Abstract
Introduction
Healthcare workers risk of exposure to the influenza virus in their work, is a high-risk group for flu infections. Thus WHO recommends prioritizing flu vaccination for them–an approach adopted by >40 countries and/or regions worldwide.
Methods
Cross-sectional studies on influenza vaccination rates among healthcare workers were collected from PubMed, EMBASE, CNKI, and CBM databases from inception to February 26, 2023. Influenza vaccination rates and relevant data for multiple logistic regression analysis, such as odds ratios (OR) and 95% confidence intervals (CI), were extracted.
Results
A total of 92 studies comprising 125 vaccination data points from 26 countries were included in the analysis. The meta-analysis revealed that the overall vaccination rate among healthcare workers was 41.7%. Further analysis indicated that the vaccination rate was 46.9% or 35.6% in low income or high income countries. Vaccination rates in the Americas, the Middle East, Oceania, Europe, Asia, and Africa were 67.1, 51.3, 48.7, 42.5, 28.5, and 6.5%, respectively. Influencing factors were age, length of service, education, department, occupation, awareness of the risk of influenza, and/or vaccines.
Conclusion
The global influenza vaccination rate among healthcare workers is low, and comprehensive measures are needed to promote influenza vaccination among this population.
Systematic review registration
www.inplysy.com, identifier: 202350051.
Keywords: influenza vaccine, vaccination rate, healthcare workers, influencing factors, meta-analysis
Introduction
The World Health Organization (WHO) reports that the flu causes 3 to 5 million severe cases and contributes to 290,000 to 650,000 respiratory disease-related deaths globally p.a (1). Thus flu imposes a substantial impact on both public health and the economy, i.e., the flu resulted in 145,000 deaths, 9.459 million hospitalizations, and 81.536 million hospitalization days due to lower respiratory tract infections (LRTIs), with the flu accounting for 11.5% of LRTI cases in 2017 (2). This aligns with that indirect costs accounted for 88% of the overall economic burden of flu in the 18–64 age group, with 75% of direct costs attributed to hospitalization. Additionally, the costs associated with flu increase with age and the presence of underlying diseases within the 18–64 age group (3).
Annual flu vaccination is widely recognized as an effective preventive measure against the flu. Evidence from a systematic review of randomized controlled trials indicates that inactivated flu vaccines administered to healthy adults can prevent 59% of laboratory-confirmed flu cases, furthermore, when the vaccine strains closely match the circulating flu virus strains, it has been shown to reduce the incidence of influenza-like illness (ILI) by 42% (4).
Healthcare workers face a significant risk of exposure to the flu virus in their daily work, making them a high-risk group for flu infections. A meta-analysis revealed that the incidence of lab-confirmed flu among non-vaccinated healthcare workers was 18.7%, which is 3.4 times higher than the rate observed in healthy adults (5). When healthcare workers contract the flu, it can lead to heightened absenteeism, causing disruptions in medical services and a greater risk of hospital-acquired infections. Furthermore, continuing to work while infected can potentially facilitate the transmission of the flu to other individuals, particularly their family members.
Influenza vaccination is the most significant prevention measure. Recognizing the importance of protecting healthcare workers and preventing the spread of flu, WHO recommends that healthcare workers be given priority for flu vaccination. This recommendation has been adopted by over 40 countries and regions worldwide. However, vaccination coverage exhibited significant variations from one country to another (6), and in some instances, it was notably low (7). In this current systematic review, our objective is to examine the influenza vaccination rates among healthcare workers and the factors that impact their adherence to flu vaccination.
Methods
Study type
This meta-analysis included cross-sectional studies that reported the seasonal influenza vaccination rate among healthcare workers.
Study population
The study population consisted of healthcare workers and healthcare professionals directly involved in providing health services globally.
Outcome measures
The primary outcome measure of interest was the seasonal influenza vaccination rate, which was defined as the percentage of vaccinated individuals among the total survey population.
Inclusion criteria
To be included in this meta-analysis, studies had to meet the following criteria:
Studies reporting the seasonal influenza vaccination rate among healthcare workers and/or its influencing factors.
The study population included healthcare workers and healthcare professionals directly involved in providing health services globally.
Studies provided specific information on sample size, vaccination rates, and the number of vaccinated individuals within a given year.
Studies were published in either Chinese or English.
The study design was cross-sectional.
Exclusion criteria
The following criteria were used to exclude studies from this meta-analysis:
Studies reporting on types of influenza vaccines other than seasonal influenza vaccines.
Studies that did not report key data such as sample size, vaccination rates, and the number of vaccinated individuals, or studies that did not specify the vaccination year or only reported combined vaccination rates for multiple years.
Studies that focused solely on healthcare institutions or the overall population of a country, without specific data on healthcare workers.
Duplicate publications, where the same study was published in multiple sources.
Studies with logical errors or inconsistencies in the reported data.
Literature search strategy
Computer-based searches were performed in multiple databases, including PubMed, EMBASE, CNKI, CBM, Wanfang, and VIP. The search aimed to identify cross-sectional studies that reported the seasonal influenza vaccination rate among healthcare workers. The search was conducted from the inception of each database up to February 26, 2023. The search strategy utilized a combination of subject terms and free-text terms, Search, terms like “Influenza Vaccine*,” “Flu Vaccine*,” “Influenza Virus Vaccine*,” “Universal Influenza Vaccine*,” “Universal Flu Vaccine*,” “Immunization Coverage*” and “Vaccination Coverage*” were utilized. This comprehensive search strategy was designed to capture relevant studies and gather a wide range of literature on the seasonal influenza vaccination rate among healthcare workers (Supplementary Table S1).
Literature screening and data extraction
The identified literature was imported into Endnote literature management software, and duplicate records were removed. Two researchers independently screened the literature and performed data extraction. In cases of discrepancies, a third senior researcher was consulted for discussion and to reach a consensus. Initially, the title and abstract of each article were reviewed to exclude obviously irrelevant studies. Subsequently, the full text of the remaining articles was thoroughly examined to determine their eligibility for inclusion in the meta-analysis.
Data extraction encompassed various key aspects, including the first author’s name, publication year, survey region, sampling location, study population, vaccination time, sample size, number of vaccinated individuals, and relevant data from multiple logistic regression analysis, such as odds ratios (ORs), 95% confidence intervals (CIs), and reference objects. This rigorous screening and data extraction process ensured that relevant and reliable information was obtained from the selected studies for further analysis.
Evaluation of bias risk in included studies
To assess the methodological quality of the included cross-sectional studies, a checklist was developed based on recommended guidelines. This checklist incorporated items from the cross-sectional study quality evaluation tool endorsed by the Agency for Healthcare Research and Quality (AHRQ) and the JBI Analytic Cross-Sectional Study Quality Evaluation Scale.
The checklist consisted of nine key items aimed at evaluating the potential biases in the included studies. These items included:
Clearly stating the source of data (e.g., survey, literature review).
Clearly defining the inclusion criteria for the study population.
Providing detailed descriptions of the study population and study site.
Offering an explanation for the exclusion of certain study subjects from the analysis.
Summarizing the patient response rate and data collection completeness.
Explaining how missing data was handled during the analysis if the research data was incomplete or had missing values.
Describe how confounding was assessed and/or controlled.
Whether to use effective and credible methods to measure outcome indicators.
Whether the data analysis method is appropriate.
By systematically assessing these aspects, the checklist enabled a comprehensive evaluation of the methodological quality of the cross-sectional studies. This evaluation helped to identify any potential biases that may have influenced the study results and ensured the reliability of the findings.
Data analysis
The data extraction and analysis were performed using Excel 2016 and STATA 12.0 software. To assess publication bias, Egger’s test and funnel plot were utilized. A significance level of 0.05 or 0.01 was considered statistically significant. Given the anticipated heterogeneity, a random-effects model was employed for the analysis. Sensitivity analysis was conducted to assess the robustness and reliability of the overall vaccination rate estimate. Additionally, subgroup analysis was performed to explore potential sources of heterogeneity.
For the analysis of vaccination rates, the formula used was as follows:
Influenza vaccine vaccination rate = number of vaccinators / sample size.
The standard error of the rate was calculated using the formula:
Standard error of rate = sqrt (rate × (1-rate) / sample size).
When adequate data were available from the included articles, the random effects model was utilized to estimate the odds ratios (OR) of the influencing factors. This approach allowed for a comprehensive assessment of the relationship between the influencing factors and the vaccination rates.
These analytical methods were employed to ensure a comprehensive evaluation of the data and to derive reliable and robust outcomes from the study. By utilizing these methods, we aimed to provide accurate and valid insights into the influencing factors of influenza vaccination rates among healthcare workers.
Results
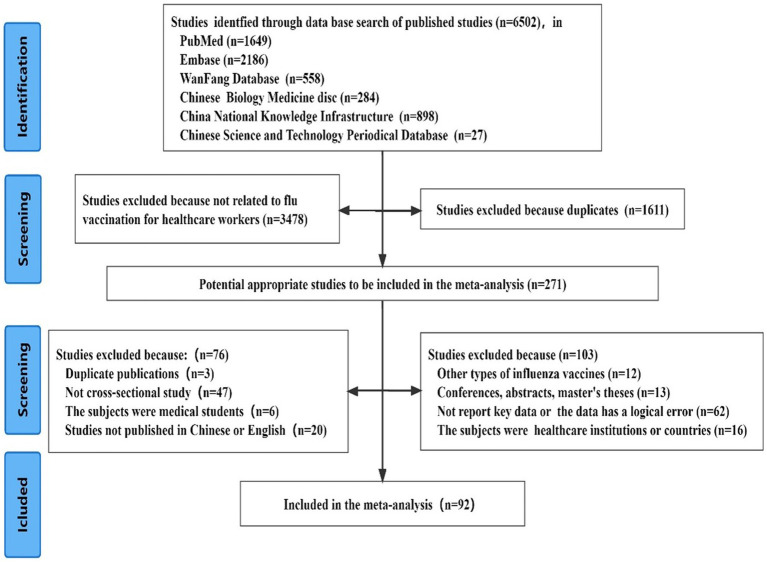
During the literature screening process
A comprehensive search of relevant articles yielded a total of 6,502 records. Following the screening process, 92 cross-sectional studies were considered eligible for inclusion in the analysis. The detailed process and results of the literature screening are presented in Figure 1. These 92 studies encompassed 125 data points on influenza vaccination, with sample sizes ranging from 106 to 8,975 participants. The reported vaccination rates varied between 3.1 and 99.6%. The studies were conducted in 26 countries across Asia, Europe, the Americas, Africa, Oceania, and the Middle East, providing a diverse geographical representation.
