ABSTRACT
India aims to provide universal health coverage to all individuals and communities thus ensuring accessibility, promotive, curative, preventive, rehabilitative, and palliative health services to all. Healthcare technologies play a critical role in ensuring eliminating healthcare disparities and encouraging quality healthcare at all levels. Technology solutions such as indigenous medical devices and diagnostic products, telemedicine, artificial intelligence, and drone technology can best integrate rural needs, improve health outcomes, patient safety, and healthcare quality and experience for patients’ values and strengths and can therefore be important contributors to advancing rural health equity. These technologies can transform India’s healthcare system by providing quality care and mitigating the risk of catastrophic financial hardship.
Keywords: Health equity, healthcare technology, out-of-pocket expenditure
Introduction
India focuses to achieve health equity by eliminating health disparities and attainment of universal health coverage. However, despite the advancement in the healthcare sector in India, access to quality healthcare remains a major obstacle due to geographical terrain or socioeconomic status, etc. The major challenges in attaining healthcare equity are suboptimal and inequitable resource allocation, accessibility of healthcare facilities, availability of skilled human resources, quality healthcare, out-of-pocket expenditure, etc.[1,2] In India, individuals with the greatest need for healthcare have the greatest difficulty in accessing healthcare services and are least likely to have their health needs met, and are highly vulnerable to catastrophic expenditure on health.[3-5]
The rising burden of diseases coupled with the coronavirus disease 2019 (COVID-19) pandemic has compounded health disparities in vulnerable and marginalized populations. India accounts for 17% of the world’s population and 20% of the global disease burden expressed as disability-adjusted life years (DALYs).[6] The country faces the dual burden of both communicable and noncommunicable diseases (NCDs).[7] The vide variations in health equity have a high impact on the out-of-pocket health expenditure in India.[8,9]
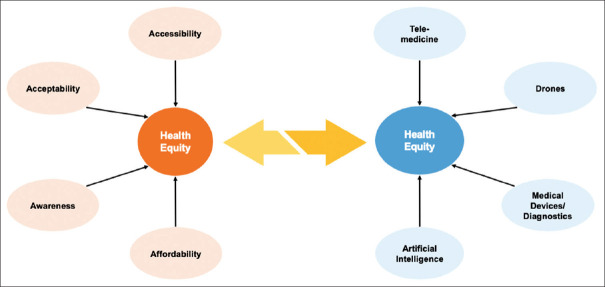
“Leaving no one behind” is the core principle of National Health Policy 2017. Availability, accessibility, affordability, and quality healthcare are the major barriers to attaining health equity. Modern healthcare technologies have enormous potential to reduce health disparities and improve human well-being in India. These advanced technologies have redefined the ways people, systems, and information interact in resource-constraints communities. The rapid proliferation of indigenous technology has strengthened the healthcare system, especially in screening, diagnosis, prognosis, availability, accessibility of advanced healthcare services, etc. The present article highlights how the use of modern healthcare technologies has helped in promoting accessibility and affordability thus achieving health equity in India. Technology solutions such as indigenous medical devices and diagnostic products, telemedicine, artificial intelligence (AI), and drone technology can best integrate rural needs, improve health outcomes, patient safety, and healthcare quality and experience for patients’ values and strengths and can therefore be important contributors to advancing rural health equity [Figure 1]. The healthcare innovations will aid in gathering and examining patient information and give primary care doctors knowledge of the patients’ medical requirements.
Figure 1.
Healthcare technologies such as indigenous medical devices and diagnostics products, telemedicine, artificial intelligence-based tools, and drones promote accessibility, affordability, availability, and awareness thus reducing healthcare disparities and improving human well-being in India
Indigenous medical devices and diagnostic products promoting health equity
India is among the top 20 markets for medical devices worldwide. The market is expected to increase at a 37% compound annual growth rate (CAGR) to reach US$ 50 billion in 2025, from ₹75,611 crore (US$ 10.36 billion) in 2020.[10] Currently, the Indian medical device market is driven by 75%–80% imports from countries such as the United States, China, and Germany. The high out-of-pocket expenditure is a major barrier to quality healthcare services and access to appropriate and affordable medicine. The Make-in-India, AtmaNirbhar Bharat (self-reliant India), Start-up India, and Production Linked Incentive (PLI) Scheme initiatives by the Government of India have promoted the development of low-cost indigenous medical devices and diagnostic products. Moreover, the Med-tech clusters being set up across the country have enhanced the production of medical devices and diagnostic products and also provided employment for local people.[11] These indigenously developed devices and diagnostic products are more adaptable and usable by diverse populations in diverse settings. Starting from prevention to diagnosis to treatment and rehabilitation, indigenous medical devices have not only decreased out-of-pocket expenditure but also promoted availability and accessibility to a greater extent.[12] With technological advancements, the role of medical devices has now expanded to improve the quality of care across all stages of healthcare including screening and diagnosis, treatment, rehabilitation, and monitoring. For example, the availability of highly sensitive and specific diagnostic products has helped in decreasing the incidence of carcinoma cervix among females. Also, a plethora of options are made available to patients and healthcare providers depending upon the clinical condition, socioeconomic condition of the patient, surgeon expertise, infrastructure available at the healthcare facility, etc. For example, in the case of cataract, the choice of surgery and a wide range of intraocular lenses are made available for both patient and the surgeon.[13]
An unprecedented rise of healthcare innovations due to its immense technological skills and medical know-how. Technologies such as mHealth, wearable devices, highly accurate, portable, and faster diagnostic/screening devices have helped in the early detection and management of NCDs such as cancer, hypertension, and diabetes and helped in decreasing DALYs and increasing quality-adjusted life years (QALYs).
