Abstract
Background:
Although the selected pedicle is important in how it maintains nipple viability and is of equal importance, it can be utilized with the remaining breast tissue to reshape the breast mound. It is ideally used as an extended pedicle, as it allows us to use the tissue in the lower pole of the breast. The purpose of this article was to evaluate additional indications and outcomes using the extended superior pedicle approach along with conventional techniques.
Methods:
This is a retrospective study over 5 years of using an extended superior dermoglandular pedicle approach for managing a variety of breast deformities. Postoperative complications, along with patient and surgeon satisfaction, were assessed.
Results:
All 68 patients expressed that the results were either excellent (85.3%) or very good (14.7%) according to the evaluation parameters. Among the 68 patients, there were 62 very good outcomes (91.2%) and six good outcomes (8.8%) according to surgeon evaluation. Only one reduction experienced a superficial partial loss, which was improved with no intervention. There was minor asymmetry in three patients (4.4%), which was not experienced by the patients, and poor scar quality in one dark-skinned patent.
Conclusions:
The author was able to expand the utility of extended superior pedicle for various breast deformities, such as reduction mammoplasty; mastopexy; augmentation mastopexy, either autoaugmentation or prosthetic; tuberous breast; after lumpectomy resection; and even in secondary breast deformities with reproducible and reliable outcomes across a wide patient population.
Takeaways
Question: Does the extended superior pedicle maintain nipple viability, and it can be used with the remaining breast tissue to reshape the breast mound in a variety of breast deformities?
Findings: We can expand the utility of the extended superior pedicle for various breast deformities, such as reduction mammoplasty; mastopexy; augmentation mastopexy, either autoaugmentation or prosthetic; tuberous breast; after lumpectomy resection; and even in secondary breast conditions with reproducible and consistent results.
Meaning: The superior pedicle is ideal to be used as an extended pedicle, as it allows use of the tissue in the lower pole of the breast.
INTRODUCTION
The objectives of breast surgery are to create a smaller, more youthful, aesthetically pleasing breast, correct breast ptosis, restore upper pole fullness, redefine the lateral border of the breast, and reshape the parenchyma into a more youthful contour. Numerous options exist to mobilize the nipple-areola complex (NAC) during breast reduction and mastopexy techniques.1 The superior pedicle is one such option, described by Weiner et al in 1973, which has gained popularity.2 Since its original description in 1957 by Arie,3 several modifications have been made. These modifications allow for its use in a wide variety of breast problems ranging from involutional atrophy and ptosis to major hypertrophies, and even in some congenital and oncological breast conditions. In addition, the superior pedicle seems more logical to use because it relocates tissues to their original position and allows easier secondary surgery in the case of recurrent ptosis and excess volume.4
Researchers agreed that the main sources of blood supply to the breast are the internal thoracic, lateral thoracic, anterior intercostal, and acromiothoracic (thoracoacromial) arteries.5 All these arteries come almost entirely from the cephalic part of the breast. Therefore, the superior pedicle appears to be the safest and the most reliable pedicle for nipple and areola mobilization.
Although the selected pedicle is important in how it maintains nipple viability and is of equal importance, it can be used with the remaining breast tissue to reshape the breast mound. In some situations, additional parenchyma is required in remote parts of the breast not appropriately filled with the pedicle and remaining breast tissue.
The use of local flaps and autoaugmentation techniques has subsequently become a popular option to rotate tissue into areas of volume emptiness. These can be taken either from within the breast mound or locally.6–10
Traditional breast reduction and mastopexy techniques using superiorly based pedicles, whether superior or superomedial, have excess dermoglandular tissue resected from the lower pole. This tissue is subsequently very amenable to being used as a vascularized extension of the NAC pedicle design for a variety of breast conditions. The use of this lower pole breast tissue as a weaving technique through the pectoralis muscles to autoaugment the breast mound in mastopexy techniques has been initially described.11
The superior pedicle is ideal for an extension-type pedicle because the removal of tissue in the lower pole is often desired to allow for a new cephalad inframammary crease, plication of the medial and lateral pillars, and breast shaping with the benefits of a vertical mammoplasty technique.4
By extended superior pedicle, parenchymatous tissue that is often abundant in the lower pole and can subsequently be rotated on a well-vascularized pedicle to the central breast and upper pole areas where volume is required.
