Abstract
Insomnia is the most common sleep disorder, with persistent insomnia being associated with greater risk and leading to a range of functional consequences that place a heavy burden on patients and healthcare systems. A weight of evidence has shown that complementary and alternative medicine (CAM) seems to have a positive effect on improving sleep. However, the research trends of CAM intervention for insomnia have not been studied systematically through bibliometrics. We searched the relevant literature over the past decade in the Web of Science Core Collection database on September 20, 2022 and used CiteSpace and gCLUTO to visually analyze and cluster countries, institutions, authors, journals and keywords. Through screening, 1655 papers were included. In the past decade, the number of articles published in this field shown an annual trend of growth, with explosive growth in 2020. The USA has the largest number of publications, the University of Hong Kong is the leading institution in this field, and the most cited journal is Sleep. Mental condition and quality of life in patients with insomnia, insomnia related to cancer, effect of mindfulness meditation, yoga and aromatherapy on insomnia and the psychiatric symptoms resulting from the COVID-19 pandemic are at the forefront of this field. In this study, bibliometrics and visualization analysis were performed on related studies on CAM intervention for insomnia. This will be the focus and development direction of insomnia treatment in the future to formulate structured treatment plans for traditional Chinese medicine-related CAM, validate large-scale clinical trials, solve cancer comorbidity insomnia and related psychiatric symptoms and deal with mental health-related insomnia after public health outbreaks.
Keywords: bibliometric analysis4, biclustering analysis5, complementary and alternative3, Insomnia1, research trends2
1. Introduction
Insomnia is the most common sleep disorder and a common clinical complaint.[1] In addition to the main insomnia symptoms, daytime social functions such as fatigue, decreased cognitive function, mood disorders, distress or personal function are also affected.[2] Epidemiological data show that the prevalence of insomnia in the general population ranges from 12% to 20%. During the extraordinary period of the global COVID-19 pandemic, the incidence of persistent insomnia was 76.5%.[3] Insomnia often takes a chronic course, with symptoms persisting for 1 year after diagnosis in 86% of patients and for more than 5 years in 59% of patients.[4] Persistent insomnia is associated with greater risk, such as increased risk of depression,[5] metabolic syndrome,[6] hypertension,[7] coronary heart disease,[8] deterioration in the quality of life,[9] and increased suicide rates worldwide.[10] In addition, insomnia leads to a number of functional consequences, such as reduced productivity, substantial work costs and increased healthcare costs,[11,12] totaling more than $100 billion[13] annually in the USA alone, thus placing a heavy burden on patients and the healthcare system.
The goals for treating insomnia are to improve the quantity and quality of sleep, reduce distress and anxiety associated with poor sleep and improve daytime functioning.[14] Current treatment mainly includes both non-drug and drug therapy. However, the clinical efficacy of insomnia is affected by many factors. For example, cognitive behavioral therapy (CBT), as a first-line non-drug therapy, is widely used in patients with all types of insomnia[15] and its efficacy has been confirmed in both chronic primary and concomitant insomnia. However, due to the different qualifications of operators, complicated CBT content, high treatment costs and insignificant short-term efficacy, patients’ compliance is poor and their trust is low. Hypnotic drugs are recommended for short-term treatment of acute insomnia,[16,17] mainly including benzodiazepine agonists, antihistamines and other types of drugs. However, drugs have the risk of abuse and can easily become addictive.[18] Long-term use is prone to lethargy, weight gain, daytime fatigue, vertigo, delirium, ataxia, anterograde amnesia, sleepwalking and other adverse reactions[19] and is even significantly associated with traffic accidents, falls in the elderly and other serious adverse events.[17,20]
Complementary and alternative medicine (CAM) has evolved over the past 20 years and is now a common treatment for insomnia. Different countries and regions have different definitions of CAM. CAM commonly used for insomnia include herbal medicine, acupuncture, qigong, massage, meditation, yoga, Tai chi, hypnosis, music therapy and aromatherapy.[21] Evidence from a series of clinical studies has shown the effectiveness of CAM for treating insomnia. For example, meditation may have beneficial effects on sleep quality in different populations, accompanied by improvements in anxiety, depression and chronic pain.[22] Yoga is effective for improving sleep quality and reducing the use of sleep medication in cancer survivors.[23] Irwin et al[24] showed that Tai chi can be considered as a useful non-pharmaceutical method to improve sleep quality in elderly people with moderate insomnia symptoms. Wang et al[25] found that acupuncture can regulate brain neurons, thereby improving sleep quality.
A weight of evidence has shown that CAM seems to have a positive effect on improving sleep. However, the literature reports on CAM in insomnia treatment are scattered and most studies do not agree on a unified answer. Therefore, it is necessary to comprehensively analyze and visualize the research hotspots and development trends of insomnia in the CAM field. Bibliometrics and visual analysis is a scientific method based on the literature system and bibliometric characteristics, using mathematics, statistics and other measurement methods to analyze the distribution structure, quantitative relationship and change rules of documents[26]; it can also describe trends in the literature, the contribution of journals, authors, teams and countries to specific research areas and information on mutual cooperation.[27,28] This study aimed to analyze the trends of CAM treatment for insomnia from 2013 to 2022 through bibliometrics. Based on the Web of Science Core Collection (WoSCC) database, this study used CiteSpace, BICOMB and gCLUTO software to analyze the trend and to systematically and comprehensively describe the hotspots, research status, and development trends in this field in order to find research hotspots and key topics for researchers in the field and provide new clues and research directions for future research.
