Patients affected by severe brain injury can experience complex states of disordered consciousness. These include the comatose state, characterized by a complete loss of spontaneous or stimulus-induced wakefulness and awareness; the vegetative state/unresponsive wakefulness syndrome, in which patients can be awake but exhibit no signs of conscious perception or deliberate action; the minimally conscious state, characterized by low-level awareness of self or environment; and the acute confusional state, which entails the recovery of wakefulness and awareness with persistent confusion.1,2 Patients with acute brain injuries may move unpredictably between these states and often evade precise and accurate assessment due to limitations in assessment techniques and patient-specific factors masking expression of consciousness.3
Uncertainty about a patient's state of consciousness or likelihood of functional recovery may importantly contribute to pervasive discordance between family members and clinicians of critically ill patients with disorders of consciousness.4-7 Families often express more optimistic predictions for recovery due to beliefs in their loved ones' resilience and personal strengths, at times in contrast to clinicians' possibly less optimistic perspectives on patient outcomes.8-11 The practical significance and gravity of such discordance are underscored by the reality that weighty decisions to continue, withhold, or withdraw life-sustaining treatments are often predicated on expectations surrounding the likelihood and degree to which consciousness will recover after severe brain injury.12-14 Because of the central role that consciousness and its potential for recovery plays in medical decision-making and discussions surrounding patients with disorders of consciousness, reconciling discordant perspectives about a patient's state of consciousness, potential for recovery, and the worthwhileness of life-sustaining treatment necessitates critical exploration of how consciousness is defined, operationalized, and valued by different stakeholder groups across clinical settings. Yet, assumptions about the nature and value of consciousness are often tacitly assumed and seldom discussed in clinical settings, thereby generating potential for conflation of distinct concepts of consciousness during key moments of medical communication. Such conflations could consequently animate misguided inferences, miscommunication, and goal-discordant decision-making during life-or-death moments for patients with disorders of consciousness. In this study, we explain and critically evaluate these underexplored issues and develop a framework for reconciling diagnostic and prognostic discordance between family members and clinicians by disambiguating types of consciousness applied in different conversational contexts that arise in clinical settings.
Conversations About Consciousness
There are at least 3 different conversational scenarios in which the disambiguation of the term “consciousness” may aid in the resolution of decisional conflicts: conversations about diagnosis; conversations about prognosis and life-sustaining treatment; and conversations about ethics.
Conversations About Diagnosis
When assessing consciousness in patients with disorders of consciousness, clinicians typically rely on standardized behavioral testing to generate statistically consistent interpretations of signs of consciousness.15,16 By contrast, families may alternatively rely on interpretive frameworks based on the patient's personality and social relationships and may believe in the presence of an underlying consciousness even in the absence of overt behavioral expression that allows the patient to experience treatment or benefit from social interactions.17-21 These perspectives may motivate caregivers to regard a patient as if they are able to hear conversations or feel self-conscious about their appearance even if they do not exhibit behavioral evidence of awareness.15,22 In this study, 2 different types of “consciousness” that may be simultaneously applied in conversations about diagnosis can be distinguished: behavioral consciousness and nonbehavioral phenomenal consciousness. Behavioral consciousness refers to consciousness that allows the patient to exhibit intentional action and communication through their functional capacities in a reliably detectable manner. On the contrary, nonbehavioral phenomenal consciousness refers to a conscious state that allows the patient to have subjective experiences, even if they are unable to express themselves. Although this type of consciousness seems to be more often informally intuited by families and clinicians, increasingly novel neurotechnologies may be used to detect consciousness beyond overt behavioral expression.17,23,24
In these disambiguated terms, by virtue of prevailing diagnostic approaches that prioritize behavioral markers of consciousness, clinicians often approach detection of consciousness and prediction of recovery by focusing on testing for behavioral consciousness while families may presume an underlying nonbehavioral phenomenal consciousness in patients who are behaviorally unexpressive. Thus, when a clinician determines that a patient “lacks consciousness” (i.e., is in coma or vegetative state/unresponsive wakefulness syndrome) after performing a series of tests for behavioral consciousness without disambiguating the kind of consciousness queried, it may conflict with a family's belief that the patient possesses nonbehavioral phenomenal consciousness, potentially magnifying skepticism about the reliability of the clinical assessment.15 To reconcile this conflict, clinicians might more appropriately describe that they were unable to detect behavioral consciousness when using standard behavioral diagnostic approaches such as the Coma Recovery Scale–Revised, leaving open the possibility of preserved nonbehavioral phenomenal consciousness. Indeed, this possibility has been evinced in recent studies on stimulus-based and task-based functional neuroimaging and EEG demonstrating preserved awareness and attention in some patients determined behaviorally to be in coma or vegetative state/unresponsive wakefulness syndrome.23,25-27 To sensitize nosology for disorders of consciousness and diagnostic approaches to these important distinctions, family caregivers can also be invited to play a role in the diagnostic process because they may be more attuned to their loved one's state of consciousness and pick up on subtle signs or expressive cues that might evade routine clinical detection.24,28
