Abstract
Purpose
This systematic review explored dental complications associated with metal ion release from oral piercings using the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines.
Methods
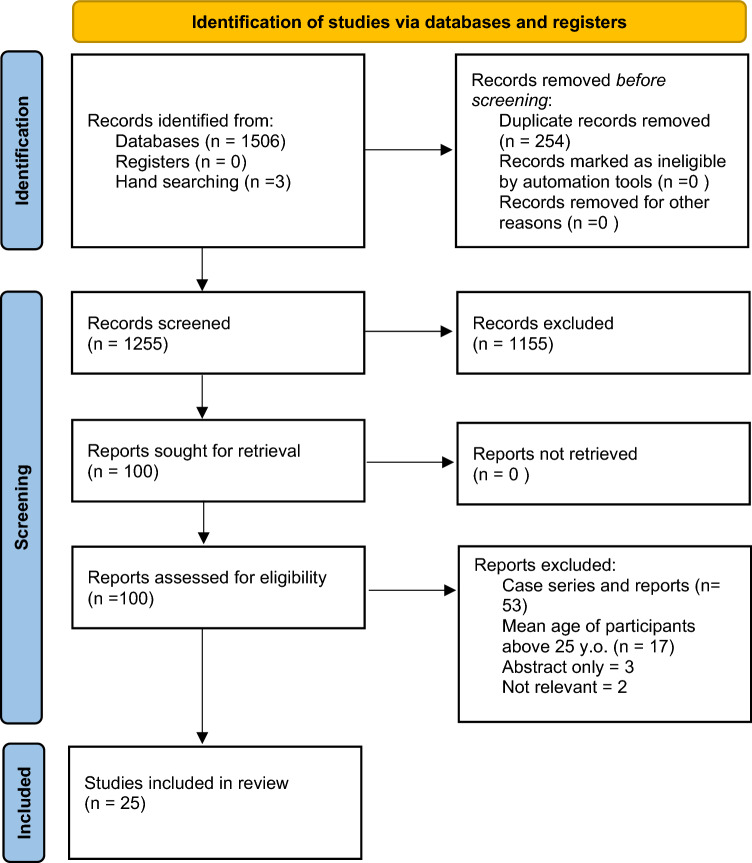
Item retrieval from October 2022 to December 2022 from databases, such as Cochrane Central Register of Controlled Trials, Medline, PubMed, Embase, Scopus and Web of Science, using predefined search terms was undertaken by two independent reviewers. Data were extracted and risk of bias was assessed using the Joanna Briggs Institute (JBI) critical appraisal checklist. From 1509 identified studies, 25 were included for analysis.
Results
Of the 25 studies, 20 included both clinical examination and questionnaire-based data. The remaining five studies were deemed low quality based on the Joanna Briggs Institute criteria. The average time piercings were worn ranged between 5 and 48 months. Most studies did not investigate complications from metal ion release. Only two studies examined the direct effects of metal ion release and showed that metal ions may cause hypersensitivity reactions and mucosal changes. Other soft tissue complications were reported, with gingival recession noted in 16 out of 25 studies, especially due to lip piercings. Studies reporting other complications were as follows: swelling (9), pain (8), infection (6), bleeding (6), inflammation (5), alterations to speech, eating and/or swallowing (5), changes to taste or metallic taste (5), and mucosal changes (4). Ten studies reported tooth chipping from tongue piercings.
Conclusion
Oral piercings leach metal ions into surrounding tissues which may cause local mucosal changes. Furthermore, oral piercings cause damage to both soft and hard oral tissues, particularly gingival recession for lip piercings and tooth chipping for tongue piercings. Thus, to prevent such adverse injuries, dental professionals should discourage patients against oral piercings.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40368-023-00831-0.
Keywords: Oral, Piercings, Metal ions, Complications
Introduction
Oral piercings are a form of body jewellery that are inserted into the oral or peri-oral tissues (Ziebolz et al. 2009). They have a long history, having been practised in diverse ancient cultures as part of ceremonial and religious practices (Vozza et al. 2014; Hennequin-Hoenderdos et al. 2016; Chadwick et al. 2005; Covello et al. 2020). However, over the last two decades, oral piercing has evolved into a common practice amongst young people in the Western world (Ziebolz et al. 2009; Vozza et al. 2014; Chadwick et al. 2005) with approximately 5.2% of young adults having oral piercings (Hennequin-Hoenderdos et al. 2016). Oral piercings are placed into the tongue, lips, cheeks or frena (Chadwick et al. 2005; Levin et al. 2005). Tongue piercings are commonly a barbell, with balls at either end of a rod, whilst lip piercings may be a ring or a labret, which is a rod with one ball and one flat disc (Ziebolz et al. 2009; Chadwick et al. 2005; Levin et al. 2005).
Common short-term complications after placing an oral piercing include pain, swelling of the site, and secondary bleeding (Ziebolz et al. 2009; Chadwick et al. 2005; Levin et al. 2005; Inchingolo et al. 2011). These problems are often self-limiting and of short duration. Erythema and haematoma can also occur, whilst tongue oedema may cause airway obstruction (Ziebolz et al. 2009; Levin et al. 2005). Changes to speech, swallowing patterns and mastication have also been reported (Kapferer et al. 2010; Firoozmand et al. 2009; Vieira et al. 2011). Less frequently, the generation of a galvanic current flow between barbell tongue piercings and metal dental restorations has been noted (Chadwick et al. 2005). Long-term complications from oral piercings include damage to gingival tissues, fractures of enamel and dentine, and allergic reactions, especially to nickel (Ziebolz et al. 2009; Hennequin-Hoenderdos et al. 2016; Levin et al. 2005). Abrasion of the enamel, fractures of tooth structure, and gingival recession, particularly affect the mandibular anterior teeth, are common long-term complications (Kapferer et al. 2010; Firoozmand et al. 2009; Kapferer et al. 2012; Vilchez-Perez et al. 2009).