2. Materials and methods
2.1. Data collection and search strategy
We conducted a literature search on the WoSCC database on September 20, 2022. The search strategy was mainly divided into 2 parts. The first part covered complementary and alternative therapy. According to the European Guidelines for the Diagnosis and Treatment of Insomnia[15] and the Management of Chronic Insomnia Disorder in Adults,[29] we determined the search terms for complementary and alternative therapy, which mainly included aromatherapy, yoga, meditative movement therapies, Tai chi, auricular acupressure, Tuina, moxibustion, acupuncture, hypnotherapy, music therapy, homeopathy, and Chinese herbal medicine. The second part comprised the search terms related to insomnia. After combining the retrieval strategies of the 2 parts, we obtained a total of 2519 records. Finally, we limited the publication year of the article to 2013 to 2022 and the document types to “Article” and limit the language to English, finally obtained 1655 documents, which were then converted into a format that could be recognized by software and exported (see Table S1, Supplemental Digital Content, http://links.lww.com/MD/J270 for detailed retrieval policies). Since the data included in the article does not contain any personal information of patients, ethical approval is not required.
2.2. Data analysis
2.2.1. Data extraction and analysis.
According to the statistical results of the WoSCC database, we collected statistics on relevant data such as publication volume, year and country and made a line chart, bar chart, national cooperation chart and map distribution chart of publication volume based on the results. Then we saved the data in RefWorks format, imported the data into CiteSpace 6.1.R3 software[30] to draw the network hotspot map and set the parameters as follows: the time interval was from January 2013 to September 2022, with year per slice = 1; we selected Pathfinder and Pruning sliced networks, set Top N = 25; and the remaining parameters are default values and are adjusted according to the requirements.
2.2.2. Biclustering analysis of high-frequency keywords.
The qualified records of the WoSCC database were exported and then the Bibliographic Item Co-Occurrence Matrix Builder (BICOMB, version 2.0, designed by Professor Lei Cui from China Medical University)[31] was used to construct a high-frequency keyword co-occurrence matrix.
Next, we unified keywords writing format and the synonyms were merged to import the high-frequency keyword co-occurrence matrix to the gCLUTO software (version 1.0, Graphical CLUstering Toolkit: a graphical front-end for the CLUTO data clustering library developed by Rasmussen, Newman and Karypis from the University of Minnesota).[32] Double clustering analysis was carried out on the high-frequency keywords and the clustering methods used repeated dichotomy, optimization function I2, a similarity coefficient as the cosine function and the rest of the settings for the default values. Finally, both matrix and mountain visualization were generated to show the correlation between the source article and high-frequency keywords, as a way to identify research hotspots related to CAM for insomnia.
3. Results
3.1. Trends in research publications
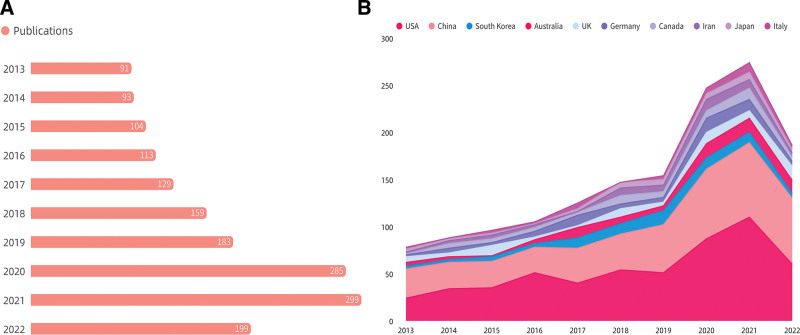
According to the search results, a total of 1655 literature records were obtained. At the same time, we produced a graph of the research trends related to the intervention of CAM for insomnia in the past 10 years and a graph of the published trends of the top 10 published countries, as shown in Figure 1. As our retrieval date is September 20, 2022, the number of articles published in 2022 does not include the complete number of articles published in the whole year. Figure 1A shows that the number of articles published in this field has been increasing year by year in the past 10 years, with explosive growth in 2020; Figure 1B shows a similar trend for the dominance of the top 10 countries in the field.
