Abstract
Point-of-care ultrasound (PoCUS) has a potentially vital role to play in emergency medicine (EM), whether it be in high-, medium-, or low-resourced settings. However, numerous barriers are present which impede EM PoCUS implementation nationally and globally: (i) lack of a national practice guideline or scope of practice for EM PoCUS, (ii) resistance from non-PoCUS users of ultrasound imaging (USI) and lack of awareness from those who undertake parallel or post-EM patient care, and (iii) heterogeneous pattern of resources available in different institutes and settings. When combined with the Indian Preconception and Prenatal Diagnostic Techniques (PCPNDT) Act, this has led to the majority of India’s 1.4 billion citizens being unable to access EM PoCUS. In order to address these barriers (globally as well as with specific application to India), this article outlines the three core principles of EM PoCUS: (i) the remit of the EM PoCUS USI must be well defined a priori, (ii) the standard of EM PoCUS USI must be the same as that of non-PoCUS users of USI, and (iii) the imaging performed should align with subsequent clinical decision-making and resource availability. These principles are contextualized using an integrated PoCUS framework approach which is designed to provide a robust foundation for consolidation and expansion across different PoCUS specialisms and health-care settings. Thus, a range of mechanisms (from optimization of clinical practice through to PoCUS educational reform) are presented to address such barriers. For India, these are combined with specific mechanisms to address the PCPNDT Act, to provide the basis for influencing national legislation and instigating an addendum to the Act. By mapping to the recent Lancet Commission publication on transforming access to diagnostics, this provides a global and cross-discipline perspective for the recommendations.
Keywords: Emergency medicine, India, point of care ultrasound, roadmap
INTRODUCTION
Point-of-care ultrasound (PoCUS) has a potentially vital role to play across a wide range of clinical scenarios commonly encountered in emergency medicine (EM).[1] PoCUS differs from traditional radiology-based ultrasound imaging (USI) in that it places USI into the hands of treating clinicians at the point of delivery.[2] Consequently, it allows for real-time, imaging-informed clinical decision-making, as well as facilitating image-guided treatment techniques. In well-resourced settings, PoCUS has the potential to expedite emergency care and it can be particularly valuable in lowe-resourced regions where diagnostic and treatment options may be limited.[3] The EM literature indicates high levels of global interest among EM physicians for using PoCUS and this spans high-, middle-and low-income regions; for example, North America,[4,5,6,7] Korea,[8] Taiwan,[9] Qatar,[10] UK,[11] South Africa,[12] India,[13,14] Vietnam,[15] Uganda,[16] Thailand,[17] and Tanzania.[18]
In order to identify the barriers to EM PoCUS uptake, a search was undertaken of the published literature using the key words “Emergency medicine,” “Emergency department,” “Point of care ultrasound,” “PoCUS,” “Barrier,” and “Challenge.” The inclusion criteria were if the papers used a survey or interview study design; were a full published paper (e.g. not a conference abstract) and reported one or more barriers to EM PoCUS uptake. From the subsequent papers,[4,5,6,8,10,13,17] the barriers identified were as follows:
A lack of USI training,[13,17] structured PoCUS curriculum,[5,8] national EM PoCUS guidelines,[10] and credentialing[10] and
A lack of trust from other department in PoCUS results by EM physicians[8] and by EM physicians in their own PoCUS scanning,[5] in parallel to a lack of quality assurance[4,10] and uncertainty with documenting of USI[6] and
Resource availability, including access to USI equipment[13] and time to train.[8,10]
In addition to the above, EM PoCUS use in India has the legal barrier presented by the “preconception and prenatal diagnostic techniques (PCPNDT) act.” Enacted in 1994, its intent is to prohibit the use of prenatal diagnostic techniques to determine foetal gender, leading to female feticide.[19] However, the PCPNDT act has created wide ranging legal and logistical barriers to PoCUS use,[20] leading to stifling of uptake of the modality across almost all medical specialisms in India, including EM.
In light of the potentially transformative role that PoCUS can affect in EM, identifying and implementing mechanisms to address the barriers to EM PoCUS should be a high priority on the global stage. The often time-critical nature of EM and the importance of optimally-informed clinical decision-making means that initiatives that can enhance these should be prioritised. This is of particular relevance for regions where EM is a rapidly emerging specialism, for example, in India, where it gained official recognition as a specialty in 2009.[21] The relatively recent emergence of the specialism in India means that opportunities for quality enhancement are manifold and pressing.
This article summarizes the key barriers to EM PoCUS and proposes integrated, multi-faceted solutions that can be applied on a global stage. Given the unique nature of EM PoCUS in India, we frame the proposals around a roadmap for EM PoCUS expansion in India, which has been borne out of a collaborative effort of a multi-national working group. This includes mechanisms to address the PCPNDT act (as applied to EM PoCUS) as a foundation for sustained access to imaging-informed EM for India’s 1.4 billion citizens.
BARRIERS TO THE USE OF EMERGENCY MEDICINE POINT-OF-CARE ULTRASOUND
For the purposes of this article – and drawing upon the published literature – we summarize in Table 1 barriers to the use of EM PoCUS and how these map to the solutions subsequently presented.
Table 1.
Barriers to the use of emergency medicine point of care ultrasound
| Barrier | Global or India-specific | Solution (see next section) |
|---|---|---|
| Lack of a national practice guideline or scope of practice for EM PoCUS | India-specific (though equally relevant in many regions and healthcare settings) | ScoP informs curriculum content; see also barrier 3 National EM PoCUS educational scrutiny body |
| Resistance from non-PoCUS users of USI and lack of awareness from those who undertake parallel or post-EM patient care | Global | Emphasis on formal training, as informed by ScoP ScoP (clinical and sonographic) defined and communicated |
| Heterogenous pattern of resources available in different institutes and settings | Global (but exacerbated in low and middle income [LMIC] regions) | ScoP aligned with local resource availability |
| PCPNDT act | India-specific | ScoP defined a priori Use of specific exclusions from ScoP; integral part of local and national agreement |
ScoP: Scope of practice, LMIC: Low and middle income country, PCPNDT: Preconception and prenatal diagnostic technique, PoCUS: Point of care ultrasound, EM: Emergency medicine, USI: Ultrasound imaging
As noted earlier, surveys of EM PoCUS (including in India[13,14]) have highlighted the lack of a national practice guideline or scope of practice (ScoP) for EM PoCUS. This places the individual EM PoCUS user at risk of potential litigation and makes it harder to establish PoCUS within the EM specialty. It has been reported that EM PoCUS educational scope may frequently be determined by the specialty of individual mentors;[14] however, PoCUS curricula and credentialing which instead are based upon pedagogical rigour and strategic alignment are required.
