ABSTRACT
Immunological dysregulation and inflammation may play a role in the nature of menstruation. Coronavirus disease 2019 (COVID-19) can produce a systemic inflammatory reaction that involves extrapulmonary organs and can also affect the immune system. This study aimed to analyze changes in the menstrual cycle in coronavirus (COVID)-positive women of reproductive age.
Methods:
The data of 35 women of reproductive age were collected telephonically from said patients admitted to the COVID Health Centre (CHC) ward of All India Institute of Ayurveda, New Delhi, during June 20, 2020, to October 31, 2020. Purposive sampling was used for data collection. Wyatt menstrual pictogram and Visual Analogue Scale (VAS) were used to assess the bleeding pattern and pain during menstruation, respectively.
Results:
Clinically, changes were noted in post-COVID menstruation such as irregularity, polymenorrhea, oligomenorrhea, clots, and menstrual flow in days. However, all results were statistically non-significant. But significant (P = 0.003) menstrual pain was reported.
Conclusion:
Menstrual changes were observed in COVID-19-positive women belonging to the reproductive age group.
Keywords: COVID-19, dysmenorrhea, heavy bleeding, menstrual cycle
Introduction
Community transmission of coronavirus disease 2019 (COVID-19) was first reported on December 2019 in Wuhan, China, and it was recognized as a pandemic by the World Health Organization (WHO) on the March 11, 2020. It may be considered as the worst health-care crisis for human society after the establishment of the WHO.[1]
It has been documented that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) attacks the organs that express angiotensin-converting enzyme 2 (ACE2), such as the lungs, kidneys, heart, breasts, intestine, testes, ovaries, etc.[2] It has also been documented in various studies that the involvement or impact of COVID-19 infection on the respiratory system,[3] gastrointestinal system,[4] circulatory systems,[5] nervous systems,[6] etc., However, there is very limited information on the effect of COVID-19 infection on the female reproductive system, especially on the menstrual cycle. Some studies reported that some viral infections directly correlate with changes in the female reproductive system, such as the duration of a menstrual cycle or the volume of menstruation.[7] One study reported that women living with Human Immunodeficiency Viruses (HIV) had approximately 1.7 times higher chance of developing amenorrhea than matched controls without HIV.[8] A few studies also observed the effects of hepatitis C and hepatitis B infection on the nature of menstrual cycle.[9] Along that line, some updated data have claimed that SARS-CoV-2 infection, COVID-19 vaccine, and/or psychological stress related to the COVID-19 pandemic may influence the menstrual cycle.[10] However, there has been very limited research on this topic worldwide.
Findings of the previous studies stated changes in the menstrual cycle: mainly a decrease in menstrual volume and a prolongation of the menstrual cycle. They also indicated that the severity of COVID-19 did not play a role in menstrual cycle changes.[11] It was also observed that women who had taken COVID-19 vaccines may have experienced menstrual abnormalities, like menorrhagia, metrorrhagia, and polymenorrhea.[12] All previous studies had limitations: They were not assessed for psychological stress levels, COVID-19 therapy, comorbidities, and other possible confounding factors to distinguish the impact of all of these.
The SARS-CoV-2 virus is mutating, and restrictions constantly change and differ between different countries. Thus, this study was designed to observe changes in the menstrual cycle of women of reproductive age after SARS-CoV-2 infection during the pandemic in India. This study’s findings could provide primary healthcare providers with valuable insights into how to better serve women of reproductive age.
Methodology
Study design
This was an observational, cross-sectional study.
Study area
COVID Health Centre (CHC) ward of All India Institute of Ayurveda (AIIA), New Delhi
Study duration
June 20, 2020, to October 31, 2020
Sampling procedure
Purposive sampling procedure was applied for the selection of samples.
Inclusion criteria
COVID-positive female patients of reproductive age group (age: 18–45 years)
Diagnosed using reverse transcription polymerase chain reaction (RT-PCR) test
Not pregnant during data collection
Registered patients in COVID Health Centre (CHC) ward of All India Institute of Ayurveda
Exclusion criteria
Women who were on hormonal replacement treatment or taking contraceptive pills
Pregnant women
Women who had chronic diseases (Type 2 diabetes mellitus, hypertension, cancer, polycystic ovarian disease, etc.)
Fever cases which were not diagnosed as COVID-19 by RT-PCR test
As there was no female patient admitted with severe symptoms of COVID-19 to the CHC during this period, severe symptoms of COVID-19 could not be included in this study.
