Supplemental Digital Content is Available in the Text.
We describe an electrocoagulation fixation technique for one-piece intraocular lens (IOL) scleral flapless fixation with sutures without knots with minimal intraocular manipulations and microcorneal incisions. This technique does not need to replace the implanted one-piece IOL previously, thus greatly reducing secondary trauma caused by IOL replacement.
Key words: electrocoagulation fixation technique, one-piece intraocular lens, scleral flapless fixation, sutures without knots, polypropylene suture
Abstract
Purpose:
To present an electrocoagulation fixation technique for one-piece intraocular lens (IOL) scleral flapless fixation with sutures without knots.
Methods:
First of all, after repeated tests and comparisons, we chose 8-0 polypropylene suture as the material for electrocoagulation fixation of one-piece IOL haptics because of its proper elasticity and size. A transscleral tunnel puncture at the pars plana was performed using an arc-shaped needle with 8-0 polypropylene suture. The suture was subsequently guided out of the corneal incision by a 1-mL syringe needle and then guided by the needle into the inferior haptics of the IOL. The suture was cut off and heated into a shape of a probe with a spherical tip using a monopolar coagulation device to prevent slippage from the haptics.
Results:
In the end, 10 eyes underwent our new surgical procedures, and the average operation time was 42.5 ± 12.4 minutes. At the 6-month follow-up, seven of 10 eyes achieved significant vision improvement and nine of 10 kept the implanted one-piece IOL stable in the ciliary sulcus. No serious intraoperative/postoperative complications were observed.
Conclusion:
The electrocoagulation fixation was a safe and effective alternative technique for previously implanted one-piece IOL scleral flapless fixation with sutures without knots.
The methods of intraocular lens (IOL) scleral fixation can be divided into many types according to the presence or absence of sutures and scleral flaps.1–4 At the same time, the implanted IOL can be classified into one-piece, three-piece, and four fenestrated haptics IOLs2 according to their characteristics. Conventional wisdom holds that the three-piece and four-loop IOLs have better stability and are, therefore, more suitable for scleral fixation. However, both types of IOLs are usually secured to the sclera with 10-0 nonabsorbable polypropylene sutures. As a result, IOL subluxation increases over time because of the very thin suture erosion or loosening. Therefore, we need to choose thicker polypropylene sutures to overcome this long-term complication.
Conversely, with the advancement of IOL manufacturing technology, one-piece IOL gradually replaces three-piece IOL. Consequently, most of the patients with IOL subluxation had previously had a one-piece IOL implanted. Therefore, it is necessary to explore a new technique for one-piece IOL scleral fixation, which can not only ensure the stability of the IOL but also overcome the long-term complications associated with a 10-0 suture. This article introduces a new technique for IOL scleral fixation with a one-piece IOL plus polypropylene nonabsorbable 8-0/7-0 sutures and investigates its efficacy and safety.
Methods
Selection of needles and sutures (Figure 1).
1. The 10-0 polypropylene suture is too thin, and if it is knotted on the one-piece IOL haptics, it is easy to slip off; in addition, if the end of the 10-0 polypropylene suture is ironed into a ball, it will also slip off due to insufficient swelling (1A). From the perspective of long-term effects, also because the 10-0 polypropylene suture is too thin, the suture will loosen or even erode at the fixed end of the sclera, which may easily lead to subluxation of the IOL.5,6
2. The 8-0 polypropylene suture has strong tensile strength. However, because it is relatively thick, it is not suitable for knots to be fixed on the haptics. Excessive knots can irritate the ciliary body or cause knot-related complications such as infection. Fortunately, the 8-0 polypropylene suture is most suitable for electrocoagulation fixation to the haptics of a one-piece IOL (1B).
3. The 7-0 polypropylene suture is also suitable for electrocautery fixation to the one-piece IOL haptics, but it is less compliant than the 8-0 polypropylene suture, so there is a risk of IOL subluxation, especially in highly myopic eyes.
