Supplemental Digital Content is Available in the Text.
We developed a new technique for four-point transscleral suture fixation of intraocular lens using the double-suture technique to reduce the risk of suture breakage. Our follow-up results showed no suture breakage, no intraocular lens decentration or dislocation, and no suture-related complications were detected. This technique offers a new selection of transscleral fixation.
Key words: intraocular lens, surgical technique, transscleral fixation, double-suture technique
Abstract
Purpose:
To report the results of a novel surgical four-point transscleral suture fixation of intraocular lens (IOL) with four hollow haptics using the double-suture technique.
Methods:
We retrospectively reviewed the medical records of 15 eyes of 15 patients who underwent 4-point transscleral suture fixation of a foldable IOL using the double-suture technique. Preoperative data and follow-up data for at least 4 months were collected for all patients.
Results:
The IOLs were fixed and centered well. The mean preoperative corrected distance visual acuity was 0.70 ± 0.54 logarithm of the minimum angle of resolution (Snellen 20/102), and it improved to 0.29 ± 0.26 logarithm of the minimum angle of resolution (Snellen 20/39) at the final follow-up (P = 0.001). No vitreous hemorrhage, hypotony, suture breakage, retinal detachment, IOL dislocation, and iris capture was detected during the follow-up period in any of the patients.
Conclusion:
We have developed a novel technique for 4-point transscleral suture fixation of IOL using the double-suture technique with 9-0 polypropylene suture. This technique seemed to be safe and it may not require the surgeon to learn any new technique.
Transscleral suture fixation of a posterior chamber intraocular lens (PC IOL) is a widely accepted way to visually rehabilitate aphakic eyes without enough capsule support or with lens luxation. Successful transscleral fixation demands good centration of IOL and avoidance of tilt. At present, the most common method used for foldable IOL scleral suture fixation is two-point scleral fixation. However, this method has some complications, such as tilting or decentration of the IOL, iris capture.1–4 Iris capture may cause pupillary block with secondary glaucoma, pigment dispersion, iritis, and patients may experience vision loss or pain.2,5 As published previously,6,7 the technique of a closed continuous-loop transscleral suture for four-point fixation of the Akreos Adapt foldable IOL (Bausch & Lomb, Rochester, NY) has achieved a reliable and reproducible procedure, which improves anatomical and visual outcomes with a low incidence of these complications.
Suture breakage, which can cause IOL dislocation, is still a significant issue when using a scleral fixation. According to reports, the rate of suture breakage ranges from 0.47% to 27.9%.8–11 The difference in the rate of suture breakage may be explained by different surgical techniques applied. An in vitro experiment shows that suture exposure, the intensity of the ultraviolet light, and tensile strength may influence the useful lifetime of polypropylene sutures.12 The closed continuous-loop transscleral suture technology our institution described previously uses a single suture. The distance that the suture passes under the conjunctiva is 7 mm, which increases exposure to ultraviolet radiation, and the suture may be degraded easily by ultraviolet.
In the present study, we have developed a new surgical procedure enabling four-point fixation of the Akreos Adapt AO IOL (Bausch & Lomb) foldable IOL using the double-suture technique. The Akreos Adapt AO IOL (Bausch & Lomb) is a foldable hydrophilic acrylic aspherical IOL and it has four haptics, each with its own eyelet for suture passage. Our follow-up results showed the double-suture technique had achieved a reliable and safe procedure with a small incision, improved visual outcomes, reduced complications. Here, we describe this technique and report its clinical results.
Methods
The study was approved by the independent ethics committee at Eye Hospital Of Shandong First Medical University (Shandong Eye Hospital), Shandong Eye Institute, Qingdao, China, for this retrospective, noncomparative, interventional case series. The study adhered to the principles of the Declaration of Helsinki. All participants treated by this technique provided written informed consent of possible benefits and risks. This retrospective study included patients who underwent transscleral IOL fixation using the double-suture technique between September 2020 and August 2021 in the Eye Hospital of Shandong First Medical University in Jinan, China. Scleral fixation of the Akreos Adapt AO IOL is currently off-label. All patients underwent comprehensive preoperative and postoperative ophthalmic examinations, and data were collected, including age, sex, best-corrected visual acuity, corneal endothelium count, and intraocular pressure (IOP).
