Graphical abstract
Figure 2 – Graphical abstract (ambulance car pictographs by Lukas Huber, with kind permission).
Keywords: Prehospital emergency medicine research, Research car, Field supervisor, Paramedic, Paramedic research, Prehospital research, Cardiac arrest, Prehospital research car
Abstract
While the initial minutes of acute emergencies significantly influence clinical outcomes, prehospital research often receives inadequate attention due to several challenges. Retrospective chart reviews carry the risk of incomplete and inaccurate data. Furthermore, prehospital intervention trials frequently encounter difficulties related to extensive training requirements, even during the planning phase. Consequently, we have implemented prospective research concepts involving additional paramedics and physicians directly at the scene during major emergency calls. Three concepts were used: (I) Paramedic field supervisor units, (II) a paramedic + physician field supervisor unit, (III) a special physician-based research car. This paper provides insights into our historical perspective, the current situation, and the lessons learned while overcoming certain barriers and using existing and novel facilitators. Our objective is to support other research groups with our experiences in their planning of upcoming prehospital trials.
Background
Conducting prehospital research is challenging.1, 2, 3 The workload for emergency medical service (EMS) teams is high and further increases with disease- or trauma severity. Especially in situations of high research interest – sudden cardiac arrest, major trauma, and pediatric emergencies – the tasks at hand are so demanding that the treating EMS teams on site are often unable to perform additional – research related – duties. Moreover, several other issues regarding prehospital research have been identified in previous studies, such as obtaining an ethics committee approval (with restricted possibilities to acquire informed consent, especially in critically ill or injured patients), or the training of study-related procedures and subsequent adherence to the trial protocols.2 As a result, large resuscitation studies in recent years have typically initiated interventions only after admission to the hospital.4, 5, 6
However, the first minutes of acute emergencies – and, therefore, often the prehospital timeframe – are the most important for outcomes in several diseases, making them of utmost scientific interest.7 While the prehospital environment is often unpredictable, the presence of strict therapy algorithms and treatment protocols for paramedics provides a more standardized and, therefore, valuable potential research setting compared to in-hospital clinical research.8
To overcome the described issues, we developed a unique cooperation of researchers and special prehospital units of the EMS Vienna (EMS-V). The aim of this paper is to describe the historical perspective, the current situation, and our lessons learned with different concepts of prehospital research. These concepts will be introduced in the following sections to support other research groups in the development of similar research structures.
Historical situation and setting
The Department of Emergency Medicine at the Medical University of Vienna is the largest academic emergency medicine facility in Austria. Located at the General Hospital of Vienna, they annually treat about 300 patients with cardiac arrest, including 30–50 cases requiring extracorporeal cardiopulmonary resuscitation. Cardiopulmonary resuscitation (CPR) has been one of the department’s primary research interests since its opening in 1991. From the beginning, Professor Fritz Sterz cultivated a close cooperation with the municipal EMS-V. Additionally, they established a joint data exchange for a CPR outcomes database.
The EMS-V is responsible for all medical emergency calls within the capital city of Vienna, which has roughly 2 million inhabitants. Austria has a physician-based prehospital system, with physician units dispatched for major codes such as CPR, respiratory failure, or severe trauma).
Concepts of prehospital research in Vienna
I - Paramedic field supervisor units
For the CIRC trial (Autopulse® versus manual CPR) starting in 20099, a special unit vehicle was established in cooperation with EMS-V. This unit was staffed with a paramedic trainer from the rescue-academy and dispatched to all cardiac arrests. While randomization and the study itself were performed by the regular on-site teams, the paramedic trainer supervised the scene to ensure optimal guideline adherence and provided feedback after the call. Additionally, they were responsible for data collection by wire, as defibrillator files could not be collected telemetrically at that time. After initial reservations regarding a supervising paramedic, this system was well-received by the crews, and feedback was mainly appreciated. Consequentially, this special car was repurposed as a “Field Supervisor” unit (FISU) after completion of the trial. FISUs within EMS-V are now specifically trained and experienced paramedics dispatched to major trauma, cardiac arrest and pediatric emergencies to assist EMS teams in the field and ensure quality management.10 Their primary focus is on clinical supervision. Due to a standardized pit crew concept (see video-link below), the FISU can concentrate on time management and documentation during CPR calls. Currently, three FISUs are on duty 24/7. In addition to supervision, FISUs also collaborate in clinical research: (I) Close cooperation with the FISUs has facilitated the generation of our CPR outcomes database using reliable prehospital data. (II) FISUs have been and are responsible for the independent conduct of non-interventional studies (e.g., near-infrared spectroscopy during cardiac arrest).11 To avoid interfering with the supervision task of the FISUs, only studies with low time requirement are carried out in this setting.
