1. Background
In the United States, childhood obesity rates have steadily risen for more than three decades. As of 2018, 16.1% of U.S. children and adolescents (2–19 years of age) have a body mass index (BMI) greater than the 85th percentile for age and sex (overweight) and 19.3% have a BMI greater than the 95th percentile (obesity) [1]. Multiple obesity prevention and treatment efforts, with particular attention directed to the first 1000 days of life, have been implemented with the goal of improving childhood nutrition and health [2]. Despite countless efforts, the prevalence of obesity in U.S preschool children (2–5 years) currently approaches 13 percent [3,4].
Pediatric obesity does not affect communities equally, with minoritized groups and specific geographic areas experiencing disproportionately higher obesity rates. Among children and adolescents aged 2–19 years, prevalence of obesity affects non-Hispanic Blacks (25.1%), Mexican Americans (24.9%), Hispanics (23.0%), American Indian/Alaska Native (AI/AN) (29.7%), and Native Hawaiian or Other Pacific Islander (NHPI) (23% at 8 years of age) at higher rates compared to non-Hispanic Whites (14.7%) [1,5,6].
Many of the racialized differences in obesity rates reflect inequities that are “neither natural nor inevitable” [7] but rather the result of unfair social structures or institutional practices that confer unearned privilege to one group while subjugating another group [8]. Additionally, obesity is a complex disease that results from complicated interactions with, and reactions to, social, environmental, and biological variables that can affect mood, energy regulation, and health status.
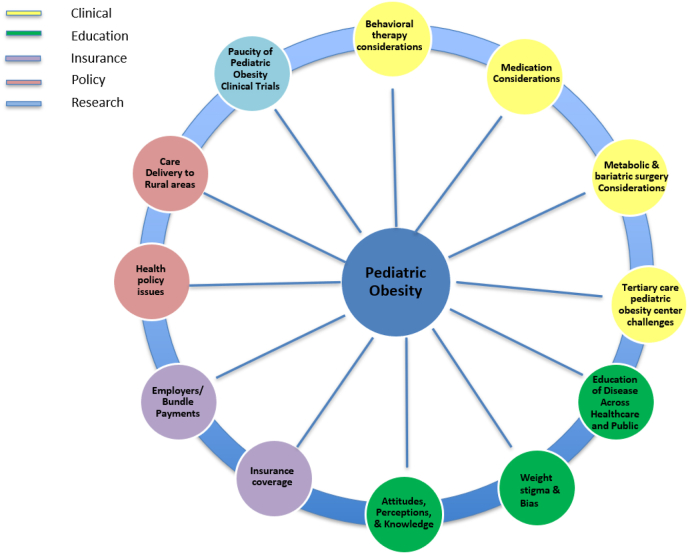
The complexity of obesity spans a lifetime. Obesity in childhood increases the risk of pediatric cardiovascular disease, diabetes, depression, and anxiety while also increasing the risk of obesity and premature death in adulthood. To develop a comprehensive, inclusive and equitable framework for the treatment and prevention of childhood obesity, clinicians are encouraged to evaluate the root causes of the inequitable access, prevalence, and outcomes observed among minoritized communities. Insight into lived experiences and the context in which the child and family views historical and present-day life are invaluable in this effort. This paper will shed light on upstream contributors to obesity, provide actionable steps for clinicians, identify gaps in obesity-related care, and propose future directions for childhood obesity management and research (Fig. 1).
Fig. 1.
Factors contributing to obesity.
2. Upstream factors contributing to obesity
2.1. Epigenetic modification, toxic stress, and adverse childhood experiences
2.1.1. Case study 1: Antonia and Daniela
15-year-old Daniela is accompanied by her mother, Antonia, to establish care and discuss weight gain and a dark rash on her neck. Past medical history is negative; however, Antonia was recently diagnosed with type 2 diabetes (T2D) after suffering from gestational diabetes (GDM) with each of her pregnancies. Daniela's pattern of weight gain and dark rash have worsened in the past year. Two years ago, Daniela and her family immigrated from Honduras after her father was killed during an armed home invasion. She now lives in a multigenerational household that includes her mother, 2 younger siblings, maternal grandmother as well as maternal aunt and her 3 children. She attends the local public high school where she plays on the soccer team – which was unavailable at her former school due to neighborhood violence. The family eats traditional Honduran meals for dinner, otherwise Daniela eats very little during the day; she skips breakfast most days and drinks soda with chips for lunch. On physical exam, the BMI is 38 (>95th percentile) and acanthosis nigricans is noted on the neck and axillae.
2.1.2. Epigenetic modifications
Daniela's story introduces the concept of epigenetics, or the study of how environment and behavior may lead to changes that affect gene function. Whereas genetic changes are irreversible and alter DNA sequences within genes, epigenetic changes are modifiable, reversible, and exert their influence on the gene expression of DNA sequences [9]. Epigenetic modifications may affect infants as they develop in-utero, and later in childhood. Maternal factors during pregnancy such as gestational diabetes, excessive weight gain, or tobacco use can manifest as epigenetic modifications that contribute to the development of pediatric obesity [10]. In the case of Daniela, her mother suffered from gestational diabetes during all 3 of her pregnancies and lived in a neighborhood affected by community violence. Postnatal environmental factors (high carbohydrate diet with few fruits and vegetables, inadequate sleep, and physical inactivity) are associated with epigenetic changes that increase the risk of obesity [2]. Additional associated threats for epigenetic changes include racial inequities and structural racism, adverse childhood events (ACEs), food insecurity, food deserts, housing instability, and community violence and disruption [11,12].
