Abstract
Background
Immersive virtual reality (iVR)-based digital therapeutics are gaining clinical attention in the field of pain management. Based on known analogies between pain and dyspnoea, we investigated the effects of visual respiratory feedback on persistent dyspnoea in patients recovering from coronavirus disease 2019 (COVID-19) pneumonia.
Methods
We performed a controlled, randomised, single-blind, crossover proof-of-concept study (feasibility and initial clinical efficacy) to evaluate an iVR-based intervention to alleviate dyspnoea in patients recovering from COVID-19 pneumonia. Included patients reported persistent dyspnoea (≥5 on a 10-point scale) and preserved cognitive function (Montreal Cognitive Assessment score >24). Assignment was random and concealed. Patients received synchronous (intervention) or asynchronous (control) feedback of their breathing, embodied via a gender-matched virtual body. The virtual body flashed in a waxing and waning visual effect that could be synchronous or asynchronous to the patient's respiratory movements. Outcomes were assessed using questionnaires and breathing recordings.
Results
Study enrolment was open between November 2020 and April 2021. 26 patients were enrolled (27% women; median age 55 years, interquartile range (IQR) 18 years). Data were available for 24 of 26 patients. The median rating on a 7-point Likert scale of breathing comfort improved from 1 (IQR 2) at baseline to 2 (IQR 1) for synchronous feedback, but remained unchanged at 1 (IQR 1.5) for asynchronous feedback (p<0.05 between iVR conditions). Moreover, 91.2% of all patients were satisfied with the intervention (p<0.0001) and 66.7% perceived it as beneficial for their breathing (p<0.05).
Conclusion
Our iVR-based digital therapy presents a feasible and safe respiratory rehabilitation tool that improves breathing comfort in patients recovering from COVID-19 infection presenting with persistent dyspnoea. Future research should investigate the intervention's generalisability to persistent dyspnoea with other aetiologies and its potential for preventing chronification.
Tweetable abstract
iVR-based DTx presents a feasible and safe respiratory rehabilitation tool that improves breathing comfort in patients recovering from COVID-19 infection presenting with persistent dyspnoea https://bit.ly/3YFnRIj
Introduction
Dyspnoea is defined as “a subjective experience of breathing discomfort made of various sensations that can vary in intensity” [1]. In simpler words, dyspnoea relates to the upsetting or distressing awareness of breathing activity. Beyond the symptom of cardiorespiratory dysfunction, dyspnoea is a frightening and disabling experience. This is particularly true when it resists optimised treatment of the underlying condition, a situation termed “chronic breathlessness” [2] or, more broadly, “persistent dyspnoea” [3]. Persistent dyspnoea deeply affects the lives of those afflicted. It profoundly deteriorates quality of life by affecting cognitive function, locomotion and mental health [4]. Implicit in the definition of persistent dyspnoea is the under-recognition of respiratory distress by caregivers (e.g. during clinical consultations) [5], which is a major clinical burden. This invisibility, an important difference between dyspnoea and pain, impairs access to care [5] and hinders the development of evidence-based targeted interventions [6]. The aim of the current study was, therefore, to develop and evaluate a noninvasive, nonpharmacological intervention that would use immersive virtual reality (iVR) to alleviate breathlessness in a clinical population, drawing on promising approaches that have also used embodied iVR for chronic pain.
Neuroscience evidence suggests that dyspnoea occurs in conjunction with the recruitment of a neural network involving the insula, dorsal anterior cingulate cortex, amygdala and medial thalamus, sharing important pathways with other brain functions such as pain processing [7] and bodily self-consciousness [8]. This evidence suggests that targeting the brain to relieve dyspnoea is a feasible option when all cardiorespiratory approaches have been exhausted [9].
In this regard, prior interventions using iVR-based digital therapeutics, also referred to as digiceuticals [10], have demonstrated alleviation of chronic pain in patients with complex regional pain syndrome or spinal cord injury [9, 11]. In the respiratory domain, visuo-respiratory stimulation has been associated with an increased feeling of breathing control (breathing agency) [12], a reduced negative emotional state related to experimental dyspnoea [13] and changes in physiological measures of breathing [14, 15].
Persistent symptoms can occur beyond the initial period of coronavirus disease 2019 (COVID-19) infection recovery and affect patients who are managed in the community or in the acute care setting [16]. Like general weakness, malaise, fatigue and impaired concentration, dyspnoea has consistently been reported in so-called long COVID cohorts with a high prevalence of ∼25% (95% CI 18–34%) [17]. In the case of persistent dyspnoea, an extensive workup to identify respiratory sequelae or muscle deconditioning should be the foremost clinical preoccupation, mostly to guide the indications of pulmonary rehabilitation [18]. However, dyspnoea can be dissociated from physiological markers such as pulmonary function tests or lung imaging in post-COVID situations [17] as well as more generally [19]. This makes treatment and even diagnosis challenging. The importance of brain mechanisms in the pathogenesis of dyspnoea justifies neuroscientific approaches for its management and implies that a cognitive intervention using a neuro-rehabilitation approach could be tested to understand and alleviate this debilitating symptom.
The present clinical study was performed to evaluate two primary outcomes: 1) the initial clinical efficacy of the COVID Virtual Reality (COVVR) intervention and 2) the overall feasibility of using iVR in patients recovering from COVID-19 pneumonia. This study followed the guidelines for clinical trials using VR and corresponds to a VR phase 2 trial [20]. The primary hypothesis with respect to efficacy was that our iVR intervention would alleviate dyspnoea by improving breathing comfort in patients recovering from COVID-19 pneumonia presenting with persistent dyspnoea. With respect to the feasibility of COVVR, we hypothesised that the intervention could be used in an inpatient setting and would be accepted by the patients. We also had two research questions regarding potential perceptual changes in patients affected by persistent dyspnoea: 1) do patients maintain accurate awareness of their breathing movements and 2) do they maintain their sense of agency, or control, over their breathing [16]?
