Abstract
Background
Believability and thoughts are considered as the pillars of behaviors over time, and anxious feelings are a risk factor for mental disorders, especially during the coronavirus disease (COVID-19) pandemic. This study aimed to explore the thought believability and anxious feelings of COVID-19 among infected and healthy families.
Methods
In this hospital-based matched case-control study, health surveillance files of COVID-19 patients were collected from January to June 2021 and were analyzed statistically. In this study, two questionnaires of demographic characteristics and the Believability of Anxious Feelings and Thoughts (BAFT) were used. Data were analyzed using the One-way ANOVA.
Results
Of 600 participants, 300 (50%) were PCR-confirmed and 300 (50%) were non-infected. Overall, 163 (54.33%) of infected people were male, 146 (48.67%) single, and 156 (52.00%) government employees. The results showed that the mean scores of physical anxiety (PA) and negative evaluation (NE) in the case group is significantly higher than the control group (P = 0.001); while emotional regulation (ER) in the control group was significantly higher than the case group (P = 0.001).
Conclusion
Having high believability to the risks of COVID-19 may be a predictor of preventive behaviors in individuals. Worrying about COVID-19 can increase the perceived risk of a pandemic in societies and consequence, increase the general public health.
Keywords: COVID-19, Believability, Anxiety
↑What is “already known” in this topic:
COVID-19 is one of those conditions that, due to its prevalence, can lead to changes in the believability of thoughts and subsequently create feelings of anxiety in all areas, especially psychological problems, and many studies have not been conducted to confirm this issue.
→What this article adds:
The COVID-19 pandemic has led to changes in attitudes and believability of thoughts, followed by anxious feelings about the disease. This change in attitude and behavior is an important predictor of preventive health behaviors for controlling the transmission chain of this disease, and having believability about this disease can help health policymakers to manage the risks of this pandemic and increase public health.
Introduction
Coronavirus disease 2019 (COVID-19) is a contagious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), that was first reported on December 31, 2019, in Wuhan, China, and after a while became a pandemic with economic, social and health consequences (1-4). The severity of the disease now appears to be more severe than originally estimated (5). As of October 28, 2021, about 245 million people worldwide have been infected with the virus and about 5 million people have lost their lives (6). Environmental and genetic factors have been suggested as the disease's plausible risk factors (7-10). Common symptoms of COVID-19 include fever, dry cough, ground-glass opacities in CT scans of the lung and increasing CRP levels (11). Also, this epidemic has affected people's believability and attitude (12-14). The COVID-19 pandemic can create far-reaching consequences for individuals. Beliefs become habits and even personality traits and manifest themselves in their behaviors. Some people continue to resist being firm and not changing their believability (15). There is ample evidence that people with anxiety disorders are immersed in metacognitive beliefs. Furthermore, anxious feelings and emotional regulation (ER) skills are very effective in predicting social anxiety in individuals, so findings indicate that reassessment and anxious feelings are important psychological components in predicting social anxiety (16). According to cognitive theories, anxious feelings resulting from the evaluation of negative cognitions about emotions are called anxiety, which is a factor in creating risk and therefore persistence of anxiety. As a vulnerable factor, anxious feelings are related to other mental disorders such as borderline personality disorder, substance abuse disorder, and especially depressive disorder and depressive symptoms (17). Thoughts' believability can be the basis for the formation of behaviors over time. On the other hand, there is a reciprocal relationship between behaviors, beliefs, and attitudes, but they do not simply change when beliefs and attitudes shape behavior; Unless significant changes occur in the context in which these beliefs are formed (18). COVID-19 is one of those conditions that due to its prevalence, can cause changes in thoughts believability in all areas, especially the psychological area, and obviously believability will change through this. Changes in attitudes and beliefs at different levels can change the type of coping methods, which in turn will lead to the formation of newer coping methods for life events (19). Perceived believability and perceived threat have been shown to be important predictors of health behaviors (20). A previous study found a direct association between the preventive believability of COVID-19 and perceived severity and sensitivity (21). Adequate knowledge and believability about COVID-19 have also become common among students and have had acceptable performance (22).