The purpose of this article was to evaluate additional indications and outcomes using the extended superior pedicle approach along with traditional reduction and mastopexy techniques. In contrast to previously described techniques, the pedicle includes parenchyma adjacent to the inframammary crease, which facilitates the narrowing of the breast base and the raising of the inframammary crease.
PATIENTS AND METHODS
This is a retrospective study over 5 years of using an extended superior dermoglandular pedicle approach for managing a variety of breast deformities. The number of surgical procedures is listed in Table 1.
Table 1.
Number of Surgical Procedures Performed Over a Period of 5 Years
| Surgical Procedure Description | No. Procedures | |
|---|---|---|
| Bilateral | Unilateral | |
| Breast reduction | 26 | |
| Mastopexy with autoaugmentation | 30 | |
| Augmentation mastopexy with submammary implants | 6 | 4 |
| Augmentation mastopexy with submuscular implants | 6 | 4 |
| Tuberous breast | 4 | |
| Oncoplastic breast conservation surgery | 8 | 15 |
| Secondary mastopexy after previous reductions | 8 | |
| Secondary augmentation mastopexy after explantation | 2 | |
Patient satisfaction with the aesthetic outcome was assessed as excellent, very good, good, and poor on a questionnaire including these parameters: shape, symmetry, ptosis correction, upper pole fullness, NAC position, and sensibility and quality of scars.
Three independent plastic surgeons were involved in the evaluation of the postoperative front, oblique, and profile photographs at 3 months. The grading was from 1 to 4 (1: poor, 2: good, 3: very good, 4: excellent) in terms of the shape of the breast, symmetry, volume, projection, ptosis, NAC position, upper pole fullness, and scar quality. The complication rate of all procedures was assessed. Informed medical photography consent was obtained from all 68 patients.
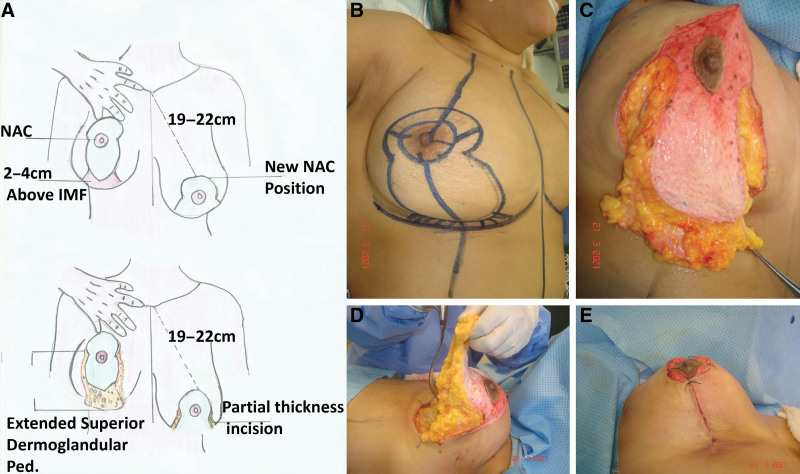
SURGICAL TECHNIQUE: PREOPERATIVE MARKING
With the patient in standing position, the preoperative markings for an extended superior pedicle are basically the same as for a regular superior pedicle mastopexy or reduction. The vertical midline of the chest, the breast meridian, and the transposition of the inframammary crease into the anterior surface of the breast, denoting the new position of the NAC were marked. Based on experience, we allowed the new nipple position around 1–2 cm inferior to the transposed inframammary crease to compensate for ptosis and the weight of the breast in an upright position. The areola with a 5-cm diameter was centered on this point. The standard Wise pattern was drawn around the areola with its vertical limbs marked by displacement of the mound medially and laterally to be tapered inferiorly to meet at the meridian of the breast 2–4 cm above the position of the original inframammary crease. The width between the vertical limbs (and therefore the width of the dermal portion of the extended dermoglandular pedicle) was determined by the amount of skin that could be excised and closed without tension. This width and the position of the NAC had been verified.
SURGICAL TECHNIQUE: DEVELOPMENT OF THE EXTENDED SUPERIOR PEDICLE
De-epithelialization was made from the existing areola to the perimeter of the new areola and the area between the vertical limbs. [See Video 1 (online) which displays the preoperative photograph, drawing, and de-epithelialization.]
Video 1. This video demonstrates the preoperative photo, drawing, and de-epithelialization.