4. The biggest disadvantage of the 6-0 polypropylene suture is that because of its relatively large needle, the haptics of the one-piece IOL will be damaged when the needle is passed through, so it is not suitable for the electrocoagulation fixation method proposed in this article (1C).
5. The composite structure of a single one-piece IOL and two 8-0 polypropylene sutures has enough tensile strength and can bear at least 30 g of weight (1D).
Fig. 1.
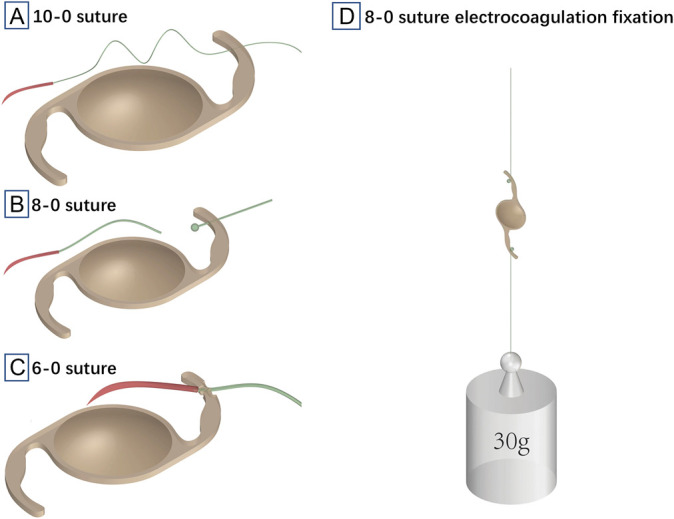
Selection of needles and sutures vs. the electrocoagulation fixation technique. A, The 10-0 polypropylene suture is too thin to be firmly fixed on one-piece IOL loop, and the broken end of it will slip off because of insufficient swelling. B, The 8-0 polypropylene suture has strong tensile strength, and its broken end is most suitable for electrocoagulation fixation to the haptics of one-piece IOL. C, The 6-0 suture and its needle are relatively large, which is easy to cause damage to the loop of one-piece IOL. D, The weight of 30 g can still not damage the composite structure of a single one-piece IOL and two 8-0 polypropylene sutures.
Surgical Procedures
All surgeries were performed under retrobulbar anesthesia by one of us (Z.J.) (see Video, Supplemental Digital Content 1, http://links.lww.com/IAE/B925, which demonstrates surgical procedures). A 3-mm incision was made at the 10 o'clock position of the clear cornea. The anterior chamber was filled with viscoelastic substances. A foldable one-piece IOL was implanted into the anterior chamber through the 3-mm incision. The bulbar conjunctival flaps were made at the 12 o'clock and six o'clock positions of the limbus. A transscleral tunnel puncture at the six o'clock position of the pars plana between 1.5 mm and 2 mm behind the corneal limbus was performed with an arc-shaped needle with an 8-0 polypropylene suture at the tail. The arc-shaped needle was guided out of the corneal incision by a 1-mL syringe needle, and then, the polypropylene suture was guided by the needle into the inferior haptics of the IOL. The arc-shaped needle was cut off, and then, the suture end was scalded into the shape of a ball with the monopolar coagulation device to prevent slippage from the haptics. The second transscleral tunnel puncture at the 12 o'clock position of the pars plana was performed with another arc-shaped needle with the polypropylene suture. The second suture was secured into the upper haptics of the IOL using the same method described above. The one-piece IOL was relocated to the posterior chamber. Finally, the suture ends outside the sclera were also ironed into the shape of a ball and buried in the sclera. The bulbar conjunctival flaps were sutured.