Data collection tools
A questionnaire [Table 1] containing past and present menstrual history, Wyatt menstrual pictogram, and the Visual Analogue Scale (VAS) were used for data collection. The Wyatt menstrual pictogram and the VAS were used to assess the flow of menstrual bleeding pattern and pain during menstruation, respectively.
Table 1.
Questionnaire on menstrual pattern before and after COVID-19
| S. No | Questions |
|---|---|
| 1 | Have you ever been COVID +ve? Yes/No |
| 2 | If yes, when did you become COVID positive? |
| 3 | After how many days did your report come out to be negative? |
| 4 | Did you face any complications during that period? |
| Yes/No. If yes, then what? | |
| 5 | Which path did you opt for the treatment? |
| 6 | Do you feel any change in your normal pattern of menstrual cycle? Yes/No |
| 7A | Past menstrual history: |
| i) Did you have regular/irregular periods? | |
| ii) What was the usual interval period between periods? | |
| iii) What were the number of flow days? | |
| Proposed gradings: | |
| Grade 0 – Normal (less than 5 days) | |
| Grade 1 – Mild (5–7 days) | |
| Grade 2 – Moderate (8–10 days) | |
| Grade 3 – Severe (greater than 10 days) | |
| iv) What was the bleeding pattern? | |
| Toilets: Volume of blood loss in the toilet when changing sanitary wear | |
| Score: 1=Light bleeding | |
| 3=Moderate bleeding | |
| 5=Heavy bleeding | |
| Clots score: 1=Small clots towels=1=Lightly stained with blood | |
| 3=Medium clots 2=Moderately stained with blood | |
| 5=Large clots 20=Heavily stained with blood | |
| v) Did you suffer from painful menstruation? | |
| No pain=0–1 | |
| Mild pain=2 | |
| Moderate pain (interferes with task) =3–4 | |
| Moderate pain (interferes with concentration) =5–6 | |
| Severe pain (interferes with basic needs) =7–8 | |
| Worst pain possible (bedrest required) =9–10 | |
| 7B | Present menstrual history: |
| i) Do you have regular/irregular periods? | |
| ii) What is the normal interval period between periods? | |
| iii) What is the number of flow days? | |
| iv) What is the bleeding pattern? (The same scale is used as in past menstrual history.) | |
| v) Do you suffer from painful menstruation? (Same VAS was used.) | |
| 8 | If any irregularity, have you undergone any investigations? |
| 9 | Obstetric history: |
| Gravida | |
| Parity | |
| Live births | |
| Abortions |
Quantitative variables
Interval period, number of flow days, bleeding pattern (Wyatt menstrual pictogram), pain (VAS) were analyzed by comparing pre- and post-COVID menstrual history.
Data collection procedure
A total of 47 female patients were admitted to the hospital during June 20, 2020, to October 31, 2020, for management of COVID-19. The list of patients was obtained from the hospital records after receiving approval from the competent authority. Over telephone, the participants were communicated for their consent to participate in this study. After receiving consent and being screened according to the inclusion and exclusion criteria, a total of 35 patients were found to be fit for this study and they were included in this project [Figure 1]. The identified subjects were communicated further on the third month of discharge from the CHC. All observed data compared and analyzed on the basis of third-month observation. Pictorial diagram was shared with the subjects over WhatsApp for better understanding. These follow up activities were the routine procedure of the institute for follow-up the COVID positive patients.
Figure 1.
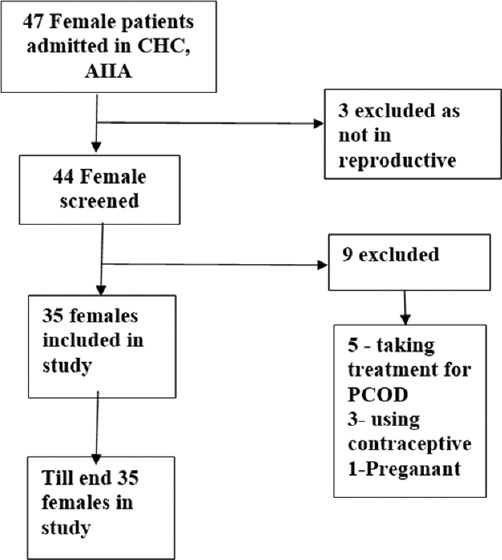
Participant recruitment flowchart
Ethical clarence
Permission for conducting this study was taken from the competent authority of the institute. All data are used only for analysis with permission of the concerned authority.
