Abstract
A 68-year-old woman with a history of diabetes mellitus type 2, depression, and migraines presented with painless, acute, consecutive vision loss affecting the right eye for 1 week and the left eye for 2 weeks. Neuro-ophthalmic examination was notable for visual acuities of finger-counting peripherally, a central scotoma, anterior uveitis, vitritis, and placoid macular pigmentary changes in each eye (OU). Proprioception was diminished in the bilateral lower extremities. Optical coherence tomography (OCT) revealed hyper-reflectivity and attenuation of the outer retina OU with normal inner retinal architecture and reflectivity. Fluorescein angiography (FA) demonstrated normal filling of the central retinal arteries with patchy choroidal perfusion in the right eye and targetoid punctate foci of leakage in the macula OU. Before the recognition of intraocular inflammation and findings on OCT and FA, the patient was treated for presumed central retinal artery occlusion at an outside hospital. Additional diagnostic testing at our institution revealed an alternate diagnosis. This case highlights a rare presentation of a well-known disease entity and underscores the importance of avoiding diagnostic anchoring in clinical practice.
Section 1
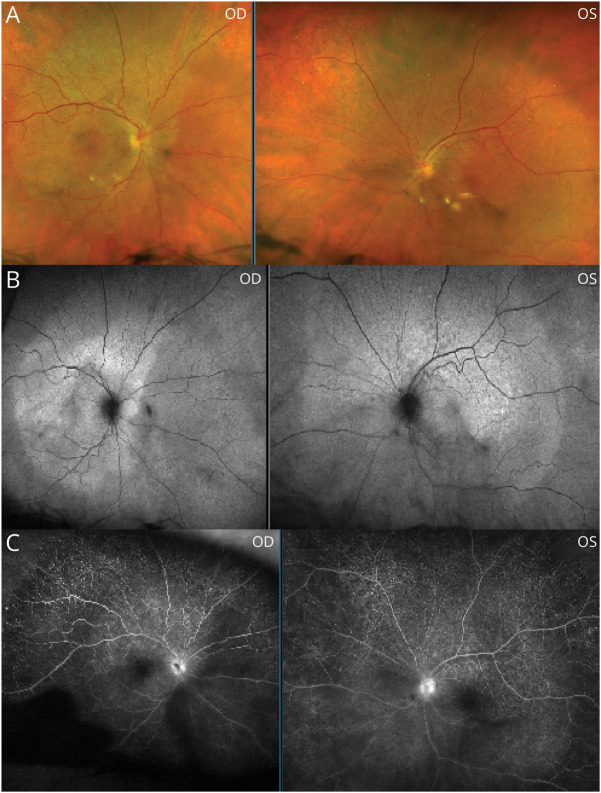
A 68-year-old woman with a history of diabetes mellitus type 2, depression, and migraines presented with painless, consecutive vision loss. She reported progressive monocular vision loss affecting the left eye 2 weeks before presentation to our institution. Giant cell arteritis was suspected because of an elevated erythrocyte sedimentation rate of 72 mm/h. Treatment included high-dose steroids, aspirin, and cilostazol. Biopsy of the left temporal artery was negative. MRI brain and CT angiogram of the head and neck were normal. One week later, while tapering prednisone, she awoke with severe central vision loss in her right eye. Examination revealed visual acuities of finger-counting in the periphery of both eyes (OU), with hand movement perceived centrally OU. Pupils reacted sluggishly to light bilaterally without evidence of a relative afferent pupillary defect. Light yellow macular placoid lesions were noted on the funduscopic examination OU (Figure 1A) with sharply delineated pigmentary changes on fundus autofluorescence OU (Figure 1B). The neurologic examination was relevant for decreased proprioception in the halluces bilaterally and absent Achilles and patellar reflexes bilaterally. Initial ophthalmic examination revealed retinal changes believed to be consistent with bilateral central retinal artery occlusion (CRAO). She subsequently developed right-sided hearing loss during admission.
Figure 1. Fundus Photography, Fundus Autofluorescence, and Fluorescein Angiography.
Placoid-like macular pigmentary changes are depicted on fundus photography (A) and fundus autofluorescence (B); the sharply delineated margin of the pigmentary change (indicative of the pathologically affected area) is seen. Note also patchy choroidal filling and disc leakage noted on fluorescein angiography (C). OD = right eye; OS = left eye.
Questions for Consideration:
What is the differential diagnosis?
What additional testing should be performed?