Conversations About Prognosis and Life-Sustaining Treatment
Clinicians who provide life-sustaining treatment for patients with disorders of consciousness routinely use standardized behavioral examination (e.g., Coma Recovery Scale–Revised and Glasgow Coma Scale) to track progress and assess the benefit of continuing treatment for patients who demonstrate little to no sign of behavioral consciousness. By contrast, some families may be inclined to make decisions about life-sustaining treatment based on their belief in the patient's possession of nonbehavioral phenomenal consciousness. Surrogate decision-makers who opt to continue life-sustaining treatment may do so because they believe that a patient who possesses nonbehavioral phenomenal consciousness will be motivated to regain behavioral consciousness.17 By contrast, those who decide to withdraw life-sustaining treatment might do so because their loved one would “not want to live like this” or due to ascriptions of low quality of life, thus opting to withdraw or withhold treatment because they believe that prolonged nonbehavioral phenomenal consciousness without behavioral consciousness is undesirable and not necessarily because they believe that their loved one lacks consciousness.29 Either decision may be animated by persistent beliefs in a patient's underlying nonbehavioral phenomenal consciousness, which could be supported by families spending more time observing and providing salient stimulation for the patient.17,30 Therefore, it may be prudent for clinicians not to render recommendations about life-sustaining treatment based solely on assessments of behavioral consciousness, but to further explicate how this affects their valuation of the patient's nonbehavioral phenomenal consciousness or other aspects of consciousness as construed by family members. Clinicians who shift decision-making conversations away from the behavior-centered paradigm can validate a family's intuitive considerations about the patient's nonbehavioral phenomenal consciousness and seriously consider their perspectives on a patient's quality of life as a nonbehavioral, conscious being.31
Clinicians can also preempt potential conflicts by proactively eliciting and accounting for family member beliefs about consciousness in clinical judgments and decisions surrounding life-sustaining treatment. This framework can move metaphysically intractable debates about whether a patient is “truly conscious” toward ethical conversations about whether and how a patient's nonbehavioral phenomenal consciousness, if it exists, should be sustained. For some families, these conversations may center on the importance of proper communication of the level of prognostic certainty in likelihood of recovery of behavioral consciousness so that families can accurately assess the value of maintaining a potential state of nonbehavioral phenomenal consciousness.32-34 Given the high degree of prognostic uncertainty in the field of disorders of consciousness, some may feel that even a small chance at recovering behavioral consciousness may justify continuing life-sustaining treatment for a period.1,14 By eliciting and acknowledging the individualized beliefs, values, and goals that might importantly bear on such treatment preferences, clinicians have the opportunity to cultivate trustworthy relationships by inviting caregivers into the diagnostic and prognostic process, highlighting how potential endpoints might align with or conflict with individual patient goals, and providing multidisciplinary, longitudinal support that affords families the time to navigate a complex decision-making process and revisit goals of care discussions as needed.
Conversations About Ethics
Discussions about continuing life-sustaining treatment for patients with disorders of consciousness may be considered in light of ethical questions about the value of living “merely” with nonbehavioral phenomenal consciousness. A study by Kostick et al.17 suggests that some family members may believe that suffering and discomfort in patients in a minimally conscious state is a “necessary evil” to eventually recover behavioral consciousness and other functions subserved thereby. By contrast, clinicians may believe that living in minimally conscious state is worse than having no consciousness because a patient could live with continuous suffering.17 This brings into question the extent to which clinicians and family members project their own conscious experiences to evaluate another's phenomenal state of mind and the possibility of pessimistic biases in such projections. Indeed, individuals with disabilities, including neurologic conditions such as spinal cord injuries and locked-in syndrome, often rate the quality of their lives substantially higher than nondisabled individuals' expectations of their ratings, a phenomenon known as the disability paradox.35,36 In the absence of empirical evidence around quality of life in states of disordered consciousness, judgments concerning well-being, suffering, or value of life across the spectrum of disorders of consciousness are vulnerable to the disability paradox and other cognitive biases. This may lead to misplaced “futility” judgments and overtly or covertly influence the conversational framing of treatment decisions.37,38 By disambiguating nonbehavioral phenomenal consciousness from behavioral consciousness, clinicians and families will be in a better position to identify and reassess potential biases about a phenomenally conscious patient's quality of life without conflating them with value judgments about inability to attain behavioral consciousness.