Full-thickness incisions were carried out in the vertical limbs down to the pectoralis fascia through the breast parenchyma, thereby creating the beginning of the superiorly based dermoglandular pedicle. The remaining breast parenchyma on either side of these incisions became the medial and lateral pillars.
The extended portion of the dermoglandular flap comprised a wider amount of breast parenchyma extending to the inframammary fold (IMF) medially and laterally. By elevating this glandular portion of the flap immediately deep to the dermis, the original inframammary crease was obliterated. The caudal border of the vertical pillars created earlier became the inferior extent of the glandular tissue, thereby constituting the new, elevated IMF (Fig. 1) The superior-based dermoglandular pedicle was then elevated off the pectoralis fascia then, in the same prepectoral plane, a small pocket was created subjacent to the NAC. [See Video 2 (online), which displays the dissection and elevation of the extended superior pedicle starting from the IMF.]
Fig. 1.
Diagram showing establishment of extended superior dermoglandular pedicle. A, Drawing, elevation and dissection of the extended superior pedicle starting from the IMF over the pectoral fascia. B, Drawing. C, Elevation of the extended portion from the inframammary area. D, Dissection of the extended pedicle from the pectoral fascia until just above the level of the nipple leaving the medial and lateral pillars. E, Shape of the breast after folding the extended portion 180 degrees over itself in the prepectoral pocket in cases of autoaugmentation mastopexy.
Video 2. This video demonstrates the dissection and elevation of the extended superior pedicle starting from the inframammary fold (IMF).
SURGICAL TECHNIQUE: SPECIAL PROCEDURES ACCORDING TO THE DIFFERENT DEFORMITIES WHERE THIS APPROACH CAN BE USED
Mastopexy with Autoaugmentation
The NAC was then provisionally fixed into position along its superior border, and the extended portion of the flap was rotated 180 degrees into the newly created pocket. Once in position, the areola was closed, and the dermal portion of the flap was then secured to the pectoralis fascia. This point of fixation is critical, as if it is too high, it causes downward traction over the NAC, and if it is too low, it causes bottoming out of the breast mound. A distance of 6–7 cm from the bottom edge of the areola to the caudal edge of the folded flap is maintained.
This glandular rearrangement maximized central mound projection without the use of an implant where enough glandular tissue was available. Approximation of the medial and lateral pillars with the inferior margin of the pillars became the new inframammary crease (Fig. 1).
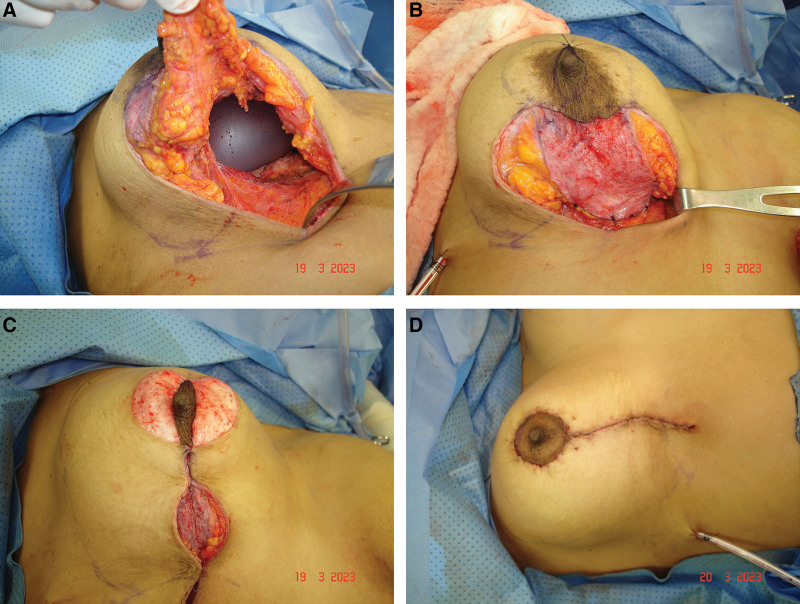
Augmentation Mastopexy with Submuscular or Submammary Implant
The dissection of the extended flap here was limited for the exposure of the pectoralis major muscle fibers. With its costal and inferior sternal origins, the submuscular pocket was dissected. The costal and lower sternal origins were released with the preservation of a lateral border strip. This strip will provide inferolateral support for the implant as a muscular sling. The upward muscular retraction results in an area that lacks the pectoralis layer over the lower pole of the implant. Then, the implant was inserted into the pocket. The implant pocket was completely sealed by suturing the extension part of the superior pedicle flap to the lateral muscle strip and the inferomedial caudal edge of the pectoralis fascia; then, the approximation of the medial and lateral pillars was performed as a second layer (Fig. 2). In cases of submammary implants, the dissection of vertical limbs was limited to full thickness in the lower portion and partial thickness in the upper portion followed by dissection of the submammary pocket. After insertion of the implant, the caudal edge of the extended flap was secured to the new inframammary crease to cover the lower pole of the implant fold, followed by closure of the pillars as a second layer.