Surgical Technique
All surgeries were performed by the same surgeon (J.Z.). The key steps to this surgical procedure are outlined in the supplemental digital content (see Video, Supplemental Digital Content, http://links.lww.com/IAE/B794). We used trypan blue to mark the corneal periphery along a horizontal meridian that was centered over the visual axis. Four scleral fixation sites are marked 2 mm from the limbus and located 3.5 mm superior and inferior to the horizontal corneal markings. The conjunctiva was incised radially and limited dissection was performed to expose the bare sclera on the two scleral fixation points of the right. A 23-gauge pars plana vitrectomy with lensectomy was performed using a Constellation Vision System (Alcon Laboratories, Inc, Duluth, GA) under retrobulbar anesthesia for the luxated lenses or aphakia. When vitrectomy and lensectomy were completed, a 2.65-mm clear corneal incision according to the steep axis was made in the anterior limbus using a keratome. The anterior chamber was filled with an ophthalmic viscosurgical device. A foldable Akreos Adapt AO IOL was implanted in the anterior chamber through the clear corneal incision using an injector system.
Transscleral passage of a straight needle attached to a 9-0 polypropylene suture (Alcon) was performed 2 mm posterior to the corneal limbus into the PC. The straight needle was then passed through one eyelet on the bottom-right haptic side of the PC IOL and pulled out of the globe using the guidance of the 29-gauge insulin needle, which passed through one eyelet on the bottom-left haptic side of the PC IOL. The 9-0 polypropylene suture was allowed to traverse the eye and 2 eyelets of IOL from the bottom-right scleral bed to the bottom-left one and parallel to the horizontal meridian with the traction of the straight needle. The straight needle was performed 2 mm posterior to the corneal limbus and greater than or equal to 0.5 mm away from the bottom-left first point into the PC again. The straight needle was then passed through one eyelet on the bottom-left haptic side of the PC IOL and pulled out of the globe using the guidance of the 29-gauge insulin needle, which performed greater than or equal to 0.5 mm away from the bottom-right first point and passed through one eyelet on the bottom-right haptic side of the PC IOL. The straight needle was cut off, and the 2 ends of the 9-0 polypropylene suture were tied on the surface of the sclera. A lumpy friction knot was formed 1 mm away from the exit point of the 9-0 polypropylene suture. The end of the suture that was originally attached to the straight needle was cut short, and then the curved needle was passed to half the scleral depth next to the exit point for a short distance. When the needle tip was visible in the subconjunctival space, it was pulled out through the conjunctiva, and the suture was pulled tight. The friction knot entered the needle track, and it was buried in the sclera. The action was repeated two times resulting in a zigzag-shaped pattern. Finally, the suture was cut flush to the conjunctival surface and the cut end retracted into the subconjunctival tissue. The same procedures were repeated to fix the other two eyelets of the IOL (Figure 1). The infusion cannula was removed, and the conjunctival incision was closed via a 10-0 nylon suture.
Fig. 1.
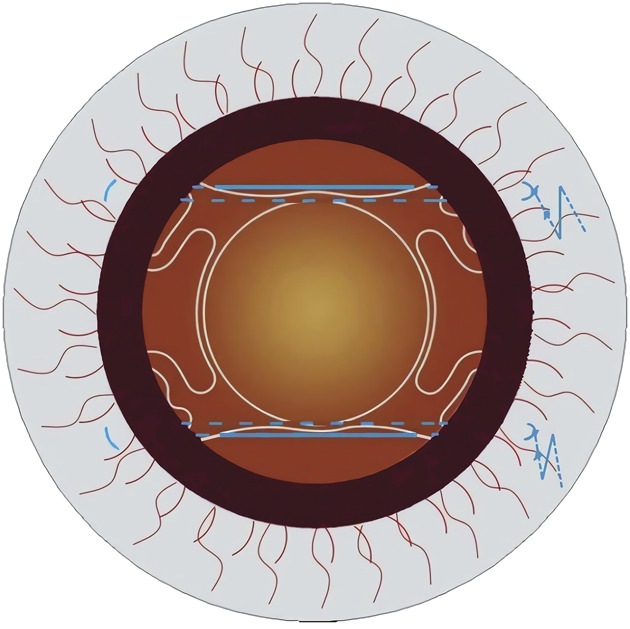
Schematic figures demonstrating four-point scleral fixation of an Akreos Adapt AO IOL using the double-suture technique at last.
