Abstract
Objective
To describe and examine potential predictors of changes in pain and disability in patients with shoulder pain who have completed 3 months of digitally delivered treatment comprising exercise and patient education.
Design
Retrospective cohort study (clinicaltrials.org Nr: NCT05402514).
Subjects
Patients with shoulder pain who completed treatment (n = 682).
Methods
Primary outcome was change in shoulder pain (numerical rating scale 0–10; minimal clinical important change: at least 2 points). Pain and disability were reported on the Shoulder Pain and Disability Index. Changes in outcomes were analysed with paired sample t-tests. Association with potential predictors (sex, age, education, body mass index, physical activity, symptom duration, baseline pain/function, and treatment adherence) were explored with linear regression models
Results
Statistically significant improvements were found for all treatment outcomes. Minimal clinically important change in pain was reached by 54.5% (n = 372). Higher baseline level of symptoms, short symptom duration, and high treatment adherence were associated with greater changes.
Conclusion
Patients with shoulder pain reported significant reductions in pain and disability following treatment, but the clinical relevance of the improvements has not been confirmed. Satisfactory treatment adherence, higher baseline pain and shorter symptom duration predicted larger improvements. A control group is needed to evaluate the actual effect of the treatment.
LAY ABSTRACT
Shoulder pain can be treated through exercise and patient education, which is often delivered by physiotherapists and other healthcare professionals. This study examined how shoulder pain and disability change following 3 months of digitally delivered treatment with exercise and patient education. Reductions in shoulder pain and disability were found after completion of treatment. However, these reductions only reached clinically meaningful levels (a change that is experienced as real change by patients) in half of the patients treated. Larger improvements were associated with the following factors: complying with treatments as prescribed; higher levels of pain at the start of treatment; and shorter symptom duration. In summary, patients appear to improve following digitally delivered treatment for shoulder pain, especially with more severe initial symptoms. Yet, approximately half of all patients do not experience meaningful changes in pain and disability. Further studies with control groups are needed to investigate the actual effect of the treatment.
Key words: exercise therapy, patient education, shoulder impingement syndrome, shoulder pain, telemedicine
The Global Burden of Disease Study identifies musculoskeletal (MSK) conditions as a leading cause of global morbidity (1). One of the most common MSK conditions is shoulder pain, with a lifetime prevalence of 7–10% (2). In primary care, approximately half of all patients with shoulder complaints are diagnosed with subacromial shoulder pain (3). The first-line treatment for subacromial shoulder pain is exercise, a modality that appears to be as effective as surgical alternatives for a variety of shoulder diagnoses (4–6).
Specific exercises for shoulder pain have been shown to improve function and reduce pain as well as the need for subacromial decompression surgery in comparison with unspecific exercises (7). However, in other studies, progressive exercise was not superior to a single face-to-face session including patient education and exercise recommendations (8), and did not outperform a placebo intervention (9). Physiotherapist (PT)-led exercise treatment, individually or group-based, is often used in clinical studies (4, 7, 10), but home-based exercise programmes yield similar clinical outcomes with lower associated costs for the healthcare system (10).
Exercise and patient education can be delivered via telehealth, the delivery of healthcare from a distance by digital information- and communication technology, which has been widely adopted during the SARS-CoV-2 (COVID-19) pandemic (11). Telehealth has been implemented successfully for a variety of MSK conditions (12), and has been shown to be associated with improvements in function and pain (12–14). Digital delivery of exercise interventions may improve patient accessibility (15) while being cost-effective (16). This model of delivery may also boost adherence compared with standard home exercises (17). Adherence to prescribed treatments is associated with improved pain and physical function in patients with musculoskeletal pain (18). According to a recent systematic review, telehealth may be an adequate alternative to face-to-face-treatment for patients with shoulder pain (19) but real-world investigations of telehealth for these patients are sparse (20). Furthermore, it is not known which patient-specific factors may associate with more favourable treatment outcomes.
The aim of this study was to describe changes in pain and perceived shoulder disability in patients with shoulder pain who had completed 3 months of digitally delivered first-line treatment comprising exercise and patient education. A further aim was to examine if, and to what extent, demographics, symptoms and health-related factors at baseline, or treatment adherence are associated with the change in outcomes.
METHODS
Study design
This is a retrospective cohort study (clinicaltrials.org Nr NCT05402514). Ethics approval was obtained through the Swedish Ethical Review Authority (Dnr: 2022-01012-01) and digital informed consent was provided by all participants.
Participants
Patients eligible for the digital first-line treatment for shoulder pain, who started the treatment between 5 October 2021 and 24 June 2022, provided informed consent, and completed the 3 months of treatment were included. Patients were eligible if they were at least 18 years of age and had subacute (> 6 weeks) or long-term (> 12 weeks) shoulder pain.
The screening process comprised 2 parts: a screening questionnaire of absolute exclusion criteria; and an assessment of relative exclusion criteria by an assigned PT via telephone or video call. Absolute exclusion criteria were: (i) acute shoulder pain, (ii) shoulder pain caused by trauma within the last 3 months that had not been physically assessed, and (iii) signs of acute infections, suspected undiagnosed cervical radiculopathy, or shortness of breath/chest pain associated with shoulder pain. Individuals with absolute exclusion criteria were excluded from treatment and strongly advised to seek face-to-face medical care. Relative exclusion criteria to be investigated further and assessed by the assigned PT through a telephone call or video consultation were: prior cancer diagnosis, suspicion of adhesive capsulitis, opioid use due to high levels of shoulder pain, pain at rest, inflammatory disease diagnosis, and chronic pain conditions with atypical shoulder pain. Once patients with absolute exclusion criteria had been physically assessed and cleared by a medical doctor or PT, they were welcomed back into the programme.
