Abstract
Occupational stress and sleep quality are prevalent issues that can impact the physical and mental well-being of adults. An association between occupational stress and sleep quality has been found. However, this association is not entirely the same across different occupational groups. Additionally, variations are present in the research design and instruments employed.This systematic review aims to investigate the association between these two factors and identify gaps and limitations in current research. Articles published between January 1, 2011, and December 31, 2022, were retrieved from the WOS, Scopus, and PubMed databases. Out of 1225 articles, 38 studies met the predetermined inclusion and exclusion criteria and were included in the review. In the study, research designs, samples, instruments, and associations between occupational stress and sleep quality were statistically analyzed.These studies encompassed a diverse range of occupations, including both blue-collar and white-collar workers. Cross-sectional study is the most common research method. The Pittsburgh Sleep Quality Index (PSQI) was the most frequently utilized tool for assessing sleep quality, while there was a wide variety of measurement tools employed to assess occupational stress. The association between occupational stress and sleep quality consistently demonstrated a negative association, although the specific dimensions varied among studies. Moreover, several other factors were identified to have direct or indirect effects on occupational stress and sleep quality. For future research in this field, we propose four recommendations: (1) Consider utilizing objective measures to assess occupational stress and sleep quality. (2) Employ controlled experiments to further validate the causal relationship between occupational stress and sleep quality. (3) Investigate occupational groups that have received less attention. (4) Take into account the potential influence of other factors on occupational stress and sleep quality.
Keywords: occupational stress, sleep quality, systematic review, occupational safety and health
Introduction
Occupational stress, also referred to as job stress, work stress, or work-related stress, encompasses the detrimental reactions that arise when job demands surpass an individual’s capacities, resources, or requirements, leading to adverse effects on their cognition and psychology.1 Common job demands encompass workload, work-life balance, physical environment, and emotional involvement.2 With societal development, job demands have generally risen across diverse industries, amplifying the prevalence of occupational stress and garnering increased attention.3,4 Occupational stress has emerged as a significant factor that affects adults, impairing not only work efficiency5 but also exerting an impact on physical health6,7 and mental well-being.8,9 Research on factors associated with occupational stress examines both stressors10 and their repercussions.11,12 Certain factors, such as sleep quality,13 appear to interact with occupational stress. Additionally, other studies delve into strategies aimed at alleviating occupational stress. Other studies explore strategies for alleviating occupational stress.4,14
Sleep plays a vital role in human health. Sleep quality is associated with various physical health problems, such as obesity,15 metabolic syndrome,16 and cardiovascular issues.17 Furthermore, sleep quality is linked to psychological factors, including mild cognitive impairment,17 low mood,18 heightened aggression,19 and depression.17 Nonetheless, sleep problems prevail among various populations, encompassing industrial workers,20 nurses,21 drivers,22 and students.23 Evaluating sleep quality entails subjective experiences, posing challenges to depend solely on objective assessments.24 Research on sleep quality primarily centers on sleep measurement,25 investigating factors associated with sleep quality,21,26 and exploring interventions to enhance sleep quality.27
Numerous studies have established an association between occupational stress and sleep quality. Research as early as 1988 indicated a link between self-reported poor sleep quality and work-related stressors.28 An investigation was conducted, involving 2116 Chinese oilfield workers in Xinjiang, in a cross-sectional survey.29 The study examined the association between occupational stress and sleep quality, which revealed that the sleep quality of these oilfield workers was poor, and as occupational stress increased, the prevalence of sleep disturbances rose. Factors such as shift work and job titles also influenced sleep quality. In a longitudinal two-wave study conducted in the Netherlands, 877 employees participated in two online surveys, and researchers employed structural equation modeling to analyze the data.13 This study also found a negative correlation between occupational stress and sleep quality, with perseverative cognition mediating the relationship between occupational stress and sleep quality. This association extends beyond blue-collar workers to include white-collar workers as well. Instances of this association have been observed in various occupations, including oil workers,30 cable manufacturing workers,31 and couriers,32 as well as in nurses,33 dentists,34 and office workers.35 Work-related factors, such as workload,36 job title,37 and role conflict,38 have been found to be associated with sleep quality. Likewise, occupational stress is also related to various dimensions of sleep quality, such as daytime dysfunction,38,39 sleep duration,40 sleep disturbances,33 and the use of sleeping medication.41
Several systematic reviews have examined the associations between occupational stress and various factors, including burnout,42 cardiovascular risk factors,12 and workplace exercise interventions.4 Some systematic reviews have also discussed the association between sleep quality and factors such as diet,43 depression,44 and exercise.45 However, a systematic review specifically examining the association between occupational stress and sleep quality has not been found.
In summary, it is evident that occupational stress and poor sleep quality have become significant issues affecting workers in various professions. Despite numerous survey and experimental studies focusing on the association between occupational stress and sleep quality, a systematic analysis and summary of these connections across different professions and regions remains a research gap. To address this gap, the primary objective of this systematic review is to examine the association between occupational stress and sleep quality. Specifically, the research questions include:
What were the study designs, samples, locations, and instruments used in the researches that examined the relationship between occupational stress and sleep quality?
Did these researches find associations between occupational stress and sleep quality, and if so, what were these associations?
What limitations were present in these studies?
Through analysis and discussion, the relationship between occupational stress and sleep quality is elucidated. Occupational stress and sleep quality can be assessed using various dimensions, and our interest lies in investigating the associations among these dimensions. Independent or interactive factors affecting occupational stress or sleep quality are also summarized. These conclusions can serve as references for scholars in related fields. Furthermore, based on the summary, this systematic review provides recommendations for future research in the field, including instrument selection, study design, population considerations, and analytical methods.
Materials and Methods
Search Strategy
This study was conducted following the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) checklist.46 The search encompassed three databases: Web of Science (WOS), Scopus, and PubMed. The search queries used to retrieve articles were as follows: In WOS, the query was ((AB=(“occupational stress” OR “job stress” OR “work stress” OR “work-related stress”)) AND AB=(sleep)) AND LA=(English). In Scopus, the query was ((AB=(“occupational stress” OR “job stress” OR “work stress” OR “work-related stress”)) AND AB=(sleep)) AND LA=(English). In PubMed, the query was ((“occupational stress” [Title/Abstract] OR “job stress”[Title/Abstract] OR “work stress” [Title/Abstract] OR “work-related stress” [Title/Abstract]) AND (sleep[Title/Abstract])) AND (English[Language]). Publications were limited to those written in English, and the time frame spanned from January 1, 2011, to December 31, 2022.
Inclusion and Exclusion Criteria
This study investigated the relationship between occupational stress and sleep quality. The study employed three inclusion criteria: (a) empirical studies that collected primary data and drew conclusions based on data analysis, (b) measurement of both occupational stress and sleep quality using objective or subjective methods with statistical description, and (c) utilization of statistical methods to examine the relationship between occupational stress and sleep quality. Consequently, articles that were not empirical studies, lacked statistical information on either occupational stress or sleep quality, or did not analyze the relationship between occupational stress and sleep quality were excluded. Importantly, only articles that directly analyzed the relationship between occupational stress and sleep quality were included. For example, studies that independently examined the relationship between occupational stress and well-being or sleep quality and well-being would not be included. Table 1 provides the inclusion and exclusion criteria used in this systematic literature review.