Given that thought of believability and anxious feelings about this disease can be an important predictor for preventive health behaviors to control the transmission chain of this disease, having believability about the disease can also help health policymakers to manage the risks of this pandemic and increase public health (23, 24). Therefore, the aim of this study was to assess the thought believability and anxious feelings of the COVID-19 virus among infected and healthy families.
Methods
Study setting and design
This is a matched case-control study conducted in the northeast of Iran. The study was approved by the THUMS ethics committee (approval No. IR.THUMS.REC.1400.002) and followed through the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline. The sample size was calculated at a 95% confidence level based on paired sample t-test was 600 persons (300 in the affected group and 300 in the healthy group) and based on similar studies (25-27). This study is based on the health surveillance data acquired from the hospital and health database, spanning over a six-month period from January to June 2021. Patients in the case group were selected based on common symptoms of fever, dry cough, and bilateral ground-glass opacities in CT scans of the lung and increased CRP level. Also, in order to further clone the case and control groups, the control group was selected from other families of covid-19 patients.
Inclusion criteria were: satisfaction with participation, ability to read and write, and access to WhatsApp Messenger. Exclusion criteria were: having a history of anxiety disorders, taking sedatives in the field of anxiety, and incomplete response to the questionnaire. Three hundred families with cases of COVID-19 with positive polymerase chain reaction (PCR) tests at the THUMS hospital laboratory was registered in the database during the study period. Only patients with at least one positive PCR test at the outpatient clinics or hospital wards of the THUMS were included.
Matching was performed based on demographic characteristics including age, Gender, Marital Status, Occupation, and Education, in two groups of damaged and healthy. Also, To further match the case and control groups, the control group was selected from other families of covid-19 patients. Individual matching was carried out for the residence place. In addition, an effort was made to match the date of diagnosis of the infections. However, if it was not possible for the same date, we selected controls from the nearest possible date of diagnosis. The sample population in case and control groups were selected by random cluster sampling through health surveillance in the north, south, center and east of the city. The request for cooperation and the link to the electronic questionnaire was sent through their mobile phone numbers. Other inclusion criteria were consent for participation and ability to read and write, and exclusion criteria included no history of anxiety disorders, no use of sedatives in the field of anxiety and incomplete response to the questionnaire.
Data collection
The demographic information of participant was retrospectively obtained as an electronic questionnaire. Demographic data included age, sex and occupation. Additionally, marital status and education level data were also recorded. To ensure identifying infected and healthy people, the question "Have you had Covid-19 in the past, based on laboratory results?" was used at the beginning of the questionnaire. Also, the instruments used included the Believability of Anxious Feelings and Thoughts Questionnaire (BAFT) by Herzberg et al.(16). This questionnaire measures the level of belief of each person on a Likert scale from 1 (I do not believe at all) to 7 (I completely believe) in each phrase. This questionnaire had 16 items and three subscales. Herzberg et al. examined the validity of this questionnaire so that the factor structure of this questionnaire showed three factors: physical symptoms, ER and negative evaluation (NE) (16).
The internal consistency of this questionnaire for healthy and anxious people was 0.90 and 0.91, respectively. Cronbach's alpha coefficient as well as the retest coefficient of the questionnaire, were 0.82 and 0.81, respectively (16). In Iran, the validity and reliability of the questionnaire were investigated by Soltani et al. There was an internal correlation between the BAFT and its subscales, and its reliability using Cronbach's alpha and the test-retest method were obtained at 0.82 and 0.81, respectively (28).
Statistical analysis
Descriptive statistical analyses (frequency and percent), and univariate analyses were designed using SPSS Software (version 16) and GraphPad Prism (version 6). The normality of data was checked by Kolmogorov–Smirnov test. Univariate analyses were conducted using either the chi-square test or Mann-Whitney U test or Student’s t-test to assess the association between demographic factors and case or control groups. Parametric approaches were applied for normally distributed data (e.g., Student’s t-test or One-way ANOVA) and non-parametric methods were used when data was not normally distributed (e.g., Mann-Whitney U or Kruskal–Wallis test). All the statistical analyses were 2-tailed and performed at a 5% significance level.
Results
During the study period, 600 matched pair individuals were included in our study (300 in the case group and 300 in the control group). Table 1 is related to the descriptive statistics of demographic variables in the two groups. Of the cases and control group, 163 (54.33) and 128 (42.67) were male, respectively.