During the baseline data collection period (5 October 2021 to 24 June 2022) 1,986 patients were registered. Patients who did not provide research consent (n = 129), participants who completed or stopped treatment prior to the 3-month follow-up evaluation (n = 1,167), and participants who completed 3-months of treatment but without follow-up data (n = 8) were not included in the final sample. The final sample comprised the 682 patients who completed the digital treatment over 3 months (Fig. 1). The final sample included in the study was predominantly female (69%; n = 473), with mean age of 63.5 years (SD 10) and consisted to 50% (n = 342) of patients in retirement, while 45% (n = 308) were working (Table I).
Fig. 1.
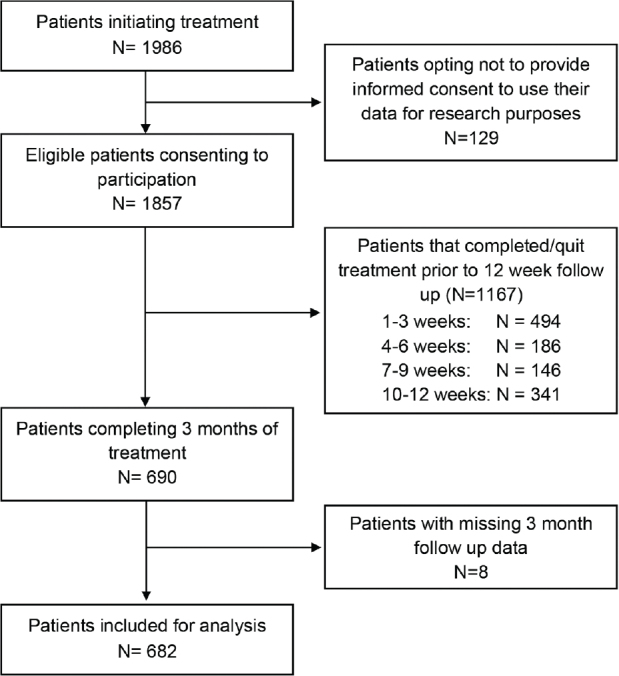
Flow of participants in the study.
Table I.
Participant characteristics (n = 682)
| Characteristics | |
|---|---|
| Sex, % (n) Male Female |
31 (209) 69 (473) |
| Age in years, mean (SD) | 63.5 (10.3) |
| Body mass index, kg/m2, mean (SD) | 26.0 (4.0) |
| Educational level (n = 660) At least senior high school, % (n) University, % (n) |
78.5 (518) 40.8 (269) |
| Occupational status, % (n) Working Retired Sick leave Other |
45.2 (308) 50.1 (342) 2.7 (18) 2.0 (14) |
| Self-reported activity level ≥ WHO recommendation, % (n) | 64.5 (440) |
| Duration of shoulder symptoms in months (n = 647), % (n) < 6 6–12 > 12 |
26.4 (171) 20.2 (131) 53.3 (345) |
| Pain in other joints, % (n) | 72.3 (493) |
World Health Organization recommendations for physical activity and exercise: ≥ 150 min moderate activity/≥ 60 min vigorous activity.
n is given for variables with missing data. When n is not reported, all 682 patients provided data. SD: standard deviation.
Digital treatment intervention
The digital first-line treatment platform Joint Academy® is a part of the public healthcare system in Sweden and costs for residents are covered by the national health insurance. Patients can enter the programme with or without referral. Commonly, patients are recommended to enter the programme by their caregiver, find an advertisement on social media, gain access via the company website, or become aware of the programme by word of mouth. Before entering the programme and getting in contact with a PT, patients are screened by a series of questions regarding existing symptoms and potential causes for these symptoms (see absolute exclusion criteria). When patients pass the screening questionnaire, they are booked for a compulsory telephone or video call with a personal PT who assesses inclusion eligibility for the treatment programme. The treatment programme is based on the existing evidence for treating subacromial shoulder pain (4, 21) and inspired by specific exercises from a RCT reporting reduced need for surgery (7). The programme focuses on strengthening the rotator cuff and the muscles stabilizing the scapula. Every day, 2 progressively adaptable exercises are delivered via an app through videos with subtitles. Exercise progression is delivered in 3 levels and automatically adjusted to the perceived difficulty reported by patients (rated as “easy”, “medium”, hard” after exercise performance). Patients also receive short education lessons 2–3 times per week. Compulsory telephone or video consultations are scheduled at baseline, at 6 weeks, and at 3 months, following initiation of treatment. Patients are able to communicate with their PT through an asynchronous chat, and with other patients through a peer support group chat. The treatment delivery and follow-up structure is identical to other digital treatments from the same digital care provider and is thoroughly described in previous studies (12, 13). A more detailed description is given in Appendix S1.
Data collection
Patients self-reported all outcomes via the digital programme interface. Outcomes were collected within the compulsory baseline questionnaire and the 3-month follow-up questionnaire.
Baseline variables and potential predictors. The baseline survey collected sociodemographic data including age, sex, weight, height, level of education, current working status, and physical activity levels. Patients also provided information related to their shoulder pain, such as intensity, disability, symptom duration, and medication use. Adherence to the programme was assessed as the percentage of completed activities throughout the 3 months of treatment. An adherence of at least 80% (corresponding to exercising ≥ 5 times a week) was considered and defined as “satisfactory adherence” (22).
Outcomes. Primary outcome: Shoulder pain was assessed by asking the patients to mark their average shoulder pain during the past week on a NRS ranging from 0 (no pain) to 10 (unbearable pain) (23), at baseline and follow-up (3 months). Minimal clinically important change (MCIC) in pain was defined as a raw NRS reduction of at least 2 points (24).
Secondary outcomes. Self-reported shoulder pain and disability was assessed with the Shoulder Pain and Disability Index (SPADI). The questionnaire has 2 dimensions; 5 questions about the severity of the patient’s pain (0–10, no pain to worst imaginable pain) and 8 questions regarding difficulty performing functional activities (0–10, no difficulty to so difficult it requires help), which are summarized in the sub-index SPADI pain and the SPADI disability and combined into the SPADI total index range 0–100 (25). SPADI has been proven valid and reliable for patients with shoulder pain, useful for both clinical and research purposes (25, 26).