The majority of piercings are made from metal, including surgical-grade stainless steel, titanium, platinum, silver or gold (Ziebolz et al. 2009; Walsh et al. 2008; Masood et al. 2023). When oral piercings come in contact with oral fluids such as saliva, they may corrode and leach out metal ions into the surrounding tissues (Domingo et al. 2019). The released ions can then cause allergic reactions, with nickel reported as the most common allergen (Vozza et al. 2014; Levin et al. 2005; Lupi et al. 2010). Other metals, such as chromium and cobalt, have been also reported to cause hypersensitivity reactions (Domingo et al. 2019; Lupi et al. 2010). Surface defects on the piercing surface may be a location where corrosion begins (Domingo et al. 2019). In addition to causing local reactions in the oral mucosa, released ions may enter the systemic circulation. Systemic complications of oral piercings include bacteraemia and infections at distant sites, including infective endocarditis and brain abscesses (Domingo et al. 2019). Whether other systemic reactions, including toxicity from released heavy metals, occurs from oral piercings is unclear.
Despite a range of serious complications caused by leaching of metal ions from oral piercings, no reviews of the literature on this topic have been conducted. A recent systematic review examined only the complications of oral piercings on hard and soft tissues (Passos et al. 2022). Therefore, the aim of this review is to investigate the oral complications as a result of metal ions released from oral piercings. The null hypothesis for this review is that the oral complications will be associated with the release of the metal ions from oral piercings.
Materials and methods
Protocol and registration
This systematic review used The Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines (Page et al. 2021). The protocol for this review was registered on PROSPERO (CRD42022336112).
Eligibility criteria, screening and selection
The eligibility for inclusion was based on the PICO criteria as described in Table 1 with (P) human participants; (I) intervention or oral metal piercings used; (C) comparison: allergy or hypersensitivity reactions and/or ion release from oral piercings; (O) outcome: incidence of hard and soft tissue injuries/complications from oral piercings and incidence of dental complications from metal ion release from oral piercings. The PICO research question for this systematic review was “Is there an association between metal ions released from oral piercings and oral complications?”
Table 1.
Inclusion and exclusion criteria adopted in the literature search
| Inclusion criteria | Exclusion criteria |
|---|---|
| P: Participants: human subjects of any gender, mean age below 25 years | Studies on piercings in other body areas (e.g. ear) |
| I: Interventions: Oral or peri-oral metal piercings located on tongue and/or lip and/or frenum and/or cheeks | Papers in alterative languages to English with no English translation |
| C: Comparison: allergy or biological or hypersensitivity reaction in relation to oral piercings; ion release from oral piercings | |
|
O: Outcomes: Incidence of hard and soft tissue injuries/complications from oral piercings. Adverse material reactions/hypersensitivity Incidence of dental complications from metal ion release from oral piercings |
Reviews, abstracts, letters to the editor, editorials |
| Study design: Nonrandomised control trials, cohort studies and case–control studies | |
|
Publication year: no restrictions Language: papers in English or with English-language abstract available |
Search strategy
Cochrane Central Register of Controlled Trials (CENTRAL), Medline (via EbscoHost), PUBMED (National Library of Medicine), Embase (via Elsevier), Scopus and Web of Science databases were searched using combinations of the following key terms: (mouth* OR oral OR lip OR tongue OR labial OR buccal OR frenulum OR mucosa OR gingiva AND (piercing* OR body piercing OR jewellery (disease OR injury OR complications) AND (allergy OR toxicity OR adverse reaction OR hypersensitivity) AND (release of metal ions OR metal ion release OR metal ions). The search was conducted from October 2022 to December 2022. Additional hand searches of article reference lists as well as Google and grey literature searches were conducted using the same keywords to identify literature not accessible via standard databases, as given in the supplemental data table.
Data collection and analysis
Studies reporting complications from oral or perioral piercings were identified. After screening of titles and abstracts, the reference lists of applicable studies were examined to identify any additional sources. The studies were imported into Endnote™ software (Clarivate, U.S.A), and duplicate articles were removed. The first level of selection was undertaken using titles and abstracts, by applying the inclusion and exclusion criteria outlined in Table 1. Subsequently, full text versions were retrieved, and a second level of selection was performed, using the same criteria. Study characteristics included in the data collection forms were as follows: author/s, year published, country where research was undertaken, study design, total number of subjects, participant characteristics (gender, mean age, type of piercing, mean period piercing worn), post-piercing oral complications, whether metal ion release was reported, conclusions and key findings. These findings were tabulated using Excel spreadsheets. For synthesis, studies were grouped into whether metal ion release was reported or not. Inter-rater reliability between the two independent assessors (M.M and S.Z) during the data extraction stages (identification, screening, eligibility, and inclusion) was calculated as a percentage. Inter-rater reliability agreement for selection and outcome was evaluated using Cohen’s kappa using the Statistical Package for the Social Sciences version 24.0 software (IBM Corp., Armonk, NY, USA).
Risk bias assessment reporting
The Joanna Briggs Institute (JBI) critical appraisal checklist for non-randomised experimental studies was used to rate the studies in terms of their risk of bias (Porritt et al. 2014). Two independent reviewers (M.S and S.Z) screened the articles, and any discrepancies were resolved by discuss with the third author (L.W).
Results
Literature results
From the database searches, a total of 1506 articles were identified, whilst three additional articles were found via hand-searching and checking reference lists. During the first level of selection, 254 duplicates were removed, and 1155 records excluded due to irrelevant titles and/or abstracts. A total of 100 papers were screened for eligibility. Case reports and series were excluded (n = 53) and articles with participants of mean age above 25 years of age were excluded (n = 17). This resulted in 30 articles that met the second level of inclusion criteria for this review.
From the 30 articles selected for inclusion, 5 articles were excluded when applying the selection criteria and through discussion amongst the reviewers. Three articles included only English abstracts. For these, it was difficult to assess study methodology against the JBI criteria, and so they were excluded. Two articles were not included due to being irrelevant, with one discussing Candida infections and another looking solely at temporomandibular disorders, which is outside the inclusion criteria. This reduced the final number of studies to 25.
The Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) flowchart is shown in Fig. 1. No papers reported an objectionable risk of bias.