Table 1.
Inclusion and Exclusion Criteria
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Empirical studies | Reviews, commentaries, methodological articles, theoretical articles or practical articles |
| Statistical description of occupational stress and sleep quality | Lack of statistical description of occupational stress or sleep quality |
| Association between occupational stress and sleep quality | Lack of association between occupational stress and sleep quality |
Selection of Articles and Data Extraction
Data extraction involved retrieving the following information from each article: (a) key study characteristics (study design, occupation, sample size, location, and measurement tools for occupational stress and sleep quality), and (b) study findings. The initial focus was to ascertain the presence of a direct positive association, negative association, or no association between occupational stress and sleep quality. Subsequently, the researchers identified specific dimensions associated with occupational stress and sleep quality. Moreover, additional factors related to occupational stress or sleep quality were also extracted. Two independent researchers conducted data extraction from the initially screened articles and organized the data in a table Studies with missing data or data not collected directly by the authors were excluded. The two researchers conducted a quality assessment, referring to the modified 22-item Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist47 which is attached in Supplementary Material. Any discrepancies were resolved through discussion.
Results
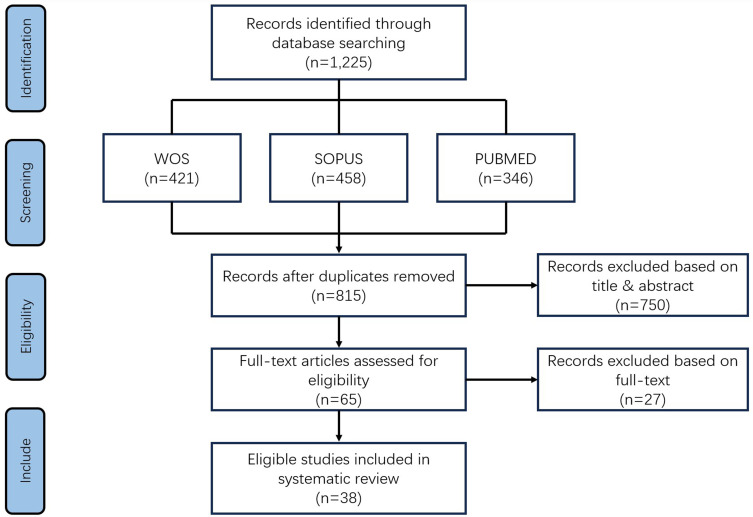
The search strategy yielded a total of 1225 articles, comprising 421 from WOS, 458 from Scopus, and 346 from PubMed. After removing 410 duplicate articles, 815 articles remained. After evaluating titles and abstracts against the inclusion and exclusion criteria, 750 articles were excluded, resulting in 65 articles remaining. Subsequently, the two researchers conducted data extraction and review, resulting in the inclusion of 37 articles, representing 38 studies, for further analysis. Figure 1 presents the PRISMA flow diagram illustrating this process.
Figure 1.
PRISMA flow diagram of study-selection process for systematic review.
Research Design
Table 2 presents a comprehensive list of the 38 included studies, including their references, study designs, sample characteristics (occupation, sample size, location), and the instruments utilized to assess occupational stress and sleep quality. Out of all the studies, only six employed a longitudinal design, with the remaining studies utilizing a cross-sectional approach.
Table 2.
Research Designs, Samples and Instruments
| Reference | Study Design | Sample | Instruments | |||
|---|---|---|---|---|---|---|
| Occupation | N | Location | Occupational Stress | Sleep Quality | ||
| (Deng et al, 2020)33 | Cross-sectional study | Nurse | 180 | China | Job Stress Questionnaire | Pittsburgh Sleep Quality Index |
| (Peng et al, 2022)48 | Cross-sectional study | Worker | 729 | China | Generic Job Stress Questionnaire | Pittsburgh Sleep Quality Index |
| (Song et al, 2017)34 | Cross-sectional study | Dentist | 231 | Korea | Doctor Job Stress Scale | Pittsburgh Sleep Quality Index |
| (Song & Kim, 2019)9 | Cross-sectional study | Dentist | 231 | Korea | Dentist Job Stress | Pittsburgh Sleep Quality Index |
| (Rabei et al, 2020)36 | Cross-sectional study | Nursing internship student | 95 | Egypt | Expanded Nursing Stress Scale | Pittsburgh Sleep Quality Index |
| (Jiang et al, 2016)49 | Cross-sectional study | Worker | 700 | China | Occupational Stress Inventory-Revised questionnaire | Pittsburgh Sleep Quality Index |
| (Li et al, 2022)30 | Cross-sectional study | Oil worker | 1142 | China | Occupational Stress Inventory | Pittsburgh Sleep Quality Index |
| (Li et al, 2019)29 | Cross-sectional study | Oilfield worker | 2116 | China | Occupational Stress Inventory Revised Edition | Pittsburgh Sleep Quality Index |
| (Gao et al, 2018)39 | Cross-sectional study | Physician | 504 | China | Job Stress Survey | Pittsburgh Sleep Quality Index |
| (Yook, 2019)50 | Cross-sectional study | Firefighter | 705 | Korea | Occupational stress scale | Pittsburgh Sleep Quality Index |
| (Takaesu et al, 2021)35 | Cross-sectional study | Office worker | 4645 | Japan | Brief Job Stress Questionnaire | Subjective sleep schedule |
| (Van Laethem et al, 2015)13 | Longitudinal study | Employee | 877 | Dutch | A one-item measure | Jenkins Sleep Scale |
| (Sousa et al, 2018)41 | Cross-sectional study | Professor | 24 | Brazil | Work Stress Scale | Pittsburgh Sleep Quality Index |
| (Gu et al, 2019)51 | Cross-sectional study | Nurse | 2889 | China | Nurse Job Stressor Questionnaire | Pittsburgh Sleep Quality Index |
| (Han et al, 2016)37 | Cross-sectional study | Nurse | 2033 | China | Effort-Reward Imbalance Questionnaire | Pittsburgh Sleep Quality Index |
| (Jiang et al, 2020)52 | Cross-sectional study | Professional from a public institution | 812 | China | Effort-reward Imbalance Scale | Pittsburgh Sleep Quality Index |
| (Dong et al, 2022)53 | Cross-sectional study | Emergency worker | 7688 | China | Job Content Questionnaire | Pittsburgh Sleep Quality Index |
| (Eskildsen et al, 2017)54 | Longitudinal study | Patient with prolonged work-related stress | 60 | Denmark | Perceived Stress Scale | Pittsburgh Sleep Quality Index |
| (J. Wang et al, 2022)55 | Cross-sectional study | Non-manual worker | 1700 | China | Effort-Reward Imbalance Inventory | Pittsburgh Sleep Quality Index |
| (Saalwirth & Leipold, 2021)40 | Cross-sectional study | Daytime worker | 438 | German | Trier Inventory for the Assessment of Chronic Stress | Pittsburgh Sleep Quality Index |
| (Dong et al, 2020)56 | Cross-sectional study | Emergency nurse | 4856 | China | Job Content Questionnaire | Pittsburgh Sleep Quality Index |
| (D’Ettorre et al, 2020)57 | Cross-sectional study | Nurse | 658 | Italy | Job Content Questionnaire | Bergen Insomnia Scale |
| Epworth Sleepiness Scale | ||||||
| (Pereira & Elfering, 2014)58 | Longitudinal study | Full-time employee | 60 | Swiss | A scale of Frese and Zapf | An original scale including sleep-onset latency, sleep efficiency and sleep fragmentation; |
| Subjective sleep diaries | ||||||
| (Wu et al, 2023)59 | Cross-sectional study | Shift-working nurse | 390 | China | Chinese Nurses Stressor Scale | Pittsburgh Sleep Quality Index |
| (Iwasaki et al, 2018)38 | Cross-sectional study | Day-shift public servant | 243 | Japan | Generic Job Stress Questionnaire | Pittsburgh Sleep Quality Index |
| (Rasdi, 2018)31 | Cross-sectional study | Cable manufacturing worker | 140 | Malaysia | Stress Overload Scale | Pittsburgh Sleep Quality Index |
| (Xie et al, 2021)32 | Cross-sectional study | Courier | 2831 | China | Work stress scale | “Over the past month, how do you feel your subjective sleep quality has been?” |