Figure 1.
The detailed process and results of the literature screening.
It is summarized that the key characteristics of the included studies, including their basic information and vaccination data (Table 1). The evaluation of literature quality resulted in an average score of 7.86 points. Among the included articles, one was rated as low-quality, 30 as medium-quality, and 61 as high-quality studies.
Table 1.
Basic information of literatures of included studies.
| Study | Sampling location | Population | Vaccination time | Study region | Sample size | Vaccination population | Quality score |
|---|---|---|---|---|---|---|---|
| Sheng et al. (8) | Internet survey | Nurses | 2017 | Mainland China | 773 | 31 | 8 |
| Liu et al. (9) | Community health centers | All HCWs | 2018 | Mainland China | 1,359 | 424 | 9 |
| Wang et al. (10) | Hospital | All HCWs | 2012 | Mainland China | 569 | 171 | 9 |
| Gao et al. (11) | Hospital | All HCWs | 2013 | Mainland China | 369 | 51 | 8 |
| Liu et al. (12) | Hospital | Nurses | 2018 | Mainland China | 299 | 68 | 9 |
| Yang and Chen (13) | Hospital | Nurses | 2013 | Mainland China | 650 | 284 | 9 |
| Gan et al. (14) | Community health centers | All HCWs | 2018 | Mainland China | 106 | 24 | 9 |
| Wang (15) | Hospital | All HCWs | 2007 | Mainland China | 199 | 15 | 6 |
| Bu et al. (16) | Hospital | All HCWs | 2012 | Mainland China | 1,521 | 98 | 8 |
| Yang et al. (17) | Hospital | All HCWs | 2016 | Mainland China | 1941 | 107 | 9 |
| Wang et al. (18) | Internet survey | Nurses | 2017 | Mainland China | 510 | 16 | 8 |
| Zhang et al. (19) | Hospital | All HCWs | 2017 | Mainland China | 943 | 131 | 9 |
| Kong et al. (20) | Hospital/Community health centers /CDC | All HCWs | 2019 | Mainland China | 8,975 | 2,241 | 9 |
| Ma et al. (21) | Hospital | All HCWs | 2017 | Mainland China | 3,260 | 226 | 8 |
| Gan et al. (22) | Influenza sentinel surveillance hospital/Hospital | All HCWs | 2018 | Mainland China | 1,412 | 237 | 8 |
| James et al. (23) | Hospital | All HCWs | 2016 | Sierra Leone | 706 | 46 | 8 |
| Liu et al. (24) | Internet survey | All HCWs | 2018 | Mainland China | 4,078 | 472 | 9 |
| Hosamirudsari et al. (25) | Hospital | All HCWs | 2015 | Iran | 378 | 218 | 7 |
| Alhammadi et al. (26) | Hamad Medical Corporation | All HCWs | 2013 | Qatar | 230 | 151 | 9 |
| Boey et al. (27) | Hospital/Nursing homes | All HCWs | 2014 | Belgium | 450 | 334 | 9 |
| Barbadoro et al. (28) | National Health Surveys. | All HCWs | 2012 | Italy | 5,336 | 1,110 | 6 |
| Wong et al. (29) | Hospital | Nurses | 2017 | Hong Kong | 708 | 309 | 5 |
| Kyaw et al. (30) | Hospital | All HCWs | 2015 | Singapore | 3,873 | 3,191 | 9 |
| Rabensteiner et al. (31) | Health Service | All HCWs | 2015 | Italy | 4,091 | 425 | 9 |
| Garcell and Ramirez (32) | Hospital | All HCWs | 2012 | Qatar | 325 | 231 | 6 |
| Esposito et al. (33) | University Hospital | All HCWs | 2006 | Italy | 2,143 | 432 | 9 |
| Hudu et al. (34) | Hospital | All HCWs | 2013 | Malaysia | 527 | 271 | 7 |
| Costantino et al. (35) | University | Medical residents | 2011 | Italy | 2,506 | 299 | 9 |
| Jimenez-Garcia et al. (36) | National Health Surveys. | All HCWs | 2003 | Spain | 518 | 102 | 8 |
| Von Perbandt et al. (37) | Hospital | All HCWs | 2014 | Switzerland | 200 | 30 | 8 |
| Haridi et al. (38) | Medical City | All HCWs | 2014 | Saudi Arabia | 447 | 394 | 9 |
| Sočan et al. (39) | Slovenian Medical Chamber | Physicians and dentists | 2009 | Slovenia | 1718 | 890 | 8 |
| Domínguez et al. (40) | Healthy primary facilities | All HCWs | 2011 | Spain | 1749 | 887 | 9 |
| Rehmani and Memon (41) | Hospital | All HCWs | 2008 | Saudi Arabia | 512 | 176 | 9 |
| Kan et al. (42) | Hospital | Nurses | 2011 | Mainland China | 895 | 295 | 9 |
| Kent et al. (43) | Public Health Directorates | All HCWs | 2007 | America | 1,203 | 871 | 9 |
| Hagemeister et al. (44) | Hospital | All HCWs | 2012 | Germany | 675 | 286 | 7 |
| Castilla et al. (45) | Hospital | All HCWs | 2008 | Spain | 1965 | 1,203 | 8 |
| Ball et al. (46) | National opt-in Internet panels | All HCWs | 2012 | America | 1944 | 1,400 | 7 |
| Black et al. (47) | National opt-in Internet panels | All HCWs | 2013 | America | 1882 | 1,415 | 7 |
| Black et al. (48) | National opt-in Internet panels | All HCWs | 2014 | America | 1914 | 1,480 | 7 |
| Black et al. (49) | National opt-in Internet panels | All HCWs | 2015 | America | 2,258 | 1784 | 7 |
| Black et al. (50) | National opt-in Internet panels | All HCWs | 2016 | America | 2,438 | 1916 | 7 |
| Black et al. (51) | National opt-in Internet panels | All HCWs | 2017 | America | 2,265 | 1776 | 7 |
| CDC (52) | National opt-in Internet panels | All HCWs | 2010 | America | 1931 | 1,226 | 7 |
| Ball at al. 2012 (53) | National opt-in Internet panels | All HCWs | 2011 | America | 2,348 | 1,571 | 7 |
| Tanguy et al. (54) | Hospital | All HCWs | 2009 | France | 532 | 119 | 5 |
| Amodio et al. (55) | University Hospital | Medical residents | 2009 | Italy | 202 | 44 | 8 |
| Hakim et al. (56) | Hospital | All HCWs | 2018 | Egypt | 3,534 | 1,087 | 9 |
| Hussain et al. (57) | Hospital | All HCWs | 2013 | Canada | 896 | 654 | 7 |
| Tagajdid et al. (58) | Hospital | All HCWs | 2011 | Morocco | 721 | 122 | 6 |
| Dorribo et al. (59) | University Hospital | All HCWs | 2009 | Switzerland | 472 | 245 | 9 |
| Bazán et al. (60) | Hospital/Health centers | All HCWs | 2010 | Peru | 672 | 544 | 9 |
| Yi et al. (61) | Internet survey | All HCWs | 2019 | Mainland China | 4,366 | 2,927 | 8 |
| Sánchez-Payá et al. (62) | University Hospital | All HCWs | 2010 | Spain | 3,126 | 762 | 8 |
| Yu et al. (63) | Internet survey | Nurses | 2017 | Mainland China | 4,153 | 257 | 8 |
| Groenewold et al. (64) | Nursing homes | Nurses | 2004 | America | 2,873 | 107 | 6 |
| Hajiabdolbaghi et al. (65) | Hospital | All HCWs | 2019 | Iran | 637 | 189 | 5 |
| Dubnov et al. (66) | Hospital | All HCWs | 2004 | Israel | 256 | 42 | 7 |
| Buxmann et al. (67) | Hospital | All HCWs | 2016 | Germany | 124 | 49 | 9 |
| Khazaeipour et al. (68) | University Hospital | All HCWs | 2008 | Iran | 139 | 93 | 7 |
| Lu and Euler (69) | National Health Surveys. | All HCWs | 2006 | America | 484 | 226 | 6 |
| Domínguez et al. (70) | Hospital | All HCWs | 2011 | Spain | 1749 | 886 | 8 |
| Toledo et al. (71) | community health centers | Pharmacists | 2013 | Spain | 463 | 116 | 9 |
| Loulergue et al. (72) | Medical departments | All HCWs | 2006 | France | 395 | 204 | 8 |
| Madewell et al. (73) | Hospital | All HCWs | 2018 | America | 706 | 393 | 8 |
| Harrison et al. (74) | Hospital | Nurses | 2013 | Austria | 107 | 45 | 8 |
| Petek and Kamnik-Jug (75) | Primary care centers | All HCWs | 2014 | Slovenia | 250 | 30 | 9 |
| Murray and Skull (76) | Hospital | All HCWs | 1999 | Australia | 269 | 131 | 7 |
| Mojamamy et al. (77) | Primary care centers | All HCWs | 2015 | Saudi Arabia | 368 | 320 | 7 |
| Vírseda et al. (78) | University Hospital | All HCWs | 2009 | Spain | 527 | 262 | 8 |
| Amani et al. (79) | Hospital/community health centers | All HCWs | 2019 | Egypt | 980 | 131 | 9 |
| Hämäläinen et al. (80) | University Hospital | All HCWs | 2015 | Finland | 985 | 586 | 7 |
| Khazaeipour et al. (81) | University Hospital | All HCWs | 2008 | Iran | 139 | 93 | 9 |
| Jiang et al. (82) | Hospital | All HCWs | 2019 | Mainland China | 2,974 | 713 | 8 |
| Fan et al. (83) | Hospital | All HCWs | 2019 | Mainland China | 6,654 | 1,037 | 7 |
