Abstract
We have highlighted the issue of overuse of tourniquets and described why tourniquet conversion and replacement should be taught and done in the prehospital setting.
“I strongly believe—education is our silver bullet. Train soldiers, teach the army, enlighten the society.”-Oleksandr Linchevskyy, MD, PhD
After WWII tourniquet (TQ) use fell out of favor secondary to excessive use for minor injuries and prolonged application without conversion, resulting in excessive harm.1–3 Tourniquets were largely not used in the Korean and Vietnam Wars. They were used in Somalia in 1993, but their resurgence began after Butler's seminal paper in 1996.4,5 When the US entered into the conflicts in Iraq in Afghanistan, most service members were not trained on TQs. By 2006 the prior controversy had disappeared; TQs are now recognized as life-saving standard of care, especially when used as soon as possible after injury.6–15 However, it is also clear that they are applied to wounds that are relatively minor: up to 49% of military and 53% of civilian extremity tourniquets may (in hindsight) not have been necessary.8,16 Increased education on: 1) indications for TQ use, 2) appropriate placement, 3) assessment for tourniquet conversion or tourniquet replacement (TC/TR), and 4) standard TC/TR techniques are essential to save lives while minimizing complications.17–19
TC is attempting to convert a TQ to a hemostatic pressure bandage as soon as safely possible. TR is attempting to exchange a TQ placed “high and tight” during emergent care with a new TQ placed 2–3 inches above the life-threatening bleeding site. TR is done when conversion to wound packing and hemostatic pressure dressing is unsuccessful for hemorrhage control, or when the injury caused a total or near-total amputation and conversion is not indicated. Both maneuvers are focused on minimizing ischemia to healthy tissue.17–19
Tourniquet use for < 2 hours has proven safe, even in those determined not to have been indicated. Tourniquets left in place for longer than 2 hours risk significant ischemic injury. Tourniquets used for less than 6 hours should have TC or TR attempted, while those in place longer than 6 hours should be left in place with an increased need for limb amputation. It is important to note that patients who remain in shock should not have TC attempted.17–19
The near ubiquitous application of tourniquets for even minor extremity bleeding has resulted in a need to further emphasize appropriate indications for tourniquet use (Fig. 1). Casualties from the ongoing war in Ukraine have endured prolonged evacuation times and combined with attrition of battlefield medics, focuses attention on the issue of who can and should be trained in TC/TR when prehospital times are prolonged.20,21
Figure 1.
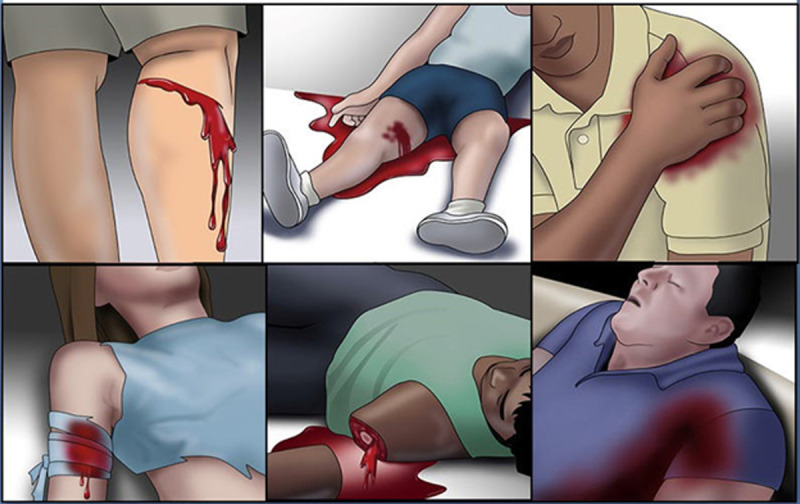
Illustrations of life threatening bleeding, clockwise from top left. (1) Pulsatile or steady bleeding from the limb wound. (2) Blood is pooling on the ground. (3) The overlying clothes are soaked in blood. (4) Bandages or makeshift bandages used to cover the wound are ineffective and steadily becoming soaked with blood. (5) Traumatic extremity amputation. (6) There was prior extremity bleeding and the patient is now in shock (unconscious, confused, pale). Reproduced with permission from the from the American College of Surgeons STOP THE BLEED® program.