| (Myllyntausta et al, 2019)60 | Longitudinal study | Retiree | 2053 | Finnish | Job Content Questionnaire | An original scale including sleep duration, sleep difficulties, daytime tiredness, and sleep loss |
| (Kim et al, 2020)61 | Cross-sectional study | Study 1: Working adult | 1031 | Korea | A measure including perceived job insecurity and negative work spillover | Sleep Problems Questionnaire |
| Longitudinal study | Study 2: Working adult | 152 | Korea | |||
| (Shimura et al, 2020)26 | Cross-sectional study | Employee | 5640 | Japan | Brief Job Stress Questionnaire | Pittsburgh Sleep Quality Index |
| (Leitaru et al, 2019)62 | Cross-sectional study | Employee | 1973 | Swedish | General Nordic Questionnaire for Psychosocial and Social factors at work | “How do you rate the overall quality of your sleep?” |
| (Bilgic et al, 2021)63 | Cross-sectional study | Nurse working during the COVID-19 pandemic | 316 | Turkey | Perceived Stress Scale | Pittsburgh Sleep Quality Index |
| (Herr et al, 2018)64 | Longitudinal study | Male industrial worker | 101 | German | Stress Reactivity Scale | Parts of the Diagnostic and Statistical Manual of Mental Disorders |
| (Bernburg et al, 2021)65 | Cross-sectional study | Outpatient nurse | 166 | German | 10-item Perceived Stress Scale | Pittsburgh Sleep Quality Index |
| (Hartley et al, 2014)66 | Cross-sectional study | Police officer | 356 | USA | Spielberger Police Stress Survey | Pittsburgh Sleep Quality Index |
| (Abbasi et al, 2018)67 | Cross-sectional study | Firefighter | 118 | Iran | HSE questionnaire for occupational stress | Pittsburgh Sleep Quality Index |
| (Zhang et al, 2016)68 | Cross-sectional study | Nursing assistant | 650 | USA | Work features questionnaire including three physical domains and five psychosocial domains | Modified questionnaire from Pittsburgh Sleep Quality Index |
Most of the research samples were obtained from hospitals, comprising ten studies on nurses, two studies on dentists, and one study on physicians. Six studies encompassed blue-collar workers, including two studies on oil workers, two studies on firefighters, one study on emergency workers, one study on cable manufacturing workers, one study on couriers, and one study on male industrial workers. Additionally, five studies focused on white-collar workers, comprising one study on office workers, one study on professionals from a public institution, one study on day-shift public servants, one study on non-manual workers, and one study on professors. Ten studies did not specify a specific occupation and employed terms such as “workers” or “employees” to describe their respective samples. One study centered on retirees. Two studies specifically concentrated on males, namely male industrial workers and male firefighters. Additionally, one study investigated a specific work schedule (shift-working nurses), while another study examined a unique period (nurses working during the COVID-19 pandemic).
The studies included samples from diverse regions, with the majority of studies conducted in Asia (14 in China, five in Korea, three in Japan, one in Malaysia, and one in Iran), followed by Europe (one in the Netherlands, one in Egypt, one in Denmark, three in Germany, one in Italy, one in Switzerland, one in Finland, and one in Sweden). Additionally, there were two studies conducted in the United States, one in Brazil, and one in Turkey (a transcontinental country). Two cross-sectional studies had sample sizes below 100, consisting of 95 nursing internship students36 and 24 professors.41 Furthermore, two longitudinal studies included fewer than 100 individuals, namely 60 patients with prolonged work-related stress54 and 60 full-time employees.58 The rest of the studies had sample sizes exceeding 100, with 13 studies surpassing a sample size of 1000.
The Pittsburgh Sleep Quality Index (PSQI)69 was the most frequently utilized instrument for assessing sleep quality, employed in 28 studies. Out of the remaining 10 studies, one study employed a modified version of the PSQI, four studies used original scales, and five studies utilized other established scales. Two of the original scales comprised a single item. The assessment tools employed for measuring occupational stress exhibited greater diversity. The most commonly utilized instruments were the Job Content Questionnaire, Occupational Stress Inventory, and Perceived Stress Scale, which were employed in four, three, and three studies, respectively. The Brief Job Stress Questionnaire, Generic Job Stress Questionnaire, Occupational Stress Scale, and Work Stress Scale were utilized in two studies, whereas the remaining studies employed scales distinct from those used in other studies.
Research Findings
Table 3 displays the findings pertinent to this systematic literature review from all the studies included. The results regarding the association between occupational stress and sleep quality were extracted from each study. To account for variations in the reporting of results among different studies, a unified presentation was adopted as follows: “Negative (N)” denotes a decrease in sleep quality with increasing occupational stress, “Positive (P)” indicates an improvement in sleep quality with increasing occupational stress, and “/” signifies no significant association. Out of all the studies, only three reported no significant association between occupational stress and sleep quality, whereas the remaining studies demonstrated a negative association. Out of the 35 studies displaying a significant negative association, 15 studies addressed dimensions of occupational stress, while 12 studies focused on dimensions of sleep quality. Sleep disturbances and daytime dysfunction were the most frequently cited factors pertaining to sleep quality, with each dimension mentioned in three studies, both of which are dimensions captured by the PSQI. Given the absence of uniformity in measuring occupational stress and the diverse range of occupational categories, the factors associated with occupational stress exhibited a relatively dispersed nature. While some factors, such as social support and work load, are general, others are specific to particular occupations and are frequently encountered in hospital-related studies, including doctor-patient relationships, demanding patients and their families, and type of nurse contract. The findings from 31 studies addressed the association of additional variables with either occupational stress or sleep quality. Certain variables exhibited independent effects on either occupational stress or sleep quality, including depression, age, and regular nutrition. Moreover, certain variables demonstrated more intricate relationships between occupational stress and sleep quality, such as specific gene polymorphisms, perseverative cognition, and circadian rhythm.
Table 3.