Fig. 2.
A case of augmentation mastopexy with a submuscular implant. A–B, The implant pocket was completely sealed by suturing the extension part of the superior pedicle flap to the lateral muscle strip and the inferomedial caudal edge of the pectoralis fascia. C–D, The approximation of the medial and lateral pillars was performed as a second layer.
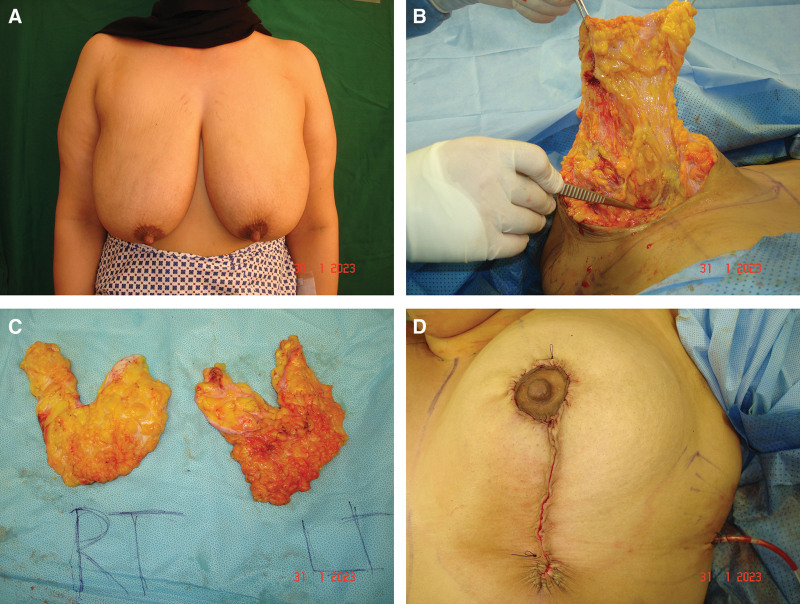
Reduction Mastopexy
Resection of the parenchyma was performed on both sides of the flap, on the edges of the pillars extending upward to the level of the areola and some extent from the lower pole of the flap. Therefore, the reduction will be inferior in a U-shaped manner. The dermal portion of the flap was then secured to the pectoralis fascia at the level of the NAC (reduction will be lateral with augmentation centrally) with a distance of 6–7 cm from the bottom edge of the areola to the caudal edge of the folded flap also maintained (Fig. 3). [See Video 3 (online), which displays the U-shaped reduction and areola fixation to its new position.] [See Video 4 (online), which displays the folding 180 degrees of the pedicle and its fixation to the pectoral fascia with the reconstruction of the pillars.]
Fig. 3.
Utility of extended superior pedicle in reduction mastopexy. A, A 40-year-old female patient with hypertrophied ptotic breasts. B, Dissection of the extended superior pedicle. C, U-shaped reduction preserving the central part of pedicle extension and the lateral pillars. D, Closure of the pillars after flap inset.
Video 3. This video demonstrates U-shaped reduction and areola fixation to its new position.
Video 4. This video demonstrates folding 180°of the pedicle and its fixation to the pectoral fascia with the reconstruction of the pillars.
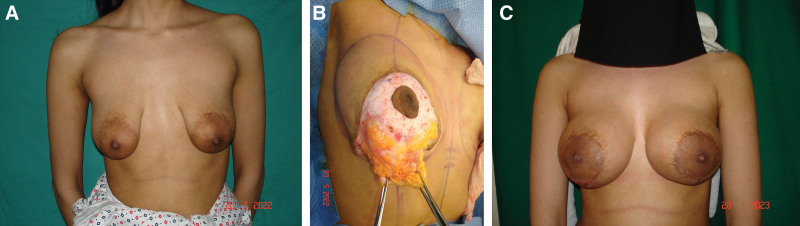
Tuberous Breast Deformity
The dissection of the pedicle was extended to the new IMF over the muscle fascia, followed by dissection of the submammary pocket. Two lateral cuts (incomplete from the under surface) were performed inferiorly at the sites of the pillars to release the constriction followed by insertion of the implant. In severe cases, no sutures either in the flap or in the pillars were left to drape over the lower pole of the implant (Fig. 4).
