Abstract
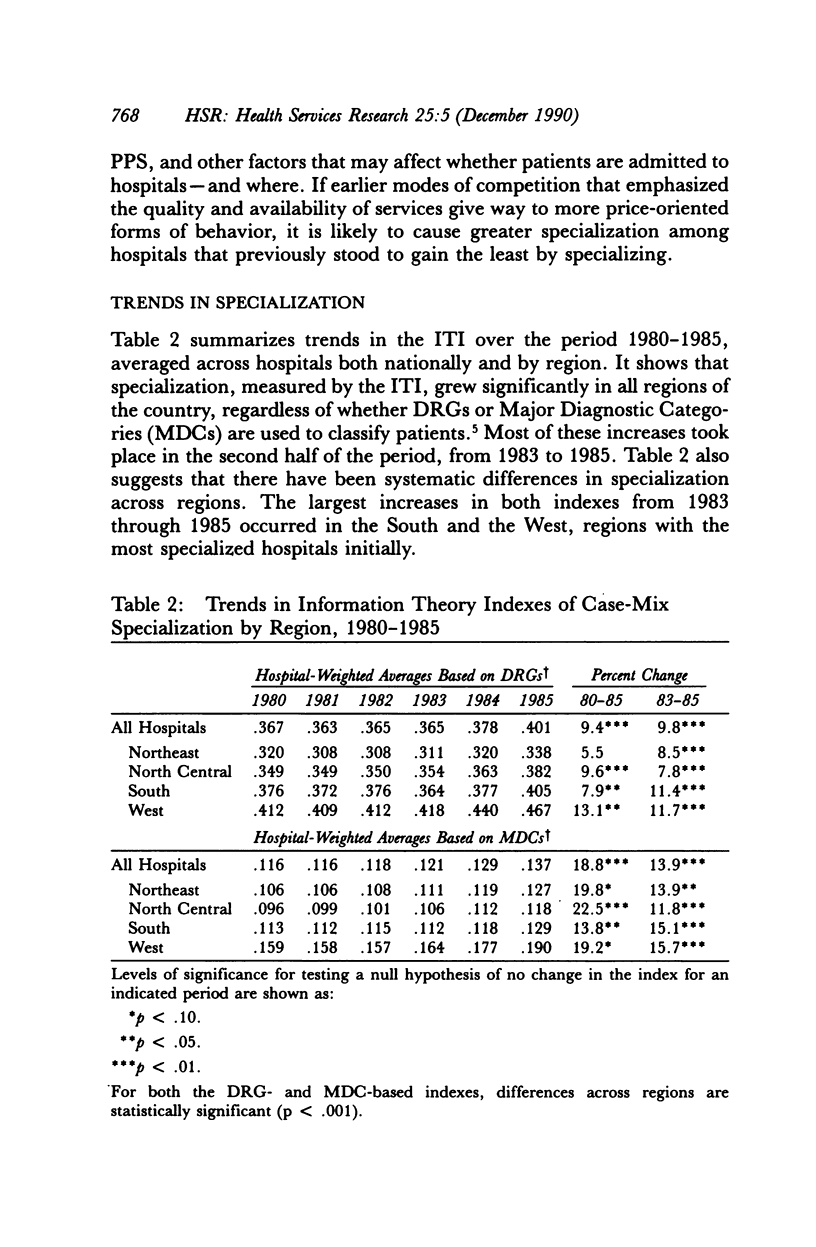
Historically, cost-based reimbursement encouraged hospitals to compete on the basis of quality, leading to duplication of services and other inefficient behavior. More recently, prospective payment, selective contracting, and other innovations in reimbursement have strengthened incentives for more efficient hospital operations. In principle, hospitals may be able to reduce their costs by limiting the array of services they provide, but there has been little empirical evidence that U.S. hospitals are moving toward greater specialization or that specialization leads to cost savings. This article explores recent changes in case-mix specialization and the relationship of these changes to hospital costs. It first describes an index of specialization derived from Information Theory and shows that this index provides intuitively reasonable results in characterizing patterns of specialization across hospitals. The analysis then demonstrates that specialization, as measured by this index, in fact increased from 1980 through 1985; that specialization can indeed lower hospital costs; and that increases in specialization have been largest in those hospitals with the greatest incentives to reduce costs.
Full text
PDF





















Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barer M. L. Case mix adjustment in hospital cost analysis: information theory revisited. J Health Econ. 1982 May;1(1):53–80. doi: 10.1016/0167-6296(82)90021-2. [DOI] [PubMed] [Google Scholar]
- Farley D. E. Measuring casemix specialization and the concentration of diagnoses in hospitals using information theory. J Health Econ. 1989 Jun;8(2):185–207. doi: 10.1016/0167-6296(89)90003-9. [DOI] [PubMed] [Google Scholar]
- Flood A. B., Scott W. R., Ewy W. Does practice make perfect? Part I: The relation between hospital volume and outcomes for selected diagnostic categories. Med Care. 1984 Feb;22(2):98–114. [PubMed] [Google Scholar]
- Hughes R. G., Hunt S. S., Luft H. S. Effects of surgeon volume and hospital volume on quality of care in hospitals. Med Care. 1987 Jun;25(6):489–503. doi: 10.1097/00005650-198706000-00004. [DOI] [PubMed] [Google Scholar]
- Kelly J. V., Hellinger F. J. Heart disease and hospital deaths: an empirical study. Health Serv Res. 1987 Aug;22(3):369–395. [PMC free article] [PubMed] [Google Scholar]
- Lave J. R., Lave L. B. The extent of role differentiation among hospitals. Health Serv Res. 1971 Spring;6(1):15–38. [PMC free article] [PubMed] [Google Scholar]
- Luft H. S., Hunt S. S., Maerki S. C. The volume-outcome relationship: practice-makes-perfect or selective-referral patterns? Health Serv Res. 1987 Jun;22(2):157–182. [PMC free article] [PubMed] [Google Scholar]
- Luft H. S., Robinson J. C., Garnick D. W., Maerki S. C., McPhee S. J. The role of specialized clinical services in competition among hospitals. Inquiry. 1986 Spring;23(1):83–94. [PubMed] [Google Scholar]
- Lutz S. Marketing. Hospitals consider product line management techniques to better meet consumers' needs. Mod Healthc. 1987 Apr 10;17(8):70–74. [PubMed] [Google Scholar]
- MacStravic R. S. Product-line administration in hospitals. Health Care Manage Rev. 1986 Spring;11(2):35–43. doi: 10.1097/00004010-198601120-00005. [DOI] [PubMed] [Google Scholar]
- Powills S. Clergy, MDs key to marketing psych care. Hospitals. 1986 Sep 20;60(18):70–71. [PubMed] [Google Scholar]
- Robinson J. C., Luft H. S. Competition and the cost of hospital care, 1972 to 1982. JAMA. 1987 Jun 19;257(23):3241–3245. [PubMed] [Google Scholar]
- Ruffner J. K. Product line management. Healthc Forum. 1986 Sep-Oct;29(5):11–14. [PubMed] [Google Scholar]
- Showstack J. A., Rosenfeld K. E., Garnick D. W., Luft H. S., Schaffarzick R. W., Fowles J. Association of volume with outcome of coronary artery bypass graft surgery. Scheduled vs nonscheduled operations. JAMA. 1987 Feb 13;257(6):785–789. [PubMed] [Google Scholar]