2.1.3. Toxic stress
Current literature suggests that chronic, toxic stress experienced through poor social determinants of health (SDOH), and life events can lead to obesity in children through two distinct physiological pathways: disruption of the hypothalamic-pituitary-adrenal (HPA) axis from allostatic overload and through epigenetic modifications [[13], [14], [15], [16]]. The body normally responds to stress through heightened energy and hormonal responses to meet the perceived threat until the stress is passed. Threats that are severe, constant or ongoing become toxic and may overtax the normal stress response [17]. Allostatic load is the term for the cumulative effect of life stressors (chronic or episodic) on the body [18]. Allostatic overload occurs when the body is unable to successfully manage these stressors. Chronic inflammation, diminished immune response, and energy dysregulation are end-results of allostatic overload [18]. In a comprehensive approach to patients and families similar to Daniela who are affected by obesity, clinicians are encouraged to consider the role of chronic, pervasive, toxic stress in the development and progression of obesity.
2.1.4. Adverse childhood experiences (ACEs)
The landmark study on ACEs identified 3 major categories of adversity experienced in childhood (household dysfunction, abuse, and neglect) which were strongly associated with increased risk of poor health [19]. As the number of ACEs that an individual experienced increased, so did the risk for adverse health outcomes such as obesity, cardiometabolic diseases, diabetes, substance abuse, depression, and suicide attempts [19,20]. Amongst middle-class, insured individuals, greater than two-thirds experienced at least one ACE and nearly 25% experienced 3 or more ACEs [20].
ACEs are associated with childhood obesity, albeit signs may be delayed, presenting as many as 5 years after the traumatic event [21]. The prevalence of ACEs is higher in children and adults from minoritized groups compared to predominantly White communities [[22], [23], [24], [25], [26]]. This association may partially explain the higher burden of poor health and life outcomes experienced by minoritized groups. The original ACEs study measured conventional ACEs (ACE-C) which assessed individuals in middle to upper middle-class communities, focusing on parameters within the home such as abuse, neglect, and household dysfunction [19]. Cronholm et al. studied a more socioeconomically and racially diverse urban population, expanding the ACE-C to include experiences within the community [27]. The expanded ACEs (ACE-E) include witnessing or experiencing community violence, placement in foster care, death of family member, and witness to frequent interpersonal or community conflict. Cronholm's results revealed that 72.9% of 1784 respondents experienced at least one ACE-C, 63.4% at least one ACE-E, and 49.3% experienced at least one of both. Most importantly, 13.9% experienced only ACE-E, suggesting that conventional ACE assessment would have missed risk factors more common in communities with more racial, ethnic and socioeconomic diversity [27].
2.1.5. Upstream contributors for immigrants
Some immigrant children like Daniela, are at high risk for chronic stress or trauma from racism, unsafe neighborhoods in country of origin, and relocation to another community or country [28]. Other potential stressors include food insecurity, limited (if any) access to health care, and fears of family separation. Poor health literacy, exacerbated by the absence of written materials and instructions in the patient's preferred language, can hinder an immigrant family's ability to manage chronic diseases including obesity and diabetes [29].
2.1.6. Case 1 actionable steps
Providers can (1) strive to learn more about patient's history and living situation, (2) use Trauma Informed Care (TIC) principles, and (3) address health literacy and cultural barriers. TIC asks clinicians to consider the role that trauma and lingering traumatic stress plays in the lives of their patients. Trauma-informed care considers physical, emotional, social, or historical trauma which can all have harmful effects on mental and physical health [30]. Clinicians can use a “trauma lens” to provide patients and their families with the tools for building supportive relationships and fostering resilience [31,32]. With over 40% of children and adolescents experiencing four or more different types of traumas and adversity [33] and because trauma is more common in families experiencing health inequities, all health systems and practices treating child obesity are encouraged to increase awareness and uniformly implement trauma-informed care techniques [34]. Table 1 describes strategies for the use of trauma informed care principles.
Table 1.
Strategies for trauma informed care (TIC).
| Core Principles of Trauma-Informed Care & Related Actions | ||
|---|---|---|
| RealizeUnderstand broad impact of trauma | Understand short and long-term impact of ACEs and toxic stress on development and health | Shift perspective from “what is wrong with you?” to “what happened to you?” |
| ACEs have physiological, biological, psychological, social, and spiritual effects on children | ||
| RecognizeSigns & symptoms of trauma in families | Use open ended questions | Assess for physiological, biological, psychological, social, and spiritual effects: suicidality, depression, anxiety, substance abuse, self-injurious behavior, developmental delay, sleep disorders, disordered eating and relational health. |
| Screen for trauma for every child, every visit | Tool: Pediatric ACEs screening and related life-events screener | |
| RespondCoordination of response to trauma particularly with family, community, and health care systems | Anticipatory guidance: Resilience promotion, ACEs education, consistency in parenting skills | |
| Resist Re-traumatizationUniversal trauma precautions for both caregivers and care receivers | Approach all children & families with trauma universal precautions mindset | TIC and resiliency training for all personnel interacting with children and families. |
| Promote a culture of TIC in organizations and communities | ||
ACEs = Adverse Childhood Experiences; TIC = Trauma informed care.