Data analysis
After data collection, all data were checked thoroughly for consistency and completeness. IBM SPSS Statistics for Windows version 11.5 (SPSS Inc., Chicago, IL, USA) was used to analyze the data. All the data were expressed as mean ± standard deviation (SD), frequency, and percentage, as appropriate. Chi-squared test was attempted for observed changes in pre- and post-infection stage.
Results
The data of 35 female participants were analyzed. According to marital status, both married and unmarried women were included in the study. During the post-COVID phase, almost half (48.57%) of the female participants experienced alterations in their menstrual cycle. The female participants were 8.57%, 2.86%, 14.29%, 25.71%, 25.71%, 22.86% of 14-18 years, 19-22 years, 23-26 yrs, 27-30 yrs, 31-34 yrs age group respectively. The average age of the 35 women was 28.4 years [Graph 1]. More than half (57%) of them were married, whereas 43% of the participants were single. A gross 28.57%, 57.14%, and 14.28% of the participants were suffering with asymptomatic, mild, and moderately symptomatic symptoms of COVID-19, respectively.
Graph 1.

Age-wise distribution of female participants
Before SARS-CoV-2 infection, 32 (91.4%) women had history of regular menstrual cycle. However, after said infection, only 25 (71.4%) women had a regular menstrual cycle. The menstrual cycle of 8 (25%) women changed to irregular from history of regular menstrual cycle [Table 2]. This change was not statistically significant (P = 0.39).
Table 2.
Cross tabulation of the regularity of menstrual cycle in pre- and post-SARS-CoV-2 infection stage
| Post-SARS-CoV-2 infection stage | Total | P | |||
|---|---|---|---|---|---|
|
| |||||
| Regular menstrual cycle | Irregular menstrual cycle | ||||
| Pre-SARS-CoV-2 infection stage | Regular menstrual cycle | 24 (75%) | 8 (25%) | 32 (91.4%) | 0.39 |
| Irregular menstrual cycle | 1 (33%) | 2 (66%) | 3 (8.6%) | ||
| Total | 25 (71.4%) | 10 (28.6%) | 35 (100%) | ||
It was observed that 32 (91.4%) and 3 (8.6%) women had normal duration of menstrual cycle (21–35 days) and oligomenorrhea, respectively, (>35 days) before SARS-CoV-2 infection [Table 3]. Among the 32 women with normal duration of menstrual cycle, 2 (6.25%) and 6 (18.75%) of them were diagnosed with polymenorrhea and oligomenorrhea after SARS-CoV-2 infection. These changes were not statistically significant (P = 0.39).
Table 3.
Cross tabulation of duration of menstrual cycle in pre- and post-SARS-CoV-2 infection stage
| Post-SARS-CoV-2 infection stage | Total | P | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Normal duration of menstrual cycle (21–35 days) | Polymenorrhea (<21 days) | Oligomenorrhea (>35 days) | ||||
| Pre-SARS-CoV-2 infection stage | Normal duration of menstrual cycle (21–35 days) | 24 (75%) | 2 (6.25%) | 6 (18.75%) | 32 (91.4%) | 0.39 |
| Oligomenorrhea (>35 days) | 1 (33%) | 0 (0%) | 2 (66%) | 3 (8.6%) | ||
| Total | 25 (71.4%) | 2 (5.7%) | 8 (22.8%) | 35 (100%) | ||
Only 32 (91.4%) women had history of small colts in their menstrual blood before SARS-CoV-2 infection. However, we observed that 24 (68.6%) women reported small clots in their menstrual blood after infection. This change was not statistically significant (P = 0.549) [Table 4].
Table 4.
Cross tabulation of type of blood clots during menstrual cycle in pre- and post-SARS-CoV-2 infection stage
| Post-SARS-CoV-2 infection stage | Total | P | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Small clots | Medium clots | Large clots | ||||
| Pre-SARS-CoV-2 infection stage | Small clots | 22 (69%) | 8 (25%) | 2 (6.25%) | 32 (91.4%) | 0.549 |
| Medium clots | 1 (50%) | 1 (50%) | 0 | 2 (6.25%) | ||
| Large clots | 1 (100%) | 0 | 0 | 1 (3.12%) | ||
| Total | 24 (68.6%) | 9 (25.7%) | 2 (5.71%) | 35 (100%) | ||
Before SARS-CoV-2 infection, the duration of menstrual flow was 4.014 ± 0.87 (mean ± SD). After the infection, the duration of menstrual flow was 4.511 ± 2.14 days [Table 5]. This difference was not statistically significant (P = 0.186) [Table 6].