Association Between Occupational Stress and Sleep Quality
| Reference | Association Between Occupational Stress And Sleep Quality | Other Factors | ||
|---|---|---|---|---|
| Occupational stress | Sleep quality | |||
| (Deng et al, 2020)33 | N | Type of nurse contract; | Sleep quality | None. |
| Self-reported job stress | ||||
| Job difficulty factor; | Sleep disturbances | |||
| Doctor-patient relationships; | ||||
| Psychosomatic state; | ||||
| Environment or events; | ||||
| Promotion or competition; | ||||
| Total pressure scores | ||||
| (Peng et al, 2022)48 | N | Job stress | Sleep quality | Occupational stress and PER3 genotype had both separate and combined effects on poor sleep quality. |
| (Song et al, 2017)34 | N | Patient factors; | Sleep quality | Depression and anxiety revealed a significant association with the doctor job stress. |
| Clinical responsibility/judgment factors | ||||
| (Song & Kim, 2019)9 | N | Job stress | Sleep quality | Dentists’ job stress was significantly associated with income, work time, job satisfaction and depression. |
| (Rabei et al, 2020)36 | N | Number and duration of shifts; | Sleep quality | None. |
| Problems related to peers | ||||
| Demanding patients and their families | Sleep duration | |||
| Demanding patients and their families; | Sleep efficiency | |||
| Work load; | ||||
| Discrimination; | ||||
| Uncertainty regarding treatment | ||||
| (Jiang et al, 2016)49 | N | Job stress | Sleep quality | 5-HTR2A genotype was significantly associated with sleep quality; |
| Occupational stress and 5-HTR2A genotypes in workers are associated both independently and in combination with increased risk of poor sleep quality. | ||||
| (Li et al, 2022)30 | N | Occupational stress | Sleep quality | Age, junior college and above, borehole operation, extraction of oil, drilling, shift work, and mental disorders are risk factors for sleep disorders. |
| (Li et al, 2019)29 | N | Occupational stress | Subjective sleep quality; | The higher the level of glycosaminoglycan, the less likely the subject is to have sleep disorders. |
| Sleep disorder; | ||||
| Daytime dysfunction | ||||
| (Gao et al, 2018)39 | N | Occupational stress | Sleep disturbances; | Stress can increase the risk of poor sleep quality, but this effect is worse in a group of people with specific gene polymorphisms. |
| Daytime dysfunction | ||||
| (Yook, 2019)50 | N | Occupational stress | Sleep quality | Occupational stress was significantly correlated with cardiorespiratory fitness and arterial stiffness. |
| (Takaesu et al, 2021)35 | N | Occupational stress | Insufficient sleep; | None. |
| Long sleep durations on free days; | ||||
| Social jetlag | ||||
| (Van Laethem et al, 2015)13 | N | Work-related stress | Sleep quality | Perseverative cognition could be an important underlying mechanism in the association between work-related stress and sleep quality; |
| Work-related stress, perseverative cognition, and sleep quality mutually influence each other over time. | ||||
| (Sousa et al, 2018)41 | N | General stress level | Use of sleeping medication | None. |
| (Gu et al, 2019)51 | N | Professional and career issues | Sleep quality | Occupational stress was correlated with anxiety. |
| (Han et al, 2016)37 | N | Many years of working; | Sleep quality | None. |
| Job title; | ||||
| Registered nurse; | ||||
| Many times of night shift per month; | ||||
| No frequent exercise | ||||
| Many efforts and few rewards; | ||||
| High decision-making autonomy | ||||
| (Jiang et al, 2020)52 | N | Professional and career issues | Sleep quality | Serum DA levels may interrelate with job stress to affect sleep. |
| (Dong et al, 2022)53 | N | Occupational stress | Sleep quality | The sleep quality was poorer in doctors than in nurses, and poorer in those working in secondary and tertiary hospitals than in primary hospitals; |
| High prevalence of sleep disturbance was significantly associated with shift work, musculoskeletal pain, fewer breaks in a work shift, and less exercise during leisure time; | ||||
| Sleep disturbance occurred in emergency workers in the following order: two-shift rotation > three-shift rotation > permanent night shift > permanent day shift. | ||||
| (Eskildsen et al, 2017)54 | N | Occupational stress | Sleep quality | Improvement in cognitive impairments is partly mediated by decreasing levels of perceived stress and, to a lesser extent, decreasing levels of sleep disturbances. |
| (J. Wang et al, 2022)55 | N | Work stress | Sleep quality | The interaction between work stress and Per3 gene polymorphism may increase the risk of sleep quality problems |
| (Saalwirth & Leipold, 2021)40 | N | Work-related stress | Shorter sleep duration; | The effect of a flexible start of work for daytime worker’s well-being depends on a person’s individual sleep timing and chronotype. |
| Greater need for additional sleep; | ||||
| Late chronotype | ||||
| (Dong et al, 2020)56 | N | Occupational stress | Sleep quality | The following factors were associated with poor sleep: hospital level (tertiary vs primary, secondary vs primary), female sex, less of exercise, long work hours per week, many patients in the charge of at night, high monthly night shift frequency (4–6 vs never, ≥ 7 vs never). |
| (D’Ettorre et al, 2020)57 | / | Significantly more women than men experienced high job strain, insomnia and daytime sleepiness; among women the level of social support was significantly and negatively associated with insomnia and daytime sleepiness. | ||
| (Pereira & Elfering, 2014)58 | N | Social stressors at work | Objectively assessed sleep fragmentation | Social stressors at work were positively related to psychosomatic health complaints; |
| Objectively assessed sleep fragmentation mediated the effect of social stressors at work on psychosomatic health complaints. | ||||
| (Wu et al, 2023)59 | N | Occupational stress | Sleep quality | Work stress could indirectly affect sleep quality through circadian rhythm amplitude and stability. |
| (Iwasaki et al, 2018)38 | N | Higher role ambiguity | Sleep quality | None. |
| Role conflict | Sleep disturbance; | |||
| Daytime dysfunction | ||||
| (Rasdi, 2018)31 | N | Work stress | Sleep quality | Higher level of being avoidance as a coping strategy were found to be significantly correlated with poorer sleep quality. |
| (Xie et al, 2021)32 | N | Occupational stress | Sleep quality | Work stress was negatively correlated with job satisfaction and psychological capital; |
| Psychological capital plays a mediating role between work stress and sleep quality among couriers. | ||||
| (Myllyntausta et al, 2019)60 | / | None. | ||
| (Kim et al, 2020)61 | N | Perceived job insecurity | Subjective sleep quality | Negative work spillover mediates the relationship between perceived job insecurity and subjective sleep quality. |
| (Shimura et al, 2020)26 | N | Job stressors and social support | Sleep quality | Irregular meal time, not eating vegetables every clay, night-cap, weight gain, lack of sunlight in the morning in the bedroom, waking up before dawn, electronic display use in bed, and daily caffeine intake were significantly associated with sleep disturbance. |
| (Leitaru et al, 2019)62 | N | Job stressors | Sleep quality | Self-rated health plays an important moderating role in the association between job strain and sleep quality. |
| (Bilgic et al, 2021)63 | N | Perceived stress; | Sleep quality | Age, years worked, fear of infecting the family with COVID-19, receiving COVID-19 education, regular nutrition, were effective predictors of stress level. |
| Shift work; | ||||
| Stress level; | ||||
| A coworker having COVID-19; | ||||
| Being out of home due to the risk of transmission; | ||||
| Having a person older than 65 in the home | ||||
| (Herr et al, 2018)64 | N | Improvement of the prolonged reactivity; | Sleep quality | The improvement of stress reactivity resulting from a work stress intervention was effective and generally long-lasting in preventing mental health. |
| Reduction of the reactivity to social conflicts | ||||
| (Bernburg et al, 2021)65 | N | Pandemic-related stress | Sleep quality | None. |
| (Hartley et al, 2014)66 | N | Perception of stress severity and frequency of stressors | Sleep quality | None. |
| (Abbasi et al, 2018)67 | / | Musculoskeletal disorders (MSDs), shift work, and high body mass index are associated with poor sleep quality. | ||
| (Zhang et al, 2016)68 | N | Work features | Sleep duration; | None. |
| Sleep quality | ||||
Discussion
Research Design
Before examining the association between occupational stress and sleep quality, we conducted a review of the study designs used in research conducted from 2011 to 2022. The objective was to identify the limitations and gaps in the existing literature. The majority of studies investigating the association between occupational stress and sleep quality were cross-sectional in nature, while only a limited number were longitudinal studies. No experimental studies were identified. In terms of study design, all researchers employed a non-interventional approach, primarily focused on describing and observing the relationship or trends between occupational stress and sleep quality. These study designs offer the advantage of large sample sizes and robust descriptive information. However, due to the absence of controlled experiments, causal relationships cannot be established. Therefore, investigating causality represents a crucial gap that researchers should address in future studies.
