Abstract
Background
Tibial intramedullary nailing is a common method of fixation for fractures of the tibia, with several approaches described. Anterior knee pain is a common complication following nailing, but the reported incidence of knee pain varies in the literature between 10 % and 86 %. There is considerable variation in incidence between nailing techniques, with an exact aetiology still unknown. We investigated the reported incidence of anterior knee pain in patients undergoing tibial nailing using the semi-extended extra synovial (SEES) technique at a Major Trauma Centre (MTC) in the UK.
Methods
A retrospective review of tibial fractures treated with the SEES technique between December 2012 to February 2021. Data collected included patient demographics, mechanism of injury, fracture characteristics, length of stay, union rates and re-operation rates. Primary outcomes were anterior knee pain rates and patient reported outcome measures (PROM), the Kujala Score. Secondary outcomes were rates of union and complications.
Results
55 fractures were identified in 53 patients. Male: Female ratio was 32:21. The average age was 45.5 years. 96 % were unilateral fractures; with 53 % being right-sided. 21(38 %) fractures were open. Prior to definitive nailing 21 fractures had temporary stabilisation with an external fixator (Ex-Fix) ± wound debridement whilst the rest received plaster backslab immobilisation. 13 of the open fractures required soft tissue cover. 75 % of patients had initial surgery (SEES Nailing/Ex-Fix) within 4 days. There was a 91 % union rate with a median time to full radiographic union of 14 months. One post-operative complication of wound dehiscence was recorded. The mean follow-up time was 13.6 months. 15 % of patients reported anterior knee pain in the postoperative follow-up period. The average Kujala PROM score was 85 (Range: 52–100)
Conclusion/findings
The SEES technique had favourable PROM scores and displayed a lower incidence of anterior knee pain than the traditional infrapatellar approach. Knee pain rates were comparable to suprapatellar approaches without violating the knee joint.
Disclosures
None.
Keywords: Semi-extended extra synovial approach, Tibia, Intramedullary nailing, Kujala score, Anterior knee pain, PROMs, Kubiak
1. Introduction
Tibial fractures are one of the most common long bone fractures and cause significant morbidity.1,2 Tibial fractures occur as part of both high and low energy trauma, with a significant proportion being open, resulting in a substantial economic burden and impact on patients and healthcare institutions.3
The method of fixation of a tibial fracture depends on various factors such as fracture location and pattern, patient factors and soft tissue status of the affected limb. The goal of management is to promote rehabilitation by restoration of alignment and stability, permitting early weight bearing and joint mobilisation while union progresses. Intramedullary fixation of tibial shaft fractures has become the predominant technique for stabilisation.4 Implants have undergone several changes from the original first-generation nails to the enhanced locking options of modern designs. These changes have led to intramedullary nailing becoming the preferred treatment of choice in a wider range of fracture patterns.5,6
Post-operative anterior knee pain is a common complication following intramedullary nailing of the tibia.7,8 Anterior knee pain is common with the traditional infrapatellar approach, rates vary between 10 and 80 %8, 9, 10 with Katsoulis et al. reporting a mean incidence of 47.4 % after a mean follow up of 23.9 months in their literature review.8 Many authors, over the years, have tried to investigate the cause of anterior knee pain, but the exact source remains unclear.8,9,11, 12, 13, 14, 15 In the infrapatellar approach, either patellar tendon splitting or medial parapatellar access has predominated, but both routes have resulted in similarly high rates of anterior knee pain.9,11,16, 17, 18, 19, 20 Alternative surgical approaches have been described, such as the supra-patellar and the semi-extended extra synovial (SEES) approaches, where the knee is far less flexed than in the infra-patellar technique which makes patient positioning easier and reduces sagittal deforming forces on the fracture. Several studies have reported the incidence of anterior knee pain with these semi-extended approaches.7,18,19,21, 22, 23, 24, 25, 26 The suprapatellar technique has low reported rates of anterior knee pain with pooled estimates as low as 10 %.16 Tornetta described a semi-extended technique of tibial nailing via an arthrotomy with the patella everted.21 Kubiak et al. later described the SEES modification of Tornetta's technique to access to the nail entry point without breaching the synovial membrane.27 The senior authors (RK and JC) have used the SEES technique for tibial nailing in our centre for the last 10 years because it does not breach the knee joint-space and can be performed using standard nailing instrumentation while retaining the advantages of the semi-extended position.