Methods
Study design
A prospective controlled, randomised, single-blind, crossover clinical study was conducted to evaluate both the efficacy and feasibility of an iVR biofeedback intervention to alleviate persistent dyspnoea in patients recovering from COVID-19 pneumonia. This single-site study was carried out at the University Hospital (HUG) in Geneva, Switzerland, and was approved by the Commission Cantonale d'Ethique de la Recherche de la République et Canton de Genève (2019-02360).
Patients
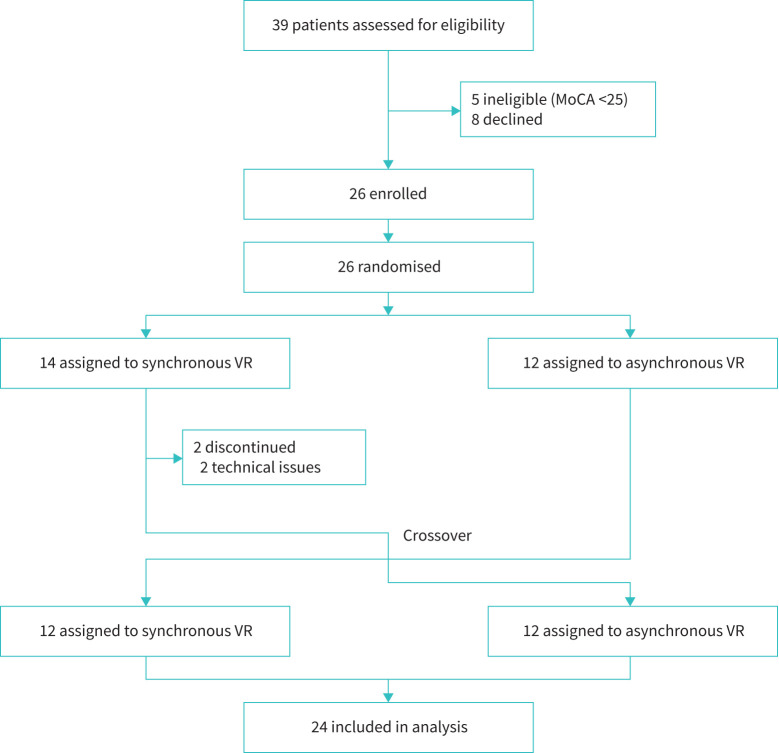
39 patients were screened by a respiratory physician (AS). Patients that scored <25 points on the Montreal Cognitive Assessment were excluded (n=5); eight declined to participate. In total, 26 patients were enrolled (figure 1). Clinical inclusion criteria were that patients 1) were recovering from COVID-19 pneumonia confirmed by reverse transcription PCR for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and 2) presented with persistent dyspnoea with a self-rated intensity of ≥5 (out of 10) on a visual analogue dyspnoea scale, at rest. The respiratory physician asked the dyspnoea question: “Do you have difficulty breathing?” then “On a scale of 0 to 10, with 0 being no difficulty to breathe and 10 being the worst difficulty to breathe that you can imagine, where do you rank?” This dyspnoea rating was only used as an inclusion criterion and not as an outcome. The delay between the initial screening by the physician and the inclusion by the researcher varied between 1 h and 2 days. As discussed below, a separate set of questions was used to evaluate the primary outcomes, because they could be directly compared to the prior studies on respiration awareness. Patients had to be able to give consent and to understand and speak French or English. Patients who presented with unstable respiratory, neurological or cardiac conditions or with psychiatric illness were excluded (supplementary material: Screening). Patients underwent randomisation in the respiratory ward during the recovering phase of COVID pneumonia only if they were in a stable respiratory, neurological or cardiac clinical condition.
FIGURE 1.
Study flow chart. MoCA: Montreal Cognitive Assessment.
Procedure
Setup
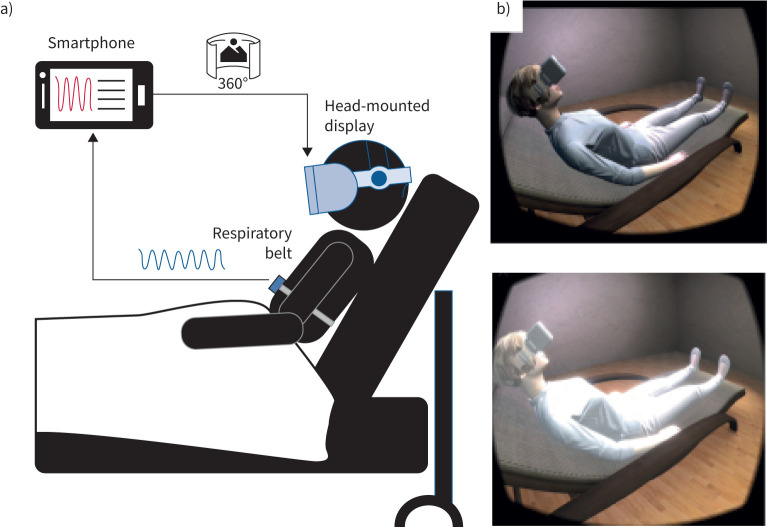
Eligible patients were installed in a semi-seated position in their hospital bed (figure 2) and wore a belt-mounted linear force sensor (Go Direct Respiration Belt; Vernier, Beaverton, OR, USA) fitted on the abdomen to allow proper recording of respiratory movements. They were also equipped with a head-mounted display (Zeiss VR ONE Plus, Oberkochen, Germany) holding a smartphone (Samsung Galaxy S8, Seoul, South Korea). The smartphone ran the VR application and connected via Bluetooth to the respiration belt. MindMaze SA (Lausanne, Switzerland) provided the hardware for the study, co-developed the application with the Laboratory of Cognitive Neuroscience at Ecole Polytechnique Federale de Lausanne and deployed this on the smartphone. The application collects and processes respiratory data to render a computer-generated virtual environment in real-time.
FIGURE 2.
