Abstract
While adverse local tissue reactions are well described in the total hip arthroplasty literature, there have only been case reports and case series in the total knee arthroplasty literature. There have been no cases described in the setting of a distal femoral replacement. In this case, we describe a 69-year-old female with a complex history of left knee revision arthroplasty with a distal femoral and proximal tibial replacement who presented with left knee pain and was found to have extensive adverse local tissue reaction with corrosion at the femoral stem-extension piece junction and the extension piece-distal femoral component junction. The femoral taper was then manually cleaned and modular components replaced. Corrosion at the stem-distal femoral component junction can result in adverse local tissue reaction in patients with distal femoral replacements. It is important to consider this diagnosis when evaluating patients with knee pain following distal femoral replacement.
Keywords: Adverse local tissue reaction, Metallosis, Distal femoral replacement
Introduction
Adverse local tissue reactions (ALTRs) have been well documented in the total hip arthroplasty (THA) literature [[1], [2], [3], [4], [5], [6]]. Conversely, ALTR in total knee arthroplasty (TKA) has been less commonly described, primarily in case reports and case series [[7], [8], [9]]. The large majority of ALTR cases in the primary TKA setting are secondary to metal-backed patellar components, polyethylene failures, or implant failures [7]. Corrosion at the modular taper junction of revision TKA components has been described in retrieval analyses, but ALTR as a result of this is a rare occurrence [[8], [9], [10], [11], [12]]. This is a case report of ALTR occurring secondary to taper corrosion in a modular, segmental distal femoral replacement (DFR) performed in the revision TKA setting. To our knowledge, this is the first report of ALTR due to taper corrosion of a DFR.
Case history
A 69-year-old female previously underwent left distal femur curettage and bone grafting for a reportedly benign tumor in 1974. This was followed by a left primary TKA in 1982, which was revised multiple times for aseptic loosening (2005 revision TKA, 2018 revision to DFR, 2019 revision to proximal tibia replacement). The implants upon presentation were the Stryker Global Modular Replacement System (GMRS, Stryker, Mahwah, NJ). All components were made of cobalt-chromium (CoCr) alloy except for the femoral stem, which was titanium alloy (Ti).
The patient presented to the senior author’s office as a new patient for evaluation of multiple months of persistent left knee swelling and pain. Her past medical history included hematuria, anemia, and obesity. Examination of the left knee revealed a well-healed midline incision. There was a moderate effusion with an area of fluctuance over the medial proximal tibia, which was tender to palpation. Range of motion testing revealed a 45-degree extensor lag, which the patient reported had been present prior to her index TKA. Limb alignment radiographs are shown in Figure 1. Left knee anterior posterior and lateral radiographs from 1 year prior to presentation (Fig. 2a and b) were also compared to those obtained at the presentation to the senior author’s office (Fig. 2c and d).
Figure 1.
Limb length x-rays upon presentation to office demonstrating prior distal femoral and proximal tibial replacements with osteolysis. The proximal press-fit femoral stem and distal cemented tibial stem appear well-fixed.