This retrospective study aimed to evaluate the incidence of anterior knee pain amongst other outcomes such as time to union and patient-reported outcomes using the Kujala score in patients treated with the SEES technique.
2. Methods
We undertook a retrospective review of patients with tibial fractures treated with the SEES approach for intramedullary nailing in our hospital, an adult Major Trauma Centre. We identified patients using a procedural code for tibia nailing through the hospital informatics system from December 2012 to February 2021. A total of 537 patients were identified who had Tibia nailing performed for tibial fractures, of which 53 patients (55 operations) were managed using the SEES technique. We used the hospital's electronic clinical data system to collect the clinical information and the hospital PACS system (Carestream) to review patient's radiographs. Patient clinical data collected were patient demographics, mechanism of injury, fracture characteristics, length of stay, union rates and reoperation rates. Patients were contacted via telephone during the data collection period. They were asked to complete a 13 point Kujala questionnaire which has previously been validated to evaluate anterior knee pain.28 The Kujala score is out of 100—a patient with no anterior knee pain symptoms would score 100/100. Primary outcomes were Kujala scores and rates of anterior knee pain. Secondary outcomes were rates of union and complications. The study was registered with the local Research and Audit department, and ethical approval was not required. Informed consent was taken from one patient prior to the procedure for intraoperative pictures to be taken and for their use in publication.
3. Technique
The patient is positioned supine on the operating table with a radiolucent extension for fluoroscopy imaging intra-operatively. A suitably shaped radiolucent support is placed under the limb to position the knee in about 20° flexion (semi-extended) (Fig. 1). The image intensifier is checked in both sagittal and coronal planes to ensure easy access to the whole tibia is available. A tourniquet is not used. Standard surgical skin preparation is made with the leg draped free.
Fig. 1.
The limb has been prepped and draped and has been positioned semi extended in 20° of flexion. Lateral based incision has been marked after assessing patella mobility. (P- Proximal, D-Distal).
The SEES technique considers patella mobility and can be adapted to either a medial or lateral-based incision, however as in all cases the authors have found a lateral based incision to be most appropriate. The succeeding description assumes a lateral release. An incision is made over the lateral aspect of the patella, slightly curving at the lower end along the contour of the patella. After superficial dissection (Fig. 2), the patella retinaculum is incised near the patella border, leaving a cuff for repair, and elevated from the underlying synovium with blunt dissection taking care not to breach the synovium (Fig. 3). At this point, if the synovium is inadvertently breached, it is repaired with absorbable sutures to avoid bone debris entering the joint and to protect the articular surface of the trochlea. A channel is created in the soft tissues posterior to the patella tendon with blunt dissection down to the proximal tibia entry point. To align instrumentation with the tibial shaft, the patella is displaced medially after the retinacular release. A guide wire is inserted and the position is checked with fluoroscopy. The fracture is reduced in sagittal and coronal planes before the guide wire is passed into the distal fragment. A soft tissue protector can be used if desired. The rest of the procedure (nail insertion and distal locking) is performed as with other techniques. The wound is irrigated and the synovial membrane is checked again for any breaches before repairing the lateral retinaculum. Post-operatively there are no restrictions to knee joint range of movement and immediate weight bearing is allowed using crutches as tolerated. Venous thromboprophylaxis is administered according to our hospital protocol. The patient is reviewed at 6 weeks in fracture clinic for post operative radiographs. The patient is kept under regular review until clinical and radiographic union.
Fig. 2.
After superficial dissection, the patella retinaculum can be seen in the picture. This is incised at the lateral border of the patella leaving a cuff for repair. (P- Proximal, D-Distal).
Fig. 3.
The intact synovium overlying the trochlea of the femur can be seen after the patella retinaculum has been divided. (P- Proximal, D-Distal).
