Abstract
Background
Telerehabilitation can be an appropriate alternative to face-to-face rehabilitation for adults; however, it is uncertain whether it is safe and effective for older adults.
Objective
This review aimed to determine the effect of physiotherapist-led, exercise-based telerehabilitation for older adults on patient outcomes (health-related quality of life, activity limitation, functional impairment) and health service costs.
Methods
Randomised or non-randomised controlled trials including community-dwelling older adults (mean age ≥ 65 years) who received exercise-based telerehabilitation led by a physiotherapist were eligible. Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medline, PubMed and Cochrane Library were searched from the earliest available date to August 2022. Methodological quality was assessed using the Physiotherapy Evidence Database scale. Data were synthesised with inverse variance, random-effects meta-analyses to determine standardised mean differences and 95% confidence intervals. Certainty of evidence was determined by applying Grading of Recommendations, Assessment, Development and Evaluation criteria.
Results
Eleven studies (10 randomised) with 1,400 participants (mean age 65–74 years) experiencing musculoskeletal and cardiopulmonary conditions were included. Telerehabilitation was safe, effective and well adhered to. Telerehabilitation was non-inferior to face-to-face physiotherapy in relation to range of movement, strength, 6-min walk distance (6MWD), timed up and go test (TUGT) and quality of life and had lower health-care costs compared with face-to-face physiotherapy. Compared with no intervention, telerehabilitation participants had significantly better range of motion, strength, quality of life, 6MWD and TUGT speed.
Conclusion
Physiotherapist-led, exercise-based telerehabilitation is non-inferior to face-to-face rehabilitation and better than no intervention for older adults with musculoskeletal and cardiopulmonary conditions.
Keywords: telerehabilitation, rehabilitation, older adults, physical therapy, exercise, systematic review, older people
Key Points
Physiotherapist-supervised, exercise-based telerehabilitation for older adults is safe.
Supervised, exercise-based telerehabilitation is non-inferior to face-to-face rehabilitation for improving patient outcomes.
Telerehabilitation may cost less than face-to-face rehabilitation.
Telerehabilitation significantly improves patient outcomes compared with no intervention.
Introduction
Regular exercise is important for achieving healthy active ageing [1] and is an effective component of physiotherapy interventions for people with musculoskeletal, neurological and cardiopulmonary health conditions [2]. However, older adults may experience barriers to accessing exercise programmes because of poor health and mobility, as well as environmental constraints such as proximity to health and fitness centres [3, 4]. Telerehabilitation may be a suitable alternative to face-to-face rehabilitation for exercise in older adults who face these challenges. During the coronavirus disease of 2019 pandemic, physiotherapists in outpatient and community settings had to rapidly transition away from face-to-face service delivery and exercise programmes to telerehabilitation [5]. However, it is unknown if exercise-based telerehabilitation provided via synchronous videoconferencing is as effective as traditional physiotherapy for older adults.
Telerehabilitation may include a range of interventions (therapeutic exercise, assessment and monitoring, functional training and education), provided via webpages, instant messaging services, telephone calls or videoconference, which may be delivered either synchronously (i.e. in real time) or asynchronously. A rapid review of 53 systematic reviews on different modalities of telerehabilitation in physiotherapy found that it was comparable to face-to-face rehabilitation for adults with various conditions [6]. Only three of the included reviews were limited to synchronous interventions and only two focussed on older adults (both in total knee arthroplasty (TKA) populations) [6]. No previous reviews have focussed on exercise-based telerehabilitation provided via synchronous videoconferencing for older adults with a variety of health conditions.
Older adults are less likely to use technology for health purposes compared with younger cohorts because of barriers such as lower levels of education and income, accessibility, usability, training and technical support, and issues around privacy and data management [7]. It may be particularly difficult to deliver exercise-based rehabilitation online as close supervision is required to ensure correct set-up and performance of exercises for safety and efficacy, particularly for older adults who may experience greater health complexity [8]. Therefore, it may be more difficult for older adults to benefit from exercise interventions if they are delivered via telerehabilitation. Although necessary during the pandemic, the continued availability of telerehabilitation may have benefits for older adults in terms of access for those living far from physiotherapy clinics, or with inadequate transport, as well as those who may be immunocompromised. Telerehabilitation may also be a cost-effective alternative to centre-based and home-based physiotherapies [9, 10]. With an ageing population and a growing demand for physiotherapy in the community, health services must ensure that physiotherapy is delivered in a safe, effective and sustainable manner.
This systematic review aimed to determine the effectiveness of physiotherapist-led, exercise-based telerehabilitation for older adults compared with usual physiotherapy care in terms of patient and health service outcomes.
Methods
Protocol and registration
This systematic review and meta-analysis was reported with reference to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [11] and was prospectively registered in the PROSPERO database of systematic reviews (registration ID: CRD42022352899).
Eligibility criteria
To be eligible for inclusion, studies had to be randomised (RCT) or non-randomised controlled trials (non-RCT) that included community-dwelling older adults (mean age ≥ 65 years) who received exercise-based telerehabilitation led by a physiotherapist in a group or individual format compared with usual care (either face-to-face or no intervention). For the purpose of this systematic review, telerehabilitation was defined as synchronous videoconferencing between a physiotherapist and their patient/s. All conditions treated with exercise-based physiotherapy were included. Studies were included if they measured patient (participation, activity or impairment) and/or health service outcomes (e.g. cost).
Studies were excluded if the telerehabilitation was not delivered by a physiotherapist, if there was only one physiotherapy consultation or the physiotherapy intervention was an assessment only. Interventions delivered only via telephone, an application, virtual reality or virtual rehabilitation systems, or gaming devices, or where monitoring was the only intervention were excluded.
Information sources
Electronic databases Cumulative Index to Nursing and Allied Health Literature (CINAHL) Complete, OVID Medline, PubMed and Cochrane Library were searched from the earliest available date to August 2 2022. Using the population, intervention, comparison, outcome format, the search strategy focussed on the ‘intervention’ component as we were interested in multiple populations, comparisons and outcomes. Therefore, search terms and synonyms for the key elements of the intervention (i.e. exercise, physiotherapy and telerehabilitation) were developed. Terms within a component were searched with the OR operator and categories were combined with the AND operator (Supplementary Appendix 1). We also searched reference lists of included papers for additional articles.