Healthcare professionals emerged as the most extensively studied group, which could be attributed to the convenience sampling facilitated by researchers based in hospitals. Notably, a greater emphasis was placed on Asian studies within this domain, evidenced by the highest number of relevant research articles. However, in light of the physiological and social variations among workers across continents and regions, it is imperative to supplement the existing body of research with studies conducted in other locations.
All studies employed subjective scales to measure occupational stress and sleep quality, which is understandable considering the subjective nature of these aspects. However, it is worth noting that objective measurement tools can complement these scales. For instance, sleep quality can be assessed using brain imaging techniques,70 polysomnography (PSG), and actigraphy.71 Some studies have utilized electroencephalogram (EEG)72 or surface electromyography (EMG)73 to evaluate stress levels. The majority of researchers relied on the PSQI69 to measure sleep quality, highlighting the widespread use and recognition of this scale. However, it also suggests that there has been limited progress in sleep quality measurement methods over the past two decades. In contrast, there is a greater diversity and specificity in the categories of occupational stress scales, such as the Expanded Nursing Stress Scale74 and the Spielberger Police Stress Survey.66 Subsequent researchers have made adjustments and developments to many of these scales, indicating advancements in this field.
Association Between Occupational Stress and Sleep Quality
Occupational stress and poor sleep quality are significant concerns on a global scale. A survey in 2022 found that 44% of respondents worldwide experienced significant work-related stress daily.75 Eastern Asia emerged as the region with the highest levels of occupational stress, with 55% of individuals reporting work stress, while North America ranked second with a rate of 50%. More than half of Generation Z and Millennials reported that work stress had a negative impact on their sleep in the word.76 In the United States, over one-third of adults sleep for less than 7 hours per night.77 It’s estimated that approximately 50 to 70 million Americans suffer from sleep disorders.78 Sleep quality among the Chinese population is also a concern, with 25.9% of residents sleeping less than 7 hours per night, and 10.04% of respondents rating their sleep quality as very poor.79
In this systematic review, the majority of the included studies consistently demonstrated a negative association between occupational stress and sleep quality. High levels of occupational stress and poor sleep quality often coexisted in many cases. Only three studies, involving nurses in Italy,57 retirees in Finland,60 and firefighters in Germany,67 using either cross-sectional surveys or longitudinal studies, reported no significant association between occupational stress and sleep quality. Based on the number and proportion of studies, we can confidently conclude that there is a reliable negative association between occupational stress and sleep quality. This association is not specific to a particular occupation, country, or region, but has been observed across various occupations and countries or regions. However, it is important to note that the causal relationship between these two factors cannot be determined at present. While one study mentioned the mutual influence between occupational stress and sleep quality,13 the mechanisms underlying this negative association cannot be identified solely through cross-sectional or longitudinal studies.
As mentioned earlier, the studies included in this systematic literature review utilized subjective assessment methods, leading to the determination of occupational stress and sleep quality dimensions based on the employed scales. The PSQI consists of seven dimensions, namely subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction.69 Among these dimensions, sleep disturbances and daytime dysfunction were frequently found to be correlated with occupational stress. On the other hand, the division of dimensions related to occupational stress varied across studies and could be broadly categorized as job demands, work environment, psychological aspects of work, and job rewards. While an overall negative association between occupational stress and sleep quality exists, drawing definitive conclusions at more specific dimensions is challenging. This challenge arises due to the variations in stress sources and subjective stress perceptions among different occupations.80,81 Therefore, when the study population does not consist of specific occupations, researchers should consider the type of work as a variable. Currently, studies primarily focus on exploring the dimensions of occupational stress among nurses or doctors, while investigations into other professions generally identify associations only at the overall level of occupational stress. Conducting more detailed studies on other professions would be a valuable area for future research. It would be meaningful to examine the association between occupational stress and sleep quality in different occupations, particularly among underrepresented groups. However, it is not sufficient to solely verify the negative association; further confirmation of the specific dimensions involved and exploration of the causal relationship between them are required.
Other Factors
Researchers have actively investigated additional factors to gain a better understanding of the relationship between occupational stress and sleep quality. Genetics has received considerable attention in this regard, as it has been found to have indirect effects on the association between occupational stress and sleep quality. Several genetic factors, such as PER3 genotype,48 5-HTR2A genotypes,39,49 and Per3 gene polymorphism,55 have been identified to have combined effects with occupational stress on sleep quality. It is worth noting that these four studies originate from China, and caution should be exercised when generalizing their findings to other countries or regions. Additionally, physical factors like circadian rhythm59 and serum dopamine (DA) levels,52 as well as psychological factors including perseverative cognition,13 psychological capital,32 negative work spillover,61 and self-rated health,62 also play indirect roles in the association between occupational stress and sleep quality. In most of these studies, sleep quality was considered as the dependent variable, with a focus on how other factors interacted with occupational stress to influence sleep quality. The results of these studies indicate the involvement of multiple factors, highlighting the importance of considering their interactions. For instance, examining the combined influence of the three aforementioned genetic factors in future research would be meaningful. Moreover, exploring potential interactive effects among genetics, physiological factors, and psychological factors could be a promising direction for future investigation.
Various factors have been investigated as independent variables to explore their relationship with occupational stress or sleep quality. Psychological factors have received repeated attention, including depression and anxiety9,34,51 mental health,30,58,64 cognitive impairments,54 avoidance,31 and psychological capital.32 Other workplace-related factors9,53,56,63,67 have been found to impact both occupational stress and sleep quality. Gender, age, educational level,30,56,57,63 lifestyle habits,26,53,56 illnesses,29,50,53,56 and pandemic situations63,65 have also shown associations. However, it is important to note that these factors may yield different results in different studies, being associated with either occupational stress, sleep quality, or showing no significant association. While these research findings enhance our understanding of occupational stress and sleep quality, limitations still exist. There is a multitude of factors that can influence occupational stress or sleep quality, and a clear framework for selecting or defining these factors is lacking in previous studies, which poses challenges for systematic reviews and hinders the integration and support among these studies. Measurement tools, particularly scales related to subjective factors, require further development. Lastly, some factors have demonstrated associations with both occupational stress and sleep quality, suggesting the potential for considering them as mediating or moderating variables in future research.