4. Results
537 patients were identified who had tibial fractures treated with Intramedullary tibial nailing (Supra-patella, Infra-patella and SEES) between December 2012 and February 2021. 55 fractures in 53 consecutive patients underwent intramedullary nailing with the SEES technique.
Table 1 displays the demographic data; there were 21 females and 32 males with an average age of 45.5 years. 2 patients (4 %) had bilateral fractures. Prior to definitive nailing procedure, 21 tibial fractures had an application of an external fixator with wound debridement as indicated with the other 34 fractures splinted in a Plaster of Paris backslab. There were no neurovascular injuries associated with the tibial fractures preoperatively. The patients’ co-morbidities are displayed in Table 2.
Table 1.
Cohort demographic data.
| Patient Demographics | Total |
|---|---|
| Sex | |
| Male | 32 |
| Female | 21 |
| Age (yrs) | |
| Average | 45.5 |
| Range | 20–83 |
| Laterality | |
| Right | 29 |
| Left | 26 |
| Open/Closed | |
| Open Fractures | 21 |
| Closed Fractures | 34 |
| Initial Management | |
| Plaster of Paris Backslab | 34 |
| External Fixation | 21 |
| Length of Stay (days) | |
| Average | 17 |
| Range | 2–67 |
| ITU admission | |
| Average length of stay (days) | 8.1 |
| Range | 2–16 |
| Total no of patients | 10 |
| Discharge Destination | |
| Home | 38 |
| Other (RLH/NH) | 15 |
| Follow-up (months) | |
| Average | 13.6 |
| Range | 3–55 |
| Evidence of Union | |
| Union | 50 |
| Median time to union (months) | 14 |
| Non-union | 5 |
| Post op Complications | |
| Wound Dehiscence | 1 |
| Non-union | 5 |
| Reason for Reoperation | |
| Prominent metalwork | 1 |
| Non-union | 5 |
| Total | 6 |
Table 2.
Co-Morbidities of patients presenting with tibial fracture.
| Co-Morbidities | |
|---|---|
| HTN | 4 |
| DM | 2 |
| COPD/Asthma | 1 |
| Hypothyroidism | 1 |
| Chronic Renal Failure | 1 |
| IHD | 1 |
| CVA | 1 |
| Malignancy | 2 |
| Mental Health | 1 |
| Visual impairment | 1 |
| Epilepsy | 2 |
| ETOH Dependence | 1 |
| IBS/GORD | 2 |
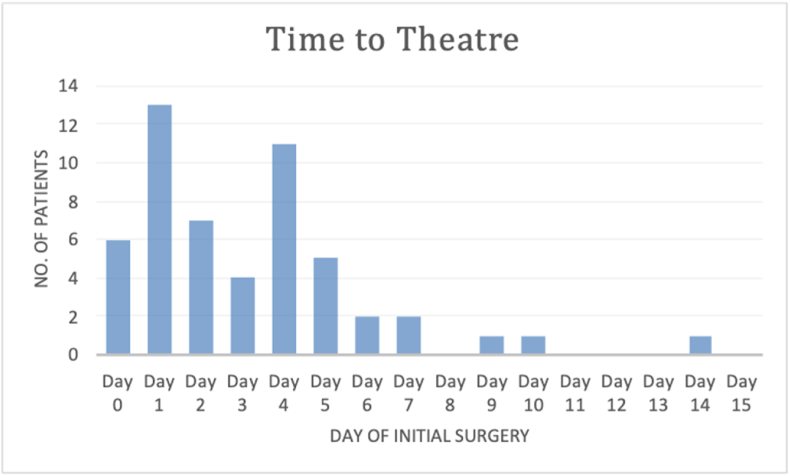
Most fractures were sustained following a high-energy mechanism; road traffic collision with pedestrian vs car being the commonest mechanism (Table 3). 34 were isolated tibial fractures, while 21 were poly-trauma patients with other associated injuries. 75 % of patients had their initial surgery (SEES Nailing/Ex-Fix) within 4 days (Fig. 4). The average length of hospitalisation was 17 days.
Table 3.