II - Paramedic + physician field supervisor unit
From 2016, one of the FISUs was additionally staffed with a physician from our department for prospective research purposes on selected weekdays. Due to organizational reasons, this cooperation was terminated in 2019. In a second phase, starting in 2021 after the first COVID-19 waves, the FISU vehicles were again supplemented by a physician from the Department of Emergency Medicine, Anesthesiology, Clinical Pharmacology or the EMS-V for 12-hour day-shifts.
The decision to include a physician in the FISU was driven by several factors: (I) Austrian legislation mandates that the investigator for pharmaceutical and medical product trials must be a board certification physician.12, 13 Additionally, the local institutional review board insisted that, in the case of pharmaceutical studies, the study member on scene must also hold a doctor’s degree. Paramedics are only permitted to administer drugs following approved standard operating procedures, making it impossible to assign the administration of study drugs to selected (research) paramedics. (II) To ensure optimal guideline adherence during the studies, we decided to have the FISU primarily concentrate on clinical supervision and assume responsibility for smaller study-related tasks, while the physician’s main focus was directed towards the study measures. (III) Given that we were conducting multiple studies simultaneously, the workload associated with study management and supervision would have been overwhelming for a single individual. However, FISU cars were naturally dispatched to missions that were not subject of the current research focus due to the standard EMS-V dispatch order. In such cases, FISU paramedics carried out their routine duties, and the accompanying physicians offered to help with patient management in addition to the routinely dispatched emergency physician units on scene, but without the intent to replace emergency physicians. This, of course, made the exclusive dispatch of these cars to as many patients in the current research focus (e.g., CPR) as possible unfeasible. Thus, to increase study inclusion rates, a special prehospital research car (PRC) was introduced.
III - Prehospital research car
This PRC is equipped identically to a physician emergency car and staffed with a paramedic as a driver and a physician from the departments listed above. Finally, this PRC was dispatched only to cardiac arrest codes (the research focus back then) in addition to all regular EMS units, including the paramedic-FISU.
The PRC was stationed at the headquarters of the EMS-V in the city center. Thus, it was possible to reach the scenes in Vienna within a mean of 14 [interquartile range: 10–18] minutes after a cardiac arrest occurred. If the PRC was the first unit on the scene, the team performed advanced life support measures. After handover to the arriving regular units, study inclusion was then performed if possible. If a FISU was present, he/she remained responsible for clinical supervision, while the PRC focused on managing the study measures.
Comparison of the three concepts
The following Table 1 provides an overview of the advantages, disadvantages, costs, and inclusion rates of the three systems.
Table 1.
Advantages and disadvantages of the three systems.
| Paramedic Field Supervisor Units | Paramedic + Physician Field Supervisor Unit | Prehospital research car | |
|---|---|---|---|
| Advantages | - Established operating unit - highest coverage |
- no legal restrictions regarding the type of research - sufficient manpower for complex/multiple studies |
- no legal restrictions regarding the type of research - sufficient manpower for complex/multiple studies - potentially shorter time to first medical contact due to an additional car - disposition only to cardiac arrest calls |
| Disadvantages | - limited resources for study conductance due to super-vision tasks - legal restrictions (pharmaceutical or medical product studies not allowed) - disposition to major trauma, cardiac arrest, and pediatric emergencies (and not solely to cardiac arrest) |
- disposition to major trauma, cardiac arrest, and pediatric emergencies (and not solely to cardiac arrest) - potential for bias (second physician on scene) |
- additional unit on scene (situations with limited space) - potential for bias (second physician on scene, additional paramedic on scene) |
| Costs | - low costs (24/7 routine schedule in the EMS-V) | - additional costs (physician) | - highest costs (additional car, additional paramedic and physician) |
| Inclusion rates (shift = 12 h) | FISU-supervised cardiac arrests: 1056/1633 (64.7 %)* (=0.5 cardiac arrest pat. per shift and FISU unit) |
0.6 included patients per shift 0.9 study inclusions per shift |
1.7 included patients per shift 2.3 study inclusions per shift |
Time period: 3/1/21 – 2/28/22.
