Abstract
Objective
Health-related quality of life (HRQoL) was an important health outcome measure for evaluating an individual’s overall health status. However, there was limited in the literature on HRQoL and its long-term changes of the Tibetan population. This study aimed to assess HRQoL of Tibetan and its changes over time, and explore the differences in HRQoL for residents at different altitudes.
Design
Data for the cross-sectional study were extracted from the fifth and sixth waves of the National Health Services Surveys which were conducted in 2013 and 2018. A multistage stratified cluster random sampling strategy was used to select representative participants.
Setting
Tibet Autonomous Region in China.
Participants
This study recruited 14 752 participants in 2013 and 13 106 participants in 2018, and after excluding observations with missing values for key variables, 10 247 in 2013 and 6436 in 2018 were included in the study analysis.
Primary and secondary outcome measures
The EQ-5D-3L was used to measure participants’ HRQoL.
Results
The mean health state utility scores of the participants were 0.969±0.078 and 0.966±0.077 in 2013 and 2018, respectively. Pain/discomfort was the most frequently prevalent issue reported in 18.1% and 17.9% of the participants in 2013 and 2018, respectively. Tibetans living 3500–4000 m altitude had the best HRQoL. Age, sex, employment status, educational attainment, chronic disease and weekly physical exercise were influencing factors associated with HRQoL.
Conclusions
The HRQoL of the Tibetan population was lower than the general Chinese population, and decreased over time between 5 years. There were differences in HRQoL among Tibetan at different altitudes, with residents living at 3500–4000 m having the best quality of life. More attention should be paid to those Tibetans who are older, female, unemployed and without formal education.
Keywords: PUBLIC HEALTH, Quality of Life, China
STRENGTHS AND LIMITATIONS OF THIS STUDY.
We used Tibetan resident data from two National Health Service Surveys conducted in 2013 and 2018.
This is the first study to assess the health-related quality of life and its changes of Tibetan over time.
We divided the residents into three different altitude groups based on the international altitude standard and analysed the differences in health-related quality of life for residents at different altitudes.
The same pool of participants was not characterised in the two surveys; however, some overlap may exist.
Introduction
Health-related quality of life (HRQoL) is considered as an important health outcome measure in recent years to inform patient-centred care, clinical decision-making, health policy and reimbursement decisions.1 HRQoL refers to the impact of health on the quality of life of individuals focusing on individuals’ health influencing their goals, expectations, standards and concerns. It is a multidimensional concept referring to people’s physical, mental and social domains of well-being, as well as personal beliefs, level of independence, and their relationships with the environment.2 The HRQoL of the residents in a region could be measured through the health surveys for the resident population.3 The HRQoL can be evaluated by generic preference-based measures (GPBMs), which provide a standardised health state classification system and a tariff of quality weights for all health states described by the classification system.4 The EuroQol 5-Dimensions (EQ-5D) is the most widely used GPBMs to measure and evaluate HRQoL in population surveys, clinical studies and economic evaluations.5 The EQ-5D-3 Level (3L) was included in the 2008 National Health Services Surveys (NHSS) for the first time to assess the population health status in China.
The Tibet Autonomous Region (TAR), located on the Qinghai-Tibet plateau in southwest China with an average altitude of 4000 m above sea level, is commonly referred to as the ‘Roof of the World’.6 The TAR has an area of >1.2 million km2, accounting for one-eighth of China’s geographical area. In 2021, the population in TAR was 3.65 million with 90% of the population being Tibetan.7 Its social and economic development levels are relatively low among China’s provinces. Most of the TAR population comprises farmers and herders, scattered in remote rural areas with limited income source mainly depending on agriculture.8 High-altitude areas present a complex ecology in physical environment and population characteristics including genetics, lifestyle, socioeconomic factors and access to medical care,9 directly or indirectly impact health.10 Previous studies have reported that high altitude is strongly associated with the many health issues including psychiatric disorders,11 12 hypertension6 13 and cardiovascular diseases.10 China has been undergoing a period of unprecedented rates of economic growth, development and poverty reduction in recent decades, including the TAR.14 Various economic, educational and health policies have been implemented for the development of society, which may have greatly affected the health of residents living in TAR.15
Previous studies have assessed the population HRQoL in various provinces of China, such as Heilongjiang,16 Gansu,17 Shanxi18 and Hunan.19 However, these studies focused on low-altitude areas and used data only from a cross-sectional survey. Moreover, there are only two studies that have assessed the change in HRQoL over time in the general population of mainland China.20 21 One study used the data from two waves of NHSS from 2008 to 2013,20 while another study used three waves of Health Services Surveys from 2008 to 2020 in Tianjin.21 Both studies reported a slight decreasing in HRQoL of the population and disparities in HRQoL across different demographic and socioeconomic subgroups in China. Additionally, previous studies on the health status of the Tibetan population are limited due to the geographical environment, lack of basic resources and facilities, and low population density. Therefore, this study aimed to assess the HRQoL of the Tibetan population and its changes over time, and explore the differences in HRQoL for residents at different altitudes.
Methods
Study design and population
Data for the cross-sectional study were extracted from the fifth and sixth waves of the NHSS in Tibet, which were conducted in 2013 and 2018. A multistage stratified cluster random sampling strategy was used to select representative participants. Each stage had a systematic random sampling approach. In the first stage, 24 counties were selected in 2013 and 25 counties were selected in 2018 from the 7 cities in Tibet in proportion to their population size. In the second stage, 60 towns/subdistricts were selected in 2013 and 59 towns/subdistricts were selected in 2018 using the random cluster method according to population size. In the third stage, three villages/communities were randomly selected from each town or subdistrict, and 155 villages/communities were selected in 2013 and 159 villages/communities were selected in 2018. The majority of the counties, towns/subdistricts, villages/communities sampled in 2018 were the same as those sampled in 2013. In the fourth stage, 20 households from each village of community were randomly selected for participation, and 4140 households were selected in 2013 and 4232 households were selected in 2018.
Questionnaires were administered to the participants through face-to-face interviews. The students majoring in Preventive Medicine at Medical College of Tibet University were uniformly recruited and trained to be interviewers by supervisors who had participated in national training. Presurvey training workshops were offered to all interviewers following a standardised protocol. Eligible interviewers had to demonstrate proper understanding of the purpose of the NHSS and their ability to meet data collection standards developed by the Centre for Health Statistics and Information. The interviewers visited the selected households, and all family members in a sampled household were eligible to participate in the survey. Before the survey commenced, participants were informed of the survey’s purposes and procedure and then provided informed consent.