| Yan et al. (84) | Hospital | All HCWs | 2019 | Mainland China | 1,332 | 614 | 7 |
| Li et al. (85) | Hospital | All HCWs | 2020 | Mainland China | 4,135 | 2,460 | 9 |
| Zhang et al. (86) | Hospital | All HCWs | 2019 | Mainland China | 775 | 255 | 9 |
| Wu et al. (87) | Hospital | All HCWs | 2018 | Mainland China | 3,507 | 413 | 8 |
| Lv et al. (88) | Community health centers | All HCWs | 2018 | Mainland China | 1,483 | 216 | 8 |
| Fan et al. (89) | Hospital | All HCWs | 2020 | Mainland China | 769 | 670 | 9 |
| Lei et al. (90) | Influenza sentinel surveillance Hospital | All HCWs | 2020 | Mainland China | 1854 | 419 | 9 |
| Ma et al. (91) | Internet survey | All HCWs | 2021 | Mainland China | 1,697 | 600 | 9 |
| Papageorgiou et al. (92) | Health care services institutions | All HCWs | 2019 | Cyprus | 962 | 306 | 8 |
| Ajejas Bazán et al. (93) | Public Health Directorates | All HCWs | 2020 | Spain | 832 | 590 | 8 |
| Bertoni et al. (94) | Cancer research institute | All HCWs | 2020 | Italy | 579 | 334 | 8 |
| Marinos et al. (95) | Athens Medical Association | All HCWs | 2020 | Greece | 1993 | 1,523 | 7 |
| Shi et al. (96) | Hospital/Community health centers | All HCWs | 2020 | Mainland China | 2,192 | 868 | 8 |
| Jędrzejek and Mastalerz-Miga (97), | Hospital | All HCWs | 2019 | Poland | 165 | 101 | 8 |
| Costantino et al. (98) | Community health centers | Pharmacists | 2020 | Italy | 1,450 | 841 | 7 |
| Ogliastro et al. (99) | University Hospital | All HCWs | 2021 | Italy | 4,753 | 1,423 | 4 |
Influenza vaccination rate and subgroup analysis
The meta-analysis included a total of 92 cross-sectional studies, and a random effects model was employed. The analysis revealed that the global influenza vaccination rate among healthcare workers was 41.7% (95% CI [35.7, 47.7%)]. However, it is noted that significant heterogeneity was observed among the studies (I2 = 99.9%, p < 0.001). To further explore the sources of heterogeneity, subgroup analyzes were conducted based on the country’s level of development, geographic region, and time of vaccination.
The countries included in the analysis were categorized as low income or high income according to their economic levels. It was revealed that the influenza vaccination rate among healthcare workers in developed or developing countries was 46.9% or 35.6%. Furthermore, the study regions were classified into Asia, Europe, America, Africa, Oceania, and the Middle East based on their geographical locations. Subgroup analysis revealed that America had the highest vaccination rate at 67.1%, followed by the Middle East, Oceania, Europe, and Asia with rates of 51.3, 48.7, 42.5, and 28.5%, respectively. Africa had the lowest vaccination rate at 6.5%. The study periods were divided based on the occurrence of the H1N1 influenza pandemic (March 2009 to August 2010) and the COVID-19 epidemic (from the end of December 2019). The vaccination rates were separately analyzed for different periods: before 2009, 2009–2012, 2013–2016, 2017–2019, and 2020-present. The subgroup analysis showed that the highest vaccination rate was observed since 2020 at 52.8%, followed by the period of 2009–2012 at 46.7%, 2013–2016 at 46.5%, before 2009 at 39.4%, and the lowest rate was during 2017–2019 at 31.4%.
Despite the subgroup analysis, there remained high heterogeneity in the vaccination rates within each subgroup, indicating that the level of economic development, geographical location, and different vaccination periods were not the primary sources of heterogeneity. The detailed results of the subgroup analysis can be found in Table 2.
Table 2.
Influenza vaccination rate of HCWs in different groups.
| Groups | Reference(n) | Test of heterogeneity result | Meta-analysis results | |||
|---|---|---|---|---|---|---|
| P | I2(%) | Effect model | Rate (%) | 95% CI | ||
| Economic development levels | ||||||
| Developing country | 67 | <0.001 | 99.9 | Random | 46.9 | (38.0, 55.9%) |
| Developed country | 58 | <0.001 | 99.8 | Random | 35.6 | (30.1, 41.1%) |
| Geographic region | ||||||
| Asia | 45 | <0.001 | 99.8 | Random | 28.5 | (23.2, 33.8%) |
| Europe | 45 | <0.001 | 99.9 | Random | 42.5 | (31.2, 53.8%) |
| America | 17 | <0.001 | 99.9 | Random | 67.1 | (48.9, 85.4%) |
| Africa | 1 | – | – | Random | 6.5 | (4.7, 8.3%) |
| Oceania | 1 | – | – | Random | 48.7 | (42.7, 54.7%) |
| Middle East | 16 | <0.001 | 99.6 | Random | 51.3 | (38.1, 64.5%) |
| Vaccination time | ||||||
| ~2008 | 13 | <0.001 | 99.8 | Random | 39.4 | (21.9, 56.8%) |
| 2009–2012 | 28 | <0.001 | 99.8 | Random | 46.7 | (37.9, 55.6%) |
| 2013–2016 | 33 | <0.001 | 99.8 | Random | 46.5 | (35.8, 57.2%) |
| 2017–2019 | 39 | <0.001 | 100.0 | Random | 31.4 | (18.5, 44.3%) |
| 2020~ | 12 | <0.001 | 99.7 | Random | 52.8 | (41.9, 63.8%) |
| Total | 125 | <0.001 | 99.9 | Random | 41.7 | (35.7, 47.7%) |
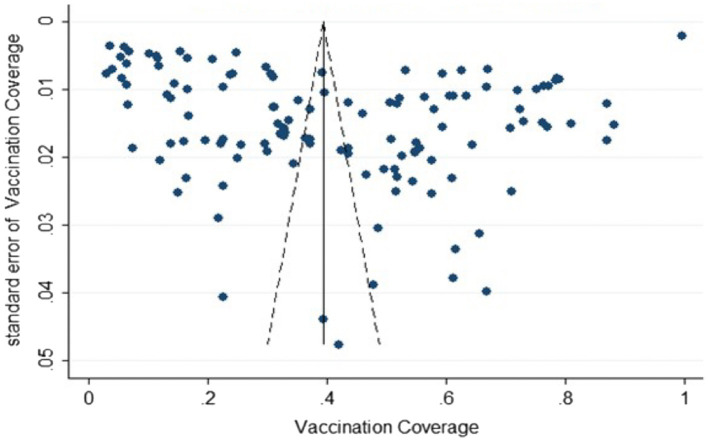
Publication bias test
A funnel plot was generated using the 125 vaccination rate data included in the study (Figure 2), which showed that the scatter was relatively dispersed and roughly symmetrical. The Egger’s test confirmed that there was no significant publication bias in the studies (t = −0.33, p = 0.741), indicating that this study had low publication bias.
Figure 2.
Funnel plot with pseudo 95% confidence limits.
Sensitivity analysis
A sensitivity analysis was performed by systematically excluding individual studies from the meta-analysis. The results indicated that the effect size remained consistent, ranging from 41 to 43%, even when each study was removed, suggesting that the meta-analysis findings were robust and stable (Supplementary Table S2).
Factors influencing influenza vaccination
A total of 32 factors were identified from the included studies that significantly influenced healthcare workers’ uptake of influenza vaccine. Several factors played a significant role in influencing vaccination uptake among healthcare workers, including age, length of employment, education level, department of work, occupation, presence of chronic diseases, perception of being at risk of infection, belief in vaccine effectiveness, willingness to receive vaccination, recommendation of influenza vaccine to patients, previous COVID-19 vaccination, participation in influenza or influenza vaccine training and health education, and knowledge of vaccination timing.
Compared with the younger age group, the middle-aged and older adult groups were more likely to receive the vaccine. Healthcare workers with more than 10 years of experience were more likely to be vaccinated than those with less than 10 years of experience. Non-clinical staff were more likely to receive the vaccine than clinical staff. Among healthcare workers who had chronic diseases, perceived themselves to be at high risk of infection, believed in the effectiveness of the vaccine, had the willingness to receive the vaccine, recommended the vaccine to patients, had previous COVID-19 vaccination, and had knowledge of vaccination timing, were more likely to receive the influenza vaccine.
Subgroup analysis of influencing factors showed that gender, marital status, professional title, perception of vaccine safety, source of vaccine information, and whether the workplace provided free vaccines may also be factors influencing healthcare workers’ uptake of influenza vaccine. The detailed findings of these significant factors are summarized in Table 3.
Table 3.