Portable setup and virtual reality feedback. a) A respiratory belt captures the respiratory movements of the chest and sends the signal to a smartphone via Bluetooth. Bespoke software generates the virtual environment. b) A matched-gender virtual body is displayed and observed by the patients by slightly turning their head to the side. The virtual body is illuminated synchronously or asynchronously with respect to the patient's chest movements. The top image represents the end of the expiration with a low flashing intensity, while the bottom image shows the end of the inspiration corresponding to the maximal luminosity in the synchronous condition. A video of the experiment can be found in the supplementary material.
Intervention conditions
Patients were asked to look around in the VR environment and orient their gaze to a gender-matched virtual body lying on a bed next to them in a similar position to theirs (figure 2b) [12, 13, 15]. The virtual body flashed in a waxing and waning visual effect which could be synchronous or asynchronous to the patient's respiratory movements. In the synchronous condition, the radiance of the visual flash was maximal at the end of inspiration and minimal at the end of the expiration. In the asynchronous condition, at the end of each visual flash, a duration between 2.5 s and 33.3 s was randomly generated for the next visual stimulation, such that the feedback was both phase-shifted and frequency-modulated with respect to the actual respiration.
Intervention procedure
Once the patient was ready, they were asked to close their eyes while their respiratory movements were recorded for 2 min. Participants were then asked to describe their current respiratory experience by answering two questions according to a classically used 7-point Likert scale (from −3=strongly disagree to +3=strongly agree): 1) “I have difficulty breathing” (breathing difficulty) and 2) “My breathing is enjoyable” (breathing comfort) [12, 13, 15, 21]. Questions were asked to patients in French. This condition served as the baseline assessment for the breathing (dis)comfort items and the breathing rate. For comparison, the two items were also included in the post-exposure questionnaires.
After baseline assessment, participants were randomly assigned in a 1:1 ratio to receive either the sequence “synchronous/asynchronous” or “asynchronous/synchronous” (supplementary material: Randomisation and masking). In each block, patients were first asked to look around in the virtual room, and then to orient their gaze towards the virtual body while relaxing for 5 min. They were not informed that the flashing of the virtual body was related to their breathing. Each block was followed by a subjective questionnaire of six items (7-point Likert scale) derived from previous visuo-respiratory studies (table 1) [12, 13, 15]. Question 1 evaluated the awareness of the visuo-respiratory experimental manipulation (breathing awareness) [12, 15], while question 3 pertained to breathing agency [12, 13, 15]. Questions 2 and 5 were included as control items. These should not have differed between conditions but could flag if participants were influenced by baseline suggestibility. The breathing comfort items matched the baseline assessment (Q4 and Q6 respectively, table 1). Finally, patients completed an ad hoc questionnaire to assess the acceptance and feasibility of the iVR intervention (7-point Likert scale, supplementary table S1). During the entire intervention (baseline included), oxygen therapy was administered through nasal cannulas to obtain a peripheral oxygen saturation of 90–92%.
TABLE 1.
Subjective questionnaire items
| Items | Domain | |
| Q1 | It seemed as if the flashing was my respiration | Breathing awareness |
| Q2 | It seemed as if I had three bodies | Control |
| Q3 | I felt as if the virtual body was breathing with me | Breathing agency |
| Q4 | I had difficulty breathing | Breathing difficulty |
| Q5 | I felt as if the virtual body was drifting with the flashing | Control |
| Q6 | My breathing was enjoyable | Comfort |
Outcomes
Following the recommendations for clinical trials in VR, we conducted a VR2-type study with a focus on initial clinical efficacy and intervention feasibility as two primary outcomes [20]. Efficacy was evaluated based on subjective feedback from the patients regarding their breathing comfort and difficulty (Q4 and Q6 of table 1). Feasibility was evaluated using a feedback questionnaire. Agreement with the questionnaire items indicates better feasibility, acceptance and perceived outcome.
Secondary outcome measures included respiratory parameters and the subjective reports of breathing awareness and agency. Both respiratory rate (breaths·min−1) and respiratory rate variability (using inter-breath intervals) were measured using the respiration belt. Respiratory rate and variability were compared across the baseline and two intervention conditions. Breathing awareness and agency were evaluated using a 7-point Likert scale where agreement indicates stronger embodiment of the feedback.
The feedback questionnaires were administered by the researcher, directly after the intervention.
Statistical analysis
All analyses were performed using R (version 4.1.0, www.r-project.org) and MATLAB (version 2020a, MathWorks, Natick, MA, USA). The effect of synchrony on each measure was assessed using a linear mixed-effects model [22], with a random intercept for each patient. In addition to the experimental condition (synchronous versus asynchronous condition), each model also included the experimental sequence (starting the experiment with synchronous or asynchronous condition) and the interaction between the experimental sequence and the experimental condition as fixed effects. The statistical significance of the interactions was assessed using the likelihood ratio test. All p-values were two-sided and statistical significance was set at a p-value of 0.05.
Median, interquartile range (QR) and rating frequency (%) were computed for each feasibility item. To ensure clarity, observed percentages for ratings from 1=agree to 3=strongly agree were grouped, indicating overall agreement with the statement. A one-sided, one-sample t-test was used to determine if the mean of ratings was significantly greater than zero, indicating that at least the majority of patients were agreeing with the statement. Details regarding the power calculation and risk assessment are in the supplementary material.
Results
Demographic and baseline information
Patient enrolment, randomisation and testing took place at the Division of Pneumology at Geneva University Hospital between November 2020 and April 2021. 26 patients were randomly assigned either to the “asynchronous/synchronous” sequence (n=12) or the “synchronous/asynchronous” sequence (n=14). At the time of database lock in May 2021, data were available for all except two of 26 patients (7.7%) (table 1).
Subjective and physiological measures are reported in table 2. At baseline, the median breathing comfort rating was 1 (IQR 2) and the mean breathing difficulty rating was 1 (IQR 3). Median values and IQRs for each experimental condition as per the experimental sequence are provided in supplementary table S2.
TABLE 2.
