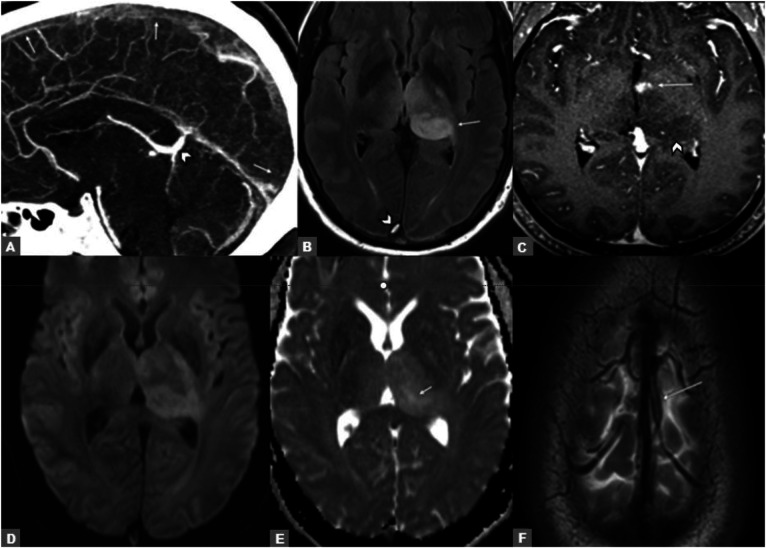
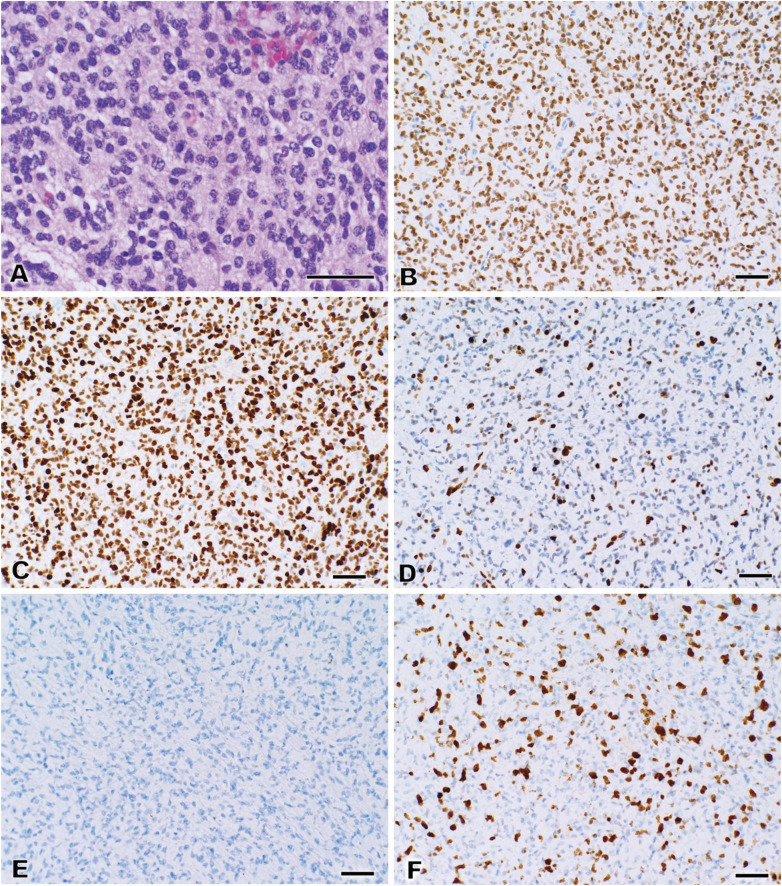
A 57-year-old man presented with 2 weeks of headache, binocular diplopia, and progressive confusion. CT venogram showed extensive cerebral venous thrombosis (CVT) (Figure 1A). He was started on a heparin drip before conversion to therapeutic enoxaparin. Initial (Figure 1B) and follow-up (Figure 1C) brain MRI showed left thalamic FLAIR hyperintensity without diffusion restriction (Figure 1, D and E). Thalamic biopsy revealed a diffuse midline glioma (DMG), H3 K27-altered, CNS WHO grade 4 (Figure 2). Whole-exome sequencing confirmed the presence of H3-3A (previously H3F3A) K27M and absence of such variants in IDH1/2.1 Initial differential diagnosis for the FLAIR hyperintensity favored edema due to venous congestion as the result of thrombosis of the left vein of Trolard (Figure 1F). Given a negative hypercoagulability panel, after biopsy-confirmed diagnosis, the CVT was believed to be precipitated by the DMG, which likely carries an increased risk of CVT similar to glioblastoma.2 By the follow-up neuro-oncology visit, his mental status had returned to normal. His anticoagulation was changed to apixaban, and he began a course of temozolomide and radiation.