In total, 14 752 participants in 2013 and 13 106 participants in 2018 completed the survey. The exclusion criteria in this study were as follows: (1) participants aged <15 years were excluded since the EQ-5D-3L is recommended to be used among ≥15 years by the user guide (n=3412 in 2013 and n=2677 in 2018); (2) participants who did not answer the questionnaires by themselves were excluded since the EQ-5D-3L need to be self-complete (n=1001 in 2013 and n=3798 in 2018); (3) participants with missing values for key variables including socio-demographic characteristics were excluded (n=4 in 2013 and n=1 in 2018) and (4) participants with ethnicities other than Tibetan were excluded (n=88 in 2013 and n=194 in 2018). Overall, the final sample size of 10 247 in 2013 and 6436 in 2018 was included in this study for analysis.
Measurement of HRQoL
The EQ-5D-3L is one of the most widely used HRQoL measurement instruments classified into five dimensions: mobility (MO), self-care (SC), usual activities (UA), pain/discomfort (PD) and anxiety/depression (AD). Each dimension contains three functioning response levels (no problems, moderate problems and extreme problems), generating 243 (35) possible health states, with the best state indicated by the response ‘11111’ and the worst health state indicated by the response ‘33333’.22 A single health state utility (HSU) score can be assigned to each health state using a value set, developed in a valuation study based on the general population’s health preferences.
Four value sets exist for the EQ-5D-3L in China with the first value set developed in 2014 (3L2014 value set) using a sample comprising residents mainly from urban areas,23 the second value set developed in 2018 (3L2018 value set) adopted a more representative sample of residents from both rural and urban areas,24 the other two value set developed in 2022 (3L2022 value set) recruited participants from rural areas of five cities.25 In this study, we chose to adopt the 3L2018 value set. The main reason for the choice was based on the participants in the 3L2014 value set being selected conveniently from big cities in urban areas through quota sampling. While the 3L2018 value set, a more representative sample of respondents was obtained from both rural and urban areas using a random sampling method.26 The rural population accounts for half of the Chinese population, and large disparities exist in socioeconomic status, lifestyle and health status between urban and rural areas in China.27 In the two waves of NHSS in the TAR, more than 75% of participants were from farming and pastoral areas. Therefore, the 3 L2018 value set, which more closely matches the distribution of the Tibetan population, was used in this study. To evaluate the robustness and sensitivity of the 3 L2018 value set, we also used the 3 L2022 value set to analyse the main results revealing that the main results of the two value sets had the same trends (online supplemental table 1).
bmjopen-2023-072854supp001.pdf (76.5KB, pdf)
Independent variables
In this study, the independent variables were sociodemographic, altitude-related, and clinical disease variables, and health-related behaviours. Sociodemographic variables were sex, age, employment status, educational attainment and marital status. We divided age into three groups: 15–44, 45–65 and ≥65 years old. Employment status was divided into employed, retired and unemployed. Educational attainment was divided into three groups: illiterate, primary school, junior high school and above. Marital status was divided into single, married, divorced and other.
The altitude-related variables included location and altitude. The participants were divided into rural and urban groups based on their geographical location. The NHSS did not collect data on the altitude of their residence; therefore, we used Google Maps to obtain the precise altitude. Altitudes were defined as high (1500–3500 m), very high (3500–5500 m) and extreme altitude (>5500 m), as suggested by the International Society for Mountain Medicine.28 The average altitude of Tibet is above 4000 m, and the high altitude (3500–5000 m) and extreme altitude areas (>5000 m) account for 93.69% of the land area of the TAR.29 The altitude range of the two surveys was 1974–4936 m, and the average altitude was 3863±515 m, with no extreme altitude areas. In addition, we considered the number of villages and participants in different altitude groupings. Therefore, we divided the plateau areas into three altitude groups, high (1500–3500 m), very high (3500–4000 m) and extreme altitude (4000–5000 m) based on the China’s policy of subsidising plateau areas in this study.30 The altitude classification criterion was consistent in two waves of surveys.
The clinical disease variables included diagnosis of the participant with any illness within 2 weeks before survey and the number of chronic diseases during the past 6 months. A chronic condition was defined as a condition diagnosed by a doctor with symptoms persisting or relevant medical treatment continuing over the past 6 months.
Health-related behavioural variables were current smoking status, divided into three groups: smoking all the time, has ever smoked and never smoked. Participants were asked to perform weekly physical exercise during the past 6 months, such as climbing, ball games, equipment exercise, swimming, jogging. The frequency of physical exercise was divided into three groups: never exercised, 1–5 times and >6 times.
Patient and public involvement
Patients and the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Statistical analysis
Descriptive statistics were used for participants’ characteristics and the reported problems on the five dimensions of the EQ-5D-3L. Continuous variable was described as mean and SD, whereas categorised variable was described as frequency and percentages. Student’s t-test or analysis of variance was used when variables conformed to an approximately normal distribution; otherwise, the Mann-Whitney U test or Kruskal-Wallis H test was used. Categorical variables were compared between the groups using the χ2 test.
The importance of changes in the HSU scores was estimated using effect sizes (ES), which were calculated as the difference between the highest and the lowest HSU scores among the two surveys divided by the pooled SD. The ES was defined ≤0.5, 0.5–0.8 and ≥0.8 were small, moderate and large.31 In this study, the moderate ES (0.5) was considered as a threshold for minimal importance of changes in the HSU scores. As the HSU score was left-skewed with a large proportion of respondents in full health, the Tobit regression model was used to assess the influencing factors associated with EQ-5D-3L HSU scores. Data were entered into Epidata V.3.1 and analysed using SPSS V.24.0, and STATA V.15.0. A two-tailed p<0.05 was considered statistically significant.
Results
Participant characteristics
The characteristics of the participants are listed in table 1. In 2013, more than half of the participants were in the 15–44 years age group (56.2%), and older participants accounted for <15% of the participants (11.0%) and less than half of the participants were male (46.5%). Moreover, 57% of participants had never received education and 15.0% of the participants were unemployed. More than four out of five participants resided in rural areas (84.9%) with an average altitude of 3838±526 m. Overall, 11.4% of participants reported having a disease during 2 weeks before data collection, while more than half of participants (65.6%) had no chronic diseases during the past 6 months.
Table 1.
