Abstract
Background:
Postpartum depression (PPD) may have adverse outcomes for mothers, their infants, and families. Despite the negative consequences of PPD many women hesitate to seek treatment. The theoretical concepts of this study were based on the health belief model, which focuses on the individual’s attitudes, beliefs, and intentions to seek treatment.
Aim:
The aim of the study was to examine whether health beliefs and social support mediate the links between sociodemographic variables and treatment preferences for PPD.
Method:
Cross-sectional survey, including 1,000 Jewish mothers attending the maternal and child health clinics in Israel for their infant’s medical exam, 4 weeks to 6 months postpartum.
Results:
Mother’s age and years of education correlated positively with preferences to receive treatment in the private sector and from professionals working in mental health clinics. The greater the number of children, the less likely new mothers were to favor these preferences. Structural equation modeling showed several mediating pathways: social support mediated the links between sociodemographic variables to health belief model components such as perceived benefits, barriers, and environmental cues. Health belief model components also mediated the links between sociodemographic factors and preferences for place of treatment, professionals, and modes of treatment for PPD.
Conclusions:
Health belief model components and social support are important mediating components that help explain mothers’ PPD treatment preferences. Health professionals such as psychiatric or public health nurses should increase awareness of women at risk for PPD and elicit their preferred treatment options.
Keywords: health belief model, social support, treatment preferences, postpartum depression
Introduction
The prevalence of postpartum depression (PPD) among the general population of new mothers in Western countries is estimated at 9% to 17% (Shorey et al., 2018; Yelland et al., 2010). Women who suffer from PPD are vulnerable to emotional and physical risks (Wisner et al., 2013) and adverse effects on their infants and families (Dias & Figueiredo, 2020; Field, 2011; Murray et al., 2015).
Early and effective intervention is the recommended course of action for easing new mother’s distress, helping her regain normal functioning in society and adjusting to her role as a new mother (Anokye et al., 2018; Zhou et al., 2020). A previous study identified three types of treatment preferences regarding PPD: place of treatment, type of professionals providing treatment, and mode of treatment, all of which are options that exist in the community and within the health care system (Simhi et al., 2019). In this article, we focus on the mediating role of health beliefs and social support in the relationship between mothers’ sociodemographic variables and treatment preferences for PPD.
Despite the negative consequences of PPD on mothers and infants, and the availability of various treatment options in the community, many women refrain from reporting PPD symptoms and hesitate to seek treatment (Eilat-Tsanani et al., 2006; Patel & Wisner, 2011). Little is known about the variables influencing women’s treatment preferences for PPD (Patel & Wisner, 2011). Previous studies that have examined women’s preferences for treating depression showed differences according to sociodemographic variables (Bina & Harrington, 2016; Dennis & Chung-Lee, 2006). For example, mothers with a high level of education and high income preferred individual psychotherapy rather than group therapy or medication (Goodman, 2009). In contrast, postpartum women with low income and education levels were less likely to seek treatment for their depression, and a third of them preferred to receive only informal support (Wisner et al., 2008). Young mothers found it difficult to decide whether to seek treatment for PPD symptoms (Patel & Wisner, 2011), while older mothers were more likely to seek therapy (MacKenzie et al., 2008).
The theoretical framework of this study is derived from the health belief model (HBM), which focuses on the individual’s attitudes, beliefs, and intentions to perform a behavior, which are in turn influenced by sociodemographic variables and thus influence health-related behaviors and outcomes (Rosenstock et al., 1994). The HBM hypothesizes that intentions to perform health-related behaviors depend on (1) perceived benefits, which reflect a person’s perception of the positive health consequences of performing a specific health behavior; (2) perceived barriers, which highlight a person’s perception of the costs or obstacles that hinder them from performing a given health behavior; and (3) environmental cues, which are external factors in an individual’s environment that encourage the person to take action, such as contact with health providers or exposure to ads associated with this health behavior (Rosenstock et al., 1994). The components of the HBM were shown to be the strongest predictors of preventive health behavior, such as vaccination (Sarid et al., 2019).
Previous studies using the HBM, found that perceived benefits predicted the actual or intended use of health services, such as the Contact Tracing App for Containing COVID-19 (Walrave et al., 2020), influenza vaccine uptake among health care workers (O’Reilly et al., 2005), infant vaccination behavior of mothers (Sarid et al., 2019; Simhi et al., 2014), and engagement in physical activity among cancer survivors (Price et al., 2020).
Barriers that make it difficult to seek treatment for PPD include negative stereotypes in the mother’s community about mental illness (Wisner et al., 2008), lack of time (Goodman, 2009), lack of child care (Goodman, 2009), inability to identify symptoms of depression (Dennis & Chung-Lee, 2006; Goodman, 2009), as well as problematic accessibility, availability, and cost of services (Dennis & Chung-Lee, 2006; Dennis & Dowswell, 2013).
Using the HBM to predict intentions to perform a certain health behavior showed the important role of environmental cues (Bish & Michie, 2010; Rosenstock et al., 1994). Previous studies have shown that environmental cues, such as discussions with health professionals regarding symptoms of PPD, increased intention to receive treatment for PPD symptoms (Dennis & Chung-Lee, 2006; Flynn et al., 2006). Women needed help in choosing the type of treatment they preferred for treating PPD, and most women indicated they would prefer to learn about treatment options from their doctors or nurses (Patel & Wisner, 2011). Several studies suggest that sociodemographic variables may affect health-promoting behaviors through an individual’s health beliefs (O’Reilly et al., 2005). For example, older age (MacKenzie et al., 2008), higher education, and higher socioeconomic status (SES; Hjelm et al., 2005; Leganger & Kraft, 2003) were correlated with fewer barriers and perceiving the treatment as more beneficial.
Another mediator between sociodemographic variables and health outcomes is social support from family, friends, and health professionals. Informal support mediated the links between SES and mental health, while formal social participation such as volunteering and political involvement mediated the links between SES and health among midlife and older adults (Achdut & Sarid, 2020). Informal support factors such as friends and family influenced the extent to which postpartum women sought professional mental health care (Schooley et al., 2009) or support from nurses and physicians (Flynn et al., 2006). Moreover, lack of social support may be a barrier to seeking treatment for PPD symptoms (Dennis & Chung-Lee, 2006).
