Public Health 2008;98(9):1678‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rhodes 2009 {published data only}
- Rhodes SD, Daniel J, Alonzo J, et al. A snapshot of how Latino heterosexual men promote sexual health within their social networks: a process evaluation findings from an efficacious community‐level intervention. AIDS Education & Prevention 2012;24:514‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Duck S, Alonzo J, Daniel‐Ulloa J, Aronson RE. Using community‐based participatory research to prevent HIV disparities: assumptions and opportunities identified by the Latino partnership. Journal of AIDS 2013;63:S32‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Eng E, Hergenrather KC, Remnitz IM, Arceo R, Montao J, et al. Exploring Latino men's HIV risk using community‐based participatory research. American Journal of Health Behavior 2007;31(2):146‐58. [DOI] [PubMed] [Google Scholar]
- Rhodes SD, Hergenrather KC, Bloom FR, Leichliter JS, Montao J. Outcomes from a community‐based, participatory lay health adviser HIV/STD prevention intervention for recently arrived immigrant Latino men in rural North Carolina. AIDS Education & Prevention 2009;21(Suppl B):103‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Hergenrather KC, Montao J, Remnitz IM, Arceo R, Bloom FR, et al. Using community‐based participatory research to develop an intervention to reduce HIV and STD infections among Latino men. AIDS Education & Prevention 2006;18(5):375‐89. [DOI] [PubMed] [Google Scholar]
Rhodes 2011 {published data only}
- *Rhodes S, McCoy T, Vissman A, DiClemente R, Duck S, Hergenrather K, et al. A randomized controlled trial of a culturally congruent intervention to increase condom use and HIV testing among heterosexually active immigrant Latino men. AIDS Behavior 2011;15:1764‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes S, Hergenrather K, Vissman A, Stowers J, Davis A, Hannah A, et al. Boys must be men and men must have sex with women: a qualitative CBPR study to explore sexual risk among African American, Latino, and white gay men and MSM. American Journal of Men's Health 2011;5(2):140‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Daniel J, Alonzo J, Vissman AT, Duck S, Downs M, et al. A snapshot of how Latino heterosexual men promote sexual health within their social networks: process evaluation findings from an efficacious community‐level intervention. AIDS Education & Prevention 2012;24(5):514‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rothman 1999 {published data only}
- Rothman NL, Lourie R, Dyer A, Gass DL. A successful community‐based partnership: formation and achievements. Metropolitan Universities: An International Forum 2000;11(2):59‐62. [Google Scholar]
- Rothman NL, Lourie R, Gaughan J, White N. A community‐developed, community‐based lead poisoning prevention program: Lead Awareness North Philly Style. Holistic Nursing Practice 1999;14(1):47‐58. [DOI] [PubMed] [Google Scholar]
- Rothman NL, Lourie RJ, Gaughan J. Lead awareness: North Philly style. American Journal of Public Health 2002;92(5):739‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Saxe 2006 {published data only}
- Hallfors D, Cho H, Livert D, Kadushin C. Fighting back against substance abuse: are community coalitions winning?. American Journal of Preventive Medicine 2002;23(4):237‐45. [DOI] [PubMed] [Google Scholar]
- Lindholm M, Ryan D, Kadushin C, Saxe L, Brodsky A. 'Fighting Back' against substance abuse: the structure and function of community coalitions. Human Organization 2004;63(3):265‐76. [Google Scholar]
- Lindholm ML. Establishing program legitimacy in multiethnic settings: the Robert Wood Johnson Foundation's 'Fighting Back' program. Journal of Drug Issues 2006;36(2):351‐76. [Google Scholar]
- Saxe L, Kadushin C, Tighe E, Beveridge AA, Livert D, Brodsky A, et al. Community‐based prevention programs in the war on drugs: findings from the" Fighting Back" demonstration. Journal of Drug Issues 2006;36(2):263. [Google Scholar]
- Saxe L, Reber E, Hallfors D, Kadushin C, Jones D, Rindskopf D, et al. Think globally, act locally: assessing the impact of community‐based substance abuse prevention. Evaluation and Program Planning 1997;20(3):357‐66. [Google Scholar]
- Tighe E, Saxe L. Community‐based substance abuse reduction and the gap between treatment need and treatment utilization: analysis of data from the 'Fighting Back' general population survey. Journal of Drug Issues 2006;36(2):295‐312. [Google Scholar]
Schorling 1997 {published data only}
- Schorling JB. The stages of change of rural African‐American smokers. American Journal of Preventive Medicine 1995;11(3):170. [PubMed] [Google Scholar]
- Schorling JB, Roach J, Siegel M, Baturka N, Hunt DE, Guterbock TM, et al. A trial of church‐based smoking cessation interventions for rural African Americans. Preventive Medicine 1997;26(1):92‐101. [DOI] [PubMed] [Google Scholar]
Spencer 2011 {published data only}
- Spencer MS, Rosland AM, Kieffer EC, Sinco BR, Valerio M, Palmisano G, et al. Effectiveness of a community health worker intervention among African American and Latino adults with Type 2 diabetes: a randomized controlled trial. American Journal of Public Health 2011;101(12):2253‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stafford 2008 {published data only}
- *Stafford M, Nazroo J, Popay JM, Whitehead M. Tackling inequalities in health: evaluating the New Deal for Communities initiative. Journal of Epidemiology and Community Heatlh 2008;62(4):298‐304. [DOI] [PubMed] [Google Scholar]
- Beatty C, Foden M, Lawless P, Wilson I. New Deal for Communities: a synthesis of new programme wide evidence: 2006‐07. London: Department for Communities and Local Government 2008.
- Lawless P. Can area‐based regeneration programmes ever work?. Policy Studies 2012;33:313‐28. [Google Scholar]
- Lawless P, Foden M, Wilson I, Beatty C. Understanding area‐based regeneration: the New Deal for Communities programme in England. Urban Studies 2010;47(2):257‐75. [Google Scholar]
Thompson 2006 {published data only}
- Tejeda S, Thompson B, Coronado GD, Heagerty PJ, Martin DP. Celebremos la Salud: a community‐based intervention for Hispanic and non‐Hispanic white women living in a rural area. Journal of Community Health 2009;34(1):47‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson B, Coronado G, Chen L, Islas I. Celebremos la Salud! A community randomized trial of cancer prevention (United States). Cancer Causes and Control 2006;17(5):733‐46. [DOI] [PubMed] [Google Scholar]
Thompson 2008 {published data only}
- Thompson B, Coronado G, Puschel K, Allen E. Identifying constituents to participate in a project to control pesticide exposure in children of farmworkers. Environmental Health Perspectives 2001;109(Suppl 3):443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson B, Coronado GD, Grossman JE, Solomon CC, Islas I, Curl CL, et al. Pesticide take‐home pathway among children of agricultural workers: study design, methods, and baseline findings. Journal of Occupational and Environmental Medicine 2003;45(1):42. [DOI] [PubMed] [Google Scholar]
- Thompson B, Coronado GD, Vigoren EM, Griffith WC, Fenske RA, Kissel JC, et al. Para Niños Saludables: a community intervention trial to reduce organophosphate pesticide exposure in children of farmworkers. Environmental Health Perspectives 2008;116(5):687‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Treno 2007 {published data only}
- Treno AJ, Gruenewald PJ, Lee JP, Remer LG. The Sacramento Neighborhood Alcohol Prevention Project: outcomes from a community prevention trial. Journal of Studies on Alcohol and Drugs 2007;68(2):197‐207. [DOI] [PMC free article] [PubMed] [Google Scholar]
Voorhees 1996 {published data only}
- Levine DM, Becker DM, Bone LR, Hill MN, Tuggle MB II, Zeger SL. Community‐academic health center partnerships for underserved minority populations. Journal of the American Medical Association 1994;272(4):309‐11. [PubMed] [Google Scholar]
- Levine DM, Becker DM, Bone LR, Stillman FA, Tuggle MB, Prentice M, et al. A partnership with minority populations: a community model of effectiveness research. Ethnicity & Disease 1992;2(3):296‐305. [PubMed] [Google Scholar]
- Stillman FA, Bone LR, Rand C, Levine DM, Becker DM. Heart, Body, and Soul: a church‐based smoking‐cessation program for urban African Americans. Preventive Medicine 1993;22(3):335‐49. [DOI] [PubMed] [Google Scholar]
- Voorhees CC, Stillman FA, Swank RT, Heagerty PJ, Levine DM, Becker DM. Heart, Body, and Soul: impact of church‐based smoking cessation interventions on readiness to quit. Preventive Medicine 1996;25(3):277‐85. [DOI] [PubMed] [Google Scholar]
Wagner 2000a {published data only}
- Wagner EH, Koepsell TD, Anderman C, Cheadle A, Curry SG, Psaty BM, et al. The evaluation of the Henry J. Kaiser Family Foundation's Community Health Promotion Grant Program: Design. Journal of Clinical Epidemiology 1991;44(7):685‐99. [DOI] [PubMed] [Google Scholar]
- Wagner EH, Wickizer TM, Cheadle A, Psaty BM, Koepsell TD, Diehr P, et al. The Kaiser Family Foundation Community Health Promotion Grants Program: findings from an outcome evaluation. Health Services Research 2000;35(3):561‐89. [PMC free article] [PubMed] [Google Scholar]