Daniela's history indicates a high risk of epigenetic changes from toxic stress related to ACEs, maternal GDM and T2DM, community violence, and witnessing the death of her father. Learning more about Daniela's history and current living situation helps her clinician consider and address sources of trauma. In order to provide care that supports the family and does not retraumatize, the clinician uses TIC principles to recognize the impact of potential, unspoken traumas brought to any clinical encounter. TIC technique are provided in Table 1 [32,34,35]. By addressing health literacy, language and cultural barriers, the clinician provides patients like Daniela with culturally relevant counseling and resources. Table 2 illustrates the impact of epigenetics, toxic stress, and ACEs through the case study of Antonia and Daniela.
Table 2.
Case study 1: Antonia and Daniela – epigenetics, toxic stress, and ACEs.
| Actionable Steps |
|
| Plan |
|
| Follow-up | Daniela returns to clinic 8 weeks later with evidence of weight stabilization and linear growth (BMI 37.5). She's eating breakfast at 4 times per week and has noticed that she has more energy. After a few weeks in intramural soccer, she had to quit because the family couldn't afford childcare for the younger siblings and cousins. However, now that they're living in a safer neighborhood, Daniela takes them to the park to play games (i.e. soccer, kickball, etc.) at least 3 times per week and once on the weekend. If it rains, they have a dance party at home. |
2.2. Historical trauma
2.2.1. Case study 2: Susan and Charlie
Charlie is a 32-week male born vaginally to a 27-year-old Choctaw mother, Susan, after premature rupture of membranes and labor. Charlie was born at the local hospital near the Choctaw reservation but required transfer to a regional neonatal intensive care unit (NICU) 50 miles away. The pregnancy was complicated by late prenatal care, gestational diabetes, and depression. After learning of the gestational diabetes, Susan became distraught and afraid, thinking about her many relatives with diabetes who required daily injections, experienced blindness, or underwent limb amputation. She has watched her relatives attempt to follow both tribal and western medicine. Susan lives on the Choctaw Indian Reservation with her husband and 3 generations of her family, as most of them have been awaiting housing assistance for years. Though she has remained sober for 11 years, multiple family members continue to struggle with alcohol use disorder.
2.2.2. The impact of historical trauma
The story of Susan and Charlie invokes images of historical trauma or the cumulative, multigenerational, collective experience of emotional and psychological injury experienced by specific cultures, races, or ethnic communities [36]. Intertwined through the interpersonal and collective experience, examples of historical trauma include enslavement, displacement (i.e. internment camps, Indian reservations), exploitation, and cultural disruption, often resulting in unresolved grief [36]. The combined emotional and psychological stresses of historical trauma impact individuals over the lifespan and across generations, stemming from massive group trauma experiences that result in cumulative and self-perpetuating consequences [37]. Younger generations of traumatized groups, who did not experience the original traumatic event, may still manifest symptoms of trauma such as low self-esteem, self-destructive behaviors, depression, anxiety and suicidality [37,38]. Susan's multigeneration household struggles with housing instability, substance use disorder and chronic disease, likely related to historical trauma, ACEs, toxic stress and epigenetic modification.
Because of familiarity with Choctaw culture, beliefs, and historical trauma, the NICU clinical team understood the barriers that Susan experienced in seeking care at the Indian Health Service, as well as her fears, mental health, and substance abuse issues. After his premature birth, Charlie's NICU clinical team screened for ACEs, SDOH, and used TIC methodology. This enabled Susan's clinician to provide more informed, empathetic care for Charlie and his family as well as offer appropriate community and cultural resources.
2.2.2. Case study 2 actionable steps
Clinicians can develop an understanding of the histories and cultures of the communities they serve, mindful that not all members of a community will have the same experiences or beliefs. Knowledge of traditional beliefs are helpful in designing integrative approaches to healing and incorporating them into clinical practice to provide culturally appropriate and safe care [33]. Trauma informed technique are included in Table 1 and resources in Appendix [32,34,35]. Table 3 illustrates the impact of historical trauma through the case study of Susan and Charlie.
Table 3.
Case study 2: Susan and Charlie - historical trauma.
| Assessment | Charlie is a 32-week gestational age Choctaw male, born to a mother with obesity, gestational diabetes and a history of alcoholism. |
| Additional History |
|
| |
| |
| |
| NICU Course & Discharge |
|
| |
| Follow-up | At the 2-month well visit, Susan is relieved when a Community Health Worker (CHW) greets her in Choctaw and offers to take Charlie's car seat. |
| |
| |
| Actionable Steps |
|
| |
| |
|
IHS=Indian Health Service.
2.3. Structural racism and social determinants of health
2.3.1. Case study 3: Rachel and Macy
Macy is a 9-month-old African American female who presents with her grandmother, Rachel, for an office visit to discuss decreased intake. Macy's weight-for-length is at the 99th percentile for age. Macy's 20-year-old mother, Renee, died within hours of delivery. The family was told it was from complications of high blood pressure but Rachel seems unsure. She has cared for Macy since birth. Macy's diet currently includes formula, juice and some table foods. Macy lives in a 2-bedroom apartment with her grandmother and boyfriend, and 2 other children ages 14 and 16 years – Macy's maternal aunt and uncle. The family would like to move out but have not been approved for home loans to afford a big enough house in a better neighborhood. They tried to rent a house, but each time the home suddenly becomes “unavailable” when the landlord meets Rachel and her boyfriend in person. The last time they looked at a property, one of the neighbors called the police complaining of “dangerous looking people lurking around.”