As far as we know, no study to date has examined the role of health beliefs and social support as mediators in the connection between sociodemographic variables and treatment preferences for PPD. Therefore, the objectives of the present study are to examine (1) the associations linking sociodemographic variables, health beliefs, and social support with the treatment preferences of new mothers and (2) whether health beliefs and social support mediate the links between sociodemographic variables and treatment preferences.
We hypothesized that (1) a positive association would be found between mothers’ preferences to receive treatment in private mental health practices from mental health care professionals and both years of education and SES; (2) a positive association would be found between age, years of education, and SES with health beliefs (perceived benefits, environmental cues) and social support; (3) a negative association would be found linking sociodemographic variables with barriers; (4) treatment preferences would be positively associated with perceived benefit, environmental cues, and social support; and negatively correlated with barriers; and finally, (5) the HBM variables and social support would have a mediating role on the relationship between mothers’ sociodemographic variables and treatment preferences for PPD.
Method
Study Design and Setting
A cross-sectional survey was conducted between December 2014 and August 2015 in eight maternal child health clinics (MCHCs). In Israel, public health nurses complete screenings for PPD in MCHCs during the 28th week of pregnancy and at 4 to 9 weeks postpartum (Ministry of Health, 2014). During the postpartum period, detection and identification of mothers with PPD is usually done when women visit the MCHC for their infant’s first-time vaccinations and medical examination (Glasser et al., 2012).
An earlier published study from this data set focused on sociodemographic variables and treatment preferences of mothers with and without PPD. In addition, exploratory factor analysis was conducted for the three types of treatment preferences and treatment preferences comparing mothers with and without PPD, which are not included in this article.
Sample
The study population included 1,000 Jewish mothers who attended the MCHCs for their infant’s medical exam. Inclusion criteria were Hebrew-speaking who had given birth to a child within the past 4 weeks to 6 months and who lived in central Israel. The study was approved by the Research Ethics Committee of the Ministry of Health in Israel. The sample size was calculated using OpenEpi software for a two-sided significance level of .05 and a statistical power of 80%. http://www.openepi.com/OE2.3/Menu/OpenEpiMenu.htm. OpenEpi indicated that 900 women were required for the study. We increased the sample to 1,000 as we assumed that approximately 10% would not provide complete data.
The average age of the respondents (N = 1,000) was 31.43 years (SD = 4.92). Almost all women were married (95.9%); and more than three quarters were native-born (77.6%). An academic education (bachelor’s degree or higher) was reported by 63.4%. Most women (91.2%) worked outside of their home before birth and 81.2% reported no difficulty paying for their basic needs (81.2%). Secular comprised 46.7% of the sample, 27% were traditional, and the rest were religious, or ultra-Orthodox (26.3%). A diagnosis of PPD in a prior pregnancy was reported by 5.5% of the respondents.
Instruments
PPD symptoms were assessed using the Edinburgh Postnatal Depression Scale (EPDS; Cox & Holden, 2003). The questionnaire included 10 questions, which focus on mothers’ feelings during the perinatal period. The 10th question is about the intention to inflict self-harm. Each question is rated on a 4-point Likert-type scale (0 to 3), and the score is the sum of all the statements (Cox & Holden, 2003). In this study, the cutoff point of 10 was selected, to maintain consistency with previous studies conducted in Israel (Bina & Harrington, 2016; Bloch et al., 2005). The internal reliability was good (Cronbach α = .82).
Independent Variables
The sociodemographic questionnaire included the following variables: age, ethnicity, years of education, SES, degree of religiosity (self-definition, i.e., secular, traditional, religious, ultra-Orthodox), marital status, number of children, and the employment status of the mother and her spouse/partner.
Mediating Variables
Health Beliefs (Rosenstock et al., 1994)
(a) Perceived barriers—11 questions referred to barriers to seeking treatment for PPD (e.g., lack of knowledge, shame, and transportation difficulties). This scale showed adequate internal reliability (Cronbach α = .75). (b) Perceived benefits—One question referred to the mothers’ belief that therapy might help ameliorate symptoms of PPD. (c) Environmental cues—Six questions examined the environmental cues that may encourage or inhibit turning to treatment centers (e.g., spouse, family doctor, gynecologist, MCHC or hospital nurses, friends, close family). In every area, the answers were on a 5-point Likert-type scale: 1 = not at all to 5 = very much (Cronbach α = .80)
Social Support
The questionnaire about social support after the birth included eight items related to the people who are part of the mother’s support system (e.g., mother/father/sister, etc.). The answers were dichotomous (yes/no). Then, we counted the number of people who supported the mother after giving birth. The questions were adapted from the parent and partner support subscales of a questionnaire, which assesses the perceived availability of baby-specific social support from multiple sources (Haslam et al., 2006).
Dependent Variables
Preferences for Getting Mental Health Treatment for PPD
The questionnaire was adapted from a study by Goodman to reflect the treatment options available in Israel (Goodman, 2009; Jimenez et al., 2012). We asked the mothers to deliberate on what their treatment preferences would be for PPD symptoms, considering that most mothers experience some PPD symptoms after birth. Women were asked questions to assess the three variables: (a) Place of treatment—“If you felt depressed after birth, to which treatment center would you prefer to go?” Eight options were presented, including MCHCs, a psychiatric clinic, or a private mental health practice; (b) Type of professionals—“If you felt depressed after childbirth, to what extent you would prefer the treatment of the following professionals?” Twelve options were presented including nurses, psychologist, social workers, or psychiatrists, and (c) Mode of treatment— “There are many ways to get treatment. To what extent do you feel that the following options would be suitable for your needs?” Fifteen options were presented, including home visits, Skype-based treatment, or group meetings.
Exploratory factor analysis for treatment preferences showed three main factors: (1) Place of treatment: community health clinic; psychiatric clinics; and private mental health practices, which was a separate variable. (2) Type of professionals: professionals in the community; mental health professionals; and paraprofessionals in the community. (3) Mode of treatment: personal-based interventions; technology-mediated interventions; and group-based interventions (Simhi et al., 2019).
Procedure
We approached new mothers who came to MCHCs and explained the purpose of the study. If they met the inclusion criteria, they were invited to participate and provided with a questionnaire. Women who filled out the EPDS questionnaire and were identified with clinical symptoms of PPD or answered anything other than “never” on EPDS item 10 (i.e., potential for harm to self) were referred by the research staff to the MCHC nurses for treatment. Out of the 1,107 women who met the inclusion criteria, 1,000 women (90.2%) agreed to participate and completed the questionnaire. Lower response rates (33%-74%) were reported in previous studies among postpartum mothers (Gjerdingen et al., 2009; Olson et al., 2006).