Fig. 4.
A case of tuberous breast. A, Preoperative; B, Intraoperative; C, Around 8 months postoperative. No sutures either in the flap or in the pillars; all these were left to drape over the lower pole of the implant.
Oncoplastic Breast Conservation Surgery (after Lumpectomy)
The therapeutic mammoplasty with extended superior pedicle reduction/mastopexy pattern is a versatile oncoplastic technique that allows breast tissue rearrangement for various tumor locations, except in the upper pole. This technique will depend on factors such as breast size, ptosis, and tumor size and location.
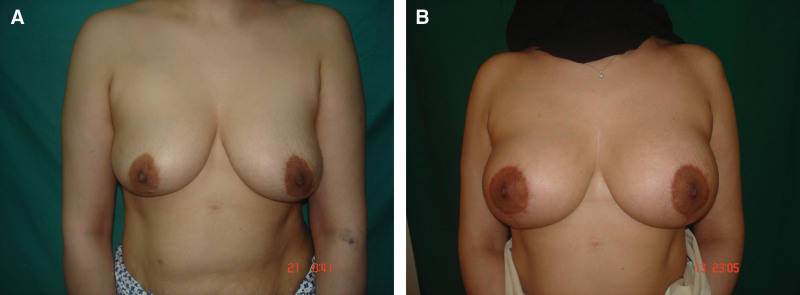
After resection of the lump, the extended part of the pedicle will fill the defect either directly or in an indirect way (Fig. 5). [See figure, Supplemental Digital Content 1, which displays (A and B) a 33-year-old female patient with hypertrophied breast and grade 111 ptosis. (C and D) Around 1 year postreduction mastopexy using the extended superior pedicle. A well-contoured elevated breast with upper pole fullness had been revealed, http://links.lww.com/PRSGO/C886.] [See figure, Supplemental Digital Content 2, which displays (A and B) 45-year-old female patient with grade 111 ptosis. (C and D) Around 1 month postmastopexy using extended superior pedicle technique showing narrow breast with upper pole fullness, http://links.lww.com/PRSGO/C887.]
Fig. 5.
Utility of extended superior pedicle after lumpectomy. A, Case of left-sided huge fibroadenoma. B, The therapeutic mammoplasty with an extended superior pedicle mastopexy pattern was used. C, More than 1 year after resection and correction of the defect without any implant.
SECONDARY MASTOPEXY AFTER PREVIOUS REDUCTIONS
These patients have bottoming out and breast ptosis, and their correction is the same as either augmentation mastopexy or autoaugmentation (Fig. 6). The de-epithelialization and elevation of the extended superior pedicle NAC flap but maintaining the blood supply not on a new “pedicle” but on a random pattern blood supply.12 Some studies suggest that the NAC can survive even after having previously been circumferentially incised, due to revascularization across the scar tissue.13,14 The dissection should be limited to full thickness in the caudal part of the flap and partial thickness in the cephalic part with a narrow tunnel in the central part to maximize flap perfusion. This maximizes the central mound simultaneously by narrowing the base.
Fig. 6.
Utility of extended superior pedicle in secondary augmentation mastopexy after previous reduction. A, Case of secondary deformities after the previous reduction. B, Six months postcorrection using extended superior pedicle with prosthetic augmentation.
SECONDARY AUGMENTATION MASTOPEXY AFTER EXPLANTATION
After the designation of the extended superior pedicle, explantation of the implants and capsulectomy were performed. Dissection of the submuscular pocket followed by insertion of the new implants. The implant pocket was completely sealed by suturing the extension of the superior pedicle flap to the lateral muscle strip and the inferomedial caudal edge of the pectoralis fascia; then, the approximation of the medial and lateral pillars was performed as a second layer. A negative suction drain was placed in each breast along the new IMF into the axilla. The vertical and circumareolar incisions were closed. A compressive foam dressing was applied around the perimeter of the breast with a lipoelastic brassiere to facilitate the obliteration of any dead space and provide external support for the creation of the new inframammary crease.