Study selection
Search results were exported into Covidence and duplicates were removed. Two reviewers (M.W. and C.L.P.) independently screened the remaining articles by title and abstract using the predefined eligibility criteria. Articles that did not meet the eligibility criteria were excluded, and the full text articles of those remaining were examined in further detail. The two reviewers independently reapplied the eligibility criteria, using discussion to reach a consensus where required. If consensus could not be reached, a third reviewer was consulted (A.M.D.). Reviewer responses were recorded and agreement between reviewers calculated using the kappa statistic (κ), with a κ of 0.21–0.40 indicating fair agreement, 0.41–0.60 moderate agreement, 0.61–0.80 substantial agreement and 0.81–0.99 almost perfect agreement [12].
Data collection process
Excel spreadsheets were developed and used to extract data on participant characteristics (age, clinical diagnosis and education status), intervention details (type, delivery and dose), outcomes related to the World Health Organisation—International Classification of Functioning, Disability and Health categories of participation, activity and impairment [13], and results (patient and health service). One reviewer (M.W.) extracted data and a second reviewer (A.M.D.) checked extracted data for accuracy.
Risk of bias in individual studies
All studies were independently appraised for methodological quality and risk of bias by two reviewers (M.W. and C.L.P.) using the Physiotherapy Evidence Database (PEDro) scale. The PEDro scale is an 11-item scale with 10 items scored for internal validity. It has been shown to be a valid measure of the methodological quality of clinical trials [14], with a score of 6 or more out of 10 considered high-quality.
Summary measures and synthesis of results
Where there were sufficient data, post-intervention means and standard deviations (SD) from RCT were pooled in meta-analyses using random-effects models and inverse variance methods using Hedges’ g in RevMan 5. Mean differences (MD) and 95% confidence intervals (CIs) were calculated when outcomes were presented in the same unit of measurement and standardised mean differences (SMD) and 95% CIs were calculated when outcomes were similar but presented in different units. A SMD of 0.2 was considered a small effect, 0.5 a moderate effect and 0.8 a large effect [15]. We hypothesised that telerehabilitation would be non-inferior to face-to-face rehabilitation and specified that telerehabilitation would be considered non-inferior if the lower band of the SMD CI was no < −0.20 or if the upper band was no > +0.2 (depending on the direction of the outcome) indicating a small effect [15]. Inconsistency was assessed using the I2 statistic with an I2 > 50% suggesting significant statistical heterogeneity [16]. Trials were pooled based on outcome measures (e.g. pain) and control group conditions (e.g. face-to-face rehabilitation or no intervention). Data from non-RCT were not included in meta-analyses but were described narratively.
Risk of bias across studies
The Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach was used to determine the certainty of evidence for each meta-analysis conducted in this review [17]. The GRADE approach involved downgrading the certainty of evidence from ‘high’ to ‘moderate’, ‘low’ and ‘very low’ each time the following criteria applied: (i) the PEDro score was <6 for the majority of trials included in the meta-analysis (risk of bias), (ii) there were high levels of statistical heterogeneity between trials (I2 ≥ 50%) (inconsistency), (iii) there was evidence of indirect comparisons between populations, interventions or outcomes (indirectness), (iv) there were large CIs (>0.80 for SMD or more than the minimal clinically important difference for MD) (imprecision) and (v) there was funnel plot asymmetry if ≥10 trials were included in the meta-analysis (publication bias).
Results
Study selection
The database search identified 584 records, and one further record was found through manual searching of reference lists. After removal of duplicates, 388 records were screened by title and abstract. Agreement between reviewers was substantial when screening titles and abstracts (κ = 0.66, 95% CI 0.55–0.77). A total of 56 full-text articles were then assessed against the eligibility criteria, with 14 articles meeting inclusion [18–31] (Figure 1). Agreement between reviewers at full text review was almost perfect (κ = 0.85, 95% CI 0.69–1.0). The 14 included studies reported data from 10 RCT and one non-RCT [21] (Table 1). Five studies reported results from two trials; therefore, throughout the review, we will refer to the main trial papers [23, 25] when referring to study results.
Figure 1.
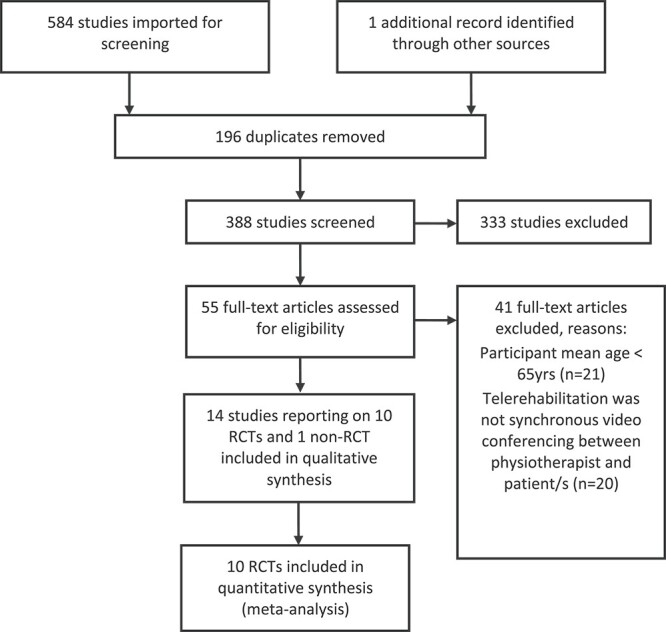
Flow of trials through the review
Table 1.