Lessons learned
The following “lessons learned” were generated based on the experiences during all study phases and the resulting discussions in periodic team meetings.
Sample size
The sample size calculations for our current CPR-related studies were based on the epidemiological city-wide cardiac arrest data from Nuernberger et al.14 However, all ongoing studies lasted longer than expected due to lower inclusion rates. We assume that this is due to the following aspects: (I) More than one CPR-call at the same time. (II) Cessation of resuscitation or return of spontaneous circulation (ROSC) prior to arrival of the study team. (III) Locations that were not approachable within a reasonable timeframe. (IV) The research team being the first on scene, necessitating clinical work rather than patient inclusion. (V) Limitation of space. We expected to have falsely high ROSC rates due to the long time from alert to scene, and thus cessation of resuscitation prior to our arrival. In fact, this was not the case: In patients with witnessed cardiac arrest, any ROSC rates were 34%, which is comparable to previously available data.14 In summary, studies following a similar system should allow for a longer inclusion period to achieve adequate power compared to those conducted in a more traditional way.
Ethics approval
Based on national legislation, research in patients unable to consent to study participation is challenging. Austrian law states that research in unconscious patients is only allowed if there is a possible benefit for each patient in the study. So far, we have successfully argued that a research car as well as a FISU provide this benefit as this concept can shorten the time to medical treatment and provide more personnel on the scene.
Planning phase and training
In the planning phase, we tested the practicability of various study measures in simulations with paramedics and physicians who were not involved in the respective trial designs (see Fig. 1). Also, the medical director of the EMS-V was involved from the start. Based on the feedback from these sessions, adaptions to the trial run sheets and the order of study-related measures were made. All studies were planned in a way that the regular EMS teams on scene did not have to modify their treatment. Further, trial-related activities were not to compromise routine patient care in any way. After completing the planning phase, all paramedics and physicians were informed about the study rationale and measures via e-mail. An additional webinar enabled prehospital staff to ask questions.
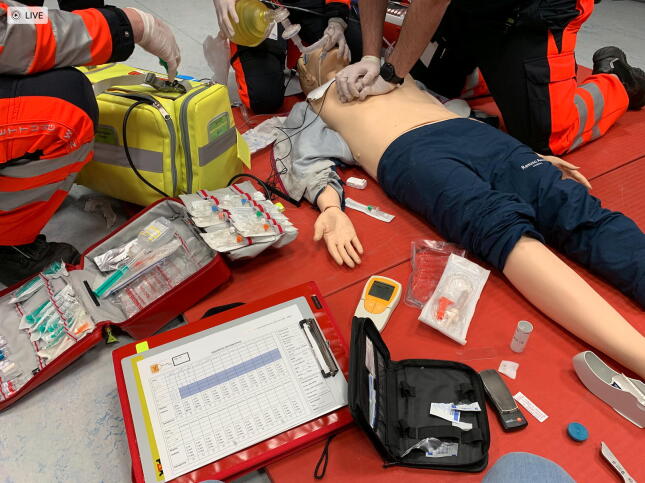
Fig. 1.
Training session.
The total number of physicians who could be on duty in the research car was purposely kept low so that we could optimally train them in a 1:1 fashion with one of the study coordinators and reduce potential inter-observer bias. For shifts on the PRC, a step-by-step protocol, checklists, and an inclusion criteria flowchart were provided to ensure the highest possible protocol adherence. A concise version of the respective inclusion criteria list was provided as a small endurable card so that It could be easily carried in a uniform pocket.
Ethical and tactical considerations on scene
In our opinion, it is imperative that the research staff on scene is trained and fully equipped for the prehospital environment for cases in which the research team is first on scene, and/or EMS personnel on scene is limited. As clinicians, it is our first and highest priority to achieve optimal patient care.
Of note, although the study team is only allowed to participate in patient care if it is absolutely necessary, the additional staff on scene could alter outcomes irrespective of study measures. This is especially true if additional measurements (lactate levels, brain perfusion, etc) are performed. To avoid this problem, the treating team was blinded to study related measurements as much as possible. We further declared that the study team is not allowed to participate in the decision to continue or terminate CPR at any time. Moreover, we decided to act as an ‘invisible study team’. This means that our staff wears ambulance uniforms without any labeling as a study team. This decision was widely discussed because the EMS teams provided feedback that clear labelling of arriving additional personnel would be desirable. Nevertheless, we think that relatives should not be irritated by labels like “research team” in situations of massive mental strain. To inform dispatched units about the arrival of a research unit, they were briefed via their radio data transmission (e.g., # study patient #, # study car #) and a short but clear verbal statement upon arrival on scene.