Figure 1.
(A) Graph of the number of publications per year over the past decade. (B) Chart of the number of publications issued by the top 10 countries from 2013 to 2022.
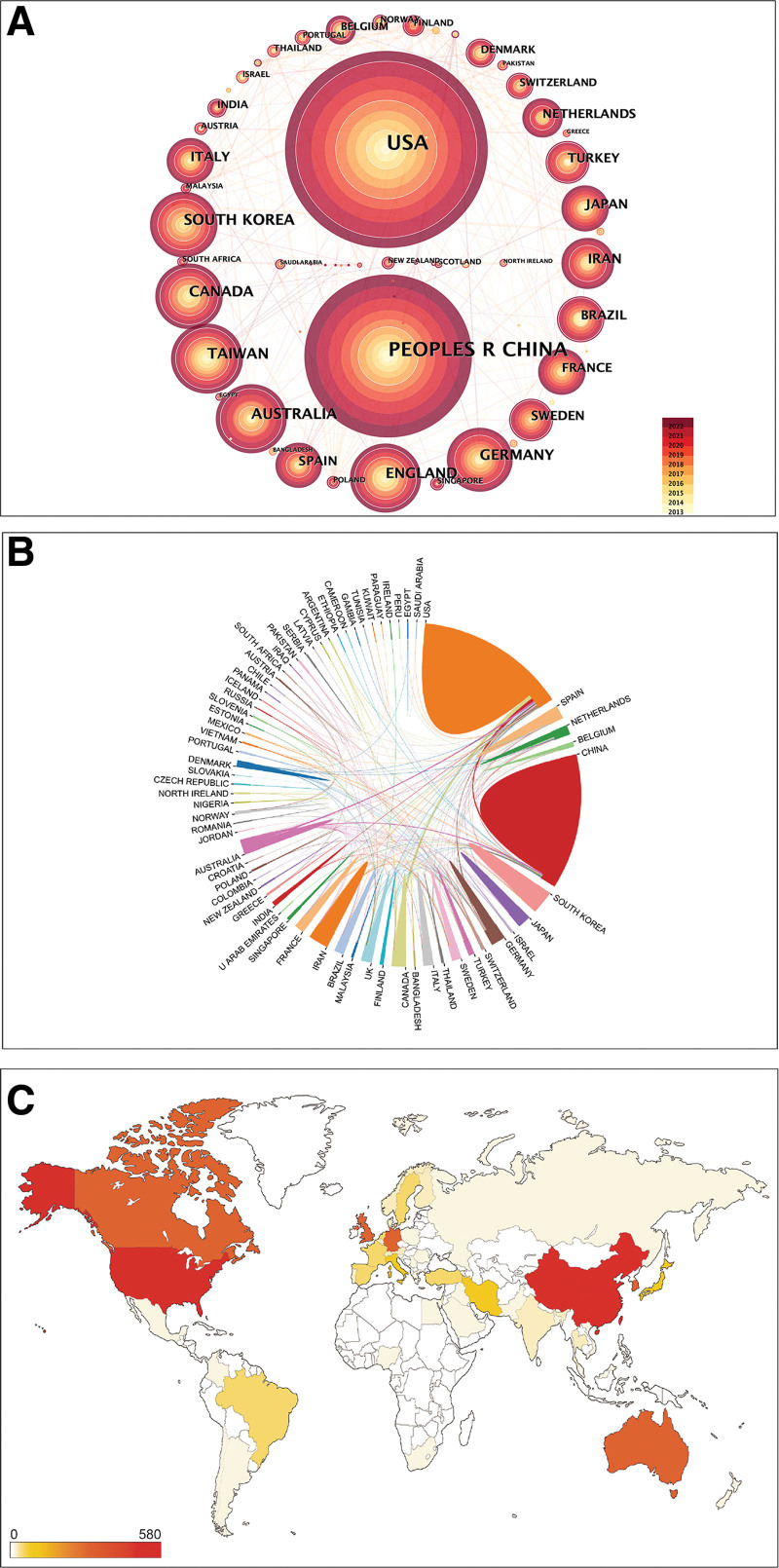
3.2. Analysis of countries’ cooperation and distribution
In the past decade, a total of 67 countries and regions have made contributions to the CAM intervention for insomnia. Figure 2A shows the network hotspot map of all countries and regions. The analysis results of published articles and the centrality of the top 10 countries and regions are listed in Table 1. With regard to the number of articles published in the USA, 573 articles were ahead of the other countries and regions, accounting for 34.62% of the total number of articles published in this field and indicating that CAM intervention for insomnia has attracted much attention in the USA. In terms of centrality, although England and Australia ranked sixth and fourth in the number of publications, their centrality was 0.25 and 0.21, respectively, leading the other countries and regions; a total of 8 countries and regions had centrality > 0.10, showing that these countries and regions have a good mediating effect and close research cooperation with other countries and regions. Finally, we made visual images of the cooperation network between countries (Fig. 2B) and a distribution map of national publication volume (Fig. 2C) so that the analysis results could be displayed better visually.
Figure 2.
(A) Countries and regions co-occurrence diagram. (B) The cooperation of countries in the field of CAM for insomnia from 2013 to 2022. (C) National and regional geographic distribution of CAM for insomnia. CAM = complementary and alternative medicine.
Table 1.
Published articles and the centrality of the top 10 countries and regions between 2013 and 2022.
| Count | Centrality | ||||
|---|---|---|---|---|---|
| Rank | Country/region | Number | Rank | Country/region | Value |
| 1 | USA | 573 | 1 | England | 0.25 |
| 2 | Peoples R China | 387 | 2 | Australia | 0.21 |
| 3 | Taiwan | 84 | 3 | USA | 0.18 |
| 4 | Australia | 83 | 4 | Peoples R China | 0.17 |
| 5 | South Korea | 82 | 5 | Taiwan | 0.14 |
| 6 | England | 77 | 6 | Spain | 0.14 |
| 7 | Canada | 73 | 7 | Canada | 0.12 |
| 8 | Germany | 70 | 8 | France | 0.10 |
| 9 | Iran | 55 | 9 | Japan | 0.07 |
| 10 | Japan | 49 | 10 | Denmark | 0.07 |
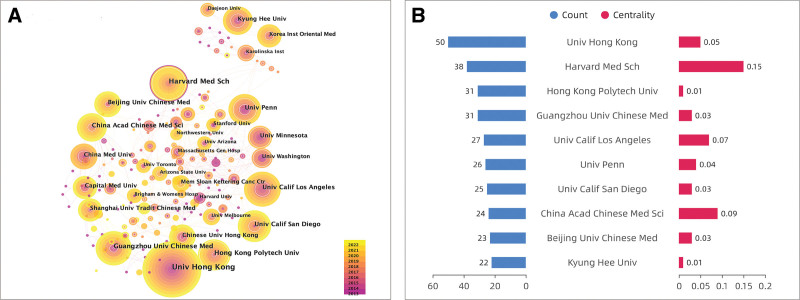
3.3. Distribution of institutions
Analysis of the network hotspots of the research institutions (Fig. 3A) shows that 321 institutions are involved in the research in this field, with 538 links indicating that a certain scale of cooperation network has been formed between the institutions. In terms of centrality (Fig. 3B), only Harvard Medical School has centrality > 0.10, indicating that it has a close cooperation network with other institutions. The rest of the top 10 institutions are mostly from the USA and China; they have different degrees of cooperation within the country as a unit and also cooperate with institutions in other countries and regions. It is worth noting that the cooperation between Korean research institutions (mainly Kyung Hee University) and other countries and regions is less, with the cooperation mainly between institutions within countries. In conclusion, the University of Hong Kong and Harvard Medical School have made significant contributions to the intervention of CAM in the field of insomnia. The main research areas of the University of Hong Kong are the effects of acupuncture, Tai chi and massage on insomnia, whereas Harvard University pays more attention to the effects of mindfulness meditation-related therapies on insomnia.
Figure 3.
(A) Co-operation between different institutions in the field of CAM for insomnia. (B) The centrality of institutions. CAM = complementary and alternative medicine.