Refining the Conversation
Given the ethical issues that arise from conflating behavioral consciousness and nonbehavioral phenomenal consciousness in various medical conversations and in light of recent prominent research enabling the detection of consciousness beyond behavioral criteria, we propose 2 areas of change that can reduce decisional discordance between providers and families of patients with disorders of consciousness. First, communicative framings around assessments of consciousness should be sensitized to different types of consciousness, with existing neurobehavioral techniques being categorized as tests for behavioral consciousness and resting state, stimulus-based or task-based neuroimaging, or electrophysiologic techniques being categorized as tests for potential nonbehavioral phenomenal consciousness. This distinct categorization of assessment types may promote broader implementation of novel neurotechnologies to assess for potential nonbehavioral phenomenal consciousness in patients who are behaviorally unexpressive due to neurologic injury and cognitive motor dissociation.23-25 Innovations in neuroimaging and electrophysiology are still largely limited to the realm of research and select academic medical centers. Recognizing the distinction between behavioral consciousness and nonbehavioral phenomenal consciousness can create more widespread incorporation of novel neurotechnology into the process of detecting consciousness. In addition, caregivers may serve a greater role in the diagnostic process by drawing upon their personal relationships to detect individualized signs of consciousness from loved ones, which may provide valuable insights into their phenomenal state of mind.30 Various studies demonstrate the importance of caregiver presence in detecting and eliciting signs of consciousness by virtue of longer bedside observations and provision of salient stimulation, which could even facilitate improvement in patients.28,39,40 Such insights may help inform clinical assessments of consciousness and reduce discrepant perceptions of consciousness between families and clinicians. These are promising assets to the diagnostic and prognostic processes in disorders of consciousness that can be incorporated into clinical practice by first recognizing the value of caregivers' perceptions of consciousness in their loved ones.
Second, disambiguating behavioral consciousness and nonbehavioral phenomenal consciousness in clinical nosology and diagnostic criteria for disorders of consciousness is necessary to preempt conceptual conflation and miscommunication. Clinical diagnoses such as coma, vegetative state/unresponsive wakefulness syndrome, and minimally conscious state are predicated on predominantly behavioral diagnostic criteria codified in clinical guidelines.1 Reframing and contextualizing these conditions as “behavioral coma” or “behavioral vegetative state/unresponsive wakefulness syndrome” when based on behavioral diagnostic techniques may aid clinicians in communicating more accurate diagnostic assessments when sharing impressions with family members. Terms such as minimally conscious state ± can also be stratified into behavioral and nonbehavioral classifications, given that levels of consciousness may be present at higher levels than what behavioral examinations of patients in those states might reveal. Incorporating this refined nosology into conversations with families may help mitigate miscommunication or erroneous dismissal of families' judgments about preserved consciousness in the absence of overt behavioral signs.
Conclusions: Remapping the Clinical Cartography of Consciousness
The prevailing clinical approach to diagnosing and classifying disorders of consciousness fails to reflect the multifaceted nature of consciousness by measuring it solely along behavioral dimensions. Distinguishing between behavioral consciousness and nonbehavioral phenomenal consciousness is a first step toward resolving the frequent conflation of different implied meanings of “consciousness,” which could animate decisional conflicts about the diagnosis, prognosis, and treatment of patients with disorders of consciousness. Refinements to prevailing clinical nosology and stakeholder involvement in the diagnostic process can further reinforce this distinction and potentially catalyze integration of neurotechnologies to improve precision detection of consciousness and prediction of recovery after severe brain injury. To promote more productive conversations about assessing, treating, and pondering the value of the lives of patients with disorders of consciousness, clinicians and researchers must first disambiguate different uses of the term consciousness in order to find a common conceptual ground with families and work cooperatively toward goal-concordant outcomes.