GO TO SECTION 2
Section 2
Ischemic, infectious, and autoimmune etiologies should be considered in the differential diagnosis for cases of rapidly consecutive vision loss associated with an abnormal retinal appearance. Ischemic etiologies can involve emboli causing central or branch retinal artery occlusions or vasculitides, such as giant cell arteritis (commonly) or Susac syndrome (rarely). A wide range of infectious etiologies should be considered, particularly in immunocompromised patients, including the family of herpesviruses, syphilis, tuberculosis, cytomegalovirus, toxoplasmosis, and Bartonella, among others. Systemic lupus erythematosus, Behcet disease, and sarcoid are relevant rheumatologic considerations.
Ophthalmologic evaluation can be critical in making the diagnosis. In particular, a slitlamp examination, fluorescein angiography (FA), and optical coherence tomography (OCT) frequently yield valuable information that is not ascertainable on the funduscopic examination, as described below. Identifying the pattern of abnormalities observed with these tests is crucial in conducting a comprehensive yet efficient workup. In cases of retinal artery occlusion, searching for an embolic source is required and MRI of the brain is valuable in determining whether cerebral ischemia is present and, if so, which vascular distributions are affected. MRI brain and audiometry are important when FA is suggestive of Susac syndrome. The presence of intraocular inflammation or retinal vasculitis merits a serologic investigation for the infectious and immune entities above, and in patients with coexisting neurologic deficits, lumbar puncture is a helpful adjunct.
A slitlamp examination can identify intraocular inflammation, which cannot be visualized on routine bedside fundoscopy. FA visualizes dye transit through the retinal vasculature and choroidal circulation, allowing for the differentiation between vaso-occlusive processes of either circulation or retinal vasculitis. OCT allows for visualization of the retinal layers and can help to distinguish processes such as central or branch retinal artery occlusions, which cause ischemia to only the inner two-third of the retina, from inflammatory or immune processes which can cause full-thickness retinitis or outer retinal processes which could not be easily differentiated from one another based on funduscopic examination alone.
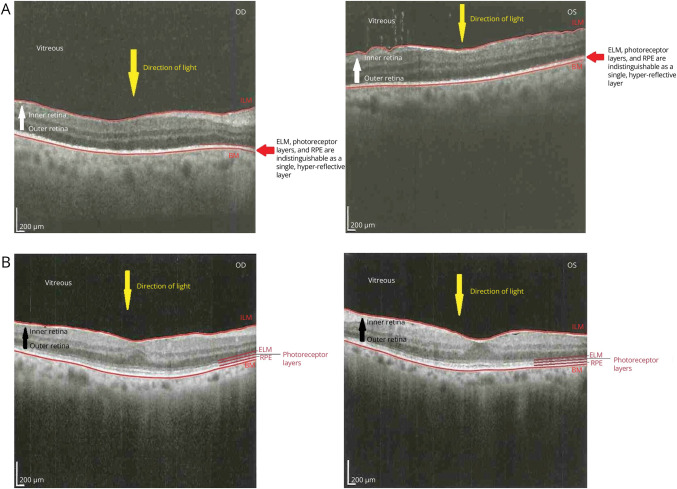
In our patient's case, retinal changes were accompanied by inflammation of the anterior chamber and the vitreous humor OU, suggesting an infectious or immune etiology rather than a retinal artery occlusion. FA demonstrated patchy choroidal perfusion in the right eye, with targetoid hyperfluorescent punctate foci in both macula (Figure 1C). OCT demonstrated loss of the outer retinal layers, inconsistent with the earlier working diagnosis of bilateral CRAO (Figure 2A).
Figure 2. OCT Before Treatment and 14 Months Post-treatment.
This OCT (A) before treatment with intravenous penicillin demonstrates loss of the delineation of the outer retinal layers—the ELM, photoreceptor layers, and RPE layers—which can be visually differentiated from one another in the healthy eye—and are here supplanted by a single, hyper-reflective layer. These changes correlate with loss of the retina peripheral to the ellipsoid zone on OCT, specifically including the RPE and photoreceptor layers. This OCT (B) from 14 months post-treatment with intravenous penicillin now demonstrates visible delineation between the outer retinal layers, including the ELM, the photoreceptor layers, and the RPE. BM = Bruch membrane; ELM = external limiting membrane; ILM = internal limiting membrane; OCT = optical coherence tomography; RPE = retinal pigment epithelium.
Questions for Consideration:
Which diagnosis best unifies rapidly consecutive vision loss with retinal pigmentary changes, hearing loss, and proprioceptive deficits?
What confirmatory testing should be pursued?