RESULTS
A total of 113 consecutive procedures in 68 female patients with various breast conditions were managed using an extended superior pedicle approach. The ages of the patients ranged from 20 to 60 years. Twenty-six breast reductions were all bilateral in 13 patients with a mean resected volume between 300 and 600 g. One of these 13 patients underwent bilateral oncoplastic therapeutic reduction with bilateral lumps located medially and laterally that were removed with the U-shaped reduction. Thirty mastopexies were in 15 patients with autoaugmentations, and all were bilateral. There were 10 augmentation mastopexies with submammary implants (six bilateral and four unilateral) in seven patients and 10 augmentation mastopexies with submuscular implants (six bilateral and four unilateral) in seven patients. For tuberous breast, there were four procedures, which were bilateral in two patients. For oncoplastic breast conservation surgery, there were 23 procedures (eight bilateral and 15 unilateral) in 19 patients. For secondary mastopexy after previous reductions, there were eight procedures, which were bilateral in four patients. For secondary mastopexy after explantation, there were two procedures, which were bilateral in one patient. All 68 patients expressed that the results were either excellent (85.3%) or very good (14.7%) according to the evaluation parameters. Patient aesthetic outcome scores are summarized in Table 2.
Table 2.
Patient Satisfaction
| Excellent | Very Good | Good | Poor | |
|---|---|---|---|---|
| Shape | 68 | |||
| Symmetry | 67 | 1 | ||
| Ptosis correction | 68 | |||
| Upper pole fullness | 60 | 8 | ||
| Scar quality | 67 | 1 |
In the assessment of the consensus of the three independent plastic surgeons, among the 68 patients, there were 62 very good outcomes (91.2%) and six good outcomes (8.8%). No major complications such as partial or total full-thickness loss of NAC, major asymmetry, or ptosis relapse. Only one reduction experienced a superficial partial loss which was improved with no intervention. There was minor asymmetry in three patients (4.4%), which was not experienced by the patients, and poor scar quality in one darker-skinned patient. The complication rate of the 113 procedures is summarized in Table 3.
Table 3.
Complication Rate for Each Surgical Procedure
| Surgical Procedures | Complications | ||
|---|---|---|---|
| Asymmetry | NAC Necrosis | Poor Scar | |
| Breast reduction | 1 Patient (7.7%) | Partial 1 (3.8%) | |
| Mastopexy with autoaugmentation | 1 Patient (6.7%) | ||
| Augmentation mastopexy with submammary implants | |||
| Augmentation mastopexy with submuscular implants | |||
| Tuberous breast | 1(25%) | ||
| Oncoplastic breast conservation surgery | 2 (8.7%) | ||
| Secondary mastopexy after previous reductions | |||
| Secondary augmentation mastopexy after explantation | |||
DISCUSSION
The correct positioning, with reliable vascularity, of the NAC is an important aspect of all mammaplasty procedures. In 1930, Schwarzmann described a surgical procedure for mammaplasty or mastopexy in which the viability of the nipple-areolar complex was only based on dermal circulation. He demonstrated that the correct positioning of the NAC was possible regardless of the type of glandular excision.15 The superior pedicle breast reduction has been refined by Pitanguy since its original description.16 The superior pedicle autoaugmentation mammaplasty had been used as a dermoglandular extension that can be transposed behind the NAC.17
In this article, the author describes the design of a superior dermoglandular pedicle that incorporates tissue from the inferior pole of the breast. This extended portion of the superior pedicle is a reliable and versatile technique for correction of various breast deformities, such as reduction mammoplasty; mastopexy; augmentation mastopexy, either autoaugmentation or prosthetic; tuberous breast; after lumpectomy resection; and even in secondary breast conditions. Also, the design of this flap is such that closure of the donor site leads to a new cephalad inframammary crease with narrowing of the breast base.
Our patients with different breast deformities were candidates for different surgical techniques. We have performed the extended superior dermoglandular pedicle technique because of the observation about the reliability of the blood supply of this pedicle and the very satisfactory results, especially in terms of breast projection.