Conclusion
The conclusion of this systematic review examines the research designs and findings of quantitative studies conducted between 2011 and 2022 that investigate the association between occupational stress and sleep quality. Cross-sectional studies were the most frequently employed method, and all studies utilized subjective scales to assess occupational stress and sleep quality. The findings consistently demonstrated a negative association between occupational stress and sleep quality, which was observed across various industries, countries, and regions. However, regarding specific dimensions, no definitive statistical conclusion could be drawn. The studies also identified several other factors that impact occupational stress or sleep quality, including genetics, psychological factors, diseases, and lifestyle habits. Based on these findings, we offer suggestions for future research in this field:
Consider incorporating objective measures in addition to subjective scales to assess occupational stress and sleep quality.
Conduct controlled experiments to establish the causal relationship between occupational stress and sleep quality.
Direct Attention Towards Occupational Groups That Have Not Been Extensively Studied.
Explore the associations between different dimensions of occupational stress and sleep quality, as well as the influence of mediating and moderating variables.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Nakao M. Work-related stress and psychosomatic medicine. Biopsychosoc Med. 2010;4(1):4. doi: 10.1186/1751-0759-4-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davies ACL. Stress at work: individuals or structures? Indust Law J. 2022;51(2):403–434. doi: 10.1093/indlaw/dwab006 [DOI] [Google Scholar]
- 3.Dávila Morán RC, Sánchez Soto JM, López Gómez HE, et al. Work stress as a consequence of the COVID-19 pandemic: a systematic review. Sustainability. 2023;15(6):4701. doi: 10.3390/su15064701 [DOI] [Google Scholar]
- 4.Park S, Jang MK. Associations between workplace exercise interventions and job stress reduction: a systematic review. Workplace Health Saf. 2019;67(12):592–601. doi: 10.1177/2165079919864979 [DOI] [PubMed] [Google Scholar]
- 5.Wu S, Pitafi AH, Pitafi S, Ren M. Investigating the consequences of the socio-instrumental use of enterprise social media on employee work efficiency: a work-stress environment. Front Psychol. 2021;12:738118. doi: 10.3389/fpsyg.2021.738118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuper H, Marmot M. Job strain, job demands, decision latitude, and risk of coronary heart disease within the Whitehall II study. J Epidemiol Community Health. 2003;57(2):147–153. doi: 10.1136/jech.57.2.147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Urbanetto JS, Magalhães MCC, Maciel VO, et al. Work-related stress according to the demand-control model and minor psychic disorder in nursing workers. Rev Esc Enferm USP. 2013;47(5):1186–1193. doi: 10.1590/S0080-623420130000500024 [DOI] [PubMed] [Google Scholar]
- 8.Gosselin E, Bourgault P, Lavoie S. Association between job strain, mental health and empathy among intensive care nurses. Nurs Crit Care. 2016;21(3):137–145. doi: 10.1111/nicc.12064 [DOI] [PubMed] [Google Scholar]
- 9.Song KW, Kim HK. Job stress and its related factors among Korean dentists: an online survey study. Int Dent J. 2019;69(6):436–444. doi: 10.1111/idj.12513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bliese PD, Edwards JR, Sonnentag S. Stress and well-being at work: a century of empirical trends reflecting theoretical and societal influences. J Appl Psychol. 2017;102(3):389–402. doi: 10.1037/apl0000109 [DOI] [PubMed] [Google Scholar]
- 11.Amiri S, Behnezhad S. Is job strain a risk factor for musculoskeletal pain? A systematic review and meta-analysis of 21 longitudinal studies. Public Health. 2020;181:158–167. doi: 10.1016/j.puhe.2019.11.023 [DOI] [PubMed] [Google Scholar]
- 12.Magnavita N, Capitanelli I, Garbarino S, Pira E. Work-related stress as a cardiovascular risk factor in police officers: a systematic review of evidence. Int Arch Occup Environ Health. 2018;91(4):377–389. doi: 10.1007/s00420-018-1290-y [DOI] [PubMed] [Google Scholar]
- 13.Van Laethem M, Beckers DCJ, Kompier MAJ, Kecklund G, van den Bossche SNJ, Geurts SAE. Bidirectional relations between work-related stress, sleep quality and perseverative cognition. J Psychosomat Res. 2015;79(5):391–398. doi: 10.1016/j.jpsychores.2015.08.011 [DOI] [PubMed] [Google Scholar]
- 14.Alkhawaldeh JMA, Soh KL, Mukhtar FBM, Ooi CP. Effectiveness of stress management interventional programme on occupational stress for nurses: a systematic review. J Nurs Manag. 2020;28(2):209–220. doi: 10.1111/jonm.12938 [DOI] [PubMed] [Google Scholar]
- 15.Sonnentag S, Frese M. Stress in Organizations. In: Handbook of Psychology. 2nd. John Wiley & Sons, Ltd; 2012. doi: 10.1002/9781118133880.hop212021 [DOI] [Google Scholar]
- 16.St-Onge MP, Grandner MA, Brown D, et al. Sleep duration and quality: impact on lifestyle behaviors and cardiometabolic health: a scientific statement from the American heart association. Circulation. 2016;134(18):e367–e386. doi: 10.1161/CIR.0000000000000444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dlugaj M, Weinreich G, Weimar C, et al. Sleep-disordered breathing, sleep quality, and mild cognitive impairment in the general population. J Alzheimers Dis. 2014;41(2):479–497. doi: 10.3233/JAD-132132 [DOI] [PubMed] [Google Scholar]
- 18.Alvaro PK, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36(7):1059–1068. doi: 10.5665/sleep.2810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gregory AM, O’connor TG. Sleep problems in childhood: a longitudinal study of developmental change and association with behavioral problems. J Am Acad Child Adolesc Psychiatry. 2002;41(8):964–971. doi: 10.1097/00004583-200208000-00015 [DOI] [PubMed] [Google Scholar]
- 20.Songkham W, Deeluea J, Suksatit B, Chaiard J. Sleep quality among industrial workers: related factors and impact. J Health Res. 2019;33(2):119–126. doi: 10.1108/JHR-08-2018-0072 [DOI] [Google Scholar]
- 21.Tarhan M, Aydin A, Ersoy E, Dalar L. The sleep quality of nurses and its influencing factors. Eurasian J Pulmonol. 2018;20(2):78–84. doi: 10.4103/ejop.ejop_35_18 [DOI] [Google Scholar]
- 22.Chaiard J, Deeluea J, Suksatit B, Songkham W. Factors associated with sleep quality of Thai intercity bus drivers. Ind Health. 2019;57(5):596–603. doi: 10.2486/indhealth.2018-0168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xue B, Xue Y, Zheng X, et al. Association of sleep with mental health in Chinese high school students: a cross-sectional study. J Sleep Res. 2022;31(6):e13697. doi: 10.1111/jsr.13697 [DOI] [PubMed] [Google Scholar]
