Abstract
Background:
The results of a recent pilot study suggest that steerable ureteroscopic renal evacuation (SURE) is safe and more effective in stone removal than basketing following laser lithotripsy. The objective of this retrospective study was to further assess the safety and efficacy of SURE using the CVAC® Aspiration System (Calyxo, Inc., Pleasanton, CA) in patients with large stone burdens.
Materials and Methods:
Patients with a baseline stone burden of ≥10 mm who underwent SURE were identified. Subject demographics, secondary procedures, complications, and stone clearance (defined as percent baseline volume reduction) were evaluated. Subanalyses were performed to explore patients identified as high risk for percutaneous nephrolithotomy (PCNL) because (1) they were on anticoagulation or antiplatelet therapy at the time of procedure or (2) they had limited mobility due to neurologic conditions.
Results:
Identified patients (N = 43) had a mean preoperative stone burden of 29 ± 12 mm and mean stone volume of 3092 ± 5002 mm3. Approximately one-half of patients (n = 24, 55.8%) had CT imaging at follow-up, and of those, 8 (33.3%) had no residual stones, 22 (91.7%) had >90% stone clearance, 23 (95.8%) had >80% stone clearance, and 24 (100%) had >60% stone clearance. Stone clearance based on baseline stone burden varied between 93.8% and 98.9%. At baseline, 21 patients were anticipated to require staged ureteroscopy; however, only two of those (9.5%) needed secondary procedures. High-risk patients (n = 22) were on anticoagulation or antiplatelet therapy (n = 12) or had neurologic conditions (n = 10). Stone clearance was 97% among patients in the anticoagulated cohort with postoperative CT imaging and 83% in the neurologic condition cohort. There were no device-related complications and no postoperative admissions.
Conclusions:
The CVAC Aspiration System is safe and effective for treating large stone burdens, including in high-risk patients, and may decrease the need for PCNL or secondary procedures.
ClinicalTrials.gov Identifier:NCT04519294.
Keywords: steerable ureteroscopic renal evacuation (SURE), CVAC Aspiration System, large stone burden, high-risk patients, retrospective study, vacuum, aspiration
Introduction
Ureteroscopy with laser lithotripsy is one of the most frequently performed operating room procedures worldwide and has seen improved technologies in many areas of the procedure, including single-use ureteroscopes and high-powered lasers.1–3 Nevertheless, stone-free rates (SFRs) remain at 55%–60%, and the rates decline with increasing renal calculi size.3
The recommended treatment for large renal calculi, particularly those >20 mm, is percutaneous nephrolithotomy (PCNL)4; however, not all patients are candidates for PCNL and, if ureteroscopy is performed, many require more than one.5 In addition, patients with complex anatomy make PCNL technically challenging and increase the likelihood of unfavorable outcomes.6,7 While ureteroscopy is frequently offered to these patients, technological advances are needed to improve outcomes for this patient population.
Steerable Ureteroscopic Renal Evacuation (SURE) is a new, minimally invasive treatment for urolithiasis8 that may be an effective option for patients with large stone burdens who are unwilling or unable to undergo PCNL. SURE entails ureteroscopic stone removal using the CVAC® Aspiration System (CVAC; Calyxo, Inc.), a novel steerable catheter system with dedicated irrigation and vacuum lumens. Following laser lithotripsy, the flexible ureteroscope is removed, and CVAC is introduced into the kidney over a guidewire through a 12/14F ureteral access sheath using fluoroscopic guidance. CVAC navigates the renal collecting system using fluoroscopy, and when suction is applied, small stone fragments as much as 2.5 mm can be aspirated through the 7.5F inner vacuum lumen. Stone fragments are collected in a stone collection container attached to the patient for visual confirmation of stone removal. After the device is removed from the kidney, the ureteroscope is reintroduced into the kidney to assess the extent of stone removal (Figs. 1 and 2). CVAC has previously been demonstrated to be safe and feasible in patients with stone burdens <15 mm.8 We hypothesized that SURE would be effective in patients with larger stone burdens, including those deemed to be at high risk for PCNL.