Characteristics of the participants
| Characteristics | 2013 (N=10 247) | 2018 (N=6436) | Total (N=16 683) | P value | |||
| N | % | N | % | N | % | ||
| Age groups | <0.001 | ||||||
| 15–44 years | 5754 | 56.2 | 3159 | 49.1 | 8913 | 53.4 | |
| 45–64 years | 3363 | 32.8 | 2568 | 39.9 | 5931 | 35.6 | |
| ≥65 years | 1130 | 11.0 | 709 | 11.0 | 1839 | 11.0 | |
| Gender | <0.001 | ||||||
| Male | 4766 | 46.5 | 2792 | 43.4 | 7558 | 45.3 | |
| Female | 5481 | 53.5 | 3644 | 56.6 | 9125 | 54.7 | |
| Educational attainment | <0.001 | ||||||
| Illiterate | 5841 | 57.0 | 3348 | 52.0 | 9189 | 55.1 | |
| Primary school | 3080 | 30.1 | 2143 | 33.3 | 5223 | 31.3 | |
| Junior high school and above | 1326 | 12.9 | 945 | 14.7 | 2271 | 13.6 | |
| Employment | 0.008 | ||||||
| Employed | 8514 | 83.1 | 5228 | 81.3 | 13 742 | 82.4 | |
| Retired | 198 | 1.9 | 131 | 2.0 | 329 | 2.0 | |
| Unemployed | 1535 | 15.0 | 1077 | 16.7 | 2612 | 15.7 | |
| Marital status | <0.001 | ||||||
| Single | 1563 | 15.3 | 748 | 11.6 | 2311 | 13.9 | |
| Married | 7718 | 75.3 | 5037 | 78.3 | 12 755 | 76.5 | |
| Separated/divorced/widowed | 966 | 9.4 | 651 | 10.1 | 1617 | 9.7 | |
| Location | <0.001 | ||||||
| Rural | 8699 | 84.9 | 4988 | 77.5 | 13 687 | 82.0 | |
| Urban | 1548 | 15.1 | 1448 | 22.5 | 2996 | 18.0 | |
| Altitude, m (mean±SD) | 3838±526 | – | 3903±495 | – | 3863±515 | – | |
| Altitude groups | <0.001 | ||||||
| 1500–3500 m | 2219 | 21.7 | 1123 | 17.5 | 3342 | 20.0 | |
| 3500–4000 m | 4816 | 47.0 | 2933 | 45.6 | 7749 | 46.4 | |
| 4000–5000 m | 3212 | 31.3 | 2380 | 36.9 | 5592 | 33.5 | |
| Diseased during the past 2 weeks | 0.366 | ||||||
| Yes | 1152 | 11.4 | 701 | 10.9 | 1853 | 11.1 | |
| No | 9002 | 88.6 | 5735 | 89.1 | 14 737 | 88.3 | |
| Number of chronic diseases | <0.001 | ||||||
| 0 | 6726 | 65.6 | 3684 | 57.2 | 10 410 | 62.4 | |
| 1 | 2634 | 25.7 | 1743 | 27.1 | 4377 | 26.2 | |
| ≥2 | 887 | 8.7 | 1009 | 15.7 | 1896 | 11.4 | |
| Smoking | <0.001 | ||||||
| Smoker | 1424 | 13.9 | 724 | 11.2 | 2148 | 12.9 | |
| Ex-smoker | 487 | 4.7 | 238 | 3.7 | 725 | 4.3 | |
| Non-smoker | 8336 | 81.4 | 5474 | 85.1 | 13 810 | 82.8 | |
| Weekly physical exercise during the past 6 months | <0.001 | ||||||
| Never exercised | 9437 | 92.3 | 4054 | 63.0 | 13 491 | 80.9 | |
| 1–5 times | 511 | 5.0 | 1247 | 19.4 | 1758 | 10.5 | |
| ≥6 times | 279 | 2.7 | 1135 | 17.6 | 1414 | 8.5 | |
In 2018, the sociodemographic characteristics of the participants were basically the same as those in 2013. The average age was 45.2±14.7 years, and more than half of the participants were female (56.6%). Of the participants, 52.0% never had education, 81.3% were employed, 78.3% were married and 77.5% lived in rural areas with an average altitude of 3903±495 m. Most of the participants (85.1%) were non-smokers, and 63.0% had never engaged in weekly physical exercise during the past 6 months. Compared with two waves of surveys, participants in the 2018 were more female (p<0.001), reported a higher level of education (p<0.001), had a lower employed proportion (p=0.008), more lived in urban with more high altitude (p<0.001).
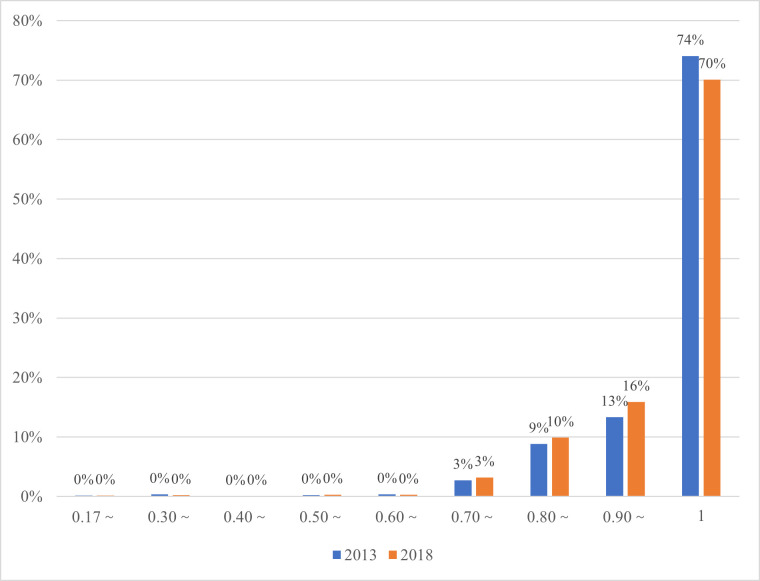
Participant’s HRQoL and its changes
The HSU scores stratified by characteristics of participants in two surveys were listed in table 2. The mean HSU scores of the participants were 0.969±0.078 in 2013 and 0.966±0.077 in 2018, which showed a significantly decreasing trend (p<0.001, ES=0.136). Figure 1 presents the distribution of participant’s HSU scores in two surveys. It revealed a left-skewed distribution with skewness of −4.189 in 2013 and −4.642 in 2018, ranging from 0.170 to 1.000. The states of 11 111 (no problems in any dimension) were reported in 74% and 70% of the participants in 2013 and 2018, respectively. The trend in HSU scores was observed to decrease in most subgroups.
Table 2.