The IOL used in this study is the Akreos Adapt AO (Bausch & Lomb), which is a foldable hydrophilic acrylic aspherical IOL with four closed eyelets at the distal end of the haptics and has an optic diameter of 6.0 mm, an over-length up to 10.5 mm – 11.0 mm. The optic power is calculated using the SRK/T formula to achieve emmetropia. The manufacturer's recommendation for A constant is 118.0.
Statistical Analyses
The decimal visual acuity was converted to the logarithm of the minimum angle of resolution units for the statistical analyses. The slit-lamp was used to assess IOL position. The Student's t-test was used to compare preoperative and postoperative best-corrected distance visual acuity, mean corneal endothelial cell counts, and IOP. The statistical analyses were performed using the statistical package for the Social Sciences program (SPSS 25.0 for Windows, Chicago, IL). A P value of less than 0.05 was considered to be statistically significant.
Results
This study included 15 eyes of 15 patients (1 female, 14 males). The mean age was 51 years (±SD, 17 years, range, 5–79 years). The indications for surgery included aphakia after pars plana vitrectomy with retinal detachment repair (n = 7), traumatically dislocated crystalline lens (n = 7), dislocated crystalline lens because of Marfan syndrome (n = 1). Different surgical approaches combined with transscleral fixation were performed.
The mean follow-up period was 6.9 ± 3.2 months (range 4–12.5 months). The mean preoperative corrected distance visual acuity (corrected distance visual acuity) was 0.70 ± 0.54 logarithm of the minimum angle of resolution (Snellen 20/102), and it improved to 0.29 ± 0.26 logarithm of the minimum angle of resolution (Snellen 20/39) at the final follow-up. The difference was statistically significant (P = 0.001). The mean corneal endothelial cell counts decreased from 2,256 cells/mm2 to 2,125 cells/mm2 at 1 month (P = 0.083). Compared with a mean preoperative IOP of 18.87 ± 9.02 mmHg, IOP was 13.06 ± 3.17 mmHg on postoperative Day 1 (P = 0.037), 13.33 ± 3.13 mmHg on Day 3 (P = 0.02), 15.73 ± 4.40 mmHg on Day 7 (P = 0.146), and 14.21 ± 3.04 mmHg at final follow-up (P = 0.035), respectively. In the present study, we did not observe any severe complications such as decentration or dislocation of the IOL, corneal decompensation, cystoid macular edema, iris capture, vitreous hemorrhage, retinal detachment, endophthalmitis, suprachoroidal hemorrhage, suture erosion, suture breakage, or glaucoma escalation. The IOLs were well-centered during the follow-up period.