RECENT HISTORY
Over the last 20 years, mortality in both the military and civilian settings has improved when casualties with life-threatening extremity bleeding are treated with TQs. In Iraq and Afghanistan prehospital “high and tight” TQ placement followed by rapid transport to a surgical team in under 2 hours mitigated the need to focus on TR or TC. Thus, the guidance for TC/TR was limited to trained medical personnel, which was appropriate given the robust, rapid and safe military evacuation system.
The civilian community lagged behind the military in TQ use. Limited adoption by hospitals and emergency medical services (EMS) began in 2008 and this subsequently increased to wider use.22–25 With the endorsement of multiple civilian professional organizations, TQ use spread into the nonmedical, law enforcement community and then lay responder and now includes placement next to automatic external defibrillators in public gathering places.26–32 However, much like in the US military, most of the reported civilian use of TQs has been in areas with rapid urban transport, mitigating the risk of prolonged TQ times. In more austere rural and wilderness settings, the issue of prolonged TQ time remains as transportation to definitive care frequently exceeds 2 hours.31–33 Furthermore, most rural, frontier, and nontrauma-designated facilities lack experience with the concept of TC/TR, prolonging potentially avoidable limb ischemia time.
Hospital-based experience in patients arriving with TQs in place has shown four categories of patients:
Limbs with minor injuries without major vascular (vein or artery) injury. These historically account for >49% of cases. TC is easily accomplished in this setting (Figs. 2 and 3)
Limbs with major vascular injury but bleeding is controlled with rapid tourniquet application. TC allows bleeding control by hemostatic/pressure dressing.
Limbs with major vascular injury but bleeding are controlled with rapid tourniquet application. When TC is attempted, bleeding resumes, thus, TC is contraindicated and the TQ is retightened. TR to just above the injury site is recommended (Figs. 4 and 5)
Limbs with an injury that is a total or near total amputation. TC is contraindicated in this situation; however, moving the TQ to just above the amputation site (TR) is recommended (Fig. 6).
Figure 2.

Limb with minimal injury but a 5-hour tourniquet use, requiring fasciotomy. Tourniquet conversion was indicated.
Figure 3.

Limb with minor injury. The only wound was minor shrapnel injury of the soft tissues of the back surface of the right forearm (under the gauze dressing). The tourniquets were applied around 11:00 am. There was no qualified medic nearby who knew what to do with the tourniquets. Evacuation during the day was impossible due to heavy artillery shelling, and the casualty arrived to the stabilization point at 10:30 pm (11.5 hours tourniquet time). There were no signs of massive bleeding, the patient was stable and awake and alert. A detailed examination revealed no other injuries. The right upper limb was cold, there was no distal pulse, there was no sensitivity, there were no active movements, and passive movements were significantly limited. The casualty underwent an amputation. Tourniquet conversion was indicated.