Health state utility score stratified by characteristics of participants in two surveys
| Characteristics | 2013 (N=10 247) | 2018 (N=6436) | Effect size | P value |
| Age | ||||
| 15–44 years | 0.987 (0.049) | 0.987 (0.041) | 0.000 | 0.003 |
| 45–64 years | 0.962 (0.078) | 0.959 (0.076) | 0.039 | 0.013 |
| ≥65 years | 0.900 (0.133) | 0.899 (0.139) | 0.007 | 0.973 |
| Gender | ||||
| Male | 0.975 (0.071) | 0.973 (0.070) | 0.030 | 0.002 |
| Female | 0.964 (0.083) | 0.961 (0.082) | 0.036 | <0.001 |
| Employment | ||||
| Employed | 0.977 (0.064) | 0.976 (0.058) | 0.016 | <0.001 |
| Retired | 0.945 (0.116) | 0.965 (0.057) | 0.205 | 0.493 |
| Unemployed | 0.926 (0.117) | 0.918 (0.128) | 0.066 | 0.011 |
| Educational attainment | ||||
| Illiterate | 0.959 (0.088) | 0.956 (0.088) | 0.034 | <0.001 |
| Primary school | 0.979 (0.064) | 0.971 (0.069) | 0.121 | <0.001 |
| Junior high school and above | 0.990 (0.046) | 0.991 (0.038) | 0.023 | 0.180 |
| Marital status | ||||
| Single | 0.975 (0.086) | 0.979 (0.068) | 0.050 | 0.182 |
| Married | 0.973 (0.069) | 0.969 (0.069) | 0.058 | <0.001 |
| Separated/divorced/widowed | 0.928 (0.111) | 0.925 (0.124) | 0.026 | 0.832 |
| Location | ||||
| Rural | 0.967 (0.080) | 0.966 (0.077) | 0.013 | 0.001 |
| Urban | 0.980 (0.065) | 0.967 (0.080) | 0.183 | <0.001 |
| Altitude groups | ||||
| 1500–3500 m | 0.966 (0.078) | 0.961 (0.079) | 0.064 | <0.001 |
| 3500–4000 m | 0.975 (0.072) | 0.970 (0.073) | 0.069 | <0.001 |
| 4000–5000 m | 0.963 (0.084) | 0.963 (0.081) | 0.000 | 0.411 |
| Diseased during the past 2 weeks | ||||
| Yes | 0.933 (0.111) | 0.934 (0.100) | 0.009 | 0.303 |
| No | 0.974 (0.072) | 0.970 (0.073) | 0.055 | <0.001 |
| Number of chronic diseases | ||||
| 0 | 0.983 (0.057) | 0.986 (0.049) | 0.055 | 0.331 |
| 1 | 0.950 (0.097) | 0.951 (0.091) | 0.010 | 0.663 |
| ≥2 | 0.920 (0.113) | 0.919 (0.106) | 0.009 | 0.223 |
| Smoking | ||||
| Smoker | 0.985 (0.056) | 0.984 (0.048) | 0.019 | 0.094 |
| Ex-smoker | 0.965 (0.073) | 0.954 (0.089) | 0.138 | 0.146 |
| Non-smoker | 0.967 (0.081) | 0.964 (0.080) | 0.037 | <0.001 |
| Weekly physical exercise during the past 6 months | ||||
| Never exercised | 0.969 (0.079) | 0.961 (0.086) | 0.098 | <0.001 |
| 1–5 times | 0.967 (0.071) | 0.973 (0.066) | 0.087 | 0.004 |
| ≥6 times | 0.985 (0.044) | 0.977 (0.051) | 0.171 | <0.001 |
| Total | 0.969 (0.078) | 0.966 (0.077) | 0.136 | <0.001 |
Figure 1.
Distribution of participant’s health state utility scores in 2013 and 2018.
The highest proportion of reporting health problems was the PD dimension (2013: 18.1%, 2018: 17.9%). Problems with SC dimension were least prevalent, 7.7% and 8.5% participants reported in 2013 and 2018, respectively. As compared with the 2013, reported problems increased in MO (by 1.2%), SC (by 0.8%), UA (by 0.6%) and AD (by 3.8%) in 2018. While reported problems in PD decreased by 0.2% (table 3).
Table 3.
Health problems reported by participants based on EQ-5D-3L
| EQ-5D-3L | 2013 | 2018 | χ2 | P value | ||
| N | % | N | % | |||
| Mobility | 12.794 | 0.002 | ||||
| No problem | 8956 | 87.4 | 5544 | 86.2 | ||
| Moderate problem | 1221 | 11.9 | 865 | 13.4 | ||
| Extreme problem | 70 | 0.7 | 27 | 0.4 | ||
| Self-care | 2.791 | 0.248 | ||||
| No problem | 9453 | 92.3 | 5891 | 91.5 | ||
| Moderate problem | 733 | 7.1 | 502 | 7.8 | ||
| Extreme problem | 61 | 0.6 | 43 | 0.7 | ||
| Usual activities | 1.407 | 0.495 | ||||
| No problem | 9014 | 88.0 | 5624 | 87.4 | ||
| Moderate problem | 1077 | 10.5 | 714 | 11.1 | ||
| Extreme problem | 156 | 1.5 | 98 | 1.5 | ||
| Pain/discomfort | 7.543 | 0.023 | ||||
| No problem | 8393 | 81.9 | 5283 | 82.1 | ||
| Moderate problem | 1750 | 17.1 | 1059 | 16.4 | ||
| Extreme problem | 104 | 1.0 | 94 | 1.5 | ||
| Anxiety/depression | 52.078 | <0.001 | ||||
| No problem | 9111 | 88.9 | 5479 | 85.1 | ||
| Moderate problem | 1047 | 10.2 | 874 | 13.6 | ||
| Extreme problem | 89 | 0.9 | 83 | 1.3 | ||
EQ-5D-3L, EuroQol-5-Dimensions-3 Level.
HRQoL of participants at different altitudes
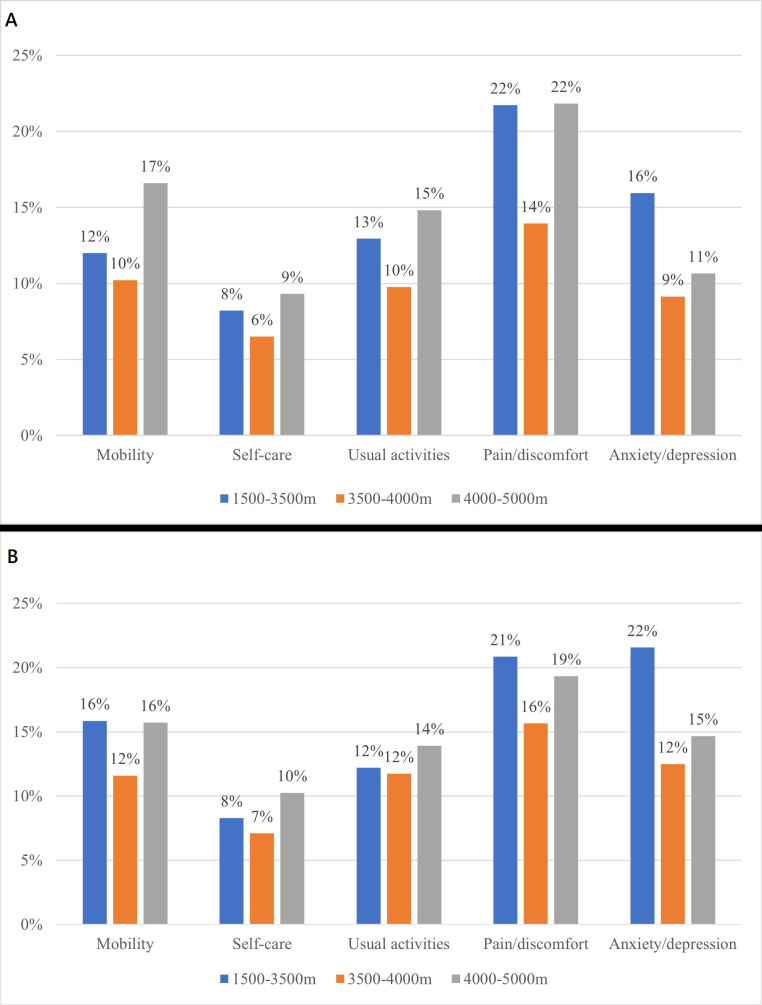
Two survey’s findings showed that participants living in the 3500–4000 m group had the highest HSU scores. Similar to the general trend, health state scores in 2018 were slightly lower than those in 2013 at different altitude groups (table 2). Figure 2 describes the percentage of participants with self-reported health problems by different altitude groups. The distribution trend was generally consistent in two surveys. Participants living in 3500–4000 m had the least reported problems in all five dimensions, while participants living in 1500–3500 m and 4000–5000 m reported more problems in PD, AD and MO dimensions.