A superior pedicle dermoglandular flap had been used as an extended flap and raised from the lower pole of the breast and transposed to the upper pole. The flap is fixed like a hammock to the pectoral fascia, and the wedge-shaped donor defect is closed by approximation and fixation of the medial and lateral pillars.18
Also, an inverted, triangular-shaped flap had been incorporated with a superior dermoglandular pedicle with a distal flap that is sutured underneath the pectoralis.19
In the above techniques, the amount of transposed breast tissue is less than with our technique because the tissue from the IMF is not incorporated as part of the flap. The benefits conferred by glandular transposition are therefore not maximized with no elevation of the IMF.
The extension of the superior pedicle can be used as an autoaugmentation with transposition behind the NAC. This reestablishes central mound projection while also reducing the base of the breast and raising the inframammary crease.
Autologous tissues may support a small or medium-sized implant in cases of augmentation mastopexy, but the large implant may require additional support by autologous tissue or acellular dermal matrix.10 A smaller implant of 200–350 mL had been used and recommended for one-stage augmentation mastopexy to minimize scar widening and the incidence of recurrent ptosis.20
The breast fascia, ligaments, and attachments21–23 may be stretched or loosened and fail to provide proper implant support, especially in larger implants with ptosis recurrence. The extended portion of the superior pedicle acts as a second strong lower pole support and can replace acellular dermal matrix for long-lasting implant stability, upper pole fullness, and limitation of caudal displacement.
In reduction mammoplasty, by using this extended superior pedicle, there will be redraping of the breast parenchyma after lateral and medial reductions in conjunction with central and upper pole autoaugmentation to get a long-term, well-contoured, projected breast with upper pole fullness. The increased thickness of the pedicle has the advantage of relocating a large amount of well-vascularized mammary tissue centrally and deeply in the new breast cone, improving projection.
The extended superior pedicle, in our opinion, is considered an ideal and logical technique for both mastopexy and reduction mammoplasty, as it moves the breast in the reverse vector of descent without excessive manipulation and distortion of the original breast shape. It also restores central mound projection while narrowing the lower breast base, raising the inframammary crease and reliably recreating a more youthful breast shape.
The extension of the superior pedicle to the inferior aspect of the breast to create the extended superior pedicle flap that can be rotated to fill the medial and lateral defects has been used easily without any complications to establish the potential advantages of therapeutic mammoplasty, which are cosmetic and psychological, and may be oncological.24
CONCLUSIONS
The extended superior pedicle is a reliable and versatile technique for various breast indications. We were able to expand its applications for various breast deformities, such as reduction mammoplasty; mastopexy; augmentation mastopexy, either autoaugmentation or prosthetic; tuberous breast; after lumpectomy resection; and even in secondary breast conditions. It gives us the ability to transfer vascularized tissue from the lower pole to the areas that require autoaugmentation and support for prosthetic augmentation. Its versatility allows also for reproducible results in a broad range of patients. Use of the extended superior pedicle flap provides consistent results concerning breast contour, nipple viability, and lasting superior fullness, and saves operating time compared with other techniques.
DISCLOSURES
The author has no financial interest to declare in relation to the content of this article. The author has no conflicts of interest.
Supplementary Material
Footnotes
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Rohrich RJ, Gosman AA, Brown SA, et al. Mastopexy preferences: a survey of board-certified plastic surgeons. Plast Reconstr Surg. 2006;118:1631–1638. [DOI] [PubMed] [Google Scholar]