Fig. 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analysis) flowchart for selection of studies
Inter-rater reliability agreement
The inter-rater reliability percentages for the two assessors were as follows: identification 98.8% (1509/1527 studies), screening 98.4% (1255/1276 studies), eligibility 100% (100/100 studies) and inclusion 83.3% (25/30 studies). It was agreed that two studies discussed the outcome of complications related to metal ion release from oral piercings. Discrepancies were resolved via discussion and agreement reached. The kappa scores were as follows: for inclusion 76.09% agreement (kappa 0.516) and for outcome 96.15% agreement (kappa 0.8999).
Outcomes from included studies
The included studies consisted of 14 cohort, 6 case–control and 5 cross-sectional studies. Three studies were published between 2020 and 2015, 12 studies between 2014 and 2009 and 10 studies, 2008 and 2003.
From the 25 included studies, the greatest number of articles published was from Brazil (n = 4). Other locations studies for studies are shown in Table 2.
Table 2.
Characteristics of included studies
| Author year Country |
Study design | Gender Mean Age (SD) Range in years |
Type of piercing Mean period for wearing piercing |
Post piercing dental/oral complications | Outcome of metal ion release | Conclusions/Key findings |
|---|---|---|---|---|---|---|
|
Samoilenko et al. [2019] Ukraine |
Cohort |
N = 36, F only Age: 18–32 yrs |
Total piercings: 37 Tongue: n = 22; Lip: n = 9 AWP: 24.11 ± 0.7 months |
Complications (total: n = 37) Pain 58.3%; Oedema 47.2%; Bleeding 11.1%; Dental fractures 35.1%; Gingival recession 29.7%; Mucosal atrophy 21.6%; Tooth sensitivity 19.4%; Plaque on piercing 43.2%; Longer barbell stem length cause greater recession and chipping |
Not reported |
Oral piercings were Associated damage to hard tissues, gingival recession, and soft tissue atrophy |
|
Domingo et al. [2019] Argentina |
Cohort | N = 16, (F: 10, M: 6); Age: 11–21 yrs |
Total piercings: n = 11 Lower lip n = 8; Upper lip n = 6; Tongue n = 4 AWP range: 5–48 months |
Lichenoid lesions on cheek and lip mucosa (n = 4); Elevated greyish lesions associated with metallosis on lip (n = 4); Mobility upper right molar and tearing at the piercing site (n = 4) | Cytological smears and EDS analysis showed: Aluminium (66.6%), Tungsten (5.5%), Molybdenum (2.7%) | Ion particles are released from metal piercings and may have caused the observed lesions |
|
Tomazevic et al. [2017] Slovenia |
Case Control |
Total: 45 Pierced group: n = 17 (F:15; M:2; Age: 22 yrs); Control group: n = 28 (F:22; M:6; Age: 22.4 yrs) |
Tongue piercing: n = 17 AWP: 31.8 months |
Complications from piercings (n = 17) Total Dental injuries: 76.5%; Enamel infractions: 23.5%; Enamel fracture: 58.8%; Enamel/dentine fracture: 5.9% |
Not reported | Subjects with tongue piercing have higher risks of dental injury including enamel fractures |
|
Simoes et al. [2014] Brazil |
Cross sectional | Total:82 (F:63; M: 19; Age: 14–30 yrs) |
Total piercings: n = 109 Lip: n = 55; Tongue: n = 28; Lingual frenum: n = 5; Labial frenum: n = 18; Cheek: n = 3 AWP: < 6 months: 24.8%; 6–12 months: 13.8%; > 12 to 24 months: 11.9%; > 24 months: 49.5% |
Gingival recession 39.4%; Changed sensation: 16%; Altered saliva: 13%; Dental fractures 11.9%; Lip depressions 9.2%; Mucosa depressions 2.6%; Inflammation 2.8%; Labial frenum oedema 1.8%; Keloid scar 1.8%; Tongue depression 0.9%; Lip hyperplasia 0.9%; Tooth mobility 0.9% | Not reported | Oral piercings were associated with complications involving hard and soft dental tissues with the most frequent complication being gingival recession |
|
Kapferer et al. [2012] Austria |
Cross sectional | Total: 47 (F: 34; M: 13; Age: 16–24 yrs) |
Lower lip labret piercing adjacent to first premolar: n = 5; Lower lip labret piercing adjacent to mandibular canine: n = 42 AWP: 37.3 ± 33.6months |
Mid-buccal recession (n = 4) with canine and first premolars most affected; Tooth chipping (n = 1); Plaque levels significantly higher in test than control; Hyperplastic tissue (4.3%) around the stud closure (n = 2) | Not reported | Lateral lower lip piercings were associated with significantly higher rates of buccal recession, tooth chipping and plaque accumulation |
|
Plessas et al. [2012] Greece |
Cohort | Total:110 (F: 58; M: 52; Age: 18–35 yrs) |
Total: 161 pierced sites Tongue: n = 51; Lip: n = 110 AWP: 30.3 months |
Self-reported complications (n = 110 subjects): Inflammation (n = 53); Gingival recession (n = 21); Dentine hypersensitivity (n = 21); Increased salivary flow (n = 15); Taste change (n = 11); Dental defects (n = 52); Soft tissue ulcer (n = 88); Tissue overgrowth (n = 12); Gingival recession (n = 64); GR defects with Miller Class II (n = 10); Biting piercing and caused dental defects (n = 43); Striking piercing and caused dental defects (n = 12) |
Not reported | Tongue and lip piercings caused increased dental defects, gingival recession, attachment loss and increased probing depths of teeth adjacent to pierced sites |
|
Ziebolz et al. (2012) Germany |
Case control |
Total: 92 (M only) Age: 21–22 yrs Test group: n = 46 Control group: n = 46 |
Tongue piercing: n = 46 AWP: 45.6 ± 36 months |
Complications (total = 46): Enamel cracks (n = 38); Enamel defects (n = 29); Gingival lingual recession 59% (n = 27) |
Not reported | Tongue piercing showed increased occurrence of enamel defects, enamel cracks and lingual recessions |
|
Vieira et al. [2011] Brazil |
Cohort | Total: 39 (F: 26; M: 13; Age: 18–24 yrs) |
Total piercings: n = 42 Tongue: n = 37; Upper lip: n = 1; Lower lip: n = 4 AWP: 15 months |