Figure 2.
(A) Proportions of health problems reported by participants at different altitude in 2013. (B) Proportions of health problems reported by participants at different altitude in 2018.
Factors associated with HSU scores
The Tobit regression analyses of the factors associated with HSU scores were presented in table 4. The result confirmed the decreased trend in HSU scores over time (β=−0.014, p<0.001), after adjustment for variations in the other independent variables. However, the ES of this change did not reach the threshold of minimal clinical importance (ES=0.04). The elderly, the unemployed, the separated/divorced/widowed and the healthy participants were significant predictors of the HSU score, with generally larger values of ES and reached the threshold of minimal clinical importance.
Table 4.
Tobit regression analysis on the EQ-5D-3L HSU scores
| Independent variable | β | SE | P value | 95% CI | Effect size |
| Age years (ref.:15–44 years) | |||||
| 45–64 years | −0.071 | 0.004 | <0.001 | −0.079 to −0.063 | 0.43 |
| ≥65 years | −0.142 | 0.006 | <0.001 | −0.153 to −0.130 | 1.26 |
| Gender (ref.: male) | |||||
| Female | −0.025 | 0.004 | <0.001 | −0.033 to −0.017 | 0.14 |
| Educational attainment (ref.: illiterate) | |||||
| Primary school | 0.016 | 0.004 | <0.001 | 0.009 to 0.024 | −0.22 |
| Junior high school and above | 0.055 | 0.007 | <0.001 | 0.041 to 0.069 | −0.40 |
| Employment (ref.: employed) | |||||
| Retired | −0.036 | 0.012 | 0.003 | −0.060 to −0.012 | 0.38 |
| Unemployed | −0.073 | 0.005 | <0.001 | −0.082 to −0.064 | 0.72 |
| Marital status (ref.: single) | |||||
| Married | 0.018 | 0.006 | 0.002 | 0.007 to 0.029 | 0.07 |
| Separated/divorced/widowed | −0.007 | 0.008 | 0.335 | −0.022 to 0.008 | 0.52 |
| Location (ref.: rural) | |||||
| Urban | 0.039 | 0.005 | <0.001 | 0.029 to 0.049 | 0.00 |
| Altitude groups (ref.: 1500–3500 m) | |||||
| 3500–4000 m | 0.028 | 0.005 | <0.001 | 0.019 to 0.037 | −0.11 |
| 4000–5000 m | 0.011 | 0.004 | 0.017 | 0.002 to 0.021 | 0.03 |
| Diseased during the past 2 weeks (ref.: Yes) | |||||
| No | 0.042 | 0.005 | <0.001 | 0.033 to 0.052 | −0.50 |
| Number of chronic diseases (ref.: 0) | |||||
| 1 | −0.083 | 0.004 | <0.001 | −0.091 to −0.075 | 0.34 |
| ≥2 | −0.125 | 0.005 | <0.001 | −0.136 to −0.115 | 0.13 |
| Smoking (ref.: smoker) | |||||
| Ex-smoker | −0.036 | 0.010 | <0.001 | −0.055 to −0.018 | 0.34 |
| Non-smoker | −0.011 | 0.006 | 0.086 | −0.0233 to 0.002 | 0.13 |
| Weekly physical exercise (ref.: never exercised) | |||||
| 1–5 times | 0.032 | 0.006 | <0.001 | 0.020 to 0.043 | 0.00 |
| ≥6 times | 0.050 | 0.007 | <0.001 | 0.036 to 0.064 | −0.13 |
| Year (ref.: 2013) | |||||
| 2018 | −0.014 | 0.004 | <0.001 | −0.022 to −0.007 | 0.04 |
EQ-5D-3L, EuroQol-5-Dimensions-3 Level; HSU, health state utility.
Discussion
To the best of our knowledge, this is the first study to evaluate the HRQoL of the Tibetan population and its changes over time, based on a representative sample from the NHSS of Tibet in China. The HRQoL of Tibetan was lower than general Chinese population, and decreased over time in 5 years (2013–2018). Moreover, we found Tibetans living at 3500–4000 m altitude had the best HRQoL. Our study also identified factors influencing HRQoL including females, elders, unemployed and more chronic diseases with a negative impact. While higher education levels, no disease during the past 2 weeks and frequent weekly physical exercise had a positive impact on HRQoL of the Tibetan population.
The mean HSU scores of the Tibetan population were 0.969 (SD=0.078) in 2013 and 0.966 (SD=0.077) in 2018, higher than that reported in Heilongjiang, Hunan and Shanxi in China.16 17 19 This may be due to the use of two different 3L value sets used to calculate the HSU score. Compared with the 3 L2018 algorithm, the 3 L2014 algorithm includes a constant term and N3, resulting in a utility value gap between full health and the second-best health state, reducing the values of other health states.32 Therefore, the 3 L2018 index score was systematically higher than the 3 L2014 index score at absolute levels.26 The result also indicated that HSU scores of two waves of surveys were significantly lower than that of the general Chinese population, confirming regional and residential disparities in HRQoL of the Chinese populations.33 The eastern–middle–western disparities in development have existed historically. Although in recent years China’s development strategy has focused more on western areas including implementing poverty alleviation policies, promoting the construction of infrastructure, low taxation and national level fiscal transfer to the middle and western areas, a huge gap still exists between regions27 with lower HRQoL in residents of western regions than that of those in the eastern region.