Factors associated with influenza vaccination rates among health care workers.
| Factor | Test of heterogeneity result | Meta-analysis results | P | |||
|---|---|---|---|---|---|---|
| P | I2(%) | Effect model | OR | OR95%CI | ||
| Sex | <0.001 | 78.5 | Random | 1.197 | (0.987, 1.452) | 0.068 |
| Female | <0.001 | 71.3 | Random | 0.960 | (0.787, 1.171) | 0.687 |
| Male | 0.001 | 85.3 | Random | 1.656 | (1.289, 2.127) | <0.001 |
| Age | <0.001 | 95.1 | Random | 1.700 | (1.600, 1.807) | <0.001 |
| Younger age | 0.001 | 70.6 | Random | 1.575 | (1.104, 2.247) | 0.012 |
| Middle-aged | <0.001 | 91.0 | Random | 2.278 | (1.790, 2.900) | <0.001 |
| Older adult | <0.001 | 90.5 | Random | 2.824 | (1.669, 4.779) | <0.001 |
| Whole population | 0.001 | 77.6 | Random | 1.018 | (1.002, 1.034) | 0.030 |
| Length of service | <0.001 | 93.7 | Random | 1.286 | (1.179, 1.402) | <0.001 |
| ≤10 | <0.001 | 90.6 | Random | 1.214 | (0.888, 1.659) | 0.224 |
| 11–30 | <0.001 | 81.6 | Random | 1.397 | (1.203, 1.622) | <0.001 |
| >30 | <0.001 | 84.9 | Random | 1.414 | (0.775, 2.582) | 0.259 |
| Other | 0.373 | 0.0 | Random | 1.009 | (0.999, 1.018) | 0.075 |
| Education level | <0.001 | 73.1 | Random | 0.837 | (0.723, 0.969) | 0.017 |
| College degree or below | <0.001 | 76.5 | Random | 0.721 | (0.582, 0.895) | 0.003 |
| Bachelor degree | 0.154 | 37.9 | Random | 0.829 | (0.666, 1.033) | 0.095 |
| Master degree or above | 0.005 | 70.2 | Random | 1.076 | (0.809, 1.431) | 0.616 |
| Marital status | 0.054 | 44.6 | Random | 1.139 | (0.976, 1.329) | 0.100 |
| Married/Cohabitant | 0.027 | 60.4 | Random | 1.096 | (0.854, 1.406) | 0.473 |
| Separated/Divorced | 0.922 | 0.0 | Random | 1.086 | (0.896, 1.318) | 0.400 |
| Widowed | 0.716 | 0.0 | Random | 1.583 | (1.162, 2.158) | 0.004 |
| Professional title | 0.058 | 41.6 | Random | 1.123 | (0.992, 1.270) | 0.066 |
| Associate senior or above | 0.015 | 67.6 | Random | 1.238 | (0.939, 1.633) | 0.130 |
| Middle | 0.434 | 0.0 | Random | 1.139 | (1.027, 1.264) | 0.014 |
| Primary | 0.110 | 60.8 | Random | 1.059 | (0.581, 1.933) | 0.851 |
| No title | 0.857 | 0.0 | Random | 0.762 | (0.481, 1.208) | 0.248 |
| Department | <0.001 | 77.2 | Random | 1.435 | (1.148, 1.794) | 0.241 |
| Clinical | <0.001 | 89.6 | Random | 1.177 | (0.896, 1.546) | 0.002 |
| Non-clinical | <0.001 | 85.2 | Random | 1.781 | (1.243, 2.551) | 0.002 |
| Occupation | <0.001 | 86.7 | Random | 1.757 | (1.503, 2.055) | <0.001 |
| Nursing staff | <0.001 | 93.1 | Random | 1.371 | (1.006, 1.868) | 0.046 |
| Others | 0.016 | 49.3 | Random | 1.397 | (1.160, 1.682) | <0.001 |
| Clinician | <0.001 | 80.0 | Random | 2.365 | (1.868, 2.993) | <0.001 |
| Hospital level | <0.001 | 88.9 | Random | 0.941 | (0.660, 1.340) | 0.734 |
| Primary | 0.002 | 84.5 | Random | 1.315 | (0.907, 1.907) | 0.148 |
| Secondary | 0.033 | 70.6 | Random | 0.618 | (0.376, 1.015) | 0.057 |
| Have children at home | 0.465 | 0.0 | Random | 1.024 | (0.907, 1.155) | 0.706 |
| Have old people at home | 0.047 | 62.3 | Random | 1.347 | (0.987, 1.838) | 0.060 |
| Have chronic medical condition | 0.399 | 4.5 | Random | 1.707 | (1.441, 2.021) | <0.001 |
| They consider themselves to be at high risk of infection | <0.001 | 87.7 | Random | 1.981 | (1.256, 3.126) | 0.003 |
| Think the vaccine is effective | <0.001 | 87.7 | Random | 2.101 | (1.249, 3.534) | 0.005 |
| Whether the vaccine is safe | <0.001 | 87.1 | Random | 1.413 | (0.921, 2.169) | 0.113 |
| Safe | <0.001 | 90.2 | Random | 1.619 | (1.008, 2.601) | 0.046 |
| Unsafe | 0.440 | 0.0 | Random | 0.741 | (0.349, 1.577) | 0.437 |
| Support HCWs to receive influenza vaccination | <0.001 | 95.2 | Random | 2.279 | (0.824, 6.308) | 0.113 |
| Worried about vaccine side effects | 0.041 | 76.0 | Random | 0.693 | (0.312, 1.537) | 0.367 |
| That vaccines cause the flu | 0.074 | 68.7 | Random | 0.834 | (0.443, 1.570) | 0.575 |
| Protect patients | 0.011 | 84.4 | Random | 2.154 | (0.971, 4.778) | 0.059 |
| Willing to vaccinate | 0.792 | 0.0 | Random | 4.104 | (2.421, 6.956) | <0.001 |
| Whether to recommend vaccines to patients | <0.001 | 86.1 | Random | 2.193 | (1.315, 3.658) | 0.003 |
| No | 0.293 | 9.5 | Random | 1.320 | (0.877, 1.986) | 0.183 |
| Yes | <0.001 | 86.1 | Random | 2.739 | (1.524, 4.922) | 0.001 |
| COVID-19 vaccination | 0.001 | 91.2 | Random | 5.922 | (1.136, 30.876) | 0.035 |
| Have participated in flu or flu vaccine training, health promotion | 0.003 | 89.0 | Random | 0.773 | (0.259, 0.309) | 0.645 |
| Yes | .. | .. | Random | 1.288 | (1.034, 1.604) | 0.024 |
| No | .. | .. | Random | 0.420 | (0.420, 0.840) | 0.014 |
| Sources of information | <0.001 | 84.5 | Random | 1.060 | (0.814, 1.380) | 0.666 |
| People around me | 0.099 | 63.3 | Random | 1.174 | (0.714, 1.928) | 0.527 |
| Mass media | <0.001 | 92.4 | Random | 0.665 | (0.320, 1.382) | 0.275 |
| Professional organization or publication | 0.245 | 24.2 | Random | 1.301 | (1.113, 1.520) | 0.001 |
| Know the vaccination time | <0.001 | 85.2 | Random | 2.224 | (1.165, 4.244) | 0.015 |
| Know the vaccine priority groups | <0.001 | 84.7 | Random | 1.327 | (0.857, 2.053) | 0.205 |
| Know that the vaccine is the most effective way to prevent flu | <0.001 | 88.7 | Random | 1.031 | (0.310, 3.432) | 0.960 |
| Know that the vaccine is given once a yea | <0.001 | 88.5 | Random | 1.028 | (0.612, 1.729) | 0.916 |
| Work units participate in the influenza sentinel network | 0.850 | 0.0 | Random | 0.920 | (0.698, 1.213) | 0.555 |
| Free vaccination at workplace | <0.001 | 98.9 | Random | 0.746 | (0.317, 1.756) | 0.502 |
| Yes | <0.001 | 98.3 | Random | 1.533 | (0.525, 4.479) | 0.435 |
| No | <0.001 | 99.4 | Random | 0.644 | (0.087, 4.777) | 0.667 |
| Unclear | <0.001 | 94.6 | Random | 0.279 | (0.088, 0.886) | 0.030 |
| Have vaccination sites at workplace | <0.001 | 91.5 | Random | 1.377 | (0.764, 2.480) | 0.287 |
| Workplace attitudes toward influenza vaccination of medical staff | <0.001 | 95.7 | Random | 0.897 | (0.498, 1.617) | 0.718 |
| Ask for or support encouragement | <0.001 | 94.0 | Random | 1.602 | (0.944, 2.717) | 0.081 |
| Do not require or encourage | 0.725 | 0.0 | Random | 0.300 | (0.207, 0.435) | <0.001 |
| Unclear | .. | .. | Random | 0.090 | (0.038, 0.216) | <0.001 |
Reasons for accepting or refusing influenza vaccination
Among the 92 studies included, 47 studies reported on the reasons why healthcare workers chose to get vaccinated against influenza, while 55 studies reported on the reasons for refusing vaccination. The comprehensive data are summarized in Table 4, providing insights into the factors that influenced healthcare workers’ decisions to either receive or decline influenza vaccination.
Table 4.