3.4. Analysis of authors
We listed the information of the top 5 authors with regard to published quantity and centrality in Table 2. In terms of the number of articles published in the field of CAM intervention for insomnia, Ka-Fai Chung[33] ranked first with 23 articles, which mainly involved studies on traditional Chinese medicine (TCM)-related CAM intervention for insomnia, such as acupuncture, electroacupuncture, Taijiquan and massage. Irwin,[34] ranked second in the number of articles published, mainly focused on Taijiquan, meditation and other CAM to alleviate insomnia and related mental conditions. It is worth noting that Ka-Fai Chung and Branda Y M Yu, the first and fourth authors, have worked closely together on acupuncture, massage and hypnotherapy for insomnia.[35]
Table 2.
The top 5 authors in terms of publication volume and centrality from 2013 to 2022.
| Rank | Author | Count | Rank | Cited author | Centrality |
|---|---|---|---|---|---|
| 1 | Ka-Fai Chung | 23 | 1 | D J Buysse | 0.46 |
| 2 | Michael R Irwin | 18 | 2 | Charles M Morin | 0.32 |
| 3 | Jun J Mao | 18 | 3 | Wing-Fai Yeung | 0.26 |
| 4 | Branda Y M Yu | 15 | 4 | Jonah N Cohen | 0.14 |
| 5 | Sheila N Garland | 14 | 5 | Maurice M Ohayon | 0.11 |
In terms of the centrality of the cited authors, Buysse was the highest, reaching 0.46, and was cited the most. In addition, the centrality values of the top 5 authors were all > 0.1. Buysse is an expert in the field of sleep and he participated in the development of Pittsburgh Sleep Quality Index, which is widely used to assess sleep quality.[36]
3.5. Most cited journals and papers
The citations and centrality of the top 10 cited journals in the past decade are shown in Table 3. Sleep (IF = 6.313) ranked first with 633 citations and second for centrality at 0.27. Although Evidence-Based Complementary Alternative Medicine (IF = 2.65) ranked sixth with 391 citations, its centrality was 0.31, ranking first and indicating a central position in the citation partnership. The research areas of the 2 journals are neurology and complementary medicine.
Table 3.
Citation frequency and centrality of top 10 cited journals in recent 10 years.
| Cited journal | Total citations | Centrality | IF 2021 | WoS categories |
|---|---|---|---|---|
| SLEEP | 633 | 0.27 | 6.313 | CLINICAL NEUROLOGY; NEUROSCIENCES |
| SLEEP MEDICINE | 522 | 0.13 | 4.842 | CLINICAL NEUROLOGY |
| SLEEP MEDICINE REVIEWS | 458 | 0.11 | 11.401 | CLINICAL NEUROLOGY; NEUROSCIENCES |
| PLOS ONE | 455 | 0.16 | 3.752 | MULTIDISCIPLINARY SCIENCES |
| JOURNAL OF ALTERNATIVE AND COMPLEMENTARY MEDICINE | 443 | 0.22 | 2.381 | INTEGRATIVE & COMPLEMENTARY MEDICINE |
| EVIDENCE-BASED COMPLEMENTARY AND ALTERNATIVE MEDICINE | 433 | 0.31 | 2.65 | INTEGRATIVE & COMPLEMENTARY MEDICIN |
| PSYCHIATRY RESEARCH | 428 | 0.23 | 11.225 | PSYCHIATRY |
| JOURNAL OF PSYCHOSOMATIC RESEARCH | 401 | 0.23 | 4.62 | PSYCHIATRY |
| JAMA-JOURNAL OF THE AMERICAN MEDICAL ASSOCIATION | 391 | 0.29 | 157.335 | MEDICINE, GENERAL & INTERNAL |
| COMPLEMENTARY THERAPIES IN MEDICINE | 300 | 0.07 | 3.335 | INTEGRATIVE & COMPLEMENTARY MEDICIN |
The citations of the top 5 highly cited papers were all > 150 (Table 4), among which 4 were from the USA and 1 was from Canada. Except for one study on the effect of yoga on sleep quality, the other 4 studies on mindfulness meditation therapy. In addition, 3 of the 5 papers were studies on the sleep quality of cancer patients, indicating that mindfulness meditation therapy is a research hotspot in this field and that the sleep quality of cancer patients has attracted much attention in this field.
Table 4.
The top 5 most cited papers.
| Rank | Author | Year | Reference title | Country | Journal | Total citations |
|---|---|---|---|---|---|---|
| 1 | Black DS, et al | 2015 | Mindfulness meditation and improvement in sleep quality and daytime impairment among older adults with sleep disturbances: a randomized clinical trial | USA | JAMA INTERNAL MEDICINE | 212 |
| 2 | Bower JE, et al | 2015 | Mindfulness meditation for younger breast cancer survivors: a randomized controlled trial | USA | CANCER | 183 |
| 3 | Garland SN, et al | 2014 | Mindfulness-Based Stress Reduction Compared with Cognitive Behavioral Therapy for the Treatment of Insomnia Comorbid with Cancer: A Randomized, Partially Blinded, Noninferiority Trial | Canada | JOURNAL OF CLINICAL ONCOLOGY | 171 |
| 4 | Mustian KM, et al | 2013 | Multicenter, Randomized Controlled Trial of Yoga for Sleep Quality Among Cancer Survivors | USA | JOURNAL OF CLINICAL ONCOLOGY | 152 |
| 5 | Ong JC, et al | 2014 | A Randomized Controlled Trial of Mindfulness Meditation for Chronic Insomnia | USA | SLEEP | 150 |
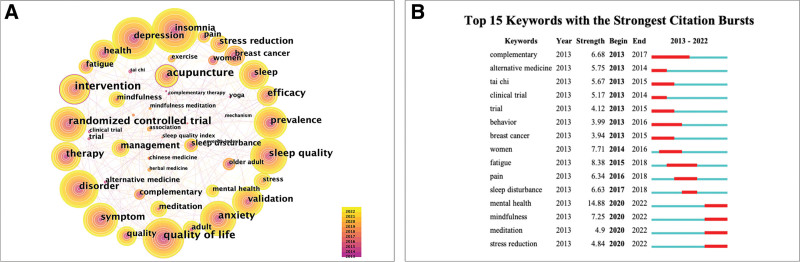
3.6. Analysis of co-occurring and cited keywords
Keyword co-occurrence (Fig. 4A) and citation (Fig. 4B) can reflect the research hotspots in this field to a certain extent. In the past decade, the top 3 keywords with the highest frequency were insomnia (count = 251), depression (count = 240), and quality of life (count = 220). The top 3 centrality rankings are intervention (centrality = 0.28), acupuncture (centrality = 0.27), and quality of life (centrality = 0.20). From 2020 to 2022, the most prominent keywords cited were mental health, mindfulness, meditation and stress reduction. Acupuncture, as a treatment method in CAM, has certain potential in alleviating insomnia and mental stress and for improving the quality of life. In recent years, mindfulness meditation therapy and the mental health of insomnia patients have received great attention as research hotspots, reflecting the latest research trends in this field.