- 2.Weiner DL, Aiache AE, Silver L, et al. A single dermal pedicle for nipple transposition in subcutaneous mastectomy, reduction mammaplasty, or mastopexy. Plast Reconstr Surg. 1973;51:115–120. [DOI] [PubMed] [Google Scholar]
- 3.Arie G. Una nueva tecnica de mastoplastia. Rev Iber Latino Am Cir Plast. 1957;3:23–31. [Google Scholar]
- 4.Lejour M. Vertical mammaplasty and liposuction of the breast. Plast Reconstr Surg. 1994;94:100–114. [DOI] [PubMed] [Google Scholar]
- 5.Van Deventer PV, Graewe FR. The blood supply of the breast revisited. Plast Reconstr Surg. 2016;137:1388–1397. [DOI] [PubMed] [Google Scholar]
- 6.Losken A, Holtz DJ. Versatility of the superomedial pedicle in managing the massive weight loss breast: the rotation-advancement technique. Plast Reconstr Surg. 2007;120:1060–1068. [DOI] [PubMed] [Google Scholar]
- 7.Kwei S, Borud LJ, Lee BT. Mastopexy with autologous augmentation after massive weight loss: the intercostal artery perforator (ICAP) flap. Ann Plast Surg. 2006;57:361–365. [DOI] [PubMed] [Google Scholar]
- 8.Hamdi M, Van Landuyt K, Blondeel P, et al. Autologous breast augmentation with the lateral intercostal artery perforator flap in massive weight loss patients. J Plast Reconstr Aesthet Surg. 2009;62:65–70. [DOI] [PubMed] [Google Scholar]
- 9.Zienowicz RJ, Karacaoglu E. Augmentation mammaplasty by reverse abdominoplasty (AMBRA). Plast Reconstr Surg. 2009;124:1662–1672. [DOI] [PubMed] [Google Scholar]
- 10.Colwell AS, Driscoll D, Breuing KH. Mastopexy techniques after massive weight loss: an algorithmic approach and review of the literature. Ann Plast Surg. 2009;63:28–33. [DOI] [PubMed] [Google Scholar]
- 11.Graf RM, Mansur AE, Tenius FP, et al. Mastopexy after massive weight loss: extended chest wall-based flap associated with a loop of pectoralis muscle. Aesthetic Plast Surg. 2008;32:371–374. [DOI] [PubMed] [Google Scholar]
- 12.Mistry RM, MacLennan SE, Hall-Findlay EJ. Principles of breast re-reduction: a reappraisal. Plast Reconstr Surg. 2017;139:1313–1322. [DOI] [PubMed] [Google Scholar]
- 13.Alperovich M, Tanna N, Samra F, et al. Nipple-sparing mastectomy in patients with a history of reduction mammaplasty or mastopexy: how safe is it? Plast Reconstr Surg. 2013;131:962–967. [DOI] [PubMed] [Google Scholar]
- 14.Frederick MJ, Lin AM, Neuman R, et al. Nipple-sparing mastectomy in patients with previous breast surgery: comparative analysis of 775 immediate breast reconstructions. Plast Reconstr Surg. 2015;135:954e–962e. [DOI] [PubMed] [Google Scholar]
- 15.Schwarzmann E. Die technik der mammaplastik the classic reprint. Plast Reconstr Surg. 1977;59:107–112. [DOI] [PubMed] [Google Scholar]
- 16.Pitanguy I. Surgical correction of breast hypertrophy. Br J Plast Surg. 1967;20:78–85. [DOI] [PubMed] [Google Scholar]
- 17.Kim P, Kim KK, Casas LA. Superior pedicle auto augmentation mastopexy: a review of 34 consecutive patients. Aesthet Surg J. 2010;30:201–210. [DOI] [PubMed] [Google Scholar]
- 18.De la Plaza R, Cruz L M. Mastopexy utilizing a dermo-glandular hammock flap. Aesthetic Surg J. 2005;25:31–36. [DOI] [PubMed] [Google Scholar]
- 19.Cerqueira A. Mammoplasty: breast fixation with dermo-glandular mono upper Pedicle flap under the pectoralis muscle. Aesthetic Plast Surg. 1988;22:276. [DOI] [PubMed] [Google Scholar]
- 20.Albert L, Daniel JH. Versatility of the superomedial pedicle in managing the massive weight loss breast: The rotation-advancement technique. Plast Reconstr Surg. 2007;120:1060–1068. [DOI] [PubMed] [Google Scholar]
- 21.Matousek SA, Corlett RJ, Ashton MW. Understanding the fascial supporting network of the breast: key ligamentous structures in breast augmentation and a proposed system of nomenclature. Plast Reconstr Surg. 2014;133:273–281. [DOI] [PubMed] [Google Scholar]
- 22.Maclin MM, II, Deigni OA, Bengtson BP. The laminated nature of the pectoralis major muscle and the redefinition of the inframammary fold: clinical implications in aesthetic and reconstructive breast surgery. Clin Plast Surg. 2015;42:465–479. [DOI] [PubMed] [Google Scholar]
- 23.Rehnke RD, Groening RM, Van Buskirk ER, et al. Anatomy of the superficial fascia system of the breast: a comprehensive theory of breast fascial anatomy. Plast Reconstr Surg. 2018;142:1135–1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McCulley SJ, Macmillan RD. Planning and use of therapeutic mammoplasty—Nottingham approach. Br J Plast Surg. 2005;58:889–901. [DOI] [PubMed] [Google Scholar]