As in many other health-care systems, USI in India is historically the domain of radiology.[22] The introduction of PoCUS as an adjunct to some preexisting USI services may generate institutional resistance. This is likely exacerbated where PoCUS users lack formal and standardised training in the modality, leading to a perception by preexisting USI services of poorly-defined or “sub-standard” practice.[1] Similarly, clinical services who undertake parallel or post-EM patient care (e.g. intensive care, ward, and community-based care) may be unfamiliar with the applications and limitations of EM PoCUS. Mechanisms to ensure robust training in EM PoCUS (see above) combined with inter-professional communication regarding the scope or remit of PoCUS are some of the key approaches to addressing this barrier.
Lack of adequate resources for both training and clinical use of PoCUS have been identified (including in India[13,14]). This includes human resources (particularly mentor expertise) and in less well-resourced regions the necessary physical resources (e.g. ultrasound machines, probes, ultrasound gel, disinfection, etc.). Given the size and diversity of India, its heterogeneous pattern of resources and health-care delivery greatly exacerbates such challenges.[23] However, this also means it presents a valuable opportunity to test and implement changes that will be of relevance to many other regions globally. Consideration must therefore be given to the availability of local resources and clinical services when considering EM PoCUS applications.
As noted earlier, EM PoCUS is particularly impeded in India by the PCPNDT Act.[24,25] This act places far reaching limitations on the use of USI, particularly in health-care settings without radiology staff.[26] The act invokes the threat of prosecution against those using USI; and EM PoCUS is not exempt from the legislation. However, the harm caused by constraints (secondary to the act) in India on the use of USI is well documented.[20,27] In light of this law serving as a static barrier to EM PoCUS development, we emphasize the importance of medicine informing and influencing national legislation. As such, a comprehensive, multi-faceted, and integrated approach to addressing it is essential.
COLLABORATION OF A MULTI-NATIONAL WORKING GROUP
The following proposals have been developed by a multi-national working group and stem from an original initiative to support the Department of EM at Kasturba Medical College (KMC), Manipal, India, with creating a formalized PoCUS education and certification process. This drew upon the expertise of senior authors based in India, with a longstanding involvement in leading PoCUS teaching, training, and research across academic EM programs. Reflecting the regional and international scope of their involvement, this includes their senior involvement with a range of initiatives (e.g. World Academic Council of EM, International Network for Critical Ultrasound [INCUS] and the All India Institute of Medical Sciences) and with nongovernmental organisations such as the WHO South-East Asia region. This was dove-tailed with the expertise of Global Health leaders from the USA (Global Health Research Collaborative and Department of Emergency Medicine, Wayne State University, Michigan) drawing upon their experience and lessons learnt from a wide range of global initiatives in the area of EM (including PoCUS).
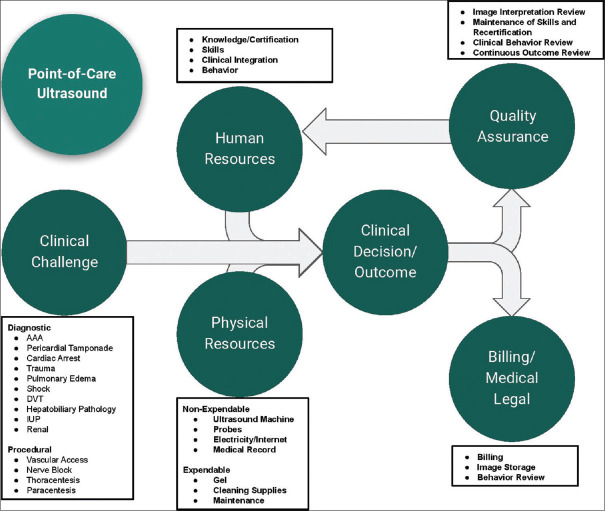
The India and USA teams utilized their collective expertise to model an EM PoCUS ecosystem [Figure 1], thereby identifying the necessary components of an EM ultrasound division. An online needs assessment [Appendix 1] was then undertaken which was completed by attending physicians and residents (n = 11) at KMC Manipal. This explored the nature of EM activity at KMC Manipal, including perceived barriers to using ultrasound in the emergency department (ED). A follow-up online group meeting of the teams further explored the emerging themes and concluded:
Figure 1.
PoCUS ecosystem. PoCUS: Point of care ultrasound
A range of diagnostic and procedural PoCUS applications were undertaken in the ED at KMC Manipal and there was the interest in expanding PoCUS from both clinicians and the ED leadership
-
The biggest threats and barriers identified were as follows:
- Legislative (PCPNDT Act)
- Historical precedent that USI is performed solely by radiologists
- Lack of integration of PoCUS imaging into patient records
- Ultrasound equipment ergonomics/availability/maintenance/failure.
Noting the close alignment of the needs assessment findings with the previously published literature,[4,5,6,8,10,13,17] the India and USA teams worked with the UK based author to collaboratively draw upon a PoCUS framework approach to frame integrated solutions for India. Through an iterative process of consultation with the senior authors from India and USA, the solutions in this paper were refined, including their potential application beyond India.
A COMPREHENSIVE APPROACH FOR CONSOLIDATING AND EXPANDING POINT-OF-CARE ULTRASOUND
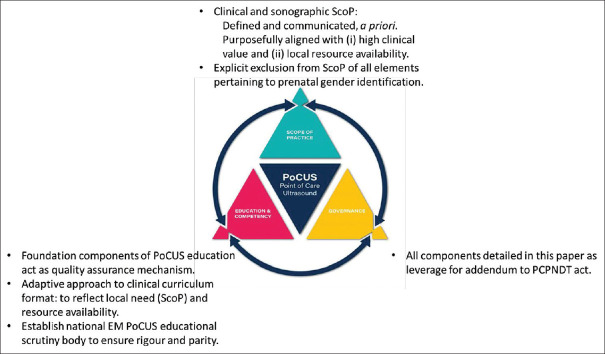
In light of the above barriers – and given the complexities of establishing and consolidating a robust, effective and sustainable healthcare service such as EM PoCUS (including across India) – two foundation elements are presented: a model of the key inter-related components of PoCUS [Figure 2- PoCUS Triangle elements] and core principles of EM PoCUS [Table 2].
Figure 2.
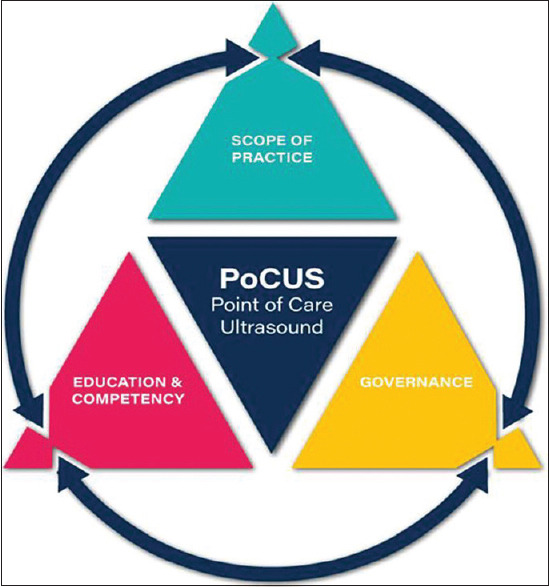
PoCUS triangle presenting the inter-related components of scope of practice, education/competency and governance. PoCUS: Point of care ultrasound
Table 2.