Complications (total = 42) Excessive bleeding (n = 29); Pain (n = 22); Syncope (n = 2); Swelling (n = 26); Parafunctional habits (n = 35); Tongue lacerations (n = 13); Palate traumas (n = 8); Gingival recessions (n = 2); Tooth fracture (n = 1) |
Not reported | Oral piercings caused mainly local complications related to soft and hard dental tissues |
|
Hickey et al. [2010] France |
Cohort | Total:201 (F: 146; M: 55; Age: 22.7 yrs) |
Tongue piercing n = 106; Lip piercing n = 55; Cheek piercing n = 7 AWP: 19.2 months |
Gingival recession 8.5%; Chipped teeth 6.9%; Tooth chipping 21.4%; Infection 3%; Swelling 51.7%; Sensitivity 1.5%; Taste disturbance 12.3%; Speaking discomfort 67%; Eating difficulty 78.3%; Difficulty swallowing 28.4%; Increased saliva 20.4% | Not reported | The occurrence of complications from oral piercings is high, and public education or awareness is needed |
|
Kapferer et al. [2010] Austria |
Cohort | Total:189 (F: 153; M: 36; Age: 13–36 yrs) |
Total: n = 210 Lip piercings: n = 130 Tongue piercings: n = 80 AWP:43.5 ± 33.1 months |
Early Complications: Mild pain (n = 124); Swelling (n = 70); Mild infection (n = 35); Speaking problem (n = 48); Problems eating (n = 99) Late Complications: Recurrent infection (n = 13); Gingiva recession (n = 45); Tooth chipping (n = 13); Tooth movement (n = 4) |
Not reported | Pain was the most common early complications. Late complications included gingival recession, tooth chipping and recurrent infections |
|
Lupi et al. [2010] Italy |
Case control |
Total: 30 Pierced tongue: (F: 12; M: 3; Age: 20–29 yrs) Control: (F: 12, M: 3; Age: 20–29 yrs) |
Tongue piercings: n = 15 AWP: 46.1 months |
Mucosal smears surrounding piercing body showed a copious and diffuse bacterial flora (n = 10); Fungi hyphae and spores located intercellularly (n = 3); Neutrophil infiltration (n = 5); Cytolysis of epithelial cells (n = 4) | Light and SEM: showed foreign metallic bodies in keratinocytes indicated ion release from piercings | Ion release from oral piercings may be related to direct toxic effects and delayed reactions of metal sensitisation |
|
Oberholzer et al. [2010] Australia |
Cohort | Total:250 (F: 195; M 55; Age range: 16–35 yrs) |
Tongue piercing Frenum piercings AWP: not stated |
Total subjects with piercings: n = 250 Tooth damage/chipping (n = 85); Gum problems (n = 40); Infections (n = 20); Soft tissue damage (n = 149) |
Not reported | Damage to hard dental tooth structure was the most common complication |
|
Pires et al. [2010] Brazil |
Case control |
Total:180; Age = 5–21 yrs) Control group: 120 (F: 77; M: 43; Tongue piercing: 60 (F 33; M 27) |
Tongue piercing: n = 60 AWP: 24 months (range: 25 months ± 2.84 months) |
Swelling (n = 11); Infection (n = 4); Inflammation (n = 4); Keloid formation (n = 1); Dental fracture (n = 12); Habit of biting piercing (n = 30); Tongue piercing have 11 times greater chance of gingival recession | Not reported | Tongue piercings were strongly associated gingival recession in the anterior lingual mandibular region compared to control |
|
Firoozmand et al. [2009] Brazil |
Cohort | N = 33; (F: 15; M: 18; Age: 14–18 yrs) |
Tongue piercings: n = 22; Lower lip: n = 10; Other: n = 3 AWP: NS |
Swallowing difficulty 2.6%; Fractured teeth 5.10%; Local inflammation 7.70%; Gingival recession 10.25%; Keloid formation 10.25%; Bacterial plaque 17.90%; Tongue fissure 20.50% | Not reported | Oral piercings were associated with local complications to gingiva and teeth |
|
Vilchez-Perez et al. [2009] Spain |
Cross sectional | N = 50 (F: 39; M:11; Age: 18–24 yrs) |
Total lip piercings: n = 76 Labret type: n = 58; Ring: n = 18 AWP: 35.4 months ± 19.5 |
Gingival recession (n = 17); Tooth fractures and cracks (n = 15); Mucosal alterations (n = 7); Hyperplastic tissues near piercing (n = 5); Greatest gingival recession around canine and first bicuspid teeth | Not reported | Lower lip piercings enhanced gingival recession and were associated with tooth fractures and cracks |
|
Ebrahim and Naidoo [2008] South Africa |
Cohort |
N = 126 (F: 107; M: 19; Age: 14–24 yrs) |
Tongue piercing: (n = 110); Lip piercing: (n = 16); Both tongue and lip:(n = 10) AWP: 37% piercing for > 2 yrs; 23% between 1 and 2 yrs; 17% for 6–12 months; 23% < 6 months |
Pain 69.05%; Swelling 52.38%; Difficulty eating, speaking and swallowing 70.63%; Irritation 33%; Taste changes 19%; Itchiness 10%; Chipped teeth 10.31% (n = 10); Gingival recession (n = 2) | Not reported | Tongue and/or lip piercings were associated with trauma to teeth and gums |
|
Slutzkey et al. [2008] Israel |
Cohort |
N = 303 (F: 177 M: 126; Age: 18–22 yrs) |
Tongue and lip piercing: NS; AWP: NS | Gingival recession (n = 9) | Not reported | Gingival recession amongst young adults was related to oral piercings |
|
Kapferer et al. 2007 Austria |
Case control |
N = 100; Age: 18–21 yrs Test: F: 50; M: 44; Control: F: 50; M = 6) |
Lower lip labret studs: n = 50 AWP: 39.4 ± 3.5 months |
Gingival recession 68%; Localised periodontitis 4% | Not reported | The prevalence of gingival recessions was associated with labial piercing |
|
López-Jornet, et al. [2006] Spain |
Cohort study | N = 97 (F: 68; M: 29; Age: 13–35 yrs) |
Tongue: n = 45; Lip: n = 52; Cheek: n = 1 AWP: 14.07 months |
Gingival recession (n = 23); Tooth damage (n = 13); Hypertrophy/atrophy (n = 9); Pain (n = 37); Swelling (n = 46); Bleeding (n = 8); Salivary flow (n = 14); Halitosis: (n = 4); Taste changes (n = 9) | Not reported | Labial piercing frequently caused gingival recession and damage to the periodontium |
|
López-Jornet, et al. [2006] Spain |
Cross sectional | N = 59 (F:48; M:11; Age = 13–25 yrs) |
Tongue: n = 17; Lip: n = 13 AWP: 0–3 months: 21%; 3 months to 1 year: 54%; > 1 year: 25% |