Trial characteristics
| Study (country) |
Clinical diagnosis | PEDro score | Participants (intervention: control) | Male:Female (intervention/control)% | Mean age (SD) (intervention: control) |
Outcomes | Timing of outcomes |
|---|---|---|---|---|---|---|---|
| An 2021 [18] (Korea) | Bilateral TKA | 7 | Telerabiltation:20 Education:20 Control:20 |
0:100/0:100/ 0:100 |
71(3):70(2):70(3) | Patient: Quadriceps muscle strength, WOMAC—(pain, stiffness, function and total score), ROM, pain and TUG | Baseline (4 weeks pre-op) 1 day pre-op 6 weeks post-op |
| Bennell 2020 [19] (Australia) | Knee OA | 7 | Telerehabilitation physiotherapy:172 telerehabilitation physiotherapy and dietetics: 175 Control: 67 |
49:51 33:67 46:54/ |
65(8):64(8):65(9) | Patient: Pain (NRS), WOMAC—physical function subscale, Incidental and Planned Exercise, QoL | Baseline 6 months 12 months |
| Bettger 2020 [20] (USA) | TKA | 6 | 143: 144 | 40:60/ 35:65 |
65(7):65(9) | Patient: KOOS, ROM, gait speed, falls, pain Health service: costs, hospital readmissions |
Baseline 6 weeks 12 weeks |
| Eriksson 2009 [21] (Sweden) | Shoulder hemiarthroplasty | 5 | 10:12 | 20:80/ 25:75 |
70(53–95):73(50–86)a | Patient: Pain (VAS), ROM, shoulder function ability (Constant score and SRQ-S) and QoL (SF-36). | Baseline 1 week pre-op 8 weeks post-op |
| Godtfredsen 2020 [22] and Hansen 2020 [23] (Denmark) | Severe COPD | 7 | 67:67 | 45:55/ 45:55 |
68(9):68(9) | Patient: 6MWD, CAT, HADS, EQ-5D, 30s STS, CCQ, steps p/day and sedentary/active time Health Service: hospital admission and mortality |
Baseline 10 weeks 22 weeks |
| Hwang 2017 [24] (Australia) | CHF | 8 | 24:29 | 79:21/ 72:28 |
68(14):67(11) | Patient: 6MWD, 10MWT, strength, TUGT, FR, static standing, step test, QoL, satisfaction, attendance rates and adverse events | Baseline 12 weeks 24 weeks |
| Moffet 2015 [25] and Tousignant 2015 [30] and Moffet 2017 [26] (Canada) | TKA | 6 | 104:101 | 42:58/ 55:45 |
65(8):67(8) | Patient: WOMAC (pain, stiffness, function and total score), KOOS, 6MWT, timed stair test, strength, ROM, HSQC satisfaction survey, Health Service: cost analysis |
Baseline 2 months 4 months |
(Continued)
Table 1.
Continued
| Study (country) |
Clinical diagnosis | PEDro score | Participants (intervention: control) | Male:Female (intervention/control)% | Mean age (SD) (intervention: control) |
Outcomes | Timing of outcomes |
|---|---|---|---|---|---|---|---|
| Peng 2018 [27] (China) | HF | 6 | 49:49 | 57:43/ 61:39 |
66(11) | Patient: QoL (Minnesota Living with Heart Failure Questionnaire), 6MWD, HADS | Baseline 2 months 4 months |
| Russell 2011 [28] (Australia) | TKA | 8 | 34:31 | Not reported | 66(8):70(7) | Patient: WOMAC (Pain, stiffness, function and global scores), Patient-Specific Functional Scale, TUGT, VAS, ROM, strength, gait, QoL (Spitzer Quality of Life Uniscale) | Baseline 6 weeks |
| Tousignant 2011 [29] (Canada) Tsai 2017 [31] (Australia) |
TKA COPD |
5 8 |
24:24 20:17 |
Not reported 63:37/ 35:65 |
66(10):66(13) 73(8):75(9) |
Patient: ROM, Berg balance scale, 30s STS, WOMAC (total score), TUGT, Tinetti, Functional Autonomy Measurement, QoL (SF-36) Patient: FEV1, FVC, 6MWT, incremental shuttle walk test, endurance shuttle walk test, QoL (Chronic Respiratory Disease Questionnaire), physical activity levels |
Baseline 2 months 4 months Baseline 8 weeks |
Abbreviations: WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index; TUG, timed up-and-go; KOOS, Knee Injury and Osteoarthritis Score; SRQ-S, Shoulder Rating Questionnaire—Sweden; SF-36, health-related quality of life scale—36-Item Short Form Survey; CAT, COPD Assessment Test; HADS, Hospital Anxiety and Depression Scale; EQ-5D, EuroQol-5 Dimension; 30s STS, 30-s sit-to-stand; CCQ, Clinical COPD Questionnaire; 10MWT, 10-m walk test; FR, Functional Reach; HSQC, Health Care Satisfaction Questionnaire; LVEF, left ventricular ejection fraction; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity.
a SD for age data not presented, range reported instead.
Study characteristics
A total of 1,400 participants were included in this review. The mean age of participants ranged from 65 to 74 years. Trials included mostly females (Table 1). Most interventions targeted people with musculoskeletal conditions including TKA [18, 20, 25, 28, 29], knee osteoarthritis [19] and total shoulder arthroplasty [21]. Two trials investigated telerehabilitation in chronic obstructive pulmonary disease [23, 31], and two in heart failure [24, 27] (Table 1). In two trials, most participants (64%) reported they were very comfortable using technology at baseline [20, 31].
In eight trials, exercise-based physiotherapy delivered via synchronous videoconferencing was delivered 1:1 [18–21, 25, 27–29]. In three trials, physiotherapy was delivered in an online group setting [23, 24, 31] with two of these trials specifying up to four participants per group [24, 31]. Physiotherapist-supervised exercise sessions varied from 20 to 60-min duration, and were delivered between three times per week to once per month for between 3 and 26 weeks (Table 2). The seven trials including participants with musculoskeletal conditions mostly focussed on range of motion (ROM) and progressive, muscle strengthening, whereas the four trials for participants with cardiopulmonary conditions included aerobic and strengthening exercises (Table 2).
Table 2.