Core principles of point of care ultrasound in emergency medicine
| Core principle | Rationale | Considerations |
|---|---|---|
| A. The remit of the PoCUS USI must be well defined a priori | The wide range of potential tissues, organ systems and differentials encountered in EM – is in contrast with the PoCUS clinician typically not being competent to image across all such areas/differentials. Additionally, much of the tissue and organs imaged are not relevant to the EM provider Therefore, to ensure patient safety and to defend against litigation risk, the PoCUS clinician must only use PoCUS within their area of established competency | Given the “emergency” nature of EM, this means that prospective agreement regarding remit is essential The largely binary nature of EM PoCUS decision making (i.e., the “rule in” principle) complements this |
| B. The standard of PoCUS USI must be the same as that of non-PoCUS users of USI | Whilst the scope of PoCUS is artificially narrow (core principle A), the standards must be the same as for radiologists and sonologists. This reflects a fundamental commitment to quality of care and patient safety | Such standards include competency in the imaging undertaken, the reporting of USI findings, recognition of boundaries of imaging competency, etc. |
| C. The imaging performed should align with subsequent clinical decision making and resource availability | Aligning with core principle A, PoCUS USI should be undertaken as part of a meaningful clinical decision making/treatment algorithm. This will be framed by the availability of resources to address the clinical problem(s); considerations include patient prognosis, local resources and likelihood of accessing tertiary facilities (where appropriate) | Core principle C is highly “site dependent” and may be influenced by transient resource demands (e.g., natural disaster) |
PoCUS: Point of care ultrasound, EM: Emergency medicine, USI: Ultrasound imaging
The PoCUS framework approach comprises the elements of (i) ScoP, (ii) education and competency, and (iii) governance. These terms are well established in the published literature, having been described by authors such as Ambasta et al.,[28] LoPresti et al.,[29] Lee and DeCara,[30] and Teunissen et al.[31] The PoCUS framework approach was devised by the lead author (stemming from longstanding work across a range of PoCUS specialities in the domains of education, work-force planning, policy, and legislation) in response to a perceived need to provide comprehensive solutions for PoCUS integration into health-care systems. It has recently been used to support the consolidation of other areas of PoCUS activity[32,33,34,35] and as such this paper shares some generic content with these publications. A central tenet of the PoCUS framework approach is that each of the elements are inter-dependent of and inform each other and when aligned provide a foundation for robust delivery of PoCUS.
In relation to these terms, ScoP refers to the USI performed plus the interpretation/reporting of that USI plus the clinical decision making informed by that USI. Crucially, it also clarifies what tissues imaged, clinical, and sonographic differentials and subsequent clinical decision making are not to be performed. The education and competency element refers to the education undertaken (both informally and formally) and subsequent assessment of competency. Transparent, purposeful and efficient education provision, and competency assessments are made possible by aligning with the ScoP. Similarly, education and competency are a foundation for quality assurance and inter-professional acceptability of EM PoCUS. Governance includes legal frameworks, professional body and insurance arrangements, billing, and quality assurance. These are in part informed by the ScoP; by professional, local and national agreements, and through workflow practices.
The PoCUS triangle [Figure 2- PoCUS Triangle elements] provides a mechanism to model, define and align each of the three key elements that impact upon PoCUS. The core principles in Table 2 then sit alongside the PoCUS triangle and provide an EM context for its application.
An example of how principle a might be applied is where a Focused Assessment with Sonography for Trauma (FAST) examination is performed. Here, USI is undertaken to identify the presence of changes secondary to tissue/organ trauma, i.e. following clinical assessment, USI is used to “rule in” such findings.[36] However, elements that could be incidentally encountered during an EM PoCUS FAST exam include liver cysts; yet the EM PoCUS user is using USI solely to answer the question of whether or not there is free fluid in the abdomen – and thus may not identify and/or report upon the presence of such lesions. Conversely, a non-PoCUS user of USI (e.g. radiologist or sonologist) undertaking a protocol based scan of the same abdomen may be expected to have identified or excluded such lesions.[37]
Such discrepancies in imaging findings could present a litigation risk to the EM PoCUS user and undermine inter-professional confidence in PoCUS imaging ability (thereby aligning with the barrier identified by Yoo et al.[8]. However, comprehensively defining the EM PoCUS ScoP means that clarity is provided to non-PoCUS users of USI (and those who undertake parallel or post-EM patient care) regarding what the EM PoCUS scan is and is not for the purpose of, having been defined a priori. A further benefit of this, is that the EM PoCUS educational and competency requirements can be more specifically defined (compared to radiologist or sonologist USI training), thus allowing for focussed and standardized EM PoCUS training.
Principle B relates to fundamental aspects around quality of USI practice;[1] a formal training program that includes credentialing would expose the clinician to such elements. Some aspects of these generic principles are of particular importance for EM PoCUS use, e.g. the capture of standardised images and integration of the images and reporting into the patient records. These help to address a barrier identified by Schnittke and Damewood.[6] The large number of potential destinations for EM patients (critical care, ward, community, etc.) means that continuity of care is essential, particularly where baseline imaging of organs may inform subsequent care (e.g. with an unstable cardiac presentation or deterioration secondary to trauma).
Principle C is an EM PoCUS-specific application of defining ScoP, specifically with respect to onward care. An example of this is the practical application of Abdominal Aortic Aneurysm (AAA) ultrasonography. In a location with no vascular surgery capabilities (e.g. remote or rural healthcare location), competency in AAA ultrasonography could be deprioritised – thus enabling techniques more specific to that healthcare setting to be gained (and just as importantly, retained, thereby addressing a barrier identified by Singh et al.[5]). Conversely in a location with readily available vascular surgery capabilities then AAA ultrasonography would be a necessary component of the EM PoCUS skillset.[2] Principle C provides a pragmatic approach to how best to target PoCUS competency levels against the backdrop of the wide range of levels of healthcare resource availability in global EM, including across a country as diverse as India.