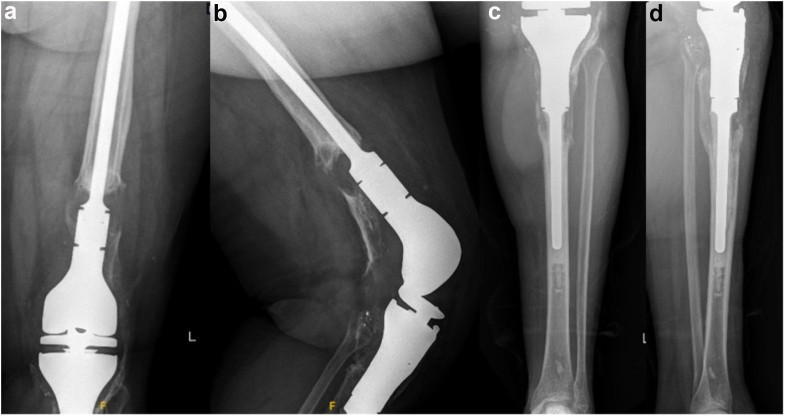
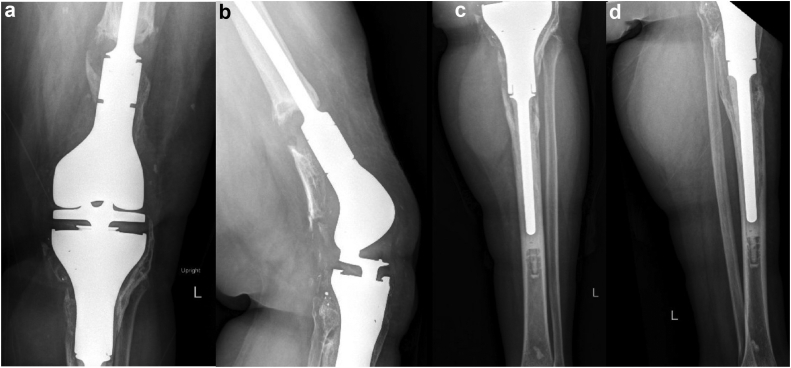
Figure 2.
(a) Left knee anterior posterior and (b) lateral x-rays 1 year prior to presentation compared to (c) left knee anterior posterior and (d) lateral x-rays 1 year later at time of presentation demonstrating severe and progressive osteolysis of the proximal tibia.
Laboratory testing demonstrated elevated inflammatory markers (erythrocyte sedimentation rate of 39 mm/hour and a C-reactive protein of 14 mg/L). Two left knee aspirations yielded brown-tinged synovial fluid with the following manual cell count results: 1) 138,679 white blood cells (WBCs), 77% neutrophils, 11% lymphocytes; 2) 8236 WBC, 62% neutrophils, 38% lymphocytes. Both cultures were negative for bacterial or fungal growth after being held for 4 weeks. Cobalt (Co), chromium (Cr), and titanium (Ti) levels were 5.3 ug/L, 1.6 ug/L, and <10 ug/L, respectively. Inflammatory markers and aspiration results were suspicious for infection, as she had 6 points based on the 2018 criteria for prosthetic hip and knee infection [13]. Given the elevated metal levels and appearance of the synovial fluid upon aspiration, there was also a suspicion for taper corrosion at one of the modular junctions of the tibial or femoral prostheses.
Treatment options were reviewed with the patient including one- and two-stage exchange arthroplasty, modular component exchange, and chronic antibiotic suppression. Given her extent of osteolysis at the distal femur and proximal tibia, there was concern for further bone loss with removal of her well-fixed stems. Consequently, it was decided to proceed with modular component exchange with extensive irrigation and debridement.
At time of surgery, there was extensive ALTR with thickening and black discoloration of the joint capsule with abundant dark brown fluid. There was also devitalized tissue, muscle necrosis, and significant bone loss of both the proximal tibia and distal femur. While there was redundant capsule from significant distension, there were no capsular or extensor mechanism defects noted. Intraoperative tissue cultures were obtained. There was no purulence or gross signs of infection. After an initial irrigation and debridement was performed, the distal femoral component was evaluated. The taper of both the femoral stem-extension piece junction and the extension piece-distal femoral component junction showed extensive corrosion (Fig. 3a and b). The femoral stem was found to be well-fixed. The femoral taper was then manually cleaned with a laparotomy pad and again analyzed to confirm its physical integrity (Fig. 4). The proximal tibia component was then disengaged from its stem. The stem’s taper was in excellent condition. The tibial stem was also tested for fixation and deemed to be well fixed.