Appendix. Authors
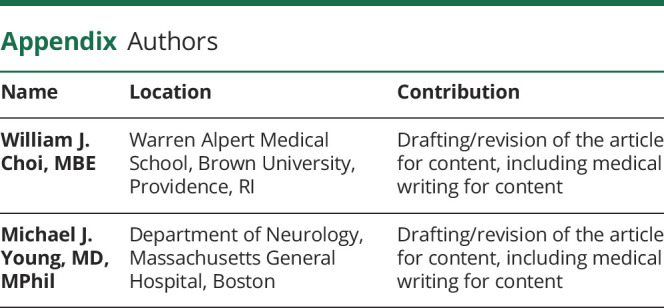
| Name | Location | Contribution |
| William J. Choi, MBE | Warren Alpert Medical School, Brown University, Providence, RI | Drafting/revision of the article for content, including medical writing for content |
| Michael J. Young, MD, MPhil | Department of Neurology, Massachusetts General Hospital, Boston | Drafting/revision of the article for content, including medical writing for content |
Study Funding
NIH BRAIN Initiative F32MH123001.
Disclosure
M.J. Young is funded by NIH BRAIN Initiative F32MH123001. W.J. Choi reports no relevant disclosures. Go to Neurology.org/N for full disclosures.
References
- 1.Giacino JT, Katz DI, Schiff ND, et al. Practice guideline update recommendations summary: disorders of consciousness: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology; the American Congress of Rehabilitation Medicine; and the National Institute on Disability, Independent Living, and Rehabilitation Research. Neurology. 2018;91(10):450-460. doi: 10.1212/WNL.0000000000005926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giacino JT, Fins JJ, Laureys S, Schiff ND. Disorders of consciousness after acquired brain injury: the state of the science. Nat Rev Neurol. 2014;10(2):99-114. doi: 10.1038/nrneurol.2013.279 [DOI] [PubMed] [Google Scholar]
- 3.Giacino JT, Schnakers C, Rodriguez-Moreno D, Kalmar K, Schiff N, Hirsch J. Behavioral assessment in patients with disorders of consciousness: gold standard or fool's gold? In: Laureys S, Schiff ND, Owen AM, eds. Progress in Brain Research. Vol. 177. Coma Science: Clinical and Ethical Implications. Elsevier; 2009:33-48. doi: 10.1016/S0079-6123(09)17704-X [DOI] [PubMed] [Google Scholar]
- 4.Goss AL, Voumard RR, Engelberg RA, Curtis JR, Creutzfeldt CJ. Do they have a choice? Surrogate decision-making after severe acute brain injury. Crit Care Med. 2023;51(7):924-935. doi: 10.1097/CCM.0000000000005850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kiker WA, Rutz Voumard R, Andrews LIB, et al. Assessment of discordance between physicians and family members regarding prognosis in patients with severe acute brain injury. JAMA Netw Open. 2021;4(10):e2128991. doi: 10.1001/jamanetworkopen.2021.28991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hwang DY, Knies AK, Mampre D, et al. Concerns of surrogate decision makers for patients with acute brain injury: a US population survey. Neurology. 2020;94(19):e2054-e2068. doi: 10.1212/WNL.0000000000009406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Muehlschlegel S. When doctors and families disagree in the neurologic intensive care unit-misunderstandings and optimistic beliefs. JAMA Netw Open. 2021;4(10):e2129079. doi: 10.1001/jamanetworkopen.2021.29079 [DOI] [PubMed] [Google Scholar]
- 8.Kiker WA, Voumard RR, Plinke W, Longstreth WT, Curtis JR, Creutzfeldt CJ. Prognosis predictions by families, physicians, and nurses of patients with severe acute brain injury: agreement and accuracy. Neurocrit Care. 2022;37(1):38-46. doi: 10.1007/s12028-022-01501-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.White DB, Ernecoff N, Buddadhumaruk P, et al. Prevalence of and factors related to discordance about prognosis between physicians and surrogate decision makers of critically ill patients. JAMA. 2016;315(19):2086-2094. doi: 10.1001/jama.2016.5351 [DOI] [PubMed] [Google Scholar]