APPLICATION OF THE COMPREHENSIVE APPROACH FOR ADDRESSING BARRIERS TO EMERGENCY MEDICINE POINT OF CARE ULTRASOUND
Solution to barrier 1: Lack of a national practice guideline or scope of practice for emergency medicine point of care ultrasound
Descriptions of EM PoCUS curricula can be found in the literature[38,39,40,41,42] and include those from the EM Society of South Africa.[43] who describe distinct training routes for “core” and “advanced” PoCUS. Such an approach may reflect the technical challenges of certain PoCUS techniques or the expertise required to interpret and integrate such scans into clinical care. However, given the diverse nature of healthcare delivery models (including in India), alignment of PoCUS curricula with ScoP provides for a strategic and adaptable approach to PoCUS curriculum development and credentialing.
Reflecting previously published curricula (e.g. Wells et al.[43]), we advocate that generic elements [*; Table 3] be included and formally assessed, as these equip the EM clinician with the foundations for safe, effective and professional use of USI. However, the EM PoCUS applications that a clinician, service or healthcare setting will be using would dictate the specifics of [Δ; Table 3] to be covered. Approaches by which these curricula might be structured include (i) grouping according to clinical presentation-related techniques, e.g. FAST, (ii) grouping according to organ/system specific related techniques, e.g. lung ultrasound, or (iii) grouping according to clinical application/procedural techniques such as image guided interventions. This reflects the wide range of applications reported as being used in the EM PoCUS literature internationally.[4,5,6,8,9,10,12,13,14,15,16,18]
Table 3.
Potential components and formats of emergency medicine point of care ultrasound curriculum and assessment
| Educational component | Rationale | Potential format (including assessment) |
|---|---|---|
| Foundation physics applied to USI* | Enables understanding of foundation principles of USI generation, limitations, artefacts and their management, etc. | Can be didactic learning material; can be asynchronous or module based; assessment format should test understanding and relevance rather than simply information retention |
| Image optimisation* | Enables image management to enhance confidence in image interpretation. Particularly relevant in time-critical situations, compromised resource circumstances, etc. | Theoretical elements overlap with “Foundation physics applied to USI” Practical application could be taught and assessed as stand-alone (e.g., using phantoms) and/or within clinical scenarios |
| Professional considerations such as image taking, integration within patient records and reporting, infection control, etc.* | Core elements to professional use of USI; including generic healthcare considerations | Can be didactic learning material; assessment format should test understanding and relevance rather than simply information retention Could be integrated within clinical scenarios |
| EM PoCUS applications: Grouped according to clinical presentation, organ/system or clinical application/procedural∆ | The USI performed + the interpretation/reporting of that USI + the clinical decision making informed by that USI In relation to the imaging techniques performed, includes consideration of what USI is not performed and/or the interpretation/reporting not undertaken from that USI and/or the clinical decision making not informed by that USI | Can be didactic learning material covering clinical indications/scenarios Practical scanning training could include healthy volunteers and scan trainers alongside actual patients. Emphasis is on directly supervised scanning experience, supplemented by peer-learning, on-line material, etc. Competency assessment should include “log book” of scans with reflective account + directly observed clinical scanning in controlled environment (e.g., OSCE format, previously unseen clinical patient, etc.) |
*Core or generic, ∆Category-specific. OSCE: Objective structured clinical examination, PoCUS: Point of care ultrasound, EM: Emergency medicine, USI: Ultrasound imaging
Advocating a nonprescriptive approach to the specific content or structuring of these EM PoCUS curricula might appear insufficient to address barrier 1. However the pedagogical and professional principles underpinning the components and format of EM PoCUS curriculum and assessment (above) mean that clinically meaningful EM PoCUS can be prioritised, robustly learnt and subsequent competency evidenced.
Opportunities for interorganizational collaboration include such education provision potentially being developed in partnership with organisations such as the (INCUS; https://incusworld.org/about-INCUS) which is dedicated to the advancement of ultrasound by developing core competencies, encouraging research, promoting regional, national and global cooperation, disseminating scientific information, and improving communication and understanding in PoCUS (http://www.indusem.org/leadership-councils/). The examples of such courses include those to strengthen prehospital care, facility-based emergency care and disaster care service delivery; and the advanced ultrasound in trauma and life support course has been undertaken widely at global level including at Nepal, Sri Lanka, Thailand, Iran, UK, and USA. The INCUS model of training nurses in POCUS was recognized in the WHO document “Strategic directions to integrate emergency care services into primary health care in the South-East Asia Region.”[44] Other initiatives by the network include utilizing POCUS to teach anatomy and physiology to undergraduate students; as such working with universities and academic institutions in India to bring structured training program for undergraduate and postgraduate medical students.
In relation to a country as diverse as of India, the likely number of EM PoCUS courses that would need to be established – and the range of different ways in which such courses might be structured [Table 3] – means that the establishing of a national body to accredit such courses is advocated. Ideally this would sit within a preexisting Indian EM organization but would draw upon broader USI education expertise both clinically (e.g. radiology and sonology) and pedagogically (e.g. postgraduate medical and health-care education). This could help facilitate a range of EM PoCUS curricula delivery models whilst ensuring parity of standards – an essential requirement to establish PoCUS within the EM speciality. Funding for such a body would ideally be derived from central healthcare funds, on the understanding that its role is ultimately one of protection of the public and optimising delivery of EM care. This funding route would be preferable to that of charging the educational institutions it accredits, in order to avoid potential or perceived conflicts of interest.
Solution to barrier 2: Resistance from nonpoint of care ultrasound users of ultrasound imaging and lack of awareness from those clinicians who undertake parallel or postemergency medicine patient care
The emphasis in this paper on formal training in both the foundation elements of USI and specific PoCUS applications (whereby ScoP is defined according to PoCUS principles of the “rule in” approach) has the potential to partly address non-PoCUS users of USIs’ concerns of poorly defined or “sub-standard” practice. Furthermore, the emphasis upon defining ScoP provides clarity regarding what an EM PoCUS clinician will and will not be imaging/reporting upon/using to inform their clinical decision making. Collectively these provide a foundation for addressing barrier 2. Examples of different curriculum components, their clinical utility and limitations/exclusions is shown in Table 4 and again reflects the wide range of applications reported as being used globally.[4,5,6,8,9,10,12,13,14,15,16,18]
Table 4.