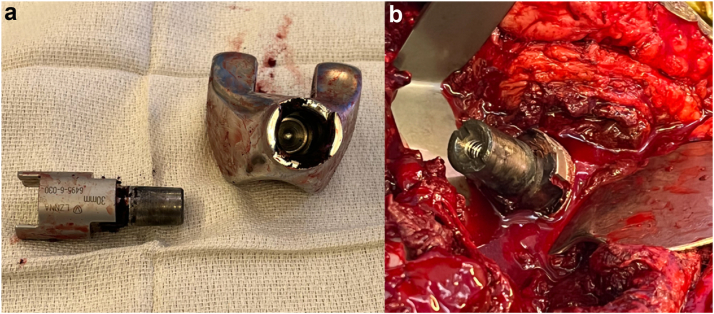
Figure 3.
(a) Intraoperative clinic photos of extensive corrosion at the male taper of the distal femur extension piece with the female taper component of the distal femur endoprosthesis and (b) the taper of the femoral stem demonstrating corrosion.
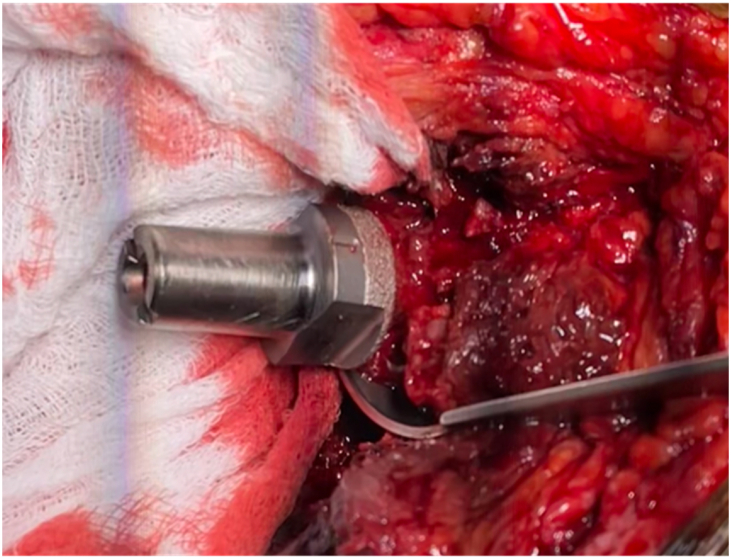
Figure 4.
The cleaned taper of the femoral stem prior to reimplantation of a new distal femur extension piece and distal femur endoprosthesis.
After extensive debridement and irrigation and using a new, uncontaminated set-up, reimplantation proceeded with new modular components. The only available femoral extension piece of appropriate size was composed of CoCr alloy. The options at this point were to reimplant a new CoCr extension piece on the taper of the cleaned Ti femoral stem or remove the femoral stem and place a new CoCr stem to limit the risk of galvanic corrosion. It was again felt that the resultant bone loss associated with stem removal would be too morbid. We therefore elected to maintain the femoral stem and reimplant a new CoCr extension piece and distal femoral prosthesis. A new proximal tibial component was placed as well.
Standing cefazolin and vancomycin were administered postoperatively while the patient was admitted. She was transitioned to oral cefadroxil for 2 weeks upon discharge. All cultures (aerobic, anaerobic, acid-fast bacteria, and fungal) were negative after being held for 4 weeks.