- Wickizer TM, Wagner E, Cheadle A, Pearson D, Beery W, Maeser J, et al. Implementation of the Henry J. Kaiser Family Foundation's Community Health Promotion Grant Program: a process evaluation. Milbank Quarterly 1998;76(1):121‐47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wagner 2000b {published data only}
- *Wagner EH, Wickizer TM, Cheadle A, Psaty BM, Koepsell TD, Diehr P, et al. The Kaiser Family Foundation Community Health Promotion Grants Program: findings from an outcome evaluation. Health Services Research 2000;35(3):561‐89. [PMC free article] [PubMed] [Google Scholar]
Wells 2013 {published data only}
- Chung B, Jones L, Dixon EL, Miranda J, Wells K. Using a community partnered participatory research approach to implement a randomized controlled trial: planning community partners in care. Journal of Health Care for the Poor and Underserved 2010;21:780‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones L, Meade B, Forge N, et al. Begin your partnership: the process of engagement. Ethnicity & Disease 2009;19:S6‐16. [PMC free article] [PubMed] [Google Scholar]
- Jones L, Meade B, Koegel P, et al. Work through the valley: plan. Ethnicity & Disease 2009;19:S6‐8. [PMC free article] [PubMed] [Google Scholar]
- Jones L, Meade B, Norris K, et al. Develop a vision. Ethnicity & Disease 2009;19:S6‐30. [PMC free article] [PubMed] [Google Scholar]
- Jones L, Wells K, Norris K, Meade B, Koegel P. The vision, valley, and victory of community engagement. Ethnicity & Disease 2009;19:S6‐7. [PMC free article] [PubMed] [Google Scholar]
- Khodyakov D, Sharif MZ, Dixon EL, et al. An implementation evaluation of the community engagement and planning intervention in the CPIC Depression Care Improvement Trial. Community Mental Health Journal 2014;50:312‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda J, Ong MK, Jones L, et al. Community‐partnered evaluation of depression services for clients of community‐based agencies in under‐resourced communities in Los Angeles. Journal of General Internal Medicine 2013;28:1279‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells K, Koegel P, Jones L, Meade B. Work through the valley: evaluate. Ethnicity & Disease 2009;19:S6‐58. [PMC free article] [PubMed] [Google Scholar]
- Wells KB, Jones L, Chung B, Dixon EL, Tang L, Gilmore J, et al. Community‐partnered cluster‐randomized comparative effectiveness trial of community engagement and planning or resources for services to address depression disparities. Journal of General Internal Medicine 2013;28(10):1268‐78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilson 2008 {published data only}
- Wilson TE, Fraser‐White M, Feldman J, Homel P, Wright S, King G, et al. Hair salon stylists as breast cancer prevention lay health advisors for African American and Afro‐Caribbean women. Journal of Health Care for the Poor and Underserved 2008;19(1):216‐26. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Aguilar 2010 {published data only}
- Aguilar DE, Abesamis‐Mendoza N, Ursua R, Divino LAM, Cadag K, Gavin NP. Lessons learned and challenges in building a Filipino health coalition. Health Promotion Practice 2010;11(3):428‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ambrose 2009 {published data only}
- Ambrose A, Short P. Integrating health planning and social planning: a case study in community‐based partnerships for better health. Australian Journal of Primary Health 2009;15(4):294‐302. [Google Scholar]
Anaya 2010 {published data only}
- Ambrose A, Short P. Integrating health planning and social planning: a case study in community‐based partnerships for better health. Australian Journal of Primary Health 2009;15(4):294‐302. [Google Scholar]
Anderson 2006 {published data only}
- Anderson E, Shepherd M, Salisbury C. 'Taking off the suit': engaging the community in primary health care decision making. Health Expectations 2006;9(1):70‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Angell 2003 {published data only}
- Angell KL, Kreshka MA, Coy R, et al. Psychosocial intervention for rural women with breast cancer. Journal of General Internal Medicine 2003;18(7):499‐507. [DOI] [PMC free article] [PubMed] [Google Scholar]
Arcury 1999 {published data only}
- Arcury TA, Austin CK, Quandt SA, Saavedra R. Enhancing community participation in intervention research: farmworkers and agricultural chemicals in North Carolina. Health Education & Behavior 1999;26(4):563‐78. [DOI] [PubMed] [Google Scholar]
Arthur 2010 {published data only}
- Arthur MW, Hawkins JD, Brown EC, Briney JS, Oesterle S, Abbott RD. Implementation of the Communities That Care prevention system by coalitions in the Community Youth Development Study. Journal of Community Psychology 2010;38(2):245‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Atkinson 2011 {published data only}
- Atkinson J, Vallely A, Fitzgerald L, Whittaker M, Tanner M. The architecture and effect of participation: a systematic review of community participation for communicable disease control and elimination. Implications for malaria elimination. Malaria Journal 2011;10:225. [DOI] [PMC free article] [PubMed] [Google Scholar]
Babu 2006 {published data only}
- Babu BV, Behera DK, Kerketta AS, et al. Use of an inclusive‐partnership strategy in urban areas of Orissa, India, to increase compliance in a mass drug administration for the control of lymphatic filariasis. Annals of Tropical Medicine and Parasitology 2006;100(7):621‐30. [DOI] [PubMed] [Google Scholar]
Bachar 2006 {published data only}
- Bachar JJ, Lefler LJ, Reed L, McCoy T, Bailey R, Bell R. Cherokee Choices: a diabetes prevention program for American Indians. Preventing Chronic Disease 2006;3(3):1‐9. [PMC free article] [PubMed] [Google Scholar]
Bailey 2011 {published data only}
- Bailey MB, Shiau R, Zola J, et al. San Francisco Hep B Free: a grassroots community coalition to prevent hepatitis B and liver cancer. Journal of Community Health 2011;36(4):538‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Baker 1997 {published data only}
- Baker EA, Bouldin N, Durham M, et al. The Latino Health Advocacy Program: a collaborative lay health advisor approach. Health Education & Behavior 1997;24(4):495‐509. [DOI] [PubMed] [Google Scholar]
Baker 2007 {published data only}
- Baker IR, Dennison BA, Boyer PS, Sellers KF, Russo TJ, Sherwood NA. An asset‐based community initiative to reduce television viewing in New York state. Preventive Medicine 2007;44(5):437‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Balcazar 2012 {published data only}
- Balcazar H, Wise S, Rosenthal EL, et al. An ecological model using promotores de salud to prevent cardiovascular disease on the US‐Mexico border: the HEART project. Prevention of Chronic Disease 2012;9:E35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Baldwin 1999 {published data only}
- Baldwin JA. Conducting drug abuse prevention research in partnership with Native American communities: meeting challenges through collaborative approaches. Drugs & Society 1999;14(1/2):29. [Google Scholar]
Barnes 2000 {published data only}
- Barnes HM. Collaboration in community action: a successful partnership between indigenous communities and researchers. Health Promotion International 2000;15(1):17‐25. [Google Scholar]
Bazzoli 1997 {published data only}
- Bazzoli GJ, Stein R, Alexander JA, Conrad DA, Sofaer S, Shortell SM. Public‐private collaboration in health and human service delivery: evidence from community partnerships. Milbank Quarterly 1997;75(4):533‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Begley 2009 {published data only}
- Begley CE, Fourney A, Elreda D, Teleki A. Evaluating outcomes of HIV prevention programs: lessons learned from Houston, Texas. AIDS Education & Prevention 2002;14(5):432‐43. [DOI] [PubMed] [Google Scholar]
Biel 2009 {published data only}
- Biel M, Evans SH, Clarke P. Forging links between nutrition and healthcare using community‐based partnerships. Family and Community Health 2009;32(3):196‐205. [DOI] [PubMed] [Google Scholar]
Bluthenthal 2006 {published data only}
- Bluthenthal RN, Jones L, Fackler‐Lowrie N, et al. Witness for Wellness: preliminary findings from a community‐academic participatory research mental health initiative. Ethnicity & Disease 2006;16(1):S18‐34. [PubMed] [Google Scholar]
Boettcher 2008 {published data only}
- Boettcher RE, Jakes L, Sigal LM. An evaluation of a community collaboration approach to psychosocial rehabilitation. Journal of Community Practice 2008;16(2):165‐81. [Google Scholar]
Brown 1991 {published data only}
- Brown K, Chavkin N. Building a multi‐ethnic family‐school‐community partnership: coalition for PRIDE. School Community Journal 1991;1(2):33‐6. [Google Scholar]
Brown 2010 {published data only}
- Brown LD, Feinberg ME, Greenberg MT. Determinants of community coalition ability to support evidence‐based programs. Prevention Science 2010;11(3):287‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
Buchanan 1993 {published data only}
- Buchanan D, Apostol E, Balfour D, et al. The CEPA project: a new model for community‐based program planning. International Quarterly of Community Health Education 1993;14(4):361‐78. [DOI] [PubMed] [Google Scholar]
CADCA 2004 {published data only}
- Community Anti‐Drug Coalitions of America (CADCA). Working together, building safe and healthy communities: Community Capacity Development Office/Weed and Seed Initiative and community anti‐drug coalitions. CADCA. Report No.: CADCA Strategizer 47 2004.