Examples of curriculum components, their clinical utility and limitations/exclusions
| Example curriculum component | Specifics of clinical-and sonographic-ScoP | Clinical utility | Limitations Example of specific exclusion (s) from ScoP and Generic exclusions from ScoP* |
|---|---|---|---|
| FAST exam | Patient presentation of trauma and/or hypotension of unclear etiology Identification of fluid around the heart (pericardial effusion) or abdominal organs (hemoperitoneum) after trauma | Informs clinical triage and (where appropriate) expedites surgical management; potentially improve morbidity/mortality rates | Does not exclude abdominal or thoracic injury Liver cysts All noncritical elements of foetal imaging; this includes any purposeful imaging of foetal genitals or reporting on gender identity |
| Lung ultrasound | Patient presentation of dyspnea, pulmonary edema, lower respiratory tract infections, etc. Identification of pneumothorax, pleural effusion, assessment for B lines, etc. | Combine with clinical signs to inform differential diagnosis and targeted management | Does not exclude pneumothorax or pleural effusion Lung masses or nodules All noncritical elements of foetal imaging; this includes any purposeful imaging of foetal genitals or reporting on gender identity |
| Image guided interventions | Central line or arterial line placement Nerve blocks Paracentesis Thoracentesis | Reduced risk of iatrogenic harm, e.g., local bleeding, infection, exposure of nontarget tissues to cytotoxin, etc. | Cannot be relied upon to sonographically exclude precautions or contraindications to procedure Incidental findings in imaged area, e.g., arterial issues when performing central line insertion; enlarged lymph nodes; solid organ abnormalities or masses All noncritical elements of foetal imaging; this includes any purposeful imaging of foetal genitals or reporting on gender identity |
*Generic exclusions from ScoP relate specifically to the PCPNDT act in India. ScoP: Scope of practice, PCPNDT: Preconception and prenatal diagnostic techniques, FAST: Focused assessment with sonography for trauma
Looking beyond EM, the above approach has merits for other areas of PoCUS, e. g. anaesthesia and critical care. Given that patients seen in EM may go on to be cared for by anaesthetists and critical care physicians, then a shared approach to learning certain PoCUS specialities – and communicating the remit of respective PoCUS scopes of practice – provides an opportunity for consolidating PoCUS more widely.
The clinical importance of integration of the images and reporting into the patient record was highlighted earlier. Along with addressing a concern identified by the survey of EM resident physicians by Schnittke and Damewood,[6] this also has a crucial role to play with helping address barrier 2; and also allows for quality assurance and education. This is because it provides greater visibility (to other members of the care pathway, including non-PoCUS users) of the type and quality of scan being undertaken. However EM PoCUS scans may often be undertaken using portable systems that are not integrated with picture archiving and communication system; thus there can be efficiency and data security challenges with taking such scans and integrating them with the electronic patient record/making them accessible within the wider health system.[45] Use of solutions such as secure cloud-based imaging repositories-and reporting systems which can integrate with preexisting patient record systems-are therefore advocated. Nonetheless the technical limitations of this (particularly in low-resource environments for accessing cloud-based services) is noted.
Solution to barrier 3: Heterogeneous pattern of resources available in different institutes
As noted in Table 1, one element of this barrier is human resources; specifically formal mentor availability is a key barrier to training. Access to a suitably experienced mentor is crucial because the combination of motor skill (probe manipulation) plus image acquisition, optimisation and interpretation all occur in real-time at the bedside.[42] Given the wide range of anatomical variations when scanning, the largely subjective nature of image interpretation and the unpredictable nature of EM case-loads, local access to a mentor and real time guidance is a crucial resource “bottle-neck.”
The use of a well-defined ScoP does allow for partial addressing of this, by identifying the EM PoCUS applications specifically relevant for that trainee – thereby allowing for highly focused mentor input. Where a trainee will go on to work in a remote region, then the selecting of a narrow, “high clinical value” ScoP[3] aligning with local need and resource availability, can help to optimise the gaining (and subsequent maintaining) of competence.
In providing a foundation for the expansion of EM PoCUS training (including in India), it is hoped that this paper will contribute to more EM clinicians training in PoCUS – and going on to become mentors themselves. In parallel it is hoped that the opportunities this paper provides for constructive relationships with Radiology services (see barrier 2) means that EM clinicians will increasingly be able to work with and learn from their non-PoCUS USI colleagues as part of gaining imaging experience.
Finally, technological advances make it possible for remote mentoring to be a parallel or even stand-alone mechanism for gaining and maintaining EM PoCUS competency. The use of web based teleguidance systems (including those associated with handheld portable USI units) mean that geographical proximity need no longer constrain training in-or even performance of-EM PoCUS.[46]
However this also illustrates the other aspect of barrier 3, namely the heterogeneity in availability of physical resources. Novel approaches such as empowering local regions via the use of “indigenously developed” ultrasound phantoms[47] can be part of the solution. Rapid advances in portable USI technology have led to a steady reduction in unit cost; and recent recommendations from the Indian National Medical Commission[48] requires EDs to procure an ultrasound machine for undergraduate medical programs.
Nonetheless in low income regions these may remain prohibitively expensive, particularly when servicing of fragile probes and use of consumables (ultrasound gel, probe covers, disinfectant, etc.) are factored in.[46] Mechanisms to potentially address this include the selecting of ScoPs that demonstrably impact the care pathway – and potentially bring onward patient care cost savings – these used to leverage for funding the purchase of USI units and associated maintenance and consumables.
Solution to barrier 4: Preconception and prenatal diagnostic techniques act
As noted previously, the PCPNDT Act is intended to limit female foeticide, which is clearly beyond the remit of this paper. Conversely the implications of the Act on EM (and other) PoCUS users in India is almost unparalleled in its restriction of use of the modality.[27] This is in contrast to the transformative potential of PoCUS across the domains of patient outcomes, healthcare systems cost-savings and addressing health inequalities.[46]
This position paper provides a comprehensive approach to ensuring the highest standards of professionalism and competency in the use of PoCUS in an EM context and can be integrated into the legal framework for defining the use of PoCUS. We advocate that all PoCUS ScoP definitions explicitly exclude any noncritical elements of foetal imaging including any imaging of foetal genitals or reporting on gender identity [Table 4]. We further propose that the integrated, multi-faceted solutions presented in this paper be used to formulate an addendum to the PCPNDT act clearly delineating the ScoP of EM PoCUS.
SUMMARY OF KEY ROLE PLAYED BY EDUCATION AND TRAINING IN THESE PROPOSALS
The explicit and bilateral alignment of ScoP with education, training and competency is a central tenet of the PoCUS framework approach
Education and competency in foundation elements of USI are necessary to provide a basis for high quality PoCUS delivery
Specifics of the EM PoCUS curriculum components to be taught [Table 4] are informed by local/regional healthcare resource availability and clinical need
Establishing a national body to accredit EM PoCUS courses in India is advocated, to ensure parity across diverse settings [Figure 3]
Educating national policy-makers – through to clinicians involved in the particular episode of care – regarding the ScoP is key to facilitating acceptance of EM PoCUS. This includes as a mechanism to address the PCPNDT act.
Figure 3.
Summary of recommendations for EM PoCUS expansion in India. EM: Emergency medicine, PoCUS: Point of care ultrasound
A ROADMAP FOR EMERGENCY MEDICINE POINT OF CARE ULTRASOUND EXPANSION IN INDIA
This paper has presented wide ranging and integrated mechanisms for the consolidation and expansion of EM PoCUS. Whilst the majority of barriers identified in Table 1 are generic across many healthcare systems, the PCPNDT Act is specific to India and is arguably the single greatest constraint on PoCUS here.