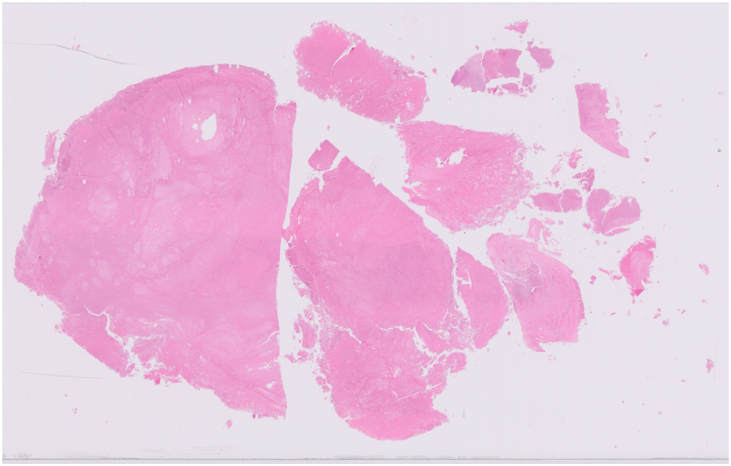
Final histopathologic evaluation of the devitalized synovium/joint capsule (Fig. 5) was performed utilizing both the Campbell and Oxford aseptic lymphocyte-dominated vasculitis-associated lesion (ALVAL) scoring systems, which resulted in a Campbell-ALVAL score of 7, indicating moderate ALVAL, and an Oxford-ALVAL semiquantitative score of 0 with no evidence of perivascular lymphocyte infiltrate but with extensive necrosis [14,15]. While there was no evidence of perivascular lymphocyte infiltration, there were dense sheets of histiocytes throughout fibrous synovial tissue.
Figure 5.
Pathology slide of the devitalized synovium/joint capsule.
The patient’s postoperative course was unremarkable, and she was most recently seen in the office 15 months postoperatively. She reported continued resolution of her left preoperative knee pain and was using a cane for ambulation. Her left knee incision was noted to be well healed. She was able to straighten her leg raise but with a 20-degree extensor lag. Radiographs from the 5- and 15-month postsurgery visits demonstrate stable, well-fixed tibial and femoral components with bone growth and remodeling, primarily of the proximal tibia (Figure 6, Figure 7). Follow-up surveillance will involve monitoring serial radiographs and patient symptoms.
Figure 6.
(a) Left knee anterior posterior and (b) lateral x-rays and (c) left tibia-fibula anterior posterior and (d) lateral x-rays from 5 months postsurgery demonstrating bone growth and remodeling, particularly at the proximal tibia, where most of the bone loss occurred.
Figure 7.
(a) Left knee anterior posterior and (b) lateral x-rays and (c) left tibia-fibula anterior posterior and (d) lateral x-rays from 15 months postsurgery demonstrating continued bone growth and remodeling.
Informed consent was obtained from the patient for publication of this case report, and the patient consented to the use of all information and imaging contained in this case report.
Discussion
In this case report, we present the rare case of ALTR secondary to taper corrosion at both the modular stem-extension piece and extension piece-distal femoral component junctions in a revision TKA with distal femur and proximal tibia endoprostheses. While ALTR secondary to corrosion at the femoral head-neck taper junction in THA has been well-described, there have been minimal reports of ALTR occurring secondary to taper corrosion in modular revision TKA and no reports of ALTR occurring secondary to taper corrosion in DFRs [[1], [2], [3], [4], [5], [6],8,9].
TKA taper junctions can be prone to corrosion similar to that seen in corrosion at the head-neck taper junction described in metal-on-polyethylene (MoP) hips [5,8,9]. Although the etiology of ALTR is still unclear, it is hypothesized that the metal ions released from corrosion create a delayed type 4 hypersensitivity reaction, which results in an ALTR [[4], [5], [6]]. The term ALVAL has been used to describe the histopathologic changes observed [4,5,14]. Histopathologic evaluation of periprosthetic tissue can be performed using the Campbell and Oxford-ALVAL scoring systems [14,15]. However, these scoring systems were initially developed to evaluate pseudotumors specifically associated with metal-on-metal hip arthroplasty [14,15].
Few studies have assessed taper corrosion in modular TKA prostheses [8,[10], [11], [12]]. Four retrieval analyses have evaluated tapers of modular TKA components undergoing revision TKA [8,[10], [11], [12]]. Up to 93% of retrieved modular TKA tapers showed mild-to-severe signs of taper corrosion [10]. Mixed metal taper junctions, conical vs threaded taper designs, and tapers with locking screws perpendicular as opposed to parallel to the taper were associated with higher corrosion scores [10,11]. Additionally, preferential corrosion of the CoCr component as compared to Ti component was observed in mixed metal junctions [11]. While corrosion occurred more frequently at the femoral junctions, the tibial junctions were more likely to have severe corrosion [8].