Figure 4.
(A) Keyword co-occurrence diagram. (B) Top 15 most cited keywords.
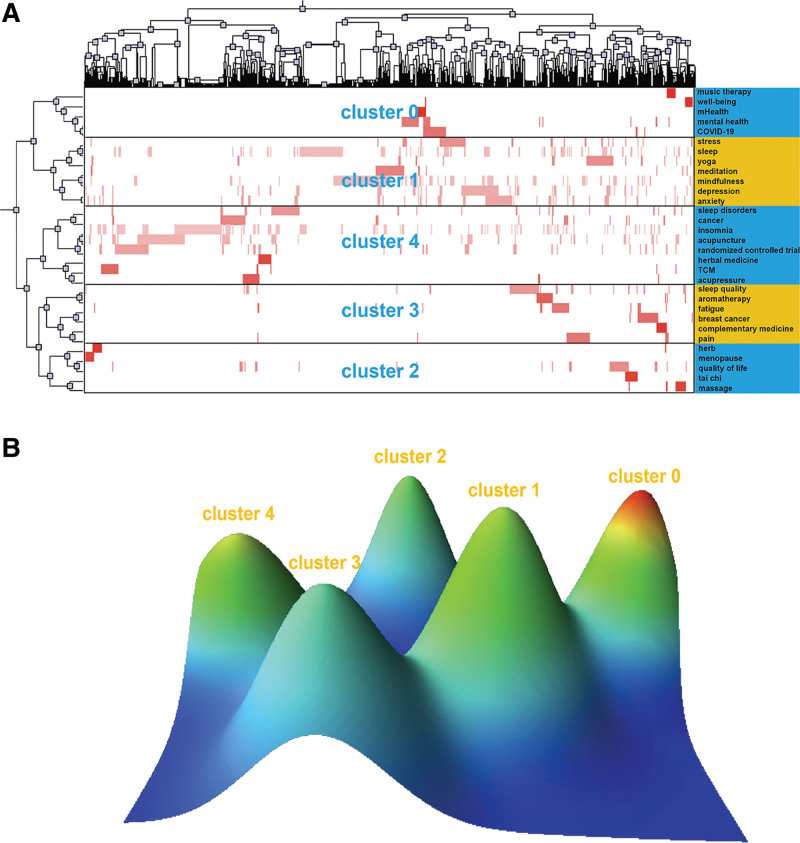
3.7. Biclustering of keywords
Keywords with frequency greater than or equal to 15 times were taken as high-frequency keywords for bicluster analysis. Then we get 31 high-frequency keywords that meet the conditions and the cumulative percentage of the total number of keywords was 27.94% (see Figure S1, Supplemental Digital Content, http://links.lww.com/MD/J271 for high-frequency keywords). We divided the 31 high-frequency keywords into 5 groups and then constructed a visualization matrix of the high-frequency keywords and the source literature (Fig. 5A). The rows represented the high-frequency keywords and the columns represented the source literature. The color depth of the red block was proportional to the frequency of the keywords. The effect of the visual matrix was verified by mountain visualization (Fig. 5B), with every mountain in the figure representing a cluster: the greater the similarity of keywords in the cluster, the higher the height of the mountain. The volume of the mountain was positively correlated with the number of keywords, with blue indicating a high standard deviation in the cluster and red showing the opposite. From the keywords contained in each cluster, we summarized the topics of each cluster to better grasp the research hotspots and trends of CAM intervention on insomnia and provide some hints for subsequent related research:
Figure 5.
(A) A bicluster matrix visualization of 31 high-frequency keywords and source articles. (B) Bicluster peak visualization of 31 high-frequency keywords and source articles.
Cluster 0: Music therapy and mobile health have helped with insomnia and mental health during the COVID-19 pandemic.
Cluster 1: Mindfulness meditation and yoga reduce mental anxiety and stress, thereby improving sleep.
Cluster 2: Herbal medicine, Tai chi and massage can improve the quality of life of menopausal women.
Cluster 3: Aromatherapy and complementary therapy relieve pain and associated fatigue in breast cancer patients, thereby improving sleep quality.
Cluster 4: Randomized controlled trials of TCM treatments such as acupuncture, massage and Chinese herbal medicine on sleep disorders have been carried out in cancer patients.