Table 1. Characteristics of study participants according to case-control status.
| Variable | Case, N (%) | Control, N (%) | P-value | |
|---|---|---|---|---|
| Gender | Male | 163 (54.33) | 128 (42.67) | 0.162 |
| Female | 137 (45.67) | 172 (57.33) | ||
| Marital Status | Single | 146(48.67) | 107(35.67) | 0.413 |
| Married | 79 (26.33) | 126 (42.00) | ||
| Other | 75 (25.00) | 67 (22.33) | ||
| Occupation | Governmental | 156 (52.00) | 78 (26.00) | 0.436 |
| Self-employment | 63 (21.00) | 129 (43.00) | ||
| Homemaker | 81 (27.00) | 93 (31.00) | ||
| Education | Under diploma | 69 (23.00) | 97 (32.33) | 0.642 |
| Diploma | 84 (28.00) | 125 (41.67) | ||
| University degree | 147 (49.00) | 78 (26.00) | ||
| Age, Mean ± SD | 35.25 ± 1.65 | 31.64 ± 1.83 | 0.135 | |
According to Table 1, the highest gender in the case group was male (54%), the highest in the control group was female (57%), most of the case group was single (49%), and most of the healthy were married people (42%). Most of the individuals in the case group had governmental jobs (52%) and the most jobs in the control group were also self-employment (43%). In addition, the education of most of the case group was a university degree (49%) and the education of the control group was a diploma (42%).
Based on Table 2, there was a significant difference between the case and control groups in physical anxiety (PA), NE, and ER (P = 0.001). However, based on the mean scores, PA and NE in the case group were higher and emotional adjustment in the control group was higher than in the case group. The median and interquartile range (IQR) of the variables of NE, PA and ER in the two groups of infected and healthy are described separately in Figure 1 to Figure 3.
Table 2. Mean of dependent variables in case-control groups.
| Variable | Case, Mean ± SD | Control, Mean ± SD | P-value |
|---|---|---|---|
| Negative evaluation | 24.98 ± 1.91 | 20.94 ± 1.67 | 0.001 |
| Physical anxiety | 34.90 ± 2.50 | 33.59 ± 2.44 | 0.001 |
| Emotional regulation | 21.70 ± 1.65 | 24.38 ± 1.66 | 0.001 |
Figure 1.
Differences of dependent variables in case and control groups. PA and NE values in the case group are significantly greater than that of the control group. On the contrary, ER value in the case group is lower than the control group, ***P< .001. Horizontal lines represent the group median. Student’s t-test analysis or Mann-Whitney U test was conducted in the comparison.
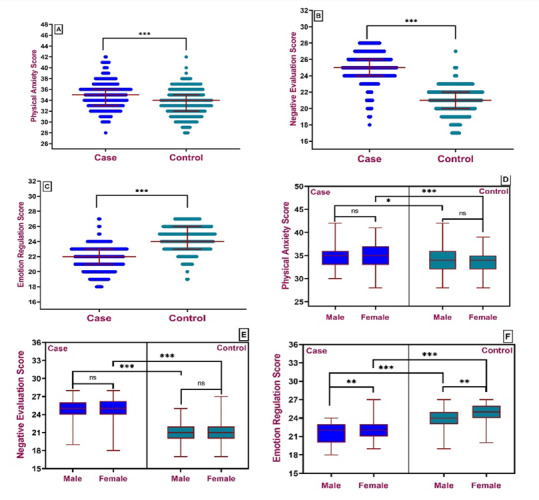
Figure 2.
Differences of dependent variables in case and control group’s age and marital status category. By box and whisker plots. There are no significant differences in the mean value for dependent variables, PA, NE and ER, in various categories of the study between groups. Ns is P>0.05. Median, lower quartile, upper quartile, Min, and Max values showed in plots. One-way ANOVA analysis or Kruskal–Wallis test was conducted in the com-parison.