Table 5.
Distribution of flow of days and VAS score during menstrual cycle in pre- and post-SARS-CoV-2 infection stage
| Paired samples statistics | |||||
|---|---|---|---|---|---|
|
| |||||
| Mean | n | Standard deviation | Standard error mean | ||
| Flow in days | Pre-SARS-CoV-2 infection | 4.014 | 35 | 0.8785 | 0.1485 |
| Post-SARS-CoV-2 infection | 4.511 | 35 | 2.1486 | 0.3632 | |
| VAS score | Pre-SARS-CoV-2 infection | 2.00 | 35 | 1.609 | 0.272 |
| Post-SARS-CoV-2 infection | 3.09 | 35 | 2.020 | 0.341 | |
Table 6.
Pair difference on flow of days and VAS score of menstrual cycle in pre- and post-SARS-CoV-2 infection stage
| Pair differences | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Mean | SD | SE mean | 95% CI of the differences | t | df | Sig. (2-tailed) | |||
|
| |||||||||
| Lower | Upper | ||||||||
| Pair 1 | Flow in days | −0.497 | 2.18 | 0.368 | −1.246 | 0.252 | −1.349 | 34 | 0.186 |
| Pair 2 | VAS score | −1.086 | 2.02 | 0.341 | −0.392 | −3.18 | −3.180 | 34 | 0.003* |
The VAS score (pain score) of participants were 2.00 ± 1.609 and 3.09 ± 2.02 before infection and after infection, respectively. The difference in pain score was statistically significant (P = 0.003) [Table 6].
Discussion
We conducted this study to analyze changes in the menstrual cycle of COVID-positive women of reproductive age. It was an observational study in which the enrolled 35 participants were observed prospectively for menstrual irregularities. Of these, 17 participants (48.57%) experienced alterations in their menstrual cycle. Among 32 women with a normal duration of menstrual cycle, 2 (6.25%) and 6 (18.75%) were diagnosed with polymenorrhea and oligomenorrhea after SARS-CoV-2 infection. Even though the symptoms were insignificant, a probable cause of these symptoms may be attributed to changes in the expression of the ACE2 receptor in the ovaries, which has an impact on menstrual hormone production.
It is reported that COVID-19 in a patient is normally followed by several post-COVID effects. The impact of SARS-CoV-2 infection on tissues is determined by its capacity to enter and infect cells in that tissue. The entry point of SARS-CoV-2 on the cell is ACE2 that plays a pivotal role in the renin-angiotensin system. When SARS-CoV-2 gains cell entry, downregulation of the expression of ACE2 occurs followed by disruption of the renin-angiotensin system, and thus begins the upregulation of many proinflammatory responses.[13] ACE2 is highly expressed in the ovaries and plays a key role in the regulation of follicular development, ovulation, and luteal angiogenesis and is responsible for the physiological changes in endometrial tissue. SARS-CoV-2 infection is usually accompanied by high levels of interleukin-6, interleukin-8, tumor necrosis factor α, and other cytokines, all of which promote a pro-coagulation state that may affect fetal implantation and development.[14]
The VAS score (pain score) of participants were 2.00 ± 1.609 and 3.09 ± 2.02 before infection and after infection, respectively. The differences in pain score were statistically significant. COVID-19 is considered a pro-inflammatory disease, which generates a cytokine storm and consequent immune exhaustion.[15] So the probable cause of post-COVID dysmenorrhea may be attributed to these inflammatory changes.
As per the WHO reports, the COVID-19 pandemic triggered a 25% increase in the prevalence of anxiety and depression worldwide.[16] As per a study, patients with high perceived stress scale (PSS) scores during COVID-19 were more likely to experience a longer duration of menses and heavier bleeding during menses compared with those with moderate COVID-19 PSS scores.[17] Unfortunately, we could not assess the mental strength of the participants the current study. However, it is clear from similar studies that menstrual symptoms are associated with different common mental health disorders. Therefore, we should take a holistic approach when caring for such patients, such as ensuring a proper dietary pattern along with patients engaging in physical activities and counseling.
Limitations
This observational study was carried out on only 35 female patients of a single center. So, there is required to conduct a multi-centric survey with large sample size for further conclusion. Stress levels and biochemical tests were not evaluated to rule out endocrinological and psychological determinants on the nature of menstrual cycle.