The Patient Acceptable Symptom State (PASS) was assessed by asking: “Considering your shoulder function, do you feel that your current state is satisfactory? Regarding shoulder function you should take into account all activities you perform during your daily life, sport and recreational activities, your level of pain and other symptoms, and your quality of life related to your shoulder.” After 3 months of treatment, patients answered all shoulder pain related questions (including PASS) again.
Statistical analysis
Baseline and demographic variables were presented with descriptive statistics. Demographics and baseline values among the final sample were also compared with dropouts (excluding patients not providing informed consent). Comparisons of continuous data were performed by independent samples t-test and categorical outcomes with χ2 test.
Change in outcomes between baseline and follow-up was analysed with paired samples t-test, presented along with standardized effect sizes (Cohen’s d; small [d ≥ 0.2]; medium [d ≥ 0.5]; large [d ≥ 0.8]) or with McNemar test for binary variables. For the prediction analysis, change in outcomes of pain (NRS) and function (SPADI pain, disability, and total index) were computed for each individual and included as a dependent variable in linear regression models. Baseline variables regarding sex, age, education (university degree), body mass index (BMI), symptom duration (categorical; < 6, 6–12 or > 12 months), pain in other joint, and fulfilment of World Health Organization (WHO) criteria of physical activity (at least 150 min light to moderate physical activity or at least 60 min vigorous physical activity per week), and treatment adherence (at least 80%) were included as potential predictors. Baseline values of outcome measures (NRS or SPADI, respectively) was also included. Separate univariate models for each, and thereafter a multivariable model including all, defined potential predictors were performed. The multiple models were performed both with and without included baseline values of the change in outcome measure. R2 is presented for both versions of multivariable models (with and without included baseline value of outcome variable), but tables present the regression coefficients (with corresponding 95% confidence intervals; 95% CI) for (i) separate univariate models and (ii) the multivariable model including baseline values of the outcome variable. Corresponding logistic regression models (univariate and multiple including baseline NRS) were used for analysis of odds ratios for achieving MCIC of NRS. Alpha level was set at 0.05.
RESULTS
In the final sample (n = 682), median adherence to the programme was 89.4% (interquartile range: 73.9–96.2%). Over the course of the treatment period, 68% of patients had satisfactory adherence (completed ≥ 80% of treatment content). No significant differences were found between the final sample and dropouts in terms of shoulder pain and disability (NRS and SPADI) as well as most other demographic and baseline variables (Table SI). The dropout group had younger age (mean difference: 4.5 years (95% CI: 3.4; 5.6)), lower BMI (mean difference: 0.4 (95% CI: 0.01; 0.80)) and higher proportion of patients with shorter symptom duration (p = 0.033). There was also a significant difference in occupational status, with a larger share of dropouts still being in employment (Table SI).
Treatment outcomes at baseline and upon completion of the intervention
All treatment outcomes improved significantly from baseline to the follow-up, with improvements in shoulder pain and disability (NRS, SPADI), reduction in the use of pain medication and an increased proportion of patients achieving the PASS (Table II). The improvements corresponded to large, standardized effect sizes for outcomes related to pain (d = –0.94) and medium effect size in relation to disability (d = –0.68). The proportion of patients achieving PASS increased from 12.2% (n = 83) to 43.5% (n = 297), and 54.5% (n = 372) achieved the MCIC in NRS at 3-month follow-up.
Table II.
Treatment outcomes before and after intervention (n = 682)
| Baseline | 3 months | Mean diff (95% CI) | d (95% CI) | p-value | |
|---|---|---|---|---|---|
| NRS Pain, mean (SD) | 5.0 (1.9) | 3.2 (2.0) | –1.8 (–2.0, –1.7) | –0.9 (–1.0, –0.8) | < 0.001 |
| SPADI, mean (SD) | |||||
| Pain | 47.4 (17.6) | 31.3 (19.7) | –16.0 (–17.3, –14.8) | –0.9 (–1.0, –0.8) | < 0.001 |
| Disability | 34.0 (21.1) | 23.1 (20.0) | –11.0 (–12.1, –9.7) | –0.7 (–0.8, –0.6) | < 0.001 |
| Total index | 40.7 (17.7) | 27.2 (18.9) | –13.5 (–14.6, –12.3) | –0.9 (–1.0, –0.8) | < 0.001 |
| PASS, % (n) | 12.2 (83) | 43.5 (297) | – | - | < 0.001 |
| Medication use, % (n) Not at all Occasionally Most days/week Daily Total n |
42.1 (278) 34.1 (225) 10.8 (71) 13.0 (86) (660) |
57.8 (394) 27.7 (189) 5.3 (36) 9.2 (63) (682) |
– – – – – |
– – – – – |
– – – – – |
| Medication usea, % (n) | 57.7 (381) | 41.9 (286) | – | – | < 0.001 |
Medication use: at least occasionally.
NRS: numerical rating scale (range: 0–10); SD: standard deviation; SPADI: Shoulder Pain and Disability Index (range 0–100); PASS: Patient Acceptable Symptom State.
Potential predictors for change in treatment outcome after the intervention
Demographic variables were not associated with changes in treatment outcomes. Satisfactory adherence was a significant predictor for changes in treatment outcome. Baseline variables related to shoulder pain and disability were also associated with subsequent change in outcomes. The explained variance (r2) in the multiple regression models without baseline level of symptoms (NRS and SPADI scores) included was 4–6% (NRS: 5%; SPADI pain: 4%; SPADI total score: 6%; SPADI disability: 6%). With baseline values of symptoms included in the model, r2 increased to 16–23% (NRS: 22%; SPADI pain: 16%; SPADI disability: 23%, SPADI total: 16%). In general, baseline pain and symptom duration of more than 12 months were significantly associated with change in treatment outcome (Table III and IV). Higher pain scores (NRS) at baseline were associated with larger decreases in reported pain scores, and symptom duration of more than 12 months was associated with less improvement (decrease) in pain scores at the 3-month follow-up. Patients with higher baseline pain had significantly higher odds of achieving MCIC in pain reduction, while patients with more than 12 months of symptoms had significantly lower odds of achieving MCIC in pain reduction (Table V).