Aligning with Figure 1, governance elements (such as legal frameworks, professional body and insurance arrangements) are informed by the ScoP and education and competency components. Given the transformative potential of EM PoCUS in India, urgent consideration at a national level is advocated, to consider the robust platform which we believe this paper provides as a mechanism to remove penal barriers from EM clinicians using PoCUS. A comprehensive understanding of the barriers and targeted solutions may cause a ripple effect in policy making and implementation (including regulation of imported ultrasound machine accessibility), leading to a transformative impact in improving care for the critically ill and injured patient in the emergency setting.
When considering this roadmap in the wider context of diagnostics, a recent publication “The Lancet Commission on diagnostics: transforming access to diagnostics”[46] provides a useful global and cross-discipline perspective, as shown in Table 5.
Table 5.
Lancet commission recommendations (1–5), including relevance to India and proposals stemming from this roadmap
| Lancet commission recommendations | Relevance to India | Proposal |
|---|---|---|
| National diagnostics strategy to include an evidence-based EDL, with a prioritised subset for universal health coverage | Current EDL[49] lists USI only under “Radiology”; and only at community health centre, sub-district hospitals and district hospitals levels | EM PoCUS has applicability across a range of healthcare setting levels. Therefore we advocate an amendment of the EDL to list PoCUS (including for EM purposes) across a range of healthcare setting levels |
| Primary health centre diagnostic availability and accessibility (specifically advocates PoCUS at “Primary health centre” and “First level hospital” settings) | Potential for EM PoCUS to have transformative impact on primary health centre care, particularly in low resourced or remote regions | We advocate embracing of Lancet commission recommendation 2 to make EM PoCUS available in such locations |
| Health workforce expansion and upskilling for contemporary diagnostic skills Includes “develop high-quality task-shifting programmes, and exploit the full capability and skills of all staff” | Existing barriers to EM PoCUS in India means that this potential is not being realised | We advocate embracing the opportunity to upskill the EM workforce to use PoCUS in highly specific applications |
| Governance and regulatory frameworks to support and oversee diagnostic quality and safety Includes “national professional bodies concerned with diagnostics should have a framework of standards for their members” | Acceptability of the expansion of USI (from solely the domain of radiology) will require governance frameworks. The PCPNDT act draws this into sharp focus | We advocate mechanisms such as the establishing of a national body to accredit EM PoCUS courses – which in turn will support the ScoP of the subsequent imaging practice of EMs |
| National financing strategy to provide sufficient, long-term financing to plan, and implement diagnostics, including infrastructure | Wide range of health-care delivery settings means an emphasis on financial sustainability is essential | When identifying EM PoCUS ScoP, undertake modelling of onward patient care cost savings (e.g., reduced risk of iatrogenic harm, fewer complications, etc.) to provide financial rationale |
EDL: Essential diagnostics list, PoCUS: Point-of-care ultrasound, EM: Emergency medicine, PCPNDT: Preconception and prenatal diagnostic techniques, USI: Ultrasound imaging, ScoP: Scope of practice
HOW DOES THIS PAPER ADD TO WHAT IS ALREADY KNOWN IN THE LITERATURE REGARDING EMERGENCY MEDICINE POINT-OF-CARE ULTRASOUND IN INDIA?
Noting evidence from India of high levels of interest among EM clinicians in learning PoCUS[13] and it being identified as an indispensable EM tool,[14] this article provides a comprehensive roadmap for EM PoCUS expansion. Previous surveys in India have identified a lack of dedicated training[13] as a substantial barrier, with the need for PoCUS guidelines in the EM curriculum.[14] This article provides integrated solutions that align EM training with the local burden of disease,[21] along with proposals for a national EM PoCUS accreditation body. Noting the bureaucratic barriers (and potential penal consequences) of the PCPNDT Act,[20,27] this article presents pragmatic and integrated solutions to address this barrier to EM PoCUS.
APPLICATION OUTSIDE OF INDIA
The generic barriers noted in Table 1 – and the solutions proposed throughout this paper – are of relevance to health-care systems worldwide, whether they be in high-, medium- or low-resourced settings.
It is noted that different regions will have their own unique challenges ranging from financial (e.g. insurance and billing); through to legislation or professional barriers; through to the breakdown in societal structures due to famine, armed conflict, etc., We advocate the use of the PoCUS triangle approach to model, define, and align each of the key elements that impact upon PoCUS delivery, alongside adoption of the core principles in Table 2. EM and PoCUS organizations are encouraged to consider these mechanisms as part of a sustainable approach to consolidating and expanding the use of PoCUS.
CONCLUSION AND NEXT STEPS
This roadmap has summarized the key barriers to the use of EM PoCUS and specifically EM PoCUS in India, from which mechanisms have been proposed to address a range of generic challenges. These have been combined with specific exclusion of any imaging applications with which the PCPNDT act is concerned.
Given the transformative potential of EM PoCUS across India’s wide range of health-care settings – and alignment with the Lancet’s recent recommendations around access to diagnostics – we urge deployment of this roadmap, a summary of which is presented in Figure 2. In this regard, reconsideration of the PCPNDT act as applied to PoCUS (and specifically EM) is urgently required, as all other components of the roadmap are otherwise critically constrained. As such, a multifaceted approach is required to provide the 1.4 billion people of India with access to the imaging-informed emergency health care they deserve.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Appendix 1: Needs assessment questionnaire
What are the top five chief complaints you have seen over the past year?
What are the top five diagnoses of patients you have seen over the past year?
What are the top 5 chief complaints that you evaluate on a regular basis where your Emergency Department work up would benefit from Point Of Care Ultrasound training?
What are the top 5 procedures you performed in your Emergency Department last year?
What are the top 5 procedures that you perform on a regular basis which you feel would benefit from ultrasound guidance?
What are the biggest day to day problems in your Emergency Department?
What are your barriers to using ultrasound in the Emergency Department?
Are there any limitations to accessing the ultrasound machine in your Emergency Department?
What type of ultrasound probes do you have access to?