Nevertheless, there is a fine line between the need for optimal patient care and the best possible research. Cardiac arrest is undoubtedly one of the most standardized processes in prehospital medicine, with clear tasks for the involved personnel and widely accepted recommendations towards team sizes.15 However, in situations like major trauma, there could be an ethical issue concerning a physician on scene who is not included in patient care. Thus, for potential studies not focusing on CPR, this topic must be revisited.
Potential risk of bias
The use of additional staff on the scene bares the risk of bias. A shorter time to first medical contact is linked with outcomes.16 Although the research personnel was clearly instructed only to perform medical interventions in the absence of other EMS-units and immediately switch to study tasks after the arrival of subsequent units, we cannot deny that there are additional, highly trained personnel on scene. The existing literature presents conflicting findings regarding the impact of staff quantity on outcomes17, 18, 19, but there is a clear indication that their training status has the potential to improve resuscitation outcomes.20, 21 It is therefore essential that the study team remains in the background and, as far as possible, does not interfere with the care process.
Data collection and quality
One of the significant advantages of having a special team with a focus on research right on scene is the high and (mostly) complete data quality. However, trial run sheets should still be designed in a way that they can be completed in space-restricted or inconvenient situations (e.g., kneeling on the floor, being in the back of an ambulance car, etc.). To facilitate the completion of the form, time critical data (e.g., continuous measurements, time of ROSC, …) was arranged on the ‘initial page’, marked with a red frame. Non-time critical data (e.g., units on scene, patient’s age, preexisting diseases, …) that could also be filled out later were grouped on the following pages. This is contrary to ‘usual’ run sheets, but in our experience easier to handle in the prehospital situation. Of note, we tried to unify / merge the run sheets of the various parallel studies as much as possible to harmonize the flow of filling in data. After the initial completion, the run sheets were aligned and updated with the files from the defibrillators and the electronic (clinical) emergency protocols.
Funding
To date, the study-related equipment is funded in part by a governmental agency and a medical society. The research projects had to undergo a competitive peer-reviewed selection process in order to be funded. For staff, there is currently no external funding. Personnel comes from the Medical University of Vienna during their “science time” and senior physicians from the EMS-V. We are grateful to have this opportunity in times of staff shortage, although planning the roster is tough and sometimes incomplete. For the administration of case report forms, patient records and data from the defibrillators, we employed medical students on a project-related basis. Nevertheless, a significant amount of administrative work had to be conducted in the free time of the principal investigators. Broader and/or continuous funding would help to overcome this suboptimal situation in the future.
Considerations for the future
Currently, we exclusively approach adult cardiac arrest codes with our study car, resulting in extended standby times. In the future, we are considering conducting several studies in various fields of prehospital medicine to utilize the full capacity of the PRC.
Comparison to other systems
To our knowledge, a special physician-based car is unique in the field of prehospital research. Less physician centered legislation in other countries might enable systems with a paramedic-based research car, which could indeed be more cost-effective and could be a better solution in regions with staff shortages. Notably, a paramedic-based model is currently in use in the United Kingdom. For the CRASH-4 study (early treatment with tranexamic acid in head injury), the South Central Ambulance Service implemented a paramedic-based research car in 2022. According to early reports, they plan to host additional clinical trials using this platform.22
Limitations
Although our PRC is capable of producing high-quality research data, our concept has several limitations: First, the data originates from a capital city and may not be extrapolated to rural regions. Second, achieving a 100 % case coverage in cardiac arrest is not possible. Therefore, the resulting data cannot be considered of an epidemiological character. Third, even though our teams are trained to act in the background, it cannot be ruled out that the additional and skilled PRC-team may affect patient outcomes. Further, our concepts may not be applicable in lower-income countries or countries with a shortage of prehospital staff. The use of a physician for prehospital research is driven by the local legislation and might not be necessary elsewhere. However, a PRC-concept is easily adaptable also to purely paramedic-based systems.
Conclusion
Conducting prehospital research with a dedicated paramedic- and physician-based study car is feasible and facilitates research in the critical initial minutes of major emergency calls. By sharing details of this concept, we aim to encourage other research groups to apply our lessons learned to their projects.