Mechanism of injury for tibial fractures.
| Mechanism of Injury | Total |
|---|---|
| Fall - Low Energy | 19 |
| Fall - High Energy | 1 |
| RTC | 30 |
| Pedestrian vs Car | 16 |
| Car vs Car | 1 |
| Car vs Object | 1 |
| Motorcycle/Bike vs car | 9 |
| Motorcycle/Bike vs Object | 1 |
| Other (Quadbike) | 2 |
| Crush | 3 |
| Sporting Injury | 2 |
Fig. 4.
Time to initial surgery following admission with tibial fracture (SEES/Ex-Fix).
Table 4 displays fracture morphology and characteristics. The majority of fractures were in the middle and distal thirds. Five fractures had an intra-articular extension of the fracture line. Two were located in the distal third extending into the ankle joint, two were at the junction of middle-distal thirds extending into the ankle joint, and one was in the proximal third extending up towards the tibial plateau.
Table 4.
Tibial fracture location and fracture morphology.
| Fracture Location | Total |
|---|---|
| Proximal Third | 2 |
| Middle Third | 21 |
| Distal Third | 17 |
| Junction Proximal-Middle Third | 0 |
| Junction Middle-Distal Third | 15 |
| Total | 55 |
| Intra Articular Extension | |
| Proximal Third | 1 |
| Junction Middle-Distal Third | 2 |
| Distal Third | 2 |
| Total | 5 |
| Fracture morphology | |
| Complex fragmented | 4 |
| Complex segmental | 7 |
| Complex spiral | 4 |
| Bending wedge | 1 |
| Fragmented wedge | 4 |
| Spiral wedge | 3 |
| Simple transverse | 7 |
| Simple spiral | 15 |
| Simple Oblique | 9 |
| Other (Periprosthetic) | 1 |
There were 21 open fractures managed according to the British Orthopaedic Association Standards for Trauma (BOAST) principles by senior Orthopaedic and Plastic surgeons. 8 of the open fractures patients (38 %) had wounds primarily closed after debridement while 13 (62 %) required reconstruction of their wounds with either local or free flap coverage by the Plastic surgeons (Table 5). 52 patients (96 %) received reamed intramedullary nailing.
Table 5.
Open tibial fractures-location and soft tissue coverage.
| Open Fractures | Total |
|---|---|
| No Soft tissue Coverage | 8 |
| Soft tissue Coverage | 13 |
| Total | 21 |
| Location | |
| Middle 1/3 | 10 |
| Distal 1/3 | 7 |
| Junction Middle-Distal 1/3 | 4 |
The Median follow-up time was 8 (3–55) months for the patients that attended follow-up appointments.
Six patients required reoperation (Table .1). One patient had a post-operative wound infection and five had evidence of non-union. Three of the non unions were in patients who sustained open fractures, of which one non-union was suspected to be an infected non-union. The Follow up range for the non unions was between 19 and 41 months. With input from our limb reconstruction team, all non-unions were successfully managed using either a circular frame or exchange nailing.
Post-operative radiographs were evaluated for union and alignment. There was a median time of 14 months for radiological union of tibial fractures. Three (5 %) fractures had evidence of varus/valgus malalignment.
Eight patients (15 %) out of the original cohort of 53 patients reported symptoms of anterior knee pain or pain on kneeling during their follow-up appointments or during telephone review questioning. 34 patients out of the original 53 agreed to provide Kujala scores following their operation. 2 patients had deceased, and the rest were not contactable, refused to provide scores or were lost to follow-up. For the 34 patients that provided responses, the mean Kujala score was 85 out of 100 with a median of 94 (52–100, standard deviation 15).
5. Discussion
Whilst chronic anterior knee pain is one of the most common complications of tibial nailing, the incidence following intramedullary nailing is variable and a wide range has been reported amongst studies comparing tibial nailing techniques.8,9,12,16,29,30
Katsoulis et al. reported a mean incidence of 48 % for anterior knee pain with a range of 10–86 % across the retrospective and prospective studies included in their review.8,9
The incidence of anterior knee pain reported in this study is only 15 %, which is much lower than the reported mean of Katsoulis et al.