Self-reported reasons for accepting or refusing influenza vaccination in healthcare workers.
| Reasons for refusing | Reference(n) | Reasons for accepting | Reference(n) |
|---|---|---|---|
| 1. The vaccine is considered to have poor or limited preventive effect | 43 | 1. Protect myself | 30 |
| 2. Concerns about adverse reactions or vaccine quality | 38 | 2. Protect my family, patients, and people around me | 26 |
| 3. I’m too busy at work to have time | 33 | 3. Worried about spreading it to the people around me | 19 |
| 4. They are considered to be in good physical condition or have strong immunity and do not need vaccination | 23 | 4. Vaccines are free or cheap | 17 |
| 5. Think the flu is mild and will not cause serious illness | 21 | 5. The vaccine is considered effective in preventing influenza and its complications | 16 |
| 6. Vaccines are out-of-pocket or too expensive | 20 | 6. Consider myself at high risk for the flu and its complications | 13 |
| 7. Vaccinations are inconvenient or lacking | 19 | 7. A work organization or employer requires or performs professional obligations | 13 |
| 8. There are contraindications to vaccination | 16 | 8. Recommended or influenced by leaders, colleagues, relatives and friends | 12 |
| 9. Do not know about influenza vaccination and related information | 14 | 9. Vaccination sites are available or readily available in the workplace | 11 |
| 10. Not considered to be at high risk of catching the flu | 14 | 10. That flu is a serious illness with serious effects | 10 |
| 11. Adverse reactions after vaccination (e.g., flu-like symptoms, pain at injection site) | 12 | 11. Avoid infection affecting my work | 8 |
| 12. Not knowing when and where to get flu shots | 11 | 12. It is recommended by government health authorities or the technical guidelines for influenza vaccines | 7 |
| 13. Forget to vaccinate | 11 | 13. Old age, underlying disease or chronic disease, fear of complications after infection | 7 |
| 14. Fear of injection | 8 | 14. Believe in the safety of flu vaccines | 4 |
| 15. It is considered easy to treat with drugs or prevent with hygiene measures or other drugs | 8 | 15. Doctor’s recommendation | 3 |
| 16. Concerned about the safety of vaccines | 7 | 16. I had the flu last season | 3 |
| 17. Being pregnant or lactating | 7 | 17. Participate in multidisciplinary campaigns or influenza vaccination campaigns | 2 |
| 18. Requires annual vaccinations or immunization procedures | 5 | 18. Have a history of influenza vaccination | 2 |
| 19. Vaccination is not mandatory or recommended by the workplace | 5 | 19. Familiarize with flu vaccination | 1 |
| 20. Does not believe in or oppose vaccination | 5 | 20. Flu infections take an economic toll | 1 |
| 21. Personal choice, reduce drug use | 4 | ||
| 22. There is no awareness of getting the flu vaccine | 1 | ||
| 23. Had the flu this year and do not need to get vaccinated | 1 |
Discussion
The present study encompasses a broad range of countries, including 26 nations across 7 different regions. The meta-analysis findings indicate a relatively low global influenza vaccination rate among healthcare personnel, estimated at 41.7%. Subgroup analysis reveals a notable disparity between developed and developing countries, with higher vaccination rates observed in the former. Among regional subgroups, the Americas exhibit the highest vaccination rate, followed by the Middle East, Oceania, and Europe, while Africa demonstrates the lowest rate. These results suggest that variations in socio-economic development, vaccine accessibility, cost, healthcare service standards, healthcare personnel’s knowledge regarding influenza and influenza vaccines, as well as disparities in awareness of preventive healthcare and vaccination, contribute to the observed differences in influenza vaccination rates across countries. This is consistent with a previous report, which highlights that while Chinese clinical workers possess extensive knowledge about disease diagnosis and treatment, their understanding of health maintenance and disease prevention is comparatively lacking (22).
Subgroup analysis based on vaccination time reveals that rate is gradually increased over the period of 14 years, suggesting that the H1N1 influenza pandemic in 2009 and the subsequent COVID-19 epidemic have played a role in promoting the seasonal influenza vaccination rate among healthcare personnel, likely due to increased awareness of the contagious nature of these diseases (95, 99). However the influenza vaccination rate gradually declined since 2009 pandemic, which aligns with the decreasing impact of the influenza outbreak. However, the occurrence of the COVID-19 epidemic led to a surge in the influenza vaccination, reaching its highest level. This could be attributed to heightened focus on self-protection during the influenza season, increased awareness of the importance of influenza vaccines, and a general promotion of vaccination practices.
The analysis of influencing factors reveals that several characteristics contribute to the higher likelihood of healthcare personnel receiving influenza vaccinations, including age, tenure, education level, professional designation (clinical doctors compared to nurses), and their inclination to recommend influenza vaccines to patients. These findings are in line with studies conducted in China (21, 22) and Cyprus (92), which similarly indicate that doctors are more likely to be vaccinated compared to nurses. This discrepancy may be due to doctors increased exposure to influenza patients due to their longer experience in the field, resulting in a stronger sense of identification as a high-risk group for influenza infection. Consequently, doctors exhibit heightened attention and awareness regarding influenza-related knowledge and information on influenza vaccines.
A study conducted in Spain focused on healthcare personnel in the armed forces, the proportion of vaccinated individuals increased with age and years of service in the 2016–2017 season, but the vaccination rate among younger/middle-ranking officers actually surpassed that of the older adult, indicating a notable shift in vaccination behavior in the 2019–2020 season (93). Such outcome could be attributed to the evolving health knowledge system, which now places greater emphasis on disease prevention and health maintenance. In another survey conducted among nurses in North-eastern China, showing an inverse correlation between vaccination and flu among nurses, maybe due to lack of knowledge among these nurses regarding influenza vaccines, necessitating further education and awareness campaigns to emphasize the importance of vaccination.
Our present findings offer valuable insights for promoting flu vaccination, particularly among healthcare workers. This may involve strategies such as cost reduction or even the implementation of mandatory vaccination policies for specific high-risk population groups. Furthermore, our current data could serve as a foundation for future studies and investments in healthcare worker well-being. Our data underscores the critical importance of flu vaccination for these healthcare workers, who often find themselves in more vulnerable conditions, serving both the older adult and other high-risk groups. This relevance is further emphasized by the ongoing threat of viral mutation and the persistence of long-term consequences from COVID-19, even though it is no longer classified as a pandemic. Hence, our present data strongly underscores the critical importance of flu vaccination for healthcare workers, especially those in more vulnerable roles, such as caring for the older adult and other high-risk groups. This relevance is further accentuated by the context of the ongoing COVID-19 outbreak, even if it is no longer considered a pandemic. The continuous viral mutation and the lingering presence of long-term COVID-19 complications make this vigilance particularly vital.
In conclusion, the influenza vaccination rate among healthcare workers globally remains low. To address this issue effectively, it is crucial to implement comprehensive measures that promote influenza vaccination among this population, as well as the general public. Efforts should be focused on raising awareness about the importance of vaccination, providing accessible and convenient vaccination services, and enhancing education regarding influenza and its prevention. By implementing these measures, we can strive to improve the influenza vaccination rates among healthcare workers and the wider population, leading to better overall public health outcomes.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary material.
Author contributions
JF: Conceptualization, Funding acquisition, Supervision, Writing – original draft, Writing – review & editing. SX: Data curation, Formal analysis, Writing – original draft. YL: Data curation, Visualization, Writing – review & editing. XM: Data curation, Formal analysis, Software, Writing – review & editing. JC: Data curation, Formal analysis, Investigation, Writing – review & editing. CF: Conceptualization, Project administration, Validation, Writing – review & editing. SB: Conceptualization, Project administration, Writing – review & editing.
Acknowledgments
We are grateful to the institutions and individuals who have helped us throughout the research process.
Funding Statement
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study was supported by Health Industry Scientific Research Management Project of Gansu Province [Grant No. GSWSKY2021-058], Wu Jieping Medical Foundation Project [Grant No. 320.6750.2022-20-21] and Natural Science Foundation of Gansu Province (22JR5RA589).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1295464/full#supplementary-material
References
- 1.WHO . Influenza (seasonal). Geneva: World Health Organization. (2023). Available at: https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal) (Accessed January 31, 2023).