Pain (n = 3); Bleeding 24%; Gingival inflammation (n = 22), Gingival swelling (n = 8); Dental fractures or fissures/cracks (n = 6); Increased salivation (n = 6); Bad breath (n = 4); Metallic taste (n = 5) | Not reported | Tongue piercing was associated with pain, inflammatory reactions, and dental problems |
|
Dougherty et al. [2005] USA |
Case control |
N = 46; Mean age:23.9 yrs Control: F: 14; M:9 Test: F:14; M: 9 |
Tongue piercings n = 23 AWP = 40.32 years, |
Mandibular anterior teeth mobility (n = 2); Gingival recession (n = 9); Periodontal pocketing (n = 4); Broken teeth (n = 8); Radiographic calculus (n = 5) | Not reported | Wearing a tongue stud increases the risk of developing abnormalities in alveolar bone surrounding mandibular anterior teeth |
|
Kieser et al. [2005] New Zealand |
Cohort |
N = 43 (F: 40; M: 3 Age: 14–34 yrs) |
Tongue piercing: n = 33 Lip piercing: n = 15 Both tongue and lip: n = 5 |
Swelling/infection (n = 12); Pain (n = 6); Lymphadenopathy (n = 1); Abnormal tooth wear (n = 12); Gingival recession -Labial sites (n = 12); Lingual sites (n = 12) | Not reported | Oral piercings were associated with pain, swelling, localised gingival recession, and abnormal tooth wear |
|
Levin et al. [2005] Israel |
Cohort | N = 389 (F: 179; M: 210; Age: 18–24 yrs) |
Tongue: n = 39; Lip piercing: n = 8; Other: n = 32 AWP: 13.04 months (range 1–60 months |
After piercing complications: (total n = 79) Swelling (n = 41); Bleeding (n = 36); Fractured teeth (n = 11); Infection (n = 9); Gingival recessions (n = 21) |
Not reported | Swelling, bleeding, tooth fractures and gingival recessions were common complications |
|
Stead et al [2006] UK |
Cohort |
N = 145 Age:13–43 yrs |
Tongue piercing (n = 123) AWP:29 months |
Swelling (n = 120); Pain (n = 87), Difficulty eating (n = 81); Speech problems (n = 63); Bleeding (n = 53); Ingestion of jewellery (n = 42); Tooth fracture (n = 38); Plaque on jewellery (n = 37); enlarged piercing hole (n = 19) | Not reported | Tongue piercing may cause complications including swelling, pain, tooth damage and difficulty speaking and eating |
|
Campbell et al. [2002] USA |
Cross sectional | N = 52 (F: 21; M: 31; Age: 18–40 yrs) |
Tongue piercings: n = 52 AWP: 20 ± 24 months |
Mandibular central incisor lingual recession 50% (n = 26) Tooth chipping 47% in tongue piercing for 4 + years (n = 24) |
Not reported | Tongue piercing was associated with lingual recession of mandibular anterior teeth and chipping of posterior teeth |
F females, M males; AWP Average worn period, NS not specified
The majority of the studies included had more female participants than males, and only three studies had more male participants than females (Levin et al. 2005; Firoozmand et al. 2009; Campbell et al. 2002). One study examined only male participants (Ziebolz et al. 2012) and one study did not specify the gender distribution of subjects (Stead et al. 2006). In terms of the mean age of participants, the most common age was 22 years old (n = 6) and the youngest mean age was 14 years old (Domingo et al. 2019).
There were 7 studies that examined tongue piercings only, whilst 3 examined lip piercings only, and 15 studies examined both tongue and lip piercings (Table 2). Five studies examined piercings in other oral locations such as the cheek or frenum in addition to tongue and lip piercings. The average period that piercings were worn ranged between 5 and 48 months.
In terms of post-piercing oral complications, reported soft tissue problems included damage to gingival tissues, and mucosal changes, such as atrophy, hyperplasia or local lichenoid reactions. Hard tissue complications were tooth-related, such as fracture or chipping. Gingival recession was the most common soft tissue complication reported in 16 out of 25 studies. Tooth fracture or chipping was noted in 10 studies. Other commonly reported complications included: swelling (n = 9), pain (n = 8), infection (n = 6), bleeding (n = 6) and inflammation (n = 5). Alterations to speech, eating and/or swallowing were noted in five studies. Changes to taste, or a metallic taste were reported in five studies. Four studies reported mucosal changes or atrophy from oral piercings.
Most studies did not report complications resulting from metal ion release. Only two studies examined the direct effects of metal ion release on surrounding oral tissues (Domingo et al. 2019; Lupi et al. 2010). One study explored different piercing materials, such as titanium, stainless steel and Teflon, in terms of the rate of gingival recession and tooth chipping from these various types of oral piercings (Hickey et al. 2010).
When applying the JBI critical appraisal criteria for non-randomised experimental studies, 20 studies included both clinical examination and questionnaire-based data, and were rated as having good methodological quality (Levin et al. 2005; Firoozmand et al. 2009; Vieira et al. 2011; Kapferer et al. 2012; Vilchez-Perez et al. 2009; Domingo et al. 2019; Lupi et al. 2010; Campbell et al. 2002; Ziebolz et al. 2012; Dougherty et al. 2005; Kapferer et al. 2007; Kieser et al. 2005; Lopez-Jornet and Camacho-Alonso 2006; Lopez-Jornet et al. 2006; Oberholzer et al. 2010; Pires et al. 2010; Plessas et al. 2012; Samoilenko et al. 2019; Slutzkey et al. 2008; Tomaževič et al. 2017). Five studies were rated as having low quality methodology (Kapferer et al. 2010; Simoes et al. 2014; Stead et al. 2006; Hickey et al. 2010; Ebrahim et al. 2008). Four of these studies used only self-reported questionnaire data and no clinical examinations were undertaken (Kapferer et al. 2010; Stead et al. 2006; Hickey et al. 2010; Ebrahim et al. 2008). Reported risk bias for the included studies is provided in the supplemental data.