- 10.Boyd EA, Lo B, Evans LR, et al. “It's not just what the doctor tells me:” factors that influence surrogate decision-makers’ perceptions of prognosis. Crit Care Med. 2010;38(5):1270-1275. doi: 10.1097/CCM.0b013e3181d8a217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hemphill JC, White DB. Clinical nihilism in neuro-emergencies. Emerg Med Clin North Am. 2009;27(1):27-37, vii-viii. doi: 10.1016/j.emc.2008.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Turgeon AF, Lauzier F, Simard JF, et al. Mortality associated with withdrawal of life-sustaining therapy for patients with severe traumatic brain injury: a Canadian multicentre cohort study. CMAJ. 2011;183(14):1581-1588. doi: 10.1503/cmaj.101786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lazaridis C. Withdrawal of life-sustaining treatments in perceived devastating brain injury: the key role of uncertainty. Neurocrit Care. 2019;30(1):33-41. doi: 10.1007/s12028-018-0595-8 [DOI] [PubMed] [Google Scholar]
- 14.Jones K, Quinn T, Mazor KM, Muehlschlegel S. Prognostic uncertainty in critically ill patients with traumatic brain injury: a multicenter qualitative study. Neurocrit Care. 2021;35(2):311-321. doi: 10.1007/s12028-021-01230-3 [DOI] [PubMed] [Google Scholar]
- 15.Edgar A, Kitzinger C, Kitzinger J. Interpreting chronic disorders of consciousness: medical science and family experience. J Eval Clin Pract. 2015;21(3):374-379. doi: 10.1111/jep.12220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thibaut A, Bodien YG, Laureys S, Giacino JT. Minimally conscious state “plus”: diagnostic criteria and relation to functional recovery. J Neurol. 2020;267(5):1245-1254. doi: 10.1007/s00415-019-09628-y [DOI] [PubMed] [Google Scholar]
- 17.Kostick KM, Halm A, O'Brien K, Kothari S, Blumenthal-Barby JS. Conceptualizations of consciousness and continuation of care among family members and health professionals caring for patients in a minimally conscious state. Disabil Rehabil. 2021;43(16):2285-2294. doi: 10.1080/09638288.2019.1697383 [DOI] [PubMed] [Google Scholar]
- 18.Latchem J, Kitzinger J, Kitzinger C. Physiotherapy for vegetative and minimally conscious state patients: family perceptions and experiences. Disabil Rehabil. 2016;38(1):22-29. doi: 10.3109/09638288.2015.1005759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Samuel G, Kitzinger J. Reporting consciousness in coma: media framing of neuro-scientific research, hope, and the response of families with relatives in vegetative and minimally conscious states. JOMEC J. 2013;3:10244. doi: 10.18573/j.2013.10244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Demertzi A, Schnakers C, Ledoux D, et al. Different beliefs about pain perception in the vegetative and minimally conscious states: a European survey of medical and paramedical professionals. Prog Brain Res. 2009;177:329-338. doi: 10.1016/S0079-6123(09)17722-1 [DOI] [PubMed] [Google Scholar]
- 21.Peterson A, Kostick KM, O'Brien KA, Blumenthal-Barby J. Seeing minds in patients with disorders of consciousness. Brain Inj. 2020;34(3):390-398. doi: 10.1080/02699052.2019.1706000 [DOI] [PubMed] [Google Scholar]
- 22.Blain-Moraes S, Racine E, Mashour GA. Consciousness and personhood in medical care. Front Hum Neurosci. 2018;12:306. doi: 10.3389/fnhum.2018.00306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morlet D, Mattout J, Fischer C, et al. Infraclinical detection of voluntary attention in coma and post-coma patients using electrophysiology. Clin Neurophysiol. 2023;145:151-161. doi: 10.1016/j.clinph.2022.09.019 [DOI] [PubMed] [Google Scholar]
- 24.Diserens K, Meyer IA, Jöhr J, et al. A focus on subtle signs and motor behavior to unveil awareness in unresponsive brain-impaired patients: the importance of being clinical. Neurology. 2023;100(24):1144-1150. doi: 10.1212/WNL.0000000000207067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Egbebike J, Shen Q, Doyle K, et al. Cognitive-motor dissociation and time to functional recovery in patients with acute brain injury in the USA: a prospective observational cohort study. Lancet Neurol. 