Discussion
With the continuous development of small incision surgery, foldable IOLs have been a good selection of transscleral fixation.13 Although a small incision means fewer complications, suture breakage still attracts greater attention largely when using a scleral fixation. Several studies published in the past 20 years show the rate of suture breakage ranges from 0.47% to 27.9%.8–11 Buckley E G and Bading G et al reported that breakage of 10 to 0 polypropylene sutures may happen after 3 to 8 years when a CZ70BD PMMA IOL or a Morcher 81 L IOL is fixed with the 10-0 polypropylene sutures.11,14 Younger patients are much more active than older adults. A large number of sports may accelerate the breakage of the 10-0 polypropylene sutures that are used to fix CZ70BD PMMA IOLs, and the possibility of suture breakage is progressive over time.9 The investigators found a polypropylene suture with a diameter of 200 μm used for transscleral fixation had a crack perpendicular to the longitudinal axis of the suture, and both ends of the suture's diameter were decreased by over 50% after 6.5 years.15 Some sutureless fixation techniques are introduced to overcome suture breakage. However, some defects are still found when using this method, including haptic exposure, haptic slippage, haptic breakage, rupture of the optic–haptic junction, iris capture.16–19
The advantages are multifold in the present study. First, given that suture breakage is one of the most severe complications, the possible use of multiple sutures on each touch, different suture materials, or thicker sutures are worthy of consideration. Nine-0 polypropylene suture used as an alternative to 10-0 polypropylene in this study has 60% greater tensile strength, 50% greater diameter, and 125% greater cross-sectional area, so it is better able to resist degradation and more suitable for long-term stability.20 Double 9-0 polypropylene sutures were used to fix two of the four haptics, respectively. Therefore, the IOL may be fixed more firmly and stably. No suture breakage was found in our patients during the follow-up period. Second, the Akreos Adapt AO IOL (Bausch & Lomb) used in this study is a foldable hydrophilic acrylic aspherical IOL with four closed eyelets at the distal end of the haptics, allowing a smaller corneal incision, so the stability of the anterior chamber can be maintained during the operation, and four-point scleral fixation may reduce risks of iris capture, lens tilt, and decentration.6,7,21,22 Because Akreos Adapt AO IOL is an aspheric lens, patient will get high-quality vision that is not influenced by lens decentration or size of the pupil. Compared with hydrophobic acrylic lens, because it is a hydrophilic acrylic, it causes less inflammation.23 Third, suture erosion is also a significant issue. If the suture knot is rotated into the eye, the suture may loosen or break in the process of rotating suture knot. To avoid the suture damage, after the 2 ends of the 9-0 polypropylene suture were tied on the surface of the sclera, the suture was buried under the conjunctiva using the technique of the modification friction knot,24 but the needle was passed through the sclera for two times in this study, resulting in a zigzag-shaped pattern. The conjunctiva is opened only near the fixation points to enable the needle to pass through the sclera. This minimizes the extent of the conjunctival opening. The suture with friction knot is fixated by zigzagging it in the sclera, which produces enough friction to prevent the suture from slipping. Fourth, the useful lifetime of polypropylene sutures is associated with the suture exposure to ultraviolet light.12 The double-suture technique reduces the distance that the suture traverses under the conjunctiva, avoiding exposure to ultraviolet light. Fifth, Gore-Tex suture is also used for scleral fixation of IOLes. At present, the common method of using Gore-Tex suture is to pass through the eyelets of Akreos A0 60 IOL or CZ70BD IOL outside the eye. But the clear corneal incision is required to be enlarged to 3.5 mm when using the Akreos AO 60 IOL and a 7-mm scleral tunnel incision needs to be made when using the CZ70BD IOL.26,27 Compared with using Gore-Tex suture, the double suture technique requires only a 2.65-mm clear corneal incision, and the suture does not need to be passed through the eyelets of the IOL outside the eye in advance.
In the current study, the postoperative IOP exceeded 21 mmHg in 2 eyes, which was successfully treated with topical antiglaucoma drugs. These two eyes had glaucoma secondary to past eyeball blunt trauma before surgery. Thus, the IOP elevation in this study can be partly explained by the previous trauma, rather than the surgery itself. In aphakic eyes after combined pars plana vitrectomy and lensectomy, the incidence of retinal detachment after secondary scleral fixation of PC-IOL implantation with sutures was 15.63%.25 Our follow-up results showed no case of retinal detachment. The double-suture technique has a crucial step during the operation. The distance between the 2 punctures of the straight needle is 0.5 mm or longer on the scleral where each haptic is fixed, avoiding scleral laceration caused by the tension of the suture, which may lead to the failure of suture fixation.