Data Analysis
All mothers with complete data were included in the analysis (N = 1,000). The data were analyzed with SPSS version 21.0 software and the AMOS module for analysis of the structural equations (IBM Corp), using a significance level of <.01, which is the convention for the Bonferroni correction for multiple comparisons.
In order to examine the first to fourth hypotheses, we used Pearson correlations, student t tests, and one-way analysis of variance tests for sociodemographic variables, health beliefs, social support, and treatment preferences. For the fifth hypothesis, we constructed three structural equation models (SEMs) for (1) preferred place of treatment, (2) care professional preferences, and (3) preferences regarding how to receive the therapy. In these models, the health beliefs and social support variables were introduced as mediators between the sociodemographic variables and the treatment preference variables. The quality of the SEM was rated by the chi-square statistic (χ2). If the χ2 value is not significant, it indicates a good fit of the model (Byrne, 2000). Additional adjustment indices are the NFI (normed fit index) and the CFI (comparative fit index). A value greater than .9 is considered a good fit (Hu & Bentler, 1999). Another index is the RMSEA (root mean square error of approximation). The value should be less than .05 to indicate a good fit (Chen et al., 2008)
Results
In this sample, 8.4% of the respondents scored 10 or higher on the EPDS. In response to question 10, a total of 10 respondents (1%) stated that they had considered hurting themselves.
Sociodemographics and Treatment Preferences
In Table 1, we present the relationships between sociodemographic variables and treatment preferences. All respondents were included in the analysis.
Table 1.
Pearson Correlations Between Sociodemographic Variables and Treatment Preferences (N = 1,000).
| Treatment preference | Education | Mother’s age | No. of children |
|---|---|---|---|
| Treatment centers | |||
| Community treatment centers | −.07 | .04 | .00 |
| Psychiatric clinics | .06 | .06 | −.06 |
| Private mental health practices | .26*** | .15*** | −.11*** |
| Type of professional | |||
| Professionals in the community | −.03 | .02 | .00 |
| Mental health professionals | .24*** | .20*** | −.11*** |
| Paraprofessionals in the community | .00 | .00 | .00 |
| Mode of treatment | |||
| Individual interventions | .21*** | .15*** | −.08** |
| Group-based interventions | .03 | .05 | −.02 |
| Technology-mediated interventions | −.05 | .12*** | .03 |
p < .05. **p < .01. ***p < .001.
Age and years of education correlated positively with preferences to receive treatment for PPD in the private sector, from professionals working in mental health clinics such as psychologist or psychiatrist. The greater the number of children, the less likely they were to favor receiving treatment in the private sector.
Differences according to immigrant status, SES, and degree of religiosity were also examined (not shown in the table). Compared with immigrants, Israeli-born women preferred treatment at private mental health practices, from mental health professionals, and personal-based interventions: t(998) = −2.65, p < .01; t(998) = −2.61, p < .01; and, t(998) = −3.13, p < .001, respectively. Compared with ultra-Orthodox women, secular women preferred private mental health practices, and personal interventions: F (3, 996) =15.41, p < .001 and F(3, 996) = 6.15, p < .001, respectively. Mothers with low SES were less likely to prefer private mental health practices, F(2, 997) = 11.42, p < .001; additionally, mothers who did not report economic difficulties preferred personal-based interventions, F(2, 997) = 7.76, p < .001.
Sociodemographics, Social Support, and Health Beliefs
In the second stage of analysis, we present the relationships between the sociodemographic variables and the mediating variables: social support and health beliefs (not shown in table) using Pearson, t, and one-way analysis of variance tests. Our findings showed that higher level of education was positively related to social support she had received (r = .10, p < .001), and to greater exposure to environmental cues (r = .16, p < .001). Compared with immigrants, Israeli-born women received more social support, t(998) = −3.52, p < .001, and were exposed to more environmental cues, t(998) = 3.20, p < .001. Compared with traditional and secular, ultra-Orthodox women were exposed to fewer environmental cues, F(4, 995) = 7.08, p < .01, and had greater number of barriers, F(4, 995) = 6.86, p < .001.
Social support, F(2, 997) = 12.24, p < .001; barriers, F(3, 997) = 25.54, p < .001; and perceived benefits, F (3, 997) = 25.54, p < .001, differed by SES level as well. Scheffe tests showed that women with higher SES, compared with lower-SES, received more social support, were exposed to more environmental cues, perceived fewer barriers, and regarded more perceived benefits in receiving treatment for PPD.
Social Support, Health Beliefs, and Treatment Preferences
In Table 2, we present the relationships linking social support and health beliefs variables with treatment preferences.
Table 2.
The Relationships Among Health Beliefs, Social Support, and Treatment Preferences (Pearson Correlation Coefficients; N = 1,000).
| Treatment preference | Barriers | Environmental cues | Perceived benefits | Social support |
|---|---|---|---|---|
| Treatment centers | ||||
| Community treatment centers | .06 | .27*** | .04 | −.02 |
| Psychiatric clinics | .05 | .19*** | .01 | .01 |
| Private mental health practices | −.09** | .14** | .11*** | .07 |
| Type of professional | ||||
| Mental health professionals | .02 | .34*** | .10** | .05 |
| Professionals in the community | −.11*** | .33*** | .19*** | .08** |
| Paraprofessionals in the community | .11*** | .22*** | .05 | .05 |
| Mode of treatment | ||||
| Individual interventions | −.02 | .36*** | .15*** | .08** |
| Group-based interventions | .09** | .21*** | .07** | .07 |
| Technology-mediated interventions | .08** | .23*** | .10*** | .05 |
p < .05. **p < .01. ***p < .001.
Social support was positively associated with preference to receive treatment for PPD at private mental health practices, from professionals in the community, and via personal-based and group-based interventions. Barriers to seeking treatment were positively associated with intent to turn to community health clinics, paraprofessionals in the community, group-based interventions, and technology-mediated interventions; and were negatively correlated with the intent to seek treatment in private mental health practices and from professionals in the community. Environmental cues were positively associated with all treatment preferences. Furthermore, if a mother perceived the treatment for PPD as more beneficial, she was more likely to prefer using private mental health practices, mental health professionals (psychologist or psychiatrist), professionals in the community (family physician or nurses) and treatment via personal-based interventions, group-based interventions, and technology-mediated interventions compared with community health clinics, psychiatric clinics, and paraprofessionals in the community.