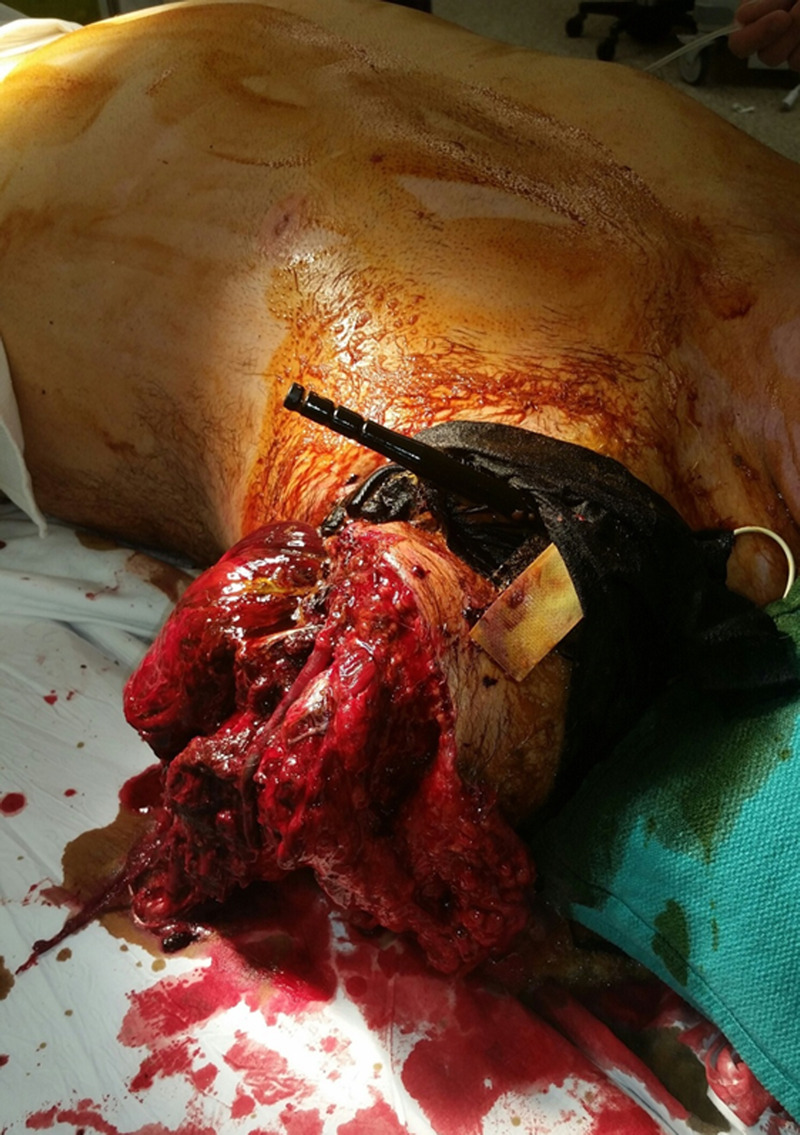
Figure 4.

Limb injury with major vascular injury and 5-hour tourniquet use, with brachial artery injury and shunt in place. The tourniquet was just above the wound and likely not amendable to tourniquet conversion or tourniquet replacement.
Figure 5.

Limb injury with major vascular injury, tourniquet conversion or tourniquet replacement not attempted as rapid transport to hospital was possible.
Figure 6.
Limb amputation injury with tourniquet in appropriate location. Tourniquet conversion or tourniquet replacement not possible.
In summary, most tourniquet applications in the prehospital setting can have safe conversion, and almost all can safely have replacement at a lower level on the limb (Table 1).
TABLE 1.
Reasons to Convert or Replace Tourniquets
| Limb preservation | Prolonged tourniquet use can lead to ischemia and tissue damage, increasing the risk of limb loss. |
| Prevention of compartment syndrome | Prolonged tourniquet application can lead to the development of compartment syndrome, a condition characterized by increased pressure within a muscle compartment, resulting in tissue damage and potential loss of limb function. |
| Prevention of reperfusion injury | When a tourniquet is released after prolonged use, reperfusion of the limb can lead to systemic complications such as acidosis, coagulopathy, hypotension, renal failure, and death. |
| Avoidance of prolonged pain and discomfort | Prolonged tourniquet application can cause significant pain and discomfort to the casualty and can increase the need for analgesia medications in a limited resource environment. |
Brief Review of Current Recommendations
When considering who should perform TC or TR, it is instructive first to briefly review the current recommendations.
-
-
Both Drew et al. and Shackelford et al. separately published excellent reviews on how to do TC in 2015. Drew et al. limited the TC procedure to medical personnel only while Shackelford et al. were silent on what level of medical experience is required.17,18
-
-
Current recommendations from the Joint Trauma System and Tactical Combat Casualty Care, National Association of Emergency Medical Technicians (NAEMT), guidelines and the civilian STOP THE BLEED® state that only a medical professional should perform TC/TR.34–36
-
-
Tactical Emergency Casualty Care (TECC) recommends that medics and law enforcement officers can perform TC.37
In summary the majority of published recommendations from military and civilian sources are either silent or state that TC/TR should only be done by medical professionals.
The Problem
Casualties in the ongoing war in Ukraine have frequently endured prolonged evacuation times and thus numerous anecdotal examples exist of extended tourniquet times (>6 hours) resulting in significant morbidity (Figs. 2-4). Because of operational security issues surrounding casualty numbers and outcomes, summary data are not available describing numbers of patients, extremity injuries, tourniquet application, and outcomes across the Ukrainian theater. However, multiple front-line medical personnel have relayed these observations (authors O.Le., A.M., G.B., O.D., and O.Li.).