The term “disability” is usually defined as the inability to perform normal life activities due to physical or mental condition. As per the National Family Health Survey-5, the total number of people with disability has already surpassed 2.7 million in India.[14] Although aging and disability are closely associated, health disparities remain unaddressed for this population subset. Assistive technologies are encouraging differently abled people to lead an independent life.[15]
Telemedicine and digital health tech for health equity
The causes of healthcare disparities are varied and multidimensional. The distribution of healthcare facility is skewed in India. A majority of healthcare facilities (and ~75% of doctors) are concentrated in the urban region, whereas 68.84% of the national population live in rural regions.[14,16] Accessibility to a healthcare facility remains a major hurdle. As of 2016, only 3.8% of patients with hypertension and diabetes have access to healthcare facilities.[17] Apart from arduous geographical terrain, accessibility challenges also include barriers such as language, hesitance, incapacitated elderly patients, or even socioeconomic inability. Healthcare disparities in India are primarily driven by three key factors: accessibility, affordability, and awareness. Telemedicine, which was considered futuristic medicine a few years ago has received an impetus to provide affordable and accessible quality healthcare, thereby ensuring holistic and equitable development in India. Mainly, during the COVID-19 pandemic, which had overwhelmed the already burdened healthcare system in the country. The COVID-19 pandemic has prompted healthcare providers, and the general public to take up telemedicine more seriously. Telemedicine has the ability to monitor health progress remotely by healthcare professionals, promote early disease diagnosis and intervention, and enhance self-management of chronic conditions.[18] Digital technology and telehealth have helped to address the disparities and provide quality healthcare services across the population. Self-monitoring wearable devices, electronic health records (EHRs), telemedicine, and telemonitoring have made real-time monitoring and interventions possible.[19]
Telemedicine has advanced significantly in terms of both healthcare delivery and technology. Telemedicine and home healthcare diagnostics platforms have been instrumental in expanding the coverage of quality healthcare, especially across marginalized and underserved populations across small towns and rural India. Telemedicine enables patients to access specialized services from hubs from nearby Health and Wellness Center (HWC) through the eSanjeevani portal, it has assisted in addressing the shortage of doctors and other healthcare professionals. Telemedicine has been implemented at HWCs (spokes) linked with doctors (hubs) and has become an integral part of the healthcare system, which has benefitted the rural patient by decreasing travel costs and out-of-pocket expenditures.
Artificial intelligence in reducing healthcare disparity
AI has radically revolutionized healthcare delivery and practice thus bridging the gap in health inequality. Advanced analytics and AI technology have greatly influenced primary care.[20] Examples include patient triaging, disease forecasting, and progression modeling,[21] population-based disease screening,[22] and also in decision support applications.[23] The data-intensive electronic medical records (EMRs), healthcare internet-of-things devices (including smartphone apps/wearable devices), and AI-based data analytics are driving decision-support systems and cost-effective therapeutic strategies.[20,23] The EMRs provide access to evidence-based tool in the healthcare provider that facilitates decision support.[23]
Timely and accurate delivery of medical supplies or transportation of patients to the healthcare facility is critical in achieving positive health outcomes. However, coordinating with transportation providers, healthcare facilities, or patients and assessing weather conditions, traffic patterns, best routes, and transport methods is a challenging task. AI has streamlined healthcare inventory management, medical transportation, managing complex medical logistics and patient transportation, and resource pooling among stakeholders.[24]
AI and blockchain have created systems for health-related data or EHRs, which are easily accessible and analyzed by medical professionals, insurance providers, etc. to receive timely updates on the services.[25] Real-time monitoring with full confidentiality visualizes and analyzes the end-to-end performance along with the entire supply chain mechanism.