Mediation Models
We constructed three models and examined whether HBM components and social support mediated the link between women’s sociodemographic variables and treatment preferences. The variables that were significant in the bivariate analysis—degree of religiosity, education, age, SES, number of children, and immigrant status—were introduced into the SEM analysis.
All models showed a high NFI and CFI with no significant χ2. In Table 3, we present the models’ goodness-of-fit indices.
Table 3.
The Models’ Goodness of Fit.
| Model | χ2 (df) | RMSEA | NFI | CFI | SRMR |
|---|---|---|---|---|---|
| Model 1 | 19.56 (14)* | .02 | .98 | .99 | .02 |
| Model 2 | 25.12 (20)* | .01 | .97 | .99 | .02 |
| Model 3 | 29.84 (21)* | .02 | .97 | .99 | .02 |
Note. RMSEA = root mean square error of approximation; NFI = normed fit index; CFI = comparative fit index; SRMR = standardized root mean square residual.
p < .05.
Health Beliefs and Social Support as a Mediator Between Sociodemographic Variables and Preferred Treatment Centers
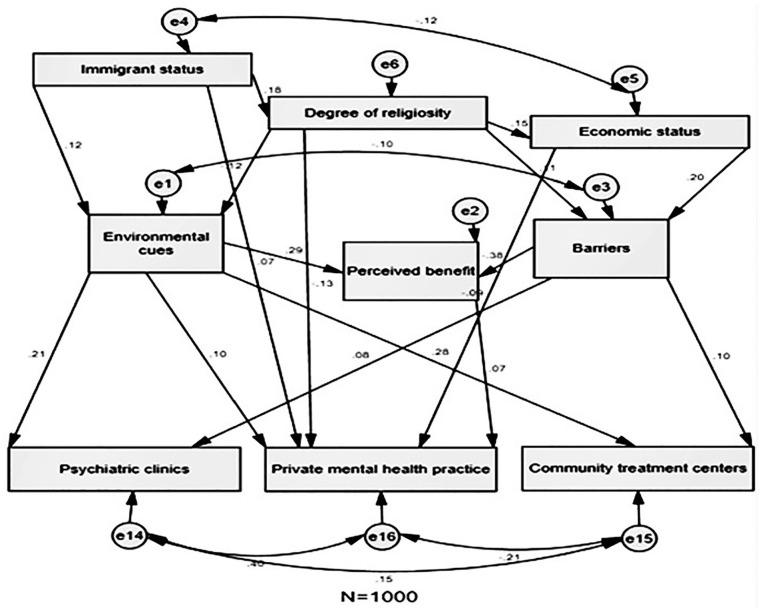
In Figure 1, we present the SEM analysis on the surveyed mothers’ preferred treatment centers (community health clinic, psychiatric clinics, and private mental health practices). The model’s beta values are significant (p <. 01).
Figure 1.
Model 1. Structural equation analysis: Preferred location of treatment.
Being of low SES, more religious, or an immigrant, were related to preferring treatment from a private mental health practice. Immigrant women, religious women, and women with financial difficulties were less likely to prefer private mental health practices.
Perceived benefits, barriers, and environmental cues mediated the links between these sociodemographic factors and preferred places of treatment. Environmental cues had a mediating effect on the relationship between both immigrant status and degree of religiosity and the three preferred places of treatment. Barriers also had a mediating effect on the relationship between both degree of religiosity and SES and preferences for community health and psychiatric clinics. Perceived benefits were found to have a mediating effect on the relationship between preference to seek treatment in private mental health practices, and both environmental cues and barriers. Social support did not mediate the links between sociodemographic factors and treatment preferences.
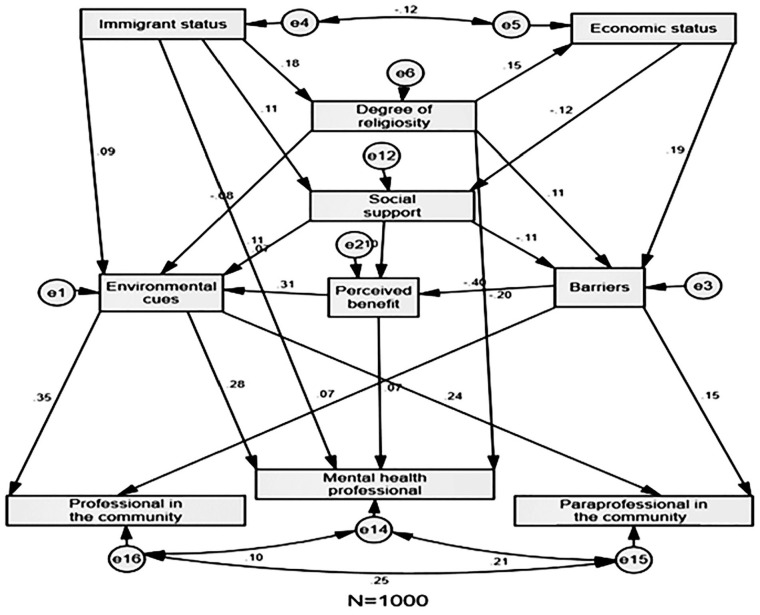
Health Beliefs and Social Support as a Mediator Between Sociodemographic Variables and Preferred Type of Professional
In Figure 2, we present the SEM analysis for the surveyed mothers’ preferred types of professionals (professionals in the community, mental health professionals, and paraprofessionals in the community). The model’s beta values are significant (p < .01).
Figure 2.
Model 2. Structural equation analysis: Preferred type of professional.
Degree of religiosity and being an immigrant were related to preferences for treatment from mental health professionals. Israeli-born were more likely to prefer mental health professionals compared with immigrants. Religious mothers were less likely to prefer mental health professionals than secular.
Social support mediated the links between sociodemographic variables and HBM components. Perceived benefits, barriers, and environmental cues mediated the links between social support and type of preferred health care professionals.