Figure 1. CT Venogram and Brain MRI.
(A) Initial CT venogram demonstrates filling defects in the superior sagittal sinus (SSS; arrows). Deep cerebral veins (arrowhead) enhanced normally. (B) Axial T2 FLAIR image demonstrates expansile left thalamic T2 hyperintensity (arrow) and SSS thrombosis (arrowhead). (C) Subsequent postcontrast T1 image shows focal enhancement (arrow) within the thalamic lesion (arrowhead). (D) Diffusion-weighted imaging and (E) apparent diffusion coefficient demonstrate facilitated diffusion (yellow arrow), which did not help distinguish between venous congestion and glioma. (F) Axial T2 image demonstrates left vein of Trolard thrombosis (arrow).
Figure 2. Diffuse Midline Glioma Pathology.
(A) Hematoxylin & eosin section demonstrating a glial neoplasm with high cellularity and mitoses, consistent with malignant glioma. Immunohistochemistry was positive for (B) Olig2 and (C) H3 K27M, a mutation-specific immunohistochemical stain characteristically positive in diffuse midline glioma. (D) Immunohistochemistry for H3K27me3, assessing for native trimethylation at the K27 position, was lost in tumor cells but retained in entrapped normal brain cells, including endothelial cells. (E) Tissue was negative for IDH1 R132H mutation. (F) Ki-67 proliferation index was elevated. Bar = 50 μm.
Appendix. Authors
| Name | Location | Contribution |
| Braydon Dymm, MD | Department of Neurology, Duke University Hospital | Drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; study concept or design |
| Walter Wiggins, MD, PhD | Department of Radiology, Duke University Hospital | Drafting/revision of the manuscript for content, including medical writing for content; analysis or interpretation of data |
| Vanessa L. Smith, MD | Department of Pathology, Duke University Hospital | Analysis or interpretation of data |
| Nada El Husseini, MD | Department of Neurology, Duke University Hospital | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design |
| Swaroop Pawar, MD, MPH | Department of Neurology, Duke University Hospital | Drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data |
| Wuwei Feng, MD | Department of Neurology, Duke University Hospital | Drafting/revision of the manuscript for content, including medical writing for content |
Study Funding
The authors report no targeted funding.
Disclosure
The authors report no relevant disclosures. Go to Neurology.org/N for full disclosures.
References
- 1.Hawkins C, Pfister SM, Varlet P, et al. Diffuse midline glioma, H3 K27-altered. In: WHO Classification of Tumours Editorial Board (Ed). Central Nervous System Tumours. (WHO Classification of Tumours Series, 5th ed., Vol. 6). International Agency for Research on Cancer; 2021. Retrieved June 22, 2023, from tumourclassification.iarc.who.int/chapters/45 [Google Scholar]
- 2.Helmi A, Chan A, Towfighi S, et al. Incidence of dural venous sinus thrombosis in patients with glioblastoma and its implications. World Neurosurg. 2019;125:e189-e197. doi: 10.1016/j.wneu.2019.01.039 [DOI] [PubMed] [Google Scholar]