Characteristics of the patients at randomisation in the intent-to-treat population and primary and secondary outcomes
| Total | Synchronous first | Asynchronous first | |
| Patients, n | 26 | 14 | 12 |
| Patient characteristics | |||
| Gender, n (%) | |||
| Male | 19 (73) | 11 (79) | 8 (67) |
| Female | 7 (27) | 3 (21) | 4 (33) |
| Age (years) | 55 (18), 35–81 | 55 (18), 38–81 | 56.5 (16.75), 35–73 |
| MoCA | 27 (3), 25–30 | 27.5 (1.75), 25–30 | 27 (4.24), 25–30 |
| SpO2 on oxygen therapy# | 94 (4.3), 90–98 | 95 (5.5), 90–98 | 92.5 (4), 91–96 |
| Oxygen flow (L·min−1)# | 1 (3), 0–8 | 2 (2), 0–8 | 0.25 (1.75), 0–4 |
| Heart rate (beats·min−1)# | 74.5 (22), 52–108 | 79.5 (24.5), 62–108 | 70.5 (11.5), 62–92 |
| Days since first symptom onset# | 17 (22), 3–39 | 14 (21), 3–39 | 18.5 (16.25), 6–37 |
| Contagious at time of testing, n (%) | 16 (62) | 10 (71) | 7 (58) |
| Primary outcomes | |||
| Breathing comfort | 1 (2), −3–2 | 0 (2), −3–2 | 1 (3.25), −2–2 |
| Breathing difficulty | 1 (3), −3–2 | 1 (3), −3–2 | 0 (3.25), −3–2 |
| Secondary outcomes | |||
| Respiratory rate (breaths·min−1) | 21 (10), 7–35 | 21 (10), 15–32 | 22 (10), 15–35 |
| Respiratory rate variability (breaths·min−1) | 3 (2), 1–12 | 3 (2), 1–12 | 3 (2), 1–5 |
Data are presented as median (IQR), range, unless otherwise stated. MoCA: Montreal Cognitive Assessment; SpO2: peripheral oxygen saturation; IQR: interquartile range. #: data were missing for some patients and the denominator in the asynchronous group was 10.
Primary outcomes
Efficacy of the intervention on breathing comfort and difficulty
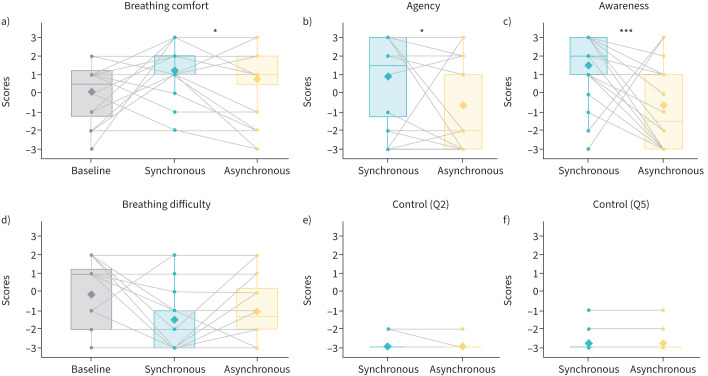
Results on the efficacy of the intervention are presented in table 3. Regarding the primary outcome of breathing comfort, we observed that the median rating significantly improved from 1 (IQR 1.5) during the asynchronous condition to 2 (IQR 1) during the synchronous condition, with an estimated difference between conditions of 0.54 (95% CI 0.05–1.04, p<0.05, figure 3a). Moreover, post hoc paired one-sided t-tests confirmed a significant difference between breathing comfort ratings during the intervention (synchronous) condition compared to baseline. No such difference was observed for the control (asynchronous) condition, excluding a mere effect of VR distraction (see supplementary material for statistical details). For the assessment of breathing difficulty, even though a similar trend was observed in the data, no significant main effect of experimental condition was observed (figure 3d). The experimental sequence had no significant effect on breathing comfort or breathing difficulty ratings.
TABLE 3.
Results summary for the subjective and physiological measures
| β (95% CI ) | p-value | |
| Breathing comfort | ||
| Main effect of synchrony# | 0.542 (0.046–1.037) | 0.033 |
| Asynchronous first¶ | 0.25 (−0.627–1.127) | 0.223 |
| Synchronous first+ | −0.583 (−1.544–0.378) | |
| Breathing difficulty | ||
| Main effect of synchrony# | −0.5 (−1.064–0.064) | 0.080 |
| Asynchronous first¶ | −1.333 (−2.260– −0.407) | 0.221 |
| Synchronous first+ | −0.667 (−1.760–0.427) | |
| Agency | ||
| Main effect of synchrony# | 1.583 (0.335–2.832) | 0.014 |
| Asynchronous first¶ | −0.667 (−1.922–0.589) | 0.336 |
| Synchronous first+ | 1.167 (−1.285–3.618) | |
| Awareness | ||
| Main effect of synchrony# | 2.167 (1.068–3.266) | <0.0001 |
| Asynchronous first¶ | 0.167 (−0.894–1.227) | 0.064 |
| Synchronous first+ | 2 (−0.121–4.121) | |
| Control (Q2) | ||
| Main effect of synchrony# | 0.042 (−0.042–0.125) | 0.312 |
| Asynchronous first¶ | −3.000 (−3.135– −2.865) | 0.302 |
| Synchronous first+ | 0.083 (−0.080–0.246) | |
| Control (Q5) | ||
| Main effect of synchrony# | Did not converge because data were similar in both conditions | |
| Asynchronous first¶ | ||
| Synchronous first+ | ||
| Respiration rate | ||
| Main effect of synchrony# | −0.275 (−1.748–1.198) | 0.704 |
| Asynchronous first¶ | 23.346 (19.460–27.231) | 0.053 |
| Synchronous first+ | 2.685 (−0.041–5.410) | |
| Respiration rate variability | ||
| Main effect of synchrony# | −0.295 (−0.779–0.190) | 0.222 |
| Asynchronous first¶ | 4.594 (3.344–5.843) | 0.810 |
| Synchronous first+ | −0.114 (−1.082–0.854) | |
Subjective ratings were measured using a 7-point Likert scale with −3=strongly disagree; −2=disagree; −1=somewhat disagree; 0=neither agree nor disagree; 1=somewhat agree; 2=agree; and 3=strongly agree. #: mean difference between synchronous and asynchronous conditions, regardless of the sequence, and 95% CI estimated by the linear mixed model (p-value corresponds to the test of this difference being equal to zero); ¶: mean difference between synchronous and asynchronous conditions and 95% CI estimated by the linear mixed model for the experimental sequence “Asynchronous first” (p-value corresponds to the result of the interaction test); +: mean difference between synchronous and asynchronous conditions and 95% CI estimated by the linear mixed model for the experimental sequence “Synchronous first” (the p-value corresponds to the result of the interaction test).