In summary, four-point scleral fixation of an Akreos Adapt AO IOL using the double-suture technique combines the advantages of a PC IOL and a simple surgery technique. Our follow-up results showed no IOL decentration or dislocation, no suture-related complications were detected, such as hyphema, macular edema, and vitreous hemorrhage during the follow-up period in this study. There are limitations of the present technique. First, the method may not be suitable for other sutures described with scleral fixation, such as Gore-Tex. Second, these eyes are often already at high risk of retinal detachment, future surgeries that requires use of air, gas, or oil tamponades can lead to the hydrophilic Akreos Adapt AO lens opacification.28,29 Air tamponade was performed in one eye in this article and lens opacification has not been found. Intraocular lens opacification will be of continued concern during later follow-up periods. Third, the follow-up time in our study is quite short, if the suture did break in one of those two loops, the loop would likely loosen over time and the IOL dislocated. A study with a longer follow-up time and more cases is required to better assess the long-term stability of this method.
Supplementary Material
Footnotes
Supported by National Natural Science Foundation of China (82101164). Natural Science Foundation of Shandong Province.China (ZR2021MH074, ZR2021MH152). Medicine and Health Science Technology Development Project of Shandong Province, China (202007021313).
None of the authors has any conflicting interests to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.retinajournal.com).
All data are available from the corresponding author upon request.
Contributor Information
Shijiu Chen, Email: chenshijiu749@126.com.
Gongqiang Yuan, Email: yuangongqiangygq@sina.com.
Wenting Zhu, Email: zhuwenhuatt@163.com.
Qian Wang, Email: 1936757294@qq.com.
Weiyun Shi, Email: weiyunshi@163.com.
References
- 1.Snyder ME, Perez MA. Tiltless and centration adjustable scleralsutured posterior chamber intraocular lens. J Cataract Refractive Surg 2014;40:1579–1583. [DOI] [PubMed] [Google Scholar]
- 2.Jürgens I, Rey A. Simple technique to treat pupillary capture after transscleral fixation of intraocular lens. J Cataract Refractive Surg 2015;41:14–17. [DOI] [PubMed] [Google Scholar]
- 3.McGrath LA, Lee GA. Transscleral fixation of a supplementary toric intraocular lens to prevent rotation in a pseudophakic patient. J Cataract Refractive Surg 2013;39:134–138. [DOI] [PubMed] [Google Scholar]
- 4.Hu BV, Shin DH, Gibbs KA, et al. Implantation of posterior chamber lens in the absence of capsular and zonular support. Archives Ophthalmol 1988;106:416–420. [DOI] [PubMed] [Google Scholar]
- 5.Nagamoto S, Kohzuka T, Nagamoto T, et al. Pupillary block after pupillary capture of an AcrySof intraocular lens. J Cataract Refractive Surg 1998;24:1271–1274. [DOI] [PubMed] [Google Scholar]
- 6.Chen S, Yuan G, Zhu W, et al. 8-0 polypropylene suture looping and overhand knot: transconjunctival approach to four-point scleral fixation of an akreos adapt intraocular lens. Retina 2020. doi: 10.1097/IAE.0000000000002873. [DOI] [PubMed] [Google Scholar]
- 7.Zhang J, Tian J, Sun X, et al. Closed continuous-loop suture: a novel surgical technique for transscleral fixation of intraocular lenses. Retina 2019. doi: 10.1097/IAE.0000000000002644. [DOI] [PubMed] [Google Scholar]
- 8.Lockington D, Ali NQ, Al-Taie R, et al. Outcomes of scleral-sutured conventional and aniridia intraocular lens implantation performed in a university hospital setting. J Cataract Refractive Surg 2014;40:609–617. [DOI] [PubMed] [Google Scholar]
- 9.Vote BJ, Tranos P, Bunce C, et al. Long-term outcome of combined pars plana vitrectomy and scleral fixated sutured posterior chamber intraocular lens implantation. Am J Ophthalmol 2006;141:308–312. [DOI] [PubMed] [Google Scholar]