-
Do you have access to the following imaging modalities:
- Xray
- CT Scan
- MRI
- Formal Ultrasound (Radiology Department)
REFERENCES
- 1.Amini R, Adhikari S, Fiorello A. Ultrasound competency assessment in emergency medicine residency programs. Acad Emerg Med. 2014;21:799–801. doi: 10.1111/acem.12408. [DOI] [PubMed] [Google Scholar]
- 2.Ultrasound guidelines: Emergency, point-of-care and clinical ultrasound guidelines in medicine. Ann Emerg Med. 2017;69:e27–54. doi: 10.1016/j.annemergmed.2016.08.457. [DOI] [PubMed] [Google Scholar]
- 3.Tafoya CA, Tafoya MJ, Osei-Ampofo M, Oteng RA, Becker TK. Sustainable resuscitation ultrasound education in a low-resource environment: The Kumasi experience. J Emerg Med. 2017;52:723–30. doi: 10.1016/j.jemermed.2017.01.050. [DOI] [PubMed] [Google Scholar]
- 4.Kim DJ, Olszynski P, Smith DJ, Lalande E, Woo MY. Point of care ultrasound training in Canadian emergency medicine residency programs. CJEM. 2022;24:329–34. doi: 10.1007/s43678-022-00269-1. [DOI] [PubMed] [Google Scholar]
- 5.Singh MR, Jackson JS, Newberry MA, Riopelle C, Tran VH, PoSaw LL. Barriers to point-of-care ultrasound utilization during cardiac arrest in the emergency department: A regional survey of emergency physicians. Am J Emerg Med. 2021;41:28–34. doi: 10.1016/j.ajem.2020.12.040. [DOI] [PubMed] [Google Scholar]
- 6.Schnittke N, Damewood S. Identifying and overcoming barriers to resident use of point-of-care ultrasound. West J Emerg Med. 2019;20:918–25. doi: 10.5811/westjem.2019.8.43967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Micks T, Sue K, Rogers P. Barriers to point-of-care ultrasound use in rural emergency departments. CJEM. 2016;18:475–9. doi: 10.1017/cem.2016.337. [DOI] [PubMed] [Google Scholar]
- 8.Yoo J, Kang SY, Jo IJ, Kim T, Lee G, Park JE, et al. The use of point-of-care ultrasound in emergency medical centers in Korea: A national cross-sectional survey. J Korean Med Sci. 2021;36:e141. doi: 10.3346/jkms.2021.36.e141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen WL, Hsu CP, Wu PH, Chen JH, Huang CC, Chung JY. Comprehensive residency-based point-of-care ultrasound training program increases ultrasound utilization in the emergency department. Medicine (Baltimore) 2021;100:e24644. doi: 10.1097/MD.0000000000024644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bashir K, Azad AM, Hereiz A, Bashir MT, Masood M, Elmoheen A. Current use, perceived barriers, and learning preference of point of care ultrasound (POCUS) in the emergency medicine in Qatar –A mixed design. Open Access Emerg Med. 2021;13:177–82. doi: 10.2147/OAEM.S304153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smallwood N, Dachsel M. Point-of-care ultrasound (POCUS): Unnecessary gadgetry or evidence-based medicine? Clin Med (Lond) 2018;18:219–24. doi: 10.7861/clinmedicine.18-3-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khanyi HB, Naicker B. The use of point-of-care ultrasound in a regional emergency department in KwaZulu-Natal, South Africa. S Afr Fam Pract (2004) 2021;63:e1–6. doi: 10.4102/safp.v63i1.5269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boniface KS, Drake A, Pyle M, Moideen F, Mehta S, Poovathumparambil V, et al. Learner-centered survey of point-of-care ultrasound training, competence, and implementation barriers in emergency medicine training programs in India. AEM Educ Train. 2020;4:387–94. doi: 10.1002/aet2.10423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thomas VK, Abraham SV, Balakrishnan JM, Krishnan SV, Amalakat A, Palatty BU. Point-of-care ultrasound training in Indian emergency medicine programs: A resident's perspective. Int J Acad Med. 2017;3:263. [Google Scholar]
- 15.Rice BT, Vu H, Tran LD, Vo QX, Mowafi H. Survey of point of care ultrasound usage in emergency medicine by Vietnamese physicians. Emerg Med Australas. 2015;27:580–3. doi: 10.1111/1742-6723.12476. [DOI] [PubMed] [Google Scholar]
- 16.Stolz LA, Muruganandan KM, Bisanzo MC, Sebikali MJ, Dreifuss BA, Hammerstedt HS, et al. Point-of-care ultrasound education for non-physician clinicians in a resource-limited emergency department. Trop Med Int Health. 2015;20:1067–72. doi: 10.1111/tmi.12511. [DOI] [PubMed] [Google Scholar]
- 17.Ienghong K, Suzuki T, Tiamkao S, Gaysonsiri D, Bhudhisawasdi V, Apiratwarakul K. Point of care ultrasound use by interns in emergency department. [[Last accessed on 2022 Apr 22]];Open Access Maced J Med Sci. 2021 9:588–91. Available from: https://oamjms.eu/index.php/mjms/article/view/6380 . [Google Scholar]
- 18.Reynolds TA, Amato S, Kulola I, Chen CJ, Mfinanga J, Sawe HR. Impact of point-of-care ultrasound on clinical decision-making at an urban emergency department in Tanzania. PLoS One. 2018;13:e0194774. doi: 10.1371/journal.pone.0194774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bhaktwani A. The PC-PNDT act in a nutshell. Indian J Radiol Imaging. 2012;22:133–4. doi: 10.4103/0971-3026.101114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tabaie S. Stopping female feticide in India: the failure and unintended consequence of ultrasound restriction. J Glob Health. 2017;7:010304. doi: 10.7189/jogh.07.010304. doi: 10.7189/jogh.07.010304. PMID: 28567276;PMCID: PMC5441446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jain M, Batra B, Clark E, Kole T. Development of post-graduate program in emergency medicine in India: Current status, scope, and career pathways. Med Educ N Front. 2014;1:218–21. [Google Scholar]
- 22.Gupta A, Peckler B, Stone MB, Secko M, Murmu LR, Aggarwal P, et al. Evaluating emergency ultrasound training in India. J Emerg Trauma Shock. 2010;3:115–7. doi: 10.4103/0974-2700.62104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Douglass K, Gidwani S, Mehta S, Jaiswal S, Kuriakose B, Vennugopalan PP, et al. White Paper on Emergency Education and Training in India: Where are we now and Where Should we Go Next? [[Last accessed on 2021 Nov 18]]. Available from: https://smhs.gwu.edu/reaganinstitute/sites/reaganinstitute/files/White%20paper-Emergency%20Medicine%20Education%20and%20Training%20in%20India.pdf .