2.3.2. Structural racism
Black maternal health inequities. Food deserts. Redlining. Profiling. Structural racism serves as a chronic and insidious accelerator of adverse environments and experiences which contribute to inequities in the prevalence of childhood obesity, infant mortality and low birth weight, and higher maternal morbidity and mortality among Black women [39,40]. A systematic review examining the relationship between racial discrimination and child health in 121 studies found significant results in 76%, and associations between racial discrimination and negative mental health [40]. The 2021 National Healthcare Quality and Disparities Report found that quality measures tracking person-centered care, patient safety, healthy living, effective treatment, care coordination, and affordable care were worse for Black (43% of quality metrics), Hispanic (36%), AI/AN (40%), Asian (28%), and NHPI (28%) individuals when compared to White counterparts [41]. The report noted that reduced health care access in minoritized groups was unchanged from annual reports over previous two decades [41]. The historical and intentional exclusion of certain minoritized groups coupled with disinvestment of specific neighborhoods that include predominantly Black, Indigenous and People of Color have contributed to the modern-day racial segregation of neighborhoods and communities. The inadequate resources of healthcare facilities and fewer primary care and subspecialty clinics result in reduced access to healthcare in these minoritized communities [42], leading to higher rates of obesity and other chronic diseases [15]. Chronic stress from racism as experienced through practices exemplified by racialized residential segregation (redlining), police violence and mass incarceration, and healthcare inequities affects individual and community health [14]. The combined interactions of ACEs, SDOH, racism, epigenetics, and historical trauma and the resultant toxic stress can accelerate and exacerbate the risk of obesity in susceptible children and adults [43].
2.3.3. Structural racism and immigrants
A literature review by Misra et al. considers how structural racism uniquely impacts the health of racialized immigrants [29]. The authors propose that structural disadvantages for immigrants are embedded into governmental and institutional policies and impact immigrant health via three pathways: formal racialization via immigration policy and citizenship status; informal racialization via disproportionate immigration enforcement and criminalization including ongoing threats of incarceration and deportation; and economic exploitation and disinvestment [29]. Racialized policies impact immigrant health through psychosocial experiences (fear, stress, and trauma); inequitable access to essential resources (food, employment, housing, and health care quality); and experiences of discrimination, neglect, violence, and abuse [[44], [45], [46], [47], [48]].
2.3.4. Social determinants of health
The case of Rachel and Macy underscores how social determinants of health can influence a child in utero and after delivery (Table 4). SDOHs are environmental conditions which influence a wide range of health outcomes and quality of life. Poor SDOHs are disproportionately experienced by children from racial and ethnic minoritized groups [49]. The common theme among the constructs of SDOH and structural racism is that upstream factors have downstream effects that manifest in measurable adverse health outcomes including obesity in children [50]. SDOHs are influenced by economic, political, and social factors, including racism, and are not the result of individual behavior choices or a genetic predisposition [51]. The American Academy of Pediatrics states that racism is a core social determinant of health that drives health inequities in children [52].
Table 4.
Case 3: Rachel and Macy - social determinants of health and structural racism.
| Birth & Family Medical Histories | Birth History: Macy's mother, Renee, worked part-time while going to school to become a nursing assistant. She did not realize she was pregnant until 10 weeks due to a history of irregular periods but was not able to establish prenatal care until the second trimester (16 weeks) because of appointment availability and her work schedule. Renee later developed gestational diabetes and pregnancy-induced hypertension. |
| Family Medical History: Mother: Renee had a history of obesity since childhood. Maternal Grandmother: Rachel has a history of obesity and tobacco use. Rachel has been divorced for more than 10 years – after enduring years of fear and uncertainty related to her husband's substance abuse disorder. For years afterward, she and her children, including Renee, lived “hand-to-mouth” despite her working as Program Coordinator of a youth literacy program. Rachel is discouraged. She feels Macy's health and Renee's death are due to being under constant stress, not to mention the lack of access to fresh affordable food and produce. There are no grocery stores in her neighborhood – only overpriced corner stores that sell mostly alcohol and cigarettes. The closest grocery story is a 30-minute bus ride away. | |
| Assessment | Macy is a 9-month-old female with elevated weight-for-length with multiple negative social determinants of health |
| Actionable Steps |
|
| |
| |
| Additional History & Discharge Plan |
|
| |
| |
| Follow-up |
|
|
2.3.5. Case Study 3 Actionable Steps
Approaching the patient and family with respectful curiosity of their story unmasks upstream contributors, directs areas of concern to better focus treatment, and suggests possible interventions. Root causes of chronic stress emerge as clinicians ask “What has happened to you and your family? Tell me your story.” Strictly counseling on diet and physical activity can be ineffective if upstream barriers are not considered. Upstream barriers include, among others, unaddressed food insecurity, lack of transportation, and undiagnosed maternal or caregiver depression which may lead to difficulty maintaining employment for financial stability, adhering to subsequent health maintenance appointments, and contribute to abnormal growth and mental health issues for the child. A more nuanced awareness of intentional exclusion and historical disinvestment of neighborhoods aids treatment plans when considering the family's living environment, housing stability, community safety, and proximity to services including food, school, and healthcare. Table 4 demonstrates, through the story of Macy and Rachel, the intersectionality of structural racism and SDOH with factors described in other cases, i.e., toxic stress, adverse childhood experiences, health inequities. Table 5 offers practice and personal-level opportunities for clinicians to address structural racism.
Table 5.