Prolonged transport times after TQ use serve as a reminder of how history repeats itself and focuses the need to improve attention on training for TQ indications and TC/TR.1–3 This quote from WWII is telling.2
“Soldiers—whether medical or nonmedical—regularly misused tourniquets. They applied them unnecessarily; left them unloosened for too long; and occasionally evacuated patients with tourniquets concealed by blankets or clothing, and hence not discovered until the limb was doomed. Trying to prevent such abuses, the Seventh Army surgeon directed that the "sole indication" for applying a tourniquet should be "active spurting hemorrhage from a major artery" and that medics in the field or at battalion aid stations should note the presence of a tourniquet on a patient in capital letters.”
Scenarios that delay a casualty from reaching trained medical personnel may include: wilderness/remote location, mass casualty incidents, lack of combat medic or corpsman support, lack of transport assets, lack of air superiority, and prolonged time in a tactical situation where a casualty is unable to be moved for many hours. In the setting (military or civilian) where a tourniquet has been effectively applied (especially “high and tight”) and the first medical personnel or facility is longer than 2 hours away, leaving the TQ until arrival risks: limb ischemia, muscle necrosis, need for fasciotomy, renal failure, amputation and death, (Fig. 7). Furthermore, if a casualty was in shock before the TQ was placed, then the “allowable” ischemic time is likely less than 2 hours.38 Both civilian and military data have identified that TQs are often placed when there is no life-threatening hemorrhage.8,16,24 Leaving such a TQ in place for an extended time causes unnecessary morbidity without any benefit, however as stated above, most recommendations state that TC/TR can only be done by medical personnel. This scenario is actively occurring in Ukraine and resulting in potentially preventable complications.20,21 What is being witnessed is a repetition of a lesson not learned from WWII, which resulted in tourniquets not being used appropriately for 60 years.
Figure 7.
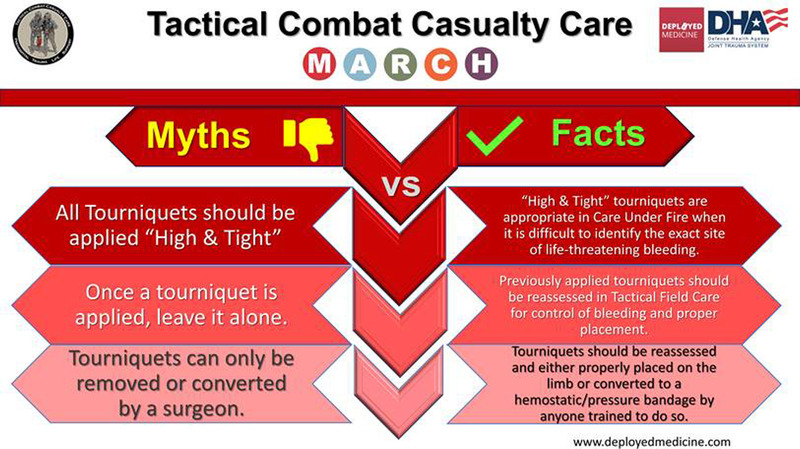
With approval from the Joint Trauma System, Tourniquet Myths and Facts.
Given that the published literature is largely based on the 20-year experience in Iraq and Afghanistan or in urban civilian trauma systems, there is little guidance for TC other than to suggest it should be done within 2 hours and by a medical professional. While recent military and civilian experience has demonstrated thousands of incidents of safe TQ use, the vast majority of patients arrived at a medical facility within 2 hours of injury and often much sooner. Rapid transport mitigates the risk of TQ application, even for minor injuries. However if transport is delayed and the TQ was not indicated, the patient assumes substantial risk with little benefit. This underscores the importance of emphasizing TQ indications as well as TC/TR as early as possible after injury.
The Solution
Care under fire demands rapid management of life-threatening limb bleeding with appropriate placement of TQs.34 This should include placement of a TQ more distally on the limb if clearly proximal to the bleeding site, or placement “high and tight” if the site of life-threatening bleeding is not readily apparent or the tactical situation prevents close examination of the limb. Tourniquets used should be those that are recommended by the Committee on Tactical Combat Casualty Care and should not be substituted by cheap or counterfeit TQs which have been shown to fail. Education on appropriate placement guidelines are essential to minimize unnecessary TQ placement.