- 2.Troeger CE, Blacker BF, Khalil IA, Zimsen SRM, Albertson SB, Abate D, et al. Mortality, morbidity, and hospitalisations due to influenza lower respiratory tract infections, 2017: an analysis for the global burden of disease study 2017. Lancet Respir Med. (2019) 7:69–89. doi: 10.1016/S2213-2600(18)30496-X, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Courville C, Cadarette SM, Wissinger E, Alvarez FP. The economic burden of influenza among adults aged 18 to 64: A systematic literature review. Influenza Other Respir Viruses. (2022) 16:376–85. doi: 10.1111/irv.12963, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Demicheli V, Jefferson T, Ferroni E, Rivetti A, Di Pietrantonj C. Vaccines for preventing influenza in healthy adults. Cochrane Database Syst Rev. (2018) 2:Cd001269. doi: 10.1002/14651858.CD001269.pub6, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuster SP, Shah PS, Coleman BL, Lam PP, Tong A, Wormsbecker A, et al. Incidence of influenza in healthy adults and healthcare workers: a systematic review and meta-analysis. PLoS One. (2011) 6:e26239. doi: 10.1371/journal.pone.0026239, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colaprico C, Ricci E, Bongiovanni A, Imeshtari V, Barletta VI, Manai MV, et al. Flu vaccination among healthcare professionals in times of COVID-19: knowledge, attitudes, and behavior. Vaccine. (2022) 10:10–1. doi: 10.3390/vaccines10081341, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mereckiene J. Seasonal influenza vaccination and antiviral use in EU/EEA member states–Overview of vaccine recommendations for 2017–2018 and vaccination coverage rates for 2015–2016 and 2016–2017 influenza seasons. European Centre for Disease Prevention and Control: Stockholm, Sweden; (2018). [Google Scholar]
- 8.Sheng YQ, Su XG, Wang L, Cui Y, Nie X. Influenza related knowledge awareness and influenza vaccination coverage in nurses in Heilongjiang, 2017-2018. Dis Surveill. (2020) 2:532–6. doi: 10.3784/j.issn.1003-9961.2020.06.016 [DOI] [Google Scholar]
- 9.Liu T, Yang R, Tao ZF, Zhang YN, Zhang GQ. Influenza vaccine vaccination status, recommendation willingness, and influencing factors among medical staff in community health service centers in Fengtai District. Beijing Dis Surveill. (2020) 6:1136–40. doi: 10.3784/j.issn.1003-9961.2020.12.016 [DOI] [Google Scholar]
- 10.Wang LJ, He HC, Ma JX, Cui SF. Survey and analysis of influenza nowledgek, attitudes and practices among medical staff in a district of Beijing. Practical. Prev Med. (2015) 7:202–4. doi: 10.3969/j.issn.1006-3110.2015.02.024 [DOI] [Google Scholar]
- 11.Gao Y, Zhao YL, Wu H, Yang XS, Zhang WL. Analysis of influenza vaccine vaccination willingness and influencing factors among medical ftaff in a tertiary hospital in Beijing. Int J Virol. (2015) 8:252–6. doi: 10.3760/cma.j.issn.1673-4092.2015.04.010 [DOI] [Google Scholar]
- 12.Liu N, Zheng YM, Li YQ, Ding YM. Current status and influencing factors of influenza vaccine vaccination behavior among respiratory nurses. J Nurs Manag. (2021) 10:360–4. doi: 10.3969/j.issn.1671-315x.2021.05.012 [DOI] [Google Scholar]
- 13.Yang LX, Chen SS. Investigation and analysis of influenza vaccine vaccination status and influencing factors among 650 emergency nurses in Huizhou City. Clin Med Pract. (2015) 11:208–10. [Google Scholar]
- 14.Gan ZK, Shen YG, Wang SY, Gu XJ, Zhou JH. Survey on knowledge, attitudes and practices of influenza and 23-valent pneumococcal polysaccharide vaccine vaccination among primary healthcare workers. Prev Med. (2019) 31:12. doi: 10.19485/j.cnki.issn2096-5087.2019.12.007 [DOI] [Google Scholar]
- 15.Wang DM. Investigation on the knowledge level of influenza and influenza vaccine among medical staff in a hospital. Occup Health. (2008) 16:2313–4. doi: 10.3969/j.issn.1004-1257.2008.21.041 [DOI] [Google Scholar]
- 16.Bu LH, Hao XN, Bo T, Li SX, Liu Z. Investigation on the knowledge, attitudes, and practices (KAP) of influenza and influenza vaccine among medical staff in Qingdao City. Chi J Health Policy. (2015) 20:474–6. [Google Scholar]
- 17.Yang JS, Zhang LJ, Feng LZ, Zhao JH, Ma YY. Analysis of influenza vaccine coverage and its influencing factors among clinical medical staff in Xining City, Qinghai Province, during 2016-2017. Chi J Epidemiol. (2018) 21:1066–70. doi: 10.3760/cma.j.issn.0254-6450.2018.08.010 [DOI] [Google Scholar]
- 18.Wang ZW, Cui Y, Zhou Q, Nie X, Peng ZL. Investigation on the knowledge, prevalence and vaccination status of influenza among nurses in Shaanxi Province. Chi J Health Stat. (2021) 22:449–52. doi: 10.3969/j.issn.1002-3674.2021.03.035 [DOI] [Google Scholar]
- 19.Zhang QH, Yao XJ, Guo XQ. Analysis of current situation and influencing factors of influenza vaccine uptake among key healthcare workers in Songjiang District. Shanghai Occup Health. (2021) 24:1920–4. [Google Scholar]
- 20.Kong QF, Zhang X, Tang L, Hou Q, Zhang GM. Investigation on the influenza vaccination coverage among healthcare workers in 2019 and the willingness to receive influenza vaccine in 2020 and its influencing factors. China J Vaccin Immun. (2021) 27:311–6. doi: 10.19914/j.CJVI.2021058 [DOI] [Google Scholar]
- 21.Ma YY, Zhang LJ, Shi Y, Ma BZ, Wang WJ. Investigation on the current status and related factors of influenza vaccination among medical staff in tertiary hospitals in Xining during the 2017-2018 influenza season. Chi J Prev Med. (2019) 3:1018–21. doi: 10.3760/cma.j.issn.0253?9624.2019.10.012 [DOI] [PubMed] [Google Scholar]
- 22.Gan L, Xiong Y, Li Q, Chen T, Tang XJ. Analysis of influenza vaccination and influencing factors among medical staff in Chongqing during the 2018-2019 influenza season. Dis Surveill. (2020) 5:1100–4. doi: 10.3784/j.issn.1003-9961.2020.12.009 [DOI] [Google Scholar]
- 23.James PB, Rehman IU, Bah AJ, Lahai M, Cole CP, Khan TM. An assessment of healthcare professionals’ knowledge about and attitude towards influenza vaccination in Freetown Sierra Leone: a cross-sectional study. BMC Public Health. (2017) 17:692. doi: 10.1186/s12889-017-4700-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu H, Tan Y, Zhang M, Peng Z, Zheng J, Qin Y, et al. An internet-based survey of influenza vaccination coverage in healthcare workers in China, 2018/2019 season. Vaccine. (2019) 8:6. doi: 10.3390/vaccines8010006, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hosamirudsari H, Kanavee AR, Ghanbari M, Akbarpour S, Alimohamadi Y. Assessment of the belief and attitudes of Iranian healthcare personnel’s toward the influenza infection and influenza vaccination. J Prev Med Hyg. (2019) 60:E178–e183. doi: 10.15167/2421-4248/jpmh2019.60.3.1056, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alhammadi A, Khalifa M, Abdulrahman H, Almuslemani E, Alhothi A, Janahi M. Attitudes and perceptions among the pediatric health care providers toward influenza vaccination in Qatar: A cross-sectional study. Vaccine. (2015) 33:3821–8. doi: 10.1016/j.vaccine.2015.06.082, PMID: [DOI] [PubMed] [Google Scholar]
- 27.Boey L, Bral C, Roelants M, De Schryver A, Godderis L, Hoppenbrouwers K, et al. Attitudes, believes, determinants and organisational barriers behind the low seasonal influenza vaccination uptake in healthcare workers - A cross-sectional survey. Vaccine. (2018) 36:3351–8. doi: 10.1016/j.vaccine.2018.04.044, PMID: [DOI] [PubMed] [Google Scholar]
- 28.Barbadoro P, Marigliano A, Di Tondo E, Chiatti C, Di Stanislao F, D’Errico MM, et al. Determinants of influenza vaccination uptake among Italian healthcare workers. Hum Vaccin Immunother. (2013) 9:911–6. doi: 10.4161/hv.22997, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wong NS, Lee S, Lee SS. Differing pattern of influenza vaccination uptake in nurses between clinical and long term care facilities setting, 2014–2018. J Infect Dis. (2018) 75:8–10. doi: 10.1016/j.ijid.2018.07.009 [DOI] [PubMed] [Google Scholar]
- 30.Kyaw WM, Chow A, Hein AA, Lee LT, Leo YS, Ho HJ. Factors influencing seasonal influenza vaccination uptake among health care workers in an adult tertiary care hospital in Singapore: A cross-sectional survey. Am J Infect Control. (2019) 47:133–8. doi: 10.1016/j.ajic.2018.08.011 [DOI] [PubMed] [Google Scholar]
- 31.Rabensteiner A, Buja A, Regele D, Fischer M, Baldo V. Healthcare worker’s attitude to seasonal influenza vaccination in the south Tyrolean province of Italy: barriers and facilitators. Vaccine. (2018) 36:535–44. doi: 10.1016/j.vaccine.2017.12.007 [DOI] [PubMed] [Google Scholar]
- 32.Garcell HG, Ramirez EC. Influenza immunization coverage for healthcare workers in a community hospital in Qatar (2011-2012 and 2012-2013 seasons). J Infect Public Health. (2014) 7:70–2. doi: 10.1016/j.jiph.2013.06.007 [DOI] [PubMed] [Google Scholar]
- 33.Esposito S, Bosis S, Pelucchi C, Tremolati E, Sabatini C, Semino M, et al. Influenza vaccination among healthcare workers in a multidisciplinary university hospital in Italy. BMC Public Health. (2008) 8:422. doi: 10.1186/1471-2458-8-422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hudu SA, Harmal NS, Malina O, Sekawi Z. Influenza vaccination among Malaysian healthcare workers: A survey of coverage and attitudes. Med J Malaysia. (2016) 72:231–7. PMID: [PubMed] [Google Scholar]