Calman 2005 {published data only}
- Calman N. Making health equality a reality: the Bronx takes action. Health Affairs 2005;24(2):491‐8. [DOI] [PubMed] [Google Scholar]
Case 2003 {published data only}
- Case S, Haines K. Promoting prevention: preventing youth drug use in Swansea, UK, by targeting risk and protective factors. Journal of Substance Use 2003;8(4):243‐51. [Google Scholar]
Cheadle 2010 {published data only}
- Cheadle A, Egger R, LoGerfo JP, Schwartz S, Harris JR. Promoting sustainable community change in support of older adult physical activity: evaluation findings from the Southeast Seattle Senior Physical Activity Network (SESPAN). J Urban Health 2010;87(1):67‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheadle A, Egger R, LoGerfo JP, Walwick J, Schwartz S. A community‐organizing approach to promoting physical activity in older adults: the Southeast Senior Physical Activity Network. Health Promotion Practice 2010;11(2):197‐204. [DOI] [PubMed] [Google Scholar]
Cheadle 2011 {published data only}
- Cheadle A, Bourcier E, Krieger J, et al. The impact of a community‐based chronic disease prevention initiative: evaluation findings from Steps to Health King County. Health Education & Behavior 2011;38(3):222‐30. [DOI] [PubMed] [Google Scholar]
Cheadle 2012 {published data only}
- Cheadle A, Rauzon S, Spring R, et al. Kaiser Permanente's Community Health Initiative in Northern California: evaluation findings and lessons learned. American Journal of Health Promotion 2012;27:e59‐68. [DOI] [PubMed] [Google Scholar]
Chinman 1990 {published data only}
- Chinman MJ, Wandersman A. The benefits and costs of volunteering in community organizations: review and practical implications. Nonprofit Voluntary Sector Quarterly 1999;28:46‐64. [Google Scholar]
Chou 2008 {published data only}
- Chou WY, Stokes SC, Citko J, Davies B. Improving end‐of‐life care through community‐based grassroots collaboration: development of the Chinese‐American Coalition for Compassionate Care. Journal of Palliative Care 2008;24(1):31‐40. [PubMed] [Google Scholar]
Clark 2009 {published data only}
- Clark CR, Baril N, Kunicki M, et al. Addressing social determinants of health to improve access to early breast cancer detection: results of the Boston REACH 2010 Breast and Cervical Cancer Coalition Women's Health Demonstration Project. Journal of Women's Health 2009;18(5):677‐90. [DOI] [PubMed] [Google Scholar]
Claus 2012 {published data only}
- Claus JM, Dessauer M, Brennan LK. Programs and promotions: approaches by 25 Active Living by Design partnerships. American Journal of Preventive Medicine 2012;43:S320‐8. [DOI] [PubMed] [Google Scholar]
Collie‐Akers 2007 {published data only}
- Collie‐Akers V, Schultz JA, Carson V, Fawcett SB, Ronan M. REACH 2010: Kansas City Missouri. Health Promotion Practice 2009;10(2 Suppl):1185‐275. [DOI] [PubMed] [Google Scholar]
- Collie‐Akers VL, Fawcett SB, Schultz JA. Measuring progress of collaborative action in a community health effort. Revista Panamericana de Salud Pública 2013;34(6):422‐8. [PMC free article] [PubMed] [Google Scholar]
- Collie‐Akers VL, Fawcett SB, Schultz JA, Carson V, Cyprus J, Pierle JE. Analyzing a community‐based coalition's efforts to reduce health disparities and the risk for chronic disease in Kansas City, Missouri. Preventing Chronic Disease 2007;4(3):A66. [PMC free article] [PubMed] [Google Scholar]
Conrad 2003 {published data only}
- Conrad DA, Cave SH, Lucas M, et al. Community care networks: linking vision to outcomes for community health improvement. Medical Care Research and Review 2003;60(4 Suppl):95S‐129S. [DOI] [PubMed] [Google Scholar]
Cornell 2009 {published data only}
- Cornell CE, Littleton MA, Greene PG, et al. A community health advisor program to reduce cardiovascular risk among rural African‐American women. Health Education Research 2009;24(4):622‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cox 2010 {published data only}
- Cox PJ, Finkelstein DM, Perez VE, Rosenbach ML. Changes in capacity among local Coordinated Community Response Coalitions (CCRCs) supported by the DELTA program. Journal of Family Social Work 2010;13(4):375‐92. [Google Scholar]
- Cox PJ, Ortega S, Cook‐Craig PG, Conway P. Strengthening systems for the primary prevention of intimate partner violence and sexual violence: CDC's DELTA and EMPOWER programs. Journal of Family Social Work 2010;13(4):287‐96. [Google Scholar]
Cramer 2003 {published data only}
- Cramer M, Roberts S, Xu L. Evaluating community‐based programs for eliminating secondhand smoke using evidence‐based research for best practices. Family and Community Health 2007;30(2):129‐43. [DOI] [PubMed] [Google Scholar]
- Cramer ME, Mueller KJ, Harrop D. Comprehensive evaluation of a community coalition: a case study of environmental tobacco smoke reduction. Public Health Nursing 2003;20(6):464‐77. [DOI] [PubMed] [Google Scholar]
Crow 2006 {published data only}
- Crow I, France A, Hacking S. Evaluation of three Communities That Care projects in the UK. Security Journal 2006;19(1):45‐57. [Google Scholar]
Cummings 1999 {published data only}
- Cummings DM, Whetstone L, White D, et al. Rural Eastern Carolina Health (REACH): a model community health improvement program. North Carolina Medical Journal 1999;60(1):26‐8. [PubMed] [Google Scholar]
Dal Conte 2011 {published data only}
- Dal Conte I, Cucco V, Salamina G, Zambon A, Members of Giocasicuro Project. The Giocasicuro Project: results of a comprehensive intervention for the prevention and diagnosis of sexually transmitted infections among men who have sex with men in Italy. Infection 2011;39(Suppl 1):S32‐3. [Google Scholar]
Daniel 1995 {published data only}
- Daniel M, Green LW. Application of the Precede‐Proceed Planning Model in diabetes prevention and control of diabetes: a case illustration from an aboriginal community. Diabetes Spectrum 1995;8:80‐123. [Google Scholar]
Darrow 2010 {published data only}
- Darrow WW, Montanea JE, Sánchez‐Braña E. Coalition contract management as a systems change strategy for HIV prevention. Health Promotion Practice 2010;11(6):867‐75. [DOI] [PubMed] [Google Scholar]
Delp 2005 {published data only}
- Delp L, Brown M, Domenzain A. Fostering youth leadership to address workplace and community environmental health issues: a university‐school‐community partnership. Health Promotion Practice 2005;6(3):270‐85. [DOI] [PubMed] [Google Scholar]
Dulin 2011 {published data only}
- Dulin MF, Tapp H, Smith HA, Hernandez BU, Furuseth OJ. A community based participatory approach to improving health in a Hispanic population. Implementation Science 2011;6(1):38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eaker 2001 {published data only}
- Eaker ED, Jaros L, Vierkant RA, Lantz P, Remington PL. Women's Health Alliance Intervention Study: increasing community breast and cervical cancer screening. Journal of Public Health Management and Practice 2001;7(5):20‐30. [DOI] [PubMed] [Google Scholar]
Ehlers 2005 {published data only}
- Ehlers J, Palermo T. Community partners for healthy farming intervention research. Journal of Agricultural Safety and Health 2005;11(2):193‐203. [DOI] [PubMed] [Google Scholar]
Eisen 1994 {published data only}
- Eisen A. Survey of neighborhood‐based, comprehensive community empowerment initiatives. Health Education & Behavior 1994;21(2):235‐52. [DOI] [PubMed] [Google Scholar]
Elder 2013 {published data only}
- Elder JP, Ayala GX, Arredondo EM, et al. Community health partnerships for chronic disease prevention among Latinos: the San Diego Prevention Research Center. Journal of Primary Prevention 2013;34(1‐2):17‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ellis 2003 {published data only}
- Ellis BH. Mobilizing communities to reduce substance abuse in Indian country. Journal of Psychoactive Drugs 2003;35(1):89‐96. [DOI] [PubMed] [Google Scholar]
English 2008 {published data only}
- English KC, Fairbanks J, Finster CE, Rafelito A, Luna J, Kennedy M. A socioecological approach to improving mammography rates in a tribal community. Health Education & Behavior 2008;35(3):396‐409. [DOI] [PubMed] [Google Scholar]
Fawcett 1997 {published data only}
- Fawcett SB, Lewis RK, Paine‐Andrews A, et al. Evaluating community coalitions for prevention of substance abuse: the case of Project Freedom. Health Education & Behavior 1997;24(6):812‐28. [DOI] [PubMed] [Google Scholar]
Feinberg 2005 {published data only}
- Feinberg ME, Greenberg MT, Osgood DW, Sartorius J, Bontempo D. Effects of the Communities That Care model in Pennsylvania on youth risk and problem behaviors. Prevention Science 2007;8(4):261‐70. [DOI] [PubMed] [Google Scholar]
- Feinberg ME, Jones D, Greenberg MT, Osgood W, Bontempo D. Effects of the Communities That Care model in Pennsylvania on change in youth risk and problem behaviors. Prevention Science 2010;11:163‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME, Riggs NR, Greenberg MT. Social networks and community prevention coalitions. The Journal of Primary Prevention 2005;26(4):279‐98. [DOI] [PubMed] [Google Scholar]
Ferdinand 1995 {published data only}
- Ferdinand KC. Lessons learned from the Healthy Heart Community Prevention Project in reaching the African American population. Journal of Health Care for the Poor and Underserved 1997;8(3):366‐71. [DOI] [PubMed] [Google Scholar]
- Ferdinand KC. The Healthy Heart Community Prevention Project: a model for primary cardiovascular risk reduction in the African‐American population. Journal of the National Medical Association 1995;87(8 Suppl):638‐41. [PMC free article] [PubMed] [Google Scholar]
Ferdinand 2013 {published data only}
- Ferdinand AS, Paradies Y, Kelaher MA. The role of effective partnerships in an Australian place‐based intervention to reduce race‐based discrimination. Public Health Report 2013;128(Suppl 3):54‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Findley 2004 {published data only}