4. Discussion
In the past decade, the research on CAM intervention for insomnia has been increasing year by year. A total of 67 countries and regions have made contributions to the research in this field. Among them, the USA and China are the main exporting countries and the research institutions in these 2 countries occupy a central position in the research field, maintaining a cooperative relationship with the research institutions in other countries and regions; this is helpful because researchers can share resources, ideas and an exchange and discussion of personal opinions in order to better develop the related research of CAM intervention on insomnia. Although China and the USA have advantages in this field in terms of the ranking of the number of articles published by authors, it is not difficult to see that the cooperation between researchers is mostly internal cooperation between countries and institutions: a situation of close internal connection but less external connection was formed. The Chinese institutions and researchers mainly studied the influence of TCM-related CAM on insomnia, such as acupuncture, massage, Chinese herbal medicine, etc., whereas the USA paid more attention to the role of meditation, yoga and aromatherapy for improving insomnia. Due to the different research fields, there is relatively little cooperation among countries, which fails to build a strong cooperation network. The cooperation and exchange between national institutions and scholars needs to be strengthened. The research interventions in different countries are not the same but they are all CAM related and the main purpose is to improve insomnia. Therefore, cooperation and exchange with experts of different research backgrounds needs to be strengthened in order to promote the development of this field of research.
The top 3 cited journals were Sleep, Sleep Medicine, and Sleep Medicine Reviews, which are classified as clinical neurology and neuroscience in the WoSCC. The WoSCC discipline classification of Evidence-Based Complementary and Alternative Medicine is integrative and complementary medicine, having the highest centrality. Research in this field mainly focuses on disciplines such as neuroscience and complementary and alternative medicine, but the top 10 cited journals also include psychiatry and multidisciplinary disciplines, indicating that experts from different disciplines have deep roots in this field. In the past decade, most of the interventions in the highly cited articles in this field have been mindfulness meditation therapy, highly focused on the sleep quality of cancer patients, and the top 5 highly cited articles involve clinical controlled trials, which will be conducive to promote more high-quality well-designed clinical trials research in high-quality journals, with research development in the direction of the rational and reasonable, and to improve the impact and provide more help to insomnia sufferers.
The high-frequency keywords, keyword citations, and keyword co-occurrence show that this field has paid more attention to the mental status and quality of life of insomnia patients in the past decade, with the related hotspots of insomnia in cancer patients being particularly prominent (such as TCM-related CAM, which mainly focuses on acupuncture, massage and Chinese herbal medicine). Mindfulness meditation, yoga and aromatherapy have been hot topics in this field in the past 2 years but insomnia and its resulting psychiatric symptoms during the COVID-19 pandemic have recently become a hot topic.
China is one of the major producing countries in the field of CAM intervention for insomnia. The CAM interventions mainly studied by the institutions and authors include acupuncture, acupressure, Tai chi and Chinese herbal medicine, which also belong to the category of TCM. Electroacupuncture has been shown to significantly improve depression-related insomnia compared with placebo acupuncture[37] and to have a lasting effect on alleviating insomnia in menopausal patients,[38] but a study involving insomnia in 160 cancer survivors showed that, compared with first-line treatment CBT, the efficacy and durability of acupuncture and moxibustion is not very optimistic.[39] A three-arm clinical trial with 2 years of follow-up showed that although Tai chi had some advantages over no intervention for alleviating insomnia in older adults, its efficacy was not significantly different from that of regular exercise.[34] Acupressure and Chinese herbal medicine have shown certain advantages in improving fatigue and anxiety, respectively, in insomnia patients but there is a lack of high-quality supporting evidence.[40,41] Anxiety and insomnia are closely related, with about 69% of anxiety and depression occurring before insomnia[42] and about a third of cancer patients having anxiety symptoms that affect sleep and quality of life.[43] Furthermore, comorbidities such as pain, fatigue and hot flashes in cancer patients are also important factors to consider in interventions for alleviating insomnia.[39] Therefore, the development of a structured treatment plan to solve insomnia comorbidities and related psychiatric symptoms, in order to achieve the effect of insomnia relief, has become crucial in the treatment of insomnia related to TCM.
As can be seen from the keyword co-occurrence and highly cited articles, mindfulness meditation therapy is a hot research and application frontier in many countries and regions. Mindfulness meditation can affect the body and mind of insomniacs, including thoughts, feelings and body awareness. Several studies have shown that mindfulness meditation is of great help for relieving insomnia in cancer patients[44] and in the elderly[45] and also for treating chronic insomnia.[46] Moreover, compared with CBT, mindfulness meditation therapy is not inferior in improving insomnia and the psychological status of patients,[47] but it still needs large-scale clinical trials and related studies for verification.
During the COVID-19 pandemic, the drastic changes in daily work and life caused by measures such as home isolation, restriction of public activities and social distancing have brought stress and distress to different people. Furthermore, the resulting mental health problems, such as anxiety and depression, as well as economic stress have produced more cases of insomnia.[48,49] During this period, tele-psychotherapy, such as music therapy,[50] has provided new ideas for future tele-psychotherapy and dealing with public health problems.
4.1. Strengths and limitations
We only analyzed the WoSCC database, which may have led to an insufficiently comprehensive survey of the literature. Secondly, we limited the type of literature to articles and there may be some deviation as the quality of all the literature cannot be guaranteed. Based on the analysis of 1655 articles on CAM intervention for insomnia in the WoSCC database in the past decade, combined with the visualization and clustering results of CiteSpace and gCLUTO, we conducted the first visual bibliometric analysis in this field. Our results not only highlight the most influential countries, institutions, authors and literatures in this field in the past decade, but also objectively reflect the research status and hot development trends in this field and provide more reference information and basis for future research.
5. Conclusion
This study conducted a comprehensive and objective bibliometric analysis of the relevant articles published in the WoSCC in the past decade on CAM intervention for insomnia. It also summarizes and predicts the development trend and research hotspots of cooperation among countries, institutions and authors in the past 10 years. The results show that this field has good development prospects and that TCM-related CAM, cancer comorbidity-related insomnia, mindfulness meditation therapy and insomnia during the COVID-19 pandemic have been research hotspots in the past decade. Therefore, it will be the focus and development direction of insomnia treatment in the future to formulate structured treatment plans for TCM-related CAM, to validate large-scale clinical trials, to solve cancer comorbidity-related insomnia and its psychiatric symptoms and to deal with mental health-related insomnia after public health outbreaks.