Description of intervention characteristics
| Study | Intervention (delivered by) | Duration and frequency of sessions | Exercise component | Equipment required | Comparison |
|---|---|---|---|---|---|
| An 2021 [18] (Korea) | 1:1 synchronous videoconferencing (physiotherapist) |
30 min/session, 2 times/day, 5 days/week |
Supervised exercise: warm-up, mobility, flexibility, strength, balance and cool-down exercises | Smartphone or tablet | Control 1—usual care: assessment and knee exercises Control 2—Preoperative patient education and home exercise programme |
| Bennell 2020 [19] (Australia) | 1:1 synchronous videoconferencing (physiotherapist ± dietitian) |
Physiotherapist only intervention: 6 × 20–45-min consults over 6 months Physiotherapist and dietitian intervention: 6 × physiotherapy consultations + 6 × dietetics consultations, 20–45-min consultations over 6 months |
Individualised management plan with progressive, muscle-strengthening, home exercise programme, physical activity plan, self-management strategies | Smart device, educational booklets, resistance bands, Fitbit | Electronic osteoarthritis information |
| Bettger 2020 [20] (USA) | 1:1 synchronous videoconferencing (physiotherapist) |
Weekly, 12 weeks with physiotherapist and unrestricted access to electronically programmed individualised prescribed physiotherapy regimen | Individualised exercise programme with review of progress and revision of therapy programme | Cloud-based virtual telehealth system with 3D tracking technology, an avatar and video connection for synchronous telehealth consult. | Traditional face-to-face home- or centre-based physiotherapy. |
| Eriksson 2009 [21] (Sweden) | 1:1 synchronous videoconferencing (physiotherapist) |
Weekly, 8 weeks | Individualised exercise programme | Standard commercial videoconferencing unit. | Traditional face-to-face physiotherapy at local treatment centre |
| Godtfredsen 2020 [22] and Hansen 2020 [23] (Denmark) | Group synchronous videoconferencing (physiotherapist) |
60 min/session, 3 days/week, 10 weeks (including 5-min rest and 20-min education). Weekly exercise volume = 105 min) | Supervised group exercise: warm up, high repetitive time-based muscle endurance training. | Videoconference software system installed on a single touch screen | Conventional outpatient hospital face-to-face pulmonary rehabilitation (90 min/session, 2 days/week, 10 weeks). Weekly exercise volume = 120 min |
| Hwang 2017 [24] (Australia) | Group synchronous videoconferencing (up to 4 participants) (physiotherapist) |
60 min/session, 2 days/week, 12 weeks | Supervised group exercise: 10-min warm-up, 40 min of aerobic and strength exercises and a 10-min cool-down. | videoconference software, laptop, mobile broadband device 3G, automatic sphygmomanometer, finger pulse oximeter, free weights, resistance bands |
Centre-based face-to-face rehabilitation programme including education, aerobic and strength training exercise (physiotherapist). 60 min/session, 2 days/week, 12 weeks |
(Continued)
Table 2.
Continued
| Study | Intervention (delivered by) | Duration and frequency of sessions | Exercise component | Equipment required | Comparison |
|---|---|---|---|---|---|
| Moffet 2015 [25] and Tousignant 2015 [30] and Moffet 2017 [26] (Canada) | 1:1 synchronous videoconferencing (physiotherapist) |
45–60 min/session, 2 days/week, 8 weeks | Supervised exercise: mobility, strengthening, gait and transfer training, and balance | Videoconferencing equipment | Face-to-face physiotherapy home visits, 45–60 min/session, 2 days/week, 8 weeks |
| Peng 2018 [27] (China) | 1:1 synchronous videoconferencing (physiotherapist) |
8 weeks, 32 ex sessions. Weeks 1–4: 3 × 20 min (aerobic exercise), Weeks 5–8: 5 × 30 (resistance training). |
Aerobic and resistance training | Videoconferencing equipment, instant messaging (QQ and WeChat software), resistance band | Usual care: simple discharge education and regular follow-up visits at clinic. No exercise instruction. |
| Russell 2011 [28] (Australia) | 1:1 synchronous videoconferencing (physiotherapist) |
45 min/session, 1 day/week, 6 weeks | Individual supervised exercise and education |
Videoconferencing equipment | Outpatient face-to-face physiotherapy, 45 min/session, 1 day/week, 6 weeks |
| Tousignant 2011 [29] (Canada) Tsai 2017 [31] (Australia) |
1:1 synchronous videoconferencing (physiotherapist) Group synchronous videoconferencing (up to four participants) (physiotherapist) |
60 min/session, 2 days/week, 2 months 45–55 min/session, 3 days/week, 8 weeks |
Progressive exercises Supervised group exercise: cycling, walking, strengthening |
Videoconferencing equipment Videoconferencing equipment, finger pulse oximeter, lower limb cycle ergometer |
Face-to-face home care/outpatients for 2 months Usual care medical management without exercise training. |
Abbreviations: VERA, Virtual Exercise Rehabilitation Assistant; QQ, instant messaging software service.
Control group conditions included face-to-face home [20, 21, 25, 29] or clinic-based [22–24, 28] physiotherapy, or usual care and advice only without supervised exercise training from a physiotherapist [18, 19, 27, 31].
Risk of bias within studies
The median PEDro score was 7 (range 5–8). Nine of the 11 studies were rated as high quality (Table 1). In 10 trials, allocation was random, and nine trials had concealed allocation. Seven of the 11 trials had blinded assessors. Intention to treat analysis was conducted in eight trials (Supplementary Appendix 2).
Adherence
Three trials reported higher attendance in the telerehabilitation groups compared with face-to-face rehabilitation [20, 23, 24]. Another two trials reported no between group difference in compliance with the exercise programme [27, 28]. In one trial, two participants in the telerehabilitation group discontinued because of the high intensity of the exercise programme [18].
Adverse events
Six trials reported no differences between the control and intervention groups in adverse events [19, 23–25] or falls [18, 20]. In one trial, 24 technical issues (12%) related to the use of technology (e.g. poor internet connection) were reported [31].