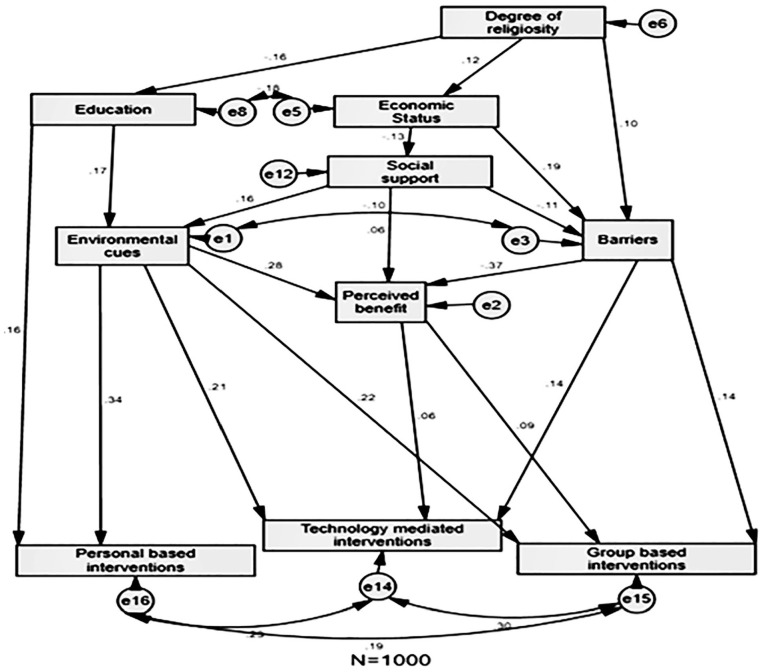
Health Beliefs and Social Support as a Mediator Between Sociodemographic Variables and Preferred Mode of Treatment
In Figure 3, we present the SEM analysis for the mothers’ preferred mode of treatment (personal-based interventions, technology-mediated interventions, and group-based interventions). The model’s beta values are significant (p < .01).
Figure 3.
Model 3. Structural equation analysis: Preferred mode of treatment.
Years of education was related to a preference for individual rather than group interventions. Mothers with more years of education were more likely to prefer individual interventions than those with fewer years of education.
Environmental cues and barriers mediated the links between sociodemographic factors and preferred modes of treatment. Environmental cues had a mediating effect on the relationship between years of education and the three preferred treatment modes. Barriers were found to have a mediating effect on the relationship between degree of religiosity and SES and both preferences for group-based and technology-mediated interventions. Perceived benefits had a mediating effect on the relationship between preferences for group-based and technology-mediated interventions, and both barriers and environmental cues. Social support mediated the relationship between preferred mode of treatment for PPD, and both sociodemographic variables and health belief components.
Discussion
The prevalence of PPD symptoms was low (8.4%) but consistent with a previous study conducted among Jewish mothers in Israel (Eilat-Tsanani et al., 2006).
Sociodemographic Variables and Treatment Preferences
Our findings show a direct relationship between sociodemographic variables and treatment preferences. Immigrant and religious mothers were less likely to prefer receiving treatment at private mental health practices from mental health professionals. The explanation for these treatment preferences may stem from differences in SES. Indeed, we found that women with a high SES preferred private mental health practices. The findings are consistent with previous studies showing a positive correlation between high SES and the preference for individual psychotherapy among women with PPD (Goodman, 2009; Scholle & Kelleher, 2003). Moreover, years of education was directly related to a preference for personal-based interventions. Mothers with more years of education were more likely to prefer personal-based interventions than those with fewer years of education. These findings are consistent with a previous study conducted among postmenopausal women, which showed that the more educated the women were, the more they preferred to receive individual psychotherapy (Goodman, 2009). On the practical level, it is important to convey to medical professionals such as public health nurses the importance of early detection of high-risk groups and provide accessible and culturally sensitive mental health services to make it easier for them to seek therapy.
Sociodemographic Variables, Social Support, and Health Beliefs
Our findings showed that social support was associated with more years of education and a high SES. These findings are consistent with a previous study that examined medical help seeking in general and which indicated positive associations linking years of education, SES, and social support (Song & Chang, 2012). We also found that mothers with a high SES reported fewer barriers and more perceived benefits to receiving treatment compared with mothers with a low SES. The literature on this issue is ambiguous. Findings from a study conducted in Sweden showed a negative relationship between income and beliefs in favor of seeking medical examinations (Hjelm et al., 2005). In contrast, findings from an Israeli study regarding administration of vaccines to infants did not find a link between economic status and health beliefs in favor of receiving vaccines (Simhi et al., 2014).
Health belief differences were related to degree of religiosity: ultra-Orthodox women reported fewer environmental cues and a greater number of barriers compared with secular or traditional women. To the best of our knowledge, no previous studies have examined differences in health beliefs regarding treatment for PPD in the contexts of religiosity and SES in Israel. This is another contribution of the present study. Further research should be conducted to expand on this issue.
Environmental cues were positively associated with years of education, which may be a function to greater exposure to media and internet among those with more years of education. These findings are supported by a study conducted in the United States among women with PPD (Flynn et al., 2006). However, no correlation was found between years of education and barriers, despite previous studies indicating a negative association between years of education and barriers (Hjelm et al., 2005; Leganger & Kraft, 2003). Israeli-born women reported more environmental cues and received more social support compared with immigrants, which, to the best of our knowledge, had never been studied before in Israel. Our findings show efforts should be made to provide support, reduce barriers, and increase environmental cues among high-risk groups such as women with a low SES and low-education levels, ultra-orthodox women, and immigrant women. These findings are especially relevant to psychiatric nurses who have an important role in providing care to postpartum mothers and their infants who are affected by PPD.
Social Support, Health Beliefs, and Treatment Preferences
The findings of our study showed that social support was positively associated with preferences to seek treatment for PPD in private mental health practices, from professionals in the community, and using personal-based, and group-based interventions. These findings are consistent with previous studies showing that social support influenced women’s intent to seek professional help for PPD (Flynn et al., 2006; Schooley et al., 2009).