Author contributions
Conceptualization: Siyun Li, Qian Xue, Yue Zhong.
Data curation: Siyun Li, Qian Xue, Pengfei Liao.
Investigation: Fengya Zhu.
Methodology: Qian Xue, Yue Zhong, Fengya Zhu.
Resources: Pengfei Liao, Xiaoyan Yang.
Software: Qiang Ji.
Visualization: Siyun Li, Yue Zhong, Qiang Ji.
Writing – original draft: Xia Feng, Li Zhou, Fengya Zhu.
Writing – review & editing: Li Zhou, Fengya Zhu.
Supplementary Material
Abbreviations:
- CAM
- complementary and alternative medicine
- CBT
- cognitive behavioral therapy
- WoSCC
- Web of Science Core Collection
SL and QX contributed equally to this work.
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are publicly available.
Supplemental Digital Content is available for this article.
How to cite this article: Li S, Xue Q, Zhong Y, Liao P, Ji Q, Yang X, Feng X, Zhou L, Zhu F. Research trends in complementary and alternative treatments for insomnia over the past decade: A bibliometrics analysis. Medicine 2023;102:29(e34346).
Contributor Information
Siyun Li, Email: 1026665151@qq.com.
Qian Xue, Email: dr_djyt@126.com.
Yue Zhong, Email: drzgyyy@foxmail.com.
Pengfei Liao, Email: notfoundy@foxmail.com.
Qiang Ji, Email: 1006922202@qq.com.
Xiaoyan Yang, Email: notfounds@foxmail.com.
Xia Feng, Email: 1334662949@qq.com.
Li Zhou, Email: 2873735419@qq.com.
References
- [1].Aikens JE, Rouse ME. Help-seeking for insomnia among adult patients in primary care. J Am Board Fam Pract. 2005;18:257–61. [DOI] [PubMed] [Google Scholar]
- [2].Buysse DJ. Insomnia. JAMA. 2013;309:706–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Morin CM, Vézina-Im LA, Ivers H, et al. Prevalent, incident, and persistent insomnia in a population-based cohort tested before (2018) and during the first-wave of COVID-19 pandemic (2020). Sleep. 2022;45:zsab258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Morin CM, Jarrin DC, Ivers H, et al. Incidence, persistence, and remission rates of insomnia over 5 years. JAMA Netw Open. 2020;3:e2018782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–9. [DOI] [PubMed] [Google Scholar]
- [6].Johnson DA, Knutson K, Colangelo LA, et al. Associations of chronic burden, sleep characteristics, and metabolic syndrome in the coronary artery risk development in young adults study. Psychosom Med. 2022;84:711–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Vgontzas AN, Liao D, Bixler EO, et al. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep. 2009;32:491–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Laugsand LE, Vatten LJ, Platou C, et al. Insomnia and the risk of acute myocardial infarction: a population study. Circulation. 2011;124:2073–81. [DOI] [PubMed] [Google Scholar]
- [9].Léger D, Morin CM, Uchiyama M, et al. Chronic insomnia, quality-of-life, and utility scores: comparison with good sleepers in a cross-sectional international survey. Sleep Med. 2012;13:43–51. [DOI] [PubMed] [Google Scholar]
- [10].Kalmbach DA, Cheng P, Ahmedani BK, et al. Cognitive-behavioral therapy for insomnia prevents and alleviates suicidal ideation: insomnia remission is a suicidolytic mechanism. Sleep. 2022;45:zsac251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kessler RC, Berglund PA, Coulouvrat C, et al. Insomnia and the performance of US workers: results from the America insomnia survey. Sleep. 2011;34:1161–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Sarsour K, Kalsekar A, Swindle R, et al. The association between insomnia severity and healthcare and productivity costs in a health plan sample. Sleep. 2011;34:443–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Wickwire EM, Shaya FT, Scharf SM. Health economics of insomnia treatments: the return on investment for a good night’s sleep. Sleep Med Rev. 2016;30:72–82. [DOI] [PubMed] [Google Scholar]
- [14].Schutte-Rodin S, Broch L, Buysse D, et al. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008;4:487–504. [PMC free article] [PubMed] [Google Scholar]
- [15].Riemann D, Baglioni C, Bassetti C, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26:675–700. [DOI] [PubMed] [Google Scholar]
- [16].Wilt TJ, MacDonald R, Brasure M, et al. Pharmacologic treatment of insomnia disorder: an evidence report for a clinical practice guideline by the American College of Physicians. Ann Intern Med. 2016;165:103–12. [DOI] [PubMed] [Google Scholar]
- [17].Smink BE, Egberts AC, Lusthof KJ, et al. The relationship between benzodiazepine use and traffic accidents: a systematic literature review. CNS Drugs. 2010;24:639–53. [DOI] [PubMed] [Google Scholar]
- [18].Hajak G, Müller WE, Wittchen HU, et al. Abuse and dependence potential for the non-benzodiazepine hypnotics zolpidem and zopiclone: a review of case reports and epidemiological data. Addiction. 2003;98:1371–8. [DOI] [PubMed] [Google Scholar]
- [19].Zeng-jie Y, Mu-Zi L, Qu H, et al. Research progress of insomnia disorders at home and abroad. Medic Philosophy (B). 2017;38:60–3. [Google Scholar]
- [20].Woolcott JC, Richardson KJ, Wiens MO, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169:1952–60. [DOI] [PubMed] [Google Scholar]
- [21].Verma K, Singh D, Srivastava A. The impact of complementary and alternative medicine on insomnia: a systematic review. Cureus. 2022;14:e28425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Wang F, Eun-Kyoung Lee O, Feng F, et al. The effect of meditative movement on sleep quality: a systematic review. Sleep Med Rev. 2016;30:43–52. [DOI] [PubMed] [Google Scholar]
- [23].Mustian KM, Sprod LK, Janelsins M, et al. Multicenter, randomized controlled trial of yoga for sleep quality among cancer survivors. J Clin Oncol. 2013;31:3233–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Irwin MR, Olmstead R, Motivala SJ. Improving sleep quality in older adults with moderate sleep complaints: a randomized controlled trial of Tai Chi Chih. Sleep. 2008;31:1001–8. [PMC free article] [PubMed] [Google Scholar]