Whilst traditional infrapatellar approaches for nailing the tibia are effective and well documented, nailing of proximal tibial metaphyseal-diaphyseal junction fractures is more challenging and difficult owing to fracture displacement secondary to the quadriceps muscle deforming force and the hyperflexed position of the knee necessary for entry point establishment.31 More recently, semi-extended approaches have become more popular, offering the benefits of easier patient positioning, fracture reduction, intraoperative fluoroscopic assessment, and implant insertion whilst at the same time reducing post-operative knee pain.7,11,18,19,25,26,32,33 Sepehri and Packer et al. documented favourable outcomes when using the suprapatellar technique and superior Lysholm scores for the suprapatellar approach with no increase in operative time or difference in complication rates.25,26 Macdonald et al. compared suprapatellar and infrapatellar approaches through the Aberdeen Weightbearing Test – Knee (AWT-K) score showing the superiority of the suprapatellar approach in reducing postoperative anterior knee pain in their multicentre clinical trial.7 Leliveld et al. showed that pooled estimates of anterior knee pain were lower with a suprapatellar approach, but functional outcomes were similar across different techniques.16
Although there are several studies regarding the supra and infrapatellar approaches, little is documented in the literature about the longer-term outcomes of the SEES technique.
Rothberg et al. assessed rates of anterior knee pain following tibial nailing with a lateral semi-extended extra-articular parapatellar approach and found at one-year follow-up no significant increase in anterior knee pain compared to their uninjured control group. Stella et al. showed low rates of anterior knee pain and favourable Lysholm scores in their prospective cohort study.34 These findings appear to be consistent with the data presented in this study. Our cohort of patients demonstrated favourable anterior knee pain incidence using the Kujala Scoring system. The average Kujala score was 84/100 and the median score was 94/100, with only 15 % of all patients reporting anterior knee pain. Given that a high proportion of tibial fractures in our cohort is secondary to high energy trauma, the low rate of anterior knee pain with the SEES technique is encouraging.
Alongside the comparable function and anterior knee pain rates to other methods of intramedullary nailing we feel that the SEES offers additional benefits over other techniques. Injured limb positioning is much easier, facilitating the rest of the procedure. We found that the fracture reduction and maintenance of the reduction throughout the procedure is more effective with this technique, and little help is needed from the surgical assistant. In addition, the positioning of the image intensifier is more straightforward and fluoroscopic examinations can be performed more efficiently due to the position of the limb on the table.31 This technique is ideal for proximal fractures as traditional techniques where the knee has to be flexed to gain access to the entry point result in displacement of the proximal fragment which does not occur with the semi-extended technique. By keeping the leg in the extended position this helps facilitate reduction the proximal fragment more anatomically. The SEES technique also doesn't require significant hip flexion, making it ideal in patients with associated pelvic and acetabular fractures, specifically where flexion of the hip is difficult or contraindicated due to the nature of their injuries. The SEES approach has the same positional benefits as suprapatellar nailing but utilises the same standard equipment as infrapatellar nailing and thus does not require additional investment or equipment storage.
Although the exact aetiology of anterior knee pain remains unknown, damage to the infrapatellar fat pad and inferior branch of the saphenous nerve are thought to be the most common cause of anterior knee pain. Other theories range from damage to the patella tendon or the Hoffa's fat pad and anterior placement of the nail irritating the patella and causing chondromalacia.7,15,35, 36, 37 Benefits of protecting these structures was shown by Weil et al. who demonstrated a chronic anterior knee pain incidence of 18 % in their cohort when performing a lateral parapatellar approach with preservation and atraumatic elevation of the infrapatellar fat pad.30 The incidence of anterior knee pain in that study is consistent with our cohort and this is likely due to the fact that the SEES technique avoids contamination of the knee joint and avoids/causes little damage to these potential structures. Unlike the suprapatellar approach there is no violation of the patello-femoral joint in the SEES technique, reducing direct pressure on the articular cartilage and potential chondral damage that may occur if not done with care or in case of failure of the supra-patellar instruments37
6. Limitations
Overall the group of patients was quite heterogeneous as demonstrated by the large age range (20–83), difference in injury mechanisms (high and low energy mechanisms) and open fractures. However whilst heterogenous this may make the results more generalisable to the wider population. The study's retrospective nature in data collection of patient-reported outcomes may have elements of recall bias.