- 10.Kokame GT, Yanagihara RT, Shantha JG, et al. Long term outcome of pars plana vitrectomy and sutured scleral-fixated posterior chamber intraocular lens implantation or repositioning. Am J Ophthalmol 2018;189:10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bading G, Hillenkamp J, Sachs HG, et al. Long-term safety and functional outcome of combined pars plana vitrectomy and scleral-fixated sutured posterior chamber lens implantation. Am J Ophthalmol 2007;144:371–377. [DOI] [PubMed] [Google Scholar]
- 12.Mowbray SL, Chang SH, Casella JF, et al. Estimation of the useful lifetime of polypropylene fiber in the anterior chamber. J Am Intraocular Implant Soc 1983;9:143–147. [DOI] [PubMed] [Google Scholar]
- 13.Kaynak S, Ozbek Z, Pasa E, et al. Transscleral fixation of foldable intraocular lenses. J Cataract Refractive Surg 2004;30:854–857. [DOI] [PubMed] [Google Scholar]
- 14.Buckley EG. Safety of transscleral-sutured intraocular lenses in children. J Am Assoc Pediatr Ophthalmol Strabismus 2008;12:431–439. [DOI] [PubMed] [Google Scholar]
- 15.Jongebloed WL, Worst JFG. Degradation of polypropylene in the human eye: a SEM-study. Documenta Ophthalmologica 1986;64:143–152. [DOI] [PubMed] [Google Scholar]
- 16.Tanaka H, Fujinami K, Watanabe K, et al. Haptic breakage after transscleral fixation of a single-piece acrylic intraocular lens. Case Rep Ophthalmol 2014;5:212–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Matsui Y, Matsubara H, Hanemoto T, et al. Exposure of haptic of posterior chamber intraocular lens after sutureless intrascleral fixation. Bmc Ophthalmol 2015;15:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yamane S, Sato S, Maruyama-Inoue M, et al. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology 2017;124:1136. [DOI] [PubMed] [Google Scholar]
- 19.Agarwal A, Kumar DA, Jacob S, et al. Fibrin glue–assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refractive Surg 2008;34:1433–1438. [DOI] [PubMed] [Google Scholar]
- 20.Price MO, Price FW, Jr, Werner L, et al. Late dislocation of scleral-sutured posterior chamber intraocular lenses. J Cataract Refractive Surg 2005;31:1320–1326. [DOI] [PubMed] [Google Scholar]
- 21.Stem MS, Todorich B, Woodward MA, et al. Scleral-fixated intraocular lenses: past and present. J Vitreoretinal Dis 2017;1:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.John T, Tighe S, Hashem O, et al. New use of 8-0 polypropylene suture for four-point scleral fixation of secondary intraocular lenses. J Cataract Refractive Surg 2018;44:1421–1425. [DOI] [PubMed] [Google Scholar]
- 23.Abela-Formanek C, Amon M, Schauersberger J, et al. Results of hydrophilic acrylic, hydrophobic acrylic, and silicone intraocular lenses in uveitic eyes with cataract: comparison to a control group. J Cataract Refractive Surg 2002;28:1141–1152. [DOI] [PubMed] [Google Scholar]
- 24.Oskala P. Friction knot to fixate scleral sutures. J Cataract Refractive Surg 2015;41:497–500. [DOI] [PubMed] [Google Scholar]
- 25.Obeng FK, Vig VK, Singh P, et al. Posterior chamber scleral fixation of intraocular lenses in post-vitrectomised aphakic eyes. J Clin Diagn Res 2017;11:NC09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khan MA, Gupta OP, Smith RG, et al. Scleral fixation of intraocular lenses using Gore-tex suture: clinical outcomes and safety profile. Br J Ophthalmol 2016;100:638–643. [DOI] [PubMed] [Google Scholar]
- 27.Khan MA, Samara WA, Gerstenblith AT, et al. Combined pars plana vitrectomy and scleral fixation of an intraocular lens using Gore-TX suture: one-year outcomes. Retina 2018;38:1377–1384. [DOI] [PubMed] [Google Scholar]
- 28.Cao D, Zhang H, Yang C, et al. Akreos adapt AO Intraocular lens opacification after vitrectomy in a diabetic patient: a case report and review of the literature. BMC Ophthalmol 2016;16:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rubin U, Baker CF. Akreos lens opacification under silicone oil. Can J Ophthalmol J Canadien D'ophtalmol 2018;53:e188–e190. [DOI] [PubMed] [Google Scholar]