Table III.
Associations between potential predictive variables and change in shoulder pain (NRS)
| Predictors | Univariate |
Multivariable model |
||||
|---|---|---|---|---|---|---|
| Regression coeff (b) | 95% CI | p-value | Regression coeff (b) | 95% CI | p-value | |
| Sex (female) | –0.20 | –0.52, 0.11 | 0.208 | 0.10 | –0.20, 0.39 | 0.530 |
| Age | 0.01 | –0.01, 0.02 | 0.268 | 0.01 | –0.001, 0.03 | 0.081 |
| Education (college or university) | –0.32 | –0.62, –0.02 | 0.039 | –0.37 | –0.65, –0.10 | 0.008 |
| BMI | –0.02 | –0.06, 0.02 | 0.276 | –0.3 | –0.06, 0.01 | 0.128 |
| Symptom durationa, months 6–12 >12 |
0.33 0.71 |
–0.11, 0.77 0.36, 1.06 |
0.138 < 0.001 |
0.31 0.57 |
–0.08, 0.70 0.25, 0.89 |
0.120 < 0.001 |
| Pain other joints | 0.22 | –0.11, 0.55 | 0.188 | 0.26 | –0.05, 0.57 | 0.095 |
| PA WHOb | –0.06 | –0.36, 0.25 | 0.719 | –0.12 | –0.40, 0.17 | 0.417 |
| Adherence ≥ 80% | –0.59 | –0.90, –0.29 | < 0.001 | –0.69 | –0.98, –0.39 | < 0.001 |
| Baseline pain (NRS) | –0.45 | –0.52, –0.38 | < 0.001 | –0.44 | –0.51, –0.36 | < 0.001 |
Reference = symptom duration < 6 months.
Dichotomized to either fulfilling WHO’s physical activity recommendations or not.
NRS: numerical rating scale (range 0–10); BMI: body mass index; PA: physical activity; WHO: World Health Organization.
Table IV.
Associations between potential predictive variables and change in shoulder pain and disability (SPADI)
| Predictors | SPADI Pain |
SPADI Disability |
SPADI Total |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate |
Multivariable model |
Univariate |
Multivariable model |
Univariate |
Multivariable model |
|||||||
| b (95% CI) | p-value | b (95% CI) | p-value | b (95% CI) | p-value | b (95% CI) | p-value | b (95% CI) | p-value | b (95% CI) | p-value | |
| Sex (female) | –2.10 (–4.88; 0.69) | 0.140 | –0.26 (–2.95; 2.44) | 0.852 | –2.25 (–4.87; 0.37) | 0.092 | 0.00 (–2.43; 2.44) | 0.997 | –2.17 (–4.63; 0.28) | 0.082 | –0.46 (–2.83; 1.92) | 0.707 |
| Age | –0.01 (–0.12; 0.13) | 0.930 | 0.05 (–0.08; 0.17) | 0.468 | –0.10 (–0.22; 0.02) | 0.095 | 0.04 (–0.08; 0.15) | 0.529 | –0.05 (–0.16; 0.06) | 0.399 | 0.03 (–0.08; 0.14) | 0.588 |
| Education (college or university) | 0.52 (–3.19; 2.14) | 0.701 | –1.11 (–3.64; 1.42) | 0.390 | 0.68 (–1.84; 3.19) | 0.598 | –0.33 (–2.60; 1.95) | 0.779 | 0.08 (–2.27; 2.42) | 0.949 | –0.50 (–2.72; 1.73) | 0.662 |
| BMI | 0.04 (–0.28; 0.36) | 0.809 | –0.01 (–0.33; 0.32) | 0.967 | –0.03 (–0.33; 0.27) | 0.846 | –0.02 (–0.31; 0.27) | 0.882 | 0.01 (–0.28; 0.29) | 0.973 | 0.05 (–0.33; 0.24) | 0.749 |
| Symptom durationa, months | ||||||||||||
| 6–12 | 3.23 (–0.63; 7.08) | 0.100 | 3.24 (–0.34; 6.82) | 0.076 | –0.27 (–3.88; 3.33) | 0.882 | 0.52 (–2.69; 3.73) | 0.751 | 1.48 (–1.89; 4.84) | 0.389 | 1.74 (–1.40: 4.88) | 0.276 |
| >12 | 5.89 (2.79; 9.00) | < 0.001 | 5.30 (2.39; 8.20) | < 0.001 | 3.99 (1.09; 6.90) | 0.007 | 3.33 (0.73; 5.94) | 0.012 | 4.94 (2.23; 7.65) | < 0.001 | 4.32 (1.77; 6.86) | < 0.001 |
| Pain other joints | 2.47 (–0.40; 5.33) | 0.092 | 2.62 (–0.19; 5.44) | 0.068 | 4.66 (1.98; 7.35) | < 0.001 | 4.64 (2.12; 7.17) | < 0.001 | 3.56 (1.04; 6.08) | 0.006 | 3.65 (1.18; 6.11) | 0.004 |
| PA WHOb | –2.33 (–5.01; 0.36) | 0.089 | –2.36 (–4.95; 0.24) | 0.075 | 1.07 (–1.45; 3.60) | 0.409 | –0.78 (–3.13; 1.57) | 0.516 | –0.63 (–3.00; –1.74) | 0.601 | –1.36 (–3.65; –0.92) | 0.242 |
| Adherence ≥ 80% | –5.5 (–8.24; –2.85) | < 0.001 | –6.15 (.8.79; –3.50) | < 0.001 | –5.11 (–7.66; .2.56) | < 0.001 | –5.25 (–7.63; –2.88) | < 0.001 | –5.33 (–7.71; –2.96) | < 0.001 | –5.73 (–8.05; –3.41) | < 0.001 |
| Baseline SPADI | –0.35 (–0.41; 0.28) | < 0.001 | –0.34 (–0.41; 0.27) | < 0.001 | –0.34 (–0.39; –0.29) | < 0.001 | –0.33 (–0.39; –0.28) | < 0.001 | –0.29 (–0.35; –0.23) | < .001 | –0.28 (–0.34; –0.22) | < 0.001 |
Reference = symptom duration < 6 months.