Video Link: https://tinyurl.com/PCCCPR
Declaration of generative AI and AI-assisted technologies in the writing process
During the preparation of this work the authors used chatGPT for grammar and tense checks. After using this tool/service, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
CRediT authorship contribution statement
Matthias Mueller: Conceptualization, Methodology, Investigation, Data curation, Writing – original draft, Writing – review & editing, Project administration, Funding acquisition. Heidrun Losert: Conceptualization, Methodology, Investigation, Writing – review & editing, Project administration. Fritz Sterz: Conceptualization, Methodology, Investigation, Resources, Data curation, Writing – review & editing, Supervision. Georg Gelbenegger: Conceptualization, Methodology, Investigation, Data curation, Writing – review & editing. Michael Girsa: Resources, Writing – review & editing. Mathias Gatterbauer: Conceptualization, Investigation, Resources, Data curation, Writing – review & editing. Andreas Zajicek: Resources, Writing – review & editing. Daniel Grassmann: Conceptualization, Investigation, Writing – review & editing. Mario Krammel: Conceptualization, Resources, Data curation, Writing – review & editing, Supervision. Michael Holzer: Conceptualization, Methodology, Investigation, Data curation, Writing – review & editing, Supervision. Thomas Uray: Conceptualization, Methodology, Investigation, Data curation, Writing – review & editing, Supervision, Project administration. Sebastian Schnaubelt: Conceptualization, Methodology, Data curation, Writing – review & editing, Visualization, Funding acquisition.
Funding
This work was funded in parts by the Medical Scientific Fund of the Mayor of the City of Vienna (No. 21171) and by the Austrian Society for Medical and General Intensive Care Medicine and Emergency Medicine – ÖGIAIN (No. 02/2022).
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We want to thank Alexander Nürnberger, Bernhard Saxinger, Bertram Schadler, Lisa Christina Horvath, Calvin L. Kienbacher, Chiara Archam, Christian Prantl, Christoph Cincera, Domenic Zajicek, Florian Ettl, Georg Sulm, Gerhard Ruzicka, Gottfried Hanna, Harald Bendl, Harald Glück, Henrik Maszar, Ingrid A.M. Magnet, Julian Raming, Jürgen Novotny, Lukas Huber, Marcel Baloun, Marcel Pfaffenlehner, Marcus Schütz, Martin Muttenthaler, Martin Thalhammer, Mathias Gonzo, Matthias Gattringer, Michael Bösze-Schaffer, Michael Braun, Michael Mareda, Oliver Gangl, Philipp Berghoffer, Philipp Gonzo, René Adler, Ronald Kopta, Sabine Dunkl, Stefan Maier, Thomas Hamp, Wolfgang Terkl and all teams of the Emergency Medical Service of Vienna for their support.
References
- 1.Menegazzi J.J. Pragmatic Problems in Prehospital Research. Prehospital Disaster Med. 1993;8:S15–S19. doi: 10.1017/S1049023X00067479. [DOI] [Google Scholar]
- 2.Lerner E.B., Weik T., Edgerton E.A. Research in prehospital care: overcoming the barriers to success. Prehosp Emerg Care. 2016;20:448–453. doi: 10.3109/10903127.2014.980480. [DOI] [PubMed] [Google Scholar]
- 3.Sayre M.R., Gausche-Hill M. Conducting randomized trials in the prehospital setting. Prehosp Emerg Care. 2002;6:S38–S47. doi: 10.3109/10903120209102681. [DOI] [PubMed] [Google Scholar]
- 4.Dankiewicz J., Cronberg T., Lilja G., et al. Hypothermia versus normothermia after out-of-hospital cardiac arrest. N Engl J Med. 2021;384:2283–2294. doi: 10.1056/NEJMoa2100591. [DOI] [PubMed] [Google Scholar]
- 5.Eastwood G., Nichol A.D., Hodgson C., et al. Mild Hypercapnia or normocapnia after out-of-hospital cardiac arrest. N Engl J Med. 2023;389:45–57. doi: 10.1056/NEJMoa2214552. [DOI] [PubMed] [Google Scholar]
