Melina Stark
Melina Stark, MSc
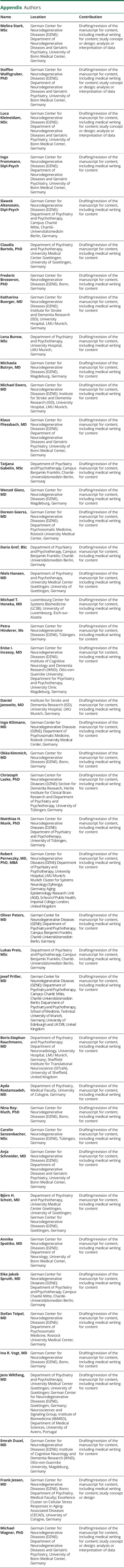
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,*,✉,
Steffen Wolfsgruber
Steffen Wolfsgruber, PhD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,*,
Luca Kleineidam
Luca Kleineidam, MSc
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Ingo Frommann
Ingo Frommann, Dipl-Psych
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Slawek Altenstein
Slawek Altenstein, Dipl-Psych
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Claudia Bartels
Claudia Bartels, PhD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Frederic Brosseron
Frederic Brosseron, PhD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Katharina Buerger
Katharina Buerger, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Lena Burow
Lena Burow, MSc
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Michaela Butryn
Michaela Butryn, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Michael Ewers
Michael Ewers, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Klaus Fliessbach
Klaus Fliessbach, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Tatjana Gabelin
Tatjana Gabelin, MSc
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Wenzel Glanz
Wenzel Glanz, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Doreen Goerss
Doreen Goerss, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Daria Gref
Daria Gref, BSc
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Niels Hansen
Niels Hansen, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Michael T Heneka
Michael T Heneka, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Petra Hinderer
Petra Hinderer, Ms
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Enise I Incesoy
Enise I Incesoy, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Daniel Janowitz
Daniel Janowitz, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Ingo Kilimann
Ingo Kilimann, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Okka Kimmich
Okka Kimmich, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Christoph Laske
Christoph Laske, PhD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Matthias H Munk
Matthias H Munk, PhD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Robert Perneczky
Robert Perneczky, MD, PhD, MBA
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Oliver Peters
Oliver Peters, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Lukas Preis
Lukas Preis, MSc
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Josef Priller
Josef Priller, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Boris-Stephan Rauchmann
Boris-Stephan Rauchmann, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Ayda Rostamzadeh
Ayda Rostamzadeh, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Nina Roy-Kluth
Nina Roy-Kluth, PhD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Carolin Sanzenbacher
Carolin Sanzenbacher, MSc
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Anja Schneider
Anja Schneider, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Björn H Schott
Björn H Schott, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Annika Spottke
Annika Spottke, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Eike Jakob Spruth
Eike Jakob Spruth, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Stefan Teipel
Stefan Teipel, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Ina R Vogt
Ina R Vogt, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Jens Wiltfang
Jens Wiltfang, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Emrah Duzel
Emrah Duzel, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Frank Jessen
Frank Jessen, MD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1,
Michael Wagner
Michael Wagner, PhD
1From the German Center for Neurodegenerative Diseases (DZNE) (M.S., S.W., L.K., I.F., F.B., K.F., O.K., N.R.-K., A. Schneider, A. Spottke, I.R.V., F.J., M.W.), Bonn; Department of Neurodegenerative Diseases and Geriatric Psychiatry (M.S., S.W., L.K., I.F., K.F., A. Schneider, M.W.), University of Bonn Medical Center, Germany; German Center for Neurodegenerative Diseases (DZNE) (S.A., O.P., J.P., E.J.S.), Berlin; Department of Psychiatry and Psychotherapy (S.A., J.P., E.J.S.), Campus Charité Mitte, Charité-Universitätsmedizin Berlin, Germany; Department of Psychiatry and Psychotherapy (C.B., N.H., B.H.S., J.W.), University Medical Center Goettingen, University of Goettingen, Germany; German Center for Neurodegenerative Diseases (DZNE) (K.B., M.E., R.P.), Munich; Institute for Stroke and Dementia Research (ISD) (K.B., M.E., D.J.), University Hospital, LMU Munich; Department of Psychiatry and Psychotherapy (L.B., R.P., B.-S.R.), University Hospital, LMU Munich, Germany; German Center for Neurodegenerative Diseases (DZNE) (M.B., W.G., E.I.I., E.D.), Magdeburg; Department of Psychiatry and Psychotherapy (T.G., D. Gref, O.P., L.P.), Campus Benjamin Franklin, Charité-Universitätsmedizin Berlin, Germany; German Center for Neurodegenerative Diseases (DZNE) (D. Goerss, I.K., S.T.), Rostock; Department of Psychosomatic Medicine (D. Goerss, I.K., S.T.), Rostock University Medical Center, Germany; Luxembourg Center for Systems Biomedicine (LCSB) (M.T.H.), University of Luxembourg, Esch-sur-Alzette; German Center for Neurodegenerative Diseases (DZNE) (P.H., C.L., M.H.M., C.S.), Tübingen; Institute for Cognitive Neurology and Dementia Research (IKND) (E.I.I., E.D.), Otto-von-Guericke University, Magdeburg, Germany; Department for Psychiatry and Psychotherapy (E.I.I.), University Clinic Magdeburg, Germany; Section for Dementia Research (C.L.), Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Germany; Department of Psychiatry and Psychotherapy (M.H.M.), University of Tübingen, Germany; Munich Cluster for Systems Neurology (SyNergy) (R.P.), Germany; Ageing Epidemiology Research Unit (AGE) (R.P.), School of Public Health, Imperial College London, United Kingdom; Department of Psychiatry and Psychotherapy (J.P.), School of Medicine, Technical University of Munich, Germany; University of Edinburgh and UK DRI (J.P.), United Kingdom; Department of Neuroradiology (B.-S.R.), University Hospital, LMU Munich, Germany; Sheffield Institute for Translational Neuroscience (SITraN) (B.-S.R.), University of Sheffield, United Kingdom; Department of Psychiatry (A.R., F.J.), Medical Faculty, University of Cologne, Germany; German Center for Neurodegenerative Diseases (DZNE) (B.H.S., J.W.), Goettingen; Department of Neurology (A. Spottke), University of Bonn Medical Center, Germany; Neurosciences and Signaling Group (J.W.), Institute of Biomedicine (iBiMED), Department of Medical Sciences, University of Aveiro, Portugal; and Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD) (F.J.), University of Cologne, Germany.
1