In two of the four scenarios (1 and 2) described above, TC can be accomplished as eloquently described by Drew or Shackelford.18,19 In summary, when in a secure location pack the wound tightly and hold pressure, then loosen the original tourniquet while ensuring that a new tourniquet can be tightened if bleeding resumes. In scenario 3 and 4, TC is contraindicated, but a new tourniquet(s) should be placed 2 inches to 3 inches above the wound (TR), thus preserving as much limb length as possible if amputation is required. In all situations, close observation and reassessment of the casualty's wound is important to monitor for possible rebleeding during transport (Table 2).
TABLE 2.
Tourniquet Conversion or Replacement Recommendations
| Indications for TQ Replacement | Indications for TQ Conversion | Indication to Leave a TQ in Place |
|---|---|---|
| Tourniquet adjustment from “high & tight”: when a “high & tight” tourniquet previously applied in a high threat situation can be better assessed for proximity to bleeding site. | Availability of alternative methods: when other methods of bleeding control, such as direct pressure, hemostatic agents, or wound closure become feasible and are readily available. | A tourniquet is controlling bleeding for an obvious amputation or a failed conversion attempt |
| Tourniquet adjustment required: if the initial application of the tourniquet was not effective in controlling bleeding, adjusting the placement or tension of the tourniquet may be necessary. In such cases, replacing the tourniquet allows for a more secure and appropriate application. | Wound is amenable to a hemostatic or pressure dressing and three criteria for conversion are met: 1. Casualty is not in shock. 2. Possible to monitor wound for rebleeding. 3. TQ is not being used to control bleeding from amputation. |
Tourniquet has been in place for more than 6 h. |
| Every effort should be made to replace TQs more distally in less than 2 h | Every effort should be made to convert TQs in less than 2 h if bleeding can be controlled by other means. |
In addition to better emphasizing which casualties actually need a tourniquet, military and civilian training courses must emphasize, train, and drill the indications for TC/TR. For both medical and non-medical personnel, training and retraining are essential to safe and effective performance of these tasks. A critical component of TQ use is frequent reassessment of its necessity and efficacy. Should a medic NOT be immediately available OR if the TQ has been in place for 2 hours, then TC/TR should be attempted by anyone who has been trained to perform those tasks. The Armed Forces of Ukraine adopted this approach July 18, 2023, with the additional provision that telemedicine communication (if available) to untrained personnel may facilitate TC/TR.39
CONCLUSION
Hemorrhage is the number one preventable cause of death on the battlefield and the emphasis should remain on preventing a casualty from bleeding to death. Tourniquet use has saved thousands of lives; however, overuse has consequences that increase when evacuation is prolonged. All three components of appropriate tourniquet use described in this article are critical. Training on who needs a tourniquet, where to replace a tourniquet and how to convert a tourniquet are all equally important, and if not implemented with appropriate training, could result in casualties bleeding to death rather than suffering the morbidity of limb ischemia/amputation. Our goal is to limit ischemia but not at the expense of losing a life. The current experience in Ukraine causes us to reexamine TQ guidance for patients with prolonged transport times and must inform civilian and military prehospital medical concepts.
We strongly believe that education and training is our “silver bullet.” We must train soldiers and civilians, teach the military and enlighten society. Every person that is trained to place a tourniquet should be trained to safely convert or replace a TQ. Appropriate tourniquet indications, application, conversion and replacement should be taught to ALL service members and civilians who carry a tourniquet.
Quote and Dedication
Quote: Don’t repeat our mistakes. Train your soldiers well now, when you have enough time for it. Because the quality training process is practically impossible during an active war.
Major Olha Levchuk,
Chief of the Medical Training Team
Armed Force of Ukraine
Dedication
To all the patients and authors that came before us, may we minimize the lessons that have to be relearned; so that lessons learned are not forgotten. To all our casualties whom we have cared for during the most recent wars, thank you for teaching us. And especially for our future patients, that they might benefit from these hard won lessons.
Supplementary Material
Footnotes
Published online: September 19, 2023.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jtrauma.com).
Contributor Information
Warren C. Dorlac, Email: Warren.Dorlac@uchealth.org.
Brendon G. Drew, Email: prehospital1996@outlook.com.
Frank K. Butler, Email: fkb064@yahoo.com.
Jennifer M. Gurney, Email: jennifer.m.gurney.mil@health.mil.
Harold R. Montgomery, Email: HRMontgomery75@gmail.com.
Stacy A. Shackelford, Email: stacy.a.shackelford.mil@health.mil.