7. Conclusion
Overall the SEES technique shows favourable outcomes in this group of patients. Kujala knee pain scores were favourable and the technique demonstrated lower rates of anterior knee pain compared to documented rates for the infrapatellar approach. Anterior knee pain rates were comparable to the suprapatellar approach whilst at the same time providing the additionally mentioned benefits. Finally, this technique may be safely considered in patients with a high risk of anterior knee pain or in those requiring to kneel as part of their daily activities.
Funding
No source of funding was utilised in the preparation of this article.
CRediT authorship contribution statement
Mohammed Junaid Choudri: Investigation, Formal analysis, Data curation, Writing – original draft, Writing – review & editing. Shakir Hussain: Conceptualization, Methodology, Writing – original draft. Sabri Bleibleh: Investigation, Formal analysis, Writing – review & editing. Mohammedabbas Remtulla: Investigation, Formal analysis, Writing – review & editing. Ravichandran Karthikeyan: Writing – review & editing, Supervision. Julian Cooper: Writing – review & editing, Supervision.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Court-Brown C.M., Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 2.Connelly C.L., Bucknall V., Jenkins P.J., Court-Brown C.M., McQueen M.M., Biant L.C. Outcome at 12 to 22 years of 1502 tibial shaft fractures. Bone Joint Lett J. 2014;96-B(10):1370–1377. doi: 10.1302/0301-620X.96B10.32914. [DOI] [PubMed] [Google Scholar]
- 3.Schade A.T., Khatri C., Nwankwo H., Carlos W., Harrison W.J., Metcalfe A.J. The economic burden of open tibia fractures: a systematic review. Injury. 2021;52(6):1251–1259. doi: 10.1016/j.injury.2021.02.022. [DOI] [PubMed] [Google Scholar]
- 4.Duan X., Al-Qwbani M., Zeng Y., Zhang W., Xiang Z. Intramedullary nailing for tibial shaft fractures in adults. Cochrane Database Syst Rev. 2012;1 doi: 10.1002/14651858.CD008241.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bong M.R., Kummer F.J., Koval K.J., Egol K.A. Intramedullary nailing of the lower extremity: biomechanics and biology. J Am Acad Orthop Surg. 2007;15(2):97–106. doi: 10.5435/00124635-200702000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Rosa N., Marta M., Vaz M., et al. Intramedullary nailing biomechanics: evolution and challenges. Proc Inst Mech Eng H. 2019;233(3):295–308. doi: 10.1177/0954411919827044. [DOI] [PubMed] [Google Scholar]
- 7.MacDonald D.R.W., Caba-Doussoux P., Carnegie C.A., et al. Tibial nailing using a suprapatellar rather than an infrapatellar approach significantly reduces anterior knee pain postoperatively: a multicentre clinical trial. The Bone Joint J. 2019;101-B(9):1138–1143. doi: 10.1302/0301-620X.101B9.BJJ-2018-1115.R2. [DOI] [PubMed] [Google Scholar]
- 8.Katsoulis E., Court-Brown C., Giannoudis P.V. Incidence and aetiology of anterior knee pain after intramedullary nailing of the femur and tibia. J Bone Joint Surg British. 2006;88-B(5):576–580. doi: 10.1302/0301-620X.88B5.16875. [DOI] [PubMed] [Google Scholar]
- 9.Toivanen J.A.K., Väistö O., Kannus P., Latvala K., Honkonen S.E., Järvinen M.J. Anterior knee pain after intramedullary nailing of fractures of the tibial shaft: a prospective, randomized study comparing two different nail-insertion techniques. J Bone Jt Surg Am Vol. 2002;84(4):580–585. doi: 10.2106/00004623-200204000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Lefaivre K.A., Guy P., Chan H., Blachut P.A. Long-term follow-up of tibial shaft fractures treated with intramedullary nailing. J Orthop Trauma. 2008;22(8):525–529. doi: 10.1097/BOT.0b013e318180e646. [DOI] [PubMed] [Google Scholar]