Dichotomized to either fulfilling WHO’s physical activity recommendations or not.
BMI: body mass index; PA: physical activity; WHO: World Health Organization; SPADI: Shoulder Pain and Disability Index (range: 0–100).
Table V.
Relative odds for achieving minimal clinical important change (change in shoulder pain [NRS])
| Predictors | Crude/univariate models |
Adjusted/multiple model |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | |
| Sex (female) | 1.12 | 0.81, 1.55 | 0.505 | 0.86 | 0.60, 1.25 | 0.432 |
| Age | 0.99 | 0.98, 1.01 | 0.261 | 0.99 | 0.97, 1.00 | 0.107 |
| Educationa | 1.28 | 0.93, 1.75 | 0.125 | 1.39 | 0.98, 1.98 | 0.062 |
| BMI | 1.03 | 0.99, 1.07 | 0.126 | 1.04 | 0.98, 1.09 | 0.067 |
| Symptom durationb, months | ||||||
| 6–12 | 1.02 | 0.64, 1.63 | 0.940 | 1.03 | 0.62, 1.69 | 0.922 |
| >12 | 0.62 | 0.43, 0.90 | 0.011 | 0.65 | 0.43, 0.97 | 0.033 |
| Pain other joints | 0.84 | 0.60, 1.18 | 0.310 | 0.82 | 0.56, 1.22 | 0.327 |
| PA WHOc | 1.11 | 0.81, 1.52 | 0.520 | 1.14 | 0.80, 1.63 | 0.472 |
| Adherence ≥ 80% | 1.56 | 1.13, 2.15 | 0.007 | 1.92 | 1.33, 2.76 | < 0.001 |
| Baseline pain (NRS) | 1.43 | 1.31, 1.57 | < 0.001 | 1.40 | 1.27, 1.54 | < 0.001 |
College/University.
Reference = symptom duration < 6 months.
Dichotomized to either fulfilling WHO’s physical activity recommendations or not.
BMI: body mass index; OR: odds ratio; PA: physical activity; WHO: World Health Organization; NRS: numerical rating scale.
DISCUSSION
Patients reported statistically significant improvements in treatment outcomes following the treatment period. The percentage of patients reporting PASS increased from 12% to 43%, and 54.5% of patients achieved MCIC in pain. Satisfactory adherence with the treatment programme was associated with larger improvements in outcomes. Also, higher levels of baseline pain and disability were associated with larger decreases in pain and disability (NRS and SPADI), respectively, following treatment.
Patients in this study reported statistically significant less shoulder pain and disability following 3 months of digitally delivered exercise and patient education for shoulder pain. Due to the observational study design with lack of a control group and randomized treatment allocation, it was not possible to determine causal effects of the treatment. Factors such as natural improvement over time and placebo effects may contribute to the improved outcomes. However, satisfactory adherence to the treatment was associated with larger improvements. Exercise is the first line of treatment for patients with shoulder pain (27, 28) and is an effective measure to improve pain levels and self-reported function in this group of patients as reported in several systematic reviews and meta-analyses (21, 27, 29, 30). The reduction in pain observed in this study was characterized by a large effect size (Cohen’s d > 0.9), but the absolute change in NRS scores (mean change –1.8) was less than the MCIC of 2 points. The observed changes in SPADI scores were also characterized by medium to large effect sizes (Cohen’s d 0.7–0.9) and at or above the suggested threshold for clinical relevance (31). These within-group changes in outcomes are within ranges of previous randomized controlled trials (29, 32–34) but do not answer the question as to whether patients are left in an acceptable symptom state.
In the current study, 43% of patients achieved PASS following 3 months of digitally delivered treatment (compared with 12% before treatment), which is similar to treatment results in other Scandinavian specialized care settings where patients often receive a supervised exercise intervention (35). In a systematic review and meta-analysis, Liaghat et al. (36) showed that self-training was equally effective as supervised training in reducing pain and improving function in patients with shoulder pain. Self-training often entails that patients receive an information leaflet with some exercises and are encouraged to perform these exercises independently. Digitally delivered treatment, such as the one delivered in the current study, is based on self-training, but includes remote supervision and guidance of a PT. The literature evaluating digital care for shoulder patients is in its infancy, but has grown during the COVID-19 pandemic. A recent systematic review included 6 randomized controlled trials comparing digitally delivered care to standard supervised or home-based exercise treatment (19). No difference was found between telehealth and in-person physiotherapy, while telehealth was found to be superior in comparison with advice alone. Gava et al. (19) also reported similar dropout rates for digitally delivered care compared with the comparison groups. The dropout rate for randomized controlled trials, the study type included in aforementioned review, is approximately 11% (37). For digital interventions, the respective rate of dropouts is reported to be higher (40% (95% CI: 16–63)) with even higher rates in less controlled study designs (49% (27–70)) (38). This study describes outcomes of a digital treatment programme implemented in the real world, which may explain the high number of dropouts. It is important to note that the group of dropouts in the current study includes both patients who stopped the programme at an early stage and patients who completed treatment earlier than the recommended 3 month and therefore did not receive the final follow-up. Nevertheless, the 37% of all included patients who actually completed treatment in the current study is close to the 45% who completed 3 months of face-to-face treatment in a similar real-world setting in Scandinavia (39).