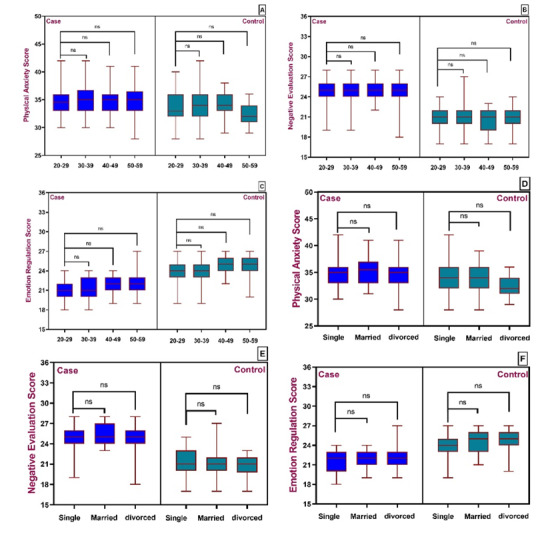
Figure 3.
Differences of dependent variables in case and control group’s occupation and educational status category. By box and whisker plots. There are no significant differences in the mean value for dependent variables, PA, NE and ER, in various categories of the study between groups. Ns is P>0.05. Median, lower quartile, upper quartile, Min, and Max values showed in plots. One-way ANOVA analysis or Kruskal–Wallis test was conducted in the comparison.
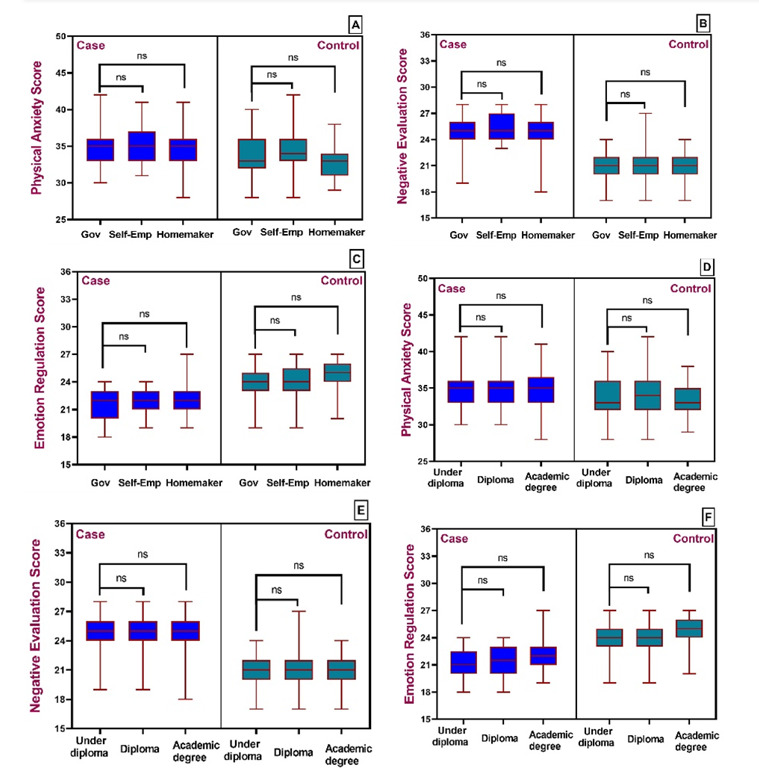
We found significant differences in the mean of NE, PA, and ER (P < 0.001). In addition, there are no significant differences in the mean value for dependent variables, PA and NE, in various categories of the study between groups. However, there was a significant difference between the mean values of the indices in the case and control groups’ categories.
Discussion
The results of the present study showed that single individuals had the highest percentage of case groups and married individuals had the highest percentage in the control group. These results were consistent with the study of Singh et al., which showed that the level of stress and disease in single nurses was higher than in married nurses (29). Explaining the low level of anxiety and less illness in married nurses during the COVID period, it can be said that married nurses are more likely to be in the family after work and will be supported by their spouse and even children (30). With family, they experience less anxiety and stress than single nurses. Our study was also in line with the study by Li et al. that married people experienced more stress than single people. The reason for the difference in results can be the differences in the living environment and the concerns of each group in their community (31).
The results of our study also showed that the education of most of the case group was a university degree (% 49) and the education of the control group was a diploma (% 42). These results are consistent with another study, which found that stress and anxiety predisposed to disease were higher in people with higher education (32). Ahmed et al. stated that despite their high level of knowledge and practice, physicians and dentists around the world experience anxiety and fear at work due to the effects of COVID-19 disease on humanity (33). Maybe this result is due to the high level of literacy in these people which allows for a proper analysis of the stressful situation, and this plays a role in increasing the rate of disease in them (30).