- 24.Dhar M, Payal YS, Krishna V. The pre-conception and pre-natal diagnostic techniques act and its implication on advancement of ultrasound in anaesthesiology;time to change mindsets rather than laws. Indian J Anaesth. 2018;62:930–3. doi: 10.4103/ija.IJA_518_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rath C, Nagpal R, Suryawanshi P. Point-of-Care Ultrasound in Neonatology in India: The Way Forward. Indian Pediatr. 2023;60:351–7. Available from: https://doi.org/10.1007/s13312-023-2879-0 . [PubMed] [Google Scholar]
- 26.Patnaik AM, Kejriwal GS. A perspective on the PCPNDT act. Indian J Radiol Imaging. 2012;22:137–40. doi: 10.4103/0971-3026.101116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Phutke G, Laux T, Jain P, Jain Y. Ultrasound in rural India: A failure of the best intentions. Indian J Med Ethics. 2019;4:39–45. doi: 10.20529/IJME.2018.041. [DOI] [PubMed] [Google Scholar]
- 28.Ambasta A, Balan M, Mayette M, Goffi A, Mulvagh S, Buchanan B, et al. Education indicators for internal medicine point-of-care ultrasound: A consensus report from the Canadian internal medicine ultrasound (CIMUS) group. J Gen Intern Med. 2019;34:2123–9. doi: 10.1007/s11606-019-05124-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.LoPresti CM, Schnobrich DJ, Dversdal RK, Schembri F. A road map for point-of-care ultrasound training in internal medicine residency. Ultrasound J. 2019;11:10. doi: 10.1186/s13089-019-0124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee L, DeCara JM. Point-of-care ultrasound. Curr Cardiol Rep. 2020;22:149. doi: 10.1007/s11886-020-01394-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Teunissen PW, Watling CJ, Schrewe B, Asgarova S, Ellaway R, Myers K, et al. Contextual competence: How residents develop competent performance in new settings. Med Educ. 2021;55:1100–9. doi: 10.1111/medu.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smith M, Donnelly GM, Berry L, Innes S, Dixon J. Point of care ultrasound in pelvic health: Scope of practice, education and governance for physiotherapists. Int Urogynecol J. 2022;33:2669–80. doi: 10.1007/s00192-022-05200-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smith M, Hayward S, Innes S. A proposed framework for point of care lung ultrasound by respiratory physiotherapists: Scope of practice, education and governance. Ultrasound J. 2022;14:24. doi: 10.1186/s13089-022-00266-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reeve R, Higginson A, Ball C, Beable R, Smith M. Role extension in advanced ultrasound practice: A framework approach and case study. Ultrasound. 2023;31:4–10. doi: 10.1177/1742271X221102577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Allen JE, Cleland J, Smith M. An initial framework for use of ultrasound by speech and language therapists in the UK: Scope of practice, education and governance. Ultrasound. 2023;31:92–103. doi: 10.1177/1742271X221122562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Savatmongkorngul S, Wongwaisayawan S, Kaewlai R. Focused assessment with sonography for trauma: Current perspectives. Open Access Emerg Med. 2017;9:57–62. doi: 10.2147/OAEM.S120145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mavilia MG, Pakala T, Molina M, Wu GY. Differentiating cystic liver lesions: A review of imaging modalities, diagnosis and management. J Clin Transl Hepatol. 2018;6:208–16. doi: 10.14218/JCTH.2017.00069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Royal College of Emergency Medicine (RCEM) Curriculum. 2021. [[Last accessed on 2022 Feb 02]]. Available from: https://rcem.ac.uk/curriculum/
- 39.Royal College of Emergency Medicine (RCEM) Ultrasound Education and Training Sub-Committee. RCEM 2021 Curriculum Ultrasound Education and Training. [[Last accessed on 2022 May 06]]. Available from: https://res.cloudinary.com/studio-republic/images/v1651663913/EM_PoCUS_2021_Curriculum-FAQ_29_April_22_AGREED/EM_PoCUS_2021_Curriculum-FAQ_29_April_22_AGREED.pdf?_i=AA .
- 40.Canadian Association of Emergency Physicians (CAEP) Recommendations for the Use of Point of-care Ultrasound (PoCUS) by Emergency Physicians in Canada. Ottawa: Canadian Association of Emergency Physicians (CAEP); 2018. [[Last accessed on 2021 Nov 18]]. Available from: https://caep.ca/wp-content/uploads/2018/11/CAEP-PoCUS-Position-Statement-Full-Text-2018-V7-draft.pdf . [Google Scholar]
- 41.American College of Emergency Physicians (ACEP) Ultrasound Guidelines: Emergency, Point of-care, and Clinical Ultrasound Guidelines in Medicine. Irving: American College of Emergency Physicians (ACEP); 2016. [[Last accessed on 2021 Nov 18]]. Available from: https://www.acep.org/patient-care/policy-statements/ultrasound-guidelines-emergency-point-of-care-and-clinicalultrasound-guidelines-in-medicine/ [Google Scholar]
- 42.International Federation for Emergency Medicine (IFEM) Point-of-care Ultrasound Curriculum Guidelines. Melbourne: International Federation for Emergency Medicine (IFEM); 2016. [[Last accessed on 2021 Nov 18]]. Available from: https://www.ifem.cc/wp-content/uploads/2016/07/IFEM-Pointof-Care-Ultrasound-Curriculum-Guidelines-2014.pdf . [Google Scholar]
- 43.Wells M, Goldstein LN, Beringer C, Farham B. Emergency medicine society of South Africa guidelines for the training and credentialing in emergency point-of-care ultrasound. S Afr Med J. 2021;111:13296. doi: 10.7196/SAMJ.2021.v111i5b.15346. [DOI] [PubMed] [Google Scholar]
- 44.World Health Organization. Strategic Directions to Integrate Emergency Care Services into Primary Health Care in the South-East Asia Region. New Delhi: World Health Organization, Regional Office for South-East Asia; 2020. [[Last accessed on 2022 Feb 18]]. Licence: CC BY-NC-SA 3.0 IGO;2020. Available from: https://apps.who.int/iris/handle/10665/336568 . [Google Scholar]
- 45.Mani N. Implementing a quality framework for storing emergency department point-of-care ultrasound examinations on a picture archiving and communication system. Ultrasound. 2021;29:252–9. doi: 10.1177/1742271X21990069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fleming KA, Horton S, Wilson ML, Atun R, DeStigter K, Flanigan J, et al. The lancet commission on diagnostics: Transforming access to diagnostics. Lancet. 2021;398:1997–2050. doi: 10.1016/S0140-6736(21)00673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Abraham SV, Melit RJ, Krishnan SV, George T, Kunhahamed MO, Kassyap CK, et al. Indigenously developed ultrasound phantom model versus a commercially available training model: Randomized double-blinded study to assess its utility to teach ultrasound guided vascular access in a controlled setting. J Med Ultrasound. 2022;30:11–9. doi: 10.4103/JMU.JMU_48_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.National Medical Commission. [[Last accessed on 2022 Feb 18]]. Available from: https://www.nmc.org.in/rules-regulations/minimum-requirements-for-annual-m-b-b-s-admissions-regul-ation2020/
- 49.Indian Council of Medical Research. National Essential Diagnostics List. New Delhi: Indian Council of Medical Research; 2019. [[Last accessed on 2021 Nov 18]]. Available from: https://main.icmr.nic.in/-sites/default/files/guidelines-/NEDL_2019.pdf . [Google Scholar]