1. Introduction
A significant challenge that ENT surgeons often encounter is managing intraoperative bleeding, a task that requires precision, adept judgment, and a thorough knowledge of the latest techniques and procedures [1].
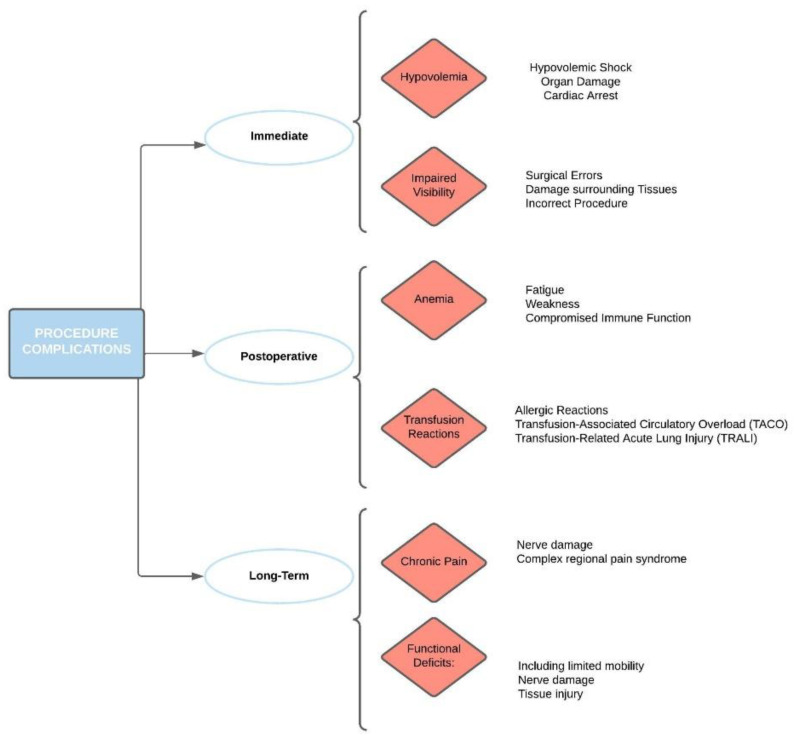
Intraoperative bleeding management is critical as it directly impacts surgical visualization, the duration of the procedure, and, most importantly, patient safety. When it comes to pediatric patients, these factors take on even greater significance due to the physiological differences and lower blood volume compared to adults, which make children more susceptible to the adverse effects of blood loss [2]. Pediatric patients present unique challenges in terms of blood volume and hemodynamic stability. Given their smaller blood volumes, children are potentially more susceptible to the effects of significant blood loss, which can rapidly lead to hemodynamic instability and hypovolemic shock [3] (Figure 1).
Figure 1.
Procedure-related complications and relative comorbidities.
Excessive bleeding obscures the surgical field, rendering it more difficult for the surgeon to navigate and potentially increases the risk of inadvertent damage to surrounding structures. It is worth noting that the sources of bleeding during otolaryngological procedures can vary widely, from larger vessels that can be directly sutured or clamped, to diffuse capillary oozing from the mucosa that might be more appropriately managed with topical hemostatic agents or cautery.
Therapeutic Management
Several strategies are often employed to manage intraoperative bleeding in pediatric otolaryngology surgeries. These might include the use of electrocautery, laser technology, radiofrequency ablation, and ultrasonic energy devices for their precision and ability to minimize tissue damage (Table 1).
Table 1.
Different techniques described in literature for intraoperative bleeding.
| Method | Description | Advantages | Disadvantages |
|---|---|---|---|
| Electrocautery | Uses electric current to coagulate tissue and stop bleeding. | Widely available and effective in achieving hemostasis. | Risk of thermal injury to surrounding tissues, smoke production. |
| Laser Technology | Uses focused light to cut or coagulate tissue. | High precision, minimal tissue damage. | Requires safety precautions to prevent eye injury and fire, expensive. |
| Radiofrequency Ablation | Uses radiofrequency energy to coagulate tissue. | Minimal tissue damage and less smoke production compared to electrocautery. | Can be slower than other methods, expensive. |
| Ultrasonic Energy Devices | Uses ultrasonic vibrations to cut and coagulate tissue. | Fast, minimal tissue damage, no smoke production. | Potential for unintended tissue damage if not used properly, expensive. |
| Topical Hemostatic Agents | These include gels, foams, and bandages that promote clotting. | Can be used in conjunction with other methods, useful for minor bleeding. | Not effective for severe bleeding, potential risk of allergic reaction. |
| Surgical Hemostats | These include sutures, clips, and staples used to control bleeding mechanically. | Direct control of bleeding vessels, permanent. | Requires access to the bleeding vessel, potential for tissue damage. |
Each of these techniques possesses its strengths and limitations, and the choice often depends on the surgeon’s preference, the nature of the procedure, and the specific patient characteristics.