Effect of telerehabilitation on patient outcomes
Participation restriction
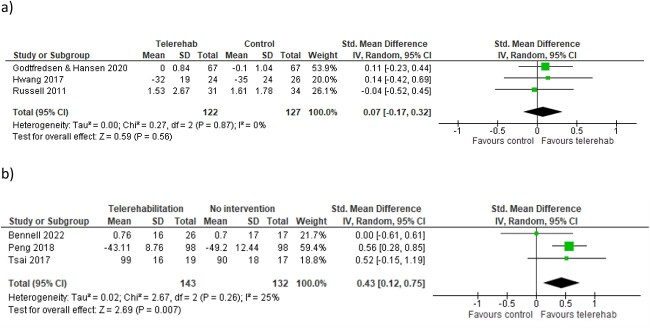
There was moderate certainty evidence from three trials with 249 participants [23, 24, 28] that telerehabilitation was non-inferior to face-to-face rehabilitation for quality of life (SMD 0.07, 95% CI −0.17 to 0.32, I2 0%) in older adults post-knee arthroplasty or in cardiopulmonary rehabilitation (Figure 2 and Table 3).
Figure 2.
SMD (95% CI) for effect of telerehabilitation on quality of life when compared with: (a) face-to-face rehabilitation (three trials, n = 249) and (b) no intervention (three trials, n = 275)
Table 3.
Meta-analysis, effect of telerehabilitation compared with usual care (no intervention or face-to face intervention)
| Outcome | Comparison group | Assessment period | Trial (n) | Participants (n) | MD (95% CI, I2) | SMD (95% CI, I2) | Certainty of evidence (GRADE) |
|---|---|---|---|---|---|---|---|
| Participation restriction | |||||||
| Quality of life | Face-to-face | Post-intervention | 3[23, 24, 28] | 249 | 0.07 [−0.07 to 0.32], 0% | Moderatea | |
| No intervention | Post-intervention | 3[19, 27, 31] | 275 | 0.43 (0.12–0.75), 25% | Moderatea | ||
| Activity limitation | |||||||
| 6MWD | Face-to-face | Post-intervention | 2[24, 25] | 248 | 1.01 [−33.83 to 35.85], 41% | Moderatea | |
| No intervention | Post-intervention | 2[27, 31] | 232 | 12.71 [9.58 to 15.84], 0% | Moderatea | ||
| TUGT | Face-to-face | Post-intervention | 2[24, 28] | 115 | −1.67 [−4.53 to 1.2], 25% | Lowb | |
| Functional impairment | |||||||
| Pain | Face-to-face | Post-intervention | 2 [20, 28] | 369 | 0.09 [−0.22 to 0.41], 39% | High | |
| No intervention | Post-intervention | 2 [18, 19] | 66 | −0.06 (−0.77 to 0.65), 51% | Lowc | ||
| ROM (knee flexion) | Face-to-face | Post-intervention | 3[20, 25, 28] | 567 | 0.09 [−0.11 to 0.28], 22% | High | |
| Strength (knee extensor) | Face-to-face | Post-intervention | 3[24, 25, 28] | 313 | 0.20 [−0.09 to 0.49], 31% | Moderatea | |
| Costs | |||||||
| Health Service Costs | Face-to-face | Post-intervention | 2 [20, 30] | 484 | −0.69 [−0.88 to −0.51], 0% | Moderated | |
GRADE, Grading of Recommendations, Assessment, Development and Evaluation working group approach (see reason for downgrade).
aReason for downgrade: indirectness.
bReason for downgrade: indirectness, imprecision.
cReason for downgrade: inconsistency, imprecision.
dReason for downgrade: risk of bias.
When compared with no intervention, there was moderate certainty evidence from three trials with 275 participants that older adults with musculoskeletal and cardiopulmonary conditions who participated in telerehabilitation had moderately higher quality of life (SMD 0.43, 95% CI 0.12–0.75, I2 25%).
Activity limitation
Six-min walk distance
There was moderate certainty evidence that telerehabilitation was non-inferior to face-to-face rehabilitation in two trials with 248 participants with musculoskeletal and cardiopulmonary conditions on the 6MWD (MD 1.01 metres, 95% CI −33.83 to 35.85, I2 41%) (Table 3 and Supplementary Appendix 3). When compared with no intervention, there was moderate certainty evidence from 232 participants in two trials that telerehabilitation increased 6MWD by MD 12.71 m (95% CI 9.58–15.84, I2 = 0%) (Table 3 and Supplementary Appendix 3).
Timed up and go test
There was low certainty evidence from two trials with 115 participants with musculoskeletal and cardiopulmonary conditions that telerehabilitation was non-inferior to face-to-face rehabilitation in terms of the timed up and go test (TUGT; MD −1.67 s, 95% CI −4.53 to 1.2, I2 25%) (Table 3 and Supplementary Appendix 3).
Compared with no intervention, one trial reported that participants of telerehabilitation were significantly faster in the TUGT (MD −2.73 s, 95% CI −3.87 to −1.59) compared with participants who did not receive intervention [18].
Functional impairment
Pain
Five trials measured pain using various outcome measures including the numeric rating scale (NRS) [19], visual analogue scale (VAS) [21, 28], pressure pain threshold [18] and a 0–10 point score [20].
There was high certainty evidence from two trials with 369 participants post-knee arthroplasty that telerehabilitation was inferior to face-to-face rehabilitation for pain (SMD 0.09, 95% CI −0.22 to 0.41, I2 39%) (Table 3 and Supplementary Appendix 3). When compared with no intervention, there was low certainty evidence from two trials with 66 participants post-knee arthroplasty of no difference in pain (SMD −0.06, 95% CI −0.77 to 0.65, I2 51%) (Table 3 and Supplementary Appendix 3).
In one study, not included in meta-analysis as it was not a RCT [21], participants post-shoulder hemiarthroplasty who received telerehabilitation reported significantly less pain compared with those who received face-to-face physiotherapy (P = 0.002).
Range of motion
There was high certainty evidence from three trials with 567 participants post-knee arthroplasty that telerehabilitation was non-inferior to face-to-face rehabilitation for improving knee flexion ROM (SMD 0.09, 95% CI −0.11 to 0.28, I2 22%) (Table 3 and Supplementary Appendix 3).