FIGURE 3.
Breathing comfort (a), agency (b), awareness (c), breathing difficulty (d) and control item (e, f) test results. a–c) Subjective measures for which the main effect of the experimental manipulation was significant. *: p<0.05; ***: p<0.001. d–f) Subjective measures for which the main effect of the experimental manipulation was nonsignificant. The boxplots depict subjects’ ratings during the asynchronous condition compared to the synchronous condition, independent of experimental sequence. The thick line within a boxplot represents the median, the diamond represents the mean, the upper boundary of the box indicates the 25th percentile (Q1) and lower boundary the 75th percentile (Q3). The whiskers above and below the box indicate the minimal and maximal values (Q1–1.5×IQR and Q3+1.5×IQR, respectively), while points above the upper or below the whiskers indicate outliers. Subjective ratings were measured using a 7-point Likert scale with −3=strongly disagree, −2=disagree, −1=somewhat disagree, 0=neither agree nor disagree, 1=somewhat agree, 2=agree, and 3=strongly agree.
Feasibility of the intervention
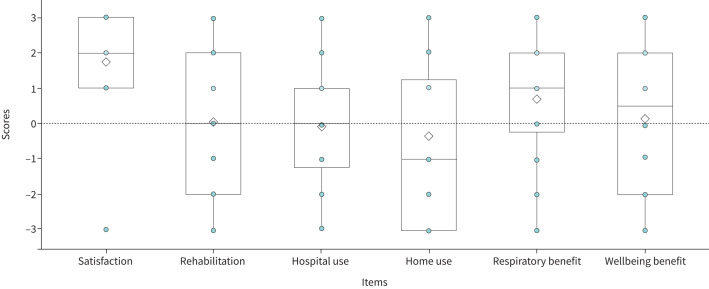
Feasibility ratings, the co-primary outcome, are depicted in figure 4. The majority of patients (91.2%) were satisfied with the intervention (Satisfaction: median 2 (IQR 2), t=5.20, p<0.0001, 95% CI 1.17–∞). In addition, 66.7% rated the iVR intervention as beneficial for their breathing (Respiratory benefit: median 1 (IQR 2.25), t=1.81, p<0.05, 95% CI 0.04–∞). Half of the patients reported that it made them feel better (Wellbeing benefit: median 0.5 (IQR 4), t=0.36, p>0.05, 95% CI −0.64–∞) and a further 45.8% indicated that they would like to continue using the device during their recovery (Rehabilitation: median 0 (IQR 4), t=0.10, p>0.05, 95% CI −0.67–∞) and at home (Home use: median −1 (IQR 4.25), t= −0.74, p>0.05, 95% CI −1.11–∞). Finally, 37.5% would have liked to use the intervention earlier during their stay at the hospital (Hospital use: median 0 (IQR 2.25), t= −0.22, p>0.05, 95% CI −0.74–∞). Descriptive statistics and statistical tests are described in supplementary table S3 and figure S2.
FIGURE 4.
Feasibility scores for all items. The boxplots depict subjects’ ratings for feasibility items. The thick line within a boxplot represents the median, the diamond represents the mean, the upper boundary of the box indicates the 25th percentile (Q1) and lower boundary the 75th percentile (Q3). The whiskers above and below the box indicate the minimal and maximal values (Q1–1.5×IQR and Q3+1.5×IQR, respectively), while points above the upper or below the whiskers indicate outliers. Subjective ratings were measured using a 7-point Likert scale with −3=strongly disagree, −2=disagree, −1=somewhat disagree, 0=neither agree nor disagree, 1=somewhat agree, 2=agree, and 3= strongly agree.
Secondary outcomes
Effect of the intervention on subjective reports of breathing awareness and agency
The secondary outcome measures of this study included the subjective ratings for breathing awareness and agency and the physiological measures. The median breathing agency rating increased from −2 (IQR 4) during the asynchronous condition to 1.5 (IQR 4.25) during the synchronous condition, with an estimated difference of 1.58 (95% CI 0.34–2.83, p<0.05, figure 3b). The median breathing awareness rating increased from −1.5 (IQR 4, asynchronous) to 2 (IQR 2, synchronous), with an estimated difference of 2.17 (95% CI 1.07–3.27, p<0.0001, figure 3c). Neither control item differed between conditions (“It seemed as if I had three bodies”, figure 3e; “I felt as if the virtual body was drifting with the flashing”, figure 3f).
Effect of the intervention on respiratory parameters
Respiration rate and its variability did not differ between experimental conditions. The order of conditions did not significantly affect any of the secondary outcomes (supplementary figure S1).
Discussion
In this study, our COVID VR intervention (COVVR) improved breathing comfort in patients with persistent dyspnoea recovering from COVID-19 pneumonia. Persistent dyspnoea, a common but underreported condition, is defined as the breathlessness reported by patients despite receiving state-of-the-art treatment of their respiratory condition. It leads to major disabilities impacting cognition, locomotion and mental health [4, 6, 23]. COVVR may therefore provide an additional noninvasive and nonpharmacological tool for aiding patient recovery and satisfaction, with the potential of alleviating some of the burden of this debilitating symptom.