Discussion
This systematic review aimed to examine the incidence of hard (teeth) and soft tissue complications relating to oral piercings, with a particular focus on complications caused by metal ion release. To the author’s knowledge, this is the first systematic review that examines metal ion release from oral piercings and the subsequent complications. The results of this review showed that metal ion release can occur from oral piercings when subject to the oral environment. They may corrode and release metal ions into surrounding oral tissues, causing local soft tissue reactions. Oral piercings are made from a variety of metals, such as surgical stainless steel, titanium, platinum, or gold, as mentioned above (Masood et al. 2023). Two included studies examining metal ion release investigated piercings made from surgical stainless steel only (Domingo et al. 2019; Lupi et al. 2010). Stainless steel piercings were found to cause a high incidence of tooth chipping (Hickey et al. 2010). One study that examined different oral piercing materials showed that titanium piercings cause greater gingival recession (Hickey et al. 2010). Teflon or acrylic piercings showed lower levels of dental complications, and the change in composition avoided the problem of metal allergy (Hickey et al. 2010; Dougherty et al. 2005).
Complications caused by metal ion release were reported by two studies (Domingo et al. 2019; Lupi et al. 2010); Domingo et al. (2019) examined both lip and tongue piercings, and reported the presence of metal particles, such as aluminium, tungsten and molybdenum, in keratinocytes at sites where the oral mucosa was pierced. Lupi et al. (2010) investigated only tongue piercings, and noted concentrations of iron, nickel, and chromium in tongue mucosal keratinocytes. These metal ions may exert local cytotoxic effects on keratinocytes (Lupi et al. 2010), which may result in local mucosal changes, such as atrophic, “hyperplastic, leukoedematous, erythematous, and/or erosive lesions” (Domingo et al. 2019). Interestingly, the rate of metal ion release is also influenced the surface quality of the piercings, where surface defects can be a site of metal corrosion (Masood et al. 2023; Domingo et al. 2019); Domingo et al. (2019) noted surface defects on both used and unused piercings.
Of the 25 articles included for analysis, there were no articles published prior to 2002 that examined lip or tongue piercings and related dental complications. The majority of the included studies had more female participants than males, indicated a higher prevalence of oral piercings in females (Walsh et al. 2008; Dougherty et al. 2005; Kapferer et al. 2007; Samoilenko et al. 2019; Simoes et al. 2014; Tomaževič et al. 2017). There may also be a higher willingness of females to participate in studies, and they may seek oral health input more readily than males (Dougherty et al. 2005; Kapferer et al. 2007).
The included studies generally reported that tongue piercings cause significantly more dental complications than lip piercings (Ebrahim et al. 2008). Pain, difficulty speaking and eating problems were reported more often with tongue piercings (Kapferer et al. 2010; Firoozmand et al. 2009; Vieira et al. 2011). These were similar findings to the 2022 systematic review by Passos et al. Immediately after piercing placement, common complications included pain, swelling, bleeding and irritation (Kapferer et al. 2007; Samoilenko et al. 2019; Ebrahim et al. 2008). One study showed that 86% of subjects with oral piercings experienced these complications (Kapferer et al. 2007). Pain was reported to occur in between 58.3 and 69% of cases and swelling in between 47.2 and 52% of cases (Kapferer et al. 2007; Samoilenko et al. 2019). Furthermore, mucosal changes were reported in 6 of the 25 studies included for analysis. Atrophy or de-papillation around the oral piercing was the most common mucosal change with tongue piercings (Oberholzer et al. 2010). Hyperplasia or tissue overgrowth at the pierced site was seen mainly in tongue piercings, at a prevalence of 16.2% to 33.3% (Vieira et al. 2011; Samoilenko et al. 2019). Complete resolution was achieved when the piercings were removed (Vieira et al. 2011).
Most studies showed that tongue piercings are associated with tooth injuries such as chipping or fractures (Firoozmand et al. 2009; Ziebolz et al. 2012; Oberholzer et al. 2010). The study by Tomaževič et al. (2017) showed that dental damage of any type, such as enamel fractures, enamel–dentin fractures, and complicated crown–root fracture, occurred twice as frequently in people with tongue piercings (76.5%) compared to community controls (32.1%). About 59% of people with tongue piercings had enamel fractures (Tomaževič et al. 2017). The majority of teeth with enamel damage (92%) were molars and premolars (Campbell et al. 2002). This may be explained by the habit of patients playing with, biting, or knocking the piercing against their teeth (Campbell et al. 2002). Of subjects with fractured teeth, this habit of playing with the piercing was noted in some 51.6% of cases (Hickey et al. 2010).
Lip or labial piercings cause more gingival recession (Kapferer et al. 2010; Firoozmand et al. 2009; Kapferer et al. 2012; Vilchez-Perez et al. 2009; Plessas et al. 2012). As such, labial piercings have been shown to be more damaging to periodontal tissues (Kieser et al. 2005; Lopez-Jornet and Camacho-Alonso 2006; Slutzkey et al. 2008). In contrast, Pires et al. (2010) noted that subjects with tongue piercings are at 11 times increased risk of developing lingual anterior gingival recession. This is supported by Dougherty et al. (2005) who reported that tongue piercings were commonly associated with the presence of calculus, which may lead to higher levels of periodontal disease. The systematic review and meta-analysis by Passos et al. showed that 33% of individuals with oral piercings had gingival recession. The problem of gingival recession is primarily related to the position of the piercing. Studies examining this issue showed that piercings placed at the CEJ caused a greater rate of buccal gingival recessions, (Kapferer et al. 2007) whilst lip piercings placed coronally to the CEJ had a lower incidence of lower lip buccal recession (Kapferer et al. 2012). This important finding regarding piercing placement is something which body piercing professionals should consider when advising patients about possible long-term complications.