In one study [21], not included in meta-analysis as it was not a RCT, participants post-shoulder hemiarthroplasty who received telerehabilitation had greater shoulder flexion ROM compared with participants who received face-to-face rehabilitation (P = 0.002) [21].
Compared with no intervention, one trial reported that participants who received telerehabilitation had significantly greater knee flexion ROM post-intervention (MD 7.23 degrees, 95% CI 1.69–12.77) [18].
Strength
There was moderate certainty evidence from three trials [24, 25, 28] with 313 participants that telerehabilitation was non-inferior to face-to-face rehabilitation for quadriceps strength (SMD 0.20, 95% CI −0.09 to 0.49, I2 31%) (Table 3 and Supplementary Appendix 3) [24].
Compared with no intervention, participants in one study who received telerehabilitation prior to TKA had significantly greater quadriceps strength (MD 15.13 N-m, 95% CI 6.64–23.62) [18].
Long-term effect of telerehabilitation on patient outcomes
Three of the trials assessed outcome measures 6–12 months post-intervention [19, 22, 24]. In one trial, compared with no intervention, the telerehabilitation group of older adults with knee osteoarthritis had superior outcomes for pain, function, quality of life and physical activity levels 6 months post-intervention [19].
In two trials where telerehabilitation was compared with face-to-face rehabilitation for people with chronic heart failure [24] and severe COPD [22], there were no significant differences in 6MWD or quality of life at 6 [24] or 12 months [22] and no difference in risk of hospitalisation or mortality [22].
Effect of telerehabilitation on health service costs
There was moderate certainty evidence from two trials [20, 30] with 484 participants post-knee arthroplasty of a moderate-to-large effect of lower health-care costs for telerehabilitation (SMD −0.69, 95% CI −0.88 to −0.51, I2 0%) compared with face-to-face rehabilitation (Table 3 and Supplementary Appendix 3).
Discussion
This review found that physiotherapist-led, exercise-based telerehabilitation is safe, well adhered to and effective for older adults with musculoskeletal or cardiopulmonary conditions. Telerehabilitation was not inferior to face-to-face physiotherapy and better than no intervention for patient health outcomes of quality of life, 6-min walk distance (6MWD), TUGT, knee flexion ROM and knee extensor strength. There was some evidence of sustained effects at 6 and 12 months and telerehabilitation was associated with lower health-care costs compared with face-to-face physiotherapy. Although there were no significant differences between groups, telerehabilitation was inferior to face-to-face physiotherapy in terms of pain and did not reduce pain more than no intervention. This review adds to previous findings that telerehabilitation is acceptable to [32] and can be as effective as face-to-face physiotherapy [33–35] by demonstrating non-inferiority and cost savings in a broader range of conditions in an at-risk older adult population.
This review found that telerehabilitation is safe and well adhered to by older adults with musculoskeletal or cardiopulmonary conditions. Previous studies have reported that clinicians have concerns about patient safety and lack of close physical supervision in telerehabilitation [36]. This is particularly important in the older population where older adults may experience more issues with mobility and falls [37]. This review found that older adults participating in physiotherapy-led telerehabilitation do not appear to be at greater risk of adverse events or falls compared with older adults who were completing their rehabilitation face-to-face. This may be because the telerehabilitation interventions were supervised by trained physiotherapists who could modify and tailor exercises to ensure safety. This review also found that adherence to exercise sessions was better via telerehabilitation compared with face-to-face which may be attributed to the removal of common barriers to accessing face-to-face rehabilitation such as transportation, physical access, fatigue and mobility issues [38]. These findings contrast to common opinion that older adults may be unable or not willing to engage in technology [39]. Rehabilitation providers should therefore be confident to provide telerehabilitation as an option for older adults to improve access and adherence.
Since older adults were able to safely engage in physiotherapist-led, exercise-based telerehabilitation, they also improved their physical function, activity outcomes and quality of life. Given that telerehabilitation was not inferior to face-to-face rehabilitation across a variety of patient outcomes (quality of life, 6MWD, TUGT, knee flexion ROM and knee extensor strength), it appears that the mode of physiotherapy delivery (i.e. face-to-face versus videoconferencing) is less important than the content of rehabilitation programmes for improving outcomes. Contrary to all other outcomes, pain outcomes in telerehabilitation were inferior to face-to-face rehabilitation and not better than any rehabilitation. This may partially be explained by a low number of studies in the meta-analyses and high variability in the data. However, this may also be explained by important elements known to impact pain (e.g. touch, peer support and therapist–patient relationship [40]) being absent in telerehabilitation. Overall, the results are promising given the common perception physiotherapy cannot be delivered successfully via telerehabilitation as it requires ‘hands on therapy’ [39]. Therefore, this allows potential for greater access to physiotherapy services for older people.
Delivery of telerehabilitation by physiotherapists demonstrated potential cost savings compared with face-to-face rehabilitation. This has positive, widespread implications for older adults who may have difficulty accessing physiotherapy in a clinic setting because of travel and cost and therefore missing out on vital interventions. By utilising telerehabilitation, health services can improve accessibility and better meet growing demand for services because of an ageing population by increasing the capacity of the services by providing high quality physiotherapy to a greater volume of patients [9]. Productivity gains and cost savings can be achieved by reducing travel by health service staff [9] enabling staff to offer more consultations to more patients. Telerehabilitation may also reduce the physical strain on health services by reducing the need for space required to deliver face-to-face services (e.g. gymnasium space, car parking, etc.). Therefore, health services should consider offering exercise-based physiotherapy services via telehealth to improve access and patient health outcomes and reduce delivery costs.
Orientation and education of service providers and older patients would further reduce the digital divide and increase the reach of telerehabilitation. This could include initial face-to-face assessment in the patient’s home, with comprehensive assessment of the patient including falls risk, their home environment and technology set up, followed by written education material and coaching to mitigate safety and adherence risks [41]. Engagement with supportive carers and family members can promote the patient’s long-term adherence [41]. Using the patient’s own device can also promote long term adherence and sustainability [41]. Promotion of telerehabilitation by other health professionals including general practitioners could improve patient engagement and knowledge. Although this review included older adults with musculoskeletal and cardiopulmonary conditions, there is potential for the use of telerehabilitation with other conditions including oncology [42] and neurological [43] conditions.