Eric A. Bank, Email: Eric.Bank@hcesd48.org.
Jeff D. Kerby, Email: jkerby@uabmc.edu.
John F. Kragh, Email: john.f.kragh.civ@health.mil.
Michael A. Person, Email: mperson97@msn.com.
Jessica L. Patterson, Email: jessica.patterson@global-response.org.
Olha Levchuk, Email: doctorstarosta15@gmail.com.
Mykola Andriievskyi, Email: Gensurvival@gmail.com.
Glib Bitiukov, Email: belgovs@gmail.com.
Oleksandr Danyljuk, Email: dr.danyljuk@gmail.com.
Oleksandr Linchevskyy, Email: linchevskyy@ukr.net.
AUTHORSHIP
J.B.H. and W.C.D. drafted the article. B.G.D., F.K.B., J.M.G., H.R.M., S.A.S., E.B., J.D.K., J.F.K., M.A.P., J.L.P., O.Le., M.A., G.B., O.D., and O.Li. edited and provided critical revision and insights. All authors reviewed and approved the article prior to final submission.
DISCLOSURE
The authors declare no funding or conflicts of interest.
Author Disclosure forms have been supplied and are provided as Supplemental Digital Content (http://links.lww.com/TA/D244).
REFERENCES
- 1.Wolff LH, Adkins TF. Tourniquet problems in war injuries. Bulletin of the US Army Medical Department. 1945;77–85. [Google Scholar]
- 2.Cosmas Graham A. and Albert E Cowdrey (Eds). (1992). Page 363. The Medical Department - Medical Service in the European Theater of Operations—U.S. Army Center of Military History. Accessed 8 Aug 2023
- 3.Mabry RL. Tourniquet use on the battlefield. Mil Med. 2006;171(5):352–356. [DOI] [PubMed] [Google Scholar]
- 4.Mabry RL, Holcomb JB, Baker AM, Cloonan CC, Uhorchak JM, Perkins DE, Canfield AJ, Hagmann JH. United States Army Rangers in Somalia: an analysis of combat casualties on an urban battlefield. J Trauma. 2000;49(3):515–528; discussion 528–529. [DOI] [PubMed] [Google Scholar]
- 5.Butler FK, Jr., Hagmann J, Butler EG. Tactical combat casualty care in special operations. Mil Med. 1996;161(Suppl):3–16. [DOI] [PubMed] [Google Scholar]
- 6.Holcomb JB, McMullin NR, Pearse L, Caruso J, Wade CE, Oetjen-Gerdes L, Champion HR, Lawnick M, Farr W, Rodriguez S, Butler FK. Causes of death in U.S. Special Operations Forces in the global war on terrorism: 2001–2004. Ann Surg. 2007;245(6):986–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beekley AC Sebesta JA Blackbourne LH Herbert GS Kauvar DS Baer DG Walters TJ Mullenix PS Holcomb JB, 31st Combat Support Hospital Research Group . Prehospital tourniquet use in Operation Iraqi Freedom: effect on hemorrhage control and outcomes. J Trauma. 2008;64(2 Suppl):S28–S37; discussion S37. [DOI] [PubMed] [Google Scholar]
- 8.Kragh JF, Jr., Walters TJ, Baer DG, Fox CJ, Wade CE, Salinas J, Holcomb JB. Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann Surg. 2009;249(1):1–7. [DOI] [PubMed] [Google Scholar]
- 9.Kelly JF, Ritenour AE, McLaughlin DF, Bagg KA, Apodaca AN, Mallak CT, Pearse L, Lawnick MM, Champion HR, Wade CE, Holcomb JB. Injury severity and causes of death from Operation Iraqi Freedom and Operation Enduring Freedom: 2003–2004 versus 2006. J Trauma. 2008;64(2 Suppl):S21–S26; discussion S26–S27. [DOI] [PubMed] [Google Scholar]
- 10.Eastridge BJ, Mabry RL, Seguin P, Cantrell J, Tops T, Uribe P, Mallett O, Zubko T, Oetjen-Gerdes L, Rasmussen TE, Butler FK, Kotwal RS, Holcomb JB, Wade C, Champion H, Lawnick M, Moores L, Blackbourne LH. Death on the battlefield (2001–2011): implications for the future of combat casualty care. J Trauma Acute Care Surg. 2012;73(6 Suppl 5):S431–S437. [DOI] [PubMed] [Google Scholar]