Although TKA taper corrosion occurs, ALTR appears to be a relatively rare manifestation in the TKA setting relative to THA [8,9]. McMaster et al. was the first to describe a case of ALTR developing from corrosion at the modular stem-femoral component taper junction in a hinged TKA prosthesis [9]. Comparably to our management, the well-fixed femoral stem was retained, and a new femoral component was implanted [9]. Our study adds to the available literature as it is only the second study discussing management of taper corrosion in modular TKA implants, and it is the first to present corrosion at the modular stem-extension piece and modular extension piece-distal femoral component taper junctions in a DFR.
It is unclear as to why ALTR with modular TKA components is a rare manifestation relative to THA. A potential theory for the THA predominance of ALTR is that, given the lower intracapsular volume of the hip joint compared to the knee, metal ions may be present at a higher relative concentration in the hip. Another potential explanation is that the micromotion at the modular head-neck taper junction in THA is greater than that in the stem-femoral component taper junction in TKA.
ALTR may also be less frequently reported after DFR, as patients receiving DFRs typically have higher comorbidity burdens, limited lifespans, and limited function [[16], [17], [18], [19]]. Christiner and Spece et al. reported associations between increased activity levels and severe taper corrosion [8,12]. Consequently, DFR patients may not live long enough or be active enough to generate significant corrosion and subsequent ALTR.
Although the workup of ALTR in MoM THA and MoP THA has been widely reported, this has not been described in TKAs [1,6]. ALTR can be difficult to discern from infection as it commonly presents with elevated inflammatory markers, synovial WBC count, and presence of purulent fluid [1,20,21]. A manual cell count is recommended when evaluating synovial fluid, as synovial WBC count may be falsely elevated when measured automatically due to metal and cellular debris [1,21,22]. Our case comparably was difficult to differentiate from infection as the patient had elevated inflammatory markers and a synovial fluid aspiration with a WBC count concerning infection. While there have been studies to aid in diagnosis of infection in the setting of failed MoM hips or in head-neck taper corrosion, there have been no studies discussing the diagnosis of infection in patients with taper corrosion in TKAs [[20], [21], [22], [23]]. Serum metal ions have been described as an initial screening test in the workup of ALTR in THA [1]. Similar to THA taper corrosion, our patient’s Co and Cr levels were elevated. Additionally, the use of metal artifact reduction sequence magnetic resonance imaging (MARS MRI) has been described in the THA literature to aid in the workup and diagnosis of ALTR [1,6]. While a MARS MRI was not obtained in this case, it can be considered during the workup of ALTR secondary to TKA taper corrosion to evaluate soft tissue quality, extensor mechanism integrity, and the presence of a pseudotumor.
The recommended treatment for ALTR secondary to TKA taper corrosion has not been described. In the THA literature, cleaning of the taper and placement of a ceramic head with titanium sleeve for the treatment of ALTR arising from taper corrosion in MoP hips have been described [1,2]. Cooper et al. described cleaning the head-neck taper with a dry laparotomy pad [2]. We extrapolated this treatment approach to our case by cleaning the taper with a laparotomy pad. A more aggressive cleaning technique with a Bovie scratch pad was not utilized due to concerns for scratching and damaging the taper. Faizan et al. performed an in vitro study to evaluate the effects of taper cleaning method on taper dimensions and surface roughness using an aggressive cleaning method with a Bovie scratch pad compared to a light cleaning method using gauze pads [24]. Tapers cleaned with the Bovie scratch pad had a decreased taper cone angle and higher surface roughness values [24].