Another finding showed that men had the highest percentage (54%) in case groups and women had the highest percentage in the control group (57%) and were consistent with the results of the study by Lau et al., which showed that women performed better than men in COVID-19 preventive behaviors (34). One of the reasons for this finding is that women are more responsible for their own health and that of their family members(35).
Regarding the incidence rate and employment status, the results of the current study showed that the highest percentage of infected people were government employees (52%) and the lowest percentage were Self-employment (21%). The results of this study were consistent with the previous study (36). Explaining this finding, it can be said that people who were self-employed probably observed more preventive behaviors than other occupations, and mastery of the personal work environment seems to be one of the reasons for this finding. The results of our study showed that there was a significant difference in the variables of PA, NE and ER in the two groups (P < 0.001). Also, according to the results, the mean score of PA and NE in the case group was higher than the control group and the mean score of ER in the control group was higher than the case group. These findings were consistent with previous studies (31, 37-39).
The emergence of COVID-19 and its rapid spread leads to increased PA and impaired health in the community (31). People who are physically concerned about their health are more sensitive to their physical signs and symptoms, which in turn increases their anxiety and stress (40). PA is a common reaction to pandemic diseases that is more common in the early stages of the disease (34). In creating PA, misinformation about COVID-19 plays an important role in creating extreme health behaviors and vulnerability. These people endure excruciating stress and suffering due to the magnification of their physical symptoms (40). Therefore, one of the reasons for the higher score of PA in the case group than the control group was high anxiety and magnification of physical symptoms. People with various anxiety disorders experience high levels of NE and anxiety (41). NE is a class of conscious thoughts that revolve around a specific topic and cause the person to be exposed to various stressful situations (42). Therefore, due to high anxiety in the case group, the mean NE score in this group was higher than the control group.
Positive ER strategies are negatively related to anxiety and negative cognitive ER strategies are positively related to anxiety (43, 44). Emotion regulation has an effective role in predicting COVID-19 anxiety (39). When people experience a lot of negative emotions, they face more difficulties in performing their behaviors (45). Therefore, people in the case group had lower ER than the control group due to having a lot of negative emotions. Previous studies have examined various dimensions of the believability of the disease and its relationship to psychological and health outcomes, so it seems that disease believability as a presupposition for people with COVID-19 can determine and help behaviors related to the health and control of the lack of believability created by this disease in the future (22).
Given the strengths of the study, its limitations should also be considered. One of the limitations of the present study is not separating patients in terms of disease severity and disease stage, which is suggested to be considered in future research.Another limitation of the study was the lack of similar studies at the time of the study, so we used similar studies on influenza. In addition, another limitation was that the sample was scattered, and to minimize this, the postal code of the regions was used to send a questionnaire by SMS. The online questionnaire, in addition to the many benefits it has, especially during the outbreak of COVID-19, may not be available to everyone, especially those with low literacy and those who do not use a smartphone. This study can be used as a guide for developing and implementing health education programs about COVID-19.
Conclusion
Believability about a threat can predict preventive behaviors toward that risk. Most people in the community are aware of the risk of COVID-19 and consider themselves exposed to it, so if people have a high degree of credibility and believability over COVID-19, they are more likely to observe preventive behaviors. Therefore, by designing educational programs by educational managers and clinical instructors, deeper believability can be created in the community.
List of abbreviations
ANOVA: Analysis of Variance
BAFT: The Believability of Anxious Feelings and Thoughts Questionnaire
COVID-19: Coronavirus Disease 2019
ER: Emotional Regulation
IQR: Interquartile Range
NE: Negative Evaluation
PA: Physical Anxiety
PCR: Polymerase Chain Reaction
SARS-CoV-2: Severe Acute Respiratory Syndrome Coronavirus 2
STROBE: Strengthening the Reporting of Observational Studies in Epidemiology
SD: Standard Deviation
THUMS: Torbat Heydariyeh University of Medical Sciences
SPSS: Statistical Package for the Social Sciences
Conflict of Interests
The authors declare that they have no competing interests.
Funding
This article was supported by the Torbat Heydariyeh University of Medical Sciences.