- 11.Butler FK, Jr. TCCC updates: two decades of saving lives on the battlefield: tactical combat casualty care turns 20. J Spec Oper Med. 2017;17(2):166–172. [DOI] [PubMed] [Google Scholar]
- 12.Howard JT, Kotwal RS, Stern CA, Janak JC, Mazuchowski EL, Butler FK, Stockinger ZT, Holcomb BR, Bono RC, Smith DJ. Use of combat casualty care data to assess the US Military Trauma System during the Afghanistan and Iraq conflicts, 2001–2017. JAMA Surg. 2019;154(7):600–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kragh JF, Jr., O’Neill ML, Beebe DF, Fox CJ, Beekley AC, Cain JS, Parsons DL, Mabry RL, Blackbourne L. Survey of the indications for use of emergency tourniquets. J Spec Oper Med. 2011;11:30–34. [DOI] [PubMed] [Google Scholar]
- 14.Kragh JF, Jr., Swan KG, Smith DC, Mabry RL, Blackbourne LH. Historical review of emergency tourniquet use to stop bleeding. Am J Surg. 2012;203(2):242–252. [DOI] [PubMed] [Google Scholar]
- 15.Shackelford SA, Del Junco DJ, Riesberg JC, Powell D, Mazuchowski EL, Kotwal RS, Loos PE, Montgomery HR, Remley MA, Gurney JM, Keenan S. Case-control analysis of prehospital death and prolonged field care survival during recent US military combat operations. J Trauma Acute Care Surg. 2021;91(2S Suppl 2):S186–S193. [DOI] [PubMed] [Google Scholar]
- 16.Scerbo MH, Mumm JP, Gates K, Love JD, Wade CE, Holcomb JB, Cotton BA. Safety and appropriateness of tourniquets in 105 civilians. Prehosp Emerg Care. 2016;20(6):712–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Drew B, Bird D, Matteucci M, Keenan S. Tourniquet conversion: a recommended approach in the prolonged field care setting. J Spec Oper Med. 2015;15(3):81–85. [DOI] [PubMed] [Google Scholar]
- 18.Shackelford SA, Butler FK, Jr., Kragh JF, Jr., Stevens RA, Seery JM, Parsons DL, Montgomery HR, Kotwal RS, Mabry RL, Bailey JA. Optimizing the use of limb tourniquets in tactical combat casualty care: TCCC guidelines change 14-02. J Spec Oper Med. 2015;15(1):17–31. [PubMed] [Google Scholar]
- 19.Drew B, Bennett BL, Littlejohn L. Application of current hemorrhage control techniques for backcountry care: part one, tourniquets and hemorrhage control adjuncts. Wilderness Environ Med. 2015;26(2):236–245. [DOI] [PubMed] [Google Scholar]
- 20.Yatsun V. Application of hemostatic tourniquet on wounded extremities in modern “trench” warfare: the view of a vascular surgeon. Mil Med. 2022;usac208. [DOI] [PubMed] [Google Scholar]
- 21.Quinn J Panasenko SI Leshchenko Y Gumeniuk K, et al. Prehospital lessons from the war in Ukraine: damage control resuscitation and surgery experiences from point of injury to role 2. Mil Med. 2023;usad253. [DOI] [PubMed] [Google Scholar]
- 22.Dorlac WC, DeBakey ME, Holcomb JB, Fagan SP, Kwong KL, Dorlac GR, Schreiber MA, Persse DE, Moore FA, Mattox KL. Mortality from isolated civilian penetrating extremity injury. J Trauma. 2005;59(1):217–222. [DOI] [PubMed] [Google Scholar]
- 23.Scerbo MH, Holcomb JB, Taub E, Gates K, Love JD, Wade CE, Cotton BA. The trauma center is too late: major limb trauma without a pre-hospital tourniquet has increased death from hemorrhagic shock. J Trauma Acute Care Surg. 2017;83(6):1165–1172. [DOI] [PubMed] [Google Scholar]
- 24.Mokhtari AK, Mikdad S, Luckhurst C, Hwabejire J, Fawley J, Parks JJ, Mendoza AE, Kaafarani HMA, Velmahos GC, Bloemers FW, Saillant NN. Prehospital extremity tourniquet placements-performance evaluation of non-EMS placement of a lifesaving device. Eur J Trauma Emerg Surg. 2022;48(5):4255–4265. [DOI] [PubMed] [Google Scholar]