- Findley S, Irigoyen M, Sanchez M, et al. Community empowerment to reduce childhood immunization disparities in New York City. Ethnicity & Disease 2004;14(Suppl 1):S135‐42. [PubMed] [Google Scholar]
- Findley SE, Irigoyen M, Sanchez M, et al. Community‐based strategies to reduce childhood immunization disparities. Health Promotion Practice 2006;7(3 Suppl):191S‐200S. [DOI] [PubMed] [Google Scholar]
- Findley SE, Irigoyen M, Sanchez M, et al. Effectiveness of a community coalition for improving child vaccination rates in New York City. American Journal of Public Health 2008;98(11):1959‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Flewelling 2005 {published data only}
- Flewelling RL, Austin D, Hale K, et al. Implementing research based substance abuse prevention in communities: effects of a coalition based prevention initiative in Vermont. Journal of Community Psychology 2005;33(3):333‐53. [Google Scholar]
Flynn 2006 {published data only}
- Flynn BS, Worden JK, Bunn JY, Dorwaldt AL, Dana GS, Callas PW. Mass media and community interventions to reduce alcohol use by early adolescents. Journal of Studies on Alcohol 2006;67(1):66‐74. [DOI] [PubMed] [Google Scholar]
Forti 2002 {published data only}
- Forti EM, Koerber M. An outreach intervention for older rural African Americans. The Journal of Rural Health 2002;18(3):407‐15. [DOI] [PubMed] [Google Scholar]
Fouad 2004 {published data only}
- Fouad MN, Nagy MC, Johnson RE, Wynn TA, Partridge EE, Dignan M. The development of a community action plan to reduce breast and cervical cancer disparities between African‐American and White women. Ethnicity & Disease 2004;14(3 Suppl 1):S53‐60. [PubMed] [Google Scholar]
- Fouad MN, Partridge E, Dignan M, et al. A community‐driven action plan to eliminate breast and cervical cancer disparity: successes and limitations. Journal of Cancer Education 2006;21(1 Suppl):S91‐100. [DOI] [PubMed] [Google Scholar]
Fox 2012 {published data only}
- Fox AM, Mann DM, Ramos MA, Kleinman LC, Horowitz CR. Barriers to physical activity in East Harlem, New York. Journal of Obesity 2012;2012:719140. [DOI] [PMC free article] [PubMed] [Google Scholar]
Friedman 2014 {published data only}
- Friedman DB, Owens OL, Jackson DD, et al. An evaluation of a community‐academic‐clinical partnership to reduce prostate cancer disparities in the South. Journal of Cancer Education 2014;29:80‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Furlong 1997 {published data only}
- Furlong MJ, Casas JM, Corral C, Gordon MC. Changes in substance use patterns associated with the development of a community partnership project. Evaluation and Program Planning 1997;20(3):299‐305. [Google Scholar]
Garvin 2004 {published data only}
- Garvin CC, Cheadle A, Chrisman N, Chen R, Brunson E. A community‐based approach to diabetes control in multiple cultural groups. Ethnicity & Disease 2004;14(Suppl 1):S83‐92. [PubMed] [Google Scholar]
Garza 2009 {published data only}
- Garza MA, Abatemarco DJ, Gizzi C, Abegglen LM, Johnson‐Conley C. Transforming the cross cultural collaborative of Pierce County through assessment capacity building. Journal of Public Health Management and Practice 2009;15(1):70‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Giachello 2003 {published data only}
- Giachello AL, Arrom JO, Davis M, et al. Reducing diabetes health disparities through community‐based participatory action research: the Chicago Southeast Diabetes Community Action Coalition. Public Health Reports 2003;118(4):309‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Glasser 2003 {published data only}
- Glasser M, Holt N, Hall K, et al. Meeting the needs of rural populations through interdisciplinary partnerships. Family and Community Health 2003;26(3):230‐45. [DOI] [PubMed] [Google Scholar]
Godley 1998 {published data only}
- Godley MD, Velasquez R. Effectiveness of the Logan Square prevention project: interim results. Drugs & Society 1998;12(1‐2):87‐103. [Google Scholar]
Goodman 1996 {published data only}
- Goodman RM, Wandersman A, Chinman M, Imm P, Morrissey E. An ecological assessment of community‐based interventions for prevention and health promotion: approaches to measuring community coalitions. American Journal of Community Psychology 1996;24(1):33‐62. [DOI] [PubMed] [Google Scholar]
Greenberg 2007 {published data only}
- Greenberg, Mark T, et al. Community and team member factors that influence the early phase functioning of community prevention teams: The PROSPER project. The journal of primary prevention 2007;28(6):485‐504. [DOI] [PMC free article] [PubMed] [Google Scholar]
Griffin 2006 {published data only}
- Griffin JP, Floyd A. How to promote effective African American partnerships for community‐based HIV/AIDS planning: lessons learned from the Atlanta Regional Minority Health Network. Journal of Health Care for the Poor and Underserved 2006;17(1 Suppl):44‐52. [DOI] [PubMed] [Google Scholar]
Grigg‐Saito 2008 {published data only}
- Grigg‐Saito D, Och S, Liang S, Toof R, Silka L. Building on the strengths of a Cambodian refugee community through community‐based outreach. Health Promotion Practice 2008;9(4):415‐25. [DOI] [PubMed] [Google Scholar]
Gutierrez 2014 {published data only}
- Gutierrez J, Devia C, Weiss L, et al. Health, community, and spirituality evaluation of a multicultural faith‐based diabetes prevention program. Diabetes Educator 2014;40:214‐22. [DOI] [PubMed] [Google Scholar]
Hamamoto 2009 {published data only}
- Hamamoto MH, Derauf DD, Yoshimura SR. Building the base: two active living projects that inspired community participation. American Journal of Preventive Medicine 2009;37(6):S345‐51. [DOI] [PubMed] [Google Scholar]
Hannon 2006 {published data only}
- Hannon C, Cradock A, Gortmaker SL, et al. Play Across Boston: a community initiative to reduce disparities in access to after‐school physical activity programs for inner‐city youths. Preventing Chronic Disease 2006;3(3):1‐8. [PMC free article] [PubMed] [Google Scholar]
Harachi 1996 {published data only}
- Harachi TW, Ayers CD, Hawkins JD, Catalano RF, Cushing J. Empowering communities to prevent adolescent substance abuse: process evaluation results from a risk‐and protection‐focused community mobilization effort. The Journal of Primary Prevention 1996;16(3):233‐54. [DOI] [PubMed] [Google Scholar]
Hawkes 2007 {published data only}
- Hawkes L, May J, Earle‐Richardson G, Paap K, Santiago B, Ginley B. Identifying the occupational health needs of migrant workers. Journal of Community Practice 2007;15(3):57‐76. [Google Scholar]
Hawkins 2012 {published data only}
- Brown EC, Hawkins JD, Arthur MW, Briney JS, Abbott RD. Effects of Communities That Care on prevention services systems: finding from the community youth development study at 1.5 years. Prevention Science 2007;8(3):180‐91. [DOI] [PubMed] [Google Scholar]
- Fagan AA, Arthur MW, Hanson K, Briney JS, Hawkins JD. Effects of Communities That Care on the adoption and implementation fidelity of evidence‐based prevention programs in communities: results from a randomized controlled trial. Prevention Science 2011;3:1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagan AA, Brooke‐Weiss B, Cady R, Hawkins JD. If at first you don't succeed...keep trying: strategies to enhance coalition/school partnerships to implement school‐based prevention programming. Australia & New Zealand Journal of Criminology 2009;42(3):387‐405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagan AA, Hawkins JD, Catalano RF. Using community epidemiologic data to improve social settings: the Communities That Care prevention system. In: Shinn M, Yoshikawa H editor(s). Toward Positive Youth Development: Transforming Schools and Community Programs. New York: Oxford University Press, 2008:292‐313. [Google Scholar]
- Hawkins JD, Oesterle S, Brown EC, Monahan KC, Abbott RD, Arthur MW, et al. Sustained decreases in risk exposure and youth problem behaviors after installation of the Communities That Care prevention system in a randomized trial. Archives of Pediatrics and Adolescent Medicine 2012;166(1):141‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Helitzer 2009 {published data only}
- Helitzer D, Willging C, Hathorn G, Benally J. Building community capacity for agricultural injury prevention in a Navajo community. Journal of Agricultural Safety and Health 2009;15(1):19‐35. [DOI] [PubMed] [Google Scholar]
Higginbotham 1999 {published data only}
- Higginbotham N, Heading G, McElduff P, Dobson A, Heller R. Reducing coronary heart disease in the Australian Coalfields: evaluation of a 10‐year community intervention. Social Science & Medicine 1999;48(5):683‐92. [DOI] [PubMed] [Google Scholar]
Higgins 2005 {published data only}
- Higgins JW, Rickert T. A taste of healthy living: a recreational opportunity for people at risk of developing type 2 diabetes. Leisure Sciences 2005;27(5):439‐58. [Google Scholar]
Hingson 1996 {published data only}
- Hingson R, McGovern T, Howland J, Heeren T, Winter M, Zakocs R. Reducing alcohol‐impaired driving in Massachusetts: the Saving Lives Program. American Journal of Public Health 1996;86(6):791‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hinton 2005 {published data only}
- Hinton A, Downey J, Lisovicz N, Mayfield‐Johnson S, White‐Johnson F. The Community Health Advisor Program and the Deep South Network for Cancer Control: health promotion programs for volunteer community health advisors. Family and Community Health 2005;28(1):20‐7. [DOI] [PubMed] [Google Scholar]
Holliday 2008 {published data only}
- Holliday CS. Understanding member engagement through participation and commitment in a community‐based health coalition, 1994‐2008: a mixed‐methodological study. Dissertation, Georgia State University 2008; Vol. http://scholarworks.gus.edu/psych_diss/49 (accessed 25 August, 2011):1‐127.