AI-based tools and technologies not only help in forecasting or modeling but also in logistics or mobilization of resources or supply chain management in an efficient manner. These technologies also play an important role in disease screening and diagnostics in rural regions.[26]
Drone technology in hard-to-reach terrain
In the healthcare sector, timely delivery of medical supplies is the essence. Drones are known for their rapid, cost-effective, and safe delivery of goods even to hard-to-reach terrains compared with other air transportation systems. Drone operations are leapfrogging the last-mile logistics solution for transporting medical supplies in hard-to-reach terrains thus reducing urban-rural disparity. Drone with integrated portable devices, which offers two-way video and audio communications, are also being explored to provide basic life-saving support equipment and offer the opportunity to access remote or hard-to-reach areas.[27,28] Using drones to deliver medical supplies to remote/difficult-to-reach areas offers an innovative approach to addressing longstanding issues of healthcare availability and accessibility.
Conclusion and Way-Forward
The Sustainable Development Goals (SDGs) have set up the challenging task of reducing morbidity and improving health condition through a number of targets. Healthcare technology is a vast sector, ranging from surgical implants to diagnostics kits to medical software. Point-of-care diagnostics, mHealth will facilitate remote diagnosis and treatment of patients in hard-to-reach areas, especially in delivering better primary care services. These technological solution aims to provide accessible, affordable, and quality healthcare services to the underprivileged. The country requires cost-effective population-specific technology solutions to cater to the aging population, rising communicable, and NCDs, and a vast underprivileged population. Countries with similar contexts and settings as India may learn from the country’s approach toward strengthening comprehensive primary healthcare and citizen-centric approach; establishing linkages with secondary and tertiary care services through the Ayushman Bharat Scheme, EHR; the continuum of care through teleconsultations; and how India has designed several reforms in healthcare system toward its journey to attain Universal Health Coverage.
New Knowledge
The healthcare system can be strengthened by the use of low-cost indigenous med-tech solutions particularly for screening, diagnosis, and even prognosis. AI and telemedicine would be crucial components of medicine in the future. Thus, it is crucial to train the new generation of healthcare providers (including medical students/nurses and paramedical staff) in the applications and implementation of AI-based tools. Furthermore, although drone technology can strengthen the medical logistics system, healthcare workers training at the spokes (PHC/SHC) is required for sample packaging and removing the supplies from the drone.
Key points
Healthcare technologies have the potential to reduce health disparities and improve human well-being in India.
mHealth, wearable devices, and point-of-care diagnostics can aid in the early detection and management of diseases.
Primary care providers may make early diagnoses and manage baseline conditions with the use of telemedicine and AI-based techniques.
Key message
Technology solutions can make a significant impact in rural healthcare setting. It can improve health outcomes and reduce out-of-pocket expenditure ensuring accessibility, affordability, and health equity thus leading to universal health coverage.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Balarajan Y, Selvaraj S, Subramanian SV. Health care and equity in India. Lancet. 2011;377:505–15. doi: 10.1016/S0140-6736(10)61894-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Banerjee S, Roy Chowdhury I. Inequities in curative health-care utilization among the adult population (20-59 years) in India:A comparative analysis of NSS 71st (2014) and 75th (2017-18) rounds. PLoS One. 2020;15:e0241994. doi: 10.1371/journal.pone.0241994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh CH, Ladusingh L. Correlates of inpatient healthcare seeking behavior in India. Indian J Public Health. 2009;53:6–12. [PubMed] [Google Scholar]
- 4.Panda BK, Kumar G, Awasthi A. District level inequality in reproductive, maternal, neonatal and child health coverage in India. BMC Public Health. 2020;20:58. doi: 10.1186/s12889-020-8151-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Government of India. National Health Accounts:2014-15. [[Last accessed on 2018 Jun 25]]. Available from: https://www.mohfw.gov.in/sites/default/files/National%20Health%20Accounts%20Estimates%20Report%202014-15.pdf .
- 6.Country Cooperation Strategy at a Glance, World Health Organization. Available from: https://apps.who.int/iris/bitstream/handle/10665/136895/ccsbrief_ind_en.pdf?sequence=1&isAllowed=y .