Acknowledgments
This article is the result of the approved research project with the code of ethics committee IR.THUMS.REC.1400.002 is supported by the Vice Chancellor for Research and Technology of Torbat Heydariyeh University of Medical Sciences. Therefore, we thank all relevant authorities and all participants for their participation in the implementation of the research project.
Cite this article as : Ghodrati Torbati A, Shirinzadeh Feizabadi A, Askari MR, Zandi A, Sarmadi M. Thought Believability and Anxious Feelings about COVID-19: A Case-Control Study in Northeastern Iran. Med J Islam Repub Iran. 2023 (29 Aug);37:93. https://doi.org/10.47176/mjiri.37.93
References
- 1.Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ. 2020;368:m408. doi: 10.1136/bmj.m408. [DOI] [PubMed] [Google Scholar]
- 2.Marques de, da Silva, Sena Oliveira, Simoes-e-Silva AC. How is COVID-19 pandemic impacting mental health of children and adolescents. Int J Disaster Risk Reduct. 2020;51:101845. doi: 10.1016/j.ijdrr.2020.101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Syed AA, Gupta S, Rai D. Psychological, social and economic impact of COVID 19 on the working population of India: Exploratory factor analysis approach. Int J Disaster Risk Reduct. 2021;66:102617. doi: 10.1016/j.ijdrr.2021.102617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rose A. COVID-19 economic impacts in perspective: A comparison to recent U.S. disasters. Int J Disaster Risk Reduct. 2021 Jun 15;60:102317. doi: 10.1016/j.ijdrr.2021.102317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fouladi Dehaghi, Ghodrati-Torbati A, Teimori G, Ibrahimi Ghavamabadi, Jamshidnezhad A. Face masks vs. COVID-19: a systematic review. . Invest Educ Enferm. 2020;38(2):e13. doi: 10.17533/udea.iee.v38n2e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization coronavirus disease (COVID-19) dashboard. 2020. https://covid19.who.int/ https://covid19.who.int/
- 7.Sarmadi M, Ahmadi-Soleimani SM, Fararouei M, Dianatinasab M. COVID-19, body mass index and cholesterol: an ecological study using global data. BMC Public Health. 2021;21(1):1712. doi: 10.1186/s12889-021-11715-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dehaghi BF, Ghodrati-Torbati A, Teimori G, Ghavamabadi LI, Jamshidnezhad A. Face masks vs. COVID-19: a systematic review. Invest Educ Enferm. 2020;38(2) doi: 10.17533/udea.iee.v38n2e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sarmadi M, Moghanddam VK, Dickerson AS, Martelletti L. Association of COVID-19 distribution with air quality, sociodemographic factors, and comorbidities: an ecological study of US states. Air Qual Atmos Health. 2020;14(4):1–11. doi: 10.1007/s11869-020-00949-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sarmadi M, Ghodrati-Torbati A, Gazerani A, Yaghoobi H, Bakhtiari-Dovvombaygi H. Association of HIV/AIDS and COVID-19 variables: an ecological study. HIV & AIDS Review. Int J HIV-Related Problems. 2021;20(2):71. doi: 10.5114/hivar.2021.107233. [DOI] [Google Scholar]
- 11.Kelvin AA, Halperin S. COVID-19 in children: the link in the transmission chain. Lancet Infect Dis. 2020 Jun 1;20(6):633. doi: 10.1016/S1473-3099(20)30236-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Torbati AG, Imeni M, Abbaspour S. Impact of Dialectical Behavior Therapy on Depression and Anxiety in Patients Following COVID-19 Discharge. Open Psychol. 2022 Nov 15;15(1) [Google Scholar]
- 13.Qiu Y, Wu Q, Chen R, Guan C. Research on psychological stress and mental health of medical staff in COVID-19 prevention and control. Int J Disaster Risk Reduct. 2021;65:102524. doi: 10.1016/j.ijdrr.2021.102524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen Y, Feng J, Chen A, Lee JE, An L. Risk perception of COVID-19: A comparative analysis of China and South Korea. Int J Disaster Risk Reduct. 2021;61:102373. doi: 10.1016/j.ijdrr.2021.102373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nowell B, Boyd N. Viewing community as responsibility as well as resource: Deconstructing the theoretical roots of psychological sense of community. J Community Psychol. 2010;38(7):828. [Google Scholar]