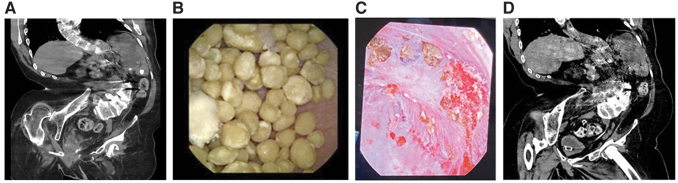
FIG. 1.
Forty-two-year-old male with spina bifida and lower pole stone burden. (A) Preoperative CT. (B) Lower pole calix before and after. (C) CVAC® stone aspiration. (D) Postoperative CT with no residual stone.
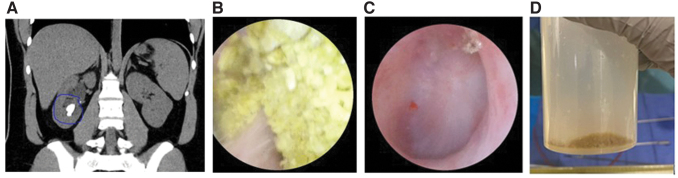
FIG. 2.
Twenty-four-year-old female with persistent right lower pole stone after SWL. (A) Preoperative CT. (B) Intraoperative findings in lower pole. (C) Lower pole after CVAC stone aspiration. (D) Evacuated stone fragments in collection cup. SWL = extracorporeal shockwave lithotripsy.
Materials and Methods
This was a retrospective study performed at two large tertiary care centers. Data from all consecutive patients who had undergone SURE with CVAC for stone burdens ≥10 mm were reviewed. Institutional Review Board approval was obtained from both centers for data accrual. All procedures were performed by two endourology fellowship-trained surgeons. Obtained data included subject gender, body mass index, comorbidities, preoperative symptoms, stone procedural history, concurrent medications, procedural details, post-op complications, plus pre- and postoperative imaging.
Due to the retrospective nature of the study, the postoperative imaging modality was chosen at surgeon discretion. Stone free was defined as zero residual fragments across all postoperative imaging. Pre- and postoperative stone volumes were calculated in patients for whom CT imaging was available. CT cuts at one institution were 0.625 mm and the other 2- or 2.5-mm. Stone clearance, the percent baseline stone volume reduction, was calculated from CT-measured volumes using the ellipsoid formula. A stone clearance stratification analysis was performed for stone burdens 10–20 mm, 20–30 mm, and >30 mm. The Journal of Endourology recently recommended an assessment of stone clearance, along with a new standard for reporting SFR through CT ranging from Grade A (zero fragments) to Grade C (stones 2.1–4 mm).
A large cohort was preoperatively planned for staged ureteroscopy and was assessed for secondary intervention. Subanalyses were performed in two high-risk groups, (1) patients on anticoagulation or antiplatelet therapy at the time of surgery, and (2) patients with limited mobility secondary to neurologic disorders (i.e., spina bifida, cerebral palsy, muscular dystrophy, quadriplegia).
Statistical analyses
Categorical variables were summarized using relative frequencies and percentages. Continuous variables were summarized using mean ± standard deviation, median, and minimum and maximum. All statistical analyses were performed using Stata, Version 17.0 (StataCorp LLS; College Station, TX).
Results
A total of 43 patients underwent SURE for stone burdens ≥10 mm between 2021 and 2022 (Table 1). Mean preoperative stone burden was 29 ± 12 mm, and mean stone volume was 3092 ± 5002 mm3. Approximately half of patients (n = 22, 51.2%) were determined to be high risk due to active anticoagulation therapy or antiplatelet therapy at the time of surgery (n = 12) or limited mobility secondary to neurologic conditions (n = 10).
Table 1.