Steps to address racism and develop resiliency.
| Steps to Address Structural Racism |
|---|
|
|
|
|
|
|
|
| Steps to Develop Resilience in Children & Families | |
|---|---|
| Assessevery child, every visit |
|
| |
| |
| |
| |
| Education |
|
| |
| |
| |
| |
| Promote Self-care |
|
| |
| |
| |
| |
Adapted from Garner et al., 2021; Goddard, 2021; National Association of Pediatric Nurse Practitioners, 2019.
2.4. Latent adverse childhood experiences
2.4.1. Case study 4: Elizabeth and Gary
Gary is an 18-month-old White male who presents for a well child visit. His mother, Elizabeth, is concerned because Gary is very clingy and doesn't talk as much as his 16-month-old cousin. Gary's weight-for-length is at the 99th percentile for age. His birth and medical histories are uncomplicated. Elizabeth received early prenatal care and experienced a “healthy” pregnancy that included adequate exercise, normal weight gain, blood sugar, and blood pressure. Gary was delivered at 39 weeks (birth weight 7 lbs. 14 oz). He was exclusively breastfed until six months of age then transitioned to baby food. Gary continues breastfeeding in addition to eating a variety of table foods, fruits and vegetables. Elizabeth works as elementary school teacher and has employer-sponsored health insurance that covers the cost of the breast pump she uses while at work. Since his parents' divorce, Gary lives with mother.
Despite having adequate financial resources, a safe community, access to health care, healthy affordable foods, and employer-sponsored health insurance, 18-month Gary developed obesity and speech delays possibly due to other risk factors. Using the Safe Environment for Every Kid (SEEK) Questionnaire, Gary screened positive for ACEs including maternal depression, domestic violence, and divorced parents [54]. Parental stressors, parental divorce and intimate partner violence can increase the risk of obesity as well as mood disorders, speech delay, and other developmental issues [55]. Unconscious or implicit bias may lead some to believe there are no “obvious” risk factors for ACEs and obesity in this case. Though the risk factors may be “hidden,” universal ACEs screening and careful history-taking assists in the discovery of such risk factors and guides clinical care. The ultimate goals are to decrease chronic stress and optimize treatment strategies.
2.4.2. Case study 4 actionable steps
ACEs constitute any potentially traumatic events that are perceived stressful to the recipient. While some ACEs may seem obvious, other events such as maternal history of depression, intimate partner violence, weight-based victimization, or peer rejection may be more difficult to detect. Consider ACEs screening for every child, but especially children with obesity, developmental delay, risk for historical trauma, or parental history of mental health disorders.
When medical practices strive to develop medical homes where every parent feels acknowledged and supported, the practice can build supportive relationships that cultivate resilience in children. Vigilance is needed to provide systematic, routine screenings to help with early detection of changes in social or household resources. To potentially mitigate the harmful effects of ACEs, clinicians are encouraged at every encounter to ask about, and listen to the stories of parents, caregivers, and children, regardless of their perceived risk.
While evaluating for past trauma is important, assessment must be balanced with the ability to provide appropriate support of what is discovered at the encounter. Providers can become familiar with supportive community resources, such as social workers, counselors, shelters or support groups, food banks, and cultural centers. Universally employ the four “R” components of trauma informed care as hidden trauma may exist in any patient or family: Realize, Recognize, Respond, and Resist Re-traumatization (Table 1) [32,34,35] [Appendix 1]. Finally, the Substance Abuse and Mental Health Services Administration (SAMHSA) publication on trauma informed approach can further inform providers and their practices [56]. Table 6 illustrates the impact of ACEs through the story of Elizabeth and Gary.
Table 6.
Case 4: Elizabeth and Gary - Easy to miss ACES.
| Assessment | Gary is an 18-month-old male with weight-for-length > 95th percentile and possible speech delay. There are no obvious risk factors for obesity or speech delay. |
| Actionable Steps | Medical Assessment: Screen every patient with obesity for ACEs and home environmental safety |
| |
| |
| |
| |
| Additional History & Discharge Plan |
|
| |
| |
| |
| Follow-Up |
|
| |
| |
|
EAP = Employee Assistance Program.
3. Discussion
Childhood obesity is a challenging disease to treat. To devise effective strategies for prevention and treatment of childhood obesity, we need to first acknowledge and understand the factors contributing to disparate prevalence and inequitable outcomes found in minoritized and other communities. By acknowledging the role of upstream contributors, pediatric clinicians are able to engage in strategies to optimize the health and well-being of their patients [52].
In addition to the actionable steps discussed earlier, clinicians can benefit from utilizing tools such as The Implicit Association Test to help explore personal biases [57]; engage in community activities or educational offerings that augment an understanding of upstream contributing factors to obesity; and continue to be curious to learn their patients’ histories and stories in order to build empathy and reduce frustration in treatment progress [58]. Providers can also consider universal screening for ACEs and SDOH.
The treatment approach to obesity has historically been overly simplified with a narrow focus of “energy in = energy out”. While diet and exercise are important, they do not tell the whole story or begin to explain the complex interactions of the upstream factors discussed in this paper. Providers are encouraged to look beyond this insufficient model of energy balance, to address historical trauma and other external contributors to health disparities including childhood obesity.
The cases of Daniela, Charlie, Macy, and Gary highlight why the status quo has not been successful in reducing childhood obesity. Providers cannot effectively treat childhood obesity without exploring and addressing the impact of upstream contributors like epigenetics, ACEs, toxic stress, structural and immigrant racism, SDOH, and latent ACEs. By understanding health disparities, we can reframe obesity and its disproportionate prevalence to focus on addressing modifiable risk factors.