- 16.Herzberg KN, Sheppard SC, Forsyth JP, Credé M, Earleywine M, Eifert GH. The Believability of Anxious Feelings and Thoughts Questionnaire (BAFT): A psychometric evaluation of cognitive fusion in a nonclinical and highly anxious community sample. Psychol Assess. 2012;24(4):877. doi: 10.1037/a0027782. [DOI] [PubMed] [Google Scholar]
- 17.Farahani M. Changes in Attitude, Beliefs and Values and COVID-19 pandemic. J Res Health Psychol. 2020;14(1):1–5. [Google Scholar]
- 18.Iman S, Khaula A, Maryam T, Sedigheh A, Anahita Z, Gholamheidar T-B. et al. Accomplices of job burnout among employees of a medical university. Russ Open Med J. 2019;8(1):105. [Google Scholar]
- 19.Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J Psychiatry. 2020;51:102076. doi: 10.1016/j.ajp.2020.102076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Noar SM, Zimmerman RS. Health behavior theory and cumulative knowledge regarding health behaviors: are we moving in the right direction. Health Educ Res. 2005;20(3):275. doi: 10.1093/her/cyg113. [DOI] [PubMed] [Google Scholar]
- 21.Bashirian S, Jenabi E, Khazaei S, Barati M, Karimi-Shahanjarini A, Zareian S. et al. Factors associated with preventive behaviours of COVID-19 among hospital staff in Iran in 2020: an application of the Protection Motivation Theory. J Hosp Infect. 2020;105(3):430. doi: 10.1016/j.jhin.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aharon AA, Ruban A, Dubovi I. Knowledge and information credibility evaluation strategies regarding COVID-19: A cross-sectional study. Nurs Outlook. 2021;69(1):22–31. doi: 10.1016/j.outlook.2020.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abbaspour S, Tajik R, Atif K, Eshghi H, Teimori G, Ghodrati-Torbati A. et al. Prevalence and correlates of mental health status among pre-hospital healthcare staff. Clin Pract Epidemiol Ment Health. 2020;16:17. doi: 10.2174/1745017902016010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seyyedmoharrami I, Dehaghi BF, Abbaspour S, Zandi A, Tatari M, Teimori G. et al. The relationship between organizational climate, organizational commitment and job burnout: Case study among employees of the university of medical sciences. Open Public Health J. 2019;12(1) [Google Scholar]
- 25.Torbati A, Abbaspour S, Zandi A. Efficacy of psychoeducational intervention on depression and anxiety after discharge in patients with covid-19. . J Public Health Dev . 2022;20(3):209–209. [Google Scholar]
- 26.Torbati AG, Zandi A, Abbaspour S. Effectiveness of educational intervention-based compassion therapy on emotional regulation and self-control after discharge of patients With COVID-19. J Educ Health Promot. 2022 Jan 1;11(1):279. doi: 10.4103/jehp.jehp_66_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ghodrati Torbati, Eshaghzadeh M, Imeni M, Abbaspour S. The Effects of Educational Intervention Based On Dialectical Behavior Therapy on Emotional Regulation and Self-Control after Discharge in Patients with Covid-19. Health Educ Health Promot. 2022 Jul 10;10(3):525. doi: 10.4103/jehp.jehp_66_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Soltani E, Bahrainian SA, Masjedi Arani, Farhoudian A, Gachkar L. Psychometric properties of the Believability of Anxious Feelings and Thoughts Questionnaire (BAFT) Pajoohandeh J. 2015;20(5):273. [Google Scholar]
- 29.Singh K, Lima G, Cha M, Cha C, Kulshrestha J, Ahn Y-Y. et al. Misinformation, Believability, and Vaccine Acceptance Over 40 Countries: Takeaways From the Initial Phase of The COVID-19 Infodemic. arXiv preprint arXiv:210410864. 2021 doi: 10.48550/arXiv.2104.10864. [DOI] [PMC free article] [PubMed]
- 30.Ariapooran S, Amirimanesh M. Depression, Anxiety and Suicidal ideation of Nurses in the Outbreak of COVID-19: The Role of Demographic Variables. J Arak Univ Medical Sci. 2020;23(5):724. [Google Scholar]