Horen 2003 {published data only}
- Horen N, Perry DF, Woodbridge M. Dejándolo en manos de la gente: la transformación del papel de los vecinos de North Capitol Community. Apuntes de Psicología 2003;21(3):509‐19. [Google Scholar]
Hull 2010 {published data only}
- Hull PC, Canedo JR, Reece MC, et al. Using a participatory research process to address disproportionate Hispanic cancer burden. Journal of Health Care for the Poor and Underserved 2010;21(1 Suppl):95‐113. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hunte 2004 {published data only}
- Hunte HE, Turner TM, Pollack HA, Lewis EY. A birth records analysis of the Maternal Infant Health Advocate Service program: a paraprofessional intervention aimed at addressing infant mortality in African Americans. Ethnicity & Disease 2004;14(3 Suppl 1):S102‐7. [PubMed] [Google Scholar]
Hussein 2014 {published data only}
- Hussein CA, Luckner M, Samson R, et al. Working with communities to achieve health equity in Maryland's five health enterprise zones. Journal of Health Care for the Poor and Underserved 2014;25:4‐10. [DOI] [PubMed] [Google Scholar]
Jenkins 2004 {published data only}
- Jenkins C, McNary S, Carlson BA, et al. Reducing disparities for African Americans with diabetes: progress made by the REACH 2010 Charleston and Georgetown Diabetes Coalition. Public Health Reports 2004;119(3):322‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins C, Myers P, Heidari K, Kelechi TJ, Buckner‐Brown J. Efforts to decrease diabetes‐related amputations in African Americans by the Racial and Ethnic Approaches to Community Health Charleston and Georgetown Diabetes Coalition. Family and Community Health 2011;34(1S):S63‐78. [DOI] [PubMed] [Google Scholar]
Jernigan 2012 {published data only}
- Jernigan VB, Salvatore AL, Styne DM, Winkleby M. Addressing food insecurity in a Native American reservation using community‐based participatory research. Health Education Research 2012;27:645‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaufman 1994 {published data only}
- Kaufman JS, Jason LA, Sawlski LM, Halpert JA. A comprehensive multi‐media program to prevent smoking among black students. Journal of Drug Education 1994;24(2):95‐108. [DOI] [PubMed] [Google Scholar]
Kegler 1998 {published data only}
- Kegler MC, Steckler A, Mcleroy K, Malek SH. Factors that contribute to effective community health promotion coalitions: a study of 10 Project ASSIST coalitions in North Carolina. Health Education & Behavior 1998;25(3):338‐53. [DOI] [PubMed] [Google Scholar]
Kegler 2003 {published data only}
- Kegler MC, Stern R, Whitecrow‐Ollis S, Malcoe LH. Assessing lay health advisor activity in an intervention to prevent lead poisoning in Native American children. Health Promotion Practice 2003;4(2):189‐96. [DOI] [PubMed] [Google Scholar]
Keys 2001 {published data only}
- Keys CB, Factor AR. Building community coalitions with people with disabilities and their families. Journal of Prevention & Intervention in the Community 2001;21(2):91‐112. [Google Scholar]
Kieffer 2004 {published data only}
- Kieffer EC, Willis SK, Odoms‐Young AM, et al. Reducing disparities in diabetes among African‐American and Latino residents of Detroit: the essential role of community planning focus groups. Ethnicity & Disease 2004;14(3):S27‐37. [PubMed] [Google Scholar]
Klerman 2005 {published data only}
- Klerman LV, Santelli JS, Klein JD. So what have we learned? The Editors' comments on the coalition approach to teen pregnancy. Journal of Adolescent Health 2005;37(3 Suppl):S115‐8. [DOI] [PubMed] [Google Scholar]
Klevens 2008 {published data only}
- Klevens J, Baker CK, Shelley GA, Ingram EM. Exploring the links between components of coordinated community responses and their impact on contact with intimate partner violence services. Violence Against Women 2008;14(3):346‐58. [DOI] [PubMed] [Google Scholar]
Komro 2001 {published data only}
- Komro KA, Perry CL, Williams CL, Stigler MH, Farbakhsh K, Veblen‐Mortenson S. How did Project Northland reduce alcohol use among young adolescents? Analysis of mediating variables. Health Education Research 2001;16(1):59‐70. [DOI] [PubMed] [Google Scholar]
Krishnan 2011 {published data only}
- Krishnan A, Ekowati R, Baridalyne N, Kusumawardani N, Kapoor SK, Leowski J. Evaluation of community‐based interventions for non‐communicable diseases: experiences from India and Indonesia. Health Promotion International 2011;26(3):276‐89. [DOI] [PubMed] [Google Scholar]
Lara 2009 {published data only}
- Lara M, Ramos Valencia G, Gonzalez Gavillon JA, et al. Reducing inequities among children with asthma in the island of Puerto Rico. Journal of Health Care for the Poor and Underserved 2009;20(4 Suppl):116‐36. [DOI] [PubMed] [Google Scholar]
Lee 2008 {published data only}
- Lee KS, Conigrave KM, Clough AR, Wallace C, Silins E, Rawles J. Evaluation of a community‐driven youth initiative in Arnhem Land, Northern Territory, Australia. Drug and Alcohol Review 2008;27(1):75‐82. [DOI] [PubMed] [Google Scholar]
Leviton 2006 {published data only}
- Leviton LC, Cassidy EF. Engaging Coalitions to Improve Health and Health Care. Engaging Coalitions to Improve Health and Health Care: Robert Wood Johnson Foundation Anthology. San Francisco, CA: Jossey‐Bass, 2006. [Google Scholar]
Lewis 1996 {published data only}
- Lewis RK, Paine‐Andrews A, Fawcett SB, et al. Evaluating the effects of a community coalition's efforts to reduce illegal sales of alcohol and tobacco products to minors. Journal of Community Health 1996;21(6):429‐36. [DOI] [PubMed] [Google Scholar]
Lewis 1999 {published data only}
- Lewis RK, Paine‐Andrews A, Fisher J, Custard C, Fleming‐Randle M, Fawcett SB. Reducing the risk for adolescent pregnancy: evaluation of a school/community partnership in a Midwestern military community. Family and Community Health 1999;22(2):16‐30. [Google Scholar]
Lewis 2005 {published data only}
- Lewis LVB, Galloway‐Gilliam L, Flynn G, Nomachi J, Keener LTC, Sloane DC. Transforming the urban food desert from the grassroots up: a model for community change. Family and Community Health 2011;34(1Suppl):S92‐101. [DOI] [PubMed] [Google Scholar]
- Lewis LVB, Sloane DC, Nascimento LM, et al. African Americans' access to healthy food options in South Los Angeles restaurants. American Journal of Public Health 2005;95(4):668‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 2007 {published data only}
- Li Y, Hotta M, Shi A, et al. Malnutrition improvement for infants under 18 months old of Dai minority in Luxi, China. Pediatrics International 2007;49(2):273‐9. [DOI] [PubMed] [Google Scholar]
Lisovicz 2006 {published data only}
- Lisovicz N, Johnson RE, Higginbotham J, et al. The Deep South Network for Cancer Control. Cancer 2006;107(S8):1971‐9. [DOI] [PubMed] [Google Scholar]
Lohrmann 2005 {published data only}
- Lohrmann DK, Alter RJ, Greene R, Younoszai TM. Long‐term impact of a district‐wide school/community‐based substance abuse prevention initiative on gateway drug use. Journal of Drug Education 2005;35(3):233‐53. [DOI] [PubMed] [Google Scholar]
Lyon 2009 {published data only}
- Lyon D, Knowles J, Slater B, Kennedy R. Improving the early presentation of cancer symptoms in disadvantaged communities: putting local people in control. British Journal of Cancer 2009;101:S49‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ma'at 2001 {published data only}
- Ma'at I, Fouad M, Grigg‐Saito D, et al. REACH 2010: a unique opportunity to create strategies to eliminate health disparities among women of color. American Journal of Health Studies 2001;17(2):93‐101. [Google Scholar]
Ma 2004 {published data only}
- Ma GX, Toubbeh JI, Su X, Edwards RL. ATECAR: an Asian American community‐based participatory research model on tobacco and cancer control. Health Promotion Practice 2004;5(4):382‐94. [DOI] [PubMed] [Google Scholar]
Maciak 1998 {published data only}
- Maciak BJ, Moore MT, Leviton LC, Guinan ME. Preventing Halloween arson in an urban setting: a model for multisectoral planning and community participation. Health Education and Behavior 1998;25(2):194‐211. [DOI] [PubMed] [Google Scholar]
Marcus 2004 {published data only}
- Marcus MT, Walker T, Swint JM, et al. Community‐based participatory research to prevent substance abuse and HIV/AIDS in African‐American adolescents. Journal of Interprofessional Care 2004;18(4):347‐59. [DOI] [PubMed] [Google Scholar]
Martinez 2014 {published data only}
- Martinez O, Roth AM, Kelle G, Downs M, Rhodes SD. Adaptation and implementation of HoMBReS: a community‐level, evidence‐based HIV behavioral intervention for heterosexual Latino men in the midwestern United States. AIDS Education and Prevention 2014;26:68‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
McCloskey 2011 {published data only}
- McCloskey J, Tollestrup K, Sanders M. A community integration approach to social determinants of health in New Mexico. Family and Community Health 2011;34(Suppl 1):S79‐91. [DOI] [PubMed] [Google Scholar]
McElmurry 2009 {published data only}
- McElmurry BJ, McCreary LL, Park CG, et al. Implementation, outcomes, and lessons learned from a collaborative primary health care program to improve diabetes care among urban Latino populations. Health Promotion Practice 2009;10(2):293‐302. [DOI] [PubMed] [Google Scholar]
McFarlane 1994 {published data only}
- McFarlane J, Fehir J. De Madres M. A community, primary health care program based on empowerment. Health Education & Behavior 1994;21(3):381‐94. [DOI] [PubMed] [Google Scholar]
- McFarlane J, Kelly E, Rodriguez R, Fehir J, Madres M. Women building community coalitions for health. Health Care for Women International 1994;15(5):465‐76. [DOI] [PubMed] [Google Scholar]
McKay 2004 {published data only}
- McKay MM, Gopalan G, Franco LM, et al. It takes a village to deliver and test child and family‐focused services. Research on Social Work Practice 2010;20(5):476‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay MMK, Chasse KT, Paikoff R, et al. Family‐level impact of the CHAMP family program: a community collaborative effort to support urban families and reduce youth HIV risk exposure. Family Process 2004;43(1):79‐93. [DOI] [PubMed] [Google Scholar]
McKeever 2004 {published data only}
- McKeever C, Faddis C, Koroloff N, Henn J. Wellness Within REACH: Mind, Body, and Soul: a no‐cost physical activity program for African Americans in Portland, Oregon, to combat cardiovascular disease. Ethnicity & Disease 2004;14(3 Suppl 1):S93‐101. [PubMed] [Google Scholar]
Miao 2011 {published data only}
- Miao TA, Umemoto K, Gonda D, Hishinuma ES. Essential elements for community engagement in evidence‐based youth violence prevention. American Journal of Community Psychology 2011;48(1):120‐32. [DOI] [PubMed] [Google Scholar]
Michelen 2006 {published data only}
- Michelen W, Martinez J, Lee A, Wheeler DP. Reducing frequent flyer emergency department visits. Journal of Health Care for the Poor and Underserved 2006;17(1Suppl):59‐69. [DOI] [PubMed] [Google Scholar]
Minkler 2006 {published data only}
- Minkler M, Vásquez VB, Warner JR, Steussey H, Facente S. Sowing the seeds for sustainable change: a community‐based participatory research partnership for health promotion in Indiana, USA and its aftermath. Health Promotion International 2006;21(4):293‐300. [DOI] [PubMed] [Google Scholar]
Minkler 2010 {published data only}
- Minkler M, Garcia AP, Williams J, LoPresti T, Lilly J. Sí se puede: using participatory research to promote environmental justice in a Latino community in San Diego, California. Journal of Urban Health 2010;87(5):796‐812. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mishra 2009 {published data only}