Electrocautery, for instance, is commonly used due to its accessibility and effectiveness in achieving hemostasis. However, it also carries risks, such as thermal injury to surrounding tissues. Laser technology provides excellent precision but requires significant safety precautions to prevent eye injuries and fire hazards [4]. However, each of these methods has potential drawbacks and risks, including thermal injury to surrounding tissues, allergic reactions, and, in the case of mechanical methods, potential damage to nearby structures.
Given the rapid advancements in technology, it is essential for surgeons to stay abreast of the latest research and developments. Formal training and continuing education in the use of these technologies are integral components of improving patient outcomes and reducing intraoperative complications.
In addition to advancements in surgical techniques and tools, effective communication between the surgical team, anesthesia providers, and nursing staff is vital for optimal intraoperative bleeding management. A well-coordinated team can promptly respond to changes in the patient’s status, making necessary adjustments to the surgical strategy and ensuring the child’s safety.
Additionally, topical hemostatic agents and surgical hemostats, such as sutures, clips, and staples, can be used to control bleeding [5]. Therefore, the choice of method often relies on the specific surgical context, the surgeon’s expertise, and the characteristics of the patient. Furthermore, the prevention of bleeding is equally as important as its management. This might involve careful preoperative planning, including assessing the patient’s coagulation status, optimizing their health prior to surgery, and meticulous surgical techniques to minimize tissue trauma.
Looking forward, the management of intraoperative bleeding in pediatric otolaryngology is a multifaceted challenge that requires a comprehensive approach tailored to the unique needs of pediatric patients, the characteristics of the surgical area, and the specific circumstances of each case. The combination of emerging technologies, evidence-based practices, ongoing training, and efficient teamwork holds the key to enhancing patient outcomes.
Research initiatives and comparative studies that focus on assessing the effectiveness and safety of different intraoperative bleeding management techniques in pediatric populations are needed. In addition, quality improvement projects focused on this topic could provide valuable insights into best practices and areas of potential improvement.
Author Contributions
Conceptualization, A.M. and S.C.; methodology, L.L.V.; software, I.L.M.; validation, A.M. and S.C.; formal analysis, R.B.M.; investigation, I.L.M.; resources, I.L.M..; data curation, S.C.; writing—original draft preparation, A.M. and S.C.; writing—review and editing, R.B.M.; visualization, A.M.; supervision, S.C.; project administration, L.L.V.; funding acquisition, A.M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Waived due to study design.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Mitchell R.B., Archer S.M., Ishman S.L., Rosenfeld R.M., Coles S., Finestone S.A., Friedman N.R., Giordano T., Hildrew D.M., Kim T.W., et al. Clinical Practice Guideline: Tonsillectomy in Children (Update)-Executive Summary. Otolaryngol. Head Neck Surg. 2019;160:187–205. doi: 10.1177/0194599818807917. [DOI] [PubMed] [Google Scholar]
- 2.Roy S., Bigcas J.L., Vandelaar L. Hemostasis in Pediatric Surgery. Otolaryngol. Clin. N. Am. 2016;49:601–614. doi: 10.1016/j.otc.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 3.Kumar A., Kumar S., Krishnan A., Verma M., Garg U., Sharma N. A Comparative Analysis of Outcomes of Conventional Cold Dissection Versus Laser Tonsillectomy in Pediatric Cases in a Tertiary Care Hospital in Haryana. Indian J. Otolaryngol. Head Neck Surg. 2022;74:5311–5318. doi: 10.1007/s12070-020-02301-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stoner M.J., Dulaurier M. Pediatric ENT emergencies. Emerg. Med. Clin. N. Am. 2013;31:795–808. doi: 10.1016/j.emc.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Epure V., Hainarosie R., Voiosu C., Gheorghe D.C. Use and Abuse of Electrocautery in Adenoidectomy Hemostasis. Medicina. 2023;59:739. doi: 10.3390/medicina59040739. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.