- 11.Ozcan C., Turkmen I., Sokucu S. Comparison of three different approaches for anterior knee pain after tibia intramedullary nailing. Eur J Trauma Emerg Surg. 2020;46(1):99–105. doi: 10.1007/s00068-018-0988-6. [DOI] [PubMed] [Google Scholar]
- 12.Pc S., Bs A.K., R R., Ba P.K. Anterior knee pain after tibial intra-medullary nailing: is it predictable? MOJ. 2016;10(2):16–20. doi: 10.5704/MOJ.1607.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leliveld M.S., Verhofstad M.H.J. Injury to the infrapatellar branch of the saphenous nerve, a possible cause for anterior knee pain after tibial nailing? Injury. 2012;43(6):779–783. doi: 10.1016/j.injury.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 14.Franke J., Brobeil A., Lips K.S., et al. Importance of mechanoreceptors and other neural structures within the anterior intermeniscal ligament in the etiology of anterior knee pain after tibial nailing. J Orthop Trauma. 2018;32(10):526–533. doi: 10.1097/BOT.0000000000001258. [DOI] [PubMed] [Google Scholar]
- 15.Chen C.Y., Lin K.C., Yang S.W., Tarng Y.W., Hsu C.J., Renn J.H. Influence of nail prominence and insertion point on anterior knee pain after tibial intramedullary nailing. Orthopedics. 2014;37(3):e221–e225. doi: 10.3928/01477447-20140225-52. [DOI] [PubMed] [Google Scholar]
- 16.Leliveld M.S., Verhofstad M.H.J., Van Bodegraven E., Van Haaren J., Van Lieshout E.M.M. Anterior knee pain and functional outcome following different surgical techniques for tibial nailing: a systematic review. Eur J Trauma Emerg Surg. 2021;47(3):763–772. doi: 10.1007/s00068-020-01458-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ahmad S, Ahmed A, Khan L, Javed S, Ahmed N, Aziz A. Comparative analysis of anterior knee pain in TRANSPATELLAR and medial parapatellar tendon approaches in tibial interlocking nailing. J Ayub Med Coll Abbottabad.:4. [PubMed]
- 18.Sanders R.W., DiPasquale T.G., Jordan C.J., Arrington J.A., Sagi H.C. Semiextended intramedullary nailing of the tibia using a suprapatellar approach: radiographic results and clinical outcomes at a minimum of 12 Months follow-up. J Orthop Trauma. 2014;28(5):11. doi: 10.1097/BOT.0000000000000082. [DOI] [PubMed] [Google Scholar]
- 19.Serbest S., Tiftikçi U., Çoban M., Çirpar M., Dağlar B. Knee pain and functional scores after intramedullary nailing of tibial shaft fractures using a suprapatellar approach. J Orthop Trauma. 2019;33(1):37–41. doi: 10.1097/BOT.0000000000001337. [DOI] [PubMed] [Google Scholar]
- 20.Bakhsh W.R., Cherney S.M., McAndrew C.M., Ricci W.M., Gardner M.J. Surgical approaches to intramedullary nailing of the tibia: comparative analysis of knee pain and functional outcomes. Injury. 2016;47(4):958–961. doi: 10.1016/j.injury.2015.12.025. [DOI] [PubMed] [Google Scholar]
- 21.Tornetta P., Collins E. Semiextended position of intramedullary nailing of the proximal tibia. Clin Orthop Relat Res. 1996;328:185–189. doi: 10.1097/00003086-199607000-00029. [DOI] [PubMed] [Google Scholar]
- 22.Cazzato G., Saccomanno M.F., Noia G., et al. Intramedullary nailing of tibial shaft fractures in the semi-extended position using a suprapatellar approach: a retrospective case series. Injury. 2018;49:S61–S64. doi: 10.1016/j.injury.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 23.Rothberg D.L., Daubs G.M., Horwitz D.S., Kubiak E.N. One-year postoperative knee pain in patients with semi-extended tibial nailing versus control group. Orthopedics. 2013;36(5) doi: 10.3928/01477447-20130426-14. [DOI] [PubMed] [Google Scholar]