Results
The electrocoagulation fixation technique was used in 10 eyes with the follow-up time of at least 6 months. At the 6-month follow-up, most of them (7/10) achieved significant improvement of uncorrected distance visual acuity. The average operation time was 42.5 ± 12.4 minutes. A majority of the implanted one-piece IOL (9/10) remained stable in the ciliary sulcus during the half-year follow-up. Demographics and clinical data of eyes undergoing electrocoagulation fixation were listed in Table 1. Of the 10 eyes, only one case was found to have vitreous incarceration in the pupil area 1 day after surgery and temporal displacement of the IOL due to vitreous traction in the pupil area 1 month after surgery. In addition, there was another case of transient intraocular hypertension and another case of postoperative vitreous hemorrhage. Within half a year of the new technique application, no severe intraoperative/postoperative complications such as suture slippage, suture breakage, persistent intraocular pressure fluctuations, persistent postoperative inflammation, or infective endophthalmitis were observed in any of the operated eyes.
Table 1.
Demographics and Clinical Data of Eyes Undergoing Electrocoagulation Fixation
| Case | Sex | Age, years | Eye | Etiology of Zonular Defect | Snellen BCVA | Refraction (DS/DC*axis) | ||
| Preop | Postop Day 1 | Preop | Postop Day 1 | |||||
| 1 | M | 52 | L | Iatrogenic | HM | 20/400 | — | −0.75/-0.75*10° |
| 2 | M | 52 | R | Iatrogenic | 20/2000 | 20/400 | — | +0.75/-2.75*170° |
| 3 | F | 46 | L | IOL dislocation | 20/25 | 20/20 | +13.25/-0.75*140° | −0.5*138° |
| 4 | F | 46 | R | IOL subluxation | 20/30 | 20/40 | −2.25*120° | +2.0/-0.75*45° |
| 5 | F | 63 | L | Iatrogenic | 20/50 | 20/40 | +12.50/-0.5*90° | −1.75*115° |
| 6 | M | 57 | L | Trauma | HM | 20/50 | — | −1.5/-1.25*15° |
| 7 | M | 57 | L | Trauma | 20/50 | 20/30 | −0.5/-2.0*30° | −3.0*15° |
| 8 | M | 70 | R | IOL subluxation | 20/25 | 20/40 | +1.75 | −0.5*160° |
| 9 | M | 51 | R | Trauma | 20/60 | 20/40 | +12.5/-1.7*135° | +2.0/-0.5*180° |
| 10 | M | 71 | L | Trauma | 20/60 | 20/60 | +10.25/-2.75*15° | −1.5*180° |
BCVA, best-corrected visual acuity; DS, diopter of sphere; DC, diopter of cylinder; R, right; L, left; preop, preoperative; postop, postoperative.
Discussion
At present, there are many technical methods for scleral fixation of three-piece and four fenestrated haptics IOLs when these IOLs cannot be implanted into the bag.1–5 But there is no effective and safe scleral fixation technique for one-piece IOL. Because the loop of one-piece IOL is relatively soft, traditional knotting methods cannot fix it well. Improper combination of one-piece IOL and sutures may lead to breakage of the one-piece IOL loop or subluxation or rotation of the IOL.
To overcome the above shortcomings, we introduced electrocoagulation fixation technique of one-piece IOL for the first time. The new technique described in this article has significant advantages such as no scleral flaps, no knots, and no need to replace the IOL, so the operation time is greatly shortened. Specifically, the electrocoagulation fixation technique eliminates noninfectious and infectious inflammation related to scleral flaps and suture knots and eliminates subluxation of IOL caused by erosion or breakage of too thin suture. If the patient was previously implanted with a one-piece IOL, the new technique does not need to replace it with a three-piece IOL, which reduces the surgical injuries caused by IOL replacement, saves the operation duration, and has the similar surgical efficacy and safety to traditional three-piece IOL scleral fixation with a polypropylene nonabsorbable 10-0 suture.