The rate of oral complications may be related to piercing length and the wear period. The barbell rod or stem length on tongue piercings appears to be directly proportional to the risks of gingival recession and tooth chipping (Campbell et al. 2002). Longer stems cause more recession due to the greater ease of the barbell piercing coming into direct contact with the gingival tissues (Campbell et al. 2002; Hickey et al. 2010). Similarly, several studies also reported a higher prevalence of gingival recession and tooth chipping with longer wear periods (Campbell et al. 2002; Plessas et al. 2012; Ebrahim et al. 2008). Interestingly, one study found that the greatest incidence of complications occurred within 2 years and involved 57.6% of cases (Lopez-Jornet and Camacho-Alonso 2006).
Multiple studies reported limitations to their study design. The main limitation reported was convenience sampling, where the participants were recruited specifically for participation in the study (Stead et al. 2006; Dougherty et al. 2005; Kieser et al. 2005; Ebrahim et al. 2008). Some studies did not have a control group (Domingo et al. 2019; Plessas et al. 2012), which prevents comparisons with the experimental group. Lastly, the majority of studies included a questionnaire in the study design, with four studies relying solely on the information collected from the survey to draw conclusions (Kapferer et al. 2010; Stead et al. 2006; Hickey et al. 2010; Ebrahim et al. 2008). Memory bias is a key limitation that may influence the results from questionnaire-based studies (Stead et al. 2006; Kapferer et al. 2007; Pires et al. 2010). Despite these limitations, the included studies have a consistent and recurring message that oral piercings frequently cause hard and soft tissue complications. Thus, education of patients and increasing their awareness of these risks is imperative, and a key responsibility of healthcare professionals.
Conclusion
The findings of the present systematic review evaluating the oral complications associated with metal ion release from oral piercings reveal the following:
Oral piercings are associated with complications involving hard and soft dental tissues.
Oral piercings leach metal ions into surrounding tissues which may cause local mucosal changes.
Additionally, the evaluated studies showed that tongue piercings are commonly associated with tooth fractures, whilst lip piercings result in a greater incidence of gingival recession.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
SZ and LJW conceived the idea; MM and SZ screened the papers; MM collected and analysed the data; MM drafted the paper and SZ and LJW revised it. All authors approved the final version and agreed to be accountable for all aspects of the study.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Data availability
Data and material the data used for this research can be made available upon request to the authors.
Declarations
Conflict of interest
The authors declare they have no financial conflict of interests related to this study.
Ethical approval
N/A.
Consent to participate
N/A.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Campbell A, Moore A, Williams E, Stephens J, Tatakis DN. Tongue piercing: impact of time and barbell stem length on lingual gingival recession and tooth chipping. J Periodontol. 2002;73(3):289–297. doi: 10.1902/jop.2002.73.3.289. [DOI] [PubMed] [Google Scholar]
- Chadwick BL, Groves G, Dransfield K. Orofacial piercings: perceptions of dental practitioners and piercing parlours. Prim Dent Care. 2005;12(3):83–88. doi: 10.1308/1355761054348477. [DOI] [PubMed] [Google Scholar]
- Covello F, Salerno C, Giovannini V, Corridore D, Ottolenghi L, Vozza I. Piercing and oral health: a study on the knowledge of risks and complications. Int J Environ Res Public Health. 2020;17(2):1–8. doi: 10.3390/ijerph17020613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domingo MG, Ferrari L, Aguas S, et al. Oral exfoliative cytology and corrosion of metal piercings. Tissue Implications Clin Oral Investig. 2019;23(4):1895–1904. doi: 10.1007/s00784-018-2626-4. [DOI] [PubMed] [Google Scholar]
- Dougherty SL, Tervort-Bingham K. Assessment of the alveolar bone surrounding the mandibular anterior teeth of individuals wearing a tongue stud. J Dent Hyg. 2005;79(4):1–9. [PubMed] [Google Scholar]
- Ebrahim R, Naidoo S. Oral and perioral piercings in Tshwane. Sth Afr Dent J. 2008;63(5):288–291. [PubMed] [Google Scholar]
- Firoozmand LM, Paschotto DR, Almeida JD. Oral piercing complications among teenage students. Oral Health Prev Dent. 2009;7(1):77–81. [PubMed] [Google Scholar]
- Hennequin-Hoenderdos NL, Slot DE, Van der Weijden GA. The incidence of complications associated with lip and/or tongue piercings: a systematic review. Int J Dent Hyg. 2016;14(1):62–73. doi: 10.1111/idh.12118. [DOI] [PubMed] [Google Scholar]
- Hickey BM, Schoch EA, Bigeard L, Musset AM. Complications following oral piercing. A study among 201 young adults in Strasbourg. France. Community Dent Health. 2010;27(1):35–40. [PubMed] [Google Scholar]
- Inchingolo F, Tatullo M, Abenavoli FM, et al. Oral piercing and oral diseases: a short time retrospective study. Int J Med Sci. 2011;8(8):649–652. doi: 10.7150/ijms.8.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapferer I, Beier US. Lateral lower lip piercing - prevalence of associated oral complications: a split-mouth cross-sectional study. Quintessence Int. 2012;43(9):747–752. [PubMed] [Google Scholar]