Summary
In conclusion, corrosion at the stem-distal femoral component junction can result in ALTR in patients with DFR. It is important to consider this diagnosis when evaluating patients with knee pain following DFR. After working up for infection with erythrocyte sedimentation rate/C-reactive protein and synovial fluid analysis, it is recommended to obtain a manual synovial fluid WBC count and serum metal ion levels if ALTR is suspected. A MARS MRI can also be considered to aid in diagnosis. Treatment of this patient involved retaining a well-fixed femoral stem, manually cleaning the femoral taper with a laparotomy pad, and exchanging the modular femoral components. Management is based on taper corrosion in THA literature, as there is currently a lack of data evaluating the optimal diagnostic and treatment strategies in the TKA setting.
Conflicts of interest
D. Chen is a paid consultant for Stryker. E. Adler is a paid consultant for Stryker and Monogram Orthopedics; all other authors declare no potential conflicts of interest.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2023.101256.
Informed patient consent
The author(s) confirm that written informed consent has been obtained from the involved patient(s) or if appropriate from the parent, guardian, power of attorney of the involved patient(s); and, they have given approval for this information to be published in this case report (series).
Appendix A. Supplementary data
References
- 1.Plummer D.R., Berger R.A., Paprosky W.G., Sporer S.M., Jacobs J.J., Della Valle C.J. Diagnosis and management of adverse local tissue reactions secondary to corrosion at the head-neck junction in patients with metal on polyethylene bearings. J Arthroplasty. 2016;31:264–268. doi: 10.1016/j.arth.2015.07.039. [DOI] [PubMed] [Google Scholar]
- 2.Cooper H.J., Della Valle C.J., Berger R.A., et al. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am. 2012;94:1655. doi: 10.2106/JBJS.K.01352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cooper H.J., Urban R.M., Wixson R.L., et al. Adverse local tissue reaction arising from corrosion at the femoral neck-body junction in a dual-taper stem with a cobalt-chromium modular neck. J Bone Joint Surg Am. 2013;95:865. doi: 10.2106/JBJS.L.01042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Willert H.G., Buchhorn G.H., Fayyazi A., et al. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am. 2005;87:28–36. doi: 10.2106/JBJS.A.02039pp. [DOI] [PubMed] [Google Scholar]
- 5.Eltit F., Wang Q., Wang R. Mechanisms of adverse local tissue reactions to hip implants. Front Bioeng Biotechnol. 2019;7:176. doi: 10.3389/fbioe.2019.00176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chalmers B.P., Perry K.I., Taunton M.J., Mabry T.M., Abdel M.P. Diagnosis of adverse local tissue reactions following metal-on-metal hip arthroplasty. Curr Rev Musculoskelet Med. 2016;9:67–74. doi: 10.1007/s12178-016-9321-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sahan I., Anagnostakos K. Metallosis after knee replacement: a review. Arch Orthop Trauma Surg. 2020;140:1791–1808. doi: 10.1007/s00402-020-03560-x. [DOI] [PubMed] [Google Scholar]
- 8.Christiner T., Pabbruwe M.B., Kop A.M., Parry J., Clark G., Collopy D. Taper corrosion and adverse local tissue reactions in patients with a modular knee prosthesis. JB JS Open Access. 2018;3 doi: 10.2106/JBJS.OA.18.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McMaster W.C., Patel J. Adverse local tissue response lesion of the knee associated with Morse taper corrosion. J Arthroplasty. 2013;28:375.e5–375.e8. doi: 10.1016/j.arth.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 10.Arnholt C.M., MacDonald D.W., Tohfafarosh M., et al. Mechanically assisted taper corrosion in modular TKA. J Arthroplasty. 2014;29(Suppl):205–208. doi: 10.1016/j.arth.2013.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martin A.J., Seagers K.A., Van Citters D.W. Assessment of corrosion, fretting and material loss of retrieved modular total knee arthroplasties. J Arthroplasty. 2017;32:2279–2284. doi: 10.1016/j.arth.2017.02.047. [DOI] [PubMed] [Google Scholar]