- 24.Kohyama J. Which is more important for health: sleep quantity or sleep quality? Children. 2021;8(7):542. doi: 10.3390/children8070542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fabbri M, Beracci A, Martoni M, Meneo D, Tonetti L, Natale V. Measuring subjective sleep quality: a review. Int J Environ Res Public Health. 2021;18(3):1082. doi: 10.3390/ijerph18031082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shimura A, Sugiura K, Inoue M, et al. Which sleep hygiene factors are important? Comprehensive assessment of lifestyle habits and job environment on sleep among office workers. Sleep Health. 2020;6(3):288–298. doi: 10.1016/j.sleh.2020.02.001 [DOI] [PubMed] [Google Scholar]
- 27.Scott RQ, Rodríguez AJ. Improving quality of sleep in healthy adults. Curr Pulmonol Rep. 2023;12(2):46–55. doi: 10.1007/s13665-023-00304-1 [DOI] [Google Scholar]
- 28.Kageyama T, Nishikido N, Kobayashi T, Kurokawa Y, Kaneko T, Kabuto M. Self-reported sleep quality, job stress, and daytime autonomic activities assessed in terms of short-term heart rate variability among male white-collar workers. Ind Health. 1998;36(3):263–272. doi: 10.2486/indhealth.36.263 [DOI] [PubMed] [Google Scholar]
- 29.Li X, Gao X, Liu J. Cross-sectional survey on the relationship between occupational stress, hormone levels, and the sleep quality of oilfield Workers in Xinjiang, China. Int J Environ Res Public Health. 2019;16(18):3316. doi: 10.3390/ijerph16183316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li X, Xue Q, Yi X, Liu J. The interaction of occupational stress, mental health, and cytokine levels on sleep in Xinjiang oil workers: a cross-sectional study. Front Psychiatry. 2022;13:924471. doi: 10.3389/fpsyt.2022.924471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rasdi I, Fadzil FF. The association between noise, work stress and coping with sleep quality among cable manufacturing workers. Asian J Agric Biol. 2018;6:108–111. [Google Scholar]
- 32.Xie Y, Tian J, Jiao Y, Liu Y, Yu H, Shi L. The impact of work stress on job satisfaction and sleep quality for couriers in China: the role of psychological capital. Front Psychol. 2021;12:730147. doi: 10.3389/fpsyg.2021.730147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Deng X, Liu X, Fang R. Evaluation of the correlation between job stress and sleep quality in community nurses. Medicine. 2020;99(4):e18822. doi: 10.1097/MD.0000000000018822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Song KW, Choi WS, Jee HJ, et al. Correlation of occupational stress with depression, anxiety, and sleep in Korean dentists: cross-sectional study. BMC Psychiatry. 2017;17(1):398. doi: 10.1186/s12888-017-1568-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Takaesu Y, Shimura A, Komada Y, et al. Association of sleep duration on workdays or free days and social jetlag with job stress. Psychiatry Clin Neurosci. 2021;75(8):244–249. doi: 10.1111/pcn.13274 [DOI] [PubMed] [Google Scholar]
- 36.Rabei S, Mourad G, Hamed AED. Work stress and sleep disturbances among internship nursing students. Middle East Curr Psychiat. 2020;27(1):24. doi: 10.1186/s43045-020-00032-1 [DOI] [Google Scholar]
- 37.Han Y, Yuan Y, Zhang L, Fu Y. Sleep disorder status of nurses in general hospitals and its influencing factors. Psychiatr Danub. 2016;28(2):176–183. [PubMed] [Google Scholar]
- 38.Iwasaki S, Deguchi Y, Inoue K. Association between work role stressors and sleep quality. Occup Med-Oxf. 2018;68(3):171–176. doi: 10.1093/occmed/kqy021 [DOI] [PubMed] [Google Scholar]
- 39.Gao X, Ge H, Jiang Y, Lian Y, Zhang C, Liu J. Relationship between job stress and 5-HT2A receptor polymorphisms on self-reported sleep quality in physicians in Urumqi (Xinjiang, China): a cross-sectional study. Int J Environ Res Public Health. 2018;15(5):1034. doi: 10.3390/ijerph15051034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Saalwirth C, Leipold B. Sleep and chronotype in relation to work-related stress and negative affect: the moderating role of a flexible start of work. Somnologie. 2021;25. doi: 10.1007/s11818-021-00294-9 [DOI] [Google Scholar]
- 41.Sousa A, Santos R, Silva R, Santos C, Lopes V, Mussi F. Occupational stress and sleep quality in professors of the health area. Revista da Rede de Enfermagem do Nordeste. 2018;19:e33088. doi: 10.15253/2175-6783.20181933088 [DOI] [Google Scholar]
- 42.Sayapathi BS, Denis N, Ting AS. Occupational stress and burnout among staffs in hospitals: a systematic review. Tarih Kult Sanat Arast Derg. 2020;9(2):425–431. doi: 10.7596/taksad.v9i2.2695 [DOI] [Google Scholar]
- 43.Godos J, Grosso G, Castellano S, Galvano F, Caraci F, Ferri R. Association between diet and sleep quality: a systematic review. Sleep Med Rev. 2021;57:101430. doi: 10.1016/j.smrv.2021.101430 [DOI] [PubMed] [Google Scholar]
- 44.Dinis J, Braganca M. Quality of sleep and depression in college students: a systematic review. Sleep Sci. 2018;11(4):290–301. doi: 10.5935/1984-0063.20180045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Banno M, Harada Y, Taniguchi M, et al. Exercise can improve sleep quality: a systematic review and meta-analysis. PeerJ. 2018;6:e5172. doi: 10.7717/peerj.5172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liberati A, Altman DG, Tetzlaff J. PRISMA Statement per il reporting di revisioni sistematiche e meta-analisi degli studi che valutano gli interventi sanitari: spiegazione ed elaborazione. Evidence. 2015. doi: 10.4470/e1000115 [DOI] [Google Scholar]
- 47.Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12(12):1500–1524. doi: 10.1016/j.ijsu.2014.07.014 [DOI] [PubMed] [Google Scholar]
- 48.Peng X, Li J, Han B, et al. Association of occupational stress, period circadian regulator 3 (PER3) gene polymorphism and their interaction with poor sleep quality. J Sleep Res. 2022;31(1):e13390. doi: 10.1111/jsr.13390 [DOI] [PubMed] [Google Scholar]
- 49.Jiang Y, Cui C, Ge H, Guan S, Lian Y, Liu J. Effect of 5-HT2A receptor polymorphisms and occupational stress on self-reported sleep quality: a cross-sectional study in Xinjiang, China. Sleep Med. 2016;20:30–36. doi: 10.1016/j.sleep.2015.12.007 [DOI] [PubMed] [Google Scholar]
- 50.Yook YS, Sanada K. Firefighters’ occupational stress and its correlations with cardiorespiratory fitness, arterial stiffness, heart rate variability, and sleep quality. PLoS One. 2019;14(12):e0226739. doi: 10.1371/journal.pone.0226739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gu B, Tan Q, Zhao S. The association between occupational stress and psychosomatic wellbeing among Chinese nurses: a cross-sectional survey. Medicine. 2019;98(22):e15836. doi: 10.1097/MD.0000000000015836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jiang Y, Liu B, Wu C, et al. Dopamine Receptor D2 Gene (DRD2) polymorphisms, job stress, and their interaction on sleep dysfunction. Int J Environ Res Public Health. 2020;17(21):8174. doi: 10.3390/ijerph17218174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dong H, Zhang Q, Zhang Z, Zhu C. Association of sleep disturbance with shift work, occupational stress, and musculoskeletal pain in Chinese public hospital emergency workers: a multicentre cross-sectional study. Chronobiol Int. 2022;39(6):886–894. doi: 10.1080/07420528.2022.2048662 [DOI] [PubMed] [Google Scholar]