Characteristics of Patients (N = 43)
| Characteristic | Mean ± SD |
|---|---|
| Mean age ± SD | 58.4 ± 16.4 |
| Gender, n (%) | |
| Male | 22 (51.2) |
| Female | 21 (48.8) |
| Mean BMI ± SD | 32.0 ± 8.6 |
| Single stone, n (%) | 25 (58.1) |
| Lower pole stone, n (%) | 21 (48.8) |
| Prestented, n (%) | 24 (55.8) |
| Staged URS anticipated preprocedure, n (%) | 21 (48.8) |
| Kidney stone procedure within past 12 months, n (%) | 26 (60.5) |
| Anticoagulated, n (%) | 12 (27.9) |
| Neurologic condition, n (%) | 10 (23.3) |
| Total mean baseline stone burden (mm) ± SD | 29.3 ± 12.3 |
| Total mean baseline stone volume (mm3) ± SD | 3092.1 ± 5002.1 |
BMI = body mass index; SD = standard deviation; URS = ureteroscopy.
SFR, including all imaging modalities (KUB, ultrasound, and CT), was 39.5% (17 of 43 patients). Twenty-four patients had CT imaging at follow-up, and the mean SFR on CT was 33% (Grade A), SFR with stones ≤2 mm was 37.5% (Grade B), and SFR with stones 2.1–4 mm was 45.8% (Grade C). The average stone clearance was 96.1%; 22 (91.7%) had >90% stone clearance, 23 (95.8%) had >80% stone clearance, and 24 patients (100%) had >60% stone clearance (Table 2). Eight patients (33.3%) had no residual fragments. Stone clearance based on baseline stone burden varied between 93.8% and 98.9% (Table 3). For total stone burden 10–20 mm, 97.9% stone clearance was achieved. For baseline stone burdens 20–30 mm, stone clearance was 98.9%, and for baseline stone burden >30 mm, stone clearance was 93.8%.
Table 2.
Stone Clearance Threshold Analysis Among Patients with Follow-Up Computed Tomography Imaging (n = 24)
| Stone clearance threshold | Patients, n (%) | Mean volume of stone removed, mm3 ± SD |
|---|---|---|
| 100% (stone free) | 8 (33.3) | 2266.8 ± 1893.8 |
| >90% | 22 (91.7) | 2588.5 ± 1930.0 |
| >80% | 23 (95.8) | 2593.1 ± 1885.8 |
| >60% | 24 (100.0) | 2513.9 ± 1884.7 |
Table 3.
Stone Clearance
| Total baseline Stone burden 10–20 mm (n = 6) | Total baseline stone burden 20–30 mm (n = 6) | Total baseline Stone burden >30 mm (n = 12) | All patients with follow-up CT imaging (n = 24) | |
|---|---|---|---|---|
| Stone clearance, % (mean ± SD) | 97.9 ± 3.0 | 98.9 ± 2.5 | 93.8 ± 11.5 | 96.1 ± 8.5 |
| Volume removed, mm3 (mean ± SD) | 945.9 ± 559.3 | 2345.1 ± 1280.8 | 3382.3 ± 2088.1 | 2513.9 ± 1884.7 |
Baseline stone burden stratification analysis among patients with follow-up CT imaging (n = 24).
Staged ureteroscopy was anticipated for 21 of the 48 patients (48.8%) and 19 of those patients were effectively treated in a single procedure, thereby avoiding the predicted second procedure (Table 4). Two patients with staghorn kidney stones required the anticipated second ureteroscopy.
Table 4.