Pain and function seemed to improve irrespective of investigated demographic or lifestyle factors. The multivariable regression models predicted only a small percentage of the variance in outcome changes (4–6%), indicating that patient demographics and other independent variables had little predictive value. The explained variance of the model increased (to 16–23%) once baseline symptoms (NRS- or SPADI-scores) had been added. Higher baseline pain and disability were associated with larger decrease/improvement in these outcomes. These results may indicate a “regression to the mean” effect. A randomized control group would have provided a better view of the actual treatment effect. In accordance with previous reports (40, 41), long symptom duration (more than 12 months) was consistently related to less improvement during the treatment. Finally, associations were found with larger improvements in outcomes, and the highest odds for clinically relevant improvements, in patients who completed treatment with satisfactory adherence. In other words, and unsurprisingly, the treatment appears to work best when it is actually performed. Nevertheless, telehealth is a critical complement to in-person care, not just during global pandemics. It also helps to reach patients in rural areas, patients with other medical diagnoses restricting personal contact, or patients who do not have the occupational flexibility to regularly meet their caregiver.
Strengths and limitations
A strength of the current study is the large sample size. However, there are some factors to consider that may affect generalizability of the results to the wider population with shoulder pain. The largest threat to generalizability is selection bias. Since the programme is marketed on social media and the company’s website there will be selection regarding which people respond to the marketing. Patients in the current study are approximately 15 years older than in other studies on patients with shoulder pain (35), which may be due to the fact that the platform was developed and is primarily used to treat osteoarthritis. Hence, while these results are generalizable to an older population with shoulder pain, they may not be generalized to younger populations, such as, for example, overhead athletes with shoulder problems. Furthermore, the study sample was restricted to patients who completed 3 months of treatment and results of the current study can therefore not be generalized to all patients offered the treatment. A large proportion of patients initiating the treatment did not complete the 3-month follow-up. Comparison of these dropouts with the included sample of patients revealed that patients completing treatment were older and had longer symptom duration. While these differences may affect the response to treatment, the most important variables, namely our dependent variables shoulder pain and function, did not differ between groups at baseline. Nevertheless, it is impossible to know if or how the drop-out has affected the results, since we do not know if patients chose to quit the programme due to either early clinical improvements, poor outcomes, or other factors. Future research is needed to investigate factors associated with dropout from offered treatments to shoulder pain. Our sample is heterogeneous in terms of medical diagnoses. Even though one may argue that face-to-face assessments may be associated with more clinical certainty regarding diagnosis, digital assessments by a physiotherapist appear to be valid and reliable (42). Lastly, but most importantly, the current study was observational and did not have a control group. Therefore, contextual factors may have contributed to treatment results. The association between higher baseline levels and higher reductions in pain may indicate natural history and regression to the mean. Yet, 3 in 4 patients had symptoms for more than 6 months and may not have sought medical care at the moment of most severe complaints.
Conclusion
Patients with shoulder pain who completed 3 months of digitally delivered exercise treatment and patient education reported statistically significant reduction in pain and disability. The clinical relevance of these improvements should, however, be interpreted with caution, since 57% of the treated patients did not achieve a PASS, and 45.5% did not show clinically relevant reductions in pain. Satisfactory treatment adherence, higher baseline pain and less than 1 year of symptoms were associated with larger improvements in shoulder pain and disability. Randomized controlled trials are needed to investigate the actual effects of the treatment.
Supplementary Material
CHANGES IN PAIN AND DISABILITY IN PATIENTS WITH SHOULDER PAIN AFTER THREE MONTHS OF DIGITALLY DELIVERED EXERCISE AND PATIENT EDUCATION
CHANGES IN PAIN AND DISABILITY IN PATIENTS WITH SHOULDER PAIN AFTER THREE MONTHS OF DIGITALLY DELIVERED EXERCISE AND PATIENT EDUCATION
ACKNOWLEDGEMENTS
The authors thank Professor Stefan Lohmander for reading and providing valuable input on the manuscript.
The study was approved by the Swedish Ethical Review Authority and registered at www.clinicaltrials.org (Nr: NCT05402514).
Conflicts of interest
PS, HN, HH, MMI are/were employed by Joint Academy® (www.jointacademy.com), an online health service reimbursed by the Swedish Healthcare system. TW and FE have no competing interests to declare.