Patients reported a significant improvement in breathing comfort after a relatively short exposure (5 min) to synchronous visuo-respiratory COVVR stimulation compared to the asynchronous control condition and compared to their baseline breathing comfort. Our results extend recent observations in chronic pain studies [11] to patients with persistent dyspnoea. This previous iVR work indicated the value of personalised stimulation using cardio-visual [8, 11], somatosensory-visual [9] and respiratory-visual feedback [12, 13, 15]. These studies using multisensory bodily stimulations, including the present VR protocol, differ from previous interventions focused on using 1) immersive or non-immersive VR as a distraction tool [24] or 2) the more recent efforts to digitise patient education and cognitive behavioural therapy [25]. By contrast, these studies were designed to impact the central processing of nociceptive and respiratory signals, respectively. The specificity of these personalised iVR interventions, including COVVR, is highlighted by the crossover randomised design of our study differing only in respiratory synchrony (synchronous versus asynchronous conditions), while being identical in all other aspects of VR exposure (e.g. presence of a virtual body animated by patient's own breathing, total duration of breathing sequence, identical three-dimensional virtual environment). This is markedly different from the more commonly applied, non-immersive VR stimulations prevalent in medical research [11, 21, 22].
Alongside the positive primary outcome, a similar beneficial effect of the intervention was observed for breathing agency, i.e. the feeling of being in control of one's breathing. Patients reported a stronger sense of control over their breathing for synchronous feedback and maintained awareness of their breathing movements. Patients further reported global satisfaction regarding the VR intervention and, more importantly, indicated that the iVR feedback improved their breathing. The COVVR study extends respiratory iVR studies in healthy individuals that have demonstrated increased breathing agency [12, 13, 15] and changes in tidal volume variability [15], and translates this approach to the bedside. Monitoring these markers, and the patient's emotional state [17], may be instrumental in decreasing dyspnoea-related anxiety and understanding its chronification.
While synchronous visuo-respiratory stimulation improved one item used for the assessment of dyspnoea (Q6: “My breathing was more enjoyable”), synchronous stimulation was only associated with a nonsignificant improvement in the other item used for this assessment (Q4: “I had difficulty breathing”). The most probable reason for this finding is a lack of power related to our sample size. Another reason is that, although participants reported persistent dyspnoea with a self-rated intensity of ≥5 when screened by the respiratory physician, their agreement with item Q4 was quite low just prior to the VR intervention, indicating a possible “white coat” effect. The semantics of the chosen items could also explain this finding. The item “My breathing is enjoyable” taps into affective processes whereas the item “I have difficulty breathing” explores sensory/perceptual processes [14]. Further work should compare both breathing comfort and breathing difficulty items to validated respiratory questionnaires.
Mounting evidence using functional neuroimaging suggests that patients with persistent dyspnoea may exhibit “hypersensitivity” to afferent respiratory signals as a result of learned expectations [26]. Perception and anticipatory processes of dyspnoea are known to share breathing control mechanisms in the brainstem and the insular cortex [26]. Consequently, once treatment of the underlying respiratory pathophysiology has been optimised, these neurorespiratory mechanisms should be considered as potential targets for pharmacological and nonpharmacological interventions [27]. Pharmacological treatments have been shown to be useful: low dose oral sustained-release morphine administered for persistent dyspnoea is associated with improved health status in COPD without affecting arterial carbon dioxide tension or causing serious side-effects (especially in patients with modified Medical Research Council stage 3–4 dyspnoea) [28]. Pulmonary rehabilitation, an evidence-based multidisciplinary nonpharmacological intervention, has also been shown to modify neural responses to learned breathlessness associations, likely due to central desensitisation to dyspnoea [29]. While not directly investigating neurorespiratory mechanisms, the present iVR paradigm, using carefully controlled visuo-respiratory conflicts, not only introduces a new complementary rehabilitation intervention but may help identify subjective (agency, awareness, dis/comfort) and physiological (breathing rate and variability) markers of hypersensitivity, based on perceptual and anticipatory brain processes of dyspnoea.
Digital therapeutics are becoming popular in the field of chronic pain management [24]. Dyspnoea and pain share several similarities [7]. They engage similar brain networks [7], are best characterised by multidimensional models [23] and both respond to opioid treatment. As the global COVID-19 pandemic has progressed, a significant proportion of patients experience prolonged symptoms beyond the initial period of acute infection, such as persistent dyspnoea [17]. The increasing number of patients isolated for prolonged periods has stressed the urgent need to develop multidisciplinary rehabilitation strategies that can be individualised and adapted to accommodate patients’ needs [30]. Given our findings, we propose that our iVR intervention is a feasible and safe neuro-rehabilitation tool that could be considered to improve breathing comfort in patients experiencing persistent dyspnoea after COVID-19 infection. Because our intervention involves neurorespiratory processes, its use could further be extended to persistent dyspnoea with other aetiologies. Offering a nonpharmacological, noninvasive intervention that can readily be adapted for home use may be particularly relevant at a time when over 40% of adults are estimated to avoid medical care because of COVID-19-related concerns [31].
Our study comes with certain limitations. First, although it is based on an adequate power calculation for a proof-of-concept study, our results stem from a small sample. Eight participants (20%) refused to participate; unfortunately reasons for refusal were not recorded. It is therefore possible that selection biases have contributed to our results. Second, almost half of the patients who were selected as being severely dyspnoeic (i.e. visual analogic dyspnoea scale ≥5) reported low agreement with the breathing difficulty item at baseline. This may be due to the delay between the initial screening and the start of the intervention or the fact that the former was completed by the respiratory physician and the latter by a researcher. Further studies should also include validated multidimensional dyspnoea scales [32], such as the Multidimensional Dyspnea Profile [33], because a multidimensional outcome would be ideal. While we here focused on a specific population of patients recovering from COVID-19 infection, our intervention should be tested in a larger cohort of patients with persistent dyspnoea to improve generalisability. Another important unanswered question is whether the effects observed after this short intervention can persist when patients are off-treatment. Nonetheless, our data demonstrate the value and adaptability of a personalised iVR intervention for clinical use based on commercially available VR hardware. Lastly, longer-term dyspnoea studies should, aside from the primary health and patient satisfaction outcomes, assess the economics of implementing this intervention as has been done for pain therapy in hospitalised patients [34].