- 24.Ryan S.P., Steen B., Tornetta P. Semi-extended nailing of metaphyseal tibia fractures: alignment and incidence of postoperative knee pain. J Orthop Trauma. 2014;28(5):7. doi: 10.1097/BOT.0000000000000083. [DOI] [PubMed] [Google Scholar]
- 25.Sepehri A, You D, Lobo AA, Schneider P, Lefaivre KA, Guy P. Comparison of patient reported outcomes following suprapatellar versus infrapatellar nailing techniques for tibial shaft fractures: a systematic review and meta-analysis. J Orthop Trauma. Published online November 15, 2021. doi:10.1097/BOT.0000000000002303. [DOI] [PubMed]
- 26.Packer T.W., Naqvi A.Z., Edwards T.C. Intramedullary tibial nailing using infrapatellar and suprapatellar approaches: a systematic review and meta-analysis. Injury. 2021;52(3):307–315. doi: 10.1016/j.injury.2020.09.047. [DOI] [PubMed] [Google Scholar]
- 27.Kubiak E.N., Widmer B.J., Horwitz D.S. Extra-articular technique for semiextended tibial nailing. J Orthop Trauma. 2010;24(11):704–708. doi: 10.1097/BOT.0b013e3181d5d9f4. [DOI] [PubMed] [Google Scholar]
- 28.Watson C.J., Propps M., Ratner J., Zeigler D.L., Horton P., Smith S.S. Reliability and responsiveness of the lower extremity functional scale and the anterior knee pain scale in patients with anterior knee pain. J Orthop Sports Phys Ther. 2005;35(3):136–146. doi: 10.2519/jospt.2005.35.3.136. [DOI] [PubMed] [Google Scholar]
- 29.Ahmad I. Mortality and morbidity in elderly patients with fracture neck of femur treated by hemiarthroplasty. J College Phys Surg–Pakistan : JCPSP. 2006;16(10):655–658. doi: 10.2006/JCPSP.655658. [DOI] [PubMed] [Google Scholar]
- 30.Weil Y.A., Gardner M.J., Boraiah S., Helfet D.L., Lorich D.G. Anterior knee pain following the lateral parapatellar approach for tibial nailing. Arch Orthop Trauma Surg. 2009;129(6):773–777. doi: 10.1007/s00402-008-0678-7. [DOI] [PubMed] [Google Scholar]
- 31.Hiesterman T.G., Shafiq B.X., Cole P.A. Intramedullary nailing of extraarticular proximal tibia fractures. American Acad Orthopaedic Surg. 2011;19(11):690–700. doi: 10.5435/00124635-201111000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Patel A.H., Wilder J.H., Lee O.C., et al. A review of proximal tibia entry points for intramedullary nailing and validation of the lateral parapatellar approach as extra-articular. Orthop Rev. 2022;14(1) doi: 10.52965/001c.31909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang C., Chen E., Ye C., Pan Z. Suprapatellar versus infrapatellar approach for tibia intramedullary nailing: a meta-analysis. Int J Surg. 2018;51:133–139. doi: 10.1016/j.ijsu.2018.01.026. [DOI] [PubMed] [Google Scholar]
- 34.Stella M., Santolini E., Felli L., Santolini F., Horwitz DS. k. J Orthop Trauma. 2019;33(10):e366–e371. doi: 10.1097/BOT.0000000000001554. [DOI] [PubMed] [Google Scholar]
- 35.Weninger P., Schultz A., Traxler H., Firbas W., Hertz H. Anatomical assessment of the Hoffa fat pad during insertion of a tibial intramedullary nail--comparison of three surgical approaches. J Trauma. 2009;66(4):1140–1145. doi: 10.1097/TA.0b013e318169cd4d. [DOI] [PubMed] [Google Scholar]
- 36.Devitt A.T., Coughlan K.A., Ward T., et al. Patellofemoral contact forces and pressures during intramedullary tibial nailing. Int Orthop. 1998;22(2):92–96. doi: 10.1007/s002640050216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zelle B.A. Intramedullary nailing of tibial shaft fractures in the semi-extended position using a suprapatellar portal technique. Int Orthop. 2017;41(9):1909–1914. doi: 10.1007/s00264-017-3457-7. [DOI] [PubMed] [Google Scholar]