GO TO SECTION 3
Section 3
Syphilis was the highest diagnosis on our differential based on the macular placoid lesions on fundoscopic examination, the patchy choroidal filling on FA, the loss of the outer retinal layers on OCT, hearing loss, and decreased proprioception in the halluces bilaterally suggestive of tabes dorsalis. Lumbar puncture was significant for 16 nucleated cells (33% polymorphonuclear leukocytes and 37% lymphocytes), 14 red blood cells, protein of 65 mg/dL, and glucose of 98 mg/dL. CSF venereal disease research laboratory (VDRL), serum treponemal antibodies, and serum rapid plasma reagin (RPR) were positive (the latter at a titer of 1:512), confirming a diagnosis of syphilis. The patient completed a 14-day course of 4 million units of intravenous penicillin G every 4 hours (24 million units daily). Repeat ophthalmic examination at 14 months post-treatment was significant for normal visual acuities (20/20) bilaterally and well-defined outer retinal layers on OCT (Figure 2B). She continued to have superonasal visual field loss in her right eye.
Discussion
This patient's presentation was in keeping with neurosyphilis, ocular syphilis, and otosyphilis.1 Neurosyphilis may manifest with meningitis, classically 1–2 years after infection, or with a dorsal root ganglionopathy with secondary changes seen in the dorsal columns due to axonal degeneration (i.e., tabes dorsalis).1 Ocular syphilis may present in a number of different ways, including with anterior uveitis, intermediate uveitis, posterior uveitis, panuveitis, keratitis, vasculitis, optic neuritis, or, as was the case here, with acute posterior placoid chorioretinitis presenting clinically as painless, acute, consecutive vision loss, which is a rare but classic manifestation of ocular syphilis.2 The placoid appearance of the macula seen in ocular syphilis occurs as a result of damage to the retinal pigment epithelium (RPE). In its early stages, the pigmentary changes may be subtle and can cause clinical confusion. The natural autofluorescence of healthy RPE cells makes fundus autofluorescence a sensitive means by which this finding can be detected earlier in the disease. Owing to direct damage and loss of support cells, the outer retina's function is impaired; the structural correlate to this can be seen on OCT (Figure 2A) wherein the inner retina's architecture is preserved—in stark contrast to the complete obscuration of the typically distinct external limiting membrane, photoreceptor layers, and RPE layers. Vision loss is secondary to this dysfunction of the outer retina. Ocular syphilis can occur at any stage of syphilis infection, and suspected cases require collaboration with ophthalmology or neuro-ophthalmology.1
In a patient with an unknown syphilis history, evaluation for current or previous treponemal infection should be obtained with serum nontreponemal (VDRL and RPR) and treponemal (fluorescent treponemal antibody absorption) testing. Testing only with nontreponemal assays is not recommended because titers may spontaneously wane or may be undetectable in the setting of very high titers. In those with known syphilis history and/or symptoms, such as in our patient, lumbar puncture is recommended.1 Diagnosis in this case was confirmed with the combination of macular placoid lesions on fundoscopic examination, patchy choroidal filling on FA, loss of the outer retinal layers on OCT, and positive VDRL in the CSF. Treatment of all forms of syphilis is with parenteral penicillin, which this patient received.1 The prognosis of ocular syphilis is excellent after treatment, with over 90% of patients having a final visual acuity of 20/40 or better.3
Appendix. Authors
| Name | Location | Contribution |
| Joseph Ditrapani, MD, MPH | Department of Neurology, Beth Israel Deaconess Medical Center, Boston, MA | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design |
| Hayley Price, MD | Department of Neurology, Beth Israel Deaconess Medical Center, Boston, MA | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design |
| Christine Shrock, MD | Department of Neurology, Boston Children's Hospital, MA | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design |
| Shuodan Zhang, MD | Department of Neurology, Beth Israel Deaconess Medical Center, Boston, MA | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design |
| Patricia E. Greenstein, MBBCh | Department of Neurology, Beth Israel Deaconess Medical Center, Boston, MA | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design |
| Marc Bouffard, MD | Department of Neurology, Beth Israel Deaconess Medical Center, Boston, MA | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design |
Study Funding
No targeted funding reported.
Disclosure
The authors report no relevant disclosures. Go to Neurology.org/N for full disclosures.
References
- 1.Ghanem KG, Ram S, Rice P. The modern epidemic of syphilis. N Engl J Med. 2020;382(9):845-854. doi: 10.1056/NEJMra1901593 [DOI] [PubMed] [Google Scholar]
- 2.Furtado JM, Arantes TE, Nascimento H, et al. Clinical manifestations and ophthalmic outcomes of ocular syphilis at a time of re-emergence of the systemic infection. Sci Rep. 2018;8(1):12071. doi: 10.1038/s41598-018-30559-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mathew R, Goh B, Westcott M. British Ocular Syphilis Study (BOSS): 2-year national surveillance study of intraocular inflammation secondary to ocular syphilis. Invest Opthalmol Vis Sci. 2014;55(8):5394. doi: 10.1167/iovs.14-14559 [DOI] [PubMed] [Google Scholar]