If it is a long time from dislocation onset to the previous implantation of in-the-bag one-piece IOL, the capsule may have been organized, resulting in tight adhesion between the capsule and the IOL, and even the haptics of the IOL cannot be naturally unfolded due to the contraction of the capsule. In this situation, it is recommended to use the capsule fixation method introduced by Professor Haiying Jin et al.7,8 Or some patients have already implanted the bag tension ring in the previous operation, so we only need to fix the tension ring and do not need to use our technique.
Of course, in the other two scenarios, our new technique could be used to deal with IOL bag complex dislocation: (1) The time from cataract surgery is short and the bag is relatively fresh, so that the PCIOL could be dissociated; (2) the anterior vitrectomy technique or cutting open the bag enables the haptics of the IOL to unfold smoothly. There are two treatment methods according to subluxation or total dislocation of IOL bag complex. (1) Subluxation: The remaining bag with intact suspension ligament was retained as the support. After the haptics of IOL was dissociated, one haptics of one-piece IOL was implanted in front of the sulcus. The other haptics was fixed at the ciliary sulcus in the contralateral bag-free area by electrocautery we proposed, so that only one haptics needed to be fixed, simplifying the surgical procedures. (2) Total dislocation: It is further divided into forward dislocation and backward dislocation. (A) Forward dislocation: After anterior vitrectomy, viscoelastic agents were used to maintain the surgical space, the capsule was cut open, and, then, the haptics of IOL was naturally unfolded and fixed; (B) backward dislocation: After posterior vitrectomy, the IOL bag complex was floated in the anterior chamber with the help of heavy water and the above procedures were performed.
Conclusions
The electrocoagulation fixation technique for one-piece IOL scleral flapless fixation with sutures without knots reduces the surgical injuries, saves the operation duration, and has ideal surgical efficacy and safety. It was a safe and effective alternative technique for previously implanted one-piece IOL. Of course, we need more cases and enough time to further verify the security of this new technique.
Supplementary Material
Footnotes
None of the authors has any financial/conflicting interests to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.retinajournal.com).
Both authors contributed equally.
References
- 1.Karadag R, Celik HU, Bayramlar H, Rapuano CJ. Sutureless intrascleral fixated intraocular lens implantation. J Refract Surg 2016;32:586–597. [DOI] [PubMed] [Google Scholar]
- 2.Zhang Y, Zheng J, Liu J. Intraocular suture technique for flapless two-point fixation of four fenestrated haptics intraocular lenses. Retina 2021. doi: 10.1097/IAE.0000000000003400. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 3.Szurman P, Petermeier K, Aisenbrey S, et al. Z-suture: a new knotless technique for transscleral suture fixation of intraocular implants. Br J Ophthalmol 2010;94:167–169. [DOI] [PubMed] [Google Scholar]
- 4.Dinç E, Vatansever M, Dursun Ö, et al. Scleral fixated intraocular lens implantation with a modified Z-suture technique. Int Ophthalmol 2018;38:2357–2361. [DOI] [PubMed] [Google Scholar]
- 5.John T, Tighe S, Hashem O, Sheha H. New use of 8-0 polypropylene suture for four-point scleral fixation of secondary intraocular lenses. J Cataract Refract Surg 2018;44:1421–1425. [DOI] [PubMed] [Google Scholar]
- 6.Mo B, Li SF. Novel use of an adjustable single 8-0 polypropylene suture of scleral fixation without conjunctival dissection. BMC Ophthalmol 2020;20:304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ou Z, Zhao P, Zhang Q, Jin H. Intrascleral fixation of implantable polypropylene capsular hook(s): a sutureless technique to fixate the capsular bag for intraocular lens implantation in subluxated lenses. Retina 2019;39;S33–S38. [DOI] [PubMed] [Google Scholar]
- 8.Jin H, Zhang Q, Zhao P, Lyv J. Intrascleral fixation of implantable polypropylene capsular hook(s) to reconstruct capsular support for out-of-the-bag intraocular lens fixation in vitrectomized eyes. Retina 2022;42:1816–1821. [DOI] [PubMed] [Google Scholar]