Reduction in Planned Secondary (Staged) Procedures
| Stone free, n = 7 | Not stone free, n = 14 | Overall, n = 21 | |
|---|---|---|---|
| Stone free, n/N, (%) | 7/7 (100.0) (7/7) | 0/14 (0.0) | 7/21 (33.3) |
| Patients with CT imaging, n/N, (%) | 5/7 (71.4) | 9/13 (69.2) | 14/20 (70.0) |
| Total baseline stone volume, mm3 (mean ± SD) | 2858.6 ± 2136.1 | 2387.9 ± 1409.5 | 2556.0 ± 1637.5 |
| Total volume of stone removed, mm3 (mean ± SD) | 2858.6 ± 2136.1 | 2212.1 ± 1356.8 | 2443.0 ± 1624.8 |
| Mean stone clearance, % (mean ± SD) | 100.0 ± 0.0 | 91.3 ± 12.6 | 94.4 ± 10.8 |
| Second procedure performed as planned, n/N, (%) | 0/7 (0.0) | 2/14 (14.3) | 2/21 (9.5) |
| Second procedure avoided, n/N, (%) | 7/7 (100) | 12/14 (85.7) | 19/21 (90.5) |
n = number; N = total number.
Six of 43 patients (14.0%) had a secondary surgical intervention (Table 5). The baseline stone burden for these patients was 36.3 ± 10.7 mm. Four patients (9.3%) required a second ureteroscopy (two planned staged ureteroscopies and two unplanned ureteroscopies), and 2 (4.7%) required a stent placement (one for Steinstrasse and one to replace premature stent removal on postoperative day 3).
Table 5.
Outcomes for Patients with Secondary Surgical Interventions (n = 6, 14%)
| Patients (n = 6) | |
|---|---|
| Mean baseline linear stone burden, mm ± SD | 36.3 ± 10.7 |
| Mean baseline stone volume, mm3 ± SD | 7121.1 ± 9424.0 |
| Mean total volume removed (CT) (n = 5) | 3135.1 ± 870.3 |
| Mean percent of stone removed (CT) (n = 5) | 95.5 ± 7.5 |
| Type of surgical intervention, n/N, (%) | |
| Planned second (staged) ureteroscopy | 2/6 (33.3) |
| Unplanned second ureteroscopy | 2/6 (33.3) |
| Secondary stent placementa | 2/6 (33.3) |
All subjected received postoperative stents. One secondary stent placement was due to Steinstrasse.
The secondary analysis on higher risk populations indicated that anticoagulation and antiplatelet therapy had no impact on outcomes (97.4% ± 2.7% stone clearance) although less stone was removed in patients with neurologic conditions (83.4% ± 19.4% stone clearance) (Table 6). Secondary interventions were not required in any subject in these higher risk cohorts.
Table 6.
Analysis of Patients on Anticoagulation Therapy and Subject with Neurologic Conditions
| Anticoagulation n = 12 | Neurologic condition n = 10 | All patients n = 43 | |
|---|---|---|---|
| Mean baseline linear stone burden, mm ± SD | 27.0 ± 8.8 | 29.6 ± 8.6 | 29.3 ± 12.3 |
| Mean baseline volumetric stone burden, mm3 ± SD | 2129 ± 2329 | 3339.8 ± 6499.5 | 3092.1 ± 5002.1 |
| Patients with CT imaging, n/N (%) | 6/12 (50) | 3/10 (30) | 24/43 (56) |
| Mean total volume of stone removed, mm3 ± SD | 3025 ± 2918 | 1928 ± 2408 | 2513.9 ± 1884.7 |
| Mean stone clearance, % ± SD | 97.4 ± 2.7 | 83.4 ± 19.4 | 96.1 ± 8.5 |
There were no complications secondary to use of the CVAC System. Two ureteral injuries related to access sheath placement were reported (Clavien-Dindo Grade II). One high-risk subject with neurologic condition was admitted postoperatively for a urinary tract infection.
Discussion
In this study we found that SURE is safe and effective for patients with large renal stones, including high-risk patients who are often poor candidates for PCNL. The study builds on prior work by Sur and colleagues in confirming the safety of SURE and its effectiveness in achieving a high stone clearance.8 We focused on volumetric analysis of baseline and residual stone using CT to assess stone clearance, which we believe to be a more precise and patient-centric outcome measurement. We are encouraged by the reduction in the frequency of staged procedures in this cohort, and more research is warranted in this area.