Based on the HRQoL changes between the two waves of surveys, HSU scores in 2018 were slightly lower than those in 2013, and statistical differences existed in the total population and at different demographic characteristics levels. However, the changes between 2013 and 2018 were minimal and failed to reach the threshold minimal clinically important difference of ~0.074 based on EQ-5D-3L.34 This is consistent with previous studies on the changes in HRQoL in the Chinese population.20 21 This could be due to the proportion of extreme problems reported by EQ-5D-3L, with 0.42%–0.45% reporting extreme problems in AD and PD compared with 2013. According to the 3 L2014 algorithm, the value in level-3 (L3) parameters is larger than level-2 (L2) or level-1 (L1) with increasing health state severity. Hence, for a health transition involving both improvement and deterioration, the magnitude of health gain from improvement in a certain dimension may be offset to a large extent by deterioration in another dimension.26 Another possible reason may be related to the changing demographic and socioeconomic status in China. Between 2013 and 2018, the government implemented a series of policies, especially the targeting poverty alleviation strategy, driving continuous rapid growth of residents’ income and further improving the consumption level and length of life. Life expectancy increased from 76.3 to 77.0 years during this time.35 However, the ageing of the population, unhealthy lifestyles and environmental exposure have led to the rising prevalence of chronic diseases and functional limitations, related to lower HRQoL among the Tibetan population.
PD was the most frequently reported problem in this study similar to previous studies in China; however, the absolute proportion of each dimension reported was higher than the general population trends based on the NHSS data33 and other provincial studies in China.16 18 19 This may be due to the plateau disease.36 Residents living on the plateau for a long time evolve a unique physiological mechanism to adapt to the environment. However, some residents gradually lose their adaptability and suffer from various acute or chronic diseases related to the plateau environment under the stimulation of continuous hypoxia and low pressure.37 The 2-week illness prevalence rate of residents aged ≥15 years in Tibet was 20.1% in 2018, and hypertension has been reported as the most common chronic disease.38 A previous study reported that the prevalence of hypertension in Tibet is higher than the Chinese national level and is the highest among all provinces, as well as higher than other residents living at high altitudes.39 40 As altitude increases, progressive reductions in barometric pressure, air temperature and air humidity are observed. Headache, shortness of breath, chest tightness, anorexia, dizziness, limb fatigue and sleep disturbances were common symptoms of Tibetan.38
Compared with other high altitudes, we found that Tibetans living at 3500–4000 m had the best HRQoL. This could be attributed to many reasons. First, most Tibetan tend to stay at their altitude of residence for extended periods of time, the complex interaction between genetic and environmental influence led to the extraordinary ability to adapt to their hypoxic environment, and less susceptible to chronic mountain sickness.41 Second, TAR is a vast territory with a sparse population with high altitude in the northwest and low in the southeast. The region can be divided into three regions based on altitude. The Qiangtang Plateau in the north (>5000 m), and the central basin region and Himalayan mountains (4000–5000 m on average). The valleys of the middle and lower reaches of the Yarlung Zangbo River and the three rivers in eastern Tibet have an altitude of 3000–4000 m, and 60% of the population is concentrated there. Of the seven cities surveyed, Lhasa, Shannan, Qamdo and Shigaze have an average altitude of 3500–4000 m with their GDP ranking among the top four in Tibet according to the Seventh National Census in 2020. Similar results have been reported previously with socioeconomic status significantly associated with higher HRQoL.20 Socioeconomic status is detrimental to health as it affects people’s living and working conditions and restricts accessibility to medical care.42 Moreover, socioeconomic status affects people’s psychological state and cognition of the world around them.43 During the last few decades, China has implemented strong policies to facilitate economic development in the Qinghai-Tibet plateau (eg, the Strategy of the Development of China’s West). The implementation of supportive strategies should help improve socioeconomic status in the future, including improving public infrastructure, medical service capacity and disease prevention improving HRQoL.
Those living in low-altitude areas (1500–3500 m) reported the most problems in AD consistent with previous studies. A large sample survey of the prevalence of depression among Tibetans of the Qinghai-Tibet Plateau was 28.6%, higher than that in the general Chinese population and higher than that reported in a western study with high-altitude samples.44 The prevalence of depression is significantly correlated with climatic pressure, particularly altitude.45 Generally, the combined effects of harsh natural environment on the plateau, high-altitude hypoxia, low atmospheric pressure, intense ultraviolet radiation, relatively weak community support caused by low population density and lack of access to mental health resources increases the severity of depression among those living in high-altitude areas.46–48 In this study, the area with an altitude of 1500–3500 m was located southeast of the TAR. Nyingchi City, with an average altitude of 3100 m, has the lowest altitude and wettest climate in TAR. With convenient transportation and multiple splendid sceneries, tourism is the main source of income in this area, attracting millions of people travelling for sightseeing, mountaineering and trekking every year.49 Previous studies have reported a significant association between tourism impact and residents’ quality of life.50 51 Tourism provides employment opportunities and tax revenues, supports economic diversity and services and products enjoyed by residents.52 53 However, negative impacts of tourisms on residents’ HRQoL have been reported including crowding, traffic and parking issues, criminality, and cost of living, changes in hosts’ way of life, and friction between tourists and residents.54 The perceived negative impacts, negative emotions, pressure and relative deprivation of the residents will affect their subjective well-being, leading to psychological problems including anxiety and depression.
This study had several limitations. First, this study did not recruit the same pool of participants in two waves of surveys, making it difficult to identify causal associations. However, the same cities were selected, and the participants may partly overlap. Second, the participants recruited in the surveys were those had lived in Tibet for more than 6 months; however, we could not determine if they were born in Tibet or came to work from other low-altitude areas. A small-scale survey could be conducted to refine the participant inclusion criteria to validate the study findings in the future. Third, many studies have reported that EQ-5D-3L has more significant ceiling effects than EQ-5D-5L. However, EQ-5D-3L is more suitable for use in large-scale population surveys because of its small cognitive burden. Moreover, the comparison of the two waves of surveys indicated the overall changing trends in HRQoL of participants were able to be derived from EQ-5D-3L.
Conclusion
This study revealed the HRQoL of the Tibetan population was lower than general Chinese population, and decreased over time between 5 years. There were differences in HRQoL among Tibetan at different altitudes, with residents living at 3500–4000 m having the best quality of life. More attention should be paid to those Tibetans who are older, female, unemployed and without formal education. Targeted policies and strategies need to be strengthened, including plateau subsidies, poverty alleviation, primary health service capacity, standardised management of chronic diseases and health education.
Supplementary Material
Acknowledgments
We gratefully acknowledge the contribution of the investigators from Preventive Medicine at Medical College of Tibet University, and we also thank all the participants who participated in the study.
Footnotes
ZD and SL contributed equally.