- Mishra SI, Luce PH, Baquet CR. Increasing Pap smear utilization among Samoan women: results from a community based participatory randomized trial. Journal of Health Care for the Poor and Underserved 2009;20(2 Suppl):85‐101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Monks 2010 {published data only}
- Monks R. Evaluation of a neighbourhood health and wellbeing programme: Rob Monks and colleagues report on the findings of an evaluation of Neighbourhood Renewal Foundation health and wellbeing projects. Primary Health Care 2010;19(3):34. [Google Scholar]
Moore 2010 {published data only}
- Moore D, Carr CA, Williams C, Richlen W, Huber M, Wagner J. An ecological approach to addressing HIV/AIDS in the African American community. Journal of Evidence‐Based Social Work 2010;7(1‐2):144‐61. [DOI] [PubMed] [Google Scholar]
Morita 2006 {published data only}
- Morita J. Addressing racial and ethnic disparities in adult immunization, Chicago. Journal of Public Health Management and Practice 2006;12(4):321‐9. [DOI] [PubMed] [Google Scholar]
Nargiso 2013 {published data only}
- Nargiso JE, Friend KB, Egan C, et al. Coalitional capacities and environmental strategies to prevent underage drinking. American Journal of Community Psychology 2013;51:222‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nelson 2005 {published data only}
- Nelson TF, Weitzman ER, Wechsler H. The effect of a campus‐community environmental alcohol prevention initiative on student drinking and driving: results from the 'A Matter of Degree' program evaluation. Traffic Injury Prevention 2005;6(4):323‐30. [DOI] [PubMed] [Google Scholar]
Nicholas 2005 {published data only}
- Nicholas SW, Hutchinson VE, Ortiz B, Klihr‐Beall S, Jean‐Louis BSK. Reducing childhood asthma through community‐based service delivery‐‐New York City, 2001‐2004. MMWR: Morbidity & Mortality Weekly Report 2005;54:11‐4. [PubMed] [Google Scholar]
Northridge 2000 {published data only}
- Northridge ME, Vallone D, Merzel C, et al. The adolescent years: an academic‐community partnership in Harlem comes of age. Journal of Public Health Management and Practice 2000;6(1):53‐60. [DOI] [PubMed] [Google Scholar]
Okafor 2003 {published data only}
- Okafor CB. Maternal and child health project in Nigeria. Journal of National Black Nurses' Association 2003;14(2):51‐8. [PubMed] [Google Scholar]
Okwumabua 1997 {published data only}
- Okwumabua JO, Martin B, Clayton‐Davis J, Pearson CM. Stroke Belt Initiative: the Tennessee experience. Journal of Health Care for the Poor and Underserved 1997;8(3):292‐9. [DOI] [PubMed] [Google Scholar]
Olaseha 2006 {published data only}
- Olaseha IO, Sridhar MKC. Participatory action research: community diagnosis and intervention in controlling urinary schistosomiasis in an urban community in Ibadan, Nigeria. International Quarterly of Community Health Education 2006;24(2):153‐60. [DOI] [PubMed] [Google Scholar]
Operario 2005 {published data only}
- Operario D, Nemoto T, Ng T, Syed J, Mazarei M. Conducting HIV interventions for Asian Pacific Islander men who have sex with men: challenges and compromises in community collaborative research. AIDS Education and Prevention 2005;17(4):334‐46. [DOI] [PubMed] [Google Scholar]
Paine‐Andrews 1997 {published data only}
- Paine‐Andrews A, Fawcett SB, Richter KP, Berkley JY, Williams EL, Lopez CM. Community coalitions to prevent adolescent substance abuse: the case of the 'Project Freedom' replication initiative. Adolescent Health Care: Program Designs and Services 1997;14(1‐2):81‐99. [Google Scholar]
Painter 2001 {published data only}
- Painter C, Clarence E. UK local action zones and changing urban governance. Urban Studies 2001;38(8):1215‐32. [Google Scholar]
Pargee 1999 {published data only}
- Pargee D, Lara‐Albers E, Puckett K. Building on tradition: promoting physical activity with American Indian community coalitions. Journal of Health Education 1999;30(2):S37‐43. [Google Scholar]
Pazoki 2007 {published data only}
- Pazoki R, Nabipour I, Seyednezami N, Imami S. Effects of a community‐based healthy heart program on increasing healthy women's physical activity: a randomized controlled trial guided by community‐based participatory research (CBPR). BMC Public Health 2007;7(1):216. [DOI] [PMC free article] [PubMed] [Google Scholar]
Perera 2002 {published data only}
- Perera FP, Illman SM, Kinney PL, et al. The challenge of preventing environmentally related disease in young children: community‐based research in New York City. Environmental Health Perspectives 2002;110(2):197‐204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Perry 1996 {published data only}
- Perry CL, Williams CL, Komro KA, et al. Project Northland: long‐term outcomes of community action to reduce adolescent alcohol use. Health Education Research 2002;17(1):117‐32. [DOI] [PubMed] [Google Scholar]
- Perry CL, Williams CL, Veblen‐Mortenson S, et al. Project Northland. Outcomes of a communitywide alcohol use prevention program during early adolescence. American Journal of Public Health 1996;86(7):956‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Person 1996 {published data only}
- Person B, Cotton D. A model of community mobilization for the prevention of HIV in women and infants: prevention of HIV in women and infants demonstration projects. Public Health Reports 1996;111(Suppl 1):89‐98. [PMC free article] [PubMed] [Google Scholar]
Plochg 2013 {published data only}
- Plochg T, Schmidt M, Klazinga NS, Stronks K. Health governance by collaboration: a case study on an area‐based programme to tackle health inequalities in the Dutch city of the Hague. European Journal of Public Health 2013;23:939‐46. [DOI] [PubMed] [Google Scholar]
Pullen‐Smith 2008 {published data only}
- Pullen‐Smith B, Carter‐Edwards L, Leathers KH. Community health ambassadors: a model for engaging community leaders to promote better health in North Carolina. Journal of Public Health Management and Practice 2008;14(6):S73‐81. [DOI] [PubMed] [Google Scholar]
Quandt 2001 {published data only}
- Quandt SA, Arcury TA, Austin CK, Cabrera LF. Preventing occupational exposure to pesticides: using participatory research with Latino farmworkers to develop an intervention. Journal of Immigrant Health 2001;3(2):85‐96. [DOI] [PubMed] [Google Scholar]
- Quandt SA, Arcury TA, Pell AI. Something for everyone? A community and academic partnership to address farmworker pesticide exposure in North Carolina. Environmental Health Perspectives 2001;109(Suppl 3):435‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quandt SA, Grzywacz JG, Talton JW, et al. Evaluating the effectiveness of a lay health promoter‐led, community‐based participatory pesticide safety intervention with farmworker families. Health Promotion Practice 2013;14:425‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Quigley 2000 {published data only}
- Quigley D, Sanchez V, Handy D, Goble R, George P. Participatory research strategies in nuclear risk management for native communities. Journal of Health Communication 2000;5(4):305‐31. [DOI] [PubMed] [Google Scholar]
Raphael 2003 {published data only}
- Raphael D. Bridging the gap between knowledge and action on the societal determinants of cardiovascular disease: how one Canadian community effort hit‐and hurdled‐the lifestyle wall. Health Education 2003;103(3):177‐89. [Google Scholar]
Rapkin 2006 {published data only}
- Rapkin BD, Massie MJ, Jansky EJ, Lounsbury DW, Murphy PD, Powell S. Developing a partnership model for cancer screening with community‐based organizations: the ACCESS breast cancer education and outreach project. American Journal of Community Psychology 2006;38(3):153‐64. [DOI] [PubMed] [Google Scholar]
Redmond 2009 {published data only}
- Redmond C, Spoth RL, Shin C, Schainker LM, Greenberg MT, Feinberg M. Long‐term protective factor outcomes of evidence‐based interventions implemented by community teams through a community‐university partnership. The Journal of Primary Prevention 2009;30(5):513‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reifsnider 2010 {published data only}
- Reifsnider E, Hargraves M, Williams KJ, Cooks J, Hall V. Shaking and rattling: developing a child obesity prevention program using a faith‐based community approach. Family and Community Health 2010;33(2):144‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rodriguez 1993 {published data only}
- Rodriguez R, McFarlane J, Mahon J, Fehir J. De madres a madres: a community partnership to increase access to prenatal care. Bulletin of the Pan American Health Organization (PAHO) 1993;27(4):403‐8. [PubMed] [Google Scholar]
Rohrbach 1997 {published data only}
- Rohrbach LA, Johnson CA, Mansergh G, Fishkin SA, Neumann FB. Alcohol‐related outcomes of the Day One community partnership. Evaluation and Program Planning 1997;20(3):315‐22. [Google Scholar]
Rowe 1997 {published data only}
- Rowe WE. Changing ATOD norms and behaviors: a Native American community commitment to wellness. Evaluation and Program Planning 1997;20(3):323‐33. [Google Scholar]
Saewyc 2008 {published data only}
- Saewyc EM, Solsvig W, Edinburgh L. The Hmong Youth Task Force: evaluation of a coalition to address the sexual exploitation of young runaways. Public Health Nursing 2008;25(1):69‐76. [DOI] [PubMed] [Google Scholar]
Sanigorski 2008 {published data only}
- Sanigorski AM, Bell AC, Kremer PJ, Cuttler R, Swinburn BA. Reducing unhealthy weight gain in children through community capacity‐building: results of a quasi‐experimental intervention program, Be Active Eat Well. International Journal of Obesity 2008;32(7):1060‐7. [DOI] [PubMed] [Google Scholar]
Schensul 1999 {published data only}
- Schensul JJ. Organizing community research partnerships in the struggle against AIDS. Health Education & Behavior 1999;26(2):266‐83. [DOI] [PubMed] [Google Scholar]
Schulz 2001 {published data only}
- Schulz AJ, Israel BA, Parker EA, Lockett M, Hill Y, Wills R. The East Side Village Health Worker Partnership: integrating research with action to reduce health disparities. Public Health Reports 2001;116(6):548‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz AJ, Parker EA, Israel BA, Allen A, Decarlo M, Lockett M. Addressing social determinants of health through community‐based participatory research: the East Side Village Health Worker Partnership. Health Education & Behavior 2002;29(3):326‐41. [DOI] [PubMed] [Google Scholar]
Schwarte 2010 {published data only}
- Schwarte L, Samuels SE, Capitman J, Ruwe M, Boyle M, Flores G. The Central California Regional Obesity Prevention Program: changing nutrition and physical activity environments in California's heartland. American Journal of Public Health 2010;100(11):2124‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Serpas 2013 {published data only}
- Serpas S, Brandstein K, McKennett M, Hillidge S, Zive M, Nader PR. San Diego Healthy Weight Collaborative: a systems approach to address childhood obesity. Journal of Health Care for the Poor and Underserved 2013;24:80‐96. [DOI] [PubMed] [Google Scholar]
Shaw 1997 {published data only}
- Shaw RA, Rosati MJ, Salzman P, Coles CR, McGeary C. Effects on adolescent ATOD behaviors and attitudes of a 5‐year community partnership. Evaluation and Program Planning 1997;20(3):307‐13. [Google Scholar]
Shearer 2005 {published data only}
- Shearer DL, Gyaben SL, Gallagher KM, Klerman LV. Selecting, implementing, and evaluating teen pregnancy prevention interventions: lessons from the CDC's Community Coalition Partnership Programs for the Prevention of Teen Pregnancy. Journal of Adolescent Health 2005;37(3):S42‐52. [DOI] [PubMed] [Google Scholar]
Shortell 2002b {published data only}