It was also found that barriers to seeking treatment were associated with preferring community health clinics, paraprofessionals in the community, group interventions, and technology-mediated interventions. A possible explanation is that women who must overcome more barriers, preferred to access treatment outside the mental health care system, compared with women with fewer barriers. This may be due to concern about the labeling of mental illness, in general, and the labeling of PPD, in particular. Previous research findings have indicated a negative association between barriers and behavioral intent to address PPD due to concerns about labeling (Dennis & Chung-Lee, 2006; McCarthy & McMahon, 2008; Wisner et al., 2008). These findings suggest it is important to challenge the stigma associated with PPD and, as a result, to decrease barriers to treatment.
Respondents who thought it beneficial to address PPD, preferred a wider range of community and mental health centers. Theoretically, this finding indicates the importance of the perceived benefits component as increasing behavioral intentions. Furthermore, a correlation was found between environmental cues and preferences regarding the three treatment modes. When the mother had more knowledge about PPD—for example, through nurses, caregivers, family, and media—she was positive about most of the treatment alternatives. These findings are in line with the findings of previous studies, which showed that talking to a professional such as a nurse or physician, getting support from informal sources such as a spouse/partner or friends, and being exposed to information from the internet increased women’s willingness to seek treatment for PPD (Flynn et al., 2006; Patel & Wisner, 2011). On a practical level, this finding demonstrates the importance of minimizing barriers, enhancing the perception of the benefit of treatment, and increasing external cues in order to make it easier to choose preferred therapy venue and style. Thus, nurses working in the field have an important role of reducing the mitigating variables as a way to enhance the intention to seek treatment for PPD.
Mediation Models
The mediation models proposed in this study showed that health beliefs and social support mediate the relationships between sociodemographic variables and treatment preferences. Our findings reinforce the theoretical conceptualization that health beliefs are shaped by sociodemographic variables, and they mediate the relationships between sociodemographic variables and treatment preferences for PPD. For example, in the mediation model environmental cues mediated the relationships linking immigrant status and degree of religiosity with preferences for treatment centers (community health clinics, psychiatric clinics, and private mental health practices). Environmental cues also mediated the relationships linking immigrant status and degree of religiosity with preferences regarding types of professionals (professionals in the community; mental health professionals; and paraprofessionals in the community). In other words, environmental cues increased the intention to seek help among a wider range of treatment centers and professionals. These findings are consistent with previous studies (Flynn et al., 2006; Patel & Wisner, 2011). Furthermore, our findings emphasize the importance of referrals for mental health care by community medical staff and psychiatric nurses during the postpartum period.
Barriers—another component of the HBM—had mediating effects on the relationship between degree of religiosity and SES and preferences to treat PPD via group and technology-mediated interventions. Social support and barriers had mediating effects on the relationship between socioeconomic difficulties and preferences to seek treatment for PPD with professionals and paraprofessionals in the community. These barriers point to risk groups that require more active intervention. The findings of previous studies have shown that lack of social support and barriers—such as fear of being labeled, feelings of shame, lack of knowledge, and financial difficulties—have prevented women from seeking help (Dennis & Chung-Lee, 2006; Dennis & Dowswell, 2013; Goodman, 2009).
Adding the perceived social support component into the HBM conceptualization is a novel contribution of our study. In other words, it is not only the woman’s attitudes that led to the intention to seek treatment but also the perceived social support from external sources increase motivation for a specific health behavior. Future studies should examine the balance between the external and internal aspects in other fields regarding women’ health as a way to enhance nurses’ influence in the clinical field.
One way to explain our results is to focus on pathways through which social determinants shape health. The social determinants of health refer broadly to any nonmedical factors influencing health, including health-related knowledge, attitudes, beliefs (Braveman et al., 2011; Braveman & Gottlieb, 2014). These factors, however, represent only the most downstream determinants in the causal pathways influencing health and are shaped by more upstream determinants, such as SES, education, the political, and cultural conditions that shape access to health-promoting living and working conditions as the fundamental causes of health outcomes (Braveman et al., 2011). Furthermore, our findings corroborate the importance of the mitigating components of the HBM, indicating that internal perceptions are important in predicting one’s intention to behave. Shaping favorable perceptions (e.g., perceptions of treatment as more beneficial and less fear of being labeled) of women at risk for PPD through nurses’ educational interventions and focused medical care can be an important venue for accessing treatment.
The primary limitation of this study is that it was cross-sectional and did not include an actual follow-up to determine health-seeking behaviors. Furthermore, the lack of Arabic-speaking women in the sample limits the generalizability of the findings. Future research should address those issues and include the attitudes and behavioral intentions of other sectors of Israeli society. Another methodological limitation is that this study did not assess for posttraumatic stress disorder (PTSD). Given the strong comorbidity of PPD and PTSD and that one of PTSD’s symptoms is avoidance, which may have a potential impact on treatment seeking (Oh et al., 2016), future studies would benefit from assessing PTSD symptoms as well.
Conclusions
Our study describes postpartum mothers’ treatment preferences for PPD in three areas: treatment centers, professionals, and treatment. Our findings show the important role of the mediation variables (components of the health belief model, such as barriers, environmental cues, and perceived benefits) on treatment preferences. On a practical level, this finding demonstrates the importance of minimizing barriers such as shame and lack of knowledge and increasing environmental cues such as encouragement to seek treatment from the spouse, family doctor, nurses, friends, and close family in order to promote treatment for PPD. Fewer years of education, young age, having many children, being an immigrant, and having low SES, were shown to influence the type of therapy preferred. It is also important to raise awareness among the mother’s support circles regarding the provision of informal support and encouragement to receive treatment. A prospective study in which mothers are asked about their treatment preferences at different time points may yield findings that reflect possible changes in behavioral intent. Finally, follow-up studies should focus specifically on mothers in relation to the variables of low SES, immigrant status, and low levels of social support.
Implications for Practice and/or Policy
This study can make a significant contribution to women’s health care and policy on several levels. First, the findings augment the theoretical concept that mothers’ health beliefs can be predictors of their treatment preferences. Second, the study findings contribute to developing a new source of information about the correlations between social-demographic variables and mother’s health beliefs on seeking treatment for PPD, as well as the relationships between health beliefs and preferences for seeking therapy.
In Israel, public health nurses conduct perinatal follow-up care, screen for PPD and provide nondirective supportive counseling and referral to mental health professionals, as necessary. MCHCs nurses have an important role in providing supportive interventions for new mothers at risk of PPD. However, they are not mental health practitioners. Thus, our findings highlight the need for further education and training in mental health practice for public health nurses in Israel, so that they can provide treatment or referrals.