- 35.Costantino C, Mazzucco W, Azzolini E, Baldini C, Bergomi M, Biafiore AD, et al. Influenza vaccination coverage among medical residents: an Italian multicenter survey. Hum Vaccin Immunother. (2014) 10:1204–10. doi: 10.4161/hv.28081, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jimenez-Garcia R, Carrasco-Garrido P, Hernandez-Barrera V, De Miguel AG. Influenza vaccination coverage and predictors for vaccination among Spanish healthcare workers. Hum Vaccin. (2007) 3:33–6. doi: 10.4161/hv.3.1.3750, PMID: [DOI] [PubMed] [Google Scholar]
- 37.Von Perbandt E, René H, Mirjam T. Influenza vaccination coverage of health care workers: a cross-sectional study based on data from a Swiss gynaecological hospital. GMS. Infect Dis. (2018) 6:94. doi: 10.3205/id000037, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haridi HK, Salman KA, Basaif EA, Al-Skaibi DK. Influenza vaccine uptake, determinants, motivators, and barriers of the vaccine receipt among healthcare workers in a tertiary care hospital in Saudi Arabia. J Hosp Infect. (2017) 96:268–75. doi: 10.1016/j.jhin.2017.02.005, PMID: [DOI] [PubMed] [Google Scholar]
- 39.Sočan M, Erčulj V, Lajovic J. Knowledge and attitudes on pandemic and seasonal influenza vaccination among Slovenian physicians and dentists. Eur J Pub Health. (2013) 23:92–7. doi: 10.1093/eurpub/cks006, PMID: [DOI] [PubMed] [Google Scholar]
- 40.Domínguez A, Godoy P, Castilla J, Soldevila N, Toledo D, Astray J, et al. Knowledge of and attitudes to influenza vaccination in healthy primary healthcare workers in Spain, 2011-2012. PLoS One. (2013) 8:e81200. doi: 10.1371/journal.pone.0081200, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rehmani R, Memon JI. Knowledge, attitudes and beliefs regarding influenza vaccination among healthcare workers in a Saudi hospital. Vaccine. (2010) 28:4283–7. doi: 10.1016/j.vaccine.2010.04.031 [DOI] [PubMed] [Google Scholar]
- 42.Kan T, Ai J, Zhang J, Liu X. Predictors of seasonal influenza vaccination behaviour among nurses and implications for interventions to increase vaccination uptake: A cross-sectional survey. Int J Nurs Stud. (2018) 79:137–44. doi: 10.1016/j.ijnurstu.2017.12.003, PMID: [DOI] [PubMed] [Google Scholar]
- 43.Kent JN, Lea CS, Fang X, Novick LF, Morgan J. Seasonal influenza vaccination coverage among local health department personnel in North Carolina, 2007-2008. Am J Prev Med. (2010) 39:74–7. doi: 10.1016/j.amepre.2010.03.007, PMID: [DOI] [PubMed] [Google Scholar]
- 44.Hagemeister MH, Stock NK, Ludwig T, Heuschmann P, Vogel U. Self-reported influenza vaccination rates and attitudes towards vaccination among health care workers: results of a survey in a German university hospital. Public Health. (2018) 154:102–9. doi: 10.1016/j.puhe.2017.10.027 [DOI] [PubMed] [Google Scholar]
- 45.Castilla J, Martínez-Baz I, Godoy P, Toledo D, Astray J, García S, et al. Trends in influenza vaccine coverage among primary healthcare workers in Spain, 2008-2011. Prev Med. (2013) 57:206–11. doi: 10.1016/j.ypmed.2013.05.021, PMID: [DOI] [PubMed] [Google Scholar]
- 46.Ball SW, Donahue SMA, Izrael D, Walker DK, DiSogra C, De Perio MA, et al. Influenza vaccination coverage among health-care personnel - United States, 2012-13 influenza season. Morb Mortal Wkly Rep. (2013) 82:781–6. PMID: 24067582 [Google Scholar]
- 47.Black CL, Yue X, Ball SW, Donahue SM, Izrael D, De Perio MA, et al. Influenza vaccination coverage among health care personnel--United States, 2013-14 influenza season. Morb Mortal Wkly Rep. (2014) 76:805–11. PMID: [PMC free article] [PubMed] [Google Scholar]
- 48.Black CL, Yue X, Ball SW, Donahue SM, Izrael D, De Perio MA, et al. Influenza vaccination coverage among health care personnel--United States, 2014-15 influenza season. Morb Mortal Wkly Rep. (2015) 78:993–9. doi: 10.15585/mmwr.mm6436a1 [DOI] [PubMed] [Google Scholar]
- 49.Black CL, Yue X, Ball SW, Donahue SM, Izrael D, De Perio MA, et al. Influenza vaccination coverage among health care personnel - United States, 2015-16 influenza season. Morb Mortal Wkly Rep. (2016) 65:1026–31. doi: 10.15585/mmwr.mm6538a2 [DOI] [PubMed] [Google Scholar]
- 50.Black CL, Yue X, Ball SW, Fink R, De Perio MA, Laney AS, et al. Influenza vaccination coverage among health care personnel - United States, 2016-17 influenza season. Morb Mortal Wkly Rep. (2017) 66:1009–15. doi: 10.15585/mmwr.mm6638a1, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Black CL, Yue X, Ball SW, Fink RV, De Perio MA, Laney AS, et al. Influenza vaccination coverage among health care personnel - United States, 2017-18 influenza season. Morb Mortal Wkly Rep. (2018) 67:1050–4. doi: 10.15585/mmwr.mm6738a2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.CDC . Influenza vaccination coverage among health-care personnel --- United States, 2010-11 influenza season. Morb Mortal Wkly Rep. (2011) 83:1073–7. PMID: [PubMed] [Google Scholar]
- 53.Ball SW, Walker DK, Donahue SMA, Izrael D, Zhang J, De Perio MA, et al. Influenza vaccination coverage among health-care personnel: 2011-12 influenza season, United States. Morb Mortal Wkly Rep. (2012) 81:753–7. PMID: [PubMed] [Google Scholar]
- 54.Tanguy M, Boyeau C, Pean S, Marijon E, Delhumeau A, Fanello S. Acceptance of seasonal and pandemic a (H1N1) 2009 influenza vaccination by healthcare workers in a French teaching hospital. Vaccine. (2011) 29:4190–4. doi: 10.1016/j.vaccine.2011.03.107, PMID: [DOI] [PubMed] [Google Scholar]
- 55.Amodio E, Tramuto F, Maringhini G, Asciutto R, Firenze A, Vitale F, et al. Are medical residents a “core group” for future improvement of influenza vaccination coverage in health-care workers? A study among medical residents at the University Hospital of Palermo. Vaccine. (2011) 29:8113–7. doi: 10.1016/j.vaccine.2011.08.033 [DOI] [PubMed] [Google Scholar]
- 56.Hakim SA, Amin W, Allam MF, Fathy AM, Mohsen A. Attitudes, beliefs and practice of Egyptian healthcare workers towards seasonal influenza vaccination. Influenza Other Respir Viruses. (2021) 15:778–88. doi: 10.1111/irv.12868, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hussain H, McGeer A, McNeil S, Katz K, Loeb M, Simor A, et al. Factors associated with influenza vaccination among healthcare workers in acute care hospitals in Canada. Influenza Other Respir Viruses. (2018) 12:319–25. doi: 10.1111/irv.12545, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tagajdid MR, El Annaz H, Belefquih B, Doblali T, Casalegno JS, Mekki Y, et al. Factors influencing uptake of influenza vaccine amongst healthcare workers in a regional center after the A(H1N1) 2009 pandemic: lessons for improving vaccination rates. Int J Risk Saf Med. (2011) 23:249–54. doi: 10.3233/JRS-2011-0544, PMID: [DOI] [PubMed] [Google Scholar]
- 59.Dorribo V, Lazor-Blanchet C, Hugli O, Zanetti G. Health care workers’ influenza vaccination: motivations and mandatory mask policy. Occup Med. (2015) 65:739–45. doi: 10.1093/occmed/kqv116, PMID: [DOI] [PubMed] [Google Scholar]
- 60.Bazán M, Villacorta E, Barbagelatta G, Jimenez MM, Goya C, Bartolini RM, et al. Health workers’ attitudes, perceptions and knowledge of influenza immunization in Lima, Peru: A mixed methods study. Vaccine. (2017) 35:2930–6. doi: 10.1016/j.vaccine.2017.04.021, PMID: [DOI] [PubMed] [Google Scholar]
- 61.Yi H, Yang Y, Zhang L, Zhang M, Wang Q, Zhang T, et al. Improved influenza vaccination coverage among health-care workers: evidence from a web-based survey in China, 2019/2020 season. Hum Vaccin Immunother. (2021) 17:2185–9. doi: 10.1080/21645515.2020.1859317, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sánchez-Payá J, Hernández-García I, García-Román V, Camargo-Angeles R, Barrenengoa-Sañudo J, Villanueva-Ruiz CO, et al. Influenza vaccination among healthcare personnel after pandemic influenza H1N1. Vaccine. (2012) 30:911–5. doi: 10.1016/j.vaccine.2011.11.095 [DOI] [PubMed] [Google Scholar]
- 63.Yu J, Ren X, Ye C, Tian K, Feng L, Song Y, et al. Influenza vaccination coverage among registered nurses in China during 2017-2018: An internet panel survey. Vaccine. (2019) 7:88. doi: 10.3390/vaccines7040134, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Groenewold M, Baron S, Tak S, Allred N. Influenza vaccination coverage among US nursing home nursing assistants: the role of working conditions. Am Med Dir Assoc. (2012) 13:85.e17–23. doi: 10.1016/j.jamda.2011.02.008, PMID: [DOI] [PubMed] [Google Scholar]
- 65.Hajiabdolbaghi M, Havastin NG, Afhami S, Montazeri M, Mohammadnejad E, Rezaei P, et al. Influenza vaccination coverage and obstacles in healthcare workers (HCWs) and the follow up of side effects: A multicenter investigation in Iran. J Prev Med Hyg. (2021) 62:E377–81. doi: 10.15167/2421-4248/jpmh2021.62.2.1827, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dubnov J, Kassabri W, Bisharat B, Rishpon S. Influenza vaccination coverage determinants among employees of the Nazareth hospital in Israel. Israel Isr Med Assoc. (2010) 92:338–41. PMID: [PubMed] [Google Scholar]
- 67.Buxmann H, Daun A, Wicker S, Schlößer RL. Influenza vaccination rates among parents and health care personnel in a German neonatology department. Vaccine. (2018) 6:1–8. doi: 10.3390/vaccines6010003, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Khazaeipour Z, Ranjbar Novin N, Hoseini N. Influenza vaccine: immunization rates, knowledge, attitudes and practice of health care workers in Iran in 2008/09. J Infect Dis. (2010) 14:e451. doi: 10.1016/j.ijid.2010.02.620 [DOI] [PubMed] [Google Scholar]