4. Conclusion
While this review describes several upstream factors contributing to childhood obesity and offers actionable steps to incorporate into in clinical practice, there are likely many other factors yet to be identified. Furthermore, implementation of actionable steps may come with challenges as clinicians often encounter barriers to optimize obesity management in their practices [59]. Fig. 2 depicts several barriers to both clinicians and patients, not to mention additional barriers like unmet or unrealistic expectations, inadequate practice space or support services to deliver weight management, and lack of clinical experience. Future research can help to determine best practices in integrating new information into obesity and weight management, clinician education, and the healthcare systems. Continued diligence and curiosity combined with additional investment in clinical research and community resources will assist clinicians in providing targeted care to children and adolescents with obesity.
Fig. 2.
Barriers to Pediatric Obesity Care∗. ∗Figure used with permission [59].
Clinicians may also benefit from acknowledging how their approach to childhood obesity may be influenced by their beliefs and lived experiences, and their lack of familiarity with these and other upstream contributors. Clinicians can reimagine clinical care and practice workflow to address obesity by incorporating the practice of trauma-informed care, and implementing the actionable items discussed in this article. Given the increasing rate of obesity among children and adolescents, clinicians and patients alike will benefit from an approach to care that includes a more comprehensive and inclusive framework.
Author contribution (CRediT authorship contribution statement)
All authors were involved in the conception of the article, contributed to the literature searches and identification of pertinent articles, critically reviewed the manuscript, and had final approval of the submitted version.
Ethical review
This submission represents the original work of the authors supported by appropriately cited professional literature. This work did not involve human subjects.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations of competing interest
None.
Acknowledgements
The authors thank Amy Randall-McSorley, MS, EdD for her critical reading and editing of the manuscript. The authors gratefully acknowledge the graphic art assistance of Amy R. Sharn, MS, RDN, LD in the preparation of Fig. 1. This manuscript received no funding.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.obpill.2022.100040.
Contributor Information
Dominique R. Williams, Email: Dominique.Williams@NationwideChildrens.org.
Amy Braddock, Email: WilliamsAmy@health.missouri.edu.
Marcella Houser, Email: Mhouse@lsuhsc.edu.
Giselle Blair, Email: gblairmd@gmail.com.
Nancy Browne, Email: nancytkacz@sbcglobal.net.
Appendix A. Supplementary data
The following are the supplementary data related to this article:
References
- 1.Fryar C.D., Carroll M.D., Afful J. Centers for Disease Control & Prevention; 2020. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2017–2018. Published. [Google Scholar]
- 2.Schwarzenberg S.J., Georgieff M.K., Committee on Nutrition Advocacy for improving nutrition in the first 1000 days to support childhood development and adult health. Pediatrics. 2018;141(2) doi: 10.1542/peds.2017-3716. [DOI] [PubMed] [Google Scholar]
- 3.Data, trend and maps. Centers for disease control and prevention. https://www.cdc.gov/nccdphp/dnpao/data-trends-maps/index.html Updated November 21 website.
- 4.Pan L., Freedman D.S., Sharma A.J., et al. Trends in obesity among participants aged 2-4 Years in the special supplemental nutrition program for Women, Infants, and Children - United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 2016;65(45):1256–1260. doi: 10.15585/mmwr.mm6545a2. [DOI] [PubMed] [Google Scholar]
- 5.Bullock A., Sheff K., Moore K., Manson S. Obesity and overweight in American Indian and Alaska Native children. Am J Publ Health. 2017;107(9):1502–1507. doi: 10.2105/AJPH.2017.303904. 2006-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Novotny R., Fialkowski M.K., Li F., et al. Systematic review of prevalence of young child overweight and obesity in the United States affiliated Pacific Region compared with the 48 contiguous states: the Children's Healthy Living Program. Am J Publ Health. 2015;105(1):e22–e35. doi: 10.2105/AJPH.2014.302283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Advancing health equity: guide on language, narrative and concepts. American Medical Association and Association of American Medical Colleges. https://www.ama-assn.org/about/ama-center-health-equity/advancing-health-equity-guide-language-narrative-and-concepts-0 Published 2021
- 8.Jones C.P. Levels of racism: a theoretic framework and a gardener's tale. Am J Publ Health. 2000;90(8):1212–1215. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Genomics and precision health. Centers for disease control and prevention. https://www.cdc.gov/genomics/disease/epigenetics.htm website. Updated August 3, 2020.
- 10.Cuda S., Censani M., O'Hara V., Browne N.T., Paisley J. Pediatric obesity algorithm eBook. https://obesitymedicine.org/childhood-obesity/ presented by the Obesity Medicine Association 2020-2022. Updated September 2020.
- 11.Leifheit K.M., Schwartz G.L., Pollack C.E., et al. Eviction in early childhood and neighborhood poverty, food security, and obesity in later childhood and adolescence: evidence from a longitudinal birth cohort. SSM Popul Health. 2020;11 doi: 10.1016/j.ssmph.2020.100575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.A public health framework for reducing health inequities. BARHII: Bay Area Regional Health Inequities Initiative. 2020. http://barhii.org/framework/ Published.