Footnotes
Authors’ Note: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (The Ministry of Health, 13/46) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors. The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors’ Roles: All authors contributed to the conception or design of the study or to the acquisition, analysis, or interpretation of the data. All authors drafted the manuscript, or critically revised the manuscript, and gave final approval of the version that was submitted for publication. All authors agree to be accountable for all aspects of the work, ensuring integrity and accuracy.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by Grant 46/2013/R from the Israel National Institute for Health Services Research.
ORCID iD: Meital Simhi  https://orcid.org/0000-0002-9923-2295
https://orcid.org/0000-0002-9923-2295
References
- Achdut N., Sarid O. (2020). Socio-economic status, self-rated health and mental health: The mediation effect of social participation on early-late midlife and older adults. Israel Journal of Health Policy Research, 9(1), 4. 10.1186/s13584-019-0359-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anokye R., Acheampong E., Budu-Ainooson A., Obeng E. I., Akwasi A. G. (2018). Prevalence of postpartum depression and interventions utilized for its management. Annals of General Psychiatry, 17(1), 18. 10.1186/s12991-018-0188-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bina R., Harrington D. (2016). The Edinburgh Postnatal Depression Scale: Screening tool for postpartum anxiety as well? Findings from a confirmatory factor analysis of the Hebrew version. Maternal and Child Health Journal, 20(4), 904-914. 10.1007/s10995-015-1879-7 [DOI] [PubMed] [Google Scholar]
- Bish A., Michie S. (2010). Demographic and attitudinal determinants of protective behaviours during a pandemic: A review. British Journal of Health Psychology, 15(4), 797-824. 10.1348/135910710X485826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloch M., Rotenberg N., Koren D., Klein E. (2005). Risk factors associated with the development of postpartum mood disorders. Journal of Affective Disorders, 88(1), 9-18. 10.1016/j.jad.2005.04.007 [DOI] [PubMed] [Google Scholar]
- Braveman P., Egerter S., Williams D. R. (2011). The social determinants of health: Coming of age. Annual Review of Public Health, 32(1), 381-398. 10.1146/annurev-publhealth-031210-101218 [DOI] [PubMed] [Google Scholar]
- Braveman P., Gottlieb L. (2014). The social determinants of health: It’s time to consider the causes of the causes. Public Health Reports, 129(1), 18-31. 10.1177/00333549141291s206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne B. M. (2000). Application 7: Testing for invariant latent mean structures. In Structural equation modeling with AMOS: Basic concepts, applications, and programming (pp. 226-246). Lawrence Erlbaum. [Google Scholar]
- Chen F., Curran P. J., Bollen K. A., Kirby J., Paxton P. (2008). An empirical evaluation of the use of fixed cutoff points in RMSEA test statistic in structural equation models. Sociological Methods & Research, 36(4), 462-494. 10.1177/0049124108314720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox J., Holden J. (2003). Perinatal mental health: A guide to the Edinburgh Postnatal Depression Scale (EPDS). Royal College of Psychiatrists. [Google Scholar]
- Dennis C. L., Chung-Lee L. (2006). Postpartum depression help-seeking barriers and maternal treatment preferences: A qualitative systematic review. Birth, 33(4), 323-331. 10.1111/j.1523-536X.2006.00130.x [DOI] [PubMed] [Google Scholar]
- Dennis C. L., Dowswell T. (2013). Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database of Systematic Reviews, 2, Article CD001134. 10.1002/14651858.CD001134.pub3 [DOI] [PubMed] [Google Scholar]
- Dias C. C., Figueiredo B. (2020). Mother’s prenatal and postpartum depression symptoms and infant’s sleep problems at 6 months. Infant Mental Health Journal, 41(5), 614-627. 10.1002/imhj.21869 [DOI] [PubMed] [Google Scholar]
- Eilat-Tsanani S., Meron A., Romano S., Reshef A., Lavi I., Tabenkin H. (2006). The effect of postpartum depression on women’s consultations with physicians. Israel Medical Association Journal, 8(6), 406-410. [PubMed] [Google Scholar]
- Field T. (2011). Prenatal depression effects on early development: A review. Infant Behavior and Development, 34(1), 1-14. 10.1016/j.infbeh.2010.09.008 [DOI] [PubMed] [Google Scholar]
- Flynn H. A., O’Mahen H. A., Massey L., Marcus S. (2006). The impact of a brief obstetrics clinic-based intervention on treatment use for perinatal depression. Journal of Women’s Health, 15(10), 1195-1204. 10.1089/jwh.2006.15.1195 [DOI] [PubMed] [Google Scholar]
- Gjerdingen D., Crow S., McGovern P., Miner M., Center B. (2009). Postpartum depression screening at well-child visits: Validity of a 2-question screen and the PHQ-9. Annals of Family Medicine, 7(1), 63-70. 10.1370/afm.933.Department [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasser S., Tanous M., Shihab S., Goldman N., Ziv A., Kaplan G. (2012). Perinatal depressive symptoms among Arab women in Northern Israel. Maternal and Child Health Journal, 16(6), 1197-1205. 10.1007/s10995-011-0845-2 [DOI] [PubMed] [Google Scholar]
- Goodman J. H. (2009). Women’s attitudes, preferences, and perceived barriers to treatment for perinatal depression. Birth, 36(1), 60-69. 10.1111/j.1523-536X.2008.00296.x [DOI] [PubMed] [Google Scholar]
- Haslam D. M., Pakenham K. I., Smith A. (2006). Social support and postpartum depressive symptomatology: The mediating role of maternal self-efficacy. Infant Mental Health Journal, 27(3), 276-291. 10.1002/imhj.20092 [DOI] [PubMed] [Google Scholar]
- Hjelm K. G., Bard K., Nyberg P., Apelqvist J. (2005). Beliefs about health and diabetes in men of different ethnic origin. Journal of Advanced Nursing, 50(1), 47-59. 10.1111/j.1365-2648.2004.03348.x [DOI] [PubMed] [Google Scholar]