- 69.Lu PJ, Euler GL. Influenza, hepatitis B, and tetanus vaccination coverage among health care personnel in the United States. Am J Infect Control. (2011) 39:488–94. doi: 10.1016/j.ajic.2010.10.009, PMID: [DOI] [PubMed] [Google Scholar]
- 70.Domínguez A, Godoy P, Castilla J, Mayoral JM, Soldevila N, Torner N, et al. Knowledge of and attitudes to influenza in unvaccinated primary care physicians and nurses: A cross-sectional study. Hum Vaccin Immunother. (2014) 10:2378–86. doi: 10.4161/hv.29142, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Toledo D, Soldevila N, Guayta-Escolies R, Lozano P, Rius P, Gascón P, et al. Knowledge of and attitudes to influenza vaccination among community pharmacists in Catalonia (Spain). 2013-2014 season: A cross sectional study. Int J Environ Res Public Health. (2017) 14:110. doi: 10.3390/ijerph14070756, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Loulergue P, Moulin F, Vidal-Trecan G, Absi Z, Demontpion C, Menager C, et al. Knowledge, attitudes and vaccination coverage of healthcare workers regarding occupational vaccinations. Vaccine. (2009) 27:4240–3. doi: 10.1016/j.vaccine.2009.03.039 [DOI] [PubMed] [Google Scholar]
- 73.Madewell Z, Chacón-Fuentes R, Badilla-Vargas X, Ramirez C, Ortiz MR, Alvis-Estrada JP, et al. Knowledge, attitudes, and practices for the use of seasonal influenza vaccination, healthcare workers, Costa Rica. J Infect Dev Ctries. (2021) 15:1004–13. doi: 10.3855/jidc.14381, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Harrison N, Brand A, Forstner C, Tobudic S, Burgmann K, Burgmann H. Knowledge, risk perception and attitudes toward vaccination among Austrian health care workers: A cross-sectional study. Hum Vaccines. (2016) 12:2459–63. doi: 10.1080/21645515.2016.1168959, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Petek D, Kamnik-Jug K. Motivators and barriers to vaccination of health professionals against seasonal influenza in primary healthcare. BMC Health Serv Res. (2018) 18:853. doi: 10.1186/s12913-018-3659-8, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Murray SB, Skull SA. Poor health care worker vaccination coverage and knowledge of vaccination recommendations in a tertiary Australia hospital. Aust N Z J Public Health. (2010) 26:65–8. doi: 10.1111/j.1467-842X.2002.tb00273.x [DOI] [PubMed] [Google Scholar]
- 77.Mojamamy GM, Albasheer OB, Mahfouz MS. Prevalence, knowledge, attitude, and practices associated with influenza vaccination among healthcare workers in primary care centers in Jazan, Saudi Arabia: A cross-sectional study. Trop J Pharm Res. (2018) 17:1201–7. doi: 10.4314/tjpr.v17i6.29 [DOI] [Google Scholar]
- 78.Vírseda S, Restrepo MA, Arranz E, Magán-Tapia P, Fernández-Ruiz M, de la Cámara AG, et al. Seasonal and pandemic A (H1N1) 2009 influenza vaccination coverage and attitudes among health-care workers in a Spanish university hospital. Vaccine. (2010) 28:4751–7. doi: 10.1016/j.vaccine.2010.04.101, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Amani W, Youssef W, Adel H, Ayman F. Seasonal influenza vaccination coverage and barriers among healthcare workers in an Egyptian Province. Med Lav. (2020) 111:449–56. doi: 10.23749/mdl.v111i6.9489, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hämäläinen A, Patovirta RL, Mauranen E, Hämäläinen S, Koivula I. Support among healthcare workers for the new mandatory seasonal influenza vaccination policy and its effects on vaccination coverage. Ann Med. (2021) 53:384–90. doi: 10.1080/07853890.2021.1889022, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Khazaeipour Z, Ranjbarnovin N, Hoseini N. Influenza immunization rates, knowledge, attitudes and practices of health care workers in Iran. J Infect Dev Ctries. (2010) 4:636–44. doi: 10.3855/jidc.1152, PMID: [DOI] [PubMed] [Google Scholar]
- 82.Jiang SQ, Cai YW, Zuo R, Xu LF, Zheng JD, Yi HY, et al. Analysis of influenza vaccination and recommendation behavior among medical staff in Nanshan District, Shenzhen City in the 2019-2020 free vaccination policy period and its associated factors. China J Prev Med. (2022) 56:6. doi: 10.3760/cma.j.cn112150-20211217-01164 [DOI] [PubMed] [Google Scholar]
- 83.Fan X, Peng ZB, Song Y, Feng LZ, Xu ZY, et al. Analysis of the current status and influencing factors of influenza vaccination among healthcare workers in Xining from 2019 to 2020. J Prev Med. (2022) 38:782–8. [Google Scholar]
- 84.Yan R, Li Z, Sun X, Wang BB, He HQ, Zhu Y. Analysis of influenza vaccine uptake and associated factors among healthcare workers in the Yangtze River Delta region during the 2020-2021 season. China J Prev Med. (2022) 56:1571–5. doi: 10.3760/cma.j.cn112150-20220727-00761 [DOI] [PubMed] [Google Scholar]
- 85.Li M, Sun B, Su JF, Zheng JD, Zhang SY, Xiao ZP, et al. Investigation of the status quo and influencing factors of influenza vaccination among primary healthcare workers in three provinces during the 2020-2021 influenza season. China J health educ. (2021) 37:1095–100. doi: 10.16168/j.cnki.issn.1002-9982.2021.12.008 [DOI] [Google Scholar]
- 86.Zhang B, Zhang X, Liu J, Song Y, An J, Zhang L, et al. Analysis of influenza vaccine uptake and associated factors among healthcare workers in the Yangtze River Delta region during the 2020-2021 season. China J Prev Med. (2022) 28:431–5. doi: 10.19914/j.CJVI.2022083 [DOI] [Google Scholar]
- 87.Wu ZL, Hao XN, Teng WJ. Influencing factors of psychological intention for influenza vaccination among medical staff in Qingdao City. China J Public Health. (2022) 38:716–8. doi: 10.11847/zgggws1129284 [DOI] [Google Scholar]
- 88.Lv LX, Li EG, Fu CW. Investigation on influenza vaccination rate and its influencing factors among community health workers in Jing’an district of Shanghai. China J Dis Control. (2021) 25:1459–62. doi: 10.16462/j.cnki.zhjbkz.2021.12.018 [DOI] [Google Scholar]
- 89.Fan ZL, Sun L, Yang XK, Zhou J, Zheng JD, Peng ZB, et al. Investigation of the knowledge, attitudes, and practices regarding influenza and influenza vaccination among primary healthcare workers in Weifang City. Forum Prev Med. (2022) 28:324–9. doi: 10.16406/j.pmt.issn.1672-9153.2022.05.019 [DOI] [Google Scholar]
- 90.Lei MY, Fang SZ, Yu C, Ping KK, Huang J, Gou Y, et al. Influenza vaccine uptake and influencing factors among healthcare workers before and after the outbreak of COVID-19. J Guizhou Univ Chin Med. (2022) 44:88–94. doi: 10.16588/j.cnki.issn2096-8426.2022.05.020 [DOI] [Google Scholar]
- 91.Ma L, Han X, Ma Y, Yang Y, Xu Y, Liu D, et al. Decreased influenza vaccination coverage among Chinese healthcare workers during the COVID-19 pandemic. Infect Dis Poverty. (2022) 11:105. doi: 10.1186/s40249-022-01029-0, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Papageorgiou C, Mazeri S, Karaiskakis M, Constantinou D, Nikolaides C, Katsouris S, et al. Exploring vaccination coverage and attitudes of health care workers towards influenza vaccine in Cyprus. Vaccine. (2022) 40:1775–82. doi: 10.1016/j.vaccine.2022.02.020, PMID: [DOI] [PubMed] [Google Scholar]
- 93.Ajejas Bazán MJ, Pérez-Rivas FJ, Wärnberg J. Flu vaccination coverage and predictors of non-vaccination in military health corps personnel 2016-2017 and 2019-2021. Vaccine. (2022) 10:10. doi: 10.3390/vaccines10030460, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bertoni L, Roncadori A, Gentili N, Danesi V, Massa I, Nanni O, et al. How has COVID-19 pandemic changed flu vaccination attitudes among an Italian cancer center healthcare workers? Hum Vaccin Immunother. (2022) 18:1978795. doi: 10.1080/21645515.2021.1978795, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Marinos G, Lamprinos D, Georgakopoulos P, Oikonomou E, Zoumpoulis G, Siasos G, et al. Increased influenza vaccination coverage among members of the Athens medical association amidst COVID-19 pandemic. Vaccine. (2022) 10:10. doi: 10.3390/vaccines10050797, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Shi X, Zhang Y, Zhou L, Zhou L, Qiao H. Influenza vaccination coverage among health-care workers during the COVID-19 epidemic in 2020/2021 influenza season: evidence from a web-based survey in northwestern China. Hum Vaccin Immunother. (2022) 18:2102354. doi: 10.1080/21645515.2022.2102354, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Jędrzejek MJ, Mastalerz-Migas A. Influenza increased influenza vaccination coverage among members of the Athens medical association amidst COVID-19 pandemic. Int J Environ Res Public Health. (2022) 19:19. doi: 10.3390/ijerph19031586, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Costantino C, Graziano G, Bonaccorso N, Conforto A, Cimino L, Sciortino M, et al. Knowledge, attitudes, perceptions and vaccination acceptance/hesitancy among the community pharmacists of Palermo’s province, Italy: from influenza to COVID-19. Vaccine. (2022) 10:10. doi: 10.3390/vaccines10030475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ogliastro M, Borghesi R, Costa E, Fiorano A, Massaro E, Sticchi L, et al. Monitoring influenza vaccination coverage among healthcare workers during the COVID-19 pandemic: a three-year survey in a large university hospital in North-Western Italy. J Prev Med Hyg. (2022) 63:E405–e414. doi: 10.15167/2421-4248/jpmh2022.63.3.2700, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary material.