- [25].Wang YK, Li T, Ha LJ, et al. Effectiveness and cerebral responses of multi-points acupuncture for primary insomnia: a preliminary randomized clinical trial and fMRI study. BMC Complement Med Ther. 2020;20:254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Kim YM, Delen D. Medical informatics research trend analysis: a text mining approach. Health Informatics J. 2018;24:432–52. [DOI] [PubMed] [Google Scholar]
- [27].Taj F, Klein MCA, van Halteren A. Digital health behavior change technology: bibliometric and scoping review of two decades of research. JMIR Mhealth Uhealth. 2019;7:e13311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Guler AT, Waaijer CJ, Palmblad M. Scientific workflows for bibliometrics. Scientometrics. 2016;107:385–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Qaseem A, Kansagara D, Forciea MA, et al.; Clinical Guidelines Committee of the American College of Physicians. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American college of physicians. Ann Intern Med. 2016;165:125–33. [DOI] [PubMed] [Google Scholar]
- [30].Yue C, Chaomei C, Zeyuan L, et al. The methodological function of CiteSpace knowledge map. Res Sci Sci. 2015;33:242–53. [Google Scholar]
- [31].Lei C, Wei L, Lei Y, et al. Development of bibliographic information co-occurrence mining system in literature database. Modern Library Inform Technol. 2008:70–5. [Google Scholar]
- [32].Yin S, Zhu F, Li Z, et al. Research hotspots and trends in music therapy intervention for patients with dementia: a bibliometrics and visual analysis of papers published from 2010 to 2021. Front Psychiatry. 2022;13:860758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Chung KF, Yeung WF, Yu BYM, et al. Combined electroacupuncture and auricular acupuncture for primary insomnia: a randomised controlled trial of dose-response effect. Hong Kong Med J. 2019;25 Suppl 2:28–33. [PubMed] [Google Scholar]
- [34].Siu PM, Yu AP, Tam BT, et al. Effects of Tai Chi or exercise on sleep in older adults with insomnia: a randomized clinical trial. JAMA Netw Open. 2021;4:e2037199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Chung KF, Yeung WF, Yu BY, et al. Acupuncture with or without combined auricular acupuncture for insomnia: a randomised, waitlist-controlled trial. Acupunct Med. 2018;36:2–13. [DOI] [PubMed] [Google Scholar]
- [36].Buysse DJ, Reynolds CF, 3rd, Monk TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. [DOI] [PubMed] [Google Scholar]
- [37].Yin X, Li W, Wu H, et al. Efficacy of Electroacupuncture on treating depression-related insomnia: a randomized controlled trial. Nat Sci Sleep. 2020;12:497–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Li S, Wang Z, Wu H, et al. Electroacupuncture versus sham acupuncture for perimenopausal insomnia: a randomized controlled clinical trial. Nat Sci Sleep. 2020;12:1201–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Romero SAD, Jiang E, Bussell J, et al. What makes one respond to acupuncture for insomnia? Perspectives of cancer survivors. Palliat Support Care. 2020;18:301–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Ho FY, Choi WT, Yeung WF, et al. The efficacy of integrated cognitive behavioral therapy (CBT) and acupressure versus CBT for insomnia: a three-arm pilot randomized controlled trial. Sleep Med. 2021;87:158–67. [DOI] [PubMed] [Google Scholar]
- [41].Chen S, Xu Z, Li Y, et al. Clinical efficacy of the Chinese herbal medicine Shumian capsule for insomnia: a randomized, double-blind, placebo-controlled trial. Neuropsychiatr Dis Treat. 2022;18:669–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res. 2006;40:700–8. [DOI] [PubMed] [Google Scholar]
- [43].Gonzalez-Ling A, Galindo Vázquez O, Espinoza Bello M, et al. Quality of life, anxiety, depression, and distress in patients with advanced and metastatic lung cancer. Palliat Support Care. 2022:1–8. [DOI] [PubMed] [Google Scholar]
- [44].Bower JE, Crosswell AD, Stanton AL, et al. Mindfulness meditation for younger breast cancer survivors: a randomized controlled trial. Cancer. 2015;121:1231–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Black DS, O’Reilly GA, Olmstead R, et al. Mindfulness meditation and improvement in sleep quality and daytime impairment among older adults with sleep disturbances: a randomized clinical trial. JAMA Intern Med. 2015;175:494–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Ong JC, Manber R, Segal Z, et al. A randomized controlled trial of mindfulness meditation for chronic insomnia. Sleep. 2014;37:1553–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Garland SN, Carlson LE, Stephens AJ, et al. Mindfulness-based stress reduction compared with cognitive behavioral therapy for the treatment of insomnia comorbid with cancer: a randomized, partially blinded, noninferiority trial. J Clin Oncol. 2014;32:449–57. [DOI] [PubMed] [Google Scholar]
- [48].Halsøy O, Johnson SU, Hoffart A, et al. Insomnia symptoms in the general population during the COVID-19 pandemic. Front Psychiatry. 2021;12:762799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Wang C, Song W, Hu X, et al. Depressive, anxiety, and insomnia symptoms between population in quarantine and general population during the COVID-19 pandemic: a case-controlled study. BMC Psychiatry. 2021;21:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Situmorang DDB. “When the first session may be the last!”: a case report of the implementation of “rapid tele-psychotherapy” with single-session music therapy in the COVID-19 outbreak. Palliat Support Care. 2022;20:290–5. [DOI] [PMC free article] [PubMed] [Google Scholar]