- Hu L. T., Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1-55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Jimenez D. E., Bartels S. J., Cardenas V., Dhaliwal S. S., Alegría M. (2012). Cultural beliefs and mental health treatment preferences of ethnically diverse older adult consumers in primary care. American Journal of Geriatric Psychiatry, 20(6), 533-542. 10.1097/JGP.0b013e318227f876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leganger A., Kraft P. (2003). Control constructs: Do they mediate the relation between educational attainment and health behaviour? Journal of Health Psychology, 8(3), 361-372. 10.1177/13591053030083006 [DOI] [PubMed] [Google Scholar]
- MacKenzie C. S., Scott T., Mather A., Sareen J. (2008). Older adults help-seeking attitudes and treatment beliefs concerning mental health problems. American Journal of Geriatric Psychiatry, 16(12), 1010-1019. 10.1097/JGP.0b013e31818cd3be [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy M., McMahon C. (2008). Acceptance and experience of treatment for postnatal depression in a community mental health setting. Health Care for Women International, 29(6), 618-637. 10.1080/07399330802089172 [DOI] [PubMed] [Google Scholar]
- Ministry of Health (2014). Procedure for Locating Women at Risk for Depression in Pregnancy and Postpartum. Public Health Services, No. 20/12. [Google Scholar]
- Murray L., Fearon P., Cooper P. (2015). Postnatal depression, mother-infant interactions, and child development. In Milgrom J., Gemmill A. W. (Eds.), Identifying perinatal depression and anxiety: Evidence-based practice in screening, psychosocial assessment, and management (pp. 139-164). Wiley. 10.1002/9781118509722.ch9 [DOI] [Google Scholar]
- Oh W., Muzik M., McGinnis E. W., Hamilton L., Menke R. A., Rosenblum K. L. (2016). Comorbid trajectories of postpartum depression and PTSD among mothers with childhood trauma history: Course, predictors, processes and child adjustment. Journal of Affective Disorders, 200, 133-141. 10.1016/j.jad.2016.04.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Reilly F. W., Cran G. W., Stevens A. B. (2005). Factors affecting influenza vaccine uptake among health care workers. Occupational Medicine, 55(6), 474-479. 10.1093/occmed/kqi099 [DOI] [PubMed] [Google Scholar]
- Olson A. L., Dietrich A. J., Prazar G., Hurley J. (2006). Brief maternal depression screening at well-child visits. Pediatrics, 118(1), 207-216. 10.1542/peds.2005-2346 [DOI] [PubMed] [Google Scholar]
- Patel S. R., Wisner K. L. (2011). Decision making for depression treatment during pregnancy and the postpartum period. Depression and Anxiety, 28(7), 589-595. 10.1002/da.20844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price J., Barrett-Bernstein M., Wurz A., Karvinen K. H., Brunet J. (2020). Health beliefs and engagement in moderate-to-vigorous-intensity physical activity among cancer survivors: A cross-sectional study. Supportive Care in Cancer, 29(1), 477-484. 10.1007/s00520-020-05515-9 [DOI] [PubMed] [Google Scholar]
- Rosenstock I. M., Strecher V. J., Becker M. H. (1994). The health belief model and HIV risk behavior change. In DiClemente R. J., Peterson J. L. (Eds.), Preventing AIDS: Theories and methods of behavioral interventions (pp. 5-24). Springer. 10.1007/978-1-4899-1193-3_2 [DOI] [Google Scholar]
- Sarid O., Shraga Y., Cwikel J., Reuveni H. (2019). Ethno-cultural origins, health beliefs and mothers’ behavior regarding infant vaccinations in Israel. Health Promotion International, 34(3), 581-590. 10.1093/heapro/day006 [DOI] [PubMed] [Google Scholar]
- Scholle S.H., Kelleher K. (2003). Preferences for depression advice among low-income women. Matern Child Health Journal, 7, 95–102. [DOI] [PubMed] [Google Scholar]
- Schooley J., Mundt C., Wagner P., Fullerton J., O’Donnell M. (2009). Factors influencing health care-seeking behaviours among Mayan women in Guatemala. Midwifery, 25(4), 411-421. 10.1016/j.midw.2007.07.011 [DOI] [PubMed] [Google Scholar]
- Shorey S., Chee C. Y. I., Ng E. D., Chan Y. H., Tam W. W. S., Chong Y. S. (2018). Prevalence and incidence of postpartum depression among healthy mothers: A systematic review and meta-analysis. Journal of Psychiatric Research, 104, 235-248. 10.1016/j.jpsychires.2018.08.001 [DOI] [PubMed] [Google Scholar]
- Simhi M., Sarid O., Cwikel J. (2019). Preferences for mental health treatment for post-partum depression among new mothers. Israel Journal of Health Policy Research, 8(1), Article 84. 10.1186/s13584-019-0354-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simhi M., Shraga Y., Sarid O. (2014). Vaccination of infants and health beliefs of ultra-orthodox mothers. Journal of Vaccines & Vaccination, 5(213), 2-8. 10.4172/2157-7560.1000213 [DOI] [Google Scholar]
- Song L., Chang T. Y. (2012). Do resources of network members help in help seeking? Social capital and health information search. Social Networks, 34(4), 658-669. 10.1016/j.socnet.2012.08.002 [DOI] [Google Scholar]
- Walrave M., Waeterloos C., Ponnet K. (2020). Tracing the COVID-19 Virus: A health belief model approach to the adoption of a contact tracing app. JMIR Public Health and Surveillance, 6(3), Article e20572. 10.2196/20572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisner K. L., Scholle S. H., Stein B. (2008). Perinatal disorders: Advancing public health opportunities. Journal of Clinical Psychiatry, 69(10), 1602-1605. 10.4088/JCP.v69n1010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisner K. L., Sit D. K. Y., McShea M. C., Rizzo D. M., Zoretich R. A., Hughes C. L., Eng H. F., Luther J. F., Wisniewski S. R., Costantino M. L., Confer A. L., Moses-Kolko E. L., Famy C. S., Hanusa B. H. (2013). Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry, 70(5), 490-498. 10.1001/jamapsychiatry.2013.87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yelland J., Sutherland G., Brown S. J. (2010). Postpartum anxiety, depression and social health: Findings from a population-based survey of Australian women. BMC Public Health, 70(5), 490-498. 10.1186/1471-2458-10-771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou C., Hu H., Wang C., Zhu Z., Feng G., Xue J., Yang Z. (2020). The effectiveness of mHealth interventions on postpartum depression: A systematic review and meta-analysis. Journal of Telemedicine and Telecare. Advance online publication. 10.1177/1357633X20917816 [DOI] [PubMed]