- 13.Cedillo Y.E., Murillo A.L., Fernández J.R. The association between allostatic load and anthropometric measurements among a multiethnic cohort of children. Pediatr Obes. 2019;14(6) doi: 10.1111/ijpo.12501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jones N.L., Gilman S.E., Cheng T.L., Drury S.S., Hill C.V., Geronimus A.T. Life course approaches to the causes of health disparities. Am J Publ Health. 2019;109(S1):S48–S55. doi: 10.2105/AJPH.2018.304738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paradies Y., Ben J., Denson N., et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One. 2015;10(9) doi: 10.1371/journal.pone.0138511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wiss D.A., Brewerton T.D. Adverse childhood experiences and adult obesity: a systematic review of plausible mechanisms and meta-analysis of cross-sectional studies. Physiol Behav. 2020;223 doi: 10.1016/j.physbeh.2020.112964. [DOI] [PubMed] [Google Scholar]
- 17.Timper K., Brüning J.C. Hypothalamic circuits regulating appetite and energy homeostasis: pathways to obesity. Dis Model Mech. 2017;10(6):679–689. doi: 10.1242/dmm.026609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fava G.A., McEwen B.S., Guidi J., Gostoli S., Offidani E., Sonino N. Clinical characterization of allostatic overload. Psychoneuroendocrinology. 2019;108:94–101. doi: 10.1016/j.psyneuen.2019.05.028. [DOI] [PubMed] [Google Scholar]
- 19.Felitti V.J., Anda R.F., Nordenberg D., et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 20.Vital signs: adverse childhood experiences (ACEs) Centers for Disease Control and Prevention website; 2019. https://www.cdc.gov/vitalsigns/aces/index.html Updated November 3. [Google Scholar]
- 21.Schroeder K., Schuler B.R., Kobulsky J.M., Sarwer D.B. The association between adverse childhood experiences and childhood obesity: a systematic review. Obes Rev. 2021;22(7) doi: 10.1111/obr.13204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Borysova M.E., Mitchell O., Sultan D.H., Williams A.R. Racial and ethnic health disparities in incarcerated populations. J Health Dispar Res Pract. 2012;5(2):92–100. [PMC free article] [PubMed] [Google Scholar]
- 23.Giano Z., Camplain R.L., Camplain C., et al. Adverse childhood events in American Indian/Alaska Native populations. Am J Prev Med. 2021;60(2):213–221. doi: 10.1016/j.amepre.2020.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giovanelli A., Reynolds A.J. Adverse childhood experiences in a low-income black cohort: the importance of context. Prev Med. 2021;148 doi: 10.1016/j.ypmed.2021.106557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Crouch E., Probst J.C., Radcliff E., Bennett K.J., McKinney S.H. Prevalence of adverse childhood experiences (ACEs) among US children. Child Abuse Negl. 2019;92:209–218. doi: 10.1016/j.chiabu.2019.04.010. [DOI] [PubMed] [Google Scholar]
- 26.Mersky J.P., Choi C., Plummer Lee C., Janczewski C.E. Disparities in adverse childhood experiences by race/ethnicity, gender, and economic status: intersectional analysis of a nationally representative sample. Child Abuse Negl. 2021;117 doi: 10.1016/j.chiabu.2021.105066. [DOI] [PubMed] [Google Scholar]
- 27.Cronholm P.F., Forke C.M., Wade R., et al. Adverse childhood experiences: expanding the concept of adversity. Am J Prev Med. 2015;49(3):354–361. doi: 10.1016/j.amepre.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 28.Perreira K.M., Ornelas I. Painful passages: traumatic experiences and post-traumatic stress among immigrant Latino adolescents and their primary caregivers. Int Migr Rev. 2013;47(4) doi: 10.1111/imre.12050. 10.1111/imre.12050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Misra S., Kwon S.C., Abraído-Lanza A.F., Chebli P., Trinh-Shevrin C., Yi S.S. Structural racism and immigrant health in the United States. Health Educ Behav. 2021;48(3):332–341. doi: 10.1177/10901981211010676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grossman S., Cooper Z., Buxton H., et al. Trauma-informed care: recognizing and resisting re-traumatization in health care. Trauma Surg Acute Care Open. 2021;6(1) doi: 10.1136/tsaco-2021-000815. Published 2021 Dec 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilson C., Pence D., Conradi L. National Association of Social Workers and Oxford University Press; 2013. Trauma-informed care. Encyclopedia of social work. Published November 4. [DOI] [Google Scholar]
- 32.Garner A., Yogman M. Committee on psychosocial aspects of child and family health, section on developmental and behavioral pediatrics, council on early childhood. Preventing childhood toxic stress: partnering with families and communities to promote relational health. Pediatrics. 2021;148(2) doi: 10.1542/peds.2021-052582. [DOI] [PubMed] [Google Scholar]
- 33.Oh D.L., Jerman P., Silvério Marques S., et al. Systematic review of pediatric health outcomes associated with childhood adversity. BMC Pediatr. 2018;18(1):83. doi: 10.1186/s12887-018-1037-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goddard A. Adverse childhood experiences and trauma-informed care. J Pediatr Health Care. 2021;35(2):145–155. doi: 10.1016/j.pedhc.2020.09.001. [DOI] [PubMed] [Google Scholar]
- 35.National Association of Pediatric Nurse Practitioners. Spratling R., Cavanaugh Derouin A., Dirks M., Searcy L. Building resilience in childhood and adolescence. J Pediatr Health Care. 2019;33(5):A11–A13. [Google Scholar]
- 36.Ortega-Williams A., Beltrán R., Schultz K., Ru-Glo Henderson Z., Colón L., Teyra C. An integrated historical trauma and posttraumatic growth framework: a cross-cultural exploration. J Trauma & Dissociation. 2021;22(2):220–240. doi: 10.1080/15299732.2020.1869106. [DOI] [PubMed] [Google Scholar]