In conclusion, our study shows that a short exposure to an iVR-based digital therapeutic can improve breathing comfort and breathing control in patients recovering from COVID-19 pneumonia. Global satisfaction and respiratory benefit from the patients are reported, attesting to the feasibility of the present intervention. Although more clinical data are needed, iVR-based interventions may become a key factor of the multidimensional treatment of persistent dyspnoea.
Acknowledgements
We thank Fosco Bernasconi (Laboratory of Cognitive Neuroscience, Brain Mind Institute and Center for Neuroprosthetics, Faculty of Life Sciences, EcolePolytechnique Federale de Lausanne, Geneva, Switzerland) for his statistical advice.
Provenance: Submitted article, peer reviewed.
Data sharing: The anonymised patient data will be shared, while safeguarding the privacy of patients, via the LNCO data repository (https://gitlab.epfl.ch/lnco-public).
Ethics committee approval: This single-site study was carried out at the University Hospital in Geneva, Switzerland, and was approved by the Commission Cantonale d'Ethique de la Recherche de la République et Canton de Genève (2019-02360).
Author contributions: Every author named in this article contributed to the study as follows. Conceptualisation: D. Adler, O. Blanke, S. Betka, B. Herbelin, O.A. Kannape and T. Similowski; data curation: S. Betka and J. Fasola; formal analysis: J. Fasole and S. Betka; funding acquisition: D. Adler, O. Blanke and S. Betka; investigation: J. Fasola and A. Schmit; methodology: D. Adler, O. Blanke, S. Betka, J. Fasola, B. Herbelin and O.A. Kannape; project administration: D. Adler, J. Fasola and A. Schmit; resources and software: S. Cardin, B. Herbelin and F. Lance; supervision: D. Adler, O. Blank, S. Betka and O.A. Kannape; visualisation: S. Betka and J. Fasola; writing the original draft: S. Betka and J. Fasola; reviewing and editing the manuscript: D. Adler, O. Blanke, S. Betka, S. Cardin, B. Herbelin, P.M. Soccal, O.A. Kannape and T. Similowski. All authors confirm that they had full access to all the data in the study and accept responsibility to submit for publication. J. Fasola and S. Betka verified the data.
Conflict of interest: S. Cardin and O.A. Kannape were employees of MindMaze SA at the time of the study. No MindMaze SA products were used in this study. T. Similowski reports grants from Lungpacer Inc.; consulting fees from ADEP Assistance, AstraZeneca France, Chiesi France, KPL consulting, Lungpacer Inc., Novartis France, TEVA France and Vitalaire; and support for attending meetings and/or travel from Novartis France, all outside the submitted work. O. Blanke is member of the board and shareholder of MindMaze SA, and is founder and shareholder of Metaphysiks SA. The remaining authors have no conflicts to disclose.
Support statement: The funders of the study had no role in study design, data collection, data analysis, data interpretation or writing of the report. The involvement of MindMaze SA was limited to providing the devices for the study and in-kind contributions for the software development. S. Betka's salary was funded by a Marie Skłodowska-Curie Individual Fellowship (H2020-MSCA-IF-2019 894111/RESPVR), awarded by the European Commission. O. Blanke is funded by the Bertarelli Foundation. Funding information for this article has been deposited with the Crossref Funder Registry.
References
- 1.Parshall MB, Schwartzstein RM, Adams L, et al. An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med 2012; 185: 435–452. doi: 10.1164/rccm.201111-2042ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnson MJ, Yorke J, Hansen-Flaschen J, et al. Towards an expert consensus to delineate a clinical syndrome of chronic breathlessness. Eur Respir J 2017; 49: 1602277. doi: 10.1183/13993003.02277-2016 [DOI] [PubMed] [Google Scholar]
- 3.Morélot-Panzini C, Adler D, Aguilaniu B, et al. Breathlessness despite optimal pathophysiological treatment: on the relevance of being chronic. Eur Respir J 2017; 50: 1701159. doi: 10.1183/13993003.01159-2017 [DOI] [PubMed] [Google Scholar]
- 4.Lawi D, Dupuis-Lozeron E, Berra G, et al. Experimental dyspnoea interferes with locomotion and cognition: a randomised trial. Eur Respir J 2020; 56: 2000054. doi: 10.1183/13993003.00054-2020 [DOI] [PubMed] [Google Scholar]
- 5.Kochovska S, Chang S, Ferreira D, et al. Invisibility of breathlessness in clinical consultations: a cross-sectional, national online survey. Eur Respir J 2022; 60: 2201603. doi: 10.1183/13993003.01603-2022 [DOI] [PubMed] [Google Scholar]
- 6.Gysels M, Higginson IJ. Access to services for patients with chronic obstructive pulmonary disease: the invisibility of breathlessness. J Pain Symptom Manage 2008; 36: 451–460. doi: 10.1016/j.jpainsymman.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 7.von Leupoldt A, Sommer T, Kegat S, et al. Dyspnea and pain share emotion-related brain network. Neuroimage 2009; 48: 200–206. doi: 10.1016/j.neuroimage.2009.06.015 [DOI] [PubMed] [Google Scholar]
- 8.Park HD, Blanke O. Coupling inner and outer body for self-consciousness. Trends Cogn Sci 2019; 23: 377–388. doi: 10.1016/j.tics.2019.02.002 [DOI] [PubMed] [Google Scholar]
- 9.Pozeg P, Palluel E, Ronchi R, et al. Virtual reality improves embodiment and neuropathic pain caused by spinal cord injury. Neurology 2017; 89: 1894–1903. doi: 10.1212/WNL.0000000000004585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rognini G, Blanke O. Cognetics: robotic interfaces for the conscious mind. Trends Cogn Sci 2016; 20: 162–164. doi: 10.1016/j.tics.2015.12.002 [DOI] [PubMed] [Google Scholar]
- 11.Solcà M, Krishna V, Young N, et al. Enhancing analgesic spinal cord stimulation for chronic pain with personalized immersive virtual reality. Pain 2020; 162: 1641–1649. doi: 10.1097/j.pain.0000000000002160 [DOI] [PubMed] [Google Scholar]