REFERENCES
- 1.Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396: 1204–1222. DOI: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luime JJ, Koes BW, Hendriksen IJ, Burdorf A, Verhagen AP, Miedema HS, et al. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol 2004; 33: 73–81. DOI: 10.1080/03009740310004667 [DOI] [PubMed] [Google Scholar]
- 3.van der Windt DA, Koes BW, Boeke AJ, Deville W, De Jong BA, Bouter LM. Shoulder disorders in general practice: prognostic indicators of outcome. Br J Gen Pract 1996; 46: 519–523. [PMC free article] [PubMed] [Google Scholar]
- 4.Haik MN, Alburquerque-Sendin F, Moreira RF, Pires ED, Camargo PR. Effectiveness of physical therapy treatment of clearly defined subacromial pain: a systematic review of randomised controlled trials. Br J Sports Med 2016; 50: 1124–1134. DOI: 10.1136/bjsports-2015-095771 [DOI] [PubMed] [Google Scholar]
- 5.Karjalainen TV, Jain NB, Page CM, Lahdeoja TA, Johnston RV, Salamh P, et al. Subacromial decompression surgery for rotator cuff disease. Cochrane Database Syst Rev 2019; 1: CD005619. DOI: 10.1002/14651858.CD005619.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ryosa A, Laimi K, Aarimaa V, Lehtimaki K, Kukkonen J, Saltychev M. Surgery or conservative treatment for rotator cuff tear: a meta-analysis. Disabil Rehabil 2017; 39: 1357–1363. DOI: 10.1080/09638288.2016.1198431 [DOI] [PubMed] [Google Scholar]
- 7.Hallgren HC, Holmgren T, Oberg B, Johansson K, Adolfsson LE. A specific exercise strategy reduced the need for surgery in subacromial pain patients. Br J Sports Med 2014; 48: 1431–1436. DOI: 10.1136/bjsports-2013-093233 [DOI] [PubMed] [Google Scholar]
- 8.Hopewell S, Keene DJ, Marian IR, Dritsaki M, Heine P, Cureton L, et al. Progressive exercise compared with best practice advice, with or without corticosteroid injection, for the treatment of patients with rotator cuff disorders (GRASP): a multicentre, pragmatic, 2 x 2 factorial, randomised controlled trial. Lancet 2021; 398: 416–428. DOI: 10.1016/S0140-6736(21)00846-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bennell K, Wee E, Coburn S, Green S, Harris A, Staples M, et al. Efficacy of standardised manual therapy and home exercise programme for chronic rotator cuff disease: randomised placebo controlled trial. BMJ 2010; 340: c2756. DOI: 10.1136/bmj.c2756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Christiansen DH, Hjort J. Group-based exercise, individually supervised exercise and home-based exercise have similar clinical effects and cost-effectiveness in people with subacromial pain: a randomised trial. J Physiother 2021; 67: 124–131. DOI: 10.1016/j.jphys.2021.02.015 [DOI] [PubMed] [Google Scholar]
- 11.Garfan S, Alamoodi AH, Zaidan BB, Al-Zobbi M, Hamid RA, Alwan JK, et al. Telehealth utilization during the Covid-19 pandemic: a systematic review. Comput Biol Med 2021; 138: 104878. DOI: 10.1016/j.compbiomed.2021.104878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cottrell MA, Galea OA, O’Leary SP, Hill AJ, Russell TG. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clin Rehabil 2017; 31: 625–638. DOI: 10.1177/0269215516645148 [DOI] [PubMed] [Google Scholar]
- 13.Dahlberg LE, Dell’Isola A, Lohmander LS, Nero H. Improving osteoarthritis care by digital means – effects of a digital self-management program after 24- or 48-weeks of treatment. PLoS One 2020; 15: e0229783. DOI: 10.1371/journal.pone.0229783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gohir SA, Eek F, Kelly A, Abhishek A, Valdes AM. Effectiveness of internet-based exercises aimed at treating knee osteoarthritis: the iBEAT-OA randomized clinical trial. JAMA Netw Open 2021; 4: e210012. DOI: 10.1001/jamanetworkopen.2021.0012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cronstrom A, Dahlberg LE, Nero H, Ericson J, Hammarlund CS. ‘I would never have done it if it hadn’t been digital’: a qualitative study on patients’ experiences of a digital management programme for hip and knee osteoarthritis in Sweden. BMJ Open 2019; 9: e028388. DOI: 10.1136/bmjopen-2018-028388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ekman B, Nero H, Lohmander LS, Dahlberg LE. Costing analysis of a digital first-line treatment platform for patients with knee and hip osteoarthritis in Sweden. PLoS One 2020; 15: e0236342. DOI: 10.1371/journal.pone.0236342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bennell KL, Marshall CJ, Dobson F, Kasza J, Lonsdale C, Hinman RS. Does a web-based exercise programming system improve home exercise adherence for people with musculoskeletal conditions?: a randomized controlled trial. Am J Phys Med Rehabil 2019; 98: 850–858. DOI: 10.1097/PHM.0000000000001204 [DOI] [PubMed] [Google Scholar]
- 18.Jakobsen MD, Sundstrup E, Brandt M, Andersen LL. Factors affecting pain relief in response to physical exercise interventions among healthcare workers. Scand J Med Sci Sports 2017; 27: 1854–1863. DOI: 10.1111/sms.12802 [DOI] [PubMed] [Google Scholar]
- 19.Gava V, Ribeiro LP, Barreto RPG, Camargo PR. Effectiveness of physical therapy given by telerehabilitation on pain and disability of individuals with shoulder pain: a systematic review. Clin Rehabil 2022; 36: 715–725. DOI: 10.1177/02692155221083496 [DOI] [PubMed] [Google Scholar]
- 20.Janela D, Costa F, Molinos M, Moulder RG, Lains J, Francisco GE, et al. Asynchronous and tailored digital rehabilitation of chronic shoulder pain: a prospective longitudinal cohort study. J Pain Res 2022; 15: 53–66. DOI: 10.2147/JPR.S343308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pieters L, Lewis J, Kuppens K, Jochems J, Bruijstens T, Joossens L, et al. An Update of systematic reviews examining the effectiveness of conservative physical therapy interventions for subacromial shoulder pain. J Orthop Sports Phys Ther 2020; 50: 131–141. DOI: 10.2519/jospt.2020.8498 [DOI] [PubMed] [Google Scholar]
- 22.Bailey DL, Holden MA, Foster NE, Quicke JG, Haywood KL, Bishop A. Defining adherence to therapeutic exercise for musculoskeletal pain: a systematic review. Br J Sports Med 2020; 54: 326–331. DOI: 10.1136/bjsports-2017-098742 [DOI] [PubMed] [Google Scholar]