- 37.Tips for Disaster Responders . SAMHSA, HHS Publication No. SMA-14-4866 (2014); 2014. Understanding historical trauma when responding to an event in Indian Country.ov/sites/default/files/d7/priv/sma14-4866 Available at. Published. [Google Scholar]
- 38.Avalos N. What does it mean to heal from historical trauma? AMA J Ethics. 2021;23(6):E494–E498. doi: 10.1001/amajethics.2021.494. [DOI] [PubMed] [Google Scholar]
- 39.Byrd A.S., Toth A.T., Stanford F.C. Racial disparities in obesity treatment. Curr Obes Rep. 2018;7(2):130–138. doi: 10.1007/s13679-018-0301-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Priest N., Paradies Y., Trenerry B., Truong M., Karlsen S., Kelly Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Soc Sci Med. 2013;95:115–127. doi: 10.1016/j.socscimed.2012.11.031. [DOI] [PubMed] [Google Scholar]
- 41.Agency for Healthcare Research and Quality; Rockville, MD: 2021. National healthcare quality and disparities report.https://www.ahrq.gov/sites/default/files/wysiwyg/research/findings/nhqrdr/2021qdr.pdf Published December 2021. AHRQ Pub. No. 21(22)-0054-EF. [PubMed] [Google Scholar]
- 42.Bailey Z.D., Krieger N., Agénor M., Graves J., Linos N., Bassett M.T. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389:1453–1463. doi: 10.1016/S0140-6736(17)30569-X. 10077. [DOI] [PubMed] [Google Scholar]
- 43.Jelley M., Wen F., Miller-Cribbs J., Coon K., Rodriguez K. Adverse childhood experiences, other psychosocial sources of adversity, and quality of life in vulnerable primary care patients. Perm J. 2020;24:18–277. doi: 10.7812/TPP/18.277cscimed.2012.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cabral J., Cuevas A.G. Health inequities among Latinos/Hispanics: documentation status as a determinant of health. J Racial Ethn Health Disparities. 2020;7(5):874–879. doi: 10.1007/s40615-020-00710-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fleming P.J., Novak N.L., Lopez W.D.U.S. immigration law enforcement practices and health inequities. Am J Prev Med. 2019;57(6):858–861. doi: 10.1016/j.amepre.2019.07.019. [DOI] [PubMed] [Google Scholar]
- 46.Lee H.Y., Rhee T.G., Kim N.K., Ahluwalia J.S. Health literacy as a social determinant of health in Asian American immigrants: findings from a population-based survey in California. J Gen Intern Med. 2015;30(8):1118–1124. doi: 10.1007/s11606-015-3217-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Philbin M.M., Flake M., Hatzenbuehler M.L., Hirsch J.S. State-level immigration and immigrant-focused policies as drivers of Latino health disparities in the United States. Soc Sci Med. 2018;199:29–38. doi: 10.1016/j.socscimed.2017.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Saadi A., Ponce N.A. Worse mental health among more-acculturated and younger immigrants experiencing discrimination: California Health Interview Survey, 2015-2016. J Gen Intern Med. 2020;35(5):1419–1426. doi: 10.1007/s11606-019-05412-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Healthy People 2030; social determinants of health (n. d.). US Department of Health and Human Services. https://health.gov/healthypeople/objectives-and-data/social-determinants-health Available at.
- 50.Schmeer K.K., Tarrence J. Racial-ethnic disparities in inflammation: evidence of weathering in childhood? J Health Soc Behav. 2018;59(3):411–428. doi: 10.1177/0022146518784592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Social determinants of health www.who.int/social_determinants/thecommission/finalreport/key_concepts/en/ World Health Organization.
- 52.Trent M., Dooley D.G., Dougé J. Section on adolescent health, council on community pediatrics, & committee on adolescence. The impact of racism on child and adolescent health. Pediatrics. 2019;144(2) doi: 10.1542/peds.2019-1765. [DOI] [PubMed] [Google Scholar]
- 53.Cox J.L., Holden J.M., Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal depression scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 54.Dubowitz H., Lane W.G., Semiatin J.N., Magder L.S., Venepally M., Jans M. The safe environment for every kid model: impact on pediatric primary care professionals. Pediatrics. 2011;127(4):e962–e970. doi: 10.1542/peds.2010-1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.IOM (Institute of Medicine) and NRC (National Research Council) The National Academies Press; Washington, DC: 2014. New directions in child abuse and neglect research. [PubMed] [Google Scholar]
- 56.Resources for child trauma informed care. SAMHSA. https://www.samhsa.gov/childrens-awareness-day/past-events/2018/child-traumatic- stress-resources Available at: Updated March 9, 2022.
- 57.Maina I.W., Belton T.D., Ginzberg S., Singh A., Johnson T.J. A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Soc Sci Med. 2018;199:219–229. doi: 10.1016/j.socscimed.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 58.Schnierle J., Christian-Brathwaite N., Louisias M. Implicit bias: what every pediatrician should know about the effect of bias on health and future directions. Curr Probl Pediatr Adolesc Health Care. 2019;49(2):34–44. doi: 10.1016/j.cppeds.2019.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Srivastava G., Browne N., Kyle T.K., O'Hara V., Browne A., Nelson T., Puhl R. Caring for us children: barriers to effective treatment in children with the disease of obesity. Obesity. 2021;29(1):46–55. doi: 10.1002/oby.22987. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.