- 7.Boutayeb A. The double burden of communicable &non-communicable diseases in developing countries. Trans R Soc Trop Med Hyg. 2006;100:191–9. doi: 10.1016/j.trstmh.2005.07.021. [DOI] [PubMed] [Google Scholar]
- 8.Chowdhury S, Gupta I, Trivedi M, Prinja S. Inequity and burden of out-of-pocket health spending:District level evidences from India. Indian J Med Res. 2018;148:180–9. doi: 10.4103/ijmr.IJMR_90_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dhankhar A, Kumari R, Bahurupi YA. Out-of-pocket, catastrophic health expenditure and distress financing on non-communicable diseases in India:A systematic review with meta-analysis. Asian Pac J Cancer Prev. 2021;22:671–80. doi: 10.31557/APJCP.2021.22.3.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. [[Last accessed on 2022 Jun 24]]. Available from: https://www.ibef.org/industry/medical-devices .
- 11.Dang A, Sharma JK. Economics of medical devices in India. Value Health Reg Issues. 2019;18:14–7. doi: 10.1016/j.vhri.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 12.Rout SK, Sahu KS, Swain S, Pati S. Out of pocket expenditure on surgical and nonsurgical conditions in Odisha. J Family Med Prim Care. 2016;5:367–72. doi: 10.4103/2249-4863.192377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Intraoccular lens for cataract surgery. [[Last accessed on 2023 Feb 18]]. Available from: https://htain.icmr.org.in/images/pdf/1_IOL_Policy_Brief.pdf .
- 14.International Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-5), 2019-21:India. Mumbai: IIPS; 2022. [Google Scholar]
- 15.Kheria M, Mishra SN. Role of assistive technology in empowering differently abled people. IOSR-JHSS. 2020;25:1–6. [Google Scholar]
- 16.Garg S, Singh R, Grover M. India's health workforce:Current status and the way forward. Natl Med J India. 2012;25:111–3. [PubMed] [Google Scholar]
- 17.National Sample Survey Office. Health in India. New Delhi: Ministry of Statistics and Programme Implementation; 2016. [Google Scholar]
- 18.Yin Y, Zeng Y, Chen X, Fan Y. The internet of things in healthcare:An overview. J Ind Inf Integration. 2016;1:3–13. [Google Scholar]
- 19.Ganapathy K. Telemedicine and neurosciences. Neurol India. 2018;66:642–51. doi: 10.4103/0028-3886.232346. [DOI] [PubMed] [Google Scholar]
- 20.Lin SY, Mahoney MR, Sinsky CA. Ten ways artificial intelligence will transform primary care. J Gen Intern Med. 2019;34:1626–30. doi: 10.1007/s11606-019-05035-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang B, Gao Z, Lin Z, Wang R. A disease-prediction protocol integrating triage priority and BERT-based transfer learning for intelligent triage. Bioengineering (Basel) 2023;10:420. doi: 10.3390/bioengineering10040420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davalagi SB, Palicheralu B, Murthy SSN, Hurlihal S. Acceptance of artificial intelligence (AI)-based screening for breast health in urban slums of central Karnataka, India –SWOC analysis. J Family Med Prim Care. 2022;11:6023–8. doi: 10.4103/jfmpc.jfmpc_143_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spanig S, Emberger-Klein A, Sowa JP, Canbay A, Menrad K, Heider D. The virtual doctor:An interactive clinical-decision-support system based on deep learning for non-invasive prediction of diabetes. Artif Intell Med. 2019;100:101706. doi: 10.1016/j.artmed.2019.101706. [DOI] [PubMed] [Google Scholar]
- 24.Kumar A, Mani V, Jain V, Gupta H, Venkatesh VG. Managing healthcare supply chain through artificial intelligence (AI):A study of critical success factors. Comput Ind Eng. 2023;175:108815. doi: 10.1016/j.cie.2022.108815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hang L, Choi E, Kim DH. A novel EMR integrity management based on a medical blockchain platform in hospital. Electronics. 2019;8:467. [Google Scholar]
- 26.Thomasian NM, Eickhoff C, Adashi EY. Advancing health equity with artificial intelligence. J Public Health Policy. 2021;42:602–11. doi: 10.1057/s41271-021-00319-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nedelea PL, Popa TO, Manolescu E, Bouros C, Grigorasi G, Andritoi D, et al. Telemedicine system applicability using drones in pandemic emergency medical situations. Electronics. 2022;11:2160. [Google Scholar]
- 28.Flemons K, Baylis B, Khan AZ, Kirkpatrick AW, Whitehead K, Moeini S, et al. The use of drones for the delivery of diagnostic test kits and medical supplies to remote First Nations communities during Covid-19. Am J Infect Control. 2022;50:849–56. doi: 10.1016/j.ajic.2022.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]