Strengths
This review was the first to evaluate telerehabilitation exclusively in older adults—a vulnerable population who may be excluded from telehealth research. This review was registered prospectively in PROSPERO and was conducted and reported using the PRISMA guidelines [11]. Robust methods were employed to extract, assess and analyse the data, and certainty of evidence was evaluated using GRADE [17].
Limitations
A limited range of age and health conditions were evaluated in the included trials therefore, it is unknown whether the results of this review could be translated to the broad range of health conditions affecting older adults, especially those with greater comorbidities and complexity and those at a high risk of falls and frailty. Selection bias could be another limitation whereby patients who are more confident and interested in using technology are more likely to adhere to a telerehabilitation exercise programme and therefore receive greater benefit. We also did not include trials of telerehabilitation programmes delivered by other health professionals or fitness trainers as the main focus of this review was on physiotherapy supervision. There was significant heterogeneity in intervention characteristics such as frequency and duration of sessions across trials that may make it difficult to implement programmes in practice; however, results were largely homogenous.
Conclusion
Physiotherapist-supervised, exercise-based telerehabilitation for older adults with musculoskeletal or cardiopulmonary conditions is safe, effective and non-inferior to face-to-face rehabilitation for improving patient outcomes and reducing health care costs. These findings, in conjunction with further robust research in the area, may have widespread implications to improve access to rehabilitation for older adults through the provision of telerehabilitation.
Supplementary Material
Contributor Information
Matoula Wicks, Community Health Program, Eastern Health, Box Hill, VIC 3128, Australia.
Amy M Dennett, Allied Health Clinical Research Office, Eastern Health, Box Hill, VIC 3128, Australia; School of Allied Health, Human Services and Sport, La Trobe University, Bundoora, VIC 3086, Australia.
Casey L Peiris, School of Allied Health, Human Services and Sport, La Trobe University, Bundoora, VIC 3086, Australia; Allied Health, Royal Melbourne Hospital, Parkville, VIC 3052, Australia.
Declaration of Conflicts of Interest
None.
Declaration of Sources of Funding
None.
Data Availability
The data that support the findings of this review are available from the corresponding author, CP, upon reasonable request.
References
- 1. Andrews GR. Care of older people: promoting health and function in An ageing population. BMJ 2001; 322: 728–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Taylor NF, Dodd KJ, Shields N, Bruder A. Therapeutic exercise in physiotherapy practice is beneficial: a summary of systematic reviews 2002–2005. Aust J Physiother 2007; 53: 7–16. [DOI] [PubMed] [Google Scholar]
- 3. Schutzer KA, Graves BS. Barriers and motivations to exercise in older adults. Prev Med 2004; 39: 1056–61. [DOI] [PubMed] [Google Scholar]
- 4. Groot GCL, Fagerström L. Older adults' motivating factors and barriers to exercise to prevent falls. Scand J Occup Ther 2011; 18: 153–60. [DOI] [PubMed] [Google Scholar]
- 5. Haines KJ, Berney S. Physiotherapists during COVID-19: usual business, in unusual times. J Physiother 2020; 66: 67–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Seron P, Oliveros M-J, Gutierrez-Arias Ret al. Effectiveness of telerehabilitation in physical therapy: a rapid overview. Phys Ther 2021; 101: 1. 10.1093/ptj/pzab053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Czaja SJ, Zarcadoolas C, Vaughon WL, Lee CC, Rockoff ML, Levy J. The usability of electronic personal health record systems for an underserved adult population. Hum Factors 2015; 57: 491–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Collado-Mateo D, Lavín-Pérez AM, Peñacoba Cet al. Key factors associated with adherence to physical exercise in patients with chronic diseases and older adults: an umbrella review. Int J Environ Res Public Health 2021; 18: 1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Snoswell CL, Taylor ML, Comans TA, Smith AC, Gray LC, Caffery LJ. Determining if telehealth can reduce health system costs: scoping review. J Med Internet Res 2020; 22: e17298. 10.2196/17298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Marks D, Kitcher S, Attrazic E, Hing W, Cottrell M. The health economic impact of musculoskeletal physiotherapy delivered by telehealth: a systematic review. Int J Telerehabilitation 2022; 14. 10.5195/ijt.2022.6524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shamseer L, Moher D, Clarke Met al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015; 349: g7647. 10.1136/bmj.g7647. [DOI] [PubMed] [Google Scholar]
- 12. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–74. [PubMed] [Google Scholar]
- 13. Stephens D. World Health Organization's international classification of functioning, disability and health - ICF. J Audiol Med 2001; 10: vii–x. [Google Scholar]
- 14. Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother 2009; 55: 129–33. [DOI] [PubMed] [Google Scholar]
- 15. Cohen J. The statistical power of abnormal-social psychological research: a review. J Abnorm Soc Psychol 1962; 65: 145–53. [DOI] [PubMed] [Google Scholar]
- 16. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003; 327: 557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guyatt G, Oxman AD, Akl EAet al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011; 64: 383–94. [DOI] [PubMed] [Google Scholar]
- 18. An J, Ryu HK, Lyu SJ, Yi HJ, Lee BH. Effects of preoperative telerehabilitation on muscle strength, range of motion, and functional outcomes in candidates for total knee arthroplasty: a single-blind randomized controlled trial. Int J Environ Res Public Health 2021; 18: 6071. 10.3390/ijerph18116071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bennell KL, Lawford BJ, Keating Cet al. Comparing video-based, telehealth-delivered exercise and weight loss programs with online education on outcomes of knee osteoarthritis: a randomized trial. Ann Intern Med 2022; 175: 198–209. [DOI] [PubMed] [Google Scholar]