- 25.Hashmi ZG, Hu PJ, Jansen JO, Butler FK, Kerby JD, Holcomb JB. Characteristics and outcomes of prehospital tourniquet use for trauma in the United States. Prehosp Emerg Care. 2023;27(1):31–37. [DOI] [PubMed] [Google Scholar]
- 26.Jacobs LM, Joint Committee to Create a National Policy to Enhance Survivability from Intentional Mass Casualty and Active Shooter Events . The Hartford Consensus IV: a call for increased national resilience. Bull Am Coll Surg. 2016;101(3):17–24. [PubMed] [Google Scholar]
- 27.Teixeira PGR Brown CVR Emigh B Long M Foreman M Eastridge B Gale S Truitt MS Dissanaike S Duane T Holcomb J Eastman A Regner J, Texas Tourniquet Study Group . Civilian prehospital tourniquet use is associated with improved survival in patients with peripheral vascular injury. J Am Coll Surg. 2018;226(5):769–776.e1. [DOI] [PubMed] [Google Scholar]
- 28.Schroll R Smith A Alabaster K, et al. AAST multicenter prospective analysis of prehospital tourniquet use for extremity trauma. J Trauma Acute Care Surg. 2022;92(6):997–1004. [DOI] [PubMed] [Google Scholar]
- 29.Mikdad S, Mokhtari AK, Luckhurst CM, Breen KA, Liu B, Kaafarani HMA, Velmahos G, Mendoza AE, Bloemers FW, Saillant N. Implications of the national stop the bleed campaign: the swinging pendulum of prehospital tourniquet application in civilian limb trauma. J Trauma Acute Care Surg. 2021;91(2):352–360. [DOI] [PubMed] [Google Scholar]
- 30.Berry C, Gallagher JM, Goodloe JM, Dorlac WC, Dodd J, Fischer PE. Prehospital hemorrhage control and treatment by clinicians: a joint position statement. Prehosp Emerg Care. 2023;27(5):544–551. [DOI] [PubMed] [Google Scholar]
- 31.Butler FK, Bennett B, Wedmore CI. Tactical combat casualty care and wilderness medicine: advancing trauma care in austere environments. Emerg Med Clin North Am. 2017;35(2):391–407. [DOI] [PubMed] [Google Scholar]
- 32.Jones MD, Paulus JA, Jacobs JV, Bogert JN, Chapple KM, Soe-Lin H, Weinberg JA. Trauma patient transport times unchanged despite trauma center proliferation: a 10-year review. J Trauma Acute Care Surg. 2021;90(3):421–425. [DOI] [PubMed] [Google Scholar]
- 33.Joarder M, Noureddine El Moussaoui H, Das A, Williamson F, Wullschleger M. Impact of time and distance on outcomes following tourniquet use in civilian and military settings: a scoping review. Injury. 2023;54(5):1236–1245. [DOI] [PubMed] [Google Scholar]
- 34.Deployed Medicine TCCC Guidelines (allogy.com). Accessed 8 Aug 2023.
- 35.https://www.naemt.org/docs/default-source/education-documents/tccc/tccc-skill-sets-by-responder-level-master-190422-approved.pdf?sfvrsn=f8c3e093_2. Accessed 8 Aug 2023.
- 36.Online Course | Stop the Bleed. Accessed 8 Aug 2023.
- 37.TECC_Guidelines_-_JUNE_2015_update.pdf (c-tecc.org). Accessed 8 Aug 2023.
- 38.Hancock HM, Stannard A, Burkhardt GE, Williams K, Dixon P, Cowart J, Spencer J, Rasmussen TE. Hemorrhagic shock worsens neuromuscular recovery in a porcine model of hind limb vascular injury and ischemia-reperfusion. J Vasc Surg. 2011;53(4):1052–1062; discussion 1062. [DOI] [PubMed] [Google Scholar]
- 39.How to carry out tourniquet conversion properly. (Ukrainian) https://armyinform.com.ua/2023/07/20/yak-provesty-konversiyu-turniketa-pravylno/?fbclid=IwAR0WNUW6UEQrCiDrUTza-FrvywMQWr8iA9elVikMXuhdzgiy0WsbBCjXyBM. Accessed 8 Aug 2023.