Contributors: SL and ZD have substantial contributions to conception and design, acquisition of funding, data and interpretation of data. CZ and ZC were involved in the acquisition of data. LD, ZS and CL were responsible for the data analysis and interpretation of data. LD drafted the manuscript, ZS, CZ, ZC and CL revised it critically for important intellectual content, LD and SL were responsible for the decision to submit the manuscript, and all authors contributed to final approval of the manuscript. SL, as guarantor, had full responsibility for the finished work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Funding: This work was supported by the Sixth National Health Service Survey Project in Tibet (grant number 18080027); and China Medical Board (grant number 11-086).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. We have included all the data produced in the present work in the manuscript. Note that the raw data used in the study were obtained from National Health Service Surveys of China. We are unable to attach all the raw data for each participant in this paper due to the ethical restrictions.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and the study was conducted with the approval of the National Health Commission of the People’s Republic of China and the Health Commission of Tibet autonomous region. Since this survey is organised by the National Health Commission every five years, the ethical approval number is not available. Participants gave informed consent to participate in the study before taking part.
References
- 1. Calvert M, Blazeby J, Altman DG, et al. Reporting of patient-reported outcomes in randomized trials. JAMA 2013;309:814–22. 10.1001/jama.2013.879 [DOI] [PubMed] [Google Scholar]
- 2. Karimi M, Brazier J. Health-related quality of life, and quality of life: what is the difference Pharmacoeconomics 2016;34:645–9. 10.1007/s40273-016-0389-9 [DOI] [PubMed] [Google Scholar]
- 3. Macran S, Weatherly H, Kind P. Measuring population health: a comparison of three generic health status measures. Med Care 2003;41:218–31. 10.1097/01.MLR.0000044901.57067.19 [DOI] [PubMed] [Google Scholar]
- 4. Goodwin E, Green C. A systematic review of the literature on the development of condition-specific preference-based measures of health. Appl Health Econ Health Policy 2016;14:161–83. 10.1007/s40258-015-0219-9 [DOI] [PubMed] [Google Scholar]
- 5. Devlin NJ, Brooks R. EQ-5D and the Euroqol group: past, present and future. Appl Health Econ Health Policy 2017;15:127–37. 10.1007/s40258-017-0310-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mingji C, Onakpoya IJ, Perera R, et al. Relationship between altitude and the prevalence of hypertension in Tibet: a systematic review. Heart 2015;101:1054–60. 10.1136/heartjnl-2014-307158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tibet autonomous region Statistics Bureau. In: Communiqué on Main Data of the Seventh National Population Census of Tibet Autonomous Region. 2021. [Google Scholar]
- 8. Zheng Z. Research on the village public service system innovation of agricultural and pastoral areas in Tibet--from the perspective of integrated anti-poverty development. Ethnology J 2012;3:34–43. 10.3969/j.issn.1674-9391.2012.01.006 [DOI] [Google Scholar]
- 9. Beall CM. Andean, Tibetan, and Ethiopian patterns of adaptation to high-altitude hypoxia. Integr Comp Biol 2006;46:18–24. 10.1093/icb/icj004 [DOI] [PubMed] [Google Scholar]
- 10. Mallet RT, Burtscher J, Richalet JP, et al. Impact of high altitude on cardiovascular health: current perspectives. Vasc Health Risk Manag 2021;17:317–35. 10.2147/VHRM.S294121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kious BM, Bakian A, Zhao J, et al. Altitude and risk of depression and anxiety: findings from the intern health study. Int Rev Psychiatry 2019;31:637–45. 10.1080/09540261.2019.1586324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wang F, Liu S, Zhang Q, et al. Prevalence of depression in older nursing home residents in high and low altitude regions: a comparative study. Front Psychiatry 2021;12:669234. 10.3389/fpsyt.2021.669234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Song C, Chongsuvivatwong V, Wangdui S, et al. Coverage and effectiveness of hypertension screening in different altitudes of Tibet autonomous region. BMC Public Health 2021;21:33. 10.1186/s12889-020-09858-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Graham C, Zhou S, Zhang J. Happiness and health in China: the paradox of progress. World Dev 2017;96:231–44. 10.1016/j.worlddev.2017.03.009 [DOI] [Google Scholar]
- 15. Huang L, Wang Z, Wang H, et al. Nutrition transition and related health challenges over decades in China. Eur J Clin Nutr 2021;75:247–52. 10.1038/s41430-020-0674-8 [DOI] [PubMed] [Google Scholar]
- 16. Huang W, Yu H, Liu C, et al. Assessing health-related quality of life of Chinese adults in Heilongjiang using EQ-5D-3L. Int J Environ Res Public Health 2017;14:224. 10.3390/ijerph14030224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Si L, Shi L, Chen M, et al. Establishing benchmark EQ-5D-3L population health state utilities and identifying their correlates in Gansu province, China. Qual Life Res 2017;26:3049–58. 10.1007/s11136-017-1614-5 [DOI] [PubMed] [Google Scholar]
- 18. Tan Z, Liang Y, Liu S, et al. Health-related quality of life as measured with EQ-5D among populations with and without specific chronic conditions: a population-based survey in Shaanxi province, China. PLoS ONE 2013;8:e65958. 10.1371/journal.pone.0065958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Deng X, Dong P, Zhang L, et al. Health-related quality of life in residents aged 18 years and older with and without disease: findings from the first provincial health services survey of Hunan, China. BMJ Open 2017;7:e015880. 10.1136/bmjopen-2017-015880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yao Q, Liu C, Zhang Y, et al. Changes in health-related quality of life of Chinese populations measured by the EQ-5D-3 L: a comparison of the 2008 and 2013 national health services surveys. Health Qual Life Outcomes 2019;17:43. 10.1186/s12955-019-1109-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wang D, Xie S, Wu J, et al. The trend in quality of life of Chinese population: analysis based on population health surveys from 2008 to 2020. BMC Public Health 2023;23:167. 10.1186/s12889-023-15075-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Brooks R. Euroqol: the current state of play. Health Policy 1996;37:53–72. 10.1016/0168-8510(96)00822-6 [DOI] [PubMed] [Google Scholar]
- 23. Liu GG, Wu H, Li M, et al. Chinese time trade-off values for EQ-5D health States. Value Health 2014;17:597–604. 10.1016/j.jval.2014.05.007 [DOI] [PubMed] [Google Scholar]
- 24. Zhuo L, Xu L, Ye J, et al. Time trade-off value set for EQ-5D-3L based on a nationally representative Chinese population survey. Value Health 2018;21:1330–7. 10.1016/j.jval.2018.04.1370 [DOI] [PubMed] [Google Scholar]
- 25. Liu GG, Guan H, Jin X, et al. Rural population's preferences matter: a value set for the EQ-5D-3L health states for China's rural population. Health Qual Life Outcomes 2022;20:14. 10.1186/s12955-022-01917-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zhang R-Y, Wang W, Zhou H-J, et al. A head-to-head comparison of the EQ-5D-3L index scores derived from the two EQ-5D-3L value sets for China. Health Qual Life Outcomes 2022;20:80. 10.1186/s12955-022-01988-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sun S, Chen J, Johannesson M, et al. Regional differences in health status in China: population health-related quality of life results from the national health services survey 2008. Health Place 2011;17:671–80. 10.1016/j.healthplace.2011.01.007 [DOI] [PubMed] [Google Scholar]
- 28. Woolcott OO, Ader M, Bergman RN. Glucose homeostasis during short-term and prolonged exposure to high altitudes. Endocr Rev 2015;36:149–73. 10.1210/er.2014-1063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tibet Autonomous Region Tourism Development Office . Tibet’s first geographic census; 2017.