- Shortell SM, Zukoski AP, Alexander JA, et al. Evaluating partnerships for community health improvement: tracking the footprints. Journal of Health Politics, Policy and Law 2002;27(1):49‐92. [DOI] [PubMed] [Google Scholar]
Sloane 2003 {published data only}
- Sloane DC, Diamant AL, Lewis LVB, et al. Improving the nutritional resource environment for healthy living through community‐based participatory research. Journal of General Internal Medicine 2003;18(7):568‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Solomon 2012 {published data only}
- Solomon E, Rees T, Ukoumunne OC, Hillsdon M. The Devon Active Villages Evaluation (DAVE) trial: study protocol of a stepped wedge cluster randomised trial of a community‐level physical activity intervention in rural southwest England. International Journal of Behavior Nutrition and Physical Activity 2012;12:581. [DOI] [PMC free article] [PubMed] [Google Scholar]
Somerville 2012 {published data only}
- Somerville M, Mueller C, Boddie‐Willis C, Folkemer D, Grossman E. Hospital community benefits after the ACA: partnerships for community health improvement. The Hilltop Institute 2012;Winter:1‐41. [Google Scholar]
Sorkin 2013 {published data only}
- Sorkin DH, Biegler KA, Peyreda M, Kilgore D, Dow E, Ngo‐Metzger Q. Unidas por la Vida (United for Life): implementing a culturally‐tailored, community‐based, family‐oriented lifestyle intervention. Journal of Health Care for the Poor and Underserved 2013;24:116‐38. [DOI] [PubMed] [Google Scholar]
Spielman 2006 {published data only}
- Spielman SE, Golembeski CA, Northridge ME, et al. Interdisciplinary planning for healthier communities: findings from the Harlem Children's Zone Asthma Initiative. Journal of the American Planning Association 2006;72(1):100‐8. [Google Scholar]
Splett 2006 {published data only}
- Splett PL, Erickson CD, Belseth SB, Jensen C. Evaluation and sustainability of the Healthy Learners Asthma Initiative. Journal of School Health 2006;76(6):276‐82. [DOI] [PubMed] [Google Scholar]
Spoth 2004 {published data only}
- Crowley DM, Greenberg MT, Feinberg ME, Spoth RL, Redmond CR. The effect of the PROSPER partnership model on cultivating local stakeholder knowledge of evidence‐based programs: a five‐year longitudinal study of 28 communities. Prevention Science 2012;13:96‐105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowley KM, Yu P, Kaftarian SJ. Prevention actions and activities make a difference: a structural equation model of coalition building. Evaluation and Program Planning 2000;23(3):381‐8. [Google Scholar]
- Spoth R, Greenberg M, Bierman K, Redmond C. PROSPER community‐university partnership model for public education systems: capacity‐building for evidence‐based, competence‐building prevention. Prevention Science 2004;5(1):31‐9. [DOI] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Clair S, Shin C, Greenberg M, Feinberg M. Preventing substance misuse through community‐university partnerships: randomized controlled trial outcomes 4 years past baseline. American Journal of Preventive Medicine 2011;40(4):440‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Shin C, Greenberg M, Clair S, Feinberg M. Substance‐use outcomes at 18 Months past baseline: the PROSPER Community University Partnership Trial. American Journal of Preventive Medicine 2007;32(5):395‐402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth RL, Greenberg MT. Toward a comprehensive strategy for effective practitioner scientist partnerships and larger‐scale community health and well‐being. American Journal of Community Psychology 2005;35(3):107‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Spoth 2011 (2) {published data only}
- Spoth R, Guyll M, Redmond C, Greenberg M, Feinberg M. Six‐year sustainability of evidence‐based intervention implementation quality by community‐university partnerships: the PROSPER study. American Journal of Community Psychology 2011;48:412‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Steckler 1992 {published data only}
- Steckler A, Orville K, Eng E, Dawson L. Summary of a formative evaluation of PATCH. Journal of Health Education 1992;23(3):174‐8. [Google Scholar]
Stevens 2003 {published data only}
- Stevens G, Seedat M, Phil D, Swart TM, Walt C. Promoting methodological pluralism, theoretical diversity and interdisciplinarity through a multi‐leveled violence prevention initiative in South Africa. Journal of Prevention & Intervention in the Community 2003;25(1):11‐29. [Google Scholar]
Tate 2003 {published data only}
- Tate RB, Fernandez N, Yassi A, Canizares M, Spiegel J, Bonet M. Change in health risk perception following community intervention in Central Havana, Cuba. Health Promotion International 2003;18(4):279‐86. [DOI] [PubMed] [Google Scholar]
TenBrink 2009 {published data only}
- TenBrink DS, McMunn R, Panken S. Project U‐Turn: increasing active transportation in Jackson, Michigan. American Journal of Preventive Medicine 2009;37(6):S329‐35. [DOI] [PubMed] [Google Scholar]
Tsui 2012 {published data only}
- Tsui E, Bylander K, Cho M, Maybank A, Freudenberg N. Engaging youth in food activism in New York City: lessons learned from a youth organization, health department, and university partnership. Journal of Urban Health 2012;89:809‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Turner 1995 {published data only}
- Turner LW, Sutherland M, Harris GJ, Barber M. Cardiovascular health promotion in north Florida African‐American churches. Health Values: The Journal of Health Behavior, Education & Promotion 1995;19(2):3‐9. [Google Scholar]
Two Feathers 2005 {published data only}
- Two Feathers J, Kieffer EC, Palmisano G, et al. Racial and Ethnic Approaches to Community Health (REACH) Detroit partnership: improving diabetes‐related outcomes among African American and Latino adults. American Journal of Public Health 2005;95(9):1552‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Urban 1995 {published data only}
- Urban N, Taplin SH, Taylor VM, et al. Community organization to promote breast cancer screening among women ages 50‐75. Preventive Medicine 1995;24(5):477‐84. [DOI] [PubMed] [Google Scholar]
Watson‐Thompson 2008 {published data only}
- Watson‐Thompson J, Fawcett SB, Schultz JA. Differential effects of strategic planning on community change in two urban neighborhood coalitions. American Journal of Community Psychology 2008;42(1):25‐38. [DOI] [PubMed] [Google Scholar]
Williams 1999 {published data only}
- Williams LC, Olano VR. Mobilizing and maintaining a coalition to promote physical activity among African Americans in Southeast Stockton, California. Journal of Health Education 1999;30(2):S31‐6. [Google Scholar]
Wynn 2006 {published data only}
- Wynn TA, Johnson RE, Fouad M, et al. Addressing disparities through coalition building: Alabama REACH 2010 lessons learned. Journal of Health Care for the Poor and Underserved 2006;17(2 Suppl):55‐77. [DOI] [PubMed] [Google Scholar]
Yancey 2004 {published data only}
- Yancey AK, Lewis LB, Guinyard JJ, et al. Putting promotion into practice: the African Americans Building a Legacy of Health organizational wellness program. Health Promotion Practice 2006;7(3 Suppl):233S‐246S. [DOI] [PubMed] [Google Scholar]
- Yancey AK, Lewis LB, Sloane DC, et al. Leading by example: a local health department‐community collaboration to incorporate physical activity into organizational practice. Journal of Public Health Management and Practice 2004;10(2):116‐23. [DOI] [PubMed] [Google Scholar]
Yassi 2003 {published data only}
- Yassi A, Fernandez N, Fernandez A, Bonet M, Tate RB, Spiegel J. Community participation in a multisectoral intervention to address health determinants in an inner‐city community in central Havana. Journal of Urban Health 2003;80(1):61‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ytterstad 2003 {published data only}
- Ytterstad B, Smith GS, Coggan CA. Harstad injury prevention study: prevention of burns in young children by community based intervention. Injury Prevention 1998;4(3):176‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ziegahn 2013 {published data only}
- Ziegahn L, Styne D, Askia J, Roberts T, Lewis ET, Edwards W. Strategies to prevent and reduce diabetes and obesity in Sacramento, California: the African American Leadership Coalition and University of California, Davis. Preventing Chronic Disease 2013;10:E187. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zoellner 2013 {published data only}
- Zoellner J, Hill JL, Grier K, et al. Randomized controlled trial targeting obesity‐related behaviors: Better Together Healthy Caswell County. Prevention of Chronic Disease 2013;10:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
Smith 2013 {published data only}
- Smith SA, Blumenthal DS. Efficacy to effectiveness transition of an educational program to increase colorectal cancer screening (EPICS): study protocol of a cluster randomized controlled trial. Implementation Science 2013;8(86):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Anderson 2003
- Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE. The Community Guide's model for linking the social environment to health. American Journal of Preventive Medicine 2003;24(3 Suppl):12‐20. [DOI] [PubMed] [Google Scholar]
Anderson 2013
- Anderson LM, Petticrew M, Chandler J, Grimshaw J, Tugwell P, O'Neill J, et al. Introducing a series of methodological articles on considering complexity in systematic reviews of interventions. Journal of Clinical Epidemiology 2013;88(11):1205‐8. [DOI] [PubMed] [Google Scholar]
Barile 2012
- Barile JP, Darnell AJ, Erickson SW, Weaver SR. Multilevel measurement of dimensions of collaborative functioning in a network of collaboratives that promote child and family well‐being. American Journal of Community Psychology 2012;49(1‐2):270‐82. [DOI] [PubMed] [Google Scholar]
Bazzoli 2003
- Bazzoli GJ, Casey E, Alexander JA, Conrad DA, Shortell SM, Sofaer S, et al. Collaborative initiatives: where the rubber meets the road in community partnerships. Medical Care Research and Review: MCRR 2003;60(4 Suppl):63S‐94S. [DOI] [PubMed] [Google Scholar]
Berkowitz 2001
- Berkowitz B. Studying the outcomes of community‐based coalitions. American Journal of Community Psychology 2001;29(2):213‐27. [DOI] [PubMed] [Google Scholar]
Bleich 2012
- Bleich SA, Jarlenski MP, Bell CN, LaVeist TA. Health inequalities: trends, progress, and policy. Annual Review of Public Health 2012;33:7‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Butterfoss 2002
- Butterfoss FD, Kegler MC. Toward a comprehensive understanding of community coalitions. In: DiClemente RJ, Crosby RA, Kegler MC editor(s). Emerging Theories in Health Promotion Practice and Research. San Francisco: Jossey‐Bass, 2002:157‐93. [Google Scholar]
Butterfoss 2007
- Butterfoss FD. Coalitions and Partnerships in Community Health. Coalitions and Partnerships in Community Health. San Francisco: Jossey‐Bass, 2007. [Google Scholar]
Chavis 1992
- Chavis D, Florin P, Felix M. Nurturing grassroots initiatives for community development: the role of enabling systems. In: Mirzrahi T, Morrison J editor(s). Community Organization and Social Administration: Advances, Trends, and Emerging Principles. Binghamton, NY: Haworth Press, 1992:41‐68. [Google Scholar]
Cochrane 2008
- Higgins JPT, Altman DG. Chapter 8. Assessing risk of bias in included studies. The Cochrane Handbook for Systematic Reviews of Interventions. New York: Wiley‐Blackwell, 2008. [Google Scholar]
Dluhy 1990
- Dluhy MJ. Building Coalitions in the Human Services. Newbury Park, CA: Sage, 1990. [Google Scholar]
EPOC 2015
- Effective Practice and Organization of Care Cochrane Group. EPOC Resources for Cochrane Authors. http://epoc.cochrane.org/epoc‐specific‐resources‐review‐authors (accessed 22 September, 2014).