- 20. Prvu Bettger J, Green CL, Holmes DNet al. Effects of virtual exercise rehabilitation in-home therapy compared with traditional care after total knee arthroplasty: VERITAS, a randomized controlled trial. J Bone Joint Surg Am 2020; 102: 101–9. [DOI] [PubMed] [Google Scholar]
- 21. Eriksson L, Lindström B, Gard G, Lysholm J. Physiotherapy at a distance: a controlled study of rehabilitation at home after a shoulder joint operation. J Telemed Telecare 2009; 15: 215–20. [DOI] [PubMed] [Google Scholar]
- 22. Godtfredsen N, Frølich A, Bieler Tet al. 12-months follow-up of pulmonary tele-rehabilitation versus standard pulmonary rehabilitation: a multicentre randomised clinical trial in patients with severe COPD. Respir Med 2020; 172: 106129. 10.1016/j.rmed.2020.106129. [DOI] [PubMed] [Google Scholar]
- 23. Hansen H, Bieler T, Beyer Net al. Supervised pulmonary tele-rehabilitation versus pulmonary rehabilitation in severe COPD: a randomised multicentre trial. Thorax 2020; 75: 413–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hwang R, Bruning J, Morris NR, Mandrusiak A, Russell T. Home-based telerehabilitation is not inferior to a centre-based program in patients with chronic heart failure: a randomised trial. J Physiother 2017; 63: 101–7. [DOI] [PubMed] [Google Scholar]
- 25. Moffet H, Tousignant M, Nadeau Set al. In-home telerehabilitation compared with face-to-face rehabilitation after total knee arthroplasty: a noninferiority randomized controlled trial. J Bone Joint Surg Am 2015; 97: 1129–41. [DOI] [PubMed] [Google Scholar]
- 26. Moffet H, Tousignant M, Nadeau Set al. Patient satisfaction with in-home telerehabilitation after total knee arthroplasty: results from a randomized controlled trial. Telemed J E Health 2017; 23: 80–7. [DOI] [PubMed] [Google Scholar]
- 27. Peng X, Su Y, Hu Zet al. Home-based telehealth exercise training program in Chinese patients with heart failure: a randomized controlled trial. Medicine 2018; 97: e12069. 10.1097/MD.0000000000012069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Russell TG, Buttrum P, Wootton R, Jull GA. Internet-based outpatient telerehabilitation for patients following total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am 2011; 93: 113–20. [DOI] [PubMed] [Google Scholar]
- 29. Tousignant M, Moffet H, Boissy P, Corriveau H, Cabana F, Marquis F. A randomized controlled trial of home telerehabilitation for post-knee arthroplasty. J Telemed Telecare 2011; 17: 195–8. [DOI] [PubMed] [Google Scholar]
- 30. Tousignant M, Moffet H, Nadeau Set al. Cost analysis of in-home telerehabilitation for post-knee arthroplasty. J Med Internet Res 2015; 17: e83. 10.2196/jmir.3844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Tsai LL, McNamara RJ, Moddel C, Alison JA, McKenzie DK, McKeough ZJ. Home-based telerehabilitation via real-time videoconferencing improves endurance exercise capacity in patients with COPD: the randomized controlled TeleR study. Respirology 2017; 22: 699–707. [DOI] [PubMed] [Google Scholar]
- 32. Hwang R, Bruning J, Morris N, Mandrusiak A, Russell T. A systematic review of the effects of telerehabilitation in patients with cardiopulmonary diseases. J Cardiopulm Rehabil Prev 2015; 35: 380–9. [DOI] [PubMed] [Google Scholar]
- 33. Pastora-Bernal JM, Martín-Valero R, Barón-López FJ, Estebanez-Pérez MJ. Evidence of benefit of telerehabitation after orthopedic surgery: a systematic review. J Med Internet Res 2017; 19: e142. 10.2196/jmir.6836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Jansson MM, Hyvämäki P, Pikkarainen M. Computer-and telephone-delivered interventions on patient outcomes and resource utilization in patients with orthopaedic conditions: a systematic review and narrative synthesis. Orthop Nurs 2020; 39: 340–52. [DOI] [PubMed] [Google Scholar]
- 35. Panda S, Bali S, Kirubakaran R, Hagenberg A. Telerehabilitation and total knee arthroplasty: a systematic review and meta-analysis of randomised controlled trials. Int J Ther Rehabil 2015; 22: S6. 10.12968/ijtr.2015.22.Sup8.S6. [DOI] [Google Scholar]
- 36. Cottrell MA, Galea OA, O’Leary SP, Hill AJ, Russell TG. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clin Rehabil 2017; 31: 625–38. [DOI] [PubMed] [Google Scholar]
- 37. Ganz DA, Latham NK. Prevention of falls in community-dwelling older adults. N Engl J Med 2020; 382: 734–43. [DOI] [PubMed] [Google Scholar]
- 38. Hopley M, Horsburgh M, Peri K. Barriers to accessing specialist care for older people with chronic obstructive pulmonary disease in rural New Zealand. J Prim Health Care 2009; 1: 207–14. [PubMed] [Google Scholar]
- 39. Wundersitz C, Caelli A, Georgy Jet al. Conducting community rehabilitation review sessions via videoconference: a feasibility study. Aust J Rural Health 2020; 28: 603–12. [DOI] [PubMed] [Google Scholar]
- 40. Cranen K, Drossaert CHC, Brinkman ES, Braakman-Jansen ALM, Ijzerman MJ, Vollenbroek-Hutten MMR. An exploration of chronic pain patients' perceptions of home telerehabilitation services. Health Expect 2012; 15: 339–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dennett AM, Hirko KA, Porter KJet al. Embedding lifestyle interventions into cancer care: has telehealth narrowed the equity gap? J Natl Cancer Inst Monogr 2023; 2023: 133–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Dennett A, Harding KE, Reimert J, Morris R, Parente P, Taylor NF. Telerehabilitation’s safety, feasibility, and exercise uptake in cancer survivors: process evaluation. JMIR Cancer 2021; 7: e33130. 10.2196/33130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Johansson T, Wild C. Telerehabilitation in stroke care – a systematic review. J Telemed Telecare 2011; 17: 1–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this review are available from the corresponding author, CP, upon reasonable request.