Conclusion
The menstrual cycle of a few women was observed to have changed after SARS-CoV-2 infection. The pain score significantly increased after the infection. Thus, special attention needs to be paid to the reproductive system when treating COVID-19 in women belonging to the reproductive age group. Further research in that domain will be the way forward for preparing the management guideline in this matter from the learning of the study.
Financial support and sponsorship
All India Institute of Ayurveda, Gautampuri, Mathura Road, New Delhi, India.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
MRD AIIA, All Patients who were supported for data collection.
References
- 1.Acharyya A. Prospect of Ayurveda system of medicine in recent COVID-19 Pandemic in India. International Journal of Ayurveda and Traditional Medicine. 2020;2:26–9. [Google Scholar]
- 2.Di Gennaro F, Pizzol D, Marotta C, Antunes M, Racalbuto V, Veronese N, et al. Coronavirus diseases (COVID-19) current status and future perspectives:A narrative review. Int J Environ Res Public Health. 2020;17:2690. doi: 10.3390/ijerph17082690. doi:10.3390/ijerph17082690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lovato A, De Filippis C. Clinical presentation of COVID-19:A systematic review focusing on upper airway symptoms. Ear Nose Throat J. 2020;99:569–76. doi: 10.1177/0145561320920762. [DOI] [PubMed] [Google Scholar]
- 4.Villapol S. Gastrointestinal symptoms associated with COVID-19:Impact on the gut microbiome. Transl Res. 2020;226:57–69. doi: 10.1016/j.trsl.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med. 2022;28:583–90. doi: 10.1038/s41591-022-01689-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spudich S, Nath A. Nervous system consequences of COVID-19. Science. 2022;375:267–9. doi: 10.1126/science.abm2052. [DOI] [PubMed] [Google Scholar]
- 7.Lebar V, Laganà AS, Chiantera V, Kunič T, Lukanović D. The Effect of COVID-19 on the menstrual cycle:A systematic review. J Clin Med. 2022;11:3800. doi: 10.3390/jcm11133800. doi:10.3390/jcm11133800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.King EM, Albert AY, Murray MC. HIV and amenorrhea:A meta-analysis. Aids. 2019;33:483–91. doi: 10.1097/QAD.0000000000002084. [DOI] [PubMed] [Google Scholar]
- 9.Kurmanova AM, Kurmanova GM, Lokshin VN. Reproductive dysfunctions in viral hepatitis. Gynecol Endocrinol. 2016;32(Supl 2):37–40. doi: 10.1080/09513590.2016.1232780. [DOI] [PubMed] [Google Scholar]
- 10.Li K, Chen G, Hou H, Liao Q, Chen J, Bai H, et al. Analysis of sex hormones and menstruation in COVID-19 women of child-bearing age. Reprod Biomed Online. 2021;42:260–7. doi: 10.1016/j.rbmo.2020.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lebar V, Laganà AS, Chiantera V, Kunič T, Lukanović D. The effect of COVID-19 on the menstrual cycle:A systematic review. J Clin Med. 2022;11:3800. doi: 10.3390/jcm11133800. doi:10.3390/jcm11133800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nazir M, Asghar S, Rathore MA, Shahzad A, Shahid A, Khan AA, et al. Menstrual abnormalities after COVID-19 vaccines:A systematic review. Vacunas. 2022;23:S77–87. doi: 10.1016/j.vacun.2022.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Henarejos-Castillo I, Sebastian-Leon P, Devesa-Peiro A, Pellicer A, Diaz-Gimeno P. SARS-CoV-2 infection risk assessment in the endometrium:Viral infection-related gene expression across the menstrual cycle. Fertil Steril. 2020;114:223–32. doi: 10.1016/j.fertnstert.2020.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Muharam R, Agiananda F, Budiman YF, Harahap JS, Prabowo KA, Azyati M, et al. Menstrual cycle changes and mental health states of women hospitalized due to COVID-19. PLoS One. 2022;4:17–e0270658. doi: 10.1371/journal.pone.0270658. doi:10.1371/journal.pone.0270658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paces J, Strizova Z, Smrz D, Cerny J. COVID-19 and the immune system. Physiol Res. 2020;69:379–88. doi: 10.33549/physiolres.934492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. [[Last accessed on 2021 Jun 02]]. Available from: https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide .
- 17.Ozimek N, Velez K, Anvari H, Butler L, Goldman KN, Woitowich NC. Impact of stress on menstrual cyclicity during the coronavirus disease 2019 pandemic:A survey study. J Womens Health. 2022;31:84–90. doi: 10.1089/jwh.2021.0158. [DOI] [PubMed] [Google Scholar]