- 30. The Ministry of Labor and Personnel and the Ministry of Finance . The Ministry of labor and personnel and the Ministry of finance responded to the people’s government of Tibet autonomous region on issues concerning the implementation of temporary subsidies for workers in plateau areas; 1984.
- 31. Cohen J. A power primer. Psychol Bull 1992;112:155–9. 10.1037//0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- 32. Pan C-W, Zhang R-Y, Luo N, et al. How the EQ-5D utilities are derived matters in Chinese diabetes patients: a comparison based on different EQ-5D scoring functions for China. Qual Life Res 2020;29:3087–94. 10.1007/s11136-020-02551-0 [DOI] [PubMed] [Google Scholar]
- 33. Yao Q, Liu C, Zhang Y, et al. Population norms for the EQ-5D-3L in China derived from the 2013 national health services survey. J Glob Health 2021;11:08001. 10.7189/jogh.11.08001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Walters SJ, Brazier JE. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res 2005;14:1523–32. 10.1007/s11136-004-7713-0 [DOI] [PubMed] [Google Scholar]
- 35. National Health Commission . 2021 China Health Statistics Yearbook. Beijing: China Union Medical University Press, 2022. [Google Scholar]
- 36. Netzer N, Strohl K, Faulhaber M, et al. Hypoxia-related altitude illnesses. J Travel Med 2013;20:247–55. 10.1111/jtm.12017 [DOI] [PubMed] [Google Scholar]
- 37. Crawford JE, Amaru R, Song J, et al. Natural selection on genes related to cardiovascular health in high-altitude adapted Andeans. Am J Hum Genet 2017;101:752–67. 10.1016/j.ajhg.2017.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Deng R, Labasangzhu, Zhaxideji, et al. Illness prevalence rate in Tibet, China: data from the 2018 national health service survey. BMC Public Health 2020;20:955. 10.1186/s12889-020-08960-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Li K, Liang Y, Sun Y, et al. The relationship between polymorphisms at 17 gene sites and hypertension among the aboriginal Tibetan people. Biomed Environ Sci 2012;25:526–32. 10.3967/0895-3988.2012.05.005 [DOI] [PubMed] [Google Scholar]
- 40. Wang J, Zhang L, Wang F, et al. Prevalence, awareness, treatment, and control of hypertension in China: results from a national survey. Am J Hypertens 2014;27:1355–61. 10.1093/ajh/hpu053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wu T. The Qinghai-Tibetan plateau: how high do Tibetans live High Alt Med Biol 2001;2:489–99. 10.1089/152702901753397054 [DOI] [PubMed] [Google Scholar]
- 42. Jiang Y, Hesser JE. Associations between health-related quality of life and demographics and health risks. Results from Rhode Island's 2002 behavioral risk factor survey. Health Qual Life Outcomes 2006;4:14. 10.1186/1477-7525-4-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Matthews KA, Gallo LC. Psychological perspectives on pathways linking socioeconomic status and physical health. Annu Rev Psychol 2011;62:501–30. 10.1146/annurev.psych.031809.130711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Golicki D, Niewada M, Jakubczyk M, et al. Self-assessed health status in Poland: EQ-5D findings from the Polish valuation study. Pol Arch Med Wewn 2010;120:276–81. 10.20452/pamw.945 [DOI] [PubMed] [Google Scholar]
- 45. Gamboa JL, Caceda R, Arregui A. Is depression the link between suicide and high altitude High Alt Med Biol 2011;12:403–4; 10.1089/ham.2011.1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wang J, Zhou Y, Liang Y, et al. A large sample survey of Tibetan people on the Qinghai-Tibet plateau: current situation of depression and risk factors. Int J Environ Res Public Health 2019;17:17. 10.3390/ijerph17010289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ding Y, Shi B, Su G, et al. Assessing suitability of human settlements in high-altitude area using a comprehensive index method: a case study of Tibet, China. Sustainability 2021;13:1485. 10.3390/su13031485 [DOI] [Google Scholar]
- 48. Li XY, Wu XY, Fu C, et al. Effects of acute mild and moderate hypoxia on human mood state. Space Med Med Eng (Beijing) 2000;13:1–5. [PubMed] [Google Scholar]
- 49. Chen Y, Zhang G, Chen Z, et al. A warming climate may reduce health risks of hypoxia on the Qinghai-Tibet plateau. Sci Bull (Beijing) 2022;67:341–4. 10.1016/j.scib.2021.10.003 [DOI] [PubMed] [Google Scholar]
- 50. Woo E, Kim H, Uysal M. Life satisfaction and support for tourism development. Ann Tour Res 2015;50:84–97. 10.1016/j.annals.2014.11.001 [DOI] [Google Scholar]
- 51. Vargas-Sánchez A, Plaza-Mejía M de los Á, Porras-Bueno N. Understanding residents' attitudes toward the development of industrial tourism in a former mining community. J Travel Res 2009;47:373–87. 10.1177/0047287508322783 [DOI] [Google Scholar]
- 52. Aref F. The effects of tourism on quality of life: a case study of Shiraz, Iran. Life Sci J 2011;8:26–30. 10.7537/marslsj080211.05 [DOI] [Google Scholar]
- 53. Andereck KL, Nyaupane GP. Exploring the nature of tourism and quality of life perceptions among residents. J Travel Res 2011;50:248–60. 10.1177/0047287510362918 [DOI] [Google Scholar]
- 54. Andereck KL, Valentine KM, Knopf RC, et al. Residents' perceptions of community tourism impacts. Ann Tour Res 2005;32:1056–76. 10.1016/j.annals.2005.03.001 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-072854supp001.pdf (76.5KB, pdf)
Data Availability Statement
Data are available on reasonable request. We have included all the data produced in the present work in the manuscript. Note that the raw data used in the study were obtained from National Health Service Surveys of China. We are unable to attach all the raw data for each participant in this paper due to the ethical restrictions.