Green 1990
- Green LW, Kreuter MW. Health promotion as a public health strategy for the 1990s. Annual Review of Public Health 1990;11:319‐34. [DOI] [PubMed] [Google Scholar]
Hasselblad 1995
- Hasselblad V, Hedges LV. Meta‐analysis of screening and diagnostic tests. Psychological Bulletin 1995;117(1):167‐78. [DOI] [PubMed] [Google Scholar]
Hayes 2012
- Hayes S, Mann MK, Morgan FM, Kelly MJ, Weightman AL. Collaboration between local health and local government agencies for health improvement. Cochrane Library 2012;10:DOI: 10.1002/14651858.CD007825.pub6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [update March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Kadushin 2005
- Kadushin C, Lindholm M, Ryan D, Brodsky A, Saxe L. Why it is so difficult to form effective community coalitions. City and Community 2005;4(3):255‐75. [Google Scholar]
Kreuter 2000
- Kreuter MW, Lezin NA, Young LA. Evaluating community‐based collaborative mechanisms: implications for practitioners. Health Promotion Practice 2000;1:49‐63. [Google Scholar]
Kreuter 2002
- Kreuter MW, Lezin N. Social capital theory: implications for community‐based health promotion. In: DiClemente RJ, Crosby RA, Kegler MC editor(s). Emerging Theories in Health Promotion Practice and Research: Strategies for Improving Public Health. San Francisco: Jossey‐Bass, 2002:228‐54. [Google Scholar]
LaVeist 2005
- LaVeist TA. Minority Populations and Health: An Introduction to Health Disparities in the United States. San Francisco: Jossey‐Bass, 2005. [Google Scholar]
LaVeist 2009
- LaVeist TA, Gaskin DJ, Richard P. The Economic Burden of Health Inequalities in the United States. Joint Center for Political and Economic Studies. Washington, DC: The Joint Center for Political and Economic Studies, 2009. [Google Scholar]
Lawless 2012
- Lawless P. Can area‐based regeneration programmes ever work? Evidence from England's New Deal for Communities Programme. Policy Studies 2012;33(4):313‐28. [Google Scholar]
Liao 2011
- Liao Y, Bang D, Cosgrove S, Dulin R, Harris Z, Taylor A, et al. Surveillance of health status in minority communities ‐ Racial and Ethnic Approaches to Community Health Across the U.S. (REACH U.S.) Risk Factor Survey, United States, 2009. MMWR. Surveillance Summaries: Morbidity and Mortality Weekly Report 2011;60(6):1‐44. [PubMed] [Google Scholar]
Litt 2013
- Litt J, Reed H, Zieff SG, Tabak RG, Eyler AA, Tompkins NO, et al. Advancing environmental and policy change through active living collaboratives: compositional and stakeholder engagement correlates of group effectiveness.. Journal of Public Health Management Practice 2013;19(3 Suppl 1):S49‐57. [DOI] [PubMed] [Google Scholar]
Mackenbach 2008
- Mackenbach JP, Stirbu I, Roskam A, Schaap MM, Menvielle G, et al. Socioeconomic inequalities in health in 22 European countries. New England Journal of Mediciine 2008;358:246881. [DOI] [PubMed] [Google Scholar]
Marmot 2006
- Marmot M. Health in an unequal world: social circumstances, biology and disease. Clinical Medicine 2006;6(6):559‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mitchell 2000
- Mitchell SM, Shortell SM. The governance and management of effective community health partnerships: a typology for research, policy, and practice. The Milbank Quarterly 2000;78(2):241‐89. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mizrahi 2001
- Mizrahi T, Rosenthal BB. Complexities of coalition building: leaders' successes, strategies, struggles, and solutions. Social Work 2001;46(1):63‐78. [DOI] [PubMed] [Google Scholar]
Nilsen 2006
- Nilsen P. The theory of community based health and safety programs: a critical examination. Injury Prevention 2006;12(3):140‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Noyes 2013
- Noyes J, Gough D, Lewin S, Mayhew A, Michie S, Pantoja T, et al. A research and development agenda for systematic reviews that ask complex questions about complex interventions. American Journal of Clinical Epidemiology 2013;66(11):1262‐70. [DOI] [PubMed] [Google Scholar]
O'Mara‐Eves 2013
- O'Mara‐Eves A, Brunton G, McDaid D, Oliver S, Kavanagh J, Jamal F, et al. Community engagement to reduce inequalities in health: a systematic review, meta‐analysis and economic analysis. Public Health Research 2013;1(4):1‐141. [PubMed] [Google Scholar]
RevMan 2011 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.1.4. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Roussos 2000
- Roussos ST, Fawcett SB. A review of collaborative partnerships as a strategy for improving community health. Annual Review of Public Health 2000;21:369‐402. [DOI] [PubMed] [Google Scholar]
Schensul 2009
- Schensul JJ, Trickett E. Introduction to multi‐level community based culturally situated interventions. American Journal of Community Psychology 2009;43(3‐4):232‐40. [DOI] [PubMed] [Google Scholar]
Shortell 2002
- Shortell SM, Zukoski AP, Alexander JA, Bazzoli GJ, Conrad DA, Hasnain‐Wynia R, et al. Evaluating partnerships for community health improvement: tracking the footprints. Journal of Health Politics, Policy and Law 2002;27(1):49‐91. [DOI] [PubMed] [Google Scholar]
South 2014
- South J, Phillips G. Evaluating community engagement as part of the public health system. Journal of Epidemiology and Community Health 2014;68:692‐6. [DOI] [PubMed] [Google Scholar]
Stokols 1992
- Stokols D. Establishing and maintaining healthy environments. Toward a social ecology of health promotion. The American Psychologist 1992;47(1):6‐22. [DOI] [PubMed] [Google Scholar]
Stokols 1996
- Stokols D. Translating social ecological theory into guidelines for community health promotion. Journal of Health Politics, Policy and Law 1996;10(4):282‐98. [DOI] [PubMed] [Google Scholar]
US AHRQ 2007
- US Agency for Healthcare Research and Quality. National Healthcare Disparities Report. AHRQ Pub. No. 08‐0040 February 2008.
Viswanathan 2004
- Viswanathan M, Ammerman A, Eng E, Gartlehner G, Lohr KN, et al. Community‐based Paticipatory Research: Assessing Evidence. Rockville, MD: AHRQ Publication 04‐E022‐1. August 2004. [PMC free article] [PubMed]
Voelker 2008
- Voelker R. Decades of work to reduce disparities in health care produce limited success. JAMA 2008;299(12):1411‐3. [DOI] [PubMed] [Google Scholar]
Wagner 2000a
- Wagner EH, Wickizer TM, Cheadle A, Psaty BM, Koepsell TD, Diehr P, et al. The Kaiser Family Foundation Community Health Promotion Grants Program: findings from an outcome evaluation. Health Services Research 2000;35(3):561‐89. [PMC free article] [PubMed] [Google Scholar]
Wandersman 1996
- Wandersman A, Valois R, Ochs L, Cruz DS, Adkins E, Goodman RM. Toward a social ecology of community coalitions. American Journal of Health Promotion 1996;10(4):299‐307. [DOI] [PubMed] [Google Scholar]
WHO 2009
- World Health Organization. Resolution WHA62.14. Reducing health inequalities through action on the social determinants of health. Sixty‐second World Health Assembly, Geneva, 18‐22 May 2009. Resolutions and decisions, annexes. Geneva: WHO, 2009 (WHA62/2009/REC/1), Resolutions: 21‐25.
WHO 2011
- World Health Organization. Rio Political Declaration on Social Determinants of Health. World Conference on Social Determinants of Health, Rio de Janeiro, Brazil, 19‐21 October 2011. www.who.int/sdhconference/declaration/Rio_political_declaration.pdf (accessed 1 May 2012).
Williams 2010
- Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Annals of the New York Academy of Sciences 2010;1186:69‐101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zakocs 2006
- Zakocs RC, Edwards EM. What explains community coalition effectiveness? A review of the literature. American Journal of Preventive Medicine 2006;30(4):351‐61. [DOI] [PubMed] [Google Scholar]