Of particular interest to us was the safety and effectiveness of SURE in large stone burden patients who are at higher risk for PCNL. Patients with spinal deformities undergoing PCNL have a 40% complication rate, including 10% Clavien-Dindo Grade 3 or higher, and 20% transfusion rate.6,9 In this study, no transfusions or re-admittances were required for the patients on active anticoagulation/antiplatelet treatment. There were no transfusions or complications among patients with neurologic conditions limiting mobility or altered anatomy. These data suggest that there may be a meaningful safety benefit to SURE vs standard ureteroscopy or PCNL in these cohorts.
This study demonstrated high stone clearance and highlights the importance of a variable outcome measure as an alternative to or in combination with the binary stone-free metric. Achieving a stone-free outcome through CT is challenging, especially for the patients with large renal stones; the SFR with zero fragments using CT was 33% in our study. Meanwhile, the average stone clearance following a single SURE procedure was high at 96.1%, especially given the large stone burden and complexity of these patients. The high stone clearance of SURE was also consistent across all baseline burdens, which is in contrast to the review by Rippel and associates that showed strong association of pretreatment stone size with residual fragments at a rate of 24%, 40%, and 58% for stones ≤5 mm, 6–10 mm, and >10 mm, respectively (p < 0.001).10 The Journal of Endourology recently recommended an assessment of stone clearance, along with a new standard for reporting SFR using CT ranging from Grade A (zero fragments) to Grade C (stones 2.14 mm). In our study, SFRs increased from Grade A of 33.3% to Grade B of 37.5% and Grade C of 45.8%. Given this variability, we believe that stone clearance may be a more meaningful way to compare the outcome of different approaches.
Achieving high stone clearance with SURE may lead to a reduction in staged procedures for large stone burden patients. In this study cohort with baseline stone burdens from 17 mm to 64 mm, only four patients (10%) required secondary ureteroscopy intervention, a rate of 1.1 procedures per patient. In comparison, a meta-analysis by Aboumarzouk and coworkers reported an average 1.6 procedures per patient for stone burdens >20 mm.11 This suggests a 31% reduction in secondary interventions which would offer significant health care savings while minimizing patient risk and reducing OR workload. If SURE can reduce the need for PCNL and staged ureteroscopy in this high-risk population, a broader patient cohort may also benefit with enhanced procedural ease.
Several limitations must be acknowledged. This was a retrospective analysis with no control arm. As this study included patients who were treated under standard clinical practice, postoperative CT imaging was not routinely performed across the entire cohort. Consequently, calculations related to SFR and stone clearance were limited to patients where postoperative CT was performed. There is potential bias in the criteria for secondary intervention, but two experienced endourologists determined 49% secondary intervention rate in this cohort, and historical control provides additional support.11 In addition, CT criteria and timing were not standardized between the sites. Finally, stone volume calculations were performed utilizing an ellipsoid formula rather than three-dimensional reconstruction from CT scans, and future studies with three-dimensional CT analysis, with standardized CT protocol, are recommended.
Taken together, SURE with the CVAC Aspiration System appears to represent a safe and effective alternative in patients with large stone burdens, even with complex neurologic conditions or active anticoagulation/antiplatelet therapy. With SURE, consistently high stone clearance regardless of the baseline stone burden can be achieved, and as a result, these patients may be more likely to avoid a secondary ureteroscopy or PCNL. More studies are needed to understand the effectiveness of SURE compared to other modalities in larger patient cohorts. A large, prospective, randomized multicenter clinical trial comparing SURE with CVAC to standard ureteroscopy (basketing) in candidates for ureteroscopy with laser lithotripsy is under way.12
Conclusions
SURE using the CVAC Aspiration System is a safe and effective procedure for large stone burdens, including anticoagulated patients and patients with neurologic conditions. The procedure significantly reduces stone volume, independent of baseline stone burden, and can reduce the frequency of secondary procedures. Further research is underway to establish the applicability of SURE in a broader patient population.
Acknowledgment
The authors acknowledge the editorial assistance of Dr. Carl S. Hornfeldt, Apothekon, Inc., during the preparation of this article.