- 12.Spece H., Underwood R.J., Baykal D., et al. Is there material loss at the conical junctions of modular components for total knee arthroplasty? J Arthroplasty. 2019;34:2479–2486. doi: 10.1016/j.arth.2019.05.030. [DOI] [PubMed] [Google Scholar]
- 13.Parvizi J., Tan T.L., Goswami K., et al. The 2018 definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. J Arthroplasty. 2018;33:1309–1314. doi: 10.1016/j.arth.2018.02.078. [DOI] [PubMed] [Google Scholar]
- 14.Campbell P., Ebramsadeh E., Nelson S., et al. Histological features of pseudotumor-like tissues from metal-on-metal hips. Clin Orthop. 2010;468:2321–2327. doi: 10.1007/s11999-010-1372-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grammatopoulos P., Pandit H., Kamali A., et al. The correlation of wear with histological features after failed hip resurfacing arthroplasty. J Bone Joint Surg Am. 2013;95:e81. doi: 10.2106/JBJS.L.00775. [DOI] [PubMed] [Google Scholar]
- 16.Kim K.I., Egol K.A., Hozack W.J., Parvizi J. Periprosthetic fractures after total knee arthroplasties. Clin Orthop Relat Res. 2006;446:167–175. doi: 10.1097/01.blo.0000214417.29335.19. [DOI] [PubMed] [Google Scholar]
- 17.Choong P.F., Sim F.H., Pritchard D.J., Rock M.G., Chao E.Y. Megaprostheses after resection of distal femoral tumors. A rotating hinge design in 30 patients followed for 2-7 years. Acta Orthop Scand. 1996;67:345–351. doi: 10.3109/17453679609002328. [DOI] [PubMed] [Google Scholar]
- 18.Obinna O.H., Uchenna K.A. Distal femoral replacement in complex revision knee arthroplasty. Niger Postgrad Med J. 2020;27:143–146. doi: 10.4103/npmj.npmj_140_19. [DOI] [PubMed] [Google Scholar]
- 19.Onubogu I.K., Relwani S., Grewal U.S., Bhamra J.S., Reddy K.G., Dhinsa B.S. Distal femoral replacement as a primary treatment method for distal femoral fractures in the Elderly. Cureus. 2021;13 doi: 10.7759/cureus.18752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mikhael M.M., Hanssen A.D., Sierra R.J. Failure of metal-on-metal total hip arthroplasty mimicking hip infection. A report of two cases. J Bone Joint Surg Am. 2009;91:443–446. doi: 10.2106/JBJS.H.00603. [DOI] [PubMed] [Google Scholar]
- 21.Yi P.H., Cross M.B., Moric M., et al. Do serologic and synovial tests help diagnose infection in revision hip arthroplasty with metal-on-metal bearings or corrosion? Clin Orthop Relat Res. 2015;473:498–505. doi: 10.1007/s11999-014-3902-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wyles C.C., Larson D.R., Houdek M.T., Sierra R.J., Trousdale R.T. Utility of synovial fluid aspirations in failed metal-on-metal total hip arthroplasty. J Arthroplasty. 2013;28:818–823. doi: 10.1016/j.arth.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 23.Okroj K.T., Calkins T.E., Kayupov E., et al. The alpha-defensin test for diagnosing periprosthetic joint infection in the setting of an adverse local tissue reaction secondary to a failed metal-on-metal bearing or corrosion at the head-neck junction. J Arthroplasty. 2018;33:1896–1898. doi: 10.1016/j.arth.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 24.Faizan A., Longaray J., Nevelos J.E., Westrich G.H. Effects of corrosion and cleaning method on taper dimensions: an in vitro investigation. Hip Int. 2020;30:87–92. doi: 10.1177/1120700018825448. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.