- Kapferer I, Benesch T, Gregoric N, Ulm C, Hienz SA. Lip piercing: prevalence of associated gingival recession and contributing factors. A Cross-Sectional Study J Periodontal Res. 2007;42(2):177–183. doi: 10.1111/j.1600-0765.2006.00931.x. [DOI] [PubMed] [Google Scholar]
- Kapferer I, Berger K, Stuerz K, Beier US. Self-reported complications with lip and tongue piercing. Quintessence Int. 2010;41(9):731–737. [PubMed] [Google Scholar]
- Kieser JA, Thomson WM, Koopu P, Quick AN. Oral piercing and oral trauma in a New Zealand sample. Dent Traumatol. 2005;21(5):254–257. doi: 10.1111/j.1600-9657.2005.00319.x. [DOI] [PubMed] [Google Scholar]
- Levin L, Zadik Y, Becker T. Oral and dental complications of intra-oral piercing. Dent Traumatol. 2005;21(6):341–343. doi: 10.1111/j.1600-9657.2005.00395.x. [DOI] [PubMed] [Google Scholar]
- López-Jornet P, Navarro-Guardiola C, Camacho-Alonso F, Vicente-Ortega V, Yánez-Gascon J. Oral and facial piercings: a case series and review of the literature. Int J Dermatol. 2006;45(7):805–809. doi: 10.1111/j.1365-4632.2006.02743.x. [DOI] [PubMed] [Google Scholar]
- Lopez-Jornet P, Camacho-Alonso F. Oral and dental complications of intra-oral piercing. J Adolesc Health. 2006;39(5):767–769. doi: 10.1016/j.jadohealth.2006.04.006. [DOI] [PubMed] [Google Scholar]
- Lupi S, Zaffe D, Baena RR, Rizzo S, Botticelli A. Cytopathological and chemico-physical analyses of smears of mucosa surrounding oral piercing. Oral Dis. 2010;16(2):160–166. doi: 10.1111/j.1601-0825.2009.01613.x. [DOI] [PubMed] [Google Scholar]
- Masood M, Walsh LJ, Zafar S. Ion release from oral piercings from in vitro acidic challenges. Aust Dent J. 2023 doi: 10.1111/adj.12954. [DOI] [PubMed] [Google Scholar]
- Oberholzer TG, George R. Awareness of complications of oral piercing in a group of adolescents and young South African adults. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110(6):744–747. doi: 10.1016/j.tripleo.2010.07.012. [DOI] [PubMed] [Google Scholar]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passos PF, Pintor AVB, Marañón-Vásquez GA, Campos T, Abrahão AC, Ferreira DMT, et al. Oral manifestations arising from oral piercings: a systematic review and meta-analyses. Oral Surg Oral Med Oral Pathol Oral Radiol. 2022;134:327–341. doi: 10.1016/j.oooo.2022.04.051. [DOI] [PubMed] [Google Scholar]
- Pires IL, Cota LO, Oliveira AC, Costa JE, Costa FO. Association between periodontal condition and use of tongue piercing: a case-control study. J Clin Periodontol. 2010;37(8):712–718. doi: 10.1111/j.1600-051X.2010.01584.x. [DOI] [PubMed] [Google Scholar]
- Plessas A, Pepelassi E. Dental and periodontal complications of lip and tongue piercing: prevalence and influencing factors. Aust Dent J. 2012;57(1):71–78. doi: 10.1111/j.1834-7819.2011.01647.x. [DOI] [PubMed] [Google Scholar]
- Porritt K, Gomersall J, Lockwood C. JBI’s systematic reviews: study selection and critical appraisal. Am J Nurs. 2014;114(6):47–52. doi: 10.1097/01.NAJ.0000450430.97383.64. [DOI] [PubMed] [Google Scholar]
- Samoilenko A, Orishchenko VY, Strelchenia T, Strelchenia O. Oral piercing is a new challenge in the dentistry. Medicni Perspektivi. 2019;24(4):133–144. doi: 10.26641/2307-0404.2019.4.189605. [DOI] [Google Scholar]
- Simões A, Manso MC, Almeida RFD, Pinho MM. Prevalence of complications associated with oral piercing placement. Revista Portuguesa De Estomatologia, Medicina Dentaria e Cirurgia Maxilofacial. 2014;55(4):243–249. doi: 10.1016/j.rpemd.2014.10.003. [DOI] [Google Scholar]
- Slutzkey S, Levin L. Gingival recession in young adults: occurrence, severity, and relationship to past orthodontic treatment and oral piercing. AJODO. 2008;134(5):652–656. doi: 10.1016/j.ajodo.2007.02.054. [DOI] [PubMed] [Google Scholar]
- Stead LR, Williams JV, Williams AC, Robinson CM. An investigation into the practice of tongue piercing in the South West of England. Br Dent J. 2006;200(2):103–107. doi: 10.1038/sj.bdj.4813150. [DOI] [PubMed] [Google Scholar]
- Tomaževič T, Gašperšič R, Kosem R. Occurrence of dental injuries and periodontal complications in tongue-piercing jewellery users. Oral Health Prev Dent. 2017;15(3):293–297. doi: 10.3290/j.ohpd.a38530. [DOI] [PubMed] [Google Scholar]
- Vieira EP, Ribeiro AL, Pinheiro Jde J, Alves Sde M, Jr. Oral piercings: immediate and late complications. J Oral Maxillofac Surg. 2011; 69 (12): 3032-7. doi: 10.1016/j.joms.2010.12.046 [DOI] [PubMed]
- Vilchez-Perez MA, Fuster-Torres MA, Figueiredo R, Valmaseda-Castellón E, Gay-Escoda C. Periodontal health and lateral lower lip piercings: a split-mouth cross-sectional study. J Clin Periodontol. 2009;36(7):558–563. doi: 10.1111/j.1600-051X.2009.01431.x. [DOI] [PubMed] [Google Scholar]
- Vozza I, Fusco F, Bove E, Ripari F, Corridore D, Ottolenghi L. Awareness of risks related to oral piercing in Italian piercers. Pilot study in Lazio region. Ann Stomatol (roma) 2014;5(4):128–130. [PMC free article] [PubMed] [Google Scholar]
- Walsh LJ. Missing the point: the risks of intra-oral piercing. Australas Dent Pract. 2008;19(4):156–158. [Google Scholar]
- Ziebolz D, Stuehmer C, van Nüss K, Hornecker E, Mausberg RF. Complications of tongue piercing: a review of the literature and three case reports. J Contemp Dent Pract. 2009;10(6):E065–E071. [PubMed] [Google Scholar]
- Ziebolz D, Hildebrand A, Proff P, Rinke S, Hornecker E, Mausberg RF. Long-term effects of tongue piercing - a case control study. Clin Oral Investig. 2012;16(1):231–237. doi: 10.1007/s00784-011-0510-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data and material the data used for this research can be made available upon request to the authors.