- 31.Li S, Wang Y, Xue J, Zhao N, Zhu T. The impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo users. Int J Environ Res Public Health. 2020;17(6):2032. doi: 10.3390/ijerph17062032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Othman N. Depression, anxiety, and stress in the time of COVID-19 pandemic in Kurdistan region, Iraq. Kurdistan Journal of Applied Research. 2020;5(3):37–44. doi: 10.24017/covid.5. [DOI] [Google Scholar]
- 33.Ahmed MA, Jouhar R, Ahmed N, Adnan S, Aftab M, Zafar MS. et al. Fear and practice modifications among dentists to combat novel coronavirus disease (COVID-19) outbreak. Int J Environ Res Public Health. 2020;17(8):2821. doi: 10.3390/ijerph17082821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bronfman N, Repetto P, Cordón P, Castañeda J, Cisternas P. Gender Differences on Psychosocial Factors Affecting COVID-19 Preventive Behaviors. Sustainability. 2021;13(11):6148. [Google Scholar]
- 35.Park JH, Cheong HK, Son DY, Kim SU, Ha C-M. Perceptions and behaviors related to hand hygiene for the prevention of H1N1 influenza transmission among Korean university students during the peak pandemic period. BMC Infect Dis. 2010;10(1):1–8. doi: 10.1186/1471-2334-10-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dai Y, Hu G, Xiong H, Qiu H, Yuan X. Psychological impact of the coronavirus disease 2019 (COVID-19) outbreak on healthcare workers in China. Soc Psychiatry Psychiatr Epidemiol. 2022;57(8):1515–1529. doi: 10.1007/s00127-022-02264-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bagheri Sheykhangafshe, Shabahang R, Tajbakhsh K, Hamideh Moghadam, Sharifipour Choukami, Mousavi SM. Role of Health Anxiety, Anxiety Sensitivity, and Somatosensory Amplification in Predictors of COVID-19 Anxiety Students. J Psychol Stud. 2021;16(4) [Google Scholar]
- 38.Ogińska-Bulik N, Michalska P. The relationship between emotional processing deficits and posttraumatic stress disorder symptoms among breast cancer patients: The mediating role of rumination. J Clin Psychol Med Settings. 2020;27(1):11–21. doi: 10.1007/s10880-019-09606-6. [DOI] [PubMed] [Google Scholar]
- 39.Ezazi Bojnourdi, Ghadampour S, Moradi Shakib, Ghazbanzadeh R. Predicting corona anxiety based on cognitive emotion regulation strategies, health hardiness and death anxiety in diabetic patients. Iranian J Psychiatric Nurs. 2020;8(2):34–44. [Google Scholar]
- 40.Blakey SM, Abramowitz JS. Psychological predictors of health anxiety in response to the Zika virus. J Clin Psychol Med Settings. 2017;24(3):270. doi: 10.1007/s10880-017-9514-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brozovich FA, Goldin P, Lee I, Jazaieri H, Heimberg RG, Gross JJ. The effect of rumination and reappraisal on social anxiety symptoms during cognitive‐behavioral therapy for social anxiety disorder. J Clin Psychol. 2015;71(3):208. doi: 10.1002/jclp.22132. [DOI] [PubMed] [Google Scholar]
- 42.Constantin K, English MM, Mazmanian D. Anxiety, depression, and procrastination among students: Rumination plays a larger mediating role than worry. J Ration Emot Cogn Behav Ther. 2018;36(1):15–27. [Google Scholar]
- 43.Huh HJ, Kim KH, Lee HK, Chae JH. The relationship between childhood trauma and the severity of adulthood depression and anxiety symptoms in a clinical sample: The mediating role of cognitive emotion regulation strategies. J Affect Disord. 2017;213:44–50. doi: 10.1016/j.jad.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 44.Domaradzka E, Fajkowska M. Cognitive emotion regulation strategies in anxiety and depression understood as types of personality. Front Psychol. 2018;9:856. doi: 10.3389/fpsyg.2018.00856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Campbell-Sills L, Barlow DH, Brown TA, Hofmann SG. Acceptability and suppression of negative emotion in anxiety and mood disorders. Emotion. 2006;6(4):587. doi: 10.1037/1528-3542.6.4.587. [DOI] [PubMed] [Google Scholar]