Abbreviations Used
- BMI
body mass index
- CT
computed tomography
- n
number
- N
total number
- PCNL
percutaneous nephrolithotomy
- SD
standard deviation
- SFR
stone-free rate
- SURE
Steerable Ureteroscopic Renal Evacuation
- SWL
extracorporeal shockwave lithotripsy
- UAS
ureteral access sheath
- URS
ureteroscopy
Authors' Contributions
K.L.S. and J.S.W. contributed to the conceptualization and design of the study, collected and analyzed the data. K.L.S. contributed to the writing of the article, and J.S.W. contributed to the editing. B.J.B. contributed to the data collection and writing of the article. All authors approved the final article in its existing form.
Author Disclosure Statement
No competing financial interests exist. Both K.L.S. and J.S.W. are trial investigators and consultants for Calyxo, Inc., but were not compensated for this submitted work.
Funding Information
The statistical analysis was sponsored by Calyxo, Inc., Pleasanton, CA.
References
- 1. Ghani KR, Sammon JD, Karakiewicz PI, et al. Trends in surgery for upper urinary tract calculi in the USA using the Nationwide Inpatient Sample: 1999-2009. BJU Int 2013;112:224–230. [DOI] [PubMed] [Google Scholar]
- 2. Johnson DB, Pearle MS. Complications of ureteroscopy. Urol Clin North Am 2004;31:157–171. [DOI] [PubMed] [Google Scholar]
- 3. Ghani KR, Wolf JS Jr. What is the stone-free rate following flexible ureteroscopy for kidney stones? Nat Rev Urol 2015;12:281–288; doi: 210.1111/bju.12059 [DOI] [PubMed] [Google Scholar]
- 4. Assimos D, Krambeck A, Miller NL, et al. Surgical management of stones: American Urological Association/Endourological Society Guideline, Part I. J Urol 2016;196:1153–1160. [DOI] [PubMed] [Google Scholar]
- 5. Bonkat G, Bartoletti R, Bruyère F, et al. Urological Infections. European Association of Urology. 2022. Available from: https://d56bochluxqnzcloudfrontnet/documents/full-guideline/EAU-Guidelines-on-Urological-Infections-2022pdf [Last accessed: April 7, 2023].
- 6. Goumas-Kartalas I, Montanari E. Percutaneous nephrolithotomy in patients with spinal deformities. J Endourol 2010;24:1081–1089. [DOI] [PubMed] [Google Scholar]
- 7. Mosavi-Bahar SH, Amirzargar MA, Rahnavardi M, et al. Percutaneous nephrolithotomy in patients with kidney malformations. J Endourol 2007;21:520–524. [DOI] [PubMed] [Google Scholar]
- 8. Sur RL, Agrawal S, Eisner BH, et al. Initial safety and feasibility of steerable ureteroscopic renal evacuation: A novel approach for the treatment of urolithiasis. J Endourol 2022;36:1161–1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Morgan M, Smith N, Thomas K, et al. Is Clavien the new standard for reporting urological complications? BJU Int 2009;104:434–436. [DOI] [PubMed] [Google Scholar]
- 10. Rippel CA, Nikkel L, Lin YK, et al. Residual fragments following ureteroscopic lithotripsy: Incidence and predictors on postoperative computerized tomography. J Urol 2012;188:2246–2251. [DOI] [PubMed] [Google Scholar]
- 11. Aboumarzouk OM, Monga M, Kata SG, et al. Flexible ureteroscopy and laser lithotripsy for stones >2 cm: A systematic review and meta-analysis. J Endourol 2012;26:1257–1263. [DOI] [PubMed] [Google Scholar]
- 12. US National Library of Medicine. ClinicalTrials.gov. Comparison of Laser Lithotripsy With and Without Steerable Ureteroscopic Renal Evacuation (SURE). Available from: https://clinicaltrials.gov/ct2/show/NCT04519294 [Last accessed: April 12, 2023].