2022;21(8):704-713. doi: 10.1016/S1474-4422(22)00212-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gomez LA, Shen Q, Doyle K, et al. Classification of level of consciousness in a neurological ICU using physiological data. Neurocrit Care. 2023;38(1):118-128. doi: 10.1007/s12028-022-01586-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Edlow BL, Chatelle C, Spencer CA, et al. Early detection of consciousness in patients with acute severe traumatic brain injury. Brain. 2017;140(9):2399-2414. doi: 10.1093/brain/awx176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moretta P, Trojano L, Masotta O, Cardinale V, Loreto V, Estraneo A. Family caregivers' opinions about interaction with the environment in consciousness disorders. Rehabil Psychol. 2017;62:208-213. doi: 10.1037/rep0000144 [DOI] [PubMed] [Google Scholar]
- 29.Kitzinger C, Kitzinger J. Family perspectives on ‘proper medical treatment’ for people in prolonged vegetative and minimally conscious states. In: Fovargue S, Mullock A, eds. The Legitimacy of Medical Treatment: What Role for the Medical Exception. Wellcome Trust–Funded Monographs and Book Chapters. Routledge; 2015. Accessed January 1, 2023. ncbi.nlm.nih.gov/books/NBK326662/. [Google Scholar]
- 30.Sattin D, Giovannetti AM, Ciaraffa F, et al. Assessment of patients with disorder of consciousness: do different Coma Recovery Scale scoring correlate with different settings? J Neurol. 2014;261(12):2378-2386. doi: 10.1007/s00415-014-7478-5 [DOI] [PubMed] [Google Scholar]
- 31.Siewert C. C1. Consciousness: value, concern, respect. In: Kriegel U, ed. Oxford Studies in Philosophy of Mind Volume 1. Oxford University Press; 2021. doi: 10.1093/oso/9780198845850.003.0001 [DOI] [Google Scholar]
- 32.van Til J, Bouwers-Beens E, Mertens M, Boenink M, Groothuis-Oudshoorn C, Hofmeijer J. Prognostication of patients in coma after cardiac arrest: public perspectives. Resuscitation. 2021;169:4-10. doi: 10.1016/j.resuscitation.2021.10.002 [DOI] [PubMed] [Google Scholar]
- 33.Steinberg A, Abella BS, Gilmore EJ, et al. Frequency of withdrawal of life-sustaining therapy for perceived poor neurologic prognosis. Crit Care Explor. 2021;3(7):e0487. doi: 10.1097/CCE.0000000000000487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Elmer J, Kurz MC, Coppler PJ, et al. Time to awakening and self-fulfilling prophecies after cardiac arrest. Crit Care Med. 2023;51(4):503-512. doi: 10.1097/CCM.0000000000005790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eisenberg MG, Saltz CC. Quality of life among aging spinal cord injured persons: long term rehabilitation outcomes. Paraplegia. 1991;29(8):514-520. doi: 10.1038/sc.1991.74 [DOI] [PubMed] [Google Scholar]
- 36.Rousseau MC, Baumstarck K, Alessandrini M, Blandin V, Billette de Villemeur T, Auquier P. Quality of life in patients with locked-in syndrome: evolution over a 6-year period. Orphanet J Rare Dis. 2015;10(1):88. doi: 10.1186/s13023-015-0304-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kothari S. Clinical (mis)judgments of quality of life after disability. J Clin Ethics. 2004;15(4):300-307. [PubMed] [Google Scholar]
- 38.Bosslet GT, Pope TM, Rubenfeld GD, et al. An official ATS/AACN/ACCP/ESICM/SCCM policy statement: responding to requests for potentially inappropriate treatments in intensive care units. Am J Respir Crit Care Med. 2015;191(11):1318-1330. doi: 10.1164/rccm.201505-0924ST [DOI] [PubMed] [Google Scholar]
- 39.Eickhoff SB, Dafotakis M, Grefkes C, et al. fMRI reveals cognitive and emotional processing in a long-term comatose patient. Exp Neurol. 2008;214(2):240-246. doi: 10.1016/j.expneurol.2008.08.007 [DOI] [PubMed] [Google Scholar]
- 40.Pape TLB, Rosenow JM, Steiner M, et al. Placebo-controlled trial of familiar auditory sensory training for acute severe traumatic brain injury: a preliminary report. Neurorehabil Neural Repair. 2015;29(6):537-547. doi: 10.1177/1545968314554626 [DOI] [PubMed] [Google Scholar]