- 54.Eskildsen A, Fentz HN, Andersen LP, Pedersen AD, Kristensen SB, Andersen JH. Perceived stress, disturbed sleep, and cognitive impairments in patients with work-related stress complaints: a longitudinal study. Stress. 2017;20(4):371–378. doi: 10.1080/10253890.2017.1341484 [DOI] [PubMed] [Google Scholar]
- 55.Wang J, Liu J, Xie H, Gao X. Effects of work stress and period3 gene polymorphism and their interaction on sleep quality of non-manual workers in Xinjiang, China: a cross-sectional study. Int J Environ Res Public Health. 2022;19(11):6843. doi: 10.3390/ijerph19116843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dong H, Zhang Q, Zhu C, Lv Q. Sleep quality of nurses in the emergency department of public hospitals in China and its influencing factors: a cross-sectional study. Health Qual Life Outcomes. 2020;18(1):116. doi: 10.1186/s12955-020-01374-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.D’Ettorre G, Pellicani V, Caroli A, Greco M. Shift work sleep disorder and job stress in shift nurses: implications for preventive interventions. Med Lav. 2020;111(3):195–202. doi: 10.23749/mdl.v111i3.9197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pereira D, Elfering A. Social stressors at work, sleep quality and psychosomatic health complaints--a longitudinal ambulatory field study. Stress Health. 2014;30(1):43–52. doi: 10.1002/smi.2494 [DOI] [PubMed] [Google Scholar]
- 59.Wu S, Wu C, Wang X, Fei W, Fu Y. Mediating effect of circadian rhythm between work stress and sleep quality in Chinese shift-working nurses: a cross-sectional survey. Nurs Open. 2023;10(2):560–569. doi: 10.1002/nop2.1322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Myllyntausta S, Salo P, Kronholm E, et al. Does removal of work stress explain improved sleep following retirement? The Finnish Retirement and Aging study. Sleep. 2019;42(8):zsz109. doi: 10.1093/sleep/zsz109 [DOI] [PubMed] [Google Scholar]
- 61.Kim YK, Kramer A, Pak S. Job insecurity and subjective sleep quality: the role of spillover and gender. Stress Health. 2020. doi: 10.1002/smi.2974 [DOI] [Google Scholar]
- 62.Leitaru N, Kremers S, Hagberg J, Björklund C, Kwak L. Associations between job-strain, physical activity, health status, and sleep quality among Swedish municipality workers. J Occup Environ Med. 2019;61(2):e56–e60. doi: 10.1097/JOM.0000000000001516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bilgic S, Celikkalp U, Misirli C. Stress level and sleep quality of nurses during the COVID-19 pandemic. Work. 2021;70(4):1021–1029. doi: 10.3233/WOR-210538 [DOI] [PubMed] [Google Scholar]
- 64.Herr RM, Barrech A, Riedel N, Gündel H, Angerer P, Li J. Long-term effectiveness of stress management at work: effects of the changes in perceived stress reactivity on mental health and sleep problems seven years later. Int J Environ Res Public Health. 2018;15(2):255. doi: 10.3390/ijerph15020255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bernburg M, Hetzmann MS, Mojtahedzadeh N, et al. Stress perception, sleep quality and work engagement of German outpatient nurses during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;19(1):313. doi: 10.3390/ijerph19010313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hartley TA, Violanti JM, Sarkisian K, et al. Association between police-specific stressors and sleep quality: influence of coping and depressive symptoms. J Law Enforc Leadersh Ethics. 2014;1(1):31–48. [PMC free article] [PubMed] [Google Scholar]
- 67.Abbasi M, Rajabi M, Yazdi Z, Shafikhani A. Factors affecting sleep quality in firefighters. Sleep Hypn. 2018;20:283–289. doi: 10.5350/Sleep.Hypn.2018.20.0163 [DOI] [Google Scholar]
- 68.Zhang Y, Punnett L, McEnany GP, Gore R. Contributing influences of work environment on sleep quantity and quality of nursing assistants in long-term care facilities: a cross-sectional study. Geriatr Nurs. 2016;37(1):13–18. doi: 10.1016/j.gerinurse.2015.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 70.Forbes O, Schwenn PE, Wu PP, et al. EEG-based clusters differentiate psychological distress, sleep quality and cognitive function in adolescents. Biol Psychol. 2022:173. doi: 10.1016/j.biopsycho.2022.108403 [DOI] [PubMed] [Google Scholar]
- 71.Krystal AD, Edinger JD. Measuring sleep quality. Sleep Med. 2008;9:S10–S17. doi: 10.1016/S1389-9457(08)70011-X [DOI] [PubMed] [Google Scholar]
- 72.Perez-Valero E, Vaquero-Blasco MA, Lopez-Gordo MA, Morillas C. Quantitative assessment of stress through EEG during a virtual reality stress-relax session. Front Comput Neurosci. 2021;15:684423. doi: 10.3389/fncom.2021.684423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pourmohammadi S, Maleki A. Continuous mental stress level assessment using electrocardiogram and electromyogram signals. Biomed Signal Process Control. 2021;68:102694. doi: 10.1016/j.bspc.2021.102694 [DOI] [Google Scholar]
- 74.Gray-Toft P, Anderson JG. Stress among hospital nursing staff: its causes and effects. Soc Sci Med A. 1981;15(5):639–647. doi: 10.1016/0271-7123(81)90087-0 [DOI] [PubMed] [Google Scholar]
- 75.Inc G. State of the global workplace report. Gallup.com; 2023. https://www.gallup.com/workplace/349484/state-of-the-global-workplace.aspx. Accessed October 24, 2023.
- 76.Deloitte Global. The Deloitte Global 2022 Gen Z and Millennial Survey; 2022. https://www.deloitte.com/global/en/issues/work/genzmillennialsurvey-2022.html. Accessed October 24, 2023.
- 77.Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB. Prevalence of healthy sleep duration among adults--United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(6):137–141. doi: 10.15585/mmwr.mm6506a1 [DOI] [PubMed] [Google Scholar]
- 78.National Heart, Lung, and Blood Institute (NHLBI). Sleep deprivation and deficiency. Sleep deprivation and deficiency; 2022. https://www.nhlbi.nih.gov/health/sleep-deprivation. Accessed October 24, 2023.
- 79.Wang J, Zhang Y, Zhang Y. Annual Sleep Report of China 2023. Social Sciences Academic Press; 2023. [Google Scholar]
- 80.Goktas O, Tekin O, Sencan I. Attitudes to the challenges of life among different occupation groups. Turk J Med Sci. 2011;41(6):1051–1057. doi: 10.3906/sag-1009-1094 [DOI] [Google Scholar]
- 81.Zhong F, Yano E, Lan Y, Wang M, Wang Z, Wang X. Mental ability and psychological work performance in Chinese workers. Ind Health. 2006;44(4):598–603. doi: 10.2486/indhealth.44.598 [DOI] [PubMed] [Google Scholar]