- 12.Adler D, Herbelin B, Similowski T, et al. Breathing and sense of self: visuo-respiratory conflicts alter body self-consciousness. Respir Physiol Neurobiol 2014; 203: 68–74. doi: 10.1016/j.resp.2014.08.003 [DOI] [PubMed] [Google Scholar]
- 13.Allard E, Canzoneri E, Adler D, et al. Interferences between breathing, experimental dyspnoea and bodily self-consciousness. Sci Rep 2017; 7: 9990. doi: 10.1038/s41598-017-11045-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Betka S, Adler D, Similowski T, et al. Breathing control, brain, and bodily self-consciousness: toward immersive digiceuticals to alleviate respiratory suffering. Biol Psychol 2022; 171: 108329. doi: 10.1016/j.biopsycho.2022.108329 [DOI] [PubMed] [Google Scholar]
- 15.Betka S, Canzoneri E, Adler D, et al. Mechanisms of the breathing contribution to bodily self-consciousness in healthy humans: lessons from machine-assisted breathing? Psychophysiology 2020; 57: e13564. doi: 10.1111/psyp.13564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lerum TV, Aaløkken TM, Brønstad E, et al. Dyspnoea, lung function and CT findings three months after hospital admission for COVID-19. Eur Respir J 2020; 57: 2003448. doi: 10.1183/13993003.03448-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Michelen M, Cheng V, Manoharan L, et al. Characterising long term COVID-19: a living systematic review. BMJ Glob Health 2021; 6: e005427. doi: 10.1136/bmjgh-2021-005427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spruit MA, Holland AE, Singh SJ, et al. COVID-19: interim guidance on rehabilitation in the hospital and post-hospital phase from a European Respiratory Society and American Thoracic Society-coordinated international task force. Eur Respir J 2020; 56: 2002197. doi: 10.1183/13993003.02197-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Demediuk BH, Manning H, Lilly J, et al. Dissociation between dyspnea and respiratory effort. Am Rev Respir Dis 1992; 146: 1222–1225. doi: 10.1164/ajrccm/146.5_Pt_1.1222 [DOI] [PubMed] [Google Scholar]
- 20.Birckhead B, Khalil C, Liu X, et al. Recommendations for methodology of virtual reality clinical trials in health care by an international working group: iterative study. JMIR Ment Health 2019; 6: e11973. doi: 10.2196/11973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pang PS, Cleland JG, Teerlink JR, et al. A proposal to standardize dyspnoea measurement in clinical trials of acute heart failure syndromes: the need for a uniform approach. Eur Heart J 2008; 29: 816–824. doi: 10.1093/eurheartj/ehn048 [DOI] [PubMed] [Google Scholar]
- 22.Robitzsch A. Why ordinal variables can (almost) always be treated as continuous variables: clarifying assumptions of robust continuous and ordinal factor analysis estimation methods. Front Educ 2020; 5: 589965. doi: 10.3389/feduc.2020.589965 [DOI] [Google Scholar]
- 23.Lansing RW, Gracely RH, Banzett RB. The multiple dimensions of dyspnea: review and hypotheses. Respir Physiol Neurobiol 2009; 167: 53–60. doi: 10.1016/j.resp.2008.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Trost Z, France C, Anam M, et al. Virtual reality approaches to pain: toward a state of the science. Pain 2021; 162: 325–331. doi: 10.1097/j.pain.0000000000002060 [DOI] [PubMed] [Google Scholar]
- 25.Garcia LM, Birckhead BJ, Krishnamurthy P, et al. An 8-week self-administered at-home behavioral skills-based virtual reality program for chronic low back pain: double-blind, randomized, placebo-controlled trial conducted during COVID-19. J Med Internet Res 2021; 23: e26292. doi: 10.2196/26292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marlow LL, Faull OK, Finnegan SL, et al. Breathlessness and the brain: the role of expectation. Curr Opin Support Palliat Care 2019; 13: 200–210. doi: 10.1097/SPC.0000000000000441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Similowski T. Treat the lungs, fool the brain and appease the mind: towards holistic care of patients who suffer from chronic respiratory diseases. Eur Respir J 2018; 51: 1800316. doi: 10.1183/13993003.00316-2018 [DOI] [PubMed] [Google Scholar]
- 28.Verberkt CA, van den Beuken-van Everdingen MHJ, Schols JMGA, et al. Effect of sustained-release morphine for refractory breathlessness in chronic obstructive pulmonary disease on health status: a randomized clinical trial. JAMA Intern Med 2020; 180: 1306–1314. doi: 10.1001/jamainternmed.2020.3134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Herigstad M, Faull OK, Hayen A, et al. Treating breathlessness via the brain: changes in brain activity over a course of pulmonary rehabilitation. Eur Respir J 2017; 50: 1701029. doi: 10.1183/13993003.01029-2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Venkatesan P. NICE guideline on long COVID. Lancet Respir Med 2021; 9: 129. doi: 10.1016/S2213-2600(21)00031-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Czeisler MÉ. Delay or avoidance of medical care because of COVID-19-related concerns – United States, June 2020. MMWR Morb Mortal Wkly Rep 2020; 69: 1250–1257. doi: 10.15585/mmwr.mm6936a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Similowski T, Serresse L. Lessons from negative dyspnoea studies: arguments for the multidimensional evaluation of multidirectional therapeutic approaches. Eur Respir J 2019; 53: 1802471. doi: 10.1183/13993003.02471-2018 [DOI] [PubMed] [Google Scholar]
- 33.Banzett RB, O’Donnell CR, Guilfoyle TE, et al. Multidimensional Dyspnea Profile: an instrument for clinical and laboratory research. Eur Respir J 2015; 45: 1681–1691. doi: 10.1183/09031936.00038914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Delshad SD, Almario CV, Fuller G, et al. Economic analysis of implementing virtual reality therapy for pain among hospitalized patients. NPJ Digit Med 2018; 1: 22. doi: 10.1038/s41746-018-0026-4 [DOI] [PMC free article] [PubMed] [Google Scholar]