- 6.Schmidt H., Kjaergaard J., Hassager C., et al. Oxygen targets in comatose survivors of cardiac arrest. N Engl J Med. 2022;387:1467–1476. doi: 10.1056/NEJMoa2208686. [DOI] [PubMed] [Google Scholar]
- 7.Pepe P.E. Out-of-hospital resuscitation research: rationale and strategies for controlled clinical trials. Ann Emerg Med. 1993;22:17–23. doi: 10.1016/s0196-0644(05)80244-6. [DOI] [PubMed] [Google Scholar]
- 8.Pepe P.E., Copass M.K., Sopko G. Clinical trials in the out-of-hospital setting: rationale and strategies for successful implementation. Crit Care Med. 2009;37:S91–S. doi: 10.1097/CCM.0b013e318192154d. [DOI] [PubMed] [Google Scholar]
- 9.Wik L., Olsen J.-A., Persse D., et al. Manual vs. integrated automatic load-distributing band CPR with equal survival after out of hospital cardiac arrest. The randomized CIRC trial. Resuscitation. 2014;85:741–748. doi: 10.1016/j.resuscitation.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 10.Girsa M. Das Field-Supervisor System: Bewährte Praxis im Wiener Rettungsdienst [Transl.: The Field Supervisor System: Best practice in Vienna’s Emergency Medical Service] Rettungsdienst. 2019;10:44. [Google Scholar]
- 11.Schnaubelt S., Mayr F., Sterz F., Zajicek A., Uray T. Feasibility of continuous NIRS monitoring during out-of hospital cardiac arrest until 72 hours post-ROSC. Resuscitation. 2019;142:e10. [Google Scholar]
- 12.Bundesgesetz vom 2. März 1983 über die Herstellung und das Inverkehrbringen von Arzneimitteln (Arzneimittelgesetz – AMG); 2023.
- 13.Bundesgesetz betreffend Medizinprodukte 2021 (Medizinproduktegesetz 2021 – MPG 2021); 2023.
- 14.Nürnberger A., Sterz F., Malzer R., et al. Out of hospital cardiac arrest in Vienna: incidence and outcome. Resuscitation. 2013;84:42–47. doi: 10.1016/j.resuscitation.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 15.Soar J., Böttiger B.W., Carli P., et al. European Resuscitation Council Guidelines 2021: adult advanced life support. Resuscitation. 2021;161:115–151. doi: 10.1016/j.resuscitation.2021.02.010. [DOI] [PubMed] [Google Scholar]
- 16.Gräsner J.-T., Herlitz J., Tjelmeland I.B.M., et al. European Resuscitation Council Guidelines 2021: Epidemiology of cardiac arrest in Europe. Resuscitation. 2021;161:61–79. doi: 10.1016/j.resuscitation.2021.02.007. [DOI] [PubMed] [Google Scholar]
- 17.Warren S.A., Prince D.K., Huszti E., et al. Volume versus outcome: More emergency medical services personnel on-scene and increased survival after out-of-hospital cardiac arrest. Resuscitation. 2015;94:40–48. doi: 10.1016/j.resuscitation.2015.02.019. [DOI] [PubMed] [Google Scholar]
- 18.Eschmann N.M., Pirrallo R.G., Aufderheide T.P., Lerner E.B. The association between emergency medical services staffing patterns and out-of-hospital cardiac arrest survival. Prehosp Emerg Care. 2010;14:71–77. doi: 10.3109/10903120903349820. [DOI] [PubMed] [Google Scholar]
- 19.Hagiwara S., Oshima K., Aoki M., et al. Does the number of emergency medical technicians affect the neurological outcome of patients with out-of-hospital cardiac arrest? Am J Emerg Med. 2017;35:391–396. doi: 10.1016/j.ajem.2016.11.020. [DOI] [PubMed] [Google Scholar]
- 20.Sun J.-T., Chiang W.-C., Hsieh M.-J., et al. The effect of the number and level of emergency medical technicians on patient outcomes following out of hospital cardiac arrest in Taipei. Resuscitation. 2018;122:48–53. doi: 10.1016/j.resuscitation.2017.11.048. [DOI] [PubMed] [Google Scholar]
- 21.Kajino K., Kitamura T., Iwami T., et al. Impact of the number of on-scene emergency life-saving technicians and outcomes from out-of-hospital cardiac arrest in Osaka City. Resuscitation. 2014;85:59–64. doi: 10.1016/j.resuscitation.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 22.SCAS.NHS.UK 2022. https://www.scas.nhs.uk/pioneering-ambulance-research-initiative-delivering-speedy-treatment-for-head-injuries-in-older-people/.