- 23.Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs 2005; 14: 798–804. DOI: 10.1111/j.1365-2702.2005.01121.x [DOI] [PubMed] [Google Scholar]
- 24.Salaffi F, Stancati A, Silvestri CA, Ciapetti A, Grassi W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain 2004; 8: 283–291. DOI: 10.1016/j.ejpain.2003.09.004 [DOI] [PubMed] [Google Scholar]
- 25.Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y. Development of a shoulder pain and disability index. Arthritis Care Res 1991; 4: 143–149. [PubMed] [Google Scholar]
- 26.MacDermid JC, Solomon P, Prkachin K. The Shoulder Pain and Disability Index demonstrates factor, construct and longitudinal validity. BMC Musculoskelet Disord 2006; 7: 12. DOI: 10.1186/1471-2474-7-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nazari G, MacDermid JC, Bryant D, Athwal GS. The effectiveness of surgical vs conservative interventions on pain and function in patients with shoulder impingement syndrome. A systematic review and meta-analysis. PLoS One 2019; 14: e0216961. DOI: 10.1371/journal.pone.0216961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saltychev M, Virolainen P, Laimi K. Conservative treatment or surgery for shoulder impingement: updated meta-analysis. Disabil Rehabil 2020; 42: 1634–1635. DOI: 10.1080/09638288.2019.1622796 [DOI] [PubMed] [Google Scholar]
- 29.Dong W, Goost H, Lin XB, Burger C, Paul C, Wang ZL, et al. Treatments for shoulder impingement syndrome: a PRISMA systematic review and network meta-analysis. Medicine (Baltimore) 2015; 94: e510. DOI: 10.1097/MD.0000000000000510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hanratty CE, McVeigh JG, Kerr DP, Basford JR, Finch MB, Pendleton A, et al. The effectiveness of physiotherapy exercises in subacromial impingement syndrome: a systematic review and meta-analysis. Semin Arthritis Rheum 2012; 42: 297–316. DOI: 10.1016/j.semarthrit.2012.03.015 [DOI] [PubMed] [Google Scholar]
- 31.Roy JS, MacDermid JC, Woodhouse LJ. Measuring shoulder function: a systematic review of four questionnaires. Arthritis Rheum 2009; 61: 623–632. DOI: 10.1002/art.24396 [DOI] [PubMed] [Google Scholar]
- 32.Clausen MB, Holmich P, Rathleff MS, Bandholm T, Christensen KB, Zebis MK, et al. Effectiveness of adding a large dose of shoulder strengthening to current nonoperative care for subacromial impingement: a pragmatic, double-blind randomized controlled Trial (SExSI Trial): response. Am J Sports Med 2022; 50: NP20–NP23. DOI: 10.1177/03635465211055449 [DOI] [PubMed] [Google Scholar]
- 33.Larsson R, Bernhardsson S, Nordeman L. Effects of eccentric exercise in patients with subacromial impingement syndrome: a systematic review and meta-analysis. BMC Musculoskelet Disord 2019; 20: 446. DOI: 10.1186/s12891-019-2796-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roddy E, Ogollah RO, Oppong R, Zwierska I, Datta P, Hall A, et al. Optimising outcomes of exercise and corticosteroid injection in patients with subacromial pain (impingement) syndrome: a factorial randomised trial. Br J Sports Med 2021; 55: 262–271. DOI: 10.1136/bjsports-2019-101268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Clausen MB, Merrild MB, Witten A, Christensen KB, Zebis MK, Holmich P, et al. Conservative treatment for patients with subacromial impingement: Changes in clinical core outcomes and their relation to specific rehabilitation parameters. PeerJ 2018; 6: e4400. DOI: 10.7717/peerj.4400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liaghat B, Ussing A, Petersen BH, Andersen HK, Barfod KW, Jensen MB, et al. Supervised training compared with no training or self-training in patients with subacromial pain syndrome: a systematic review and meta-analysis. Arch Phys Med Rehabil 2021; 102: 2428–2441 e2410. DOI: 10.1016/j.apmr.2021.03.027 [DOI] [PubMed] [Google Scholar]
- 37.Walters SJ, Bonacho Dos Anjos Henriques-Cadby I, Bortolami O, Flight L, Hind D, Jacques RM, et al. Recruitment and retention of participants in randomised controlled trials: a review of trials funded and published by the United Kingdom Health Technology Assessment Programme. BMJ Open 2017; 7: e015276. DOI: 10.1136/bmjopen-2016-015276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Meyerowitz-Katz G, Ravi S, Arnolda L, Feng X, Maberly G, Astell-Burt T. Rates of attrition and dropout in app-based interventions for chronic disease: systematic review and meta-analysis. J Med Internet Res 2020; 22: e20283. DOI: 10.2196/20283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Clausen MB, Merrild MB, Holm K, Pedersen MW, Andersen LL, Zebis MK, et al. Less than half of patients in secondary care adheres to clinical guidelines for subacromial pain syndrome and have acceptable symptoms after treatment: A Danish nationwide cohort study of 3306 patients. Musculoskelet Sci Pract 2021; 52: 102322. DOI: 10.1016/j.msksp.2021.102322 [DOI] [PubMed] [Google Scholar]
- 40.Chester R, Shepstone L, Daniell H, Sweeting D, Lewis J, Jerosch-Herold C. Predicting response to physiotherapy treatment for musculoskeletal shoulder pain: a systematic review. BMC Musculoskelet Disord 2013; 14: 203. DOI: 10.1186/1471-2474-14-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Struyf F, Geraets J, Noten S, Meeus M, Nijs J. A Multivariable prediction model for the chronification of non-traumatic shoulder pain: a systematic review. Pain Physician 2016; 19: 1–10 [PubMed] [Google Scholar]
- 42.Zischke C, Simas V, Hing W, Milne N, Spittle A, Pope R. The utility of physiotherapy assessments delivered by telehealth: A systematic review. J Glob Health 2021; 11: 04072. DOI: 10.7189/jogh.11.04072 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
CHANGES IN PAIN AND DISABILITY IN PATIENTS WITH SHOULDER PAIN AFTER THREE MONTHS OF DIGITALLY DELIVERED EXERCISE AND PATIENT EDUCATION
CHANGES IN PAIN AND DISABILITY IN PATIENTS WITH SHOULDER PAIN AFTER THREE MONTHS OF DIGITALLY DELIVERED